Professional Documents
Culture Documents
Cost Stdunitcost Thailand
Cost Stdunitcost Thailand
Uploaded by
Ery SetiawanOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Cost Stdunitcost Thailand
Cost Stdunitcost Thailand
Uploaded by
Ery SetiawanCopyright:
Available Formats
See discussions, stats, and author profiles for this publication at: https://www.researchgate.
net/publication/263431375
Standard cost lists for health economic evaluation in Thailand
Article in Journal of the Medical Association of Thailand = Chotmaihet thangphaet · May 2014
Source: PubMed
CITATIONS READS
31 2,144
1 author:
Arthorn Riewpaiboon
Mahidol University
105 PUBLICATIONS 1,366 CITATIONS
SEE PROFILE
Some of the authors of this publication are also working on these related projects:
Epidemiological and Economic Burden of AMR in Thailand View project
Systematic review in unit cost of medical services in Asia View project
All content following this page was uploaded by Arthorn Riewpaiboon on 11 April 2016.
The user has requested enhancement of the downloaded file.
Standard Cost Lists for Health Economic Evaluation
in Thailand
Arthorn Riewpaiboon BPharm, MSc, PhD*
* Social and Administrative Pharmacy Excellence Research (SAPER) Unit, Department of Pharmacy,
Faculty of Pharmacy, Mahidol University, Bangkok, Thailand
This analysis was undertaken to generate a set of standard costs for medical services and those incurred by patients
receiving treatment, for use in health economic evaluations. Medical service unit cost data were derived from a survey of
3,091 hospital medical services in five hospitals, disaggregated by type of hospital (district or provincial/regional) and
analyzed using the relative value unit method. Patient-borne ambulatory cost values were derived from data gathered
through 905 patient interviews that took place in six health centers, three district hospitals, and three provincial/regional
hospitals. The survey gathered data on costs a rising from the distance travelled to access the medical service, the time spent
in the healthcare facility, as well as travel and meal costs. The analysis generated a set of standard cost data for Thailand that
will make conducting economic evaluations more accurate, faster, and more convenient, as well as allowing better comparability
between studies. This is the first standard cost menu that has been developed specifically for Thailand, and as such should be
revised and refined in the future. Some areas that would benefit from revision are suggested.
Keywords: Medical service, Unit cost, Standard cost list, Health economic evaluation, Thailand
J Med Assoc Thai 2014; 97 (Suppl. 5): S127-S134
Full text. e-Journal: http://www.jmatonline.com
Economic evaluation is a tool that is widely The costing process involves three basic
used tool to aid decision-making, both from a practical, steps: identification, measurement, and valuation of
individual standpoint and as part of the development resource use(4,5). While the first two steps are relatively
of national policies. Despite this, implementation of straightforward, the final step-valuation-involves
the approach is not always straightforward. One issue multiplying the unit cost of the resource in question by
that can impede accurate economic evaluation is the the quantity used. For medical services, the unit cost
process of obtaining accurate cost measurements, can be determined by direct measurement, standard or
which may be derived using a variety of concepts, reference lists for both price and cost, average market
methods, and reference values(1,2). This can lead to prices, or estimation(6). While the specific objective and
instances where one technology is assigned various limitations of some studies may mean that average
different values, as a result of the researchers using market prices, or estimation are used to determine unit
different methods and/or references in the calculations. cost, in general, the use of direct measurement or
This difference in costing may not necessarily reflect a standard/reference cost lists is preferred. Using direct
real difference in resource usage, but merely a different measurement at a study site to ascertain unit cost is
calculation approach on the part of the researcher. One appropriate when the results are to be used for
recent study in Thailand found that the capital cost of organizational management, while standard unit cost
a district hospital calculated using an economic is used when the results are needed for national-level
approach was 13% higher than that calculated using management.
an accounting approach. The same study also found In Thailand, health economic evaluation (HEE)
that using a 6% discount rate comparing to 3% rate is a standard tool that is used to inform policy
increased the calculated cost by 4.8%(3). development. For instance, before a new drug is
included on the national list of essential drugs it must
Correspondence to: first be subjected to an HEE; the same is true for a new
Riewpaiboon A, Social and Administrative Pharmacy treatment regimen, before it is accepted for coverage
Excellence Research (SAPER) Unit, Department of Pharmacy, under the national health insurance benefit package.
Faculty of Pharmacy, Mahidol University, 447 Sri Ayutthaya
Road, Ratchathewi, Bangkok 10400, Thailand.
To establish standardized study methods in 2008, the
Phone: 0-2644-8677-90 ext. 5745, Fax: 0-2644-8694 Health Intervention and Technology Assessment
E-mail: arthorn.rie@mahidol.ac.th Program (HITAP) of the Ministry of Public Health
J Med Assoc Thai Vol. 97 Suppl. 5 2014 S127
developed a set of National Health Technology each service. The method starts by measuring the direct
Assessment Guidelines, published in book form and in cost (labor, material, and capital costs) of each service.
the Journal of the Medical Association of Thailand After that, the sum of direct costs of all services is
(volume 91, supplement 2)(7). These guidelines included subtracted from the full cost, resulting in indirect cost
a chapter on measurement of costs written by this (of the service outputs). Finally, the indirect cost is
author(8,9). Although the establishment of national allocated to each service, and then added to the direct
standard guidelines on cost measurement has provided cost to obtain the unit cost.
researchers with much more clarity, conducting For the RCC method, the unit price of each
comparisons between studies at a national level remains service is multiplied by the number of service outputs,
a challenge, as researchers continue to use unit costs which then generates a total charge for that service.
that cannot be compared. To help address this challenge After this, the full cost is divided by sum of the charges
and provide clear guidance on unit costing processes, of all services to obtain the ratio of cost to charge.
HITAP assigned this author to develop a list of Finally, this ratio is used to multiply each unit price,
standard unit costs of medical services for Thailand. resulting in unit cost.
The list is intended to increase the efficiency of study The RVU method is based on the ratio of
implementation, improve the reliability of data, and allow resources used for all services in terms of standard
more accurate cross-study comparison. RVUs. Although this method is not as accurate as the
micro-costing method, it offers greater time savings(14,15).
Material and Method First, standard RVUs of all services are developed.
Overall methods Then, the total RVUs used by the hospital are calculated
The present study employed a standard or by multiplying the results of the standard RVU by the
conventional costing method, which is comprised of number of services for all medical services. After that,
five steps(3): cost centre identification, direct cost the cost per RVU is calculated by dividing the full cost
determination, indirect cost allocation, full cost by the total RVUs of the hospital. Finally, the cost per
calculation, and unit cost calculation. To classify cost RVU is multiplied by the number of RVUs for each
centers, it is necessary to know which service outputs service to obtain a unit cost. Standard RVUs can be
and resources are used by those units: transient cost developed using a ranking method or an objective data
centers provide support to patient service units and method(16-18). The ranking method is a subjective
absorbing cost centre provide medical services to technique that compares resource usage by
patients. Direct cost determination is a method used to establishing the smallest amount, and then estimating
calculate those costs that are directly incurred by the subsequent amounts in multiples of this initial amount.
cost centers-labor cost, material cost, and capital cost. The objective data method is based on real resource
Costs incurred by transient cost centers are allocated consumption, based either on the consumption of a
to absorbing cost centers. Many alternative allocation major selected resource (for instance time or material
methods are available, including direct allocation, step- use), or the costing data derived from other studies.
down allocation, double distribution, and simultaneous
equation methods(10), the latter of which is the most Specific methods
complicated but also the most accurate. Full cost is The standard cost list used here in was
calculated by adding together all direct and indirect developed based on the following sub-research
costs. Finally, the full cost is allocated to output services projects conducted by the author, and on theses of
(or cost objects or cost products). graduate students supervised by the author:
There are several unit cost allocation methods. 1. Development of standard relative value
The average method is used for cost centers producing units of health services(19).
only one service or a set of homogeneous services 2. Unit cost analysis of hospital medical
assumed to be the same service. For multi-service cost services(20).
centers, there are a number of alternative methods, 3. Direct non-medical costs for outpatients(21)
including micro-costing(11,12), ratio of costs to charges
(RCC)(12,13), and relative value unit (RVU) or weight Development of standard relative value units of health
procedure method(12,13). services(19)
The micro-costing method is the most accurate The present study was conducted in 2009 to
since it is based on the real resource consumption of develop standard RVUs for Thailand. The objective
S128 J Med Assoc Thai Vol. 97 Suppl. 5 2014
data method was used for the analysis, based on existing medical costs for outpatient services received at health
service cost or price lists. In Thailand, there are three centers, district hospitals, and regional/provincial
main lists-the price list of medical services of hospitals hospitals by way of a descriptive study using a face-
under the Ministry of Public Health(22), which is to-face interview technique. Study sites were selected
developed based on costing concepts; the from the central, northeastern, and northern regions of
reimbursement list for medical services of public health Thailand. In each region, one regional or provincial
facilities under the Civil Servant Medical Benefit Scheme hospital, one district hospital, and two health centers
(CSMBS)(23), a modified version of the Ministry of were selected based on convenience sampling. In
Public Health list using assigned service codes available each study hospital, approximately 100 patients were
in hospital databases and used by all public hospitals; selected for interview. For each health centre,
and the reimbursement list of medical services for road approximately 50 patients were interviewed. All study
traffic injuries under the victims compensation fund, sample patients were at least 18 years old. Patients
based on charges. The authors used the reimbursement who came for general physical examinations,
list to develop our RVUs, as it included all services appointments for injections, and wound dressing were
with codes used in public hospital databases. excluded. The interviews were conducted between
October and December 2009, and focused on gathering
Unit cost analysis of hospital medical services(20) information on the distance traveled between the
To calculate unit costs of hospital medical home and health facility, time spent, costs involved
services, the standard costing approach was used(3). with transportation, meal costs, and income loss in
For unit cost calculation, the RVU method(12,13) was the course of obtaining medical services. The Mahidol
employed, using the aforementioned standard RVUs University institutional review board approved the
of Thailand(19). Costs were presented based on 2009 study. Interviewers explained the process of the study
values. The study covered regional (>500 beds), to respondents and obtained their written informed
provincial (120-500 beds), and district (10-120 beds) consent before conducting the interview.
hospitals. In larger provinces, regional hospitals provide
the same services as provincial hospitals, in addition Results
to offering more advanced treatment. Therefore, The results from this study generated the first
regional and provincial hospitals were classified into set of standard cost lists for Thailand. These have been
the same group for the purposes of this study. Only published, along with the methodology used, in Thai,
those hospitals that met specific efficiency criteria were in hard copy and online (http://www.hitap.net/
included(25). Study sites were composed of three research), and in software form (http://www.hitap.net/
regional/provincial hospitals and two district hospitals. costingmenu/). Five hundred copies of the book were
Total hospital costs were calculated, including labor, distributed to academics and related organizations(28).
material, and capital costs but excluding pharmacy All costs are given in 2009 values, but these can be
costs. Capital costs included cost of using durable adjusted by applying the consumer price index for
assets and opportunity cost of land used. Capital cost medical care(29). For international readers, the exchange
of durable assets was calculated using an economic- rate was 34.34 Thai baht (THB) per $1US in 2009(30).
based approach(10) with a 3% discount rate(9). Useful The standard cost list is composed of,
years were defined according to the guidelines of the - standard RVUs of medical services
Ministry of Finance(26). Items used beyond their useful - unit cost of medical services at regional/
years were still included in the cost (6,27) . After provincial hospitals
determining total hospital costs, total RVUs were - unit cost of medical services of district
calculated by multiplying the RVU of each service by hospitals
the total number of service outputs. Then, the cost per - direct non-medical cost of outpatients at all
RVU was calculated by dividing the hospital’s total levels of health facilities
cost by the total RVUs. Finally, the cost per RVU was Lists of medical services, standard RVUs, and
multiplied by the number of standard RVUs of each unit costs at regional/provincial hospitals and district
service, which results in the unit cost. hospitals are presented in Table 1. In the analysis, no
data of variability (standard error) is included, as the
Direct non-medical costs for out-patients(21) hospitals in the survey did not provide the same set of
The present study estimated the direct non- services. To broaden the information base, data for
J Med Assoc Thai Vol. 97 Suppl. 5 2014 S129
services rendered by all hospitals at the same level wage rate.
were incorporated into one tabulation. The services
were composed of 3,091 items in 12 groups, as follows: Discussion
Group 1: Routine service at outpatient and A number of countries have developed
inpatient departments (visit and hospitalization day). standard cost lists to help standardize their economic
Group 2: Blood transfusion services. evaluations; the most well known are those of
Group 3: Diagnostic and clinical pathology Australia(31), Canada(32,33), the Netherlands(34) and the
services. United Kingdom(35). The first cost list in health care to
Group 4: Diagnostic and therapeutic radiology be produced was the “Manual of Resource Items and
services. Their Associated Costs”(31). First developed in Australia
Group 5: Special investigations. in 1993 by the Common wealth Department of Health
Group 6: Medical supplies and services. and Ageing(33), the list gives a standard list of service
Group 7: Medical procedures and anesthesia. costs that can be used in economic analyses, the results
Group 8: Nursing care services. of which are then submitted to the Pharmaceutical
Group 9: Dentistry services. Benefits Advisory Committee. In Canada, the first cost
Group 10: Physical therapy and medical list was developed in Alberta province in 1997; in 1999,
rehabilitation. a specific cost list for Manitoba health services was
Group 11: Acupuncture and other alternative developed(36). This list was then incorporated into the
medicine. national list of provincial costs for health care in 2000(33).
Group 12: Health promotion and disease In the UK, the first costing guidelines, known as NHS
prevention and control. Costing Manual, was first developed in 1998 by the
Some services in the list were not provided at Department of Health. It is revised every year, published
the time of study; in these cases, the unit costs were in manual form, and provided to all hospitals(37), who
listed as not available (N/A). The unit cost of these then conduct cost analyses based on the values within.
services can be calculated by multiplying the number Participating hospitals calculate the unit costs of the
of RVUs per service (taken from the standard RVU value medical services they provide, and the reference cost
list) by cost per RVU. The cost per RVU for regional/ list is then developed, based on average costs obtained
provincial hospitals and district hospitals was found from data submitted by participating hospitals. In the
to be 134.95 THB and 128.67 THB, respectively (2009 Netherlands, the first “Dutch Manual for Costing:
values). In the case of services beyond the scope of Methods and Reference Prices for Economic
the list, unit costs were estimated by multiplying the Evaluations in Healthcare” was first published in 2000,
unit price by the cost to charge ratio developed by this and a new and revised version was published in 2010,
program, giving ratios of 1.63 and 1.45 for regional/ according to the guidelines on pharmacoeconomic
provincial hospitals and district hospitals, respectively. evaluation issued by the Dutch Health Insurance Board.
To calculate the direct nonmedical cost data The guidelines have been approved by the Ministry of
for outpatients, 905 patients were interviewed. The Health, Welfare, and Sport(34,38,39).
interview asked participants about the various factors By comparing the Thailand list to other
that contribute to the direct medical costs, specifically- international lists in terms of costing methods, it is
distance travelled from home to health facilities, time clear that the present study used similar costing steps
spent travelling and receiving services, costs of travel to those conducted in other countries-resource
and meals, and real income loss of patients and identification, quantity measurement, and valuation of
accompanying persons (Table 2). All values were resources used. The main difference is that, while most
calculated according to one hospital visit. All data were other countries with costing lists have had regularly
disaggregated for health centers, district hospitals, revised standard cost lists for more than a decade, in
regional/provincial hospitals, and the average across Thailand, this is the first version. A clear benefit of this
all facilities was calculated. To calculate real income list is that the results were determined from the
loss, the statistical analysis also included persons who calculations using data from actual health facilities
had incurred no income loss, due to being on a fixed meeting criteria of efficiency and quality. Nevertheless,
monthly salary, being self-employed, or being as with all first versions, there are some limitations.
unemployed. In addition, the opportunity cost could The CSMBS reimbursement rate used for the standard
be calculated based on the time spent versus a reference RVU development was established several years ago,
S130 J Med Assoc Thai Vol. 97 Suppl. 5 2014
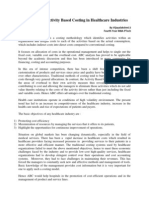
Table 1. Sample of standard RVUs and unit costs of hospital medical services in Thai baht (THB), 2009 values
Service Unit Code RVU Unit cost (THB)
RH/PH DH
Group 2 Blood transfusion services
2.1 Diagnosis
2.1.1 Antibody identification (tube method) Test 22101 2.0 270 n/a
2.1.2 Antibody identification (gel test) Test 22102 4.0 540 n/a
2.1.3 Antibody screening, indirect antiglobulin (tube method) Test 22103 0.5 n/a 64
2.1.4 Antibody screening, indirect antiglobulin (gel test) Test 22104 1.0 135 129
2.1.5 Blood group (ABO) (tube method) Test 22105 1.0 135 129
2.1.6 ABO cell grouping Test 22106 0.5 67 64
2.1.7 ABO serum grouping Test 22107 0.5 67 64
2.1.8 Rh.(D) typing Test 22108 0.4 54 51
2.1.9 Rh. typing (complete) Test 22109 3.5 472 n/a
2.1.10 Direct antiglobulin test Test 22110 0.5 n/a n/a
2.1.11 Direct antiglobulin test (gel test) Test 22111 1.0 135 n/a
2.1.12 Cross matching Test 22114 0.8 108 103
2.1.13 Cross matching (gel test) Test 22115 1.5 202 n/a
RH = regional hospital; PH = provincial hospital; DH = district hospital, THB = Thai baht, n/a = not available
Table 2. Data on direct nonmedical costs for outpatients per visit
Data Mean (SE)
HC DH RH/PH Average
Distance from home to health facilities (km) 3.85 (0.28) 10.86 (0.67) 29.52 (1.82) 14.35 (0.72)
Time spent from home to health facilities (min) 18 (0.72) 40 (3.51) 60 (2.68) 39 (1.59)
Time spent for receiving service, including 69 (3.10) 175 (7.00) 361 (7.91) 201 (5.43)
traveling (from home to home) (min)
Traveling cost* 53.72 (3.53) 72.33 (4.12) 142.55 (11.60) 89.16 (4.39)
Meal cost* 13.36 (1.81) 26.23 (3.17) 52.51 (5.35) 30.76 (2.23)
Patient real income loss* 13.71 (3.67) 49.07 (5.84) 80.29 (13.74) 47.69 (5.20)
Accompanying person real income loss* 5.76 (1.96) 43.52 (5.45) 95.51 (35.41) 48.27 (12.02)
SE = standard error, HC = health center; RH = regional hospital; PH = provincial hospital; DH = district hospital, km =
kilometer, min = minute
* Thai baht, 2009 values
which may mean that some of the methods may be facilities. The authors recommend that an institute be
slightly out of date. This rate was modified from the established to oversee this job as a continuing
Ministry of Public Health price list-a list which was responsibility.
developed by different working groups for different
service groups. Each group might therefore have used Conclusion
different methods in determining specific details. This is the first standard cost menu to be
Another limitation is the small sample size of health developed for Thailand. It covers a range of medical
facilities used for the calculation. Future revisions to services, and covers district hospitals and provincial/
the list should ideally be performed every few years, regional hospitals. At present, the list does not include
and the medical services and corresponding codes services at a super tertiary level or at a university
should be standardized among the various health hospital level. This standard cost menu should make
J Med Assoc Thai Vol. 97 Suppl. 5 2014 S131
economic evaluations more convenient, faster, and 7. Chaikledkaew U, Teerawattananon Y,
more reliable for national policy decision-making. The Kongpittayachai S, Sooksomboon N. Guidelines
next revision should be developed on the back of the for health technology assessment in Thailand.
recommendations suggested herein. Nonthaburi: The Graphico Systems; 2008.
8. Riewpaiboon A. Measurement of costs. J Med
Acknowledgement Assoc Thai 2008; 91 (Suppl 2): S28-37.
The author wish to give particular thanks to 9. Riewpaiboon A. Measurement of costs. In:
the funding support through the Health Intervention Chaikledkaew U, Teerawatananon Y,
and Technology Assessment Program (HITAP) from Kongpittayachai S, Sooksomboon N, editors.
the National Health Security Office, the Thailand Guidelines for health technology assessment in
Research Fund under the Senior Research Scholar on Thailand. Nonthaburi: The Graphico Systems;
Health Technology Assessment (RTA5580010) and Thai 2008: 79-114. (in Thai)
Health Global Link Initiative Program (TGLIP), 10. Drummond MF, Sculpher MJ, Torrance GW,
supported by Thai Health Promotion Foundation. The O’Brien BJ, Stoddart GL. Methods for the economic
author wishes to thank graduate students in Pharmacy evaluation of health care programmes third edition.
Administration at the Faculty of Pharmacy, Mahidol Oxford: Oxford University Press; 2005.
University for participating in the project and Professor 11. Lerner WM, Wellman WL. Pricing hospital units
Peter Coyte, Department of Health Policy, Management of service using microcosting techniques. Hosp
and Evaluation, Faculty of Medicine University of Health Serv Adm 1985; 30: 7-28.
Toronto, Canada for giving suggestions on manuscript 12. Suver JD, Cooper JC. Principles and methods of
preparation. managerial cost-accounting systems. Am J Hosp
Pharm 1988; 45: 146-52.
Potential conflicts of interest 13. Cooper JC, Suver JD. Product line cost estimation:
None. a standard cost approach. Healthc Financ Manage
1988; 42: 60, 62, 64.
References 14. Dowless RM. What’s the procedure? Your guide
1. Rizzo JD, Powe NR. Methodological hurdles in to costing methods and terminology. Nurs Manage
conducting pharmacoeconomic analyses. 2007; 38: 52-7.
Pharmacoeconomics 1999; 15: 339-55. 15. Dowless RM. Procedure costing flexibility. Healthc
2. Cairns J. Discounting in economic evaluation. In: Financ Manage 2007; 61: 103-4.
Drummond M, McGuire A, editors. Economic 16. Cost Accounting Workshop. The preparation and
evaluation in health care; merging theory with development of cost accounting information
practice. Oxford: Oxford University Press; 2001: [Internet]. n.d. [cited 2012 Aug 12]. Available from:
236-55. http://www.health.gov.ua/zpr/101-200/0145/
3. Riewpaiboon A, Malaroje S, Kongsawatt S. Effect English/caprep.doc
of costing methods on unit cost of hospital medical 17. Christie GHW. A guide to cost analysis: developing
services. Trop Med Int Health 2007; 12: 554-63. cost based fees. Syracuse: Health Policy Analysts;
4. Brouwer W, Rutten F, Koopmanschap M. Costing 2008.
in economic evaluations. In: Drummond M, 18. Hankins RW, Baker JJ. Management accounting
McGuire A, editors. Economic evaluation in health for health care organizations. Sudbury: Jones and
care-merging theory with practice. New York: Bartlett Publishers; 2004.
Oxford University Press; 2001: 68-93. 19. Koopitakkajorn T, Riewpaiboon A, Chaikledkaew
5. Luce BR, Manning WG, Siegel JE, Lipscomb J. U. Development of relative value units of health
Estimating costs in cost-effectiveness analysis. services in Thailand. Bangkok: Faculty of
In: Gold MR, Sigel JE, Russell LB, Weinstein MC, Pharmacy, Mahidol University; 2010.
editors. Cost-effectiveness in health and medicine. 20. Kamluang S, Riewpaiboon A, Chaikledkaew U. Unit
Oxford: Oxford University Press; 1996: 176-213. cost analysis of medical services employing
6. Mogyorosy Z, Smith P. The main methodologyical relative value unit method. In: Proceedings of the
issues in costing health care services; a literature 4th Ubon Ratchathani University Research
review. York: Centre for Health Economics, The Conference; 9-10 August 2010. Ubon Ratchathani,
University of York; 2005. Thailand: Ubon Ratchathani University; 2010: 234-
S132 J Med Assoc Thai Vol. 97 Suppl. 5 2014
42. wealth, Department of Health and Ageing Australia.
21. Riewpaiboon A. Direct nonmedical cost of Manual of resources items and their associated
outpatients in Thailand. Bangkok: Faculty of costs [Internet]. 2009 [cited 2012 Aug 18]. Available
Pharmacy, Mahidol University; 2009. from: http://www.health.gov.au/internet/main/
22. Department of Health Service Support. Price list of publishing.nsf/content/health-pbs-general-pubs-
medical services. Nonthaburi: Ministry of Public manual-content.htm/$FILE/manual.pdf
Health; 2004. (in Thai) 32. Jacobs P, Roos NP. Standard cost lists for
23. The Comptroller General’s Department. healthcare in Canada. Issues in validity and inter-
Reimbursement rate for medical services of public provincial consolidation. Pharmacoeconomics
health facilities. Bangkok: Ministry of Finance; 1999; 15: 551-60.
2006. (in Thai) 33. Institute of Health Economics. A national list of
24. Department of Insurance. Reimbursement list of provincial costs for health care: Canada 1997/8
medical services for road traffic injuries under the [Internet]. 2004 [cited 2012 Aug 15]. Available from:
victims compensation fund. Bangkok: Ministry of http://www.cadth.ca/media/pdf/Costlist_e.pdf
Finance; 2004. (in Thai) 34. Tan SS, Bouwmans CA, Rutten FF, Hakkaart-van
25. Pattamasiriwat D. Efficiency of hospital cost Roijen L. Update of the Dutch Manual for Costing
management: a case of hospitals under the Ministry in Economic Evaluations. Int J Technol Assess
of Public Health. In: National conference of Health Care 2012; 28: 152-8.
economists on self-sufficiency economy. Bangkok: 35. Department of Health. 2011-12 reference costs
University of Agriculture; 2007. (in Thai) publication [Internet]. 2011 [cited 2012 Aug 15].
26. Ministry of Finance. Revaluation of assets Available from: http://www.dh.gov.uk/en/
[Internet]. 2003 [cited 2012 Aug 12]. Available from: Publications and statistics/Publications/
http://www.moe.go.th/webfnd/mo29.htm Publications Policy and Guidance/DH_131140
27. Edejer TT-T, Baltussen R, Adam T, Hutubessy R, 36. Jacobs P, Shanahan M, Roos NP, Farnworth M.
Acharya A, Evans DB, et al. Making choices in Cost list for Manitoba health services [Internet].
health: WHO guide to cost-effectiveness analysis. 1999 [cited 2012 Aug 15]. Available from: http://
Geneva: World Health Organization; 2003. mchp-appserv.cpe.umanitoba.ca/reference/
28. Riewpaiboon A. Standard cost lists for health costlist.pdf
technology assessment. Nonthaburi: Health 37. Department of Health. NHS costing manual 2009/
Intervention and Technology Assessment 10 [Internet]. 2010 [cited 2012 Aug 15]. Available
Program (HITAP), Ministry of Public Health; 2011. from: http://www.dh.gov.uk/prod_consum_dh/
(in Thai) groups/dh_digitalassets/@dh/@en/@ps/
29. Bureau of Trade and Economic Indices, Ministry documents/digitalasset/dh_113295.pdf
of Commerce. Report for consumer price index of 38. Oostenbrink JB, Koopmanschap MA, Rutten FF.
Thailand [Internet]. 2013 [cited 2013 Feb 19]. Dutch manual for costing-research: methods and
Available from: http://www.price.moc.go.th/price/ guideline-prices. In: Annual Meeting of
cpi/index_new_all.asp International Society of Technology Assessment
30. Bank of Thailand. Rates of exchange of commercial Health Care Int Soc Technol Assess Health Care
banks in Bangkok metropolis [Internet]. 2011 [cited Meet; 2000: 162.
2011 Dec 4]. Available from: http://www2.bot.or.th/ 39. Oostenbrink JB, Koopmanschap MA, Rutten FF.
statistics/ReportPage.aspx?reportID=123 Standardisation of costs: the Dutch Manual for
&language=eng Costing in economic evaluations. Pharmaco-
31. Pharmaceutical Evaluation Section Common- economics 2002; 20: 443-54.
J Med Assoc Thai Vol. 97 Suppl. 5 2014 S133
⌫⌫
⌫
⌫ ⌦
⌦ ⌫
⌫⌫⌦
⌫⌫ ⌦
S134 J Med Assoc Thai Vol. 97 Suppl. 5 2014
View publication stats
You might also like
- Informatics Application in Evidence Based Nursing PracticeDocument25 pagesInformatics Application in Evidence Based Nursing PracticeVhince Pisco55% (31)
- The Entrepreneurial MindDocument70 pagesThe Entrepreneurial MindJavan Domanico100% (2)
- TR2390 Electrical, Optical ConnectorsDocument57 pagesTR2390 Electrical, Optical ConnectorsCandice Williams100% (1)
- Fanuc BasicDocument0 pagesFanuc BasicMarco A. Miranda RamírezNo ratings yet
- 2.5 Quiz-ContinuityDocument4 pages2.5 Quiz-Continuitybilal5202050No ratings yet
- Measurement of Costs For Health Economic EvaluationDocument10 pagesMeasurement of Costs For Health Economic EvaluationEry SetiawanNo ratings yet
- Development of Cost Analysis Guidance For Indonesian HospitalsDocument8 pagesDevelopment of Cost Analysis Guidance For Indonesian Hospitalssyaiful rinantoNo ratings yet
- Jurnal InternasionalDocument20 pagesJurnal Internasionalitho23No ratings yet
- PE Article Review FinalDocument7 pagesPE Article Review FinalSaron AlemayehuNo ratings yet
- Effect of Costing Methods On Unit Cost of Hospital Medical ServicesDocument10 pagesEffect of Costing Methods On Unit Cost of Hospital Medical Servicesbarkiest24No ratings yet
- Application of The Activity-Based Costing Method For Unit-Cost Calculation in A HospitalDocument11 pagesApplication of The Activity-Based Costing Method For Unit-Cost Calculation in A Hospitalkivoka titritNo ratings yet
- Economic Evaluation Strategies in Telehealth: Obtaining A More Holistic Valuation of Telehealth InterventionsDocument5 pagesEconomic Evaluation Strategies in Telehealth: Obtaining A More Holistic Valuation of Telehealth InterventionsAlejandro CardonaNo ratings yet
- Rev4 - Epp - Unit Cost RS - RD Rosyadi - 05 12 2021Document7 pagesRev4 - Epp - Unit Cost RS - RD Rosyadi - 05 12 2021rosyd rosyadiNo ratings yet
- Economic Evaluation of Pharmacy ServicesDocument23 pagesEconomic Evaluation of Pharmacy ServicesMaryam JavaidNo ratings yet
- Activity Based Costing in Health Care Center PDFDocument6 pagesActivity Based Costing in Health Care Center PDFFreddy VargasNo ratings yet
- What Is Pharmacoeconomics?Document4 pagesWhat Is Pharmacoeconomics?pinto princeNo ratings yet
- Published Researches in The Year 2010Document16 pagesPublished Researches in The Year 2010hsrimediaNo ratings yet
- Aghajani 2019Document8 pagesAghajani 2019The Sunday StoryNo ratings yet
- Computer Generated in Nursing Care PlansDocument4 pagesComputer Generated in Nursing Care PlansCake Man100% (1)
- BUS 644 Week 2 Assignment-A.randolphDocument5 pagesBUS 644 Week 2 Assignment-A.randolphAntdrone RandolphNo ratings yet
- Fasilita RefDocument10 pagesFasilita RefsukrangNo ratings yet
- Cost Analysis: Fixed CostDocument8 pagesCost Analysis: Fixed CostjayasankariNo ratings yet
- Project ReportDocument41 pagesProject ReportAnoop PunathilNo ratings yet
- PJ ONLINE Pharmacoeconomics 2Document3 pagesPJ ONLINE Pharmacoeconomics 2Anshari StressNo ratings yet
- BUS6004 Quality Management in A Care Setting - EditedDocument13 pagesBUS6004 Quality Management in A Care Setting - EditedMashaal FNo ratings yet
- Value Based Healthcare Initiatives in Practice A.5Document26 pagesValue Based Healthcare Initiatives in Practice A.5Mario Luna BracamontesNo ratings yet
- 06 How Much Does Management of An Asthma-Related Event Cost in A Malaysian Suburban HospitalDocument6 pages06 How Much Does Management of An Asthma-Related Event Cost in A Malaysian Suburban HospitalHardin DiazNo ratings yet
- Analisis de CostosDocument60 pagesAnalisis de CostosWilson Ramirez ZuniniNo ratings yet
- Abstrak 6Document4 pagesAbstrak 6Gesti RachmaniNo ratings yet
- Ko, Lee and Lim, 2007) : 1. Structure AssessmentDocument3 pagesKo, Lee and Lim, 2007) : 1. Structure AssessmentRazaNo ratings yet
- Cost Analysis HospitalsDocument85 pagesCost Analysis HospitalsGeta_Varvaroi_6157100% (1)
- Applying Activity Based Costing (ABC) Method To Calculate Cost Price in Hospital and Remedy ServicesDocument8 pagesApplying Activity Based Costing (ABC) Method To Calculate Cost Price in Hospital and Remedy ServicesTri YuliasihNo ratings yet
- 8E Meitria Nur Sabrina EnglishDocument18 pages8E Meitria Nur Sabrina Englishmeitria nur sabrinaNo ratings yet
- Pharmacoeconomics As Applied To Hospital Pharmacy HandoutDocument20 pagesPharmacoeconomics As Applied To Hospital Pharmacy HandoutLeylu RepatoNo ratings yet
- EBMgt 1Document8 pagesEBMgt 1Delelegn EmwodewNo ratings yet
- NCP FAQsDocument16 pagesNCP FAQsEl Avion NoelNo ratings yet
- 2008 2231 20 88Document7 pages2008 2231 20 88maulikpatel2709No ratings yet
- Hello Good MorningDocument5 pagesHello Good MorningAllan SaquinNo ratings yet
- Process Mining For Clinical Processes A Comparative AnalysisDocument18 pagesProcess Mining For Clinical Processes A Comparative AnalysisbenNo ratings yet
- Economic EvaluationDocument4 pagesEconomic Evaluationkajojo joyNo ratings yet
- Ispor Alonside TrialsDocument12 pagesIspor Alonside TrialsJulivaiNo ratings yet
- Cost-Effectiveness Analysis Alongside Clinical Trials II-An ISPOR Good Research Practices Task Force ReportDocument30 pagesCost-Effectiveness Analysis Alongside Clinical Trials II-An ISPOR Good Research Practices Task Force Reportelisabeth jawanNo ratings yet
- How To Determine Cost Effective Analysis - RatikaDocument14 pagesHow To Determine Cost Effective Analysis - Ratikatifanny carolinaNo ratings yet
- NI Final ExamDocument7 pagesNI Final ExamJoseph Burra LagodNo ratings yet
- Informatics Application in Evidence (Report Content)Document4 pagesInformatics Application in Evidence (Report Content)krystelle jade labineNo ratings yet
- Effects of Results-Based Financing Intervention On Technical Efficiency of Health Services in AfghanistanDocument10 pagesEffects of Results-Based Financing Intervention On Technical Efficiency of Health Services in AfghanistanNational Graduate ConferenceNo ratings yet
- EDBADocument11 pagesEDBABilal SalamehNo ratings yet
- Application of ABC in Healthcare IndustriesDocument3 pagesApplication of ABC in Healthcare IndustriesVijayalakshmi SridharNo ratings yet
- Term Paper ON The Management Information System Model For Process-Oriented Health CareDocument5 pagesTerm Paper ON The Management Information System Model For Process-Oriented Health CareAyush SharmaNo ratings yet
- Public Health BNNNDocument8 pagesPublic Health BNNNOmpal SinghNo ratings yet
- 2016 - LeeDocument7 pages2016 - LeeazeemathmariyamNo ratings yet
- Module 6-Key Attributes of Cost AnalysesDocument3 pagesModule 6-Key Attributes of Cost AnalysesLou CalderonNo ratings yet
- Health Care Provider Adoption of EHealthDocument22 pagesHealth Care Provider Adoption of EHealthvoNo ratings yet
- Health RecordsDocument36 pagesHealth RecordsMatthew NdetoNo ratings yet
- 294 1044 1 PBDocument8 pages294 1044 1 PBrindha dwi sihantoNo ratings yet
- The Positive Impact of Continuous ImprovementDocument15 pagesThe Positive Impact of Continuous ImprovementMane DaralNo ratings yet
- Conjoint in HEALTH ResearchDocument17 pagesConjoint in HEALTH ResearchDiana Tan May KimNo ratings yet
- Eview F Herapeutics: Economic Evaluations of Clinical Pharmacy Services: 2006 - 2010Document23 pagesEview F Herapeutics: Economic Evaluations of Clinical Pharmacy Services: 2006 - 2010Igor SilvaNo ratings yet
- Choices in Methods For Economic EvaluationDocument55 pagesChoices in Methods For Economic EvaluationHanan AhmedNo ratings yet
- Outcome Assessment in Routine Clinical Practice inDocument21 pagesOutcome Assessment in Routine Clinical Practice inicuellarfloresNo ratings yet
- Test Bank For Evidence Based Practice For Nursing and Healthcare Quality Improvement 1st Edition by Lobiondo WoodDocument8 pagesTest Bank For Evidence Based Practice For Nursing and Healthcare Quality Improvement 1st Edition by Lobiondo WoodSusan Palacios100% (40)
- MX and Medico Legal AssignDocument14 pagesMX and Medico Legal AssignyeapgyNo ratings yet
- Development of Pharmacy Service Weights in the Implementation of Casemix System for Provider Payment: Concept, Methods and ApplicationsFrom EverandDevelopment of Pharmacy Service Weights in the Implementation of Casemix System for Provider Payment: Concept, Methods and ApplicationsNo ratings yet
- Introduction to Clinical Effectiveness and Audit in HealthcareFrom EverandIntroduction to Clinical Effectiveness and Audit in HealthcareNo ratings yet
- Measurement of Costs For Health Economic EvaluationDocument10 pagesMeasurement of Costs For Health Economic EvaluationEry SetiawanNo ratings yet
- International Journal of Surgery: GuidelineDocument9 pagesInternational Journal of Surgery: GuidelineEry SetiawanNo ratings yet
- ILO Informal EconomyDocument133 pagesILO Informal EconomyEry SetiawanNo ratings yet
- Social Change and Human DevelopmentDocument43 pagesSocial Change and Human DevelopmentEry SetiawanNo ratings yet
- Bakhai, 2006Document9 pagesBakhai, 2006Ery SetiawanNo ratings yet
- Public Health Advocacy Toolkit 07Document36 pagesPublic Health Advocacy Toolkit 07Ery SetiawanNo ratings yet
- Points-Based CalculatorDocument1 pagePoints-Based CalculatorEry SetiawanNo ratings yet
- Unit III Sliding Contact BearingDocument26 pagesUnit III Sliding Contact BearingSHUBHAM GOVILNo ratings yet
- GDC Tech Bulletin Hard Drive Diagnostics v2Document5 pagesGDC Tech Bulletin Hard Drive Diagnostics v2guerreroNo ratings yet
- Tax 2 PrelimDocument10 pagesTax 2 PrelimreymardicoNo ratings yet
- Order Management Developer GuideDocument356 pagesOrder Management Developer GuidePrakash KolheNo ratings yet
- Modern Gurukul PDFDocument17 pagesModern Gurukul PDFthanuja7chandrasekerNo ratings yet
- Colder Catalog 27-30 PMC ConnectorsDocument4 pagesColder Catalog 27-30 PMC ConnectorsDENNIZNo ratings yet
- Action Research On Late ComingDocument13 pagesAction Research On Late ComingMeklit Abinet100% (9)
- Destination Management Organizations: Dr. Harsh Varma UNWTO ExpertDocument32 pagesDestination Management Organizations: Dr. Harsh Varma UNWTO ExpertBernard MalhommeNo ratings yet
- Test 1Document14 pagesTest 1Phương LinhNo ratings yet
- Somalia PI 49 Required Date 14 04 2023Document3 pagesSomalia PI 49 Required Date 14 04 2023Saifu M AsathNo ratings yet
- BRMDocument6 pagesBRMGagan Kumar RaoNo ratings yet
- Brain ChildDocument8 pagesBrain ChildGabriel PiticasNo ratings yet
- Scott Cooley Lyric and Chord Songbook Volume OneDocument272 pagesScott Cooley Lyric and Chord Songbook Volume OneScott CooleyNo ratings yet
- Commonwealth High School: Consumer Preference Between Chicken Adobo and Bistek Tagalog Maki in Commonwealth High SchoolDocument10 pagesCommonwealth High School: Consumer Preference Between Chicken Adobo and Bistek Tagalog Maki in Commonwealth High SchoolBianca Marie Uypala ErquilangNo ratings yet
- Commscope CV3PX308R1Document5 pagesCommscope CV3PX308R1klamar5No ratings yet
- Wealth-Insight - May 2021Document66 pagesWealth-Insight - May 2021vnmasterNo ratings yet
- Hairpin Heat ExchangerDocument9 pagesHairpin Heat ExchangerBrandon HaleNo ratings yet
- BA Outline ChecklistDocument44 pagesBA Outline ChecklisttomNo ratings yet
- MIT1 264JF13 Lect 10Document21 pagesMIT1 264JF13 Lect 10Habtamu Hailemariam AsfawNo ratings yet
- EBCS EN 1991 1.7 2014 - Final - Accidental ActionsDocument64 pagesEBCS EN 1991 1.7 2014 - Final - Accidental ActionsGirum Menassie100% (1)
- Contact UsDocument258 pagesContact UsSuplemento Deportivo100% (1)
- TheSun 2009-09-04 Page02 Tee Keat Quizzed by Macc On PKFZDocument1 pageTheSun 2009-09-04 Page02 Tee Keat Quizzed by Macc On PKFZImpulsive collectorNo ratings yet
- Livne-Ofer Et Al. - (2019 - AMJ) - Perceived Exploitative and Its ConsequecesDocument30 pagesLivne-Ofer Et Al. - (2019 - AMJ) - Perceived Exploitative and Its Consequeces李佩真No ratings yet
- Tuck ShopDocument21 pagesTuck ShopfaizlpuNo ratings yet
- Actuat 97Document36 pagesActuat 97Nithish Kumar K MNo ratings yet
- PL17 Accelerate MySQL Apache Ignite 4656Document35 pagesPL17 Accelerate MySQL Apache Ignite 4656Kishor pNo ratings yet