Professional Documents
Culture Documents
Praise Poster Identifying The Neural Signature of Motivation For Exercise
Praise Poster Identifying The Neural Signature of Motivation For Exercise
Uploaded by
api-296220851Copyright:
Available Formats
You might also like
- Positional Release Therapy Asseement and Treatment PDFDocument269 pagesPositional Release Therapy Asseement and Treatment PDFDiana Iuliana Petcu86% (7)
- Super Brain by Deepak Chopra and Rudolph E Tanzi - ExcerptDocument18 pagesSuper Brain by Deepak Chopra and Rudolph E Tanzi - ExcerptCrown Publishing Group75% (12)
- Materi PIR - Dr. Norhayati Hussein, MD, Physiatrist Potential Rehabiliation Strategies To Enhance Neuroplasticy Regeneration in Movement RecoveryDocument38 pagesMateri PIR - Dr. Norhayati Hussein, MD, Physiatrist Potential Rehabiliation Strategies To Enhance Neuroplasticy Regeneration in Movement RecoveryGhea Putri HendrianiNo ratings yet
- Deep Brain StimulationDocument54 pagesDeep Brain StimulationNarinder AroraNo ratings yet
- Neurosciences Advances and Physiotherapy in Neurological Conditions - No PreloDocument20 pagesNeurosciences Advances and Physiotherapy in Neurological Conditions - No PreloSM199021No ratings yet
- NDT FinalDocument8 pagesNDT Finalapi-228136529No ratings yet
- Answers H Lzel WorkbookDocument6 pagesAnswers H Lzel WorkbookhaulatamirNo ratings yet
- Evidence Based TableDocument13 pagesEvidence Based Tableneometal_86No ratings yet
- Neuromodulación No Invasiva para Potenciar La Rehabilitación de La Heminegligencia Tras Un IctusDocument1 pageNeuromodulación No Invasiva para Potenciar La Rehabilitación de La Heminegligencia Tras Un IctusRed Menni de Daño CerebralNo ratings yet
- Journal Pone 0286443Document14 pagesJournal Pone 0286443aliuaishangaduNo ratings yet
- Psychology of Sport & Exercise: Nicola J. Robinson, Catharine Montgomery, Laura Swettenham, Amy WhiteheadDocument12 pagesPsychology of Sport & Exercise: Nicola J. Robinson, Catharine Montgomery, Laura Swettenham, Amy WhiteheadSanghita BiswasNo ratings yet
- Cat 2Document7 pagesCat 2api-301127234No ratings yet
- Origins of Theoretical ApproachDocument15 pagesOrigins of Theoretical ApproachnrusinghNo ratings yet
- Dodge - Symposium MCI 2014 V5Document33 pagesDodge - Symposium MCI 2014 V5WorldEventsForumNo ratings yet
- PNF 6 Proprioceptive Neuromuscular Facilitation (PNF) vs. Task Specific TrainingDocument6 pagesPNF 6 Proprioceptive Neuromuscular Facilitation (PNF) vs. Task Specific TrainingAnonymous j0xAgHs3No ratings yet
- Jpts 27 673Document4 pagesJpts 27 673Lazlo SecretNo ratings yet
- 3 Examination and Evaluation in Neuromuscular Disorders - Lifespan Neurorehabilitation 2018Document20 pages3 Examination and Evaluation in Neuromuscular Disorders - Lifespan Neurorehabilitation 2018Abi Dennise Nahuelpán LienlafNo ratings yet
- Bobath Approach NotesDocument5 pagesBobath Approach NotesJuling Perales100% (3)
- ApproachDocument37 pagesApproachAshu AshNo ratings yet
- Psychology of Sport and Exercise: Christopher Ring, Andrew Cooke, Maria Kavussanu, David Mcintyre, Rich MastersDocument10 pagesPsychology of Sport and Exercise: Christopher Ring, Andrew Cooke, Maria Kavussanu, David Mcintyre, Rich MastersjcurazanNo ratings yet
- Mini Mental State Examination Cognitive FIM Instrument and The Loewenstein Occupational Therapy Cognitive Assessment Relation To Functional Outco PDFDocument4 pagesMini Mental State Examination Cognitive FIM Instrument and The Loewenstein Occupational Therapy Cognitive Assessment Relation To Functional Outco PDFDamira HalilovicNo ratings yet
- Physiotherapy Based On Problem Solving in Upper Limb Function and Neuroplasticity in Chronic Stroke Patients: A Case SeriesDocument9 pagesPhysiotherapy Based On Problem Solving in Upper Limb Function and Neuroplasticity in Chronic Stroke Patients: A Case SeriesAlfredo TovarNo ratings yet
- The Stroke Recovery TimelineDocument15 pagesThe Stroke Recovery TimelineLucia NatashaNo ratings yet
- Attention Process TrainingDocument22 pagesAttention Process TrainingLara Perez MurciaNo ratings yet
- Neurodevelopmental Treatment (NDT) in Paediatrics: Victoria Prooday Manuela Ocrainschi Alda MeloDocument36 pagesNeurodevelopmental Treatment (NDT) in Paediatrics: Victoria Prooday Manuela Ocrainschi Alda MeloDnyanesh Patil100% (1)
- A Retrospective Study of Predictors of Return To DutyDocument12 pagesA Retrospective Study of Predictors of Return To Dutyunge.victoriaNo ratings yet
- Meditation Improves Self-Regulation Over The Life SpanDocument8 pagesMeditation Improves Self-Regulation Over The Life SpanMichael MooreNo ratings yet
- Nihms 645411Document13 pagesNihms 645411sampathNo ratings yet
- Jurnal InternasionalDocument7 pagesJurnal Internasional34. Putu Mariska Abdi CahyaniNo ratings yet
- Effects of Mental Imagery Technique in Addition To Conventional Physical Therapy To Improve Hand Functions in Chronic Stroke PatientDocument7 pagesEffects of Mental Imagery Technique in Addition To Conventional Physical Therapy To Improve Hand Functions in Chronic Stroke PatientMuhajir AjiNo ratings yet
- Sharp Brains Checklist - 10 Questions To Choose The Right Brain Fitness Program For YouDocument1 pageSharp Brains Checklist - 10 Questions To Choose The Right Brain Fitness Program For YouchlscNo ratings yet
- Psychophysiological assessment of human cognition and its enhancement by a non-invasive methodFrom EverandPsychophysiological assessment of human cognition and its enhancement by a non-invasive methodNo ratings yet
- Dodge Symposium MCI 2014 V7 LatestDocument34 pagesDodge Symposium MCI 2014 V7 LatestWorldEventsForumNo ratings yet
- AuthorDocument10 pagesAuthorQianqian FanNo ratings yet
- 23 - Functional Training and Advanced RehabilitationDocument21 pages23 - Functional Training and Advanced RehabilitationCarlos GarciaNo ratings yet
- Piis0007091217349061 2Document6 pagesPiis0007091217349061 2Ana Belén Artero CastañoNo ratings yet
- Phe PPR ReportDocument11 pagesPhe PPR ReportadarazaaraNo ratings yet
- Effectiveness of Neurobic Exercise in Improving Cognition in Young Individuals - February - 2020 - 1580738309 - 1931195Document2 pagesEffectiveness of Neurobic Exercise in Improving Cognition in Young Individuals - February - 2020 - 1580738309 - 1931195Zalinah Mohd YusofNo ratings yet
- Part One: and Practical Aspects of TestingDocument22 pagesPart One: and Practical Aspects of TestingCIK FATHINNo ratings yet
- Statistical Procedures For Determining The Extent of Cognitive Change Following ConcussionDocument7 pagesStatistical Procedures For Determining The Extent of Cognitive Change Following Concussionpsyquis2No ratings yet
- Early Sitting, Standing, and Walking in Conjunction With Contemporary Bobath Approach For Stroke Patients With Severe Motor Defi CitDocument8 pagesEarly Sitting, Standing, and Walking in Conjunction With Contemporary Bobath Approach For Stroke Patients With Severe Motor Defi CitCarlos LunaNo ratings yet
- Occupational Performance Coaching For Stroke Survivors A PilotDocument7 pagesOccupational Performance Coaching For Stroke Survivors A PilotEtneciv ParedesNo ratings yet
- José Afonso, Filipe Manuel Clemente, Fábio Yuzo Nakamura, Pedro Morouço, Hugo Sarmento, Richard A. Inman and Rodrigo Ramirez-CampilloDocument25 pagesJosé Afonso, Filipe Manuel Clemente, Fábio Yuzo Nakamura, Pedro Morouço, Hugo Sarmento, Richard A. Inman and Rodrigo Ramirez-CampilloJOSÁRIA FERRAZ AMARALNo ratings yet
- Mechanism of Integrative Body-Mind Training: Neuroscience Bulletin December 2011Document7 pagesMechanism of Integrative Body-Mind Training: Neuroscience Bulletin December 2011juanNo ratings yet
- Parkinson e ExercicioDocument9 pagesParkinson e ExercicioMariana CastroNo ratings yet
- Attentional Concentration During Physiotherapeutic Intervention Improves Gait and Trunk Control in Patients With StrokeDocument5 pagesAttentional Concentration During Physiotherapeutic Intervention Improves Gait and Trunk Control in Patients With StrokeEsterGrefielNo ratings yet
- Sleep Restriction Therapy PDFDocument37 pagesSleep Restriction Therapy PDFFenyNo ratings yet
- Needs Assessment For Holistic Health Providers Using Movement As MedicineDocument10 pagesNeeds Assessment For Holistic Health Providers Using Movement As Medicineapi-399928223No ratings yet
- PT in Head InjuryDocument33 pagesPT in Head InjuryArko duttaNo ratings yet
- General Internal Medicine - 2004 - LeeDocument6 pagesGeneral Internal Medicine - 2004 - LeeHenry CogoNo ratings yet
- 2021 - Yang B. & Wang S. - Meta-Analysis On Cognitive Benefit of Exercice After StrokeDocument12 pages2021 - Yang B. & Wang S. - Meta-Analysis On Cognitive Benefit of Exercice After Strokerichard LemieuxNo ratings yet
- Holzel Et Al 2Document20 pagesHolzel Et Al 2jlawrenceNo ratings yet
- Standards of Practice for Neurofeedback and NeurotDocument12 pagesStandards of Practice for Neurofeedback and NeurotSubrat SahooNo ratings yet
- Review: Strategies For Stroke RehabilitationDocument9 pagesReview: Strategies For Stroke RehabilitationElias VillalonNo ratings yet
- Jde Ding RCB T ManualDocument18 pagesJde Ding RCB T ManualLinNo ratings yet
- Co NFB+Course+Outline+2019Document7 pagesCo NFB+Course+Outline+2019Thomas MartiNo ratings yet
- 3mbwt Inservice Presentation-SawleDocument40 pages3mbwt Inservice Presentation-Sawleapi-623462188No ratings yet
- Optimizing Microsurgical Skills With EEG NeurofeedbackDocument11 pagesOptimizing Microsurgical Skills With EEG NeurofeedbackgenerjustnNo ratings yet
- Neuro Developmental Treatment (NDT) Techniques: HistoryDocument3 pagesNeuro Developmental Treatment (NDT) Techniques: HistoryGafencu SergiuNo ratings yet
- Effect of Repetition Duration During Resistance Training On Muscle Hypertrophy: A Systematic Review and Meta-AnalysisDocument10 pagesEffect of Repetition Duration During Resistance Training On Muscle Hypertrophy: A Systematic Review and Meta-AnalysisrobinsonNo ratings yet
- Functional Rehabilitation of Some Common Neurological Conditions: A Physical Management Strategy to Optimise Functional Activity LevelFrom EverandFunctional Rehabilitation of Some Common Neurological Conditions: A Physical Management Strategy to Optimise Functional Activity LevelNo ratings yet
- Journal of Thoracic Oncology Volume Issue 2016Document30 pagesJournal of Thoracic Oncology Volume Issue 2016Daniela RoaNo ratings yet
- The 4 Phases of Cardiac RehabilitationDocument3 pagesThe 4 Phases of Cardiac RehabilitationStepyn SalvadorNo ratings yet
- Labor Cases 7Document112 pagesLabor Cases 7MaryStefanieNo ratings yet
- Jurnal CopdDocument11 pagesJurnal Copdgemarawan abadiNo ratings yet
- Health Care Communication 2Document45 pagesHealth Care Communication 2Holy DishNo ratings yet
- 2012-08-09 The County TimesDocument40 pages2012-08-09 The County TimesSouthern Maryland OnlineNo ratings yet
- InterestDocument16 pagesInterestmohanaaprkash100% (1)
- Springer: Tokyo Berlin Heidelberg New York Barcelona Budapest Hong Kong London Milan Paris Santaclara SingaporeDocument153 pagesSpringer: Tokyo Berlin Heidelberg New York Barcelona Budapest Hong Kong London Milan Paris Santaclara SingaporeCarlos EsescritorNo ratings yet
- Clinical Outcomes of Rehabilitation For Patients Following Lateral Patellar Dislocation: A Systematic ReviewDocument13 pagesClinical Outcomes of Rehabilitation For Patients Following Lateral Patellar Dislocation: A Systematic ReviewHarshoi KrishannaNo ratings yet
- Crabtales 066Document20 pagesCrabtales 066Crab Tales100% (1)
- Lesson 1: Planning For Heath Promotion, Health Maintenance, and Home Health Consideration in The Older AdultDocument6 pagesLesson 1: Planning For Heath Promotion, Health Maintenance, and Home Health Consideration in The Older AdultCzeremar Chan0% (1)
- Telehealth in Occupational Therapy: AOTA Position PaperDocument18 pagesTelehealth in Occupational Therapy: AOTA Position PaperdanielNo ratings yet
- Wellness CenterDocument6 pagesWellness CenterMuntasir SizanNo ratings yet
- Mot SyllabusDocument30 pagesMot SyllabusShanthoshini Baskaran100% (1)
- Holland CodeDocument5 pagesHolland CodeAlisha RohdeNo ratings yet
- Examining The Efficacy of Dance Movement and Music Mixed Treatment On Social Communication Impairment in Children With Autism - Based On Family Parent-Child SituationDocument10 pagesExamining The Efficacy of Dance Movement and Music Mixed Treatment On Social Communication Impairment in Children With Autism - Based On Family Parent-Child Situation賴莙儒No ratings yet
- Occupational Therapy ResumeDocument6 pagesOccupational Therapy Resumeqozthnwhf100% (1)
- Alternative Approaches in The Special EducationDocument11 pagesAlternative Approaches in The Special EducationKiriakos Kiritsopoulos100% (1)
- Major Injury Case Study - Below Knee AmputationDocument2 pagesMajor Injury Case Study - Below Knee AmputationQBE European Operations Risk ManagementNo ratings yet
- ST ND RDDocument20 pagesST ND RDVenkatesh SadasivuniNo ratings yet
- Protocoale Sold ComparativDocument8 pagesProtocoale Sold ComparativLilianaNo ratings yet
- HPCZ Application FormDocument11 pagesHPCZ Application FormQualis LabsNo ratings yet
- Daftar PustakaDocument2 pagesDaftar Pustakadi.yulianiNo ratings yet
- How To Write A SOAP Note-3-10Document2 pagesHow To Write A SOAP Note-3-10mohamed_musaferNo ratings yet
- Low Back Pain Case Study - A Nasty One! But A Good Outcome. - Witty, Pask & BuckinghamDocument4 pagesLow Back Pain Case Study - A Nasty One! But A Good Outcome. - Witty, Pask & BuckinghamermanmahendraNo ratings yet
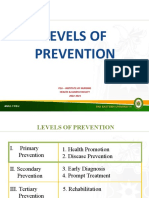
- Module 4 Levels of PreventionDocument29 pagesModule 4 Levels of PreventionZaren James D. RacaNo ratings yet
- Models of Rehabilitation Component IA Role Name Affiliation: Swe/Swfd/Mr/M23 by Dr. P. Saleel KumarDocument13 pagesModels of Rehabilitation Component IA Role Name Affiliation: Swe/Swfd/Mr/M23 by Dr. P. Saleel KumarRainbowsNo ratings yet
- Strain Counter-Strain PDFDocument7 pagesStrain Counter-Strain PDFCarlosCarpinteroRubioNo ratings yet
Praise Poster Identifying The Neural Signature of Motivation For Exercise
Praise Poster Identifying The Neural Signature of Motivation For Exercise
Uploaded by
api-296220851Original Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Praise Poster Identifying The Neural Signature of Motivation For Exercise
Praise Poster Identifying The Neural Signature of Motivation For Exercise
Uploaded by
api-296220851Copyright:
Available Formats
Identifying the Neural Signature of Motivation for Exercise
Kaitlyn Bigner BS, SPT; Jenna Calvelage BS, SPT; Sarah Doren BS, SPT; Katie Preston BS, SPT; Pierce Boyne PT, DPT, PhD, NCS
College of Allied Health Sciences, Department of Rehabilitation, Exercise and Nutrition Sciences
BACKGROUND RESULTS / DISCUSSION
• Motivation is critical for rehabilitation because it likely improves exercise adherence, • As expected,5 motor regions (M1-LL, SMA, PMd) were
rehabilitation engagement and community participation, leading to better recovery1 active during gait
• However, it is difficult to measure, as current methods rely on subjective questionnaires1,2
• Understanding the neural underpinnings of motivation could: • Several cortical regions were more active with extra
• Provide a more objective and reliable measure of motivation motivation (or showed trends in that direction)
• Uncover unconscious aspects of motivation that are not captured by questionnaires • Possible mechanism explaining positive effects of
• Better predict those who may respond positively to rehabilitation3 motivational feedback on locomotor
• Inform targeted brain stimulation intervention to improve motivation rehabilitation6
• Identify the need for targeted behavioral intervention to supplement physical rehab
• No previous studies have measured neural activity related to motivation during exercise • SFG/ACC and DLPFC seemed the most specifically
• The purpose of this study was to determine brain regions that are upregulated during periods of related to motivation
higher motivation while performing physical activity • Minimal activity with standard trials
• SFG/ACC had highest activation and earliest
onset with extra motivation (Fig 6).
METHODS • Recent MRI research has also suggested the
SFG/ACC may be involved with motivation for
• Functional Near-Infrared Spectroscopy (fNIRS) uses light to measure changes in brain activity. physical activity.7
• Healthy adults performed a single-visit, walking experiment with fNIRS:
• 20 trials of maximal speed walking, 20 feet x 4 per trial, with 20 seconds of standing rest
between trials
• Walking bursts randomized as either:
• Extra Motivation: lap timer, tracked best lap time, verbal encouragement
• Standard: no external feedback
• Oxygenated hemoglobin (HbO2) response was measured from brain regions of interest (Fig 1), Fig 6: Select HbO2 time courses during walking trials
compared between conditions and averaged across participants using multi-level general linear
modeling.4
SFG/
ACC
M1_LL
Figure 1: Brain Montage Figure 2: fNIRS set-up Figure 3: Walking trial
RESULTS
DLPFC
Standard Trials vs rest Extra-Motivation vs Standard
Region of Interest T-value P-value T-value P-value
SFG/ACC 1.81 0.11 2.02 0.08
M1_LL 3.10 0.01 4.38 0.002
SMA 3.56 0.007 1.67 0.13 • Limitations:
PMD 2.86 0.02 4.07 0.004 • Small sample size
• Difficult to determine independent effects of
aPFC 3.23 0.01 8.46 <0.001
each brain region
DLPFC 0.21 0.84 1.55 0.14
• Future research should test different motivation
Fig 4. Fig 5. conditions, longitudinal outcomes and effects of brain
stimulation
REFERENCES
• [1] Frederick CM, Morrison C, Manning T. Motivation to participate, exercise affect, and outcome behaviors toward physical activity.
Percept Mot Skills. 1996 Apr;82(2):691-701. doi: 10.2466/pms.1996.82.2.691. PMID: 8724948.
• [2] Mahony R, Blake C, Matthews J, Donnoghue GO, Cunningham C. Physical activity levels and self-determined motivation among
future healthcare professionals: Utility of the Behavioral Regulation in Exercise Questionnaire (BREQ-2). Physiother Theory Pract.
2019;35(9):884-890. doi:10.1080/09593985.2018.1457112]
• [3] Thilarajah S, Bower KJ, Pua Y-H, et al. Modifiable Factors Associated With Poststroke Physical Activity at Discharge From
Rehabilitation: Prospective Cohort Study. Physical Therapy. 2020;100(5):818-828. doi:10.1093/ptj/pzaa022
• [4] Santosa H, Zhal X, Fishburn F, Huppert T. The NIRS Brain AnalyzIR Toolbox. Algorithms. 2018;11(5):73.
• [5] Miyai I, Tanabe HC, Sase I, et al. Cortical Mapping of Gait in Humans: A Near-Infrared Spectroscopic Topography Study. NeuroImage.
2001;14(5):1186-1192. doi:10.1006/nimg.2001.0905
• [6] Dobkin BH, Plummer-D'Amato P, Elashoff R, Lee J; SIRROWS Group. International randomized clinical trial, stroke inpatient
rehabilitation with reinforcement of walking speed (SIRROWS), improves outcomes. Neurorehabil Neural Repair. 2010;24(3):235-242.
• Sample: 5 healthy adults (4 females; mean age 26.2±5.5) • [7] Boyne P, Maloney T, DiFrancesco M, et al. Resting-state functional connectivity of subcortical locomotor centers explains variance in
walking capacity. Human Brain Mapping. 2018;39(12):4831-4843. doi:10.1002/hbm.2432
You might also like
- Positional Release Therapy Asseement and Treatment PDFDocument269 pagesPositional Release Therapy Asseement and Treatment PDFDiana Iuliana Petcu86% (7)
- Super Brain by Deepak Chopra and Rudolph E Tanzi - ExcerptDocument18 pagesSuper Brain by Deepak Chopra and Rudolph E Tanzi - ExcerptCrown Publishing Group75% (12)
- Materi PIR - Dr. Norhayati Hussein, MD, Physiatrist Potential Rehabiliation Strategies To Enhance Neuroplasticy Regeneration in Movement RecoveryDocument38 pagesMateri PIR - Dr. Norhayati Hussein, MD, Physiatrist Potential Rehabiliation Strategies To Enhance Neuroplasticy Regeneration in Movement RecoveryGhea Putri HendrianiNo ratings yet
- Deep Brain StimulationDocument54 pagesDeep Brain StimulationNarinder AroraNo ratings yet
- Neurosciences Advances and Physiotherapy in Neurological Conditions - No PreloDocument20 pagesNeurosciences Advances and Physiotherapy in Neurological Conditions - No PreloSM199021No ratings yet
- NDT FinalDocument8 pagesNDT Finalapi-228136529No ratings yet
- Answers H Lzel WorkbookDocument6 pagesAnswers H Lzel WorkbookhaulatamirNo ratings yet
- Evidence Based TableDocument13 pagesEvidence Based Tableneometal_86No ratings yet
- Neuromodulación No Invasiva para Potenciar La Rehabilitación de La Heminegligencia Tras Un IctusDocument1 pageNeuromodulación No Invasiva para Potenciar La Rehabilitación de La Heminegligencia Tras Un IctusRed Menni de Daño CerebralNo ratings yet
- Journal Pone 0286443Document14 pagesJournal Pone 0286443aliuaishangaduNo ratings yet
- Psychology of Sport & Exercise: Nicola J. Robinson, Catharine Montgomery, Laura Swettenham, Amy WhiteheadDocument12 pagesPsychology of Sport & Exercise: Nicola J. Robinson, Catharine Montgomery, Laura Swettenham, Amy WhiteheadSanghita BiswasNo ratings yet
- Cat 2Document7 pagesCat 2api-301127234No ratings yet
- Origins of Theoretical ApproachDocument15 pagesOrigins of Theoretical ApproachnrusinghNo ratings yet
- Dodge - Symposium MCI 2014 V5Document33 pagesDodge - Symposium MCI 2014 V5WorldEventsForumNo ratings yet
- PNF 6 Proprioceptive Neuromuscular Facilitation (PNF) vs. Task Specific TrainingDocument6 pagesPNF 6 Proprioceptive Neuromuscular Facilitation (PNF) vs. Task Specific TrainingAnonymous j0xAgHs3No ratings yet
- Jpts 27 673Document4 pagesJpts 27 673Lazlo SecretNo ratings yet
- 3 Examination and Evaluation in Neuromuscular Disorders - Lifespan Neurorehabilitation 2018Document20 pages3 Examination and Evaluation in Neuromuscular Disorders - Lifespan Neurorehabilitation 2018Abi Dennise Nahuelpán LienlafNo ratings yet
- Bobath Approach NotesDocument5 pagesBobath Approach NotesJuling Perales100% (3)
- ApproachDocument37 pagesApproachAshu AshNo ratings yet
- Psychology of Sport and Exercise: Christopher Ring, Andrew Cooke, Maria Kavussanu, David Mcintyre, Rich MastersDocument10 pagesPsychology of Sport and Exercise: Christopher Ring, Andrew Cooke, Maria Kavussanu, David Mcintyre, Rich MastersjcurazanNo ratings yet
- Mini Mental State Examination Cognitive FIM Instrument and The Loewenstein Occupational Therapy Cognitive Assessment Relation To Functional Outco PDFDocument4 pagesMini Mental State Examination Cognitive FIM Instrument and The Loewenstein Occupational Therapy Cognitive Assessment Relation To Functional Outco PDFDamira HalilovicNo ratings yet
- Physiotherapy Based On Problem Solving in Upper Limb Function and Neuroplasticity in Chronic Stroke Patients: A Case SeriesDocument9 pagesPhysiotherapy Based On Problem Solving in Upper Limb Function and Neuroplasticity in Chronic Stroke Patients: A Case SeriesAlfredo TovarNo ratings yet
- The Stroke Recovery TimelineDocument15 pagesThe Stroke Recovery TimelineLucia NatashaNo ratings yet
- Attention Process TrainingDocument22 pagesAttention Process TrainingLara Perez MurciaNo ratings yet
- Neurodevelopmental Treatment (NDT) in Paediatrics: Victoria Prooday Manuela Ocrainschi Alda MeloDocument36 pagesNeurodevelopmental Treatment (NDT) in Paediatrics: Victoria Prooday Manuela Ocrainschi Alda MeloDnyanesh Patil100% (1)
- A Retrospective Study of Predictors of Return To DutyDocument12 pagesA Retrospective Study of Predictors of Return To Dutyunge.victoriaNo ratings yet
- Meditation Improves Self-Regulation Over The Life SpanDocument8 pagesMeditation Improves Self-Regulation Over The Life SpanMichael MooreNo ratings yet
- Nihms 645411Document13 pagesNihms 645411sampathNo ratings yet
- Jurnal InternasionalDocument7 pagesJurnal Internasional34. Putu Mariska Abdi CahyaniNo ratings yet
- Effects of Mental Imagery Technique in Addition To Conventional Physical Therapy To Improve Hand Functions in Chronic Stroke PatientDocument7 pagesEffects of Mental Imagery Technique in Addition To Conventional Physical Therapy To Improve Hand Functions in Chronic Stroke PatientMuhajir AjiNo ratings yet
- Sharp Brains Checklist - 10 Questions To Choose The Right Brain Fitness Program For YouDocument1 pageSharp Brains Checklist - 10 Questions To Choose The Right Brain Fitness Program For YouchlscNo ratings yet
- Psychophysiological assessment of human cognition and its enhancement by a non-invasive methodFrom EverandPsychophysiological assessment of human cognition and its enhancement by a non-invasive methodNo ratings yet
- Dodge Symposium MCI 2014 V7 LatestDocument34 pagesDodge Symposium MCI 2014 V7 LatestWorldEventsForumNo ratings yet
- AuthorDocument10 pagesAuthorQianqian FanNo ratings yet
- 23 - Functional Training and Advanced RehabilitationDocument21 pages23 - Functional Training and Advanced RehabilitationCarlos GarciaNo ratings yet
- Piis0007091217349061 2Document6 pagesPiis0007091217349061 2Ana Belén Artero CastañoNo ratings yet
- Phe PPR ReportDocument11 pagesPhe PPR ReportadarazaaraNo ratings yet
- Effectiveness of Neurobic Exercise in Improving Cognition in Young Individuals - February - 2020 - 1580738309 - 1931195Document2 pagesEffectiveness of Neurobic Exercise in Improving Cognition in Young Individuals - February - 2020 - 1580738309 - 1931195Zalinah Mohd YusofNo ratings yet
- Part One: and Practical Aspects of TestingDocument22 pagesPart One: and Practical Aspects of TestingCIK FATHINNo ratings yet
- Statistical Procedures For Determining The Extent of Cognitive Change Following ConcussionDocument7 pagesStatistical Procedures For Determining The Extent of Cognitive Change Following Concussionpsyquis2No ratings yet
- Early Sitting, Standing, and Walking in Conjunction With Contemporary Bobath Approach For Stroke Patients With Severe Motor Defi CitDocument8 pagesEarly Sitting, Standing, and Walking in Conjunction With Contemporary Bobath Approach For Stroke Patients With Severe Motor Defi CitCarlos LunaNo ratings yet
- Occupational Performance Coaching For Stroke Survivors A PilotDocument7 pagesOccupational Performance Coaching For Stroke Survivors A PilotEtneciv ParedesNo ratings yet
- José Afonso, Filipe Manuel Clemente, Fábio Yuzo Nakamura, Pedro Morouço, Hugo Sarmento, Richard A. Inman and Rodrigo Ramirez-CampilloDocument25 pagesJosé Afonso, Filipe Manuel Clemente, Fábio Yuzo Nakamura, Pedro Morouço, Hugo Sarmento, Richard A. Inman and Rodrigo Ramirez-CampilloJOSÁRIA FERRAZ AMARALNo ratings yet
- Mechanism of Integrative Body-Mind Training: Neuroscience Bulletin December 2011Document7 pagesMechanism of Integrative Body-Mind Training: Neuroscience Bulletin December 2011juanNo ratings yet
- Parkinson e ExercicioDocument9 pagesParkinson e ExercicioMariana CastroNo ratings yet
- Attentional Concentration During Physiotherapeutic Intervention Improves Gait and Trunk Control in Patients With StrokeDocument5 pagesAttentional Concentration During Physiotherapeutic Intervention Improves Gait and Trunk Control in Patients With StrokeEsterGrefielNo ratings yet
- Sleep Restriction Therapy PDFDocument37 pagesSleep Restriction Therapy PDFFenyNo ratings yet
- Needs Assessment For Holistic Health Providers Using Movement As MedicineDocument10 pagesNeeds Assessment For Holistic Health Providers Using Movement As Medicineapi-399928223No ratings yet
- PT in Head InjuryDocument33 pagesPT in Head InjuryArko duttaNo ratings yet
- General Internal Medicine - 2004 - LeeDocument6 pagesGeneral Internal Medicine - 2004 - LeeHenry CogoNo ratings yet
- 2021 - Yang B. & Wang S. - Meta-Analysis On Cognitive Benefit of Exercice After StrokeDocument12 pages2021 - Yang B. & Wang S. - Meta-Analysis On Cognitive Benefit of Exercice After Strokerichard LemieuxNo ratings yet
- Holzel Et Al 2Document20 pagesHolzel Et Al 2jlawrenceNo ratings yet
- Standards of Practice for Neurofeedback and NeurotDocument12 pagesStandards of Practice for Neurofeedback and NeurotSubrat SahooNo ratings yet
- Review: Strategies For Stroke RehabilitationDocument9 pagesReview: Strategies For Stroke RehabilitationElias VillalonNo ratings yet
- Jde Ding RCB T ManualDocument18 pagesJde Ding RCB T ManualLinNo ratings yet
- Co NFB+Course+Outline+2019Document7 pagesCo NFB+Course+Outline+2019Thomas MartiNo ratings yet
- 3mbwt Inservice Presentation-SawleDocument40 pages3mbwt Inservice Presentation-Sawleapi-623462188No ratings yet
- Optimizing Microsurgical Skills With EEG NeurofeedbackDocument11 pagesOptimizing Microsurgical Skills With EEG NeurofeedbackgenerjustnNo ratings yet
- Neuro Developmental Treatment (NDT) Techniques: HistoryDocument3 pagesNeuro Developmental Treatment (NDT) Techniques: HistoryGafencu SergiuNo ratings yet
- Effect of Repetition Duration During Resistance Training On Muscle Hypertrophy: A Systematic Review and Meta-AnalysisDocument10 pagesEffect of Repetition Duration During Resistance Training On Muscle Hypertrophy: A Systematic Review and Meta-AnalysisrobinsonNo ratings yet
- Functional Rehabilitation of Some Common Neurological Conditions: A Physical Management Strategy to Optimise Functional Activity LevelFrom EverandFunctional Rehabilitation of Some Common Neurological Conditions: A Physical Management Strategy to Optimise Functional Activity LevelNo ratings yet
- Journal of Thoracic Oncology Volume Issue 2016Document30 pagesJournal of Thoracic Oncology Volume Issue 2016Daniela RoaNo ratings yet
- The 4 Phases of Cardiac RehabilitationDocument3 pagesThe 4 Phases of Cardiac RehabilitationStepyn SalvadorNo ratings yet
- Labor Cases 7Document112 pagesLabor Cases 7MaryStefanieNo ratings yet
- Jurnal CopdDocument11 pagesJurnal Copdgemarawan abadiNo ratings yet
- Health Care Communication 2Document45 pagesHealth Care Communication 2Holy DishNo ratings yet
- 2012-08-09 The County TimesDocument40 pages2012-08-09 The County TimesSouthern Maryland OnlineNo ratings yet
- InterestDocument16 pagesInterestmohanaaprkash100% (1)
- Springer: Tokyo Berlin Heidelberg New York Barcelona Budapest Hong Kong London Milan Paris Santaclara SingaporeDocument153 pagesSpringer: Tokyo Berlin Heidelberg New York Barcelona Budapest Hong Kong London Milan Paris Santaclara SingaporeCarlos EsescritorNo ratings yet
- Clinical Outcomes of Rehabilitation For Patients Following Lateral Patellar Dislocation: A Systematic ReviewDocument13 pagesClinical Outcomes of Rehabilitation For Patients Following Lateral Patellar Dislocation: A Systematic ReviewHarshoi KrishannaNo ratings yet
- Crabtales 066Document20 pagesCrabtales 066Crab Tales100% (1)
- Lesson 1: Planning For Heath Promotion, Health Maintenance, and Home Health Consideration in The Older AdultDocument6 pagesLesson 1: Planning For Heath Promotion, Health Maintenance, and Home Health Consideration in The Older AdultCzeremar Chan0% (1)
- Telehealth in Occupational Therapy: AOTA Position PaperDocument18 pagesTelehealth in Occupational Therapy: AOTA Position PaperdanielNo ratings yet
- Wellness CenterDocument6 pagesWellness CenterMuntasir SizanNo ratings yet
- Mot SyllabusDocument30 pagesMot SyllabusShanthoshini Baskaran100% (1)
- Holland CodeDocument5 pagesHolland CodeAlisha RohdeNo ratings yet
- Examining The Efficacy of Dance Movement and Music Mixed Treatment On Social Communication Impairment in Children With Autism - Based On Family Parent-Child SituationDocument10 pagesExamining The Efficacy of Dance Movement and Music Mixed Treatment On Social Communication Impairment in Children With Autism - Based On Family Parent-Child Situation賴莙儒No ratings yet
- Occupational Therapy ResumeDocument6 pagesOccupational Therapy Resumeqozthnwhf100% (1)
- Alternative Approaches in The Special EducationDocument11 pagesAlternative Approaches in The Special EducationKiriakos Kiritsopoulos100% (1)
- Major Injury Case Study - Below Knee AmputationDocument2 pagesMajor Injury Case Study - Below Knee AmputationQBE European Operations Risk ManagementNo ratings yet
- ST ND RDDocument20 pagesST ND RDVenkatesh SadasivuniNo ratings yet
- Protocoale Sold ComparativDocument8 pagesProtocoale Sold ComparativLilianaNo ratings yet
- HPCZ Application FormDocument11 pagesHPCZ Application FormQualis LabsNo ratings yet
- Daftar PustakaDocument2 pagesDaftar Pustakadi.yulianiNo ratings yet
- How To Write A SOAP Note-3-10Document2 pagesHow To Write A SOAP Note-3-10mohamed_musaferNo ratings yet
- Low Back Pain Case Study - A Nasty One! But A Good Outcome. - Witty, Pask & BuckinghamDocument4 pagesLow Back Pain Case Study - A Nasty One! But A Good Outcome. - Witty, Pask & BuckinghamermanmahendraNo ratings yet
- Module 4 Levels of PreventionDocument29 pagesModule 4 Levels of PreventionZaren James D. RacaNo ratings yet
- Models of Rehabilitation Component IA Role Name Affiliation: Swe/Swfd/Mr/M23 by Dr. P. Saleel KumarDocument13 pagesModels of Rehabilitation Component IA Role Name Affiliation: Swe/Swfd/Mr/M23 by Dr. P. Saleel KumarRainbowsNo ratings yet
- Strain Counter-Strain PDFDocument7 pagesStrain Counter-Strain PDFCarlosCarpinteroRubioNo ratings yet