Professional Documents
Culture Documents
College of Health Sciences: Urdaneta City University
College of Health Sciences: Urdaneta City University
Uploaded by
Dan Dan ManaoisOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
College of Health Sciences: Urdaneta City University
College of Health Sciences: Urdaneta City University
Uploaded by
Dan Dan ManaoisCopyright:
Available Formats
URDANETA CITY UNIVERSITY
San Vicente West, Urdaneta City, Pangasinan 2428
COLLEGE OF HEALTH SCIENCES
Bachelor of Science in Nursing
NCM 118N- N231
Darlene Dana S. Manaois BSN IV-Block IV
Identify the different intervention for a specific shock. Cite the rationale for each
intervention.
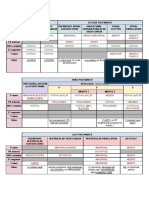
HYPOVOLEMIC SHOCK NURSING INTERVENTIONS
Safe administration of blood. It is important to acquire blood specimens quickly,
to obtain baseline complete blood count, and to type and crossmatch the blood in
anticipation of blood transfusions.
Safe administration of fluids. The nurse should monitor the patient closely for
cardiovascular overload, signs of difficulty of breathing, pulmonary edema, jugular
vein distention, and laboratory results.
Monitor weight. Monitor daily weight for sudden decreases, especially in the
presence of decreasing urine output or active fluid loss.
Monitor vital signs. Monitor vital signs of patients with deficient fluid volume every
15 minutes to 1 hour for the unstable patient, and every 4 hours for the stable
patient.
Oxygen administration. Oxygen is administered to increase the amount of oxygen
carried by available hemoglobin in the blood.
CARDIOGENIC SHOCK NURSING INTERVENTIONS
Prevent recurrence. Identifying at-risk patients early, promoting adequate
oxygenation of the heart muscle, and decreasing cardiac workload can prevent
cardiogenic shock.
Hemodynamic status. Arterial lines and ECG monitoring equipment must be well
maintained and functioning; changes in hemodynamic, cardiac, and pulmonary
status and laboratory values are documented and reported; and adventitious breath
sounds, changes in cardiac rhythm, and other abnormal physical assessment findings
are reported immediately.
Fluids. IV infusions must be observed closely because tissue necrosis and sloughing
may occur if vasopressor medications infiltrate the tissues, and it is also necessary to
monitor the intake and output.
Intra-aortic balloon counterpulsation. The nurse makes ongoing timing
adjustments of the balloon pump to maximize its effectiveness by synchronizing it
with the cardiac cycle.
Enhance safety and comfort. Administering of medication to relieve chest pain,
preventing infection at the multiple arterial and venous line insertion sites, protecting
the skin, and monitoring respiratory and renal functions help in safeguarding and
enhancing the comfort of the patient.
Arterial blood gas.Monitor ABG values to measure oxygenation and detect acidosis
from poor tissue perfusion.
Positioning. If the patient is on the IABP, reposition him often and perform passive
range of motion exercises to prevent skin breakdown, but don’t flex the patient’s
“ballooned” leg at the hip because this may displace or fracture the catheter.
ANAPHYLACTIC SHOCK NURSING INTERVENTIONS
Monitor client’s airway. Assess the client for the sensation of a narrowed airway.
Monitor the oxygenation status. Monitor oxygen saturation and arterial blood
gas values.
Focus breathing. Instruct the client to breathe slowly and deeply.
Positioning. Position the client upright as this position provides oxygenation by
promoting maximum chest expansion and is the position of choice during respiratory
distress.
Activity. Encourage adequate rest and limit activities to within client’s tolerance.
Hemodynamic parameters. Monitor the client’s central venous pressure (CVP),
pulmonary artery diastolic pressure (PADP), pulmonary capillary wedge pressure,
and cardiac output/cardiac index.
Monitor urine output. The renal system compensates for low blood pressure by
retaining water, and oliguria is a classic sign of inadequate renal perfusion.
Monitor client’s airway. Assess the client for the sensation of a narrowed airway.
Monitor the oxygenation status. Monitor oxygen saturation and arterial blood
gas values.
Focus breathing. Instruct the client to breathe slowly and deeply.
Positioning. Position the client upright as this position provides oxygenation by
promoting maximum chest expansion and is the position of choice during respiratory
distress.
Activity. Encourage adequate rest and limit activities to within client’s tolerance.
Hemodynamic parameters. Monitor the client’s central venous pressure (CVP),
pulmonary artery diastolic pressure (PADP), pulmonary capillary wedge pressure,
and cardiac output/cardiac index.
Monitor urine output. The renal system compensates for low blood pressure by
retaining water, and oliguria is a classic sign of inadequate renal perfusion.
SEPTIC SHOCK NURSING INTERVENTIONS
Infection control. All invasive procedures must be carried out with aseptic
technique after careful hand hygiene.
Collaboration. The nurse must collaborate with the other members of the
healthcare team to identify the site and source of sepsis and specific organisms
involved.
Management of fever. The nurse must monitor the patient closely for shivering.
Pharmacologic therapy. The nurse should administer prescribed IV fluids and
medications including antibiotic agents and vasoactive medications.
Monitor blood levels. The nurse must monitor antibiotic toxicity, BUN, creatinine,
WBC, hemoglobin, hematocrit, platelet levels, and coagulation studies.
Assess physiologic status. The nurse should assess the patient’s hemodynamic
status, fluid intake and output, and nutritional status.
NEUROGENIC SHOCK NURSING INTERVENTIONS
Elevate head of bed. Elevation of the head helps prevent the spread of the
anesthetic agent up the spinal cord when a patient receives spinal or epidural
anesthesia.
Lower extremity interventions. Applying anti-embolism stockings and elevating
the foot of the bed may help minimize pooling of the blood in the legs and prevent
thrombus formation.
Exercise. Passive range of motion of the immobile extremities helps promote
circulation.
Airway patency. Maintain patent airway: keep head in neutral position, elevate
head of bed slightly if tolerated, use airway adjuncts as indicated.
Oxygen. Administer oxygen by appropriate method (nasal prongs, mask, intubation,
ventilator).
Activities. Plan activities to provide uninterrupted rest periods and encourage
involvement within individual tolerance and ability.
BP monitoring. Measure and monitor BP before and after activity in acute phases or
until stable.
Reduce anxiety. Assist patient to recognize and compensate for alterations in
sensation.
You might also like
- Amazing DIY Breathing DeviceDocument60 pagesAmazing DIY Breathing DeviceArtour Rakhimov67% (9)
- Eclampsia Nursing Care Plan - Altered Tissue PerfusionDocument2 pagesEclampsia Nursing Care Plan - Altered Tissue PerfusionCyrus De Asis84% (32)
- Immediate Post-Operative CareDocument4 pagesImmediate Post-Operative CareHeidi Avediz Del Fuerte100% (1)
- Nursing Process of PneumoniaDocument5 pagesNursing Process of Pneumoniatin2x061275% (8)
- Orthopedic Inpatient Protocols: A Guide to Orthopedic Inpatient RoundingFrom EverandOrthopedic Inpatient Protocols: A Guide to Orthopedic Inpatient RoundingNo ratings yet
- Steth OgraphyDocument13 pagesSteth Ographyshahidkhan 6543216543210% (1)
- Promoting Adequate Gas ExchangeDocument5 pagesPromoting Adequate Gas Exchangeali sarjunipadangNo ratings yet
- Cardiac ComplicationDocument12 pagesCardiac ComplicationResa ShotsNo ratings yet
- DiagnosisDocument12 pagesDiagnosisHCX dghhqNo ratings yet
- DAY 6 SHOCK StudentsDocument38 pagesDAY 6 SHOCK StudentsTrisha UmaliNo ratings yet
- ShockDocument22 pagesShockDiana RamberNo ratings yet
- Basic NursingDocument7 pagesBasic Nursingbritishsam57No ratings yet
- Nursing Management of Patient With Mechanical VentilationDocument77 pagesNursing Management of Patient With Mechanical Ventilationrojina poudel0% (1)
- CABG PresentationDocument55 pagesCABG Presentationnmaykanathan100% (7)
- Hypovolemic Shock Nursing Care Management and Study GuideDocument1 pageHypovolemic Shock Nursing Care Management and Study GuideRoselyn VelascoNo ratings yet
- Nursing Diagnosis Impaired Gas ExchangeDocument7 pagesNursing Diagnosis Impaired Gas ExchangeZycon Rodney Ae'zecquel Gachallan50% (2)
- CP PowerpointDocument4 pagesCP PowerpointSallegoNo ratings yet
- Monitoring & Devices Used in ICU CCUDocument48 pagesMonitoring & Devices Used in ICU CCUProf. Ramsharan MehtaNo ratings yet
- Chapter 20 Nursing Management Postoperative CareDocument7 pagesChapter 20 Nursing Management Postoperative Caredcrisostomo8010No ratings yet
- Sanaani Nur Hathi M. Nso Jugular Venous Oximetry Staff Nurse 1Document7 pagesSanaani Nur Hathi M. Nso Jugular Venous Oximetry Staff Nurse 1Nur SanaaniNo ratings yet
- Postoperative PhaseDocument8 pagesPostoperative PhasereymarhayNo ratings yet
- 3E Group 4 H Dysfunction.Document6 pages3E Group 4 H Dysfunction.Shane PangilinanNo ratings yet
- Assess and Evaluate PatientDocument3 pagesAssess and Evaluate PatientCindy Babsa-ay MaslagNo ratings yet
- Intrapartal HypertensionDocument9 pagesIntrapartal Hypertensionnursereview100% (3)
- Medical Management: Can Help Control Weight, Blood Pressure and CholesterolDocument2 pagesMedical Management: Can Help Control Weight, Blood Pressure and CholesterolKen BaxNo ratings yet
- Cardiovascular System (Diagnostic Procedure) : Prepared By: Kriegel Paman Bihasa RM, RN, UsrnDocument17 pagesCardiovascular System (Diagnostic Procedure) : Prepared By: Kriegel Paman Bihasa RM, RN, UsrnKriegel Paman BihasaNo ratings yet
- Hypovolemic Shock Neurogenic ShockDocument40 pagesHypovolemic Shock Neurogenic ShockWemslaiNo ratings yet
- ABC ResuscitationDocument5 pagesABC ResuscitationIamTineshNo ratings yet
- Observing and Monitoring During General AnaesthesiaDocument7 pagesObserving and Monitoring During General AnaesthesiaREVATHY.ANo ratings yet
- 004 Practical-Manual PDFDocument72 pages004 Practical-Manual PDFRicardo Domingos100% (1)
- First Aid & EmergencyDocument3 pagesFirst Aid & Emergencybritishsam57No ratings yet
- Online LectureDocument9 pagesOnline LectureJobelle AcenaNo ratings yet
- Cabg TeachingDocument54 pagesCabg Teachingharmeet_dad100% (4)
- Flashcard Critical CareDocument11 pagesFlashcard Critical CaresnehaNo ratings yet
- Respiratory DisordersDocument8 pagesRespiratory DisordersCezanne CruzNo ratings yet
- Nursing Diagnosis Objectives Nursing Interventions Rationale EvaluationDocument9 pagesNursing Diagnosis Objectives Nursing Interventions Rationale EvaluationJezza Sanchez-Rellita VillariasNo ratings yet
- Total Anomalous Venous ReturnDocument4 pagesTotal Anomalous Venous ReturnJohn Bernard Ting TizonNo ratings yet
- Ineffective Tissue Perfusion R/T Impaired RAS Mechanism As Manifested by A High Blood Pressure LevelDocument3 pagesIneffective Tissue Perfusion R/T Impaired RAS Mechanism As Manifested by A High Blood Pressure LevelRiza Angela BarazanNo ratings yet
- Cardiogenic ShockDocument3 pagesCardiogenic Shockmerin sunilNo ratings yet
- Nursing Care Plan - EndocarditisDocument2 pagesNursing Care Plan - EndocarditisJoanna Marie Datahan Estomo100% (12)
- Blood TransfusionDocument27 pagesBlood Transfusionronalikapanda2005No ratings yet
- Req ERDocument9 pagesReq ERmayxzineNo ratings yet
- Objective DataDocument12 pagesObjective DataTherese BattungNo ratings yet
- SHOCKDocument17 pagesSHOCKChithra Saju100% (1)
- 4 Phases of IV Fluid Therapy FinalDocument29 pages4 Phases of IV Fluid Therapy FinalLuqmanul Hakim Junaidden100% (1)
- Shock: Ivan Mucharry Dalitan - PPDS Orthopaedi & Traumatologi Semester IVDocument5 pagesShock: Ivan Mucharry Dalitan - PPDS Orthopaedi & Traumatologi Semester IVusnulNo ratings yet
- Respiratory Emergencies PDFDocument4 pagesRespiratory Emergencies PDFAidan RajkumarNo ratings yet
- INTRAVENOUSDocument38 pagesINTRAVENOUSLorelyn DelfinNo ratings yet
- Perioperative Blood Pressure Control and ManagementDocument17 pagesPerioperative Blood Pressure Control and ManagementNathalia gallegoNo ratings yet
- Nursing Care Plan # 5Document5 pagesNursing Care Plan # 5Tin DuapaNo ratings yet
- 10 1016@j Anclin 2020 08 004Document11 pages10 1016@j Anclin 2020 08 004Luis David Gárate CastañedaNo ratings yet
- Mechanism of TraumaDocument46 pagesMechanism of TraumauutNo ratings yet
- Amniotic Fluid EmbolismDocument12 pagesAmniotic Fluid EmbolismSanchita PandeyNo ratings yet
- HemodialysisDocument4 pagesHemodialysisJon Adam Bermudez SamatraNo ratings yet
- CHP 66 Common Problems of Critical Care PatientsDocument18 pagesCHP 66 Common Problems of Critical Care Patientshops23No ratings yet
- Initial Assessment and Management Atls 10Document39 pagesInitial Assessment and Management Atls 10Fadhila K.100% (1)
- Case Study Multiple Organ Dysfunction and ShockDocument3 pagesCase Study Multiple Organ Dysfunction and ShockJrBong SemaneroNo ratings yet
- Post Operative MGTDocument10 pagesPost Operative MGTNatukunda DianahNo ratings yet
- Truma Sllide 3Document22 pagesTruma Sllide 3adnanreshunNo ratings yet
- 1 2 Revised UpdatedDocument26 pages1 2 Revised UpdatedDan Dan ManaoisNo ratings yet
- Chapter 5Document32 pagesChapter 5Dan Dan ManaoisNo ratings yet
- AppendicesDocument2 pagesAppendicesDan Dan ManaoisNo ratings yet
- Study Guide:: DialysisDocument8 pagesStudy Guide:: DialysisDan Dan ManaoisNo ratings yet
- Urdaneta City University: Nursing Care PlanDocument3 pagesUrdaneta City University: Nursing Care PlanDan Dan ManaoisNo ratings yet
- Chapter 1Document28 pagesChapter 1Dan Dan ManaoisNo ratings yet
- College of Health Sciences: Urdaneta City UniversityDocument3 pagesCollege of Health Sciences: Urdaneta City UniversityDan Dan ManaoisNo ratings yet
- Manaois - Culturally Competent Health Care OrganizationsDocument2 pagesManaois - Culturally Competent Health Care OrganizationsDan Dan ManaoisNo ratings yet
- College of Health Sciences: Urdaneta City UniversityDocument1 pageCollege of Health Sciences: Urdaneta City UniversityDan Dan ManaoisNo ratings yet
- Manaois NCP On HyperthermiaDocument1 pageManaois NCP On HyperthermiaDan Dan ManaoisNo ratings yet
- Shock and Multisystem Failure: Rudolf M. TanDocument22 pagesShock and Multisystem Failure: Rudolf M. TanDan Dan ManaoisNo ratings yet
- Study Guide:: DialysisDocument13 pagesStudy Guide:: DialysisDan Dan ManaoisNo ratings yet
- Misread Chest X Ray Role PlayDocument2 pagesMisread Chest X Ray Role PlayDan Dan ManaoisNo ratings yet
- Misread Chest X-Ray of The Patient Led To Respiratory Failure and DeathDocument2 pagesMisread Chest X-Ray of The Patient Led To Respiratory Failure and DeathDan Dan ManaoisNo ratings yet
- College of Health Sciences: Urdaneta City UniversityDocument5 pagesCollege of Health Sciences: Urdaneta City UniversityDan Dan ManaoisNo ratings yet
- Study Guide 7-Nursing Practice and The Law: Topic OutlineDocument14 pagesStudy Guide 7-Nursing Practice and The Law: Topic OutlineDan Dan ManaoisNo ratings yet
- Two Year Old With Spiking Fevers and Depressed Level of ConsciousnessDocument8 pagesTwo Year Old With Spiking Fevers and Depressed Level of ConsciousnessDan Dan ManaoisNo ratings yet
- Cardiovascular Summary Saunders Comprehensive Review For The Nclex RN ExaminationDocument40 pagesCardiovascular Summary Saunders Comprehensive Review For The Nclex RN ExaminationdanicaNo ratings yet
- CH 01Document12 pagesCH 01TahmidNo ratings yet
- Unit 5 Respiration, Internal Environment, Coordination and Gene TechnologyDocument55 pagesUnit 5 Respiration, Internal Environment, Coordination and Gene TechnologyMaha NaserNo ratings yet
- Respiration Worksheet - AnswersDocument5 pagesRespiration Worksheet - AnswersSophia NgNo ratings yet
- Chapter 4Document80 pagesChapter 4Dever GeronaNo ratings yet
- Anesthetics Inhalation SevofluranceDocument2 pagesAnesthetics Inhalation SevofluranceFatinahNo ratings yet
- Fitness GoalsDocument14 pagesFitness GoalsAlyanna CunananNo ratings yet
- Beta-Adrenergic BlockersDocument14 pagesBeta-Adrenergic BlockersAnonymous NVAWeVWNo ratings yet
- Potter, Perry, (2010) - Fundamental of Nursing Fundamental Keperawatan, Ed 7 Buku 2Document3 pagesPotter, Perry, (2010) - Fundamental of Nursing Fundamental Keperawatan, Ed 7 Buku 2KelvinNo ratings yet
- Capnography ExplainedDocument22 pagesCapnography ExplainedmarceloNo ratings yet
- Respi Demo Lesson PlanDocument6 pagesRespi Demo Lesson PlanBunny BansNo ratings yet
- BurnsDocument31 pagesBurnsLouis Carlos RoderosNo ratings yet
- Maharlika Highway, Brgy. Magsaysay, Lopez, Quezon: Lopez National Comprehensive High SchoolDocument5 pagesMaharlika Highway, Brgy. Magsaysay, Lopez, Quezon: Lopez National Comprehensive High SchoolJoenell CabungcalNo ratings yet
- BurnDocument67 pagesBurnhossein boloorianNo ratings yet
- Sarcodes: The Important Sarcodes Are Adrenalinum Cholesterinum Insulinum Pituitarinum Pepsinum Pancreatinum ThyroidinumDocument17 pagesSarcodes: The Important Sarcodes Are Adrenalinum Cholesterinum Insulinum Pituitarinum Pepsinum Pancreatinum ThyroidinumMADHURI DHUMAKNo ratings yet
- Virtual Heart Dissection PDFDocument7 pagesVirtual Heart Dissection PDFrosalyn gaboniNo ratings yet
- NCM 118 MIDTERMS PG 7Document1 pageNCM 118 MIDTERMS PG 7Kai SamaNo ratings yet
- Group 6 Part 1 Review of The Aging of Physiological System Notes Part 1Document7 pagesGroup 6 Part 1 Review of The Aging of Physiological System Notes Part 1Crissan Jejomar AbanesNo ratings yet
- Baby Sleep Simplified Newborn Sleep Schedules + Patterns - Nested BeanDocument1 pageBaby Sleep Simplified Newborn Sleep Schedules + Patterns - Nested BeanWinnie NginaNo ratings yet
- Seattle Angina QuestionnaireDocument6 pagesSeattle Angina QuestionnaireAmelia SianiparNo ratings yet
- Inflammation & Healing of Soft & Hard TissueDocument3 pagesInflammation & Healing of Soft & Hard TissueLakshita PrajapatiNo ratings yet
- ACLS Megacode Checklist For StudentsDocument3 pagesACLS Megacode Checklist For StudentsKhrisha Anne DavilloNo ratings yet
- Pressure Ulcer CareDocument26 pagesPressure Ulcer CarekurapotaNo ratings yet
- Calvin Cycle (Dark Reactions / Light Independent Reaction)Document47 pagesCalvin Cycle (Dark Reactions / Light Independent Reaction)L'ya Lieslotte100% (2)
- BiofeedbackDocument15 pagesBiofeedbackSofía Esquivel100% (1)
- Q1 Periodic Test in Science 9Document4 pagesQ1 Periodic Test in Science 9Jezha Mae NelmidaNo ratings yet
- Job Shift Meal Plan by Guru MannDocument4 pagesJob Shift Meal Plan by Guru MannMajid KhanNo ratings yet
- Case Reports AbstractsDocument7 pagesCase Reports AbstractsNovie AstiniNo ratings yet