Professional Documents
Culture Documents
Mosby's Comprehensive Review of Nursing For The NCLEX-RN® Examination
Mosby's Comprehensive Review of Nursing For The NCLEX-RN® Examination
Uploaded by
NursyNurse0 ratings0% found this document useful (0 votes)
431 views2 pagesThis document provides an overview of infection and the pathology of infection. It discusses the chain of infection, including the infectious agent, reservoir, portals of exit and entry, and modes of transmission. It also describes different types of pathogens that can cause infection, including bacteria, viruses, fungi, and their characteristics. The document concludes with a discussion of antibiotic sensitivity tests and examples of common antibiotics used to treat bacterial infections.
Original Description:
Original Title
Mosby's Comprehensive Review of Nursing for the NCLEX-RN® Examination
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThis document provides an overview of infection and the pathology of infection. It discusses the chain of infection, including the infectious agent, reservoir, portals of exit and entry, and modes of transmission. It also describes different types of pathogens that can cause infection, including bacteria, viruses, fungi, and their characteristics. The document concludes with a discussion of antibiotic sensitivity tests and examples of common antibiotics used to treat bacterial infections.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
0 ratings0% found this document useful (0 votes)
431 views2 pagesMosby's Comprehensive Review of Nursing For The NCLEX-RN® Examination
Mosby's Comprehensive Review of Nursing For The NCLEX-RN® Examination
Uploaded by
NursyNurseThis document provides an overview of infection and the pathology of infection. It discusses the chain of infection, including the infectious agent, reservoir, portals of exit and entry, and modes of transmission. It also describes different types of pathogens that can cause infection, including bacteria, viruses, fungi, and their characteristics. The document concludes with a discussion of antibiotic sensitivity tests and examples of common antibiotics used to treat bacterial infections.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
You are on page 1of 2
Infection 29
REVIEW OF MICROBIOLOGY sneezing, talking, or suctioning respiratory secretions
(e.g., common cold)
Pathology of Infection c. Airborne transmission: small droplet nuclei (5 µm or
A. Infection: invasion of body by pathogenic microorganisms smaller) or dust particles that contain pathogen
(pathogens) and reaction of tissues to their presence and to remain suspended in air for extended period (e.g.,
toxins generated by them Mycobacterium tuberculosis)
1. Pathogenicity: ability of a microbe to cause disease d. Common vehicle transmission: microorganisms are
2. Virulence: degree of pathogenicity transmitted by contaminated food, water, or
B. Classifications equipment (e.g., typhoid fever)
1. Extent of involvement e. Vector-borne transmission: microorganisms
a. Local infection: limited to one locality (e.g., abscess), transmitted by vectors such as mosquitoes, flies,
causing pain, swelling, and erythema; may have ticks, and rats (e.g., Rocky Mountain spotted fever,
systemic repercussions such as fever, malaise, and Lyme disease)
lymphadenopathy 5. Portals of entry: same as portals of exit except skin;
b. Systemic infection: infectious agent is spread intact skin prevents infection
throughout body (e.g., typhoid fever) 6. Susceptible host
2. Length of infectious process a. Developmental level: extremes of age
a. Acute infection: one that develops rapidly, usually b. Inadequate nutritional status
resulting in high fever and severe sickness; resolves c. Coexisting disease
in a short time d. Decreased immune responses
b. Chronic infection: one that develops slowly, with e. Surgical client; client in intensive care unit (ICU);
mild but longer-lasting clinical manifestation; presence of invasive lines
sometimes an acute infection can become chronic Types of Pathogens
3. Etiology of infectious process A. Bacteria
a. Primary infection: develops after initial exposure to 1. Unicellular microbes without chlorophyll
pathogen, unrelated to other health problems 2. Capsule: material secreted by cell, protects it from
b. Secondary infection: develops when pathogens take phagocytosis and increases its virulence (e.g., Diplococcus
advantage of weakened defenses resulting from a pneumoniae)
primary infection (e.g., staphylococcal pneumonia as 3. Spores: inactive resistant structures into which bacterial
sequela of measles) protoplasm can transform under adverse conditions;
c. Opportunistic infection: develops when host defenses under favorable conditions spore germinates into active
are diminished because of disease process or cell (e.g., Clostridium tetani, Clostridium defficile)
therapeutic modalities (e.g., vaginal yeast infection 4. Examples of disease-producing bacteria
following antibiotic therapy) a. Eubacteriales: divided into five families based on
C. Chain of infection shape, gram stain, and endospore formation
1. Infectious agent (1) Gram-positive cocci
2. Reservoir: source of almost all pathogens is human or (a) Diplococci: occurring predominantly in pairs
animal (e.g., Diplococcus pneumoniae)
a. Persons exhibiting manifestations of disease (b) Streptococci: occurring predominantly in
b. Carriers: persons who harbor pathogens in absence chains (e.g., Streptococcus pyogenes)
of discernible clinical disease (c) Staphylococci: occurring predominantly in
(1) Healthy carriers: those who have never had the grapelike bunches (e.g., S. aureus)
disease in question (2) Gram-negative cocci include Neisseria gonorrhoeae
(2) Incubatory carriers: those in incubation phase of and Neisseria meningitidis
disease (3) Gram-negative rods include enterobacteria such
(3) Chronic carriers: those who have recovered from as Escherichia, Salmonella, and Shigella species
disease but continue to harbor pathogens (4) Gram-positive rods that do not produce
3. Portals of exit: route by which microorganisms leave endospores include Corynebacterium diphtheriae
body; blood and body fluids, skin, mucous membranes, (5) Gram-positive rods that produce endospores
and respiratory, genitourinary, and GI tracts include Bacillus anthracis, Clostridium botulinum,
4. Mode of transmission and Clostridium tetani
a. Contact transmission (e.g., Staphylococcus aureus) b. Actinomycetales (actinomycetes): moldlike microbes
(1) Direct: contact between body surfaces with elongated cells, frequently filamentous (e.g.,
(2) Indirect: contact between susceptible host and Mycobacterium tuberculosis, Mycobacterium leprae)
contaminated intermediate object (e.g., sink c. Spirochaetales (spirochetes): flexuous, spiral
faucets) organisms (e.g., Treponema pallidum)
b. Droplet transmission: droplets from infected d. Mycoplasmatales (mycoplasmas): delicate, nonmotile
individual are propelled short distance by coughing, microbes displaying a variety of sizes and shapes
30 CHAPTER 3 Integral Aspects of Nursing Care
B. Viruses B. Antibiotic sensitivity tests: identify antibiotics that are
1. Obligate intracellular parasite; replicates only within cell effective against a particular organism
of another organism; composed of either ribonucleic C. Mechanism of action: interfere with or inhibit cell-wall
acid (RNA) or deoxyribonucleic acid (DNA), not both synthesis of RNA or DNA of pathogen
2. Examples of disease-producing viruses D. Examples
a. Human immunodeficiency virus (HIV): AIDS 1. Penicillins (broad spectrum): amoxicillin may be
b. Hepatitis B virus (HBV): hepatitis type B combined with a second drug to prevent bacterial
c. Haemophilus influenza virus: influenza resistance such as amoxicillin and clavulanate
d. Varicella-zoster virus: chickenpox, herpes zoster, (Augmentin), ampicillin and sulbactam (Unasyn),
shingles piperacillin and tazobactam (Zosyn)
C. Fungi 2. Cephalosporins (broad spectrum): cefazolin (Ancef ),
1. Saprophytic organisms that live on organic material cephalexin (Keflex)
2. Molds: fuzzy growths of interlacing filaments called 3. Erythromycins: clindamycin HCl (Cleocin HCl),
hyphae; reproduce by spores azithromycin (Zithromax), erythromycin (Ery-Tab, Eryc)
3. Yeasts: organisms that usually are single-celled; usually 4. Tetracyclines (broad spectrum): doxycycline
reproduce by budding (Vibramycin), tetracycline (Sumycin)
4. Examples of disease-producing fungi 5. Aminoglycosides (broad spectrum): gentamicin,
a. Candida albicans, a yeast: moniliasis (“thrush”) neomycin, streptomycin
b. Histoplasmosis capsulatum: histoplasmosis 6. Quinolones (broad spectrum): ciprofloxacin (Cipro) and
c. Trichophyton rubrum: tinea pedis (“athlete’s foot”) levofloxacin (Levaquin)
D. Control of microorganisms 7. Polymyxin group: polymyxin B
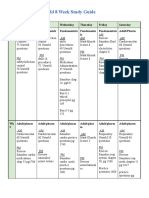
1. Medical asepsis (Table 3-1: Precautions to Prevent the 8. Glycopeptides: vancomycin (Vancocin)
Spread of Microorganisms) E. Major side effects
a. Standard precautions (e.g., hand hygiene, personal 1. Depressed appetite (altered taste sensitivity)
protective equipment [PPE]) 2. Nausea, vomiting (normal flora imbalance)
b. Transmission-based precautions (e.g., airborne, 3. Diarrhea (normal flora imbalance)
droplet, contact) 4. Suppressed absorption of variety of nutrients including
2. Surgical asepsis fat; protein; lactose; vitamins A, D, K, and B12; and
3. Disinfection: removal or destruction of pathogens the minerals calcium, iron, and potassium (normal
4. Sterilization: removal or destruction of all microbes flora imbalance)
5. Antiseptic: inhibits microbial growth 5. Increased excretion of water-soluble vitamins and
6. Heat sterilization minerals (normal flora imbalance)
a. Moist heat 6. Superinfection (normal flora imbalance)
(1) Steam under pressure (autoclave) 7. Allergic reactions, anaphylaxis (hypersensitivity)
(2) Boiling objects in water; some spores resist boiling 8. Nephrotoxicity (direct kidney toxic effect)
b. Dry heat 9. Can render oral contraceptives ineffective
7. Radiation: all types of radiation injurious to microbes 10. Tetracyclines
a. Gamma rays: sterilize food and drugs a. Hepatotoxicity (direct liver toxic effect)
b. Ultraviolet light: inhibits microbial population of air b. Phototoxicity (degradation to toxic products by
in operating rooms, nurseries, and laboratories ultraviolet rays)
c. Hyperuricemia (impaired kidney function)
RELATED PHARMACOLOGY d. Enamel hypoplasia, dental caries, and bone defects
in children younger than 8 years of age (drug binds
Definition of Terms to calcium in tissue)
A. Bactericidal effect: destroys bacteria at low concentrations 11. Aminoglycosides
B. Bacteriostatic effect: slows reproduction of bacteria a. Ototoxicity (direct toxic effect to auditory [eighth
C. Superinfection (secondary infection): emergence of cranial] nerve)
microorganism growth when natural protective flora are b. Leukopenia (decreased white blood cell [WBC]
destroyed by an anti-infective drug synthesis)
D. Bacterial resistance: natural or acquired characteristic of an c. Thrombocytopenia (decreased platelet synthesis)
organism that prevents destruction by a drug to which it d. Headache, confusion (neurotoxicity)
was previously susceptible e. Peripheral neuropathy (neurotoxicity)
Antibiotics f. Nephrotoxicity (direct kidney toxic effect)
A. Description g. Respiratory paralysis (neuromuscular blockade)
1. Destroy bacteria or inhibit bacterial reproduction to 12. Vancomycin
control infection a. Ototoxicity (hearing loss)
2. Available in oral, parenteral, and topical forms, b. Nephrotoxicity (kidney damage)
including ophthalmic and ear drop preparations F. Nursing care
You might also like
- The Nursing School Complete Bundle (Stephanee Beggs) OG-compressed-40-290Document251 pagesThe Nursing School Complete Bundle (Stephanee Beggs) OG-compressed-40-290rnelaitotherescueNo ratings yet
- Mark Klimek Full Nclex ReviewerDocument30 pagesMark Klimek Full Nclex ReviewerAlex BellNo ratings yet
- OB MIdterm ExamDocument31 pagesOB MIdterm Examkatiana louisNo ratings yet
- NCLEX RN Review For Reduction of Risk PotentialDocument7 pagesNCLEX RN Review For Reduction of Risk Potentialpaulinatia100% (1)
- Clinical Nursing JudgmentDocument7 pagesClinical Nursing Judgmentapi-502994344No ratings yet
- Hesi Management of A Emergent Care UnitDocument5 pagesHesi Management of A Emergent Care UnitAna Bienne0% (1)
- RPN - Pharmacology (A)Document12 pagesRPN - Pharmacology (A)Ana BienneNo ratings yet
- Guidelines To Start 100 Bed HospitalDocument19 pagesGuidelines To Start 100 Bed HospitalRahul KashyapNo ratings yet
- Reviewer C AnswersDocument39 pagesReviewer C AnswersDavis WhiteNo ratings yet
- Hurst Review CDC Infection Control ChartDocument44 pagesHurst Review CDC Infection Control ChartTerry Thun100% (2)
- Antepartum 1Document3 pagesAntepartum 1Emily DavisNo ratings yet
- GuideDocument5 pagesGuideHu Tao100% (1)
- NCLEX Review ExamplefinalDocument52 pagesNCLEX Review Examplefinalisapatrick8126100% (1)
- Airborne PrecautionDocument6 pagesAirborne PrecautionBa LitNo ratings yet
- HESI Exam PracticeDocument33 pagesHESI Exam PracticeJean AustenNo ratings yet
- Ati Funds ReviewDocument11 pagesAti Funds Reviewmrsfelic08No ratings yet
- Chapter 41: The Child With An Infectious Disease Test Bank: Multiple ChoiceDocument10 pagesChapter 41: The Child With An Infectious Disease Test Bank: Multiple ChoiceNurse UtopiaNo ratings yet
- Tubes NclexDocument3 pagesTubes NclexYoke W Khoo100% (1)
- Individual Performance Profile PN Nursing Care of Children 2011 Form BDocument4 pagesIndividual Performance Profile PN Nursing Care of Children 2011 Form BStan Tan67% (3)
- U World ReproductiveDocument5 pagesU World ReproductiveAce LabosNo ratings yet
- Infection Control For NclexDocument9 pagesInfection Control For NclexMadora SamuelNo ratings yet
- NclexDocument34 pagesNclexErnie John OyaoNo ratings yet
- Kaplan Focus ReviewDocument9 pagesKaplan Focus ReviewSaidel ElizondoNo ratings yet
- Nclex-Pn Chapter 21 BwfinalDocument12 pagesNclex-Pn Chapter 21 BwfinalatmojdNo ratings yet
- Open Pediatric ArcherDocument84 pagesOpen Pediatric Archerbaharada1979No ratings yet
- Nclex 3500Document4 pagesNclex 3500chitorNo ratings yet
- Answer: CDocument34 pagesAnswer: CLola OladapoNo ratings yet
- Precautions NclexDocument1 pagePrecautions NclexAngelo Karzovic100% (1)
- NLE - CGFNS - Nclex Review Materials 4Document6 pagesNLE - CGFNS - Nclex Review Materials 4ChieChay DubNo ratings yet
- NCLEX Quick FactsDocument7 pagesNCLEX Quick FactsMary Aurine FullanteNo ratings yet
- View AnswersDocument4 pagesView AnswersFaith Levi Alecha AlferezNo ratings yet
- L Lfiicht : Rtti L (If 1 Ffis1I'1Document14 pagesL Lfiicht : Rtti L (If 1 Ffis1I'1Gloria JaisonNo ratings yet
- IV Therapy Lippincott Manual of Nursing PracticeDocument20 pagesIV Therapy Lippincott Manual of Nursing PracticeHejia MagangcongNo ratings yet
- 6 - Basic Care and ComfortDocument15 pages6 - Basic Care and ComfortKristen NateNo ratings yet
- Exam ReviewDocument4 pagesExam ReviewMya Thomas100% (1)
- Testing Strategies For The Nclex-Rn Examination: Chapter OneDocument22 pagesTesting Strategies For The Nclex-Rn Examination: Chapter OneShiraishiNo ratings yet
- Nursing BulletsDocument72 pagesNursing BulletsJoanna Mae Carolino100% (1)
- Nclex QuestionsDocument29 pagesNclex QuestionsRichard TandaguenNo ratings yet
- NCLEX Practice QuestionsDocument12 pagesNCLEX Practice QuestionsDane WrightNo ratings yet
- Strategy DefinitionsDocument8 pagesStrategy DefinitionskwameNo ratings yet
- Week 5 NCLEX QuestionsDocument6 pagesWeek 5 NCLEX QuestionsGwenn SalazarNo ratings yet
- Select All That ApplyDocument10 pagesSelect All That ApplyJohnasse Sebastian NavalNo ratings yet
- NCLEXDocument95 pagesNCLEXrikkapupuNo ratings yet
- Hesi Management of A Medical UnitDocument2 pagesHesi Management of A Medical UnitAna Bienne100% (1)
- NCLEX Review GuideDocument3 pagesNCLEX Review GuidefallenangelleNo ratings yet
- Ignatavicius Chapter 59 (Evolve), Ignatavicius Chapter 57 (Evolve), GI CH 56, 57, 58, 59 Ignatavicius, Ignatavicius Chapter 54 (Evolve), Sole Ch 19, Ignatavicius Chapter 63 (Evolve), Sole Ch 16 Flashcards _ QuizletDocument63 pagesIgnatavicius Chapter 59 (Evolve), Ignatavicius Chapter 57 (Evolve), GI CH 56, 57, 58, 59 Ignatavicius, Ignatavicius Chapter 54 (Evolve), Sole Ch 19, Ignatavicius Chapter 63 (Evolve), Sole Ch 16 Flashcards _ QuizletNursyNurseNo ratings yet
- Medical Surgical ATI Review Flashcards - QuizletDocument27 pagesMedical Surgical ATI Review Flashcards - QuizletNursyNurseNo ratings yet
- NCLEX QuestionsDocument5 pagesNCLEX Questionsijeoma00100% (2)
- 13 2023 Surgery Revised HandoutsDocument26 pages13 2023 Surgery Revised HandoutswesamNo ratings yet
- Lippincott's PEDIATRIC3 ANSWERSDocument8 pagesLippincott's PEDIATRIC3 ANSWERSNursyNurseNo ratings yet
- Fall 2023, 1R8 - Maternal Newborn Study Guide (Comprehensive)Document16 pagesFall 2023, 1R8 - Maternal Newborn Study Guide (Comprehensive)Tia Liveandlearn0% (1)
- Positioning NCLEXDocument4 pagesPositioning NCLEXShazaNo ratings yet
- NCLEX Examination Review QuestionsDocument14 pagesNCLEX Examination Review Questionsmstags100% (1)
- Q&A Psychocosocial 1Document12 pagesQ&A Psychocosocial 1api-3818438No ratings yet
- Nclex PrepDocument2 pagesNclex PrepJeremy HodgesNo ratings yet
- NCLEX PN Practice Exam Set I-VDocument56 pagesNCLEX PN Practice Exam Set I-Vaajo136No ratings yet
- Ob Final Exam Review Summary Maternity NursingDocument40 pagesOb Final Exam Review Summary Maternity NursingVin Lorenzo CampbellNo ratings yet
- Navigating Long-Term Care - A Practical Approach for NursesFrom EverandNavigating Long-Term Care - A Practical Approach for NursesNo ratings yet
- NURSING CARE OF ADULTS I: Passbooks Study GuideFrom EverandNURSING CARE OF ADULTS I: Passbooks Study GuideNo ratings yet
- Mental Status Assessment#2Document5 pagesMental Status Assessment#2NursyNurseNo ratings yet
- Online Connect Verbatim Report (Sample)Document5 pagesOnline Connect Verbatim Report (Sample)NursyNurseNo ratings yet
- Dosage Calculation Review Part 3 - Flow Rate CalculationsDocument3 pagesDosage Calculation Review Part 3 - Flow Rate CalculationsNursyNurseNo ratings yet
- Nursing Care Plan #1 Mental HealthDocument13 pagesNursing Care Plan #1 Mental HealthNursyNurseNo ratings yet
- 3 Chapter 29 Practice Questions CardioDocument17 pages3 Chapter 29 Practice Questions CardioNursyNurseNo ratings yet
- Skin Pediatric NotesDocument8 pagesSkin Pediatric NotesNursyNurseNo ratings yet
- Dosage Calculation Review Part 2 - Medication DosagesDocument2 pagesDosage Calculation Review Part 2 - Medication DosagesNursyNurseNo ratings yet
- Procedure Checklist Chapter 38, Skill 38-01: Administering IV Medication Via PRN Lock or IV LineDocument2 pagesProcedure Checklist Chapter 38, Skill 38-01: Administering IV Medication Via PRN Lock or IV LineNursyNurseNo ratings yet
- Dosage by Weight Exercises and AnswersDocument3 pagesDosage by Weight Exercises and AnswersNursyNurseNo ratings yet
- Dosage Titration PresentationDocument17 pagesDosage Titration PresentationNursyNurseNo ratings yet
- Procedure Checklist Chapter 26, Skill 26-04: Obtaining A Wound CultureDocument1 pageProcedure Checklist Chapter 26, Skill 26-04: Obtaining A Wound CultureNursyNurseNo ratings yet
- Pedi Math Packet 2016-2017-1Document26 pagesPedi Math Packet 2016-2017-1NursyNurseNo ratings yet
- Antidiuretic Hormone: Manifestations of Dehydration-ElderlyDocument15 pagesAntidiuretic Hormone: Manifestations of Dehydration-ElderlyNursyNurseNo ratings yet
- Procedure Checklist Chapter 34, Skill 34-02: Performing VenipunctureDocument3 pagesProcedure Checklist Chapter 34, Skill 34-02: Performing VenipunctureNursyNurseNo ratings yet
- BNS Insulins & Other Meds We Covered - Details - Kahoot!Document22 pagesBNS Insulins & Other Meds We Covered - Details - Kahoot!NursyNurseNo ratings yet
- BNS Exam 4 CH 31 Book Review Questions, Questions Taken From Key Points, and Within Book - Details - Kahoot!Document32 pagesBNS Exam 4 CH 31 Book Review Questions, Questions Taken From Key Points, and Within Book - Details - Kahoot!NursyNurseNo ratings yet
- Important Slides Nutrition ch5Document18 pagesImportant Slides Nutrition ch5NursyNurseNo ratings yet
- Procedure Checklist Chapter 37, Skill 37-01: Reconstituting and Withdrawing Medication From A VialDocument2 pagesProcedure Checklist Chapter 37, Skill 37-01: Reconstituting and Withdrawing Medication From A VialNursyNurseNo ratings yet
- Biology Notes: Topic 1CDocument3 pagesBiology Notes: Topic 1Claiba amirNo ratings yet
- TCCC Quick Reference Guide 2017Document54 pagesTCCC Quick Reference Guide 2017https://www.t-medical.orgNo ratings yet
- Manual, Blood CultureDocument41 pagesManual, Blood CultureFilipus HendiantoNo ratings yet
- Sarcopenia 2Nd Edition John E Morley Full Download ChapterDocument51 pagesSarcopenia 2Nd Edition John E Morley Full Download Chapterdawn.payne642100% (15)
- 782Document20 pages782Aarathi raoNo ratings yet
- Consultant Job Description Proforma J Oct10Document21 pagesConsultant Job Description Proforma J Oct10myjesus123No ratings yet
- CHAPTER 2 Science Form 4Document59 pagesCHAPTER 2 Science Form 4Lopak TikeNo ratings yet
- Chap 05 Abdominal TraumaDocument24 pagesChap 05 Abdominal TraumaAndra SNo ratings yet
- Perioperative Fluids in ChildrenDocument7 pagesPerioperative Fluids in ChildrenRosallia MegawatiNo ratings yet
- Thyroid Cancer and It's Management: Dr. Nurun Nahar CMO Head, Thyroid Division InmuDocument44 pagesThyroid Cancer and It's Management: Dr. Nurun Nahar CMO Head, Thyroid Division InmuParvez AhmedNo ratings yet
- Villareal - NCMA216 Drug StudyDocument10 pagesVillareal - NCMA216 Drug StudyRozen VillarealNo ratings yet
- Paracetamol Dosing: For Children in Primary CareDocument3 pagesParacetamol Dosing: For Children in Primary Careacha kyungsooNo ratings yet
- Journal of Cranio-Maxillo-Facial Surgery: Matthias Zimmermann, Emeka NkenkeDocument6 pagesJournal of Cranio-Maxillo-Facial Surgery: Matthias Zimmermann, Emeka Nkenkekarla gonzalezNo ratings yet
- 1 SMDocument6 pages1 SMedi_wsNo ratings yet
- Iv PrimingDocument16 pagesIv PrimingZahra jane A.No ratings yet
- Semi Final Exam in LeadershipDocument6 pagesSemi Final Exam in LeadershipJessa Mae JabegueroNo ratings yet
- Technical Notes Community Health NursingDocument8 pagesTechnical Notes Community Health NursingMary JoyNo ratings yet
- Comparative Anatomy of Circulation in Annelid, Arthopoda and MolluscsDocument4 pagesComparative Anatomy of Circulation in Annelid, Arthopoda and MolluscsNarasimha MurthyNo ratings yet
- April 29 8:30AM - Dental Residency by Alvin ThienDocument21 pagesApril 29 8:30AM - Dental Residency by Alvin Thienjordyn1990No ratings yet
- Planning For Health PromotionDocument55 pagesPlanning For Health Promotionsweetsai05No ratings yet
- AbdomenDocument43 pagesAbdomenEmmanuel CuevasNo ratings yet
- Radbook 2016Document216 pagesRadbook 2016seisNo ratings yet
- A List of Prioritized Nursing DiagnosisDocument3 pagesA List of Prioritized Nursing DiagnosisRica DiazNo ratings yet
- RH Fs Risk FactorsDocument2 pagesRH Fs Risk FactorsfentroispNo ratings yet
- Hamstring Injury - NHSDocument3 pagesHamstring Injury - NHSAndy Delos ReyesNo ratings yet
- Surgical Gastroenterologist in ChennaiDocument2 pagesSurgical Gastroenterologist in ChennaiSrivatsan GurumurthyNo ratings yet
- Schizophrenia and Psychosis: Group 4 Presentation PharmacologyDocument4 pagesSchizophrenia and Psychosis: Group 4 Presentation PharmacologyVon Valentine MhuteNo ratings yet
- 9 Unknown High Cholesterol Symptoms!Document2 pages9 Unknown High Cholesterol Symptoms!Feronica Felicia Imbing IINo ratings yet
- CSBP Post Stroke Checklist ENDocument2 pagesCSBP Post Stroke Checklist ENEduardo BessoloNo ratings yet