Professional Documents
Culture Documents
Patient-Centered Collaborative Care: The Impact of A New Approach To Postpartum Rounds On Residents' Perception of Their Work Environment
Patient-Centered Collaborative Care: The Impact of A New Approach To Postpartum Rounds On Residents' Perception of Their Work Environment
Uploaded by
Setiaty PandiaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Patient-Centered Collaborative Care: The Impact of A New Approach To Postpartum Rounds On Residents' Perception of Their Work Environment
Patient-Centered Collaborative Care: The Impact of A New Approach To Postpartum Rounds On Residents' Perception of Their Work Environment
Uploaded by
Setiaty PandiaCopyright:
Available Formats
ORIGINAL RESEARCH
Patient-Centered Collaborative Care: Maureen Baldwin, MD, MPH
The Impact of a New Approach to Jason Hashima, MD, MPH
Jeanne-Marie Guise, MD, PhD
Postpartum Rounds on Residents’ William Thomas Gregory, MD
Alison Edelman, MD, MPH
Perception of Their Work Environment Sally Segel, MD
Abstract
Objective At our institution, traditional postpartum Results Ninety-two percent of the obstetrics residents
rounds consisted of separate visits from all members of (n 5 23) completed the preintervention survey, and 79%
the obstetric team. This led to patient care inefficiencies (n 5 19) completed the postintervention survey. For most
and miscommunication. In an effort to improve patient measures, there was no difference in resident perception
care, patient-centered collaborative care (PCCC) was between the 2 time points. After implementation of PCCC
established, whereby physicians, residents, medical rounds, fewer residents felt that rounds were educational
students, nurses, case managers, and social workers (preintervention 5 39%, postintervention 5 7%; P 5
conduct rounds as a team. The goal of this observational .03).
study was to evaluate how PCCC rounds affected resident Conclusion Residents did not report negative impacts on
physicians’ assessment of their work environment. workflow, cohesion, or general well-being after the
Methods Obstetrics and gynecology residents completed implementation of PCCC rounds. However, there was a
a 13-question written survey designed to assess their perception that PCCC rounds negatively impacted the
sense of workflow, education, and workplace cohesion. educational value of postpartum rounds. This
Surveys were completed before and 6 months after the information will help identify ways to improve the
implementation of PCCC. Responses were compared in resident physician experience in the obstetric service
aggregate for preintervention and postintervention with while optimizing patient care.
Pearson x2 test.
Introduction rounding formats have been shown to successfully reduce
Typical inpatient postpartum rounds at a teaching hospital costs, shorten hospital stays, and facilitate the implementation
involve several independent visits by nurses, medical students, of standardized disease-specific protocols.2,3
residents, and attending physicians. An increased focus on Most literature on interdisciplinary rounds points toward
safety, patient-centered care, and satisfaction has led to a benefit for physicians, physician learners, and patients in
innovations in the approach to inpatient rounds.1 One such the assessment of care as well as objective measures for
innovation is the development of interdisciplinary rounds, improved care. Studies addressing the educational merits of
which involves learners of all levels as well as other important interdisciplinary rounds are rare. One such study observed
hospital staff involved in regular patient care. Interdisciplinary whether patients and physician learners preferred bedside
case presentations versus hallway or conference room
presentations. Most patients preferred bedside presentations
All authors are at Oregon Health & Science University. Maureen Baldwin, MD,
MPH, is Resident in Obstetrics-Gynecology; Jason Hashima, MD, MPH, is (85%), but most physician learners and students preferred
Fellow in Maternal-Fetal Medicine; Jeanne-Marie Guise, MD, PhD, is Associate presentations away from the bedside (95%).4 Two studies by
Professor of Obstetrics-Gynecology; William Thomas Gregory, MD, is Associate
Professor of Obstetrics-Gynecology; Alison Edelman, MD, MPH, is Assistant the same group5,6 demonstrated that patients preferred to be
Professor of Obstetrics-Gynecology; and Sally Segel, MD, is Assistant Professor included in the conversations about their care.
of Maternal-Fetal Medicine.
Few studies have evaluated the effect of bedside
This work was presented in a poster at the Annual Clinical Meeting for the presentation or interdisciplinary rounds on physicians,
American College of Obstetricians and Gynecologists in May 2009 in Chicago,
Illinois. particularly residents. One study, which compared
communication between nurses and physicians for
Corresponding author: Maureen Baldwin, MD, MPH, Oregon Health & Science
University, 2181 SW Sam Jackson Park Rd, L446, Portland, OR 97239, interdisciplinary rounds and traditional rounds,
503.819.7747, schaum@ohsu.edu demonstrated a significantly improved impression of
Received September 23, 2009; revision received November 26, 2009, accepted communication with interdisciplinary rounds between
December 23, 2009. physicians and nurses, particularly for residents.7 Though
DOI: 10.4300/JGME-D-09-00058.1 no significant improvement in the impression of
62 Journal of Graduate Medical Education, March 2010
ORIGINAL RESEARCH
communication between physicians and nurses was or off-going nurse, the nurse case manager, social worker,
demonstrated in this study, the time interval between medical student, obstetrics-gynecology resident, obstetrics-
implementation of PCCC rounds and the follow-up survey gynecology intern or off-service intern, attending physician,
was relatively short and there were no specific survey mobile computer, and Spanish translator or phone
questions regarding communication. translator if necessary.
All obstetrics and gynecology residents who would have
Department of Obstetrics and Gynecology, Oregon Health & the opportunity to work on the obstetric service, both before
Science University and after implementation of PCCC rounds, were eligible to
Our institution is an academic tertiary care facility, where complete a written survey. A record was kept of residents
residents on the obstetric service participate in the antepartum who had completed the surveys, to prevent duplication.
and postpartum care of women for approximately 250 These residents were then asked to complete an identical
deliveries per month. Traditional postpartum rounds survey after the PCCC rounding system had been in place for
consisted of serial patient visits by various levels of medical 6 months. To enable honest responses, the surveys were not
students, residents, and faculty, which would begin at 5:00 identifiable by resident. Therefore, it was not possible to
perform paired comparisons. The survey included 13
AM. Management plans were often deferred until the patients’
statements about workplace cohesion, work satisfaction, and
condition was presented in a group setting with the attending
education with 5-point Likert scale responses (1 5 strongly
physician, charge nurse, social worker, and case manager.
disagree, 2 5 disagree, 3 5 ambivalent, 4 5 agree, or
In the traditional system, rounds were inefficient and
5 5 strongly agree) and space for narrative comments. For
required duplication of patient evaluation. Patient
example, ‘‘I feel good about being on the OB team.’’ The
satisfaction was low, with multiple provider visits and a
postintervention survey also included 3 questions about
nonuniform or delayed plan, as demonstrated by
whether workplace interactions had changed since
postdischarge patient satisfaction surveys. The time
implementation of PCCC rounds.
constraints on resident responsibilities left little time to
Comparing the percentage of residents who agreed to
complete discharge paperwork, resulting in later discharge
statements about their work environment (agree, strongly
time. Lastly, the traditional rounding format did not
agree) for traditional rounds against those for PCCC rounds
account for the time needed for the attending physician to
was the primary outcome. Respondents were separated into
see each of the postpartum patients. On busy labor and
2 groups by those who agreed or strongly agreed and were
delivery days, some patients would not be seen by the
compared to those who responded that they were
attending physician until late in the afternoon, which
ambivalent, disagreed, or strongly disagreed for each survey
significantly delayed care plans or discharge. question.
Because medical students, interns, and off-service Statistical analysis included descriptive statistics and
residents were not observed during their patient Pearson x2 tests for categorical variables, with a level of
interactions, it was difficult to teach them about the normal significance of P , .05. All analyses were conducted with
postpartum examination and counseling and to give them Statistical Package for the Social Sciences (SPSS, version
feedback about their patient interactions. However, these 14.0 for Windows, Chicago, IL). This study was approved
experiences are necessary under educational objectives by the Oregon Health & Science University Institutional
developed by the Accreditation Council for Graduate Review Board.
Medical Education (ACGME) in 1999. The ACGME core
competencies include patient care, medical knowledge, Results
practice-based learning and improvement, interpersonal and
Twenty-three of 25 eligible residents (92%) completed the
communication skills, professionalism, and systems-based
pre-PCCC survey, and 19 of 22 eligible residents (86%)
practice. These are areas that residency programs have been
completed the post-PCCC survey. One resident was not
responsible for evaluating since 2002.8
eligible for the pre-PCCC survey because of no prior
Because of these concerns, a new patient-centered
experience with our traditional rounds. Four residents were
collaborative care (PCCC) rounds format was developed
not eligible for the post-PCCC survey: 2 because of lack of
and implemented in September 2007. Resident physicians experience with PCCC rounds and 2 because they had left
were surveyed to determine the impact of PCCC rounds on the program. All completed surveys were included in the
assessment of their work environment. The measures of analysis, regardless of whether a resident had completed
interest in the survey were questions related to workflow, both surveys.
education, and workplace cohesion. For most statements in the survey, resident responses did
not change significantly between traditional rounds and
Methods PCCC rounds. However, fewer residents agreed with the
The patient-centered collaborative care team at our statement ‘‘rounds are educational’’ after implementation of
institution consists of the patient and family, an on-coming PCCC rounds. Thirty-nine percent of residents agreed with
Journal of Graduate Medical Education, March 2010 63
ORIGINAL RESEARCH
Discussion
In our institution, the introduction of PCCC for postpartum
rounds has required adjustments in workflow for all
members of the care team. While the underlying premise of
the PCCC system was to improve patient care and
satisfaction, our survey was designed to anonymously assess
the impact of PCCC on the resident providers’ perception of
workflow, education, and workplace cohesion. The major
finding of this study is that resident perception of the
educational value of postpartum rounds decreased with the
implementation of PCCC rounds.
On traditional rounds, case-based teaching occurred in a
large group setting away from the patient rooms after the
patients had been seen by residents. Medical students
presented the patients’ condition and residents were called
on to devise a patient plan or educate the group about a
particular disease entity. Often the faculty would discuss a
treatment plan in depth, providing alternative strategies and
lively debate over disagreements. In contrast, on PCCC
rounds, the medical student presents the patient’s condition
outside the patient room, and case-based teaching occurs
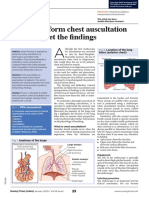
FI GU R E Comparison of Resident Responses to there, in a small group setting as time allows. Because of the
the Survey Statement, ‘‘Rounds Are increased amount of time needed for PCCC rounds, there is
Educational,’’ Before and After less time available for traditional case-based resident
Implementation of PCCC Rounds education for each patient, and residents are exposed to
management discussions for fewer overall patients.
However, the PCCC rounds format does allow faculty
to witness resident interactions with patients and, therefore,
to provide more directed teaching and feedback about
this statement during traditional rounds, as compared to
physical examination findings, and postpartum and follow-
7% for PCCC rounds, P 5 .03 (FI GUR E ).
up care. Attending physicians have commented that this is
The shift in rounding paradigms had no effect on
their only current format to witness resident interactions
residents’ positive perceptions of workplace cohesion. The with inpatients. The PCCC rounds have been able to
TABL E shows that after the introduction of PCCC rounds,
address the ACGME core competencies’ goals of
residents continued to feel valued by the obstetric team or professionalism and communication skills.
patient, feel respected, have a sense of cohesion and team The impression of a negative impact on resident
spirit, have a good relationship with the nurses, and feel education conveyed by this survey reflects the changing
good about being a member of the obstetric team. expectations for learners in the current medical education
Similarly, the change to the PCCC rounding system had environment. The expectation for resident learners has
no effect on residents’ negative perceptions regarding historically been that they be able to understand the disease
patient care and workflow. The survey revealed that entity, clinical assessment, treatment, and long-term
residents feel rushed during rounds, and that there is an management. However, residents have not always been
unequal burden on provider responsibility. Many residents challenged to communicate the assessment and plan to the
also reported feeling that patient care was compromised patient and have not always been the ones to answer
with the PCCC rounds, compared to the traditional rounds difficult patient questions, particularly in situations of
(20% versus 9%, P 5 .31). However, this was not uncertainty. In the PCCC rounds format, residents can be
statistically significant and would require further assessed while performing this skill in a supportive
investigation, as the response rate was lower for the environment in which the attending physician can reinforce
postintervention survey. a consistent message to the patient.
Not surprisingly, residents reported a decrease in the Residents were previously accustomed to a larger group
number of nursing calls regarding patient care after the format of formal presentation, with group decision-making,
implementation of PCCC rounds. During traditional during which they could absorb a large amount of
rounds, 48% of residents thought there were 10 or more information about all patients. However, the final decisions
calls per day about patient care, as compared to 13% after for treatment plans were often made later in the day, after
implementation of PCCC rounds (P 5 .03). the patient was seen by the attending physician, and the
64 Journal of Graduate Medical Education, March 2010
ORIGINAL RESEARCH
TA BLE Comparison of Resident Responses to Survey Questions Between Traditional and PCCC Rounds
Disagree or Ambivalent Agree x2
Survey Question Survey Type n % n % P value
Common sense of purpose Traditional 10 44 13 57 .85
PCCC rounds 7 47 8 53
I feel valued by OB team Traditional 7 30 16 70 .85
PCCC rounds 5 33 10 67
All providers listen actively Traditional 13 57 10 44 .32
PCCC rounds 6 40 9 60
All providers share responsibility Traditional 17 74 6 26 .75
PCCC rounds 11 79 3 21
I understand the problem-solving process Traditional 4 17 19 83 .84
PCCC rounds 3 20 12 80
I feel respected Traditional 7 30 16 70 .80
PCCC rounds 4 27 11 73
I feel good about being an OB team member Traditional 4 18 18 82 .24
PCCC rounds 5 36 9 64
OB team has a sense of cohesion and team spirit Traditional 9 39 14 61 .72
PCCC rounds 5 33 10 67
I have a good relationship with the nurses Traditional 10 44 13 57 .53
PCCC rounds 5 33 10 67
I feel valued by the patients Traditional 5 22 18 78 .23
PCCC rounds 6 40 9 60
Rounds are educational Traditional 14 61 9 39 .03a
PCCC rounds 14 93 1 7
I feel rushed during rounds Traditional 5 23 17 77 .78
PCCC rounds 4 27 11 73
Patient care is compromised in the current system Traditional 21 91 2 9 .31
PCCC rounds 12 80 3 20
Abbreviations: OB, obstetric; PCCC, patient-centered collaborative care.
a
statistically significant at p , 0.05.
reasoning for decisions was not always discussed. Our postpartum depression and evaluation of insurance
former case-based didactic teaching still continues, but on a coverage for contraception has been streamlined into the
smaller scale, whereby each resident conducts rounds for PCCC rounding format. Resident participation in
about half the patients, but is more responsible for multidisciplinary case management fulfills the systems-
understanding the patient characteristics and creating a plan based practice and practice-based learning goals of the
from start to finish. Residents are more hurried during ACGME core competencies.
PCCC rounds, so the perception is that there is less time for Most residents agreed that workplace cohesion exists, and
learning. But by explaining the plan to each patient at the this was not negatively impacted by PCCC rounds. Before
bedside, learners are creating a context for the case, which is PCCC rounds, residents rarely interacted with nurses directly
much easier to commit to memory. to discuss the patient care plan at the beginning of the shift.
Rounds in a multidisciplinary format have provided Instead, residents were frequently called by nursing staff
residents more insight into the roles of case management during the day to clarify a plan and to answer questions about
and social work in postpartum care. Screening for orders. The relationship between residents and nursing staff
Journal of Graduate Medical Education, March 2010 65
ORIGINAL RESEARCH
has improved now that more residents know the nurses by Finally, use of the interdisciplinary model as a platform for
name and interact directly with them on rounds. formal resident assessment of ACGME core competencies
This study was limited by the number of residents should be pursued.
involved and the inability to track an individual’s change in
response over time. Some of the survey questions were References
vague in their description of the ‘‘obstetrics team’’ and may 1 Zwarenstein M, Goldman J, Reeves S. Interprofessional collaboration: effects
have been misinterpreted by the residents as the current of practice-based interventions on professional practice and healthcare
resident obstetric team rather than the interdisciplinary outcomes. Cochrane Database of Syst Rev. 2009;(3) Art. No.: CD000072. DOI:
10.1002/14651858.CD000072.pub2. http://www.cochrane.org/reviews/en/
team. Furthermore, the time lapse from the beginning of ab000072.html.
implementation of PCCC rounds to the follow-up survey 2 Ellrodt G, Glasener R, Cadorette B, et al. Multidisciplinary rounds (MDR): an
implementation system for sustained improvement in the American Heart
was 6 months, but schedule adjustments had been ongoing
Association’s Get with the Guidelines program. Crit Pathw Cardiol.
during that period. This may have impacted residents 2007;6(3):106–116.
differently throughout the implementation period and may 3 Curley C, McEachern JE, Speroff T. A firm trial of interdisciplinary rounds on
the inpatient medical wards: an intervention designed using continuous
have changed their survey responses. quality improvement. Med Care. 1998;36(suppl 8):AS4-AS12.
Areas for further investigation include objective 4 Wang-Cheng RM, Barnas GP, Sigmann P, Riendl PA, Young MJ. Bedside case
assessment of the number of calls to residents by nursing presentations: why patients like them but learners don’t. J Gen Intern Med.
1989;4(4):284–287.
before and after implementation of PCCC rounds. The 5 Fletcher KE, Rankey DS, Stern DT. Bedside interactions from the other side of
survey demonstrated an impression of decreased volume of the bedrail. J Gen Intern Med. 2005;20(1):58–61.
pages from nursing to residents regarding questions about 6 Fletcher KE, Furney SL, Stern DT. Patients speak: what’s really important
about bedside interactions with physician teams. Teach Learn Med.
patient care, and it would be interesting to assess paging 2007;19(2):120–127.
volume during that time. Additionally, some concerns were 7 Vazirani S, Hays RD, Shapiro MF, Cowan M. Effect of a multidisciplinary
intervention on communication and collaboration among physicians and
raised about areas of improvement for patient safety and nurses. Am J Crit Care. 2005;14(1):71–77.
satisfaction because of negative resident responses to 8 Accreditation Council for Graduate Medical Education. Outcome project.
statements about patient care on the postpartum ward. http://www.acgme.org/Outcome/. Accessed August 11, 2009.
66 Journal of Graduate Medical Education, March 2010
You might also like
- Gateway B2+ Test Unit 1 ADocument6 pagesGateway B2+ Test Unit 1 Aana maria csalinas56% (9)
- Psychology and Health Notes - CIE Psychology A-LevelDocument18 pagesPsychology and Health Notes - CIE Psychology A-LevelRajasekar KrishnasamyNo ratings yet
- Social Sciences Geography (SSG302-22-AG) (Jul)Document8 pagesSocial Sciences Geography (SSG302-22-AG) (Jul)Valencia MohlalaNo ratings yet
- 60 Minutes-60 Questions: Mathematics TestDocument14 pages60 Minutes-60 Questions: Mathematics TestJihyun YeonNo ratings yet
- Utilizing Bedside Shift Report To Improve The Effectiveness of Shift HandoffDocument6 pagesUtilizing Bedside Shift Report To Improve The Effectiveness of Shift HandoffselviNo ratings yet
- The Case of The Port of Antwerp PDFDocument11 pagesThe Case of The Port of Antwerp PDFCastilla CarlosNo ratings yet
- Patient-Centered Collaborative Care: The Impact of A New Approach To Postpartum Rounds On Residents' Perception of Their Work EnvironmentDocument5 pagesPatient-Centered Collaborative Care: The Impact of A New Approach To Postpartum Rounds On Residents' Perception of Their Work EnvironmentSetiaty PandiaNo ratings yet
- The Result of Inpatient Lengths of Stay On Hospital Readmission RatesDocument8 pagesThe Result of Inpatient Lengths of Stay On Hospital Readmission Ratesapi-309980971No ratings yet
- Sample - Critical Review of ArticleDocument11 pagesSample - Critical Review of Articleacademicproffwritter100% (1)
- NUR 340 - Nursing Reasearch Problem-Based Research PaperDocument7 pagesNUR 340 - Nursing Reasearch Problem-Based Research Papercharlene doverNo ratings yet
- Bucknall 2016Document13 pagesBucknall 2016mnazri98No ratings yet
- 211.full Two Words To Improve Physician-Patient Communication What ElseDocument4 pages211.full Two Words To Improve Physician-Patient Communication What ElsepassionexcellenceNo ratings yet
- Effectiveness of Formal Observation in Inpatient Psychiatry in Preventing Adverse Outcomes: The State of The ScienceDocument7 pagesEffectiveness of Formal Observation in Inpatient Psychiatry in Preventing Adverse Outcomes: The State of The Sciencelovely99_dyahNo ratings yet
- Research Nurse FinDocument5 pagesResearch Nurse FinFredrickNo ratings yet
- Capstone PaperDocument6 pagesCapstone Paperapi-353940265No ratings yet
- Bmjopen 2014 006578Document18 pagesBmjopen 2014 006578Ortopedia HGMNo ratings yet
- Nur Final PaperDocument9 pagesNur Final Paperapi-404050277No ratings yet
- Capstone-Scholarly Capstone PaperDocument5 pagesCapstone-Scholarly Capstone Paperapi-653324233No ratings yet
- Bedside Nursing Handover A Case StudyDocument8 pagesBedside Nursing Handover A Case StudyAisha MagarangNo ratings yet
- Quality and Synthesis PaperDocument6 pagesQuality and Synthesis Paperapi-253093073No ratings yet
- Clinical Nursing JudgementDocument6 pagesClinical Nursing Judgementapi-507960658No ratings yet
- En CuestaDocument6 pagesEn CuestaToño VargasNo ratings yet
- Family-Centred Care in Paediatric and Neonatal Nursing - A Literature ReviewDocument4 pagesFamily-Centred Care in Paediatric and Neonatal Nursing - A Literature Reviewhyzypif0gif3No ratings yet
- Clinical Nursing Journal CapstoneDocument7 pagesClinical Nursing Journal Capstoneapi-455776552No ratings yet
- Researchproposal 328Document9 pagesResearchproposal 328api-291554509100% (3)
- Diabetes Spectr 2007 Derr 177 85Document9 pagesDiabetes Spectr 2007 Derr 177 85Juankarloz MedinaNo ratings yet
- Clinical Nursing Judgement PaperDocument6 pagesClinical Nursing Judgement Paperapi-663939857No ratings yet
- Clinical Nursing JudgementDocument6 pagesClinical Nursing Judgementapi-455775909No ratings yet
- Open VsDocument16 pagesOpen Vsapi-482726932No ratings yet
- Reflective JournalsDocument19 pagesReflective JournalsisisvlvtNo ratings yet
- Professional Med J Q 2013 20 6 973 980Document8 pagesProfessional Med J Q 2013 20 6 973 980Vikram AripakaNo ratings yet
- Bedside Nursing Handover A Case Studyijn - 1809Document9 pagesBedside Nursing Handover A Case Studyijn - 1809muhammad-antareja-lana-pratama-6821No ratings yet
- Ebp Paper 1Document11 pagesEbp Paper 1api-738483796No ratings yet
- Ramon Magsaysay Memorial Medical Center Inc. #64 Aurora Boulevard, Barangay Doña Imelda, Quezon CityDocument41 pagesRamon Magsaysay Memorial Medical Center Inc. #64 Aurora Boulevard, Barangay Doña Imelda, Quezon Cityjosemia1No ratings yet
- Detailed NotesDocument18 pagesDetailed NotesAleeza MalikNo ratings yet
- Impact of Supervision and Self-Assessment On Doctor-Patient Communication in Rural MexicoDocument9 pagesImpact of Supervision and Self-Assessment On Doctor-Patient Communication in Rural MexicoUtari UbNo ratings yet
- Improving Nurse Knowledge and Attitudes of Early Mobilization ofDocument68 pagesImproving Nurse Knowledge and Attitudes of Early Mobilization ofMuhammad Alif AlfajriqoNo ratings yet
- Managing Change Towards Bedside Shift ReportDocument12 pagesManaging Change Towards Bedside Shift Reportapi-438607141No ratings yet
- Leadership AnalysisDocument8 pagesLeadership Analysisapi-260554694No ratings yet
- ContentServer AspDocument6 pagesContentServer AspYuda FhunkshyangNo ratings yet
- Effects of Nursing RoundsDocument14 pagesEffects of Nursing RoundsTatiana SiregarNo ratings yet
- Ghosh 2021Document6 pagesGhosh 2021Yonatan MeshaNo ratings yet
- Clinical Nursing JudgmentDocument6 pagesClinical Nursing Judgmentapi-739523749No ratings yet
- Capstone PaperDocument5 pagesCapstone Paperapi-741814100No ratings yet
- Roy Adaptation Model-Based Nursing Diagnosis and Implementation Reduces TheDocument9 pagesRoy Adaptation Model-Based Nursing Diagnosis and Implementation Reduces TheRahayu SisriNo ratings yet
- Unit 4 Assessment: Literature ReviewDocument5 pagesUnit 4 Assessment: Literature Reviewyetunde badruNo ratings yet
- Compliance With Hand Therapy Programs - Therapist and Patients PerceptionsDocument10 pagesCompliance With Hand Therapy Programs - Therapist and Patients PerceptionssammyrasaNo ratings yet
- 908 FullDocument4 pages908 FullJorgecelyNo ratings yet
- Of The Effectiveness: A Study of Family Planning Clinics in The PhilippinesDocument8 pagesOf The Effectiveness: A Study of Family Planning Clinics in The PhilippinesJerome CabalesNo ratings yet
- An Insight Into Clinical Nursing JudgementDocument7 pagesAn Insight Into Clinical Nursing Judgementapi-546705901No ratings yet
- Kalisch - The Impact of Teamwork On Missed - Nursing CareDocument9 pagesKalisch - The Impact of Teamwork On Missed - Nursing CarePutri NabillaNo ratings yet
- Capstone Nursing PaperDocument6 pagesCapstone Nursing Paperapi-505543314No ratings yet
- Comprehensive Discharge Planning-Ebp PowerpointDocument45 pagesComprehensive Discharge Planning-Ebp Powerpointapi-24187790No ratings yet
- The Role of Nurse Practitioners in Care Coordination and TransitionDocument10 pagesThe Role of Nurse Practitioners in Care Coordination and Transitionapi-312364579No ratings yet
- Communication Between Anaesthesiologists and Patients-2Document5 pagesCommunication Between Anaesthesiologists and Patients-2Atahualpa YupanquiNo ratings yet
- Compliance With Universal Precautions in A Medical Practice With A High Rate of HIV InfectionDocument6 pagesCompliance With Universal Precautions in A Medical Practice With A High Rate of HIV InfectionDirga Rasyidin LNo ratings yet
- E027258 FullDocument10 pagesE027258 Fullshazwany nazarNo ratings yet
- Running Head: LITERATURE REVIEW 1Document8 pagesRunning Head: LITERATURE REVIEW 1Maxine FomunungNo ratings yet
- Effects of Nursing Rounds: On Patients' Call Light Use, Satisfaction, and SafetyDocument13 pagesEffects of Nursing Rounds: On Patients' Call Light Use, Satisfaction, and SafetyhanimozaghiNo ratings yet
- (Journal of Neurosurgery - Spine) Patient Misconceptions Concerning Lumbar Spondylosis Diagnosis and TreatmentDocument7 pages(Journal of Neurosurgery - Spine) Patient Misconceptions Concerning Lumbar Spondylosis Diagnosis and Treatmentefancoolhand09No ratings yet
- Clinical Nursing JudgementDocument7 pagesClinical Nursing Judgementapi-539065201No ratings yet
- Scholarly PaperDocument5 pagesScholarly Paperapi-663941296No ratings yet
- PROF JONA Casey Fink Nurse Retention ArticleDocument9 pagesPROF JONA Casey Fink Nurse Retention ArticleMaryam Teodosio Al JedawyNo ratings yet
- 019 - Ulil Chiqmatuss'diah - KMB 1Document4 pages019 - Ulil Chiqmatuss'diah - KMB 1Setiaty PandiaNo ratings yet
- 019 - Ulil Chiqmatussa'diah - EPN 2 - Assessment On Respiratory Problems..Document7 pages019 - Ulil Chiqmatussa'diah - EPN 2 - Assessment On Respiratory Problems..Setiaty PandiaNo ratings yet
- Simple East Asian Landscape Campaign - by SlidesgoDocument54 pagesSimple East Asian Landscape Campaign - by SlidesgoSetiaty PandiaNo ratings yet
- Assessment On Respiratory ProblemsDocument7 pagesAssessment On Respiratory ProblemsSetiaty PandiaNo ratings yet
- Qi Muslimah Talk 1 Ivana FixDocument16 pagesQi Muslimah Talk 1 Ivana FixSetiaty PandiaNo ratings yet
- Jurnal KMB Diva - 015Document10 pagesJurnal KMB Diva - 015Setiaty PandiaNo ratings yet
- 4927 20042 1 PBDocument7 pages4927 20042 1 PBSetiaty PandiaNo ratings yet
- 1385 FullDocument10 pages1385 FullSetiaty PandiaNo ratings yet
- Patient-Centered Collaborative Care: The Impact of A New Approach To Postpartum Rounds On Residents' Perception of Their Work EnvironmentDocument5 pagesPatient-Centered Collaborative Care: The Impact of A New Approach To Postpartum Rounds On Residents' Perception of Their Work EnvironmentSetiaty PandiaNo ratings yet
- Hubungan Tingkat Kecemasan Dengan Tingkat Kemandirian Activities of Daily Living Pada LansiaDocument8 pagesHubungan Tingkat Kecemasan Dengan Tingkat Kemandirian Activities of Daily Living Pada LansiaSetiaty PandiaNo ratings yet
- JCM 10 00522 v2Document12 pagesJCM 10 00522 v2Setiaty PandiaNo ratings yet
- Impact of Osteoarthritis On Activities of Daily LiDocument9 pagesImpact of Osteoarthritis On Activities of Daily LiSetiaty PandiaNo ratings yet
- Alat Ukur Untuk Menilai Kemampuan Fungsional Pasien Dengan Osteoartritis Lutut: Tinjauan PustakaDocument6 pagesAlat Ukur Untuk Menilai Kemampuan Fungsional Pasien Dengan Osteoartritis Lutut: Tinjauan PustakaSetiaty PandiaNo ratings yet
- Reike DIyah Setiawati - 042 - PSIK ADocument28 pagesReike DIyah Setiawati - 042 - PSIK ASetiaty PandiaNo ratings yet
- Health and Quality of Life OutcomesDocument8 pagesHealth and Quality of Life OutcomesSetiaty PandiaNo ratings yet
- Progress in Disaster Science: Jeremy Spoon, Drew Gerkey, Ram B. Chhetri, Alisa Rai, Umesh Basnet, Chelsea E. HunterDocument15 pagesProgress in Disaster Science: Jeremy Spoon, Drew Gerkey, Ram B. Chhetri, Alisa Rai, Umesh Basnet, Chelsea E. HunterSetiaty PandiaNo ratings yet
- Vital Signs and Monitoring - Podcast - IntermediateDocument4 pagesVital Signs and Monitoring - Podcast - IntermediateSetiaty PandiaNo ratings yet
- Material - Using Equipment For Patients' Examination - 019 - Ulil ChiqmatussadiahDocument2 pagesMaterial - Using Equipment For Patients' Examination - 019 - Ulil ChiqmatussadiahSetiaty PandiaNo ratings yet
- Faktor-Faktor Yang Berhubungan Dengan Terjadinya PreeklampsiaDocument13 pagesFaktor-Faktor Yang Berhubungan Dengan Terjadinya PreeklampsiaSetiaty PandiaNo ratings yet
- Consulatation Liaison Psychiatry English Lecture 2012 10Document58 pagesConsulatation Liaison Psychiatry English Lecture 2012 10Setiaty PandiaNo ratings yet
- 116-Article Text-415-1-10-20190507Document8 pages116-Article Text-415-1-10-20190507Setiaty PandiaNo ratings yet
- Alasan Dilakukannya 4 Kali Amandemen Uud 1945 Tujuan Dan Sejarah PerkembanganDocument11 pagesAlasan Dilakukannya 4 Kali Amandemen Uud 1945 Tujuan Dan Sejarah PerkembanganSetiaty PandiaNo ratings yet
- Deteksi Mycobacterium Tuberculosis Pada Sampel Sputum Menggunakan Teknik Loop-Mediated Isothermal Amplification (LAMP-TB)Document7 pagesDeteksi Mycobacterium Tuberculosis Pada Sampel Sputum Menggunakan Teknik Loop-Mediated Isothermal Amplification (LAMP-TB)Setiaty PandiaNo ratings yet
- Lista CartiDocument33 pagesLista CartiCris Ti67% (3)
- 25 Common Surgical ConditionsDocument3 pages25 Common Surgical ConditionsMu AbNo ratings yet
- Syllabus 8 SemDocument9 pagesSyllabus 8 SemRahulNo ratings yet
- HSM 541 Week 7 Course ProjectDocument5 pagesHSM 541 Week 7 Course ProjecttheresajonesasNo ratings yet
- 98 EntrepreneurshipDocument11 pages98 Entrepreneurshipdolly gorlakorakanaNo ratings yet
- Chapter IwarDocument20 pagesChapter IwartamilNo ratings yet
- KIK614441 IC Part1Document49 pagesKIK614441 IC Part1Hafid FajriNo ratings yet
- Csec 2015-2017 PoemsDocument8 pagesCsec 2015-2017 PoemsKaminie SinghNo ratings yet
- 1677071391BS German Final Term Result Jan 2023Document2 pages1677071391BS German Final Term Result Jan 2023Raja ZainNo ratings yet
- TosDocument2 pagesTosHubert S. Banting100% (1)
- Commander SK Trip and Status Diagnostic CodesDocument4 pagesCommander SK Trip and Status Diagnostic CodesNikolayNo ratings yet
- Sikkim PrintDocument3 pagesSikkim Printdinesh1407No ratings yet
- 31Document5 pages31iskricaman7No ratings yet
- Irrigation and Water Power Engineering by Dr. B. C. Punmia - Dr. Pande Brij Basi Lal - Ashok Kumar Jain - Arun Kumar JainDocument187 pagesIrrigation and Water Power Engineering by Dr. B. C. Punmia - Dr. Pande Brij Basi Lal - Ashok Kumar Jain - Arun Kumar JainSaritha Reddy85% (85)
- For Review OAPDocument144 pagesFor Review OAPKim John Rull NateNo ratings yet
- GGN DD 033 - D0 PDFDocument250 pagesGGN DD 033 - D0 PDFAkshit KhuranaNo ratings yet
- Chapter2 PDFDocument18 pagesChapter2 PDFshaik jaheerNo ratings yet
- Schools of Criminology A Comparative AnalysisDocument9 pagesSchools of Criminology A Comparative AnalysisSudeep MishraNo ratings yet
- Freud's Model of The Human Mind - Journal Psyche PDFDocument1 pageFreud's Model of The Human Mind - Journal Psyche PDFJazmen folkNo ratings yet
- UntitledDocument218 pagesUntitledAnshuman TripathyNo ratings yet
- Wilderness Survival - Edible and Medicinal Plants PDFDocument60 pagesWilderness Survival - Edible and Medicinal Plants PDFprivatnoNo ratings yet
- Unification SensibilityDocument3 pagesUnification SensibilityAhsan LavaNo ratings yet
- ASLA Investment PlanDocument8 pagesASLA Investment PlanYiannisNo ratings yet
- Control Systems Design TPDocument7 pagesControl Systems Design TPChhaylySrengNo ratings yet
- Cosmology GitaDocument122 pagesCosmology GitabaijumohanNo ratings yet
- LPI - Company Profile - 2022Document4 pagesLPI - Company Profile - 2022Chrisneil DelosreyesNo ratings yet