Professional Documents
Culture Documents
PDL-1 Expression in Young Age and CD8 SCC
PDL-1 Expression in Young Age and CD8 SCC
Uploaded by
elisasitohangOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
PDL-1 Expression in Young Age and CD8 SCC
PDL-1 Expression in Young Age and CD8 SCC
Uploaded by
elisasitohangCopyright:
Available Formats
International Journal of Gynecological Pathology
00:1–8, Lippincott Williams & Wilkins, Baltimore
Copyright © 2019 by the International Society of Gynecological Pathologists
Original Article
PD-L1 Expression Correlates With Young Age and CD8+
TIL Density in Poorly Differentiated Cervical Squamous
Cell Carcinoma
Ozlen Saglam, M.D., Junmin Zhou, Ph.D., Xuefeng Wang, Ph.D.,
and Jose R. Conejo-Garcia, M.D., Ph.D.
Summary: Management options are limited in advanced or recurrent cervical carcinoma. The
Food and Drug Administration has recently approved programed cell death-1 (PD-1)/PD-
ligand-1 (PD-L1) inhibitors for the treatment of advanced PD-L1 positive cervical cancer. We
studied PD-L1 expression in cervical squamous cell carcinoma (CSCC) samples initially on a
tissue microarray and then in full-tissue sections from poorly differentiated (grade 3) cancers.
Tissue microarray was composed of 45 grade 3 and 2 (moderately differentiated) tumors.
PD-L1 expression was evaluated as categorical data and by obtaining combined positive
score of neoplastic and mononuclear inflammatory cells. In tissue microarray samples PD-L1
expression was higher in poorly differentiated cancers compared with grade 2 tumors by
immunohistochemistry. Full-tissue sections from grade 3 CSCC (n = 22) were stained with
PD-L1, CD8, and VEGF antibodies. Poorly differentiated CSCC samples had diffuse
( ≥ 50%) and focal/patchy staining patterns. The latter pattern showed localized tumor-stroma
interface staining in 5 samples with low combined positive score. Importantly, younger
patients (median = 36) had tumors with higher expression. PD-L1 expression was associated
with larger tumor size and absent lymphovascular invasion. In addition, CD8+ tumor-
infiltrating lymphocyte density within the neoplastic tissue matched with PD-L1 levels. The
overall survival rates did not correlate with PD-L1 expression. However, in early-stage disease
high CD8+ tumor-infiltrating lymphocyte density within the peritumoral stroma was
associated with better survival outcomes in multivariate analysis. PD-L1 expression and
CD8+ tumor-infiltrating lymphocyte density may be useful to define a subgroup of patients
with relatively better prognosis in poorly differentiated CSCC. It is warranted to validate our
results in a larger sample size. Key Words: Cervix—Squamous cell carcinoma—PD-L1.
Cervical cancer is the third most common gyneco-
From the Departments of Pathology (O.S.); Biostatistics and logic cancer in the United States with an estimated
Bioinformatics (J.Z., X.W.); and Immunology (J.R.C.-G), Moffitt
Cancer Center, Tampa, Florida. incidence rate of 13,240 in 2018 (1). In the last decades,
Support for Shared Resources was provided by Cancer Center effective screening programs and preventive vaccines
Support Grant (CCSG) CA076292 to H. Lee Moffitt Cancer facilitated early detection of precursor lesions and
Center. This study was supported by R01CA157664, R01CA
124515, and U01CA232758. decreased cancer rates in developed countries (2).
The authors declare no conflict of interest. Currently, recommended therapy for advanced stage
Address correspondence and reprint requests to Ozlen Saglam, cancers defined as International Federation of Gyne-
MD, Department of Pathology, Moffitt Cancer Center, 12902 USF
Magnolia Drive, Tampa, FL 33602. E-mail: ozlen.saglam@moffitt. cology and Obstetrics stages IB2-IVA is concurrent
org. chemoradiation (CCR) therapy (3). However, recurrent
1 DOI: 10.1097/PGP.0000000000000623
Copyright r 2019 International Society of Gynecological Pathologists.
2 O. SAGLAM ET AL.
or metastatic disease develops in 15% to 61% of women performed in the latter group. Results were correlated
within the first 2 yr after completion of the primary with clinicopathologic parameters.
therapy (4). The management of recurrent cervical
cancer depends on previous treatment modalities. In the
MATERIAL AND METHODS
presence of prior pelvic irradiation, the only curative
therapy is pelvic exenteration, associated with high Study Design
morbidity and mortality rates (5,6). The majority of
patients with recurrent or metastatic cervical cancer are Step 1: TMA
treated with palliative platinum-based chemotherapy The TMA was composed of 45 CSCC and 37
without significant survival benefits (7,8). The addition matching benign squamous epithelium from cancer
of vascular endothelial growth factor (VEGF) inhib- patients and 8 normal squamous mucosa from healthy
itors reduce disease progression and prolong overall individuals. CSCC samples were taken from the most
survival (OS) (9). Epithelial growth factor inhibitors, invasive portion of the tumor in the definitive excision
targeting of PI3K/AKT/mTOR pathway and therapeu- specimens. All available routine slides were reviewed
tic vaccines are other new treatment modalities included and the tumor grade was confirmed before TMA
in clinical trials for recurrent or metastatic cervical construction. When there was a disagreement in
cancer (10–12). Until recently, immunotherapy was histologic grade a consensus between the reviewer
emphasized as maintenance therapy for high-risk and primary gynecologic pathologist was obtained.
patients with multiple positive pelvic lymph nodes, There were 21 moderately differentiated (grade 2)
uterine corpus extension and positive paraaortic lymph and 24 poorly differentiated (grade 3) samples. TMA
nodes in patients treated with CRR (13). The Food was stained with PD-L1 antibody. In cervical cancer,
Drug Administration (FDA) approved programmed the combined positive score (CPS) is the recom-
death receptor-1 (PD-1) blocker, pembrolizumab, to mended method of evaluation for the FDA-approved
treat programed cell death ligand-1 (PD-L1) positive commercial PD-L1 assays and defined as percentage
advanced cervical cancer in June 2018. of positively stained neoplastic and mononuclear
PD-L1 is a member of B7 family and the receptor of inflammatory cells. In addition to CPS, PD-L1
a transmembrane protein, PD-1 (14). PD-1 is ex- immunostaining in neoplastic cells was evaluated as
pressed in effector immune cells and PD-L1 associated categorical data (o1% membranous staining: nega-
with antigen presenting cells such as dendritic and tive; 1%–49% positivity in neoplastic cells: expressed;
cancer cells (15). The expression of PD-1 is upregu- 50%–100% positivity: diffusely expressed). In both
lated after T-cell and B-cell activation. The immune analyses, partial and complete membranous staining
checkpoint inhibitors maintain tolerance against was evaluated. Clinicopathologic parameters such as
autoimmunity under physiological conditions. PD-1/ patient’s age, tumor size, lymphovascular invasion
PD-L1 interaction leads to blockage of T-cell (LVI), lymph node status, disease stage, and OS were
activation by inhibiting T-cell receptor signal trans- correlated with marker expression.
duction and CD28-C80 costimulation (16). As an
immune resistance mechanism PD-L1 is overex-
pressed in several cancer types (17,18) and immune Step 2: Poorly Differentiated CSCC Samples
checkpoint inhibitors are already in use for the Twenty-two of 24 poorly differentiated CSCC from
treatment of metastatic melanoma, non–small cell TMA samples were available for additional immuno-
lung carcinoma, head and neck, kidney and urothelial histochemical studies. Representative full-tissue sections
carcinomas, Hodgkin lymphoma, and mismatch were stained with PD-L1, CD8, and VEGF antibodies.
repair-deficient cancers (19). Even though the FDA PD-L1 expression was evaluated in a similar way to
has recently approved PD-L1 blockers in advanced TMA samples and included both categorical data and
cervical cancer, it is not well defined which patient CPS. Even though there was a high-grade squamous
subgroup would benefit most from the treatment. We intraepithelial lesion (HSIL) component in a sample
studied PD-L1 expression of cervical squamous cell only invasive carcinoma was graded in readings. CD8+
carcinoma (CSCC) by immunohistochemistry in a tumor-infiltrating lymphocytes (TIL) were evaluated
stepwise approach, first on a tissue microarray (TMA) separately in the neoplastic tissue and surrounding
and then in full-tissue sections from poorly differ- peritumoral stroma. The number of CD8+ TIL was
entiated cancer (grade 3) samples. In addition to counted in 20 high-power fields (400×). The field
PD-L1, immunostains for CD8 and VEGF were diameter was 0.55 mm. A mean was obtained for
Int J Gynecol Pathol Vol. 00, No. 00, ’’ 2019
Copyright r 2019 International Society of Gynecological Pathologists.
PD-L1 EXPRESSION IN CSCC 3
neoplastic cells and surrounding stroma. The number of each tumor and nontumor regions. Next we combined
TILs per high-power field was recorded separately for the tally for positive and negative cells from all 20 fields
tumor and peritumoral stroma. The density of TIL per to determine the percentage of lymphocytes (number of
high-power field was divided into 3 groups: (1+): 5 or strongly and moderately stained cells/total number of
less TIL, (2+): 6 to 19 TIL, and (3+): 20 or more CD8+ cells). The calculation was done separately for the
TIL (20). Analytic microscopy was used as a second tumor and nontumor areas. The total area of analysis
reviewer for CD8 evaluation. VEGF staining was for the tumor and peritumoral stroma was 0.2 mm2 for
recorded as percent of positively stained neoplastic cells. each component.
Immunohistochemistry
Statistical Analyses
Ventana Discovery XT automated system (Ventana
Patient characteristics were summarized using
Medical Systems, Tucson, AZ) was used as per the
descriptive statistics including mean, median and
manufacturer’s protocol with proprietary reagents for
range for continuous measures and proportions and
all antibodies. Briefly, 4 μm-thick tissue sections were
frequencies for categorical measures. The association
deparaffinized on the automated system with EZ Prep
between continuous variables and PD-L1/CD8 status
solution. Heat-induced antigen retrieval method was
were assessed using Kruskal-Wallis tests or Student t
used in Cell Conditioning for 1 hr. Sections were
test. The associations between categorical variables
stained with rabbit PD-L1 monoclonal antibody (CST
and PD-L1/CD8 status were evaluated using Fisher
13684, Cell Signaling Technology, Danvers, MA) at a
exact tests. Results from the overlapping TMA and
concentration of 1:50 with appropriate positive and
full-tissue samples were compared by Pearson Corre-
negative controls. A mouse monoclonal CD8 anti-
lation test. Log-rank tests were used to determine if
body (#760-4250, Ventana, Oro Valley, AZ) was used
clinical variables were independently associated with
at a prediluted concentration and incubated for 32
OS. Cox proportional hazards models were used to
min. The protocol is the suggested baseline standard
incorporate clinical variables into a multivariate
from the Ventana platform system. A rabbit VEGF
survival model. Model development was completed
(#ab52917, Abcam, Cambridge, MA) antibody was
by first including any clinical variable with Po0.05
diluted to 1:200 concentration. The Ventana Chro-
into an initial model, followed by backward elimi-
moMap kit was used as a detection system. Slides
nation to remove variables with P > 0.05 from the
were counterstained with Hematoxylin which was
final model. All analyses were performed with SAS
followed by dehydration and cover slipping.
version 9.4.
Analytic Microscopy
RESULTS
CSCC slides stained for CD8 positivity were scanned
using the Aperio (Leica Biosystems Inc., Vista, CA) PD-L1 Expression in Cervical Squamous Cell Cancer
ScanScope AT2 with a 20×/0.8NA objective lens. does not Correlate With OS
Images were stored in an Eslide Manager database In TMA samples (n = 45), median patient age was 42
and viewed with Imagescope version 12.3.3.5048 (Leica (24–83). Primary surgeries were performed between
Biosystems Inc.). Under the direction of a pathologist 1991 and 2006. Only one patient received preoperative
random identical sized regions of interest from each radiation therapy. Locoregional lymph node dissection
specimen were selected in the tumor and peritumoral was performed in 44 patients and 14 of them had
stroma regions (10 from each). A customized Aperio positive regional lymph nodes. The majority of patients
algorithm (based on the default algorithm) was used on were diagnosed at stage I (n = 34) and stage II (n = 5)
these regions of interests to identify all cells within the diseases. Only 1 patient had stage III and 2 patients had
region and classify them into one of 4 categories: stage IV disease. There were 3 patients with unstaged
negative (0), weak (1+), moderate (2+), or strong (3+) cancer. PD-L1 expression was significantly higher in
CD8 staining. We considered true positive only strongly tumor compared with normal tissue (Po0.001) and in
(3+) and moderately (2+) stained cells. CD8+ cells were grade 3 tumors compared with grade 2 lesions
used to calculate the percentage of lymphocytes within (P = 0.04). The difference was more pronounced
the selected tumor and stroma regions. The images were between moderately and poorly differentiated cancers
captured at 200× magnification and 20 random fields when using CPS scores (P = 0.027). Mean CPS was 3%
(100×100 μm) were selected for cell count analysis from for grade 2 CSCC and 14% for poorly differentiated
Int J Gynecol Pathol Vol. 00, No. 00, ’’ 2019
Copyright r 2019 International Society of Gynecological Pathologists.
4 O. SAGLAM ET AL.
CSCC. Patients with stage I disease (n = 34) had higher patchy staining pattern (Fig. 1C). Twelve samples of 22
PD-L1 expressing tumors compared with patient with poorly differentiated CSCC samples had matching
stage II, III, and IV disease (n = 8) (P = 0.026). positive or negative PD-L1 categorical results with
Clinicopathologic parameters such as patient’s age, TMA samples. Even though there was a positive trend,
LVI, tumor size, lymph node status, and OS did not PD-L1 expression did not correlate between TMA and
correlate with PD-L1 expression in TMA cohort. overlapping full-tissue sections from poorly differentiated
CSCC samples (P = 0.07). Four of 8 PD-L1 negative
tumors in categorical analysis had low CPS (1%–5%). In
Younger Patients With Poorly Differentiated CSCC one poorly differentiated CSCC sample, diffuse and
had Higher PD-L1 Expressing Tumors strong PD-L expression was limited to HSIL. Invasive
The subset of poorly differentiated CSCC (n = 22) from carcinoma component of the sample had 0% PD-L1
the TMA was studied more in depth by evaluating tumors expression score (Fig. 1D). Final result was recorded as
with available full sections for analysis. Table 1 shows 0% for the sample. There were no other HSIL in our
summary of clinicopathologic parameters and PD-L1 samples.
expression in poorly differentiated CSCC. The median The median patient age was 56 (34–73) for PD-L1
patient age was 47 (24–73). There were 16 stage I, 4 stage negative tumors and 36 (31–41) for diffuse PD-L1
II, and 2 stage IV disease. In categorical analyses, 8 (50% or more) expressing tumors. PD-L1 expression
samples (36%) had <1% PD-L1 expression and negative levels were correlated with diagnosis at young age
result. Fourteen samples expressed or diffusely expressed when PD-L1 was categorical variable (P = 0.028) and
PD-L1 antibody ( ≥ 1% PD-L1 expression). There was also in CPS analysis (P = 0.016). The median tumor
diffuse PD-L1 expression (50% or more membranous size was 2.5 cm for PD-L1 negative tumors and 4.5 cm
positivity) in 5 cases (23%) (Fig. 1A). CPS for PD-L1 for diffuse PD-L1 expressing tumors. The tumor size
varied from 0% to 80% (median: 5%). There were 4 cases was correlated with high PD-L1 expression with a
with 0% CPS. PD-L1 expression was localized around borderline significance (P = 0.048) in the categorical
tumor-stroma interface in 5 samples (Fig. 1B). All 5 analysis. The association was stronger in CPS result
samples had low total PD-L1 scores (5%–20%). (P = 0.014). Five of 8 lymph node positive patients
Remaining 8 cases with <50% PD-L1 expression had had tumor with no PD-L1 expression. None of the
patients with diffuse PD-L1 expressing tumors had
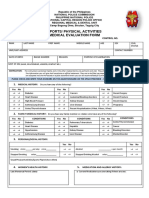
TABLE 1. Summary of clinicopathologic parameters positive regional lymph nodes. However, negative
and PD-L1 expression in poorly differentiated cervical
squamous cell carcinoma trend between PD-L1 expression and positive lymph
node status was not significant (P = 0.07). Fourteen of
Margin PD-L1
No. Age (yr) Stage status LIV tumor CPS (%) 22 samples had LVI. PD-L1 expression was inversely
associated with LVI in both categorical and CPS
1 34 I N Y Neg 5
2 53 II N Y Neg 5 analysis (P = 0.03). Other clinicopathologic parame-
3 36 I N N E 40 ters such as disease stage, margin status and OS did
4 57 I N Y E 5 not correlate with PD-L1 expression levels in poorly
5 38 I N Y DE 60
6 36 I N N DE 70 differentiated CSCC.
7 54 I N Y E 5
8 41 I N N DE 70
9 61 IV N Y Neg 1
10 62 II N Y E 20 High CD8+ T Cell Density in Both Tumor and Stroma
11 31 I N N DE 60 Correlates With Low-stage Disease
12 42 I N Y E 20 CD8+ TIL density was high (3+) within the neo-
13 61 IV N Y Neg 0
14 42 I N Y Neg 0 plastic tissue in 9 of 16 patients with stage I disease.
15 46 II N Y E 15 Fourteen of 16 stage I tumors and all stage II cancers
16 72 II Y Y E 5 (4 cases) had (3+) CD8 positivity in peritumoral stroma
17 33 I N N DE 80
18 24 I N Y E 1 (Fig. 2). None of the stage I and II cancers had (1+)
19 50 I N Y Neg 0 TIL levels in the surrounding stroma. In 2 stage IV
20 33 I N N E 10 cancers, TIL density was (1+) for neoplastic tissue and
21 73 I N N Neg 0
22 59 I N N Neg 5 (2+) for surrounding stroma. CD8+ T cell density both
in neoplastic tissue and stroma was positively correlated
CPS indicates combined positive score; DE, diffusely expressed;
E, expressed; LIV, lymphovascular involvement; N, no; Neg, with low-stage disease. CPS was associated with CD8+
negative; Y, yes. TIL density in tumor (P = 0.04) and stroma (P = 0.036).
Int J Gynecol Pathol Vol. 00, No. 00, ’’ 2019
Copyright r 2019 International Society of Gynecological Pathologists.
PD-L1 EXPRESSION IN CSCC 5
FIG. 1. PD-L1 expression in poorly differentiated cervical squamous cell carcinoma (CSCC). (A) Complete or partial membranous PD-L1
expression in > 50% of neoplastic cells (200×). (B) Interface staining pattern between tumor and peritumoral stroma (50×). Inset: localized
membranous staining in neoplastic cells (400×). (C) Patchy staining in neoplastic cells (200×). (D) Diffuse and strong PD-L1 expression in high-
grade squamous intraepithelial lesion and negative staining in the invasive CSCC (arrow) (200×).
There was no correlation between CD8+ TIL and the VEGF expression was localized to neoplastic tissue
patient age. Clinical follow-up period varied from 9 to and surrounding vasculature. Only marker expression
245 months in patients with poorly differentiated CSCC in the neoplastic tissue was evaluated. VEGF expres-
(mean: 113 mo). Patients with (1+), (2+) and (3+) CD8 sion varied from 0% to 20% (median: 1%). Even though
expressing tumors had different OS rates in univariate there was a negative trend between VEGF and PD-L1
analysis. After disease stage was adjusted for stage I and expression, the expression levels did not correlate in our
II cancers, high CD8+ TIL density in peritumoral limited sample size. There was no association between
stroma (3+ TIL) was associated with better OS rates VEGF expression and clinicopathologic parameters.
compared intermediate TIL levels (2+) (P = 0.009)
(Fig. 3). When we included patients with stage IV
DISCUSSION
cancers (n = 2) in survival analysis OS was not
correlated with high CD8+ T cell density. In analytic Immunotherapy can potentially be a significant
microscopy, CD8 percent score varied from 4.6 to 43 in treatment modality in cervical cancer as its oncogenesis
peritumoral stroma (median: 17%) and it was between involves presence of human papilloma virus infection as
7% and 53% for the neoplastic tissue (median: 10%). In an etiologic factor (2). Currently clinical trials are in
early-stage disease CD8 density within the stromal progress to determine efficacy of PD-1/PD-L1 blockers
tissue was also correlated with better survival rates in (21) in advanced cervical cancer. PD-L1 expression by
multivariate analysis (P = 0.016). immunohistochemistry has been tested as a biomarker
Int J Gynecol Pathol Vol. 00, No. 00, ’’ 2019
Copyright r 2019 International Society of Gynecological Pathologists.
6 O. SAGLAM ET AL.
FIG. 2. CD8+ tumor infiltrating lymphocytes (TIL). (A) (1+) staining in the peritumoral stroma: <5 CD8+ TIL (400×). (B) (2+) staining in the
peritumoral stroma: 6 to 19 TIL (400×). (C) (3+) staining in the peritumoral stroma: 20 or more TIL (400×). (D) (1+) staining in the neoplastic
tissue (400×). (E) (2+) staining in the neoplastic tissue (400×). (F) (3+) staining in the neoplastic tissue (400×).
to predict treatment response to anti PD-1/PD-L1 had clinical benefit from anti PD-L1 treatment (22). The
therapy with conflicting results in the literature. In some diagnostic challenges involved in interpretation of PD-
instances, patients whose tumors did not express PD-L1 L1 immunostaining include tumor heterogeneity, tran-
sient marker expression and lack of standard PD-L1
Hazard Ratio
readings (15). In cervical cancer, CPS evaluation is
Variable Level (95% CI) P Value recommended for the FDA-approved assays. We used
CD8 2+ 16.188 (2.033, 128.905) 0.009 both CPS and categorical analysis of PD-L1 expression
3+ - -
in the neoplastic tissue. The evaluation of full-tissue
Stage I 0.387 (0.091, 1.646) 0.199
II - - sections showed 3 distinct staining patterns in poorly
differentiated carcinoma: diffuse (50% or more mem-
Survivor Functions
1.0 branous positivity), focal/patchy, and interface pattern
with low CPS. The tumor-stroma interface staining
0.8 pattern was recognized by prior investigators (23) and
associated with better prognosis compared with diffuse
Survival Probability
0.6 PD-L1 expression in patients with CSCC (24). Only 5 of
22 poorly differentiated CSCC cases had diffuse CPS in
0.4 our samples. Interestingly, there was lack of correlation
between our PD-L1 scores on the TMA compared with
0.2 matching full-tissue section samples. This further con-
firms the spatial heterogeneity of marker expression,
0.0 which can potentially give positive or negative results
0 20 40 60 80 100 depending on the area tested. PD-L1 expression can also
OS
be a dynamic or transient process and be affected by
Group CD8=3+ CD8=2+
prior radiation treatment (25). Surgery was the first-line
FIG. 3. Overall survival (OS) rate and CD8+ tumor-infiltrating treatment modality in our cohort. Only one patient
lymphocytes (TIL) density in periturmoral stroma. Multivariable received radiation therapy before surgical treatment.
analysis shows that high CD8+ TIL density is associated with better
OS rates compared with intermediate TIL levels. CI indicates The majority of our patients was treated before the
confidence interval. practice shift to primary CCR therapy in advanced
Int J Gynecol Pathol Vol. 00, No. 00, ’’ 2019
Copyright r 2019 International Society of Gynecological Pathologists.
PD-L1 EXPRESSION IN CSCC 7
cervical carcinoma around early 2000s (26). It makes PD-L1 expression was associated with CD8+ T-cell
difficult to expand our sample size and limits the power levels both in tumor and peritumoral stroma in poorly
of our study. differentiated CSSC samples. In another human papil-
The level of PD-L1 expression is known to vary by loma virus–associated cancer, squamous cell carcinoma
tumor histologic subtype in cervical cancer. CSCC of head and neck (SCCHN) had similar association
samples express higher PD-L1 levels compared with between PD-L1 expression and CD8+ TIL levels. CD8+
adenocarcinoma and adenosquamous carcinoma of the T cells were found to express higher levels of PD-1 in
cervix (27). We showed poorly differentiated SCCC had tumor microenvironment (23). In addition aggressive
higher PD-L1 expression compared with grade 2 tumor morphology was correlated with high PD-L1
tumors. The result is comparable with poorly differ- levels and high CD3 and CD8 positive lymphocytic
entiated cancers involving bladder (28), endometrium infiltrates in SCCHN (38). In our poorly differentiated
(29), ovary (30) and the lung (31). However, lack of CSSC group, high-CD8+ TIL levels in peritumoral
well-differentiated CSCC samples in the TMA is one of stroma were correlated with low-stage disease and better
the shortcomings of our study. In addition to tumor OS rates even after disease stage was adjusted for
grade, the disease stage was also correlated with PD-L1 patients with stage I and II cancers. The limited sample
expression in TMA samples. There was a difference in size in advanced cancers precluded a detailed analysis of
PD-L1 expression between early-stage (stage I) and TIL density and OS. In agreement with our results in
higher stage disease. The limited sample size of early stage cancers, high CD8+ TIL levels were
advanced cancers (only 8 patients) hampers our result reportedly observed in lymph node-negative disease
and a cautious interpretation is required. Another (39) and low CD8/treg ratio was associated with poor
interesting but limited finding involved a sample. There survival rates (40) in cervical cancer. CD8+ TIL density
was a loss PD-L1 expression in the invasive carcinoma was also correlated with better survival outcomes in
even though diffuse and strong PD-L1 positivity was SCCHN (38,41) and non–small cell lung cancer (42).
noted in HSIL. In contrast to our observation a In summary, clinicopathologic features can be impor-
proportional increase in the marker expression with tant in selecting patients for pembroluzimab treatment in
the increasing grade of cervical intraepithelial neoplasia CSCC. PD-L1 expression was higher in grade 3 CSCC
and invasive SCC was reported in a prior study (32). compared with grade 2 samples. In addition, patient age,
Among the clinicopathologic parameters, young- tumor size, and LVI were all correlated with PD-L1
age was associated with high PD-L1 expression in expression in poorly differentiated CSCC. CD8+ TIL
poorly differentiated CSCC. Immune-senescence can levels in neoplastic tissue and peritumoral stroma were
be a plausible explanation for the result. In later life, positively correlated with PD-L1 expression. In poorly
thymic involution and lower amounts of T-cell differentiated CSCC, PD-L1 expression, and CD8+ TIL
progenitors from bone marrow result in very few density may define a subgroup of patients with relatively
naive T-cell production. Elderly people have marked better survival outcomes. Our results should be validated
expression of CD27 and CD28-negative and CD8+ in a larger patient cohort especially in patients treated
senescent T cells (33). In a recent meta-analysis the with prior CCR therapy.
efficacy of PD-1/PD-L1 blockers had comparable
results in adult patients younger and older than 65 yr
in current clinical trials involving head and neck, lung
REFERENCES
and kidney cancers (34). In contrast, hyper-progres-
sive disease was associated with old age and worse 1. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA
Cancer J Clin 2018;68:7–30.
OS in patients with non–small cell carcinoma treated 2. Lee SJ, Yang A, Wu TC, et al. Immunotherapy for human
with PD1/PD-L1 blockers (35). Other pathologic papillomavirus-associated disease and cervical cancer: review of
parameters associated with PD-L1 expressions were clinical and translational research. J Gynecol Oncol 2016;27:e51.
3. Verma J, Monk BJ, Wolfson AH. New strategies for multi-
tumor size and LVI. LVI was positively associated modality therapy in treating locally advanced cervix cancer.
with PD-L1 expression in several cancer types Semin Radiat Oncol 2016;26:344–8.
including endometrial (36) and lung cancers (37). 4. Pfaendler KS, Tewari KS. Changing paradigms in the systemic
treatment of advanced cervical cancer. Am J Obstet Gynecol
The negative correlation with LVI and PD-L1 2016;214:22–30.
expression in our study contradicts prior results, yet 5. Marnitz S, Kohler C, Muller M, et al. Indications for primary
our analysis focused on only poorly differentiated and secondary exenterations in patients with cervical cancer.
Gynecol Oncol 2006;103:1023–30.
CSCC samples. PD-L1 expression was not correlated 6. Goldberg GL, Sukumvanich P, Einstein MH, et al. Total pelvic
with LVI in our TMA cohort. exenteration: the Albert Einstein College of Medicine/Montefiore
Int J Gynecol Pathol Vol. 00, No. 00, ’’ 2019
Copyright r 2019 International Society of Gynecological Pathologists.
8 O. SAGLAM ET AL.
Medical Center Experience (1987 to 2003). Gynecol Oncol escape from NK cell cytotoxicity via IL-6-MEK/Erk signaling
2006;101:261–8. pathway. Oncotarget 2017;8:80506–20.
7. Boussios S, Seraj E, Zarkavelis G, et al. Management of 26. Maneo A, Landoni F, Cormio G, et al. Concurrent carboplatin/
patients with recurrent/advanced cervical cancer beyond first 5-fluorouracil and radiotherapy for recurrent cervical carcinoma.
line platinum regimens: where do we stand? A literature review. Ann Oncol 1999;10:803–7.
Crit Rev Oncol Hematol 2016;108:164–74. 27. Reddy OL, Shintaku PI, Moatamed NA. Programmed death-
8. Monk BJ, Sill MW, McMeekin DS, et al. Phase III trial of four ligand 1 (PD-L1) is expressed in a significant number of the
cisplatin-containing doublet combinations in stage IVB, recur- uterine cervical carcinomas. Diagn Pathol 2017;12:45.
rent, or persistent cervical carcinoma: a Gynecologic Oncology 28. Kawahara T, Ishiguro Y, Ohtake S, et al. PD-1 and PD-L1 are
Group study. J Clin Oncol 2009;27:4649–55. more highly expressed in high-grade bladder cancer than in low-
9. Tewari KS, Sill MW, Long HJ III, et al. Improved survival grade cases: PD-L1 might function as a mediator of stage
with bevacizumab in advanced cervical cancer. N Engl J Med progression in bladder cancer. BMC Urol 2018;18:97.
2014;370:734–43. 29. Rabal O, San Jose-Eneriz E, Agirre X, et al. Discovery of reversible
10. Monk BJ, Mas Lopez L, Zarba JJ, et al. Phase II, open-label study DNA methyltransferase and lysine methyltransferase G9a inhibitors
of pazopanib or lapatinib monotherapy compared with pazopanib with antitumoral in vivo efficacy. J Med Chem 2018;61:6518–45.
plus lapatinib combination therapy in patients with advanced and 30. Wieser V, Gaugg I, Fleischer M, et al. BRCA1/2 and TP53
recurrent cervical cancer. J Clin Oncol 2010;28:3562–9. mutation status associates with PD-1 and PD-L1 expression in
11. Tinker AV, Ellard S, Welch S, et al. Phase II study of ovarian cancer. Oncotarget 2018;9:17501–11.
temsirolimus (CCI-779) in women with recurrent, unresectable, 31. Driver BR, Miller RA, Miller T, et al. Programmed death ligand-
locally advanced or metastatic carcinoma of the cervix. A trial 1 (PD-L1) expression in either tumor cells or tumor-infiltrating
of the NCIC Clinical Trials Group (NCIC CTG IND 199). immune cells correlates with solid and high-grade lung adeno-
Gynecol Oncol 2013;130:269–74. carcinomas. Arch Pathol Lab Med 2017;141:1529–32.
12. Yang A, Farmer E, Lin J, et al. The current state of therapeutic 32. Yang W, Lu YP, Yang YZ, et al. Expressions of programmed
and T cell-based vaccines against human papillomaviruses. death (PD)-1 and PD-1 ligand (PD-L1) in cervical intra-
Virus Res 2017;231:148–65. epithelial neoplasia and cervical squamous cell carcinomas are
13. Sagae S, Monk BJ, Pujade-Lauraine E, et al. Advances and of prognostic value and associated with human papillomavirus
Concepts in Cervical Cancer Trials: A Road Map for the status. J Obstet Gynaecol Res 2017;43:1602–12.
Future. Int J Gynecol Cancer 2016;26:199–207. 33. Henson SM, Riddell NE, Akbar AN. Properties of end-stage
14. Sharpe AH, Wherry EJ, Ahmed R, et al. The function of human T cells defined by CD45RA re-expression. Curr Opin
programmed cell death 1 and its ligands in regulating Immunol 2012;24:476–81.
autoimmunity and infection. Nat Immunol 2007;8:239–45. 34. Elias R, Giobbie-Hurder A, McCleary NJ, et al. Efficacy of
15. Xu-Monette ZY, Zhang M, Li J, et al. PD-1/PD-L1 blockade: PD-1 & PD-L1 inhibitors in older adults: a meta-analysis.
have we found the key to unleash the antitumor immune J Immunother Cancer 2018;6:26.
response. Front Immunol 2017;8:1597. 35. Ferrara R, Mezquita L, Texier M, et al. Hyperprogressive
16. Riley JL. PD-1 signaling in primary T cells. Immunol Rev disease in patients with advanced non-small cell lung cancer
2009;229:114–25. treated with PD-1/PD-L1 inhibitors or with single-agent
17. Garon EB, Rizvi NA, Hui R, et al. Pembrolizumab for the chemotherapy. JAMA Oncol 2018;4:1543–52.
treatment of non-small-cell lung cancer. N Engl J Med 36. Crumley S, Kurnit K, Hudgens C, et al. Identification of a
2015;372:2018–28. subset of microsatellite-stable endometrial carcinoma with high
18. Herbst RS, Baas P, Kim DW, et al. Pembrolizumab versus PD-L1 and CD8+ lymphocytes. Mod Pathol 2018;32:396–404.
docetaxel for previously treated, PD-L1-positive, advanced 37. Shi X, Wu S, Sun J, et al. PD-L1 expression in lung
non-small-cell lung cancer (KEYNOTE-010): a randomised adenosquamous carcinomas compared with the more common
controlled trial. Lancet (London, England) 2016;387:1540–50. variants of non-small cell lung cancer. Sci Rep 2017;7:46209.
19. Gong J, Chehrazi-Raffle A, Reddi S, et al. Development of PD- 38. Karpathiou G, Casteillo F, Giroult JB, et al. Prognostic impact
1 and PD-L1 inhibitors as a form of cancer immunotherapy: of immune microenvironment in laryngeal and pharyngeal
a comprehensive review of registration trials and future squamous cell carcinoma: immune cell subtypes, immuno-
considerations. J Immunother Cancer 2018;6:8. suppressive pathways and clinicopathologic characteristics.
20. Zhang L, Conejo-Garcia JR, Katsaros D, et al. Intratumoral T Oncotarget 2017;8:19310–22.
cells, recurrence, and survival in epithelial ovarian cancer. 39. Piersma SJ, Jordanova ES, van Poelgeest MI, et al. High
N Engl J Med 2003;348:203–13. number of intraepithelial CD8+ tumor-infiltrating lymphocytes
21. Borcoman E, Le Tourneau C. Pembrolizumab in cervical is associated with the absence of lymph node metastases in
cancer: latest evidence and clinical usefulness. Ther Adv Med patients with large early-stage cervical cancer. Cancer Res
Oncol 2017;9:431–9. 2007;67:354–61.
22. Gibney GT, Weiner LM, Atkins MB. Predictive biomarkers for 40. Jordanova ES, Gorter A, Ayachi O, et al. Human leukocyte
checkpoint inhibitor-based immunotherapy. Lancet Oncol antigen class I, MHC class I chain-related molecule A, and CD8
2016;17:e542–51. +/regulatory T-cell ratio: which variable determines survival of
23. Lyford-Pike S, Peng S, Young GD, et al. Evidence for a role of cervical cancer patients. Clin Cancer Res 2008;14:2028–35.
the PD-1:PD-L1 pathway in immune resistance of HPV- 41. Ou D, Adam J, Garberis I, et al. Clinical relevance of tumor
associated head and neck squamous cell carcinoma. Cancer infiltrating lymphocytes, PD-L1 expression and correlation with
Res 2013;73:1733–41. HPV/p16 in head and neck cancer treated with bio- or chemo-
24. Heeren AM, Punt S, Bleeker MC, et al. Prognostic effect of radiotherapy. Oncoimmunology 2017;6:e1341030.
different PD-L1 expression patterns in squamous cell carcinoma 42. El-Guindy DM, Helal DS, Sabry NM, et al. Programmed cell
and adenocarcinoma of the cervix. Mod Pathol 2016;29:753–63. death ligand-1 (PD-L1) expression combined with CD8 tumor
25. Shen MJ, Xu LJ, Yang L, et al. Radiation alters PD-L1/ infiltrating lymphocytes density in non-small cell lung cancer
NKG2D ligand levels in lung cancer cells and leads to immune patients. J Egypt Natl Cancer Inst 2018;30:125–31.
Int J Gynecol Pathol Vol. 00, No. 00, ’’ 2019
Copyright r 2019 International Society of Gynecological Pathologists.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5825)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (903)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (541)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (823)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (403)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Management of Cerebral Edema, Brain Compression, and Intracranial PressureDocument29 pagesManagement of Cerebral Edema, Brain Compression, and Intracranial PressureNicolle Carrillo ForeroNo ratings yet
- 2010 Acr Criteria PDFDocument3 pages2010 Acr Criteria PDFMuhammad Abdul RahmanNo ratings yet
- Uterine CarcinosarcomaDocument8 pagesUterine CarcinosarcomaelisasitohangNo ratings yet
- Tumor Staging of Endocervical Adenocarcinoma .8Document10 pagesTumor Staging of Endocervical Adenocarcinoma .8elisasitohangNo ratings yet
- Buku Biopsi InterpretationDocument552 pagesBuku Biopsi InterpretationelisasitohangNo ratings yet
- Gambar Warna UrineDocument1 pageGambar Warna UrineelisasitohangNo ratings yet
- Pathophysiology of GERD and Its ComplicationDocument25 pagesPathophysiology of GERD and Its ComplicationalmiraNo ratings yet
- Budd - Chiari (Hepatic VenousDocument43 pagesBudd - Chiari (Hepatic VenousRamy ElbarodyNo ratings yet
- Panc Adenocarcinoma Recent Data and Perspective JR Delpero HPB Course 2022 V4-NuoveDocument176 pagesPanc Adenocarcinoma Recent Data and Perspective JR Delpero HPB Course 2022 V4-NuoveDiana MitreaNo ratings yet
- Prepared by Inzar Yasin Ammar LabibDocument47 pagesPrepared by Inzar Yasin Ammar LabibJohn Clements Galiza100% (1)
- Nosocomial Infection Control - White Paper - Greg Luther - BioWarn LLCDocument10 pagesNosocomial Infection Control - White Paper - Greg Luther - BioWarn LLCGregNo ratings yet
- Cardiac-Cath-Lab FormDocument3 pagesCardiac-Cath-Lab FormMr ShoaiBiNo ratings yet
- Pre Medical Evaluatiom Form PFT 1 PDFDocument2 pagesPre Medical Evaluatiom Form PFT 1 PDFAIEN WENDELEIH Q. CAPINPIN100% (2)
- Medical Surgical Nursing Exam 1Document23 pagesMedical Surgical Nursing Exam 1Zymer Lee AbasoloNo ratings yet
- Picornaviridae - CDocument9 pagesPicornaviridae - Cميمونه عبد الرحيم مصطفىNo ratings yet
- Ger10357 FMDocument2 pagesGer10357 FMTryas YulithaNo ratings yet
- Excited DeliriumDocument10 pagesExcited DeliriumMujahidul HasanNo ratings yet
- Alexis Mirar PcsoDocument3 pagesAlexis Mirar Pcsodivine mercyNo ratings yet
- Neckdissections 130421031843 Phpapp02Document62 pagesNeckdissections 130421031843 Phpapp02azizNo ratings yet
- Disfagia Sarcopenica y Fragilidad OralDocument23 pagesDisfagia Sarcopenica y Fragilidad OralPatriciaNo ratings yet
- Renal Calculi IntroductionDocument4 pagesRenal Calculi IntroductionirysatherfinestNo ratings yet
- Anorectal DiseaseDocument122 pagesAnorectal DiseasejolagusuNo ratings yet
- @ebookmedicinee2021 Hayat Tumors of The Central Nervous SystemDocument132 pages@ebookmedicinee2021 Hayat Tumors of The Central Nervous Systemvito100% (1)
- Emphysematous Cystitis: A Radiographic Diagnosis: Meriam Islam, Aaron Singh Bancil, Owen IngramDocument2 pagesEmphysematous Cystitis: A Radiographic Diagnosis: Meriam Islam, Aaron Singh Bancil, Owen IngramR9. agam maulanaNo ratings yet
- Melody Doria - Chapter 20 ActivityDocument3 pagesMelody Doria - Chapter 20 ActivityMelody MirandaNo ratings yet
- Principles of RadiotherapyDocument41 pagesPrinciples of Radiotherapywabaly100% (1)
- Impaired Skin IntegrityDocument3 pagesImpaired Skin IntegrityAubrey SungaNo ratings yet
- NDT Lab - Finals (Transes)Document19 pagesNDT Lab - Finals (Transes)Aleah JayaganNo ratings yet
- Si Gede Teguh Surya Negara 011.06.0043: 28/08/2017 1 FK Unizar Mataram 2017Document50 pagesSi Gede Teguh Surya Negara 011.06.0043: 28/08/2017 1 FK Unizar Mataram 2017'aac' JujuuNo ratings yet
- Sugar and Blood 2Document19 pagesSugar and Blood 2shaira ubaldeNo ratings yet
- Summative Test No. 2 4 Quarter Name: - ScoreDocument2 pagesSummative Test No. 2 4 Quarter Name: - ScoreRobieDeLeonNo ratings yet
- Irritable Bowel Syndrome (IBS) - Symptoms - NHSDocument3 pagesIrritable Bowel Syndrome (IBS) - Symptoms - NHSadni_wgNo ratings yet
- What Is Outpatient Treatment ProgramDocument3 pagesWhat Is Outpatient Treatment ProgramSharon DikirrNo ratings yet
- Ganzoni Equation For Iron Deficiency AnemiaDocument1 pageGanzoni Equation For Iron Deficiency AnemiaL ZANo ratings yet