Professional Documents
Culture Documents
Chronic Renal Failure
Chronic Renal Failure
Uploaded by
Marinill Soliman0 ratings0% found this document useful (0 votes)
42 views4 pagesChronic renal failure results when the kidneys cannot remove metabolic wastes or perform regulatory functions. This leads to a buildup of wastes in the body and disruption of endocrine and metabolic functions. Renal failure is progressive and irreversible, eventually requiring dialysis or transplantation for patient survival. As renal function declines, wastes accumulate in the blood causing uremia and affecting every body system. Clinical manifestations vary depending on the degree of impairment but may include hypertension, heart failure, acidosis, anemia, gastrointestinal issues, and neurological changes.
Original Description:
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentChronic renal failure results when the kidneys cannot remove metabolic wastes or perform regulatory functions. This leads to a buildup of wastes in the body and disruption of endocrine and metabolic functions. Renal failure is progressive and irreversible, eventually requiring dialysis or transplantation for patient survival. As renal function declines, wastes accumulate in the blood causing uremia and affecting every body system. Clinical manifestations vary depending on the degree of impairment but may include hypertension, heart failure, acidosis, anemia, gastrointestinal issues, and neurological changes.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
0 ratings0% found this document useful (0 votes)
42 views4 pagesChronic Renal Failure
Chronic Renal Failure
Uploaded by
Marinill SolimanChronic renal failure results when the kidneys cannot remove metabolic wastes or perform regulatory functions. This leads to a buildup of wastes in the body and disruption of endocrine and metabolic functions. Renal failure is progressive and irreversible, eventually requiring dialysis or transplantation for patient survival. As renal function declines, wastes accumulate in the blood causing uremia and affecting every body system. Clinical manifestations vary depending on the degree of impairment but may include hypertension, heart failure, acidosis, anemia, gastrointestinal issues, and neurological changes.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
You are on page 1of 4
CHRONIC RENAL FAILURE reduced renal reserve, renal insufficiency, and
Renal failure results when the kidneys cannot ESRD.
remove the body’s metabolic wastes or perform GFR categories in CKD
their regulatory functions. Category GFR Terms Clinical
The substances normally eliminated in the urine presentations
G1 ≥90 Normal or high Markers of kidney
accumulate in the body fluids as a result of damage (nephrotic
G2 60-89 Mildly decreased syndrome, nephritic
impaired renal excretion, leading to a disruption syndrome, tubular
in endocrine and metabolic functions as well as syndrome, urinary
tract symptoms,
fluid, electrolyte, and acid-base disturbances. asymptomatic
urinalysis
Renal failure is a systemic disease and is a final abnormalities,
common pathway of many different kidney and asymptomatic
radiologic
urinary tract diseases. abnormalities,
hypertension due to
AZOTEMIA kidney disease)
Defined as excess of urea and nitrogenous G3a 45-59 Mildly to Mild to severe
moderately complications:
compounds in blood. decreased -anemia
-mineral and bone
Due to breakdown of protein G3b 30-44 Moderately to disorder (elevated
severe decreased
(Metabolism of carbohydrates and fats yields parathyroid
G4 15-29 Severely hormone)
water and CO2) decreased -cardiovascular
disease
If symptoms, use term “uremia” (hypertension, lipid
Chronic renal failure, or ESRD, is a abnormalities, low
serum albumin)
progressive, irreversible deterioration in renal G5 <15 Kidney failure -includes all of
function in which the body’s ability to maintain the above in
metabolic and fluid and electrolyte balance fails, addition
-uremia
resulting in uremia or azotemia (retention of urea
and other nitrogenous wastes in the blood).
STAGES OF RENAL FAILURE
ESRD may be caused by systemic disease, such
What happen?
as diabetes mellitus (leading cause); hypertension;
There are no specific symptoms, but kidney
chronic glomerulonephritis; pyelonephritis;
function can slowly decline.
obstruction of the urinary tract; hereditary lesions,
Kidney function is very low, and treatment
as in polycystic kidney disease; vascular disorders:
for kidney failure may be needed soon.
infections; medications; or toxic agents.
Kidneys can no longer keep up with
Dialysis or kidney transplantation eventually
removing waste products and extra water. This is
becomes necessary for patient survival. Dialysis is an
called kidney failure. Although there is no cure,
effective means of correcting metabolic toxicities at
treatment options are available.
any age, although the mortality rate in infants and
Stage Description GFR,
young children is greater than adults in the presence ml/min/1.73 m2
of other, nonrenal diseases and in the presence of At increased risk ≥ 60
anuria or oliguria. 1 Kidney damage ≥90
with normal or
PATHOPHYSIOLOGY increased GFR
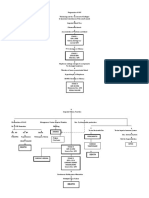
As renal function declines, the end products of 2 Kidney damage 60-89
protein metabolism (which are normally excreted with mild
in urine) accumulate in the blood. Uremia decreased GFR
3 Moderately 30-59
develops and adversely affects every system in decreased GFR
the body. 4 Severely 15-29
The greater the buildup of waste products, the decreased GFR
more severe the symptoms. There are three well- 5 Kidney failure <15 (dialysis)
recognized stages of chronic renal disease;
CLINICAL MANIFESTATION Hypertension may also result from activation of
Because virtually every body system is affected the renin-angiotensin-aldosterone axis and the
by the uremia of chronic renal failure, patients concomitant increased aldosterone secretion.
exhibit a number of signs and symptoms depends Episodes of vomiting and diarrhea may produce
in part on the degree of renal impairment, other sodium and water depletion, which worsens the
underlying conditions, and the patient’s age. uremic state.
CARDIOVASCULAR MANIFESTATION ACIDOSIS
Hypertension (due to sodium and water retention With advanced renal disease, metabolic acidosis
or from activation of the renin-angiotensin- occurs because the kidney cannot excrete
aldosterone system), heart failure and pulmonary increased loads of acid.
edema (due to fluid overload), and pericarditis Decreased acid secretion primarily results from
(due to irritation of the pericardial lining by inability of the kidney tubules to excrete
uremic toxins) are among the cardiovascular ammonia (NH3-) and to reabsorb sodium
problems manifested in ESRD. bicarbonate (HCO3-).
Strict fluid volume control has been found to ANEMIA
normalize hypertension in patients receiving Anemia develops as a result of inadequate
peritoneal dialysis. erythropoietin production, the shortened life span
DERMATOLOGIC SYMPTOMS of RBCs, nutritional deficiencies, and the
Severe itching (prutitus) is common. Uremic patient’s tendency to bleed, particularly from the
frost, the deposit of urea crystals on the skin, is GI tract.
uncommon today because of early and Erythropoietin, a substance normally produced
aggressive treatment of ESRD with dialysis. by the kidney, stimulates bone marrow to
OTHER SYSTEMIC MANIFESTATIONS produce RBCs.
GI signs and symptoms are common and include In renal failure, erythropoietin production
anorexia, nausea, vomiting and hiccups. decreases and profound anemia results,
Neurologic changes, including altered levels of producing fatigue, angina, and shortness of
consciousness, inability to concentrate, muscle breath.
twitching, and seizures, have been observed. CALCIUM AND PHOSPHORUS IMBALANCE
It is generally thought, however, that the Serum calcium and phosphate levels have a
accumulation of uremic waste products is the reciprocal relationship in the body: as one rises,
probable cause. the other decreases.
GLOMERULAR FILTRATION RATE With decreased filtration through the glomerulus
Decreased GFR can be detected by obtaining a of the kidney, there is an increase in the serum
24-hour urinalysis for creatinine clearance. phosphate level and a reciprocal or
As glomerular filtration decrease (due to corresponding decrease in the serum calcium
nonfunctional glomeruli), the creatinine level.
clearance value decreases, whereas the serum The decreased serum calcium level causes
creatinine and BUN levels increase. increased secretion of parathormone from the
Serum creatinine is the more sensitive indicator parathyroid glands. In renal failure, however, the
of renal function because of its constant body does not respond normally to the increased
production in the body secretion of parathormone; as a result, calcium
SODIUM AND WATER RETENTION leaves the bone. Often producing bone changes
The kidney cannot concentrate or dilute the urine and bone disease.
normally in ESRD.
Some patients retain sodium and water,
increasing the risk for edema, heart failure, and COMPLICATIONS
hypertension. Potential complications of chronic renal failure
that concern the nurse and that necessitate a
collaborative approach to care include the Usually, the fluid allowance is 500-600 mL more
following: than the previous day’s 24-hour urine output.
o Hyperkalemia –due to decreased (give 1L of water to patient good for 1 day)
excretion, metabolic acidosis, DIALYSIS
catabolism and excessive intake (diet, Hyperkalemia is usually prevented by ensuring
medications, fluids). adequate dialysis treatments with potassium
o Pericarditis –pericardial effusion, and removal and careful monitoring of all
pericardial tamponade due to retention medications, both oral and intravenous, for their
of uremic waste products and potassium content. The patient is placed on a
inadequate dialysis potassium-restricted diet.
o Hypertension –due to sodium and water The patient with increasing symptoms of chronic
retention and malfunction of the renin- renal failure is referred to a dialysis and
angiotensin-aldosterone system. transplantation center early in the course of
o Anemia –due to decreased progressive renal disease.
erythropoietin production, decreased Dialysis is usually initiated when the patient
RBC life span, bleeding in the GI tract cannot maintain a reasonable lifestyle with
from irritating toxins, and blood loss conservative treatment.
during hemodialysis. ASSESS FLUID STATUS:
o Bone disease and metastatic a. Daily weight
calcifications due to retention of b. Intake and output balance
phosphorus, low serum calcium levels, c. Skin turgor and presence of edema
abnormal vitamin D metabolism, and d. Distention of neck veins
elevated aluminum levels. e. Blood pressure, pulse rate, and rhythm
MEDICAL MANAGEMENT f. Respiratory rate and effort
The goal of management is to maintain kidney FLUID RESTRICTION
function and hemostasis for as long as possible. L –limit fluid intake to prescribed volume
All factors that contribute to ESRD and all E –explain to patient and family rationale for
factors that are rerversible (e.g., obstruction) are restriction
identified and treated. A –assist patient to cope with the discomforts
Management is accomplished primarily with resulting from fluid retention.
medications and diet therapy, although dialysis P –provide or encourage frequent oral hygiene.
may also be needed to decrease the level of ASSESSMENT:
Assess possible risk factors To obtain baseline data
uremic waste products in the blood.
Monitor and record vital To obtain baseline data
PHARMACOLOGIC THERAPY signs
Complications can be prevented or delayed by Assess patient’s appetite To note for presence of
administering prescribed antihypertensives, nausea and vomiting
erythropoietin (Epogen), iron supplements, Note amount/rate of fluid To prevent fluid overload
intake from all sources and monitor intake and
phosphate-binding agents, and calcium output
supplements. Compare current weight To monitor fluid retention
NUTRITIONAL THERAPY gain with admission or and evaluate degree of
previous stated weight excess
Dietary intervention is necessary with
Auscultate breath sounds For presence of crackle or
deterioration of renal function and includes congestion
careful regulation of protein intake, fluid intake Record occurrence of To evaluate degree of
to balance fluid losses, sodium intake to sodium dyspnea excess
Note presence of edema To determine fluid retention
losses, and some restriction of potassium.
Measure abdominal girth May indicate increase in
FLUID INTAKE for changes fluid retention
Evaluate mentation for May indicate cerebral
confusion and personality edema
changes
Observe skin mucous To evaluate degree of fluid
membrane excess
Change position of client To prevent pressure ulcers
timely
Review lab data like BUN, To monitor fluid and
creatinine, serum electrolyte electrolyte imbalances
Restrict sodium and fluid To lessen fluid retention
intake if indicated and overload
Record I&O accurately and To monitor kidney function
calculate fluid volume and fluid retention
balance
Weigh client Weight gain indicated fluid
retention or edema
Encourage quiet, restful To conserve energy and
atmosphere lower tissue oxygen
demand
Promote overall health To promote wellness
measure
You might also like
- PD (Peritoneal Dialysis) Exit Site CareDocument35 pagesPD (Peritoneal Dialysis) Exit Site CareMarc Pipoy100% (1)
- Pathophysiology Diagram: Breast Cancer: Predisposing Factors: Precipitating FactorsDocument2 pagesPathophysiology Diagram: Breast Cancer: Predisposing Factors: Precipitating FactorsMarinill Soliman100% (1)
- Blood Test Results: CMP Explained: Comprehensive Metabolic Panel (CMP)Document1 pageBlood Test Results: CMP Explained: Comprehensive Metabolic Panel (CMP)giuzolinNo ratings yet
- Hemodialysis Delivery SystemDocument6 pagesHemodialysis Delivery SystemShemae Quilacio100% (2)
- Nursing Care Plan Priorities: Risk For InjuryDocument6 pagesNursing Care Plan Priorities: Risk For InjuryPauling FrezNo ratings yet
- Lec 13 - Renal Sys IIDocument3 pagesLec 13 - Renal Sys IIpNo ratings yet
- Renal SystemDocument20 pagesRenal SystemRahul DasNo ratings yet
- MHD Exam 5 MaterialDocument122 pagesMHD Exam 5 Materialnaexuis5467100% (1)
- Renal Failure TableDocument26 pagesRenal Failure TableIgwe SolomonNo ratings yet
- Askep CKDDocument55 pagesAskep CKDyuli ariyantiNo ratings yet
- Chronic Kidney Disease: Prepared by D. ChaplinDocument53 pagesChronic Kidney Disease: Prepared by D. Chaplinmutia aNo ratings yet
- Chronic Kidney Disease: Diagnosis and TherapyDocument21 pagesChronic Kidney Disease: Diagnosis and TherapyLindsNo ratings yet
- Chronic KidneyDocument40 pagesChronic KidneyAni Budiati Sehat SejahteraNo ratings yet
- Jurnal CKD FaizDocument12 pagesJurnal CKD FaizToxic idNo ratings yet
- 2 CKDDocument69 pages2 CKDDammaqsaa W BiyyanaaNo ratings yet
- RenalDocument48 pagesRenalabelzzinnoNo ratings yet
- Introduction & Epidemiology Clinical Features: End-Stage Renal Disease (ESRD)Document2 pagesIntroduction & Epidemiology Clinical Features: End-Stage Renal Disease (ESRD)Nikki VillanuevaNo ratings yet
- Kidney GM Eng 2020Document31 pagesKidney GM Eng 2020snowrose2609No ratings yet
- Chronic Kidney DiseaseDocument29 pagesChronic Kidney DiseaseEsayas KebedeNo ratings yet
- CKD EsrdDocument83 pagesCKD EsrdRita Lakhani100% (1)
- Chronic Kidney FailureDocument9 pagesChronic Kidney Failurekat garciaNo ratings yet
- Farmakoterapi GinjalDocument13 pagesFarmakoterapi GinjaldameriaNo ratings yet
- 4 Kidney Diseases TogleMDDocument1 page4 Kidney Diseases TogleMDMarianneNo ratings yet
- MNT Penyakit GinjalDocument41 pagesMNT Penyakit GinjalNurfitriana DwiNo ratings yet
- Askep Gagal Ginjal - Ns. FitrioDocument32 pagesAskep Gagal Ginjal - Ns. FitriodesyNo ratings yet
- Test 4 OutlineDocument13 pagesTest 4 Outlinemara5140No ratings yet
- Renal Failure: SMF Urologi FK-Unpar / RSUD Dr. Doris SylvanusDocument53 pagesRenal Failure: SMF Urologi FK-Unpar / RSUD Dr. Doris SylvanusClarissa SuheryNo ratings yet
- LP CKD AnemiaDocument12 pagesLP CKD AnemiaNanan SaputraNo ratings yet
- 1 Patho5 - Kidney I 2015bDocument10 pages1 Patho5 - Kidney I 2015bmiguel cuevasNo ratings yet
- Renal Osmosis HY Pathology Notes ATF - ATFDocument109 pagesRenal Osmosis HY Pathology Notes ATF - ATFTran Thai Huynh NgocNo ratings yet
- Chronic Renal Failure: PathophysiologyDocument1 pageChronic Renal Failure: PathophysiologyCindy Mae Dela Torre100% (2)
- Renal FailureDocument61 pagesRenal FailureEdward XiamNo ratings yet
- Chronic Kidney Disease: Dr. Des Riyadi Anas, Sp. PD M. HashemyDocument43 pagesChronic Kidney Disease: Dr. Des Riyadi Anas, Sp. PD M. HashemyAris DaooNo ratings yet
- CKD AweDocument25 pagesCKD AweMunawwar AweNo ratings yet
- Chronic Kidney DiseaseDocument47 pagesChronic Kidney DiseaseSaowda HussainNo ratings yet
- Chronic Kidney DiseaseDocument6 pagesChronic Kidney DiseasekejarabriNo ratings yet
- Pathophysiology Notes: - Glomerulus - Proximal Convoluted TubuleDocument14 pagesPathophysiology Notes: - Glomerulus - Proximal Convoluted TubuleHaifa ibrahimNo ratings yet
- Definition and Criteria For Chronic Kidney DiseaseDocument2 pagesDefinition and Criteria For Chronic Kidney DiseaseImelda Nicolas GarciaNo ratings yet
- Chronic Kidney DiseaseDocument47 pagesChronic Kidney DiseaseTamzid Rabby TanmoyNo ratings yet
- Farmakoterapi Ginjal Dan HDDocument42 pagesFarmakoterapi Ginjal Dan HDDenniWahyuniSafitriNo ratings yet
- LP CKD FiksDocument16 pagesLP CKD FiksWahyu7.8No ratings yet
- Progression of ARFDocument7 pagesProgression of ARFjuzz22No ratings yet
- Chronic Kidney DiseaseDocument4 pagesChronic Kidney DiseaseImnot YouNo ratings yet
- PathoDocument1 pagePathoRhabdoNo ratings yet
- ARF PathophysiologyDocument2 pagesARF Pathophysiologykathy100% (9)
- Gagal Ginjal Akut Pada AnakDocument37 pagesGagal Ginjal Akut Pada AnakNycoNo ratings yet
- Cystatin C A Comparison To Creatinine and Other Clearance MarkersDocument5 pagesCystatin C A Comparison To Creatinine and Other Clearance MarkersRalphael CataloNo ratings yet
- Presented By: Sonia Dagar: Renal FailureDocument40 pagesPresented By: Sonia Dagar: Renal FailureRavanshi ThakurNo ratings yet
- GGK PKMRS PugerDocument12 pagesGGK PKMRS Pugersyamsul arifinNo ratings yet
- POLON, THAGREED BSN3D - KIDNEY DISORDERSDocument4 pagesPOLON, THAGREED BSN3D - KIDNEY DISORDERSThagreed PolonNo ratings yet
- Bloodcharts CMP PDFDocument1 pageBloodcharts CMP PDFSujay DhumalNo ratings yet
- Chronic Renal Failre Chronic Kidney Disease: DefinitionDocument3 pagesChronic Renal Failre Chronic Kidney Disease: DefinitionAhmed almahdiNo ratings yet
- Chronickidneydisease 160201102541Document33 pagesChronickidneydisease 160201102541fatimabashir0234No ratings yet
- Chronic Kidney DiseaseDocument40 pagesChronic Kidney DiseaseEsayas KebedeNo ratings yet
- Idexx Sdma Test Algorithm PDFDocument2 pagesIdexx Sdma Test Algorithm PDFblueice999No ratings yet
- Diseases of Urogenital TractDocument170 pagesDiseases of Urogenital TractMuhammadNo ratings yet
- Lab Values Chart 120511 PDFDocument5 pagesLab Values Chart 120511 PDFVanessaMUeller100% (3)
- Chronic Kidney Failure Transplant 2Document22 pagesChronic Kidney Failure Transplant 2Gail Leslie HernandezNo ratings yet
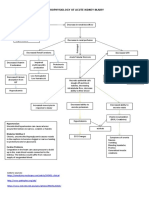
- Pathophysiology of Acute Renal FailureDocument1 pagePathophysiology of Acute Renal FailureAina HaravataNo ratings yet
- Kimia DarahDocument3 pagesKimia DarahmayrzaNo ratings yet
- 6 Med Ward (WK - 1) PathophysiologyDocument3 pages6 Med Ward (WK - 1) PathophysiologyZaijean Kate Dianne LigutomNo ratings yet
- Hepatorenal Syndrome, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandHepatorenal Syndrome, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Notes 2 (Research Protocols)Document2 pagesNotes 2 (Research Protocols)Marinill SolimanNo ratings yet
- Obstetrics Outline (MCHN) Chapter 1Document8 pagesObstetrics Outline (MCHN) Chapter 1Marinill Soliman100% (1)
- Tuberculosis NclexDocument3 pagesTuberculosis NclexMarinill SolimanNo ratings yet
- Labor and Delivery MCNDocument1 pageLabor and Delivery MCNMarinill SolimanNo ratings yet
- QuizDocument9 pagesQuizMarinill SolimanNo ratings yet
- Intravenous Medications (IV) Administering IV MedicationsDocument6 pagesIntravenous Medications (IV) Administering IV MedicationsMarinill SolimanNo ratings yet
- Iv TherapyDocument11 pagesIv TherapyMarinill SolimanNo ratings yet
- Different Types of IV FluidsDocument10 pagesDifferent Types of IV FluidsMarinill SolimanNo ratings yet
- HIV & AIDS PathophysiologyDocument3 pagesHIV & AIDS PathophysiologyMarinill Soliman100% (3)
- Hemodialysis: Stressors and Coping Strategies: ArticleDocument13 pagesHemodialysis: Stressors and Coping Strategies: ArticleAdita AyuNo ratings yet
- Blood Transfusion On Dialysis Guidelines Aug 2017 PDFDocument5 pagesBlood Transfusion On Dialysis Guidelines Aug 2017 PDFYolanda IrawatiNo ratings yet
- NURSING Review Session (Nur 220) Part 1Document8 pagesNURSING Review Session (Nur 220) Part 1Mariel EstoniloNo ratings yet
- Homeostatic MechanismsDocument5 pagesHomeostatic MechanismsMonkey LoverNo ratings yet
- Bio-Artificial Liver: Rituparna Addy 12/BT/23 Department of Biotechnology Haldia Institute of TechnologyDocument17 pagesBio-Artificial Liver: Rituparna Addy 12/BT/23 Department of Biotechnology Haldia Institute of TechnologyPratik KalambeNo ratings yet
- 11 June 2021: 9 Block 15 Bashorun Okusanya Street, Lekki Phase 1, Lagos, NigeriaDocument2 pages11 June 2021: 9 Block 15 Bashorun Okusanya Street, Lekki Phase 1, Lagos, NigeriaAsuquo DukeNo ratings yet
- 2008K Operator's Manual 490042 Rev NDocument239 pages2008K Operator's Manual 490042 Rev NShareDialysis100% (2)
- Angiotensin-Converting Enzyme Inhibitors and Angiotensin Receptor Blockers in Patients With Congestive Heart Failure and Chronic Kidney DiseaseDocument10 pagesAngiotensin-Converting Enzyme Inhibitors and Angiotensin Receptor Blockers in Patients With Congestive Heart Failure and Chronic Kidney DiseaseElizabeth SniderNo ratings yet
- Quick Start GuideDocument20 pagesQuick Start GuideHyacinthe KOSSINo ratings yet
- Transplantation: Treatment Methods For Kidney FailureDocument28 pagesTransplantation: Treatment Methods For Kidney FailurecopiimeiNo ratings yet
- Lesson 9 - OsmoregulationDocument18 pagesLesson 9 - OsmoregulationAimee GraceNo ratings yet
- Eng 2Document346 pagesEng 2Ramona Maria BleotuNo ratings yet
- AluminumDocument84 pagesAluminumaptureinc100% (2)
- Engaging People With Chronic Kidney Disease in Their Own Care An Integrative ReviewDocument10 pagesEngaging People With Chronic Kidney Disease in Their Own Care An Integrative ReviewyutefupNo ratings yet
- Slow, Low, Efficient, Daily Dialysis (SLEDD) in The Critically Ill PatientDocument1 pageSlow, Low, Efficient, Daily Dialysis (SLEDD) in The Critically Ill PatientarisyiNo ratings yet
- 2008K Hemodialysisi Machine Operator's Manual PDFDocument208 pages2008K Hemodialysisi Machine Operator's Manual PDFBasir Ahmad NooriNo ratings yet
- Indian School of Business: January 31, 2019Document23 pagesIndian School of Business: January 31, 2019Sarvesh KashyapNo ratings yet
- Exvretion: Removal of Waste MaterialsDocument20 pagesExvretion: Removal of Waste MaterialsQazi QaziNo ratings yet
- Manual de Maquina de DialisisDocument145 pagesManual de Maquina de DialisisOscar OcañoNo ratings yet
- Electrolyte Repletion Guideline PMGDocument4 pagesElectrolyte Repletion Guideline PMGHany ElbarougyNo ratings yet
- Kalibrasi Mesin DialDocument78 pagesKalibrasi Mesin DialMrQmonkNo ratings yet
- Fresenius For The Exam PDFDocument2 pagesFresenius For The Exam PDFvikas bansalNo ratings yet
- Dialysis Machines Challenges and SolutionsDocument13 pagesDialysis Machines Challenges and SolutionsrickypinaNo ratings yet
- Keto Acid Therapy in CKDDocument23 pagesKeto Acid Therapy in CKDDrajad PriyonoNo ratings yet
- Peritoneal Dialysis.Document2 pagesPeritoneal Dialysis.alex_cariñoNo ratings yet
- Ncmb312 Rle:: Bachelor of Science in NursingDocument7 pagesNcmb312 Rle:: Bachelor of Science in NursingVAL ASHLIE ACEBAR100% (1)
- The Lived Experiences of Patients Undergoing Hemodialysis With The Concept of Care: A Phenomenological StudyDocument8 pagesThe Lived Experiences of Patients Undergoing Hemodialysis With The Concept of Care: A Phenomenological StudyJor GarciaNo ratings yet