Professional Documents
Culture Documents
WB COVID19 Latest Treatment Protocol
WB COVID19 Latest Treatment Protocol
Uploaded by
Rahul AwasthiOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
WB COVID19 Latest Treatment Protocol
WB COVID19 Latest Treatment Protocol
Uploaded by
Rahul AwasthiCopyright:
Available Formats
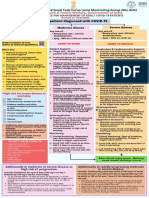
Published by Department of Health & Family Welfare, Govt of West Bengal
LABORATORY CONFIRMED COVID 19 PATIENT
1. All asymptomatic patients. Symptomatic patientswith the following co- Symptomatic patients (irrespective of comorbid
2. Comorbid patients with no morbidities conditions) with any of the following signs:
symptoms (prioritise to control the Age > 60 yrs Fever > 100.4 F
comorbid state) DM Respiratory rate > 22/ min
3. Mild symptoms (low fever, dry HTN /IHD Systolic BP <= 100 mmHg
cough, anosmia, ageusia, COPD/Chronic lung disease SpO2 <95%
weakness, diarrhea, myalgia etc) Immuno-compromised state Respiratory distress
with Immunosuppressive drugs Chest pain
No comorbidity CKD Change in mental status
Low fever (<100.4 F) Chronic Liver Disease Cyanosis
No signs of respiratory distress Obesity
Normal SpO2
Normal mental status, systolic
BP > 100 mmHg and
No oxygen requirement or Oxygen requirement >10 L/min
Respiratory rate < 22/min
Oxygen requirement <10 L/min
HOME ISOLATION/ SAFE HOME COVID WARD HDU/ ICU
MONITOR: Temp, Pulse, BP, SpO2, Pneumonia (LRTI) Pneumonia (LRTI) WITH RESPIRATORY SUPPORT
WITHOUT respiratory failure (RR> 24
Sensorium HFNC if work of breathing is HIGH
respiratory failure /min,
Preferable Investigations: CBC, (Fever/ cough/ SpO2 < 95% on room air, A cautious trial of NIV /CPAP with full face
CRP, D-Dimer dyspnea & SpO2 PaO2 < 60 mmHg) mask/ oronasal mask
ECG, CBG, Serum Creatinine: as ≥95% on room air, Consider Intubation if work of breathing is
PaO2 > 60 mmHg &
required RED FLAG SIGNS high/ NIV is not tolerated
RR< 24/min)
1. SBP<100
Lung protective ventilation strategy by
Supportive Management 2. Altered sensorium
ARDS net protocol
Mask, Hand Hygiene, Physical RED FLAG SIGNS 3. Raised Troponin-I /
distancing, droplet precaution 1. NLR > 3.13 CPK-MB Prone ventilation in refractory Hypoxemia
PARACETAMOL (if fever/bodyache) 2. CRP > 5 times of 4. P:F ratio <200
Vit C ● Laxative (if required) ULN 5. Sepsis/ Septic Shock STEROID
7. Multi Organ
Inhalational BUDESONIDE 800 3. D-Dimer > 2 times Dexamethasone 0.2 to 0.4 mg/kg for at
of ULN Dysfunction Syndrome
mcg twice daily for 5 days if fever least 5-10 days
8. Rapidly increasing
persists for more than 5 days
Oxygen Demand
and/ or distressing cough. ANTICOAGULATION
Systemic Steroids should NOT be Prophylactic dose of UFH or LMWH (e.g.
ANTIPYRETICS: Paracetamol for fever
used routinely in mild cases. Enoxaparin 0.5 mg/kg BD SC), if not at high
OXYGEN SUPPORT
Target SpO2 ≥ 95% (≥90% in pts. with COPD) risk of bleeding (consider UFH if CrCl<30)
Following therapy should be used in
high risk patients: appropriate Oxygen delivery device (cannula / Face
ANTIVIRAL
mask/ non-re-breathing face mask)
Monoclonal antibody therapy Antiviral agents are less likely to be
Conscious proning may be used in whom hypoxia
(Cocktail of Casirivimab and beneficial at this stage; use of Remdesivir
persist despite use of high flow oxygen. (position
Imdevimab): 600 mg each single to be decided on case to case basis, Not to
change at every 1-2 hours)
dose (NOT MUCH EFFECTIVE AGAINST th
start after 10 days of symptom onset
OMICRON)
STEROID
Molnupiravir: 800 mg (four 200- Dexamethasone 0.1 to 0.2 mg/kg for at least 5-10 /Test date
mg capsules) orally every 12 days
TOCILIZUMAB may be considered on a case
hours for 5 days (TO BE USED ANTICOAGULATION
WITHIN 5 DAYS) Prophylactic dose of UFH or LMWH (Enoxaparin to case basis after shared decision making
40mg/ day SC)
Warning Signs MONOCLONAL ANTIBODY THERAPY (Cocktail of
ANTIBIOTICS should be used judiciously as
Difficulty in breathing Casirivimab and Imdevimab): 600 mg each per Antibiotic protocol
Persistent Fever/ High grade fever/
ANTIVIRAL INVESTIGATIONS
Recurrence of Fever
Palpitations REMDESIVIR: to be decided on case to case basis. Not to Essential investigations along with Cultures
Chest pain/ Chest tightness start after 10th days of symptom onset /Test date
(Blood / Urine), FBS, PPBS, CBC, CRP,
Severe Cough MOLNUPIRAVIR: 800 mg (four 200-mg capsules)
Ferritin, D-Dimer, Trop-T/ Quantitative
Any new onset symptoms orally every 12 hours for 5 days (NOT TO BE USED IN
PATIENTS WITH O2 THERAPY) Troponins, Procalcitonin, Coagulation
SpO2 <95% ( Room Air) Profile, HRCT Thorax.
ANTIBIOTICS
CRP > 5 times of ULN
(Antibiotics should be used judiciously as per Antibiotic
D-Dimer > 2 times of ULN SUPPORTIVE MEASURES
NLR > 3.13
protocol)
MONITORING • Maintain euvolemia
Or, as advised by physician
specially in High-Risk Group CBC, CRP, D-Dimer: 48-72 hourly • Sepsis/septic shock: manage as per
LFT, KFT: 48-72 hourly protocol and antibiotic policy
Trop T, ECG, Coagulation Profile • Sedation and Nutrition therapy along with
HRCT Chest/ CXR - PA as per existing guidelines (FAST HUG)
Admit the patient at Covid Ward/ Change in oxygen requirement, Work of breathing,
HDU/ ICU Hemodynamic instability
You might also like
- Rhetorical Analysis EssayDocument5 pagesRhetorical Analysis Essayapi-320095543No ratings yet
- Anemia Concept Mapping. Group 1Document82 pagesAnemia Concept Mapping. Group 1Giselle EstoquiaNo ratings yet
- Adult Patient Diagnosed With COVID-19: Ministry of Health & Family Welfare, Government of IndiaDocument1 pageAdult Patient Diagnosed With COVID-19: Ministry of Health & Family Welfare, Government of Indiapramodbankhele3845No ratings yet
- COVID Clinical Management 14012022Document1 pageCOVID Clinical Management 14012022Naina DesaiNo ratings yet
- COVID Management 17th January 2022 DR Suvrankar Datta AIIMSDocument1 pageCOVID Management 17th January 2022 DR Suvrankar Datta AIIMSWhiteNo ratings yet
- Treatment Protocol Covid-19Document4 pagesTreatment Protocol Covid-19Shiv singhNo ratings yet
- Family Medicine Case FilesDocument44 pagesFamily Medicine Case FilesTazan VoNo ratings yet
- COVID - Management 14 April 2021Document20 pagesCOVID - Management 14 April 2021Zain ZaidiNo ratings yet
- KEM Protocols - Hypertensive Emergency (Dr. Pritha)Document3 pagesKEM Protocols - Hypertensive Emergency (Dr. Pritha)Sonu AntonyNo ratings yet
- Resource ViewDocument54 pagesResource ViewHamza AdeelNo ratings yet
- Asma 1Document8 pagesAsma 1punkgatitNo ratings yet
- COVID MX BsmmuDocument2 pagesCOVID MX BsmmuNuhiat NahreenNo ratings yet
- CopdDocument16 pagesCopdHot MathNo ratings yet
- Laboratory Confirmed Covid 19 Patient: Department of Health & Family Welfare, Govt of West BengalDocument2 pagesLaboratory Confirmed Covid 19 Patient: Department of Health & Family Welfare, Govt of West BengalSujoyDeNo ratings yet
- COVID19 Management Algorithm 22042021 v1Document1 pageCOVID19 Management Algorithm 22042021 v1shivani shindeNo ratings yet
- PcolDocument17 pagesPcolThea JulianaNo ratings yet
- Treatment Protocol Covid EnglishDocument3 pagesTreatment Protocol Covid EnglishIchigo SnijdersNo ratings yet
- Icu Guidelines - 024219Document6 pagesIcu Guidelines - 024219M Hammad AshrafNo ratings yet
- AIIMS/ ICMR-COVID-19 National Task Force/ Joint Monitoring Group (Dte - GHS) Ministry of Health & Family Welfare, Government of IndiaDocument1 pageAIIMS/ ICMR-COVID-19 National Task Force/ Joint Monitoring Group (Dte - GHS) Ministry of Health & Family Welfare, Government of IndiaSomnath Das GuptaNo ratings yet
- Case 1: Health Maintenance in GeneralDocument44 pagesCase 1: Health Maintenance in GeneralJoshuaNo ratings yet
- COVID-19 Disease SeverityDocument7 pagesCOVID-19 Disease SeverityParishan SaeedNo ratings yet
- Management of Acute Severe Asthma in PediatricsDocument53 pagesManagement of Acute Severe Asthma in PediatricsAmit AnandNo ratings yet
- Allergy and Immunology 2023 FINALDocument18 pagesAllergy and Immunology 2023 FINALBelinda ELISHANo ratings yet
- COVID-19 Management of Critical Care Cases PDFDocument6 pagesCOVID-19 Management of Critical Care Cases PDFLubna AliNo ratings yet
- Management Algorithm For Community COVID-19 CentersDocument1 pageManagement Algorithm For Community COVID-19 CentersSi Thu LwinNo ratings yet
- FINAL COVID19 1 April 2021Document14 pagesFINAL COVID19 1 April 2021Wleed KhledNo ratings yet
- Paediatricshouseofficerguidehospitalkulim 151026150042 Lva1 App6891Document14 pagesPaediatricshouseofficerguidehospitalkulim 151026150042 Lva1 App6891Nadia SalwaniNo ratings yet
- Severe Sepsis&Septic Shock in Pediatrics.: Abdel Razzaq Abu Mayaleh, MDDocument27 pagesSevere Sepsis&Septic Shock in Pediatrics.: Abdel Razzaq Abu Mayaleh, MDlotskiNo ratings yet
- AIIMS Issues New Guidelines For Treatment of Covid-19 Cases: (Enter Post Title Here)Document7 pagesAIIMS Issues New Guidelines For Treatment of Covid-19 Cases: (Enter Post Title Here)senthil kumarNo ratings yet
- Bronchial Asthma (1) SKDocument24 pagesBronchial Asthma (1) SKSafoora RafeeqNo ratings yet
- Covid-19 Protocol Severity and ManagementDocument4 pagesCovid-19 Protocol Severity and ManagementMardy DeponaNo ratings yet
- WB Covid Protocol Book 25.09 .20 (1)Document49 pagesWB Covid Protocol Book 25.09 .20 (1)El MirageNo ratings yet
- Acute Asthma - Care in The Emergency DepartmentDocument5 pagesAcute Asthma - Care in The Emergency DepartmentTanitNo ratings yet
- ANAESTHESIA For Copd AsthmaDocument20 pagesANAESTHESIA For Copd AsthmashikhaNo ratings yet
- Bronchial Asthma!: A C E S G V CDocument10 pagesBronchial Asthma!: A C E S G V CAmalNo ratings yet
- Respiratory EmergenciesDocument34 pagesRespiratory EmergenciesRoshana MallawaarachchiNo ratings yet
- AIIMS Issues New Guidelines For Treatment of CovidDocument7 pagesAIIMS Issues New Guidelines For Treatment of Covidsenthil kumarNo ratings yet
- BCCA AB in Febrile Neutropenia GuidelinesDocument2 pagesBCCA AB in Febrile Neutropenia GuidelinesAlvy SyukrieNo ratings yet
- MIS C Algorithim Version 2Document8 pagesMIS C Algorithim Version 2Saima UmairNo ratings yet
- Ace FinalDocument11 pagesAce FinalJude Andrian CasugayNo ratings yet
- Drugs For Treatment of Bronchial Asthma: DR Sanjay Junior Resident Department of Pharmacology Ims-BhuDocument19 pagesDrugs For Treatment of Bronchial Asthma: DR Sanjay Junior Resident Department of Pharmacology Ims-BhuBisweswar OjhaNo ratings yet
- AIIMS COVID Algorithm 1.5-1 PDFDocument1 pageAIIMS COVID Algorithm 1.5-1 PDFAnutosh BhaskarNo ratings yet
- Comprehensive Life Support Tutorial Case 1: Question/Action Information Note/Reference TipsDocument3 pagesComprehensive Life Support Tutorial Case 1: Question/Action Information Note/Reference Tipshyukkie minnieNo ratings yet
- CPAMSDocument7 pagesCPAMSDominic chuaNo ratings yet
- Lecture 6Document5 pagesLecture 6Grafu Andreea AlexandraNo ratings yet
- AIIMS COVID Doc 1.6.1-1Document1 pageAIIMS COVID Doc 1.6.1-1mbhangaleNo ratings yet
- REVISED COVID-19 TREATMENT PROTOCOL - Version 3Document17 pagesREVISED COVID-19 TREATMENT PROTOCOL - Version 3abhishekNo ratings yet
- Status Asthmaticus: Triwahju AstutiDocument41 pagesStatus Asthmaticus: Triwahju AstutirianiNo ratings yet
- Common Pediatric Emergencies - A2Document46 pagesCommon Pediatric Emergencies - A2Ahmad JustNo ratings yet
- Asthma 1Document79 pagesAsthma 1DanishMandiNo ratings yet
- Referat Sepsis Dan ARDS - Lea SichiliaDocument24 pagesReferat Sepsis Dan ARDS - Lea SichiliaLea SichiliaNo ratings yet
- JLN Nafas 2 PDFDocument27 pagesJLN Nafas 2 PDFDiga AnaNo ratings yet
- Acute Severe Asthma Critical Care Management: Lokesh Tiwari Aiims PatnaDocument53 pagesAcute Severe Asthma Critical Care Management: Lokesh Tiwari Aiims PatnaYohana SepthiyaNo ratings yet
- Asthma Harrisons ClubDocument84 pagesAsthma Harrisons ClubLady AngodNo ratings yet
- Etiology & Triggers: AsthmaDocument6 pagesEtiology & Triggers: AsthmaNichole CollinsNo ratings yet
- Bronchial Asthma: Mariam Lwasa Naluwugge Afrah 215-083011-07387Document25 pagesBronchial Asthma: Mariam Lwasa Naluwugge Afrah 215-083011-07387NinaNo ratings yet
- High-Flow Nasal Cannula-Protocol For Initiation, Titration and WeaningDocument3 pagesHigh-Flow Nasal Cannula-Protocol For Initiation, Titration and WeaningMahmoud khedrNo ratings yet
- Critical Care Medications: Vasopressors, Inotropes and Anti-Hypertensives Study Guide: Critical Care EssentialsFrom EverandCritical Care Medications: Vasopressors, Inotropes and Anti-Hypertensives Study Guide: Critical Care EssentialsNo ratings yet
- Fast Facts: Respiratory Allergies: Understand aeroallergens, improve treatment responseFrom EverandFast Facts: Respiratory Allergies: Understand aeroallergens, improve treatment responseNo ratings yet
- Nursing Care PlanDocument12 pagesNursing Care Plantzichi80% (5)
- A Study On The Relationship Between Sport and AggressionDocument16 pagesA Study On The Relationship Between Sport and AggressionNur SyuhadahNo ratings yet
- ENS Guide To Diagnosis & Management (v2 - 09.2016)Document37 pagesENS Guide To Diagnosis & Management (v2 - 09.2016)Renato Mondani0% (1)
- Change'your'water.' ' ' ' ''Change'your'life'222': Some Beneficial Uses of Kangen WaterDocument1 pageChange'your'water.' ' ' ' ''Change'your'life'222': Some Beneficial Uses of Kangen WaterGyaan WallahNo ratings yet
- NEW SOP - ReviewedDocument2 pagesNEW SOP - ReviewedAparna RoyNo ratings yet
- Public Health Surveillance & ScreeningDocument58 pagesPublic Health Surveillance & ScreeningKonjit MitikuNo ratings yet
- Delsa Hea WD HWP (2021) 4Document140 pagesDelsa Hea WD HWP (2021) 4ghoudzNo ratings yet
- Documentation Asset Doc Loc 3417883 DeckingDocument9 pagesDocumentation Asset Doc Loc 3417883 DeckingCristiano SilvaNo ratings yet
- Daftar Pustaka Makalah Tahap IDocument2 pagesDaftar Pustaka Makalah Tahap IAulina Refri RahmiNo ratings yet
- Ross, C. (2020) - PTSD As A Future-Oriented Survival Strategy. Richardson The Colin A. Ross Institute For Psychological TraumaDocument5 pagesRoss, C. (2020) - PTSD As A Future-Oriented Survival Strategy. Richardson The Colin A. Ross Institute For Psychological TraumaEraNo ratings yet
- Remunerasi RSDocument39 pagesRemunerasi RSalfanNo ratings yet
- (Oxford Handbooks of Political Science) R. A. W. Rhodes, Sarah A. Binder, Bert A. Rockman-Handbook Political Institutions-Oxford University Press, USA (2006)Document456 pages(Oxford Handbooks of Political Science) R. A. W. Rhodes, Sarah A. Binder, Bert A. Rockman-Handbook Political Institutions-Oxford University Press, USA (2006)Perico de los Palotes100% (2)
- A Generation of Couch Potatoes Lesson Plan PDFDocument2 pagesA Generation of Couch Potatoes Lesson Plan PDFFBNo ratings yet
- Outline of Dissertation On ObesityDocument16 pagesOutline of Dissertation On ObesityLavarn PillaiNo ratings yet
- Bridging The Care GapDocument50 pagesBridging The Care GapChetna AroraNo ratings yet
- Juvenile Justice Reform/Restoring Arkansas Families BillDocument12 pagesJuvenile Justice Reform/Restoring Arkansas Families BillMarine GlisovicNo ratings yet
- Injury Statistics SheetDocument4 pagesInjury Statistics SheetEslam IsmaeelNo ratings yet
- Hostage Negotiation Semi FinalDocument10 pagesHostage Negotiation Semi Finalarianne ayalaNo ratings yet
- Clinical Significance Blood Group AntibodiesDocument8 pagesClinical Significance Blood Group AntibodiesSudeep RathoreNo ratings yet
- Nutrition of Blueberry 10-7-11 MO StrikDocument60 pagesNutrition of Blueberry 10-7-11 MO StrikJesús Miguel Maguiña EspinozaNo ratings yet
- EHS 085 General Security Procedure For Manufacturing Area SampleDocument3 pagesEHS 085 General Security Procedure For Manufacturing Area Samplerozario100% (1)
- Method Statement - MS PipingDocument13 pagesMethod Statement - MS PipingAnish KumarNo ratings yet
- Presentation 1Document15 pagesPresentation 1Hala YousefNo ratings yet
- CG 2nd QuarterDocument9 pagesCG 2nd QuarterAura Anne Rose TanNo ratings yet
- Three Legs of The Practitioner's (Skovholt & Starkey 2010)Document6 pagesThree Legs of The Practitioner's (Skovholt & Starkey 2010)Mia Valdes100% (1)
- Hiradc TableDocument1 pageHiradc TablejookapleeNo ratings yet
- EAPP Week 1-5Document10 pagesEAPP Week 1-5Mon Rey B. DuranNo ratings yet
- Hyperkalemia Approach AND Management: Dr. Renuka RayanaDocument38 pagesHyperkalemia Approach AND Management: Dr. Renuka RayanaSap Modules100% (1)
- VACCP Template Checklist - SafetyCultureDocument7 pagesVACCP Template Checklist - SafetyCulturepattysaborio520No ratings yet