Professional Documents
Culture Documents
NDT Digest Diagnostic and Therapeutic Approach To Peritonitis
NDT Digest Diagnostic and Therapeutic Approach To Peritonitis
Uploaded by
Rendra SyaniOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
NDT Digest Diagnostic and Therapeutic Approach To Peritonitis
NDT Digest Diagnostic and Therapeutic Approach To Peritonitis
Uploaded by
Rendra SyaniCopyright:
Available Formats
Nephrol Dial Transplant (2017) 32: 1283–1284
doi: 10.1093/ndt/gfx226
NDT Digest
Diagnostic and therapeutic approach to peritonitis
Wim Van Biesen1 and Edwina A. Brown2
1
Renal Division, Ghent University Hospital, Ghent, Belgium and 2Imperial College Renal and Transplant Centre, Hammersmith Hospital,
Downloaded from https://academic.oup.com/ndt/article/32/8/1283/4056839 by guest on 18 January 2022
London, UK
Correspondence and offprint requests to: Wim Van Biesen; E-mail: wim.vanbiesen@ugent.be
|| and/or cloudy dialysis effluent, dialysis effluent white cell
INTRODUCTION
|| count >100/ml (after a dwell time of at least 2 h) with >50% poly-
||
Peritonitis is commonly perceived as a frequent complication of || morphonuclear cells or positive dialysis effluent culture.
peritoneal dialysis (PD). In reality, the incidence of peritonitis is
|| It is obligatory for each centre to have a standardized protocol
||
limited to one episode per 24–48 patient-months (0.25– || to ensure correct sampling of dialysate as rapidly as possible, and
0.5 episodes/year), a number comparable to access-related
|| before therapy is initiated, to allow rapid bacterial identification.
||
infection risk in haemodialysis patients. Peritonitis rates vary || Rates of culture-negative peritonitis should be <15%, to allow
within centres and regions due to centre size, patient training
|| targeted therapy. Inoculation of blood culture bottles with dialy-
||
and local expertise with PD [1]. The impact of peritonitis on the || sate effluent is the preferred technique for bacterial culture [4].
success of PD programmes worldwide is substantial. PD perito-
|| Microbiologists should be aware that slow-growing fastidious
||
nitis is associated with a small increase in mortality in patients || bacteria are not uncommon in PD peritonitis and should adapt
|| their culture techniques accordingly, especially if initial cultures
with multiple comorbidities [2]; more importantly, failure to ||
respond to treatment, with subsequent catheter removal, is a || remain negative after 3 days. The place of more advanced identi-
|| fication techniques such as polymerase chain reaction (PCR) or
significant cause of PD technique failure. ||
Within this NDT Digest, we will briefly discuss the diagnos- || 16S-RNA gene sequencing is unclear in the diagnostic workup of
|| PD-associated peritonitis, and so far studies underpinning their
tic and empiric treatment approach to patients presenting with ||
symptoms of PD-associated peritonitis. || utility in the clinical management of peritonitis are lacking [3].
|| Non-infectious causes of cloudy effluent should be considered,
||
|| although they are rather rare. Chemical peritonitis, e.g. due to
|| high concentrations of glucose degradation products, eosinophilic
DIAGNOSTIC APPROACH ||
|| peritonitis, chylous ascites and malignancies are rare causes of
|| non-infectious cloudy effluent. In patients who have a day off
Patients presenting with cloudy dialysis effluent or abdominal ||
pain should trigger a diagnostic and management pathway (flow- || from PD or who are on automated peritoneal dialysis (APD)
|| with a dry day, cloudy effluent can be observed in the first drain
chart). Systemic features such as vomiting, fever and general ||
unwellness can also be present, particularly in patients who || because of accumulation of peritoneal debris; this should disap-
|| pear after rinsing of the peritoneal cavity with fresh dialysate.
present late. These are more common in patients with vision or ||
cognition problems who do not notice or do not realize the signif- || There is no additional diagnostic value of computed tomography
|| scans of the abdomen unless there is a clear indication for a sec-
icance of cloudy dialysate. The clinical appearance of the patient ||
is important in the decision of whether the patient is seriously ill, || ondary peritonitis, e.g. in patients with signs of cholecystitis, or
|| pancreatitis or when the culture shows multi-bacterial growth. In
and thus needs hospitalization, or the course is more benign and ||
can be managed on an outpatient basis. PD units should have a || the latter case, urgent surgical advice should be considered.
||
protocol to inform patients who to contact and where to go as ||
soon as peritonitis is suspected. The key diagnostic step is to
||
||
obtain a sample of dialysate for microscopy and culture as soon || THERAPEUTIC APPROACH
as possible after presentation. The International Society of
||
||
Peritoneal Dialysis (ISPD) criterion [3] for diagnosis of peritonitis || Appropriate antimicrobial therapy should be started as rapidly
is the presence of at least two of the following: abdominal pain
|| as possible. All centres should develop protocols so that therapy
C The Author 2017. Published by Oxford University Press
V 1283
on behalf of ERA-EDTA. All rights reserved.
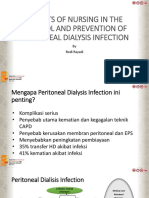
Cloudy effluent
|| ciprofloxacin or fluconazole can be administered orally, but
|| their bioavailability intraperitoneally might vary with inflamma-
||
|| tion and thus sharply decrease when inflammation improves.
|| Antibiotic treatment should be modified once cultures are avail-
White blood cell count and ||
differentiation on effluent || able and the causative organism has been identified. The ISPD
|| peritonitis guidelines provide a useful guide of individual antibi-
||
|| otic dosing [3].
Consider || Although peritonitis is an important complication of PD,
non-infectious > 100 WBC/µl with ||
causes of > 50% polymorphonuclear cells || pharmacokinetics, pharmacodynamics, impact of protein bind-
cloudy effluent ||
|| ing and transperitoneal membrane transport are scarcely inves-
|| tigated. In general, sufficient dwell time should be allowed after
Culture ||
|| intraperitoneal administration, to permit transperitoneal equili-
• Inoculate blood culture bottles with dialysate || bration. Antibiotics should therefore be injected into the day-
||
|| time dwell in APD or into an exchange lasting for a minimum
|| of 6 h on continuous ambulatory peritoneal dialysis.
Start empiric antibiotics
||
|| Vancomycin, gentamicin, cefazolin and ceftazidime can be
Downloaded from https://academic.oup.com/ndt/article/32/8/1283/4056839 by guest on 18 January 2022
• Keep a registry of peritonitis cases in your centre || mixed with dialysate solutions and are stable for at least 24–
with microbial cultures and sensitivity patterns and
||
|| 48 h, and even longer, allowing preparation of a dialysate bag in
adapt antimicrobial therapy accordingly || the centre or by a nurse for self-administration by the patient
• Take into account pharmacokinetics, ||
pharmacodynamics and compatibility with || later on. However, there is concern about mixing vancomycin
dialysate solutions
|| and ceftazidime, and vancomycin might not be stable in alkal-
||
|| ized solutions.
|| Some centres will administer heparin (500 units/L) to avoid
||
Gram positive covering: Gram negative covering: || clotting of the catheter by fibrin, and some centres will use one
Vancomycin 30 mg/kg IP + Gentamicin 1 mg/kg IP || instillation of urokinase to avoid biofilm formation, although
or Cefazolin 1.5 g IP or Ceftazidime 1.5 g IP ||
|| evidence to support these practices is lacking.
• Allow a dwell time of at least 6 hours for equilibration
|| Under normal conditions, signs of inflammation (cloudy efflu-
||
• Avoid mixing vancomycin in alkaline solutions || ent and cell count) should substantially improve in the first 3
NDT DIGEST
• Aim at trough levels for Vancomycin of > 15 µg/ml || days for a non-complicated peritonitis episode. If after 5 days the
||
|| dialysate has not become clear, further diagnostic workup should
FIGURE 1: Flowchart for management of patients presenting with || be done and catheter removal should be considered. After a short
cloudy effluent. ||
|| recovery period on haemodialysis, PD can be successfully
|| resumed after reinsertion of the catheter in most cases [8].
||
||
covers the most frequent causative organisms of peritonitis ||
||
(both Gram negative and Gram positive) in that centre or || REFERENCES
region [5]. With that aim, all centres should register antimicro- ||
|| 1. Rocha A, Rodrigues A, Teixeira L et al. Temporal trends in peritonitis rates,
bial resistance in peritonitis. A recent Cochrane review revealed || microbiology and outcomes: the major clinical complication of peritoneal
that no combination of antimicrobial agents has proven superi- ||
|| dialysis. Blood Purif 2012; 33: 284–291
ority in the management of peritonitis [6]. Most centres will || 2. Boudville N, Kemp A, Clayton P et al. Recent peritonitis associates with mor-
nowadays opt for a regimen with intraperitoneal administration || tality among patients treated with peritoneal dialysis. J Am Soc Nephrol 2012;
||
of vancomycin and an aminoglycoside in the first dwell. This || 23: 1398–1405
choice is based on the broad antimicrobial spectrum covered
|| 3. Li PK, Szeto CC, Piraino B et al. ISPD Peritonitis recommendations: 2016
|| update on prevention and treatment. Perit Dial Int 2016; 36: 481–508
with this combination, the strong post-antimicrobial effect of || 4. Alfa MJ, Degagne P, Olson N et al. Improved detection of bacterial growth in
aminoglycosides and the favourable pharmacokinetics of van-
||
|| continuous ambulatory peritoneal dialysis effluent by use of BacT/Alert FAN
comycin. Single administrations of aminoglycosides (e.g. genta- || bottles. J Clin Microbiol 1997; 35: 862–866
micin 1 mg/kg) do not impact residual renal function [7].
|| 5. Van Biesen W, Vanholder R, Vogelaers D et al. The need for a center-tailored
|| treatment protocol for peritonitis. Perit Dial Int 1998; 18: 274–281
Vancomycin can be added to each bag in low doses (30 mg/kg ||
|| 6. Campbell D, Mudge DW, Craig JC et al. Antimicrobial agents for preventing
loading dose, maintenance 1.5 mg/kg per bag) or intermittently || peritonitis in peritoneal dialysis patients. Cochrane Database Syst Rev 2017; 4:
(30 mg/kg every 5–7 days depending on residual renal function || CD004679
||
and dialysis clearance). It is strongly advisable to monitor van- || 7. Baker RJ, Senior H, Clemenger M et al. Empirical aminoglycosides for perito-
comycin serum levels to ensure adequate serum trough levels || nitis do not affect residual renal function. Am J Kidney Dis 2003; 41: 670–675
|| 8. Cho Y, Badve SV, Hawley CM et al. Peritoneal dialysis outcomes after tempo-
(aim for minimum of 15 lg/mL to avoid emerging || rary haemodialysis transfer for peritonitis. Nephrol Dial Transplant 2014; 29:
vancomycin resistance). ||
|| 1940–1947
There is no clear advantage to administering antibiotics ||
intravenously. In mild cases, antimicrobial agents such as || Received: 24.4.2017; Editorial decision: 23.5.2017
||
||
||
1284 W. Van Biesen and E.A. Brown
You might also like
- Solved Problems Axial DeformationDocument6 pagesSolved Problems Axial DeformationChristopher Largado67% (3)
- ECG PowerApp Bill 1696522537220Document1 pageECG PowerApp Bill 1696522537220hiteshgoti4uNo ratings yet
- CH 04Document110 pagesCH 04Angela Kuswandi100% (1)
- Comic Relief Core Strength Fund - AnalysisDocument25 pagesComic Relief Core Strength Fund - AnalysisNCVO100% (3)
- GFW 411Document8 pagesGFW 411khangha.ptNo ratings yet
- Aspects of Nursing in The Control and Prevention of Peritoneal Dialysis InfectionsDocument27 pagesAspects of Nursing in The Control and Prevention of Peritoneal Dialysis InfectionsNanang AdhoniNo ratings yet
- ANZ Journal of Surgery - 2016 - Gandy - Should The Non Operative Management of Appendicitis Be The New Standard of CareDocument4 pagesANZ Journal of Surgery - 2016 - Gandy - Should The Non Operative Management of Appendicitis Be The New Standard of CarezzethsniperNo ratings yet
- Percutaneous Transhepatic Biliary InterventionsDocument11 pagesPercutaneous Transhepatic Biliary InterventionsLe Hu ThaNo ratings yet
- Absceso Hepatico HarrisonDocument2 pagesAbsceso Hepatico HarrisonZafiss ChaconNo ratings yet
- Peritoneal DialysisDocument6 pagesPeritoneal Dialysisguillermo espinosaNo ratings yet
- CH 7Document35 pagesCH 7Al VinaNo ratings yet
- Classification of Hydatid Cysts According To Gharbi and The World... Download Scientific DiagramDocument1 pageClassification of Hydatid Cysts According To Gharbi and The World... Download Scientific DiagramMucNo ratings yet
- Acute Peritoneal Dialysis in COVID-19Document4 pagesAcute Peritoneal Dialysis in COVID-19Angel SotoNo ratings yet
- Peritoneal Dialysis - Associated Peritonitis: Suggestions For Management and Mistakes To AvoidDocument9 pagesPeritoneal Dialysis - Associated Peritonitis: Suggestions For Management and Mistakes To AvoidAbidi HichemNo ratings yet
- Comparative Effectiveness of Lactulose and Sennosides For The Prevention of Peritoneal Dialysis Related Peritonitis An Open Label Randomized ActiveDocument11 pagesComparative Effectiveness of Lactulose and Sennosides For The Prevention of Peritoneal Dialysis Related Peritonitis An Open Label Randomized ActiveLieblingsmensch andipaNo ratings yet
- AskrpDocument6 pagesAskrpNia marethaNo ratings yet
- Pelvic Inflammatory Disease PDFDocument11 pagesPelvic Inflammatory Disease PDFMa OlayaNo ratings yet
- Guidelines For Patients On Chronic Haemodialysis Programme QehbDocument33 pagesGuidelines For Patients On Chronic Haemodialysis Programme QehbRhys Espinosa100% (2)
- Acute Kidney Injury BMJDocument144 pagesAcute Kidney Injury BMJAreli Rolando SinarahuaNo ratings yet
- Prevention of Adverse ReactionsDocument15 pagesPrevention of Adverse Reactionscupuwatie cahyaniNo ratings yet
- 37-Efectrle Fumatului 3Document3 pages37-Efectrle Fumatului 3Ionut OvidiuNo ratings yet
- PSCRS Guidelines For Colorectal Surgeries During COVID-19: Philippine Journal of Surgical SpecialtiesDocument3 pagesPSCRS Guidelines For Colorectal Surgeries During COVID-19: Philippine Journal of Surgical SpecialtiesAla'a Emerald AguamNo ratings yet
- E023064 FullDocument8 pagesE023064 FullChiperi CristinaNo ratings yet
- Jurnal 1 - Sarhan 2020Document8 pagesJurnal 1 - Sarhan 2020yosefNo ratings yet
- Ppi IadpDocument41 pagesPpi IadpJamal AchmadNo ratings yet
- CoryneDocument8 pagesCoryneEsther Najera GalarretaNo ratings yet
- I Us Tip Id Guideline 2017Document7 pagesI Us Tip Id Guideline 2017dhikaNo ratings yet
- Skin Antisepsis With Chlorhexidine-Alcohol Versus Povidone Iodine-Alcohol, Combined or Not With Use of A Bundle of New DevicesDocument8 pagesSkin Antisepsis With Chlorhexidine-Alcohol Versus Povidone Iodine-Alcohol, Combined or Not With Use of A Bundle of New DevicesHugo PiresNo ratings yet
- Drenaje Quirurgico Vs Endoscopico PsudoquisteDocument9 pagesDrenaje Quirurgico Vs Endoscopico Psudoquistecore6406No ratings yet
- 31435-Texto Do Trabalho (Obrigatório) - 135033-1-10-20230613Document7 pages31435-Texto Do Trabalho (Obrigatório) - 135033-1-10-20230613triutamisunuNo ratings yet
- 20-Dialysis 2016Document10 pages20-Dialysis 2016duchess juliane mirambelNo ratings yet
- J Amjmed 2019 03 025Document6 pagesJ Amjmed 2019 03 025Justin WilliemNo ratings yet
- University of Co Picc Poster Ana ConferenceDocument1 pageUniversity of Co Picc Poster Ana Conferenceingrid.naruto.fbNo ratings yet
- IV Therapy Skills Related To Central Access DevicesDocument81 pagesIV Therapy Skills Related To Central Access DevicesfatmawatiNo ratings yet
- Lammers 2014Document9 pagesLammers 2014DavorIvanićNo ratings yet
- Smith 2021Document4 pagesSmith 2021Sergio Alberto Sulub NavarreteNo ratings yet
- ACI Urology Bladder IrrigationDocument20 pagesACI Urology Bladder IrrigationOlivia BawaedaNo ratings yet
- NigerJClinPract217827-2343919 063039Document5 pagesNigerJClinPract217827-2343919 063039dkprsmdr.yapNo ratings yet
- Nonsurgical Treatment of Appendiceal Abscess or Phlegmon: A Systematic Review and Meta-AnalysisDocument8 pagesNonsurgical Treatment of Appendiceal Abscess or Phlegmon: A Systematic Review and Meta-AnalysisOscar VillacresNo ratings yet
- Peritonitis Clinical Pathway PDFDocument4 pagesPeritonitis Clinical Pathway PDFIndah95No ratings yet
- Peritonitis - The Western Experience: World Journal of Emergency Surgery February 2006Document6 pagesPeritonitis - The Western Experience: World Journal of Emergency Surgery February 2006IbrahimNo ratings yet
- Market FailureDocument3 pagesMarket FailureYappi NaniNo ratings yet
- PIIS0016508519303786Document17 pagesPIIS0016508519303786GdfgdFdfdfNo ratings yet
- Diagnosis and Management of Central Diabetes Insipidus in AdultsDocument8 pagesDiagnosis and Management of Central Diabetes Insipidus in AdultsPenta AssiddiqiNo ratings yet
- AsedrffgvChapter QwescDocument16 pagesAsedrffgvChapter Qwesch68wqhk9nnNo ratings yet
- Derrame Pleural 2015Document16 pagesDerrame Pleural 2015MARIA NEGRETE MOSCOTENo ratings yet
- Giant Bullous Reaction in Response To Tuberculin Test in A Patient of Pelvic Inflammatory DiseaseDocument2 pagesGiant Bullous Reaction in Response To Tuberculin Test in A Patient of Pelvic Inflammatory DiseaseGopal ChawlaNo ratings yet
- Urgent Start Peritoneal DialysisDocument9 pagesUrgent Start Peritoneal Dialysiscarlolo_26No ratings yet
- Complicaciones Endosco AltaDocument7 pagesComplicaciones Endosco AltaJorge Adrian Romero SanchezNo ratings yet
- Oj 2 PDFDocument6 pagesOj 2 PDFAnisah Maryam DianahNo ratings yet
- Distinguishing Fungal and Bacterial Keratitis On Clinical Signs PDFDocument2 pagesDistinguishing Fungal and Bacterial Keratitis On Clinical Signs PDFJennifer ChávezNo ratings yet
- Management of Acute Pelvic Inflammatory Disease: Green-Top Guideline No. 32Document11 pagesManagement of Acute Pelvic Inflammatory Disease: Green-Top Guideline No. 32drshalinikuriNo ratings yet
- Role of DOAC in The Management of COVID-19 Patients: Desak Nyoman Desy LestariDocument32 pagesRole of DOAC in The Management of COVID-19 Patients: Desak Nyoman Desy Lestaridesy lestariNo ratings yet
- The Challenge of Kidney Damage During Interventional Cardiology ProceduresDocument6 pagesThe Challenge of Kidney Damage During Interventional Cardiology ProceduresIJAR JOURNALNo ratings yet
- Bab 1Document1 pageBab 1sari murnaniNo ratings yet
- Bab 1Document5 pagesBab 1sari murnaniNo ratings yet
- Pid 2018Document26 pagesPid 2018Nousen TaraNo ratings yet
- Jurnal 11Document9 pagesJurnal 11adika negaraNo ratings yet
- DiphtheriaDocument1 pageDiphtheriazyanya ceronNo ratings yet
- Eficacy MPIDocument3 pagesEficacy MPIIndah95No ratings yet
- HAI bUNDLESDocument54 pagesHAI bUNDLESNurhayati100% (1)
- COVID-19 Guidelines For Renal Dialysis: 10 February 2022Document19 pagesCOVID-19 Guidelines For Renal Dialysis: 10 February 2022zulfiqarNo ratings yet
- 1 s2.0 S0973688320300281 MainDocument5 pages1 s2.0 S0973688320300281 MainRendra SyaniNo ratings yet
- Mesentery, Omentum, Peritoneum: Inflammatory, Infectious Diseases and Pseudo LesionsDocument11 pagesMesentery, Omentum, Peritoneum: Inflammatory, Infectious Diseases and Pseudo LesionsRendra SyaniNo ratings yet
- 519 968 1 SMDocument13 pages519 968 1 SMRendra SyaniNo ratings yet
- Gut Microbiota, Endocrine-Disrupting Chemicals, and The Diabetes EpidemicDocument14 pagesGut Microbiota, Endocrine-Disrupting Chemicals, and The Diabetes EpidemicRendra SyaniNo ratings yet
- Qgui (@ni (Ir Qgui (@ni (Ir: Fhpishn Hek'dgnDocument8 pagesQgui (@ni (Ir Qgui (@ni (Ir: Fhpishn Hek'dgnRendra SyaniNo ratings yet
- 1 SMDocument9 pages1 SMRendra SyaniNo ratings yet
- UNIT-II AminoglycosideantibioticsDocument5 pagesUNIT-II AminoglycosideantibioticsRendra SyaniNo ratings yet
- Hearing Loss and Associated Risk Factors in Low Birth Weight Infants - A Clinical StudyDocument3 pagesHearing Loss and Associated Risk Factors in Low Birth Weight Infants - A Clinical StudyRendra SyaniNo ratings yet
- Risk Factors of Hearing Defects and Their Relationship To The Outcome of Hearing Screening Among NeonatesDocument6 pagesRisk Factors of Hearing Defects and Their Relationship To The Outcome of Hearing Screening Among NeonatesRendra SyaniNo ratings yet
- Cristobal 2008Document8 pagesCristobal 2008Rendra SyaniNo ratings yet
- Paediatrica IndonesianaDocument8 pagesPaediatrica IndonesianaRendra SyaniNo ratings yet
- Jackson 2018Document13 pagesJackson 2018Rendra SyaniNo ratings yet
- Skin Microbiota: Majalah Kedokteran Sriwijaya, Th. 52 Nomor 1, January 2020Document6 pagesSkin Microbiota: Majalah Kedokteran Sriwijaya, Th. 52 Nomor 1, January 2020Rendra SyaniNo ratings yet
- JurnalDocument9 pagesJurnalRendra SyaniNo ratings yet
- COVID-19 and The Gastrointestinal Tract: More Than Meets The EyeDocument2 pagesCOVID-19 and The Gastrointestinal Tract: More Than Meets The EyeRendra SyaniNo ratings yet
- Homework, References PDFDocument2 pagesHomework, References PDFSeavMeng SengNo ratings yet
- Introduction To Mineral Processing 2010Document24 pagesIntroduction To Mineral Processing 2010elmonemNo ratings yet
- Battery Soc Prediction JournalDocument12 pagesBattery Soc Prediction JournalketamencoNo ratings yet
- Steel Body - Lever Hoists: A e B A e B A e BDocument1 pageSteel Body - Lever Hoists: A e B A e B A e BtylerlhsmithNo ratings yet
- Cinnamon Contact StomatitisDocument2 pagesCinnamon Contact StomatitisDwiNo ratings yet
- Compressor Control, Load Sharing and Anti-SurgeDocument6 pagesCompressor Control, Load Sharing and Anti-SurgeJason Thomas100% (1)
- Police Visibility in The Prevention of Crime PreventionDocument4 pagesPolice Visibility in The Prevention of Crime PreventionDarcknyPusodNo ratings yet
- Maja Blanca RecipeDocument5 pagesMaja Blanca RecipeChristopher PadillaNo ratings yet
- Rega Brio ManualDocument17 pagesRega Brio ManualjamocasNo ratings yet
- Pattern Recognition: Zhiming Liu, Chengjun LiuDocument9 pagesPattern Recognition: Zhiming Liu, Chengjun LiuSabha NayaghamNo ratings yet
- Antiozonates: Rossari Biotech LTDDocument4 pagesAntiozonates: Rossari Biotech LTDEdward MenezesNo ratings yet
- August 12, 2016 Strathmore TimesDocument20 pagesAugust 12, 2016 Strathmore TimesStrathmore TimesNo ratings yet
- Computerized Accounting Using Tally - Erp 9 - Student GuideDocument546 pagesComputerized Accounting Using Tally - Erp 9 - Student Guideshruti100% (1)
- March/April 2016 Cadillac Area Business MagazineDocument16 pagesMarch/April 2016 Cadillac Area Business MagazineCadillac Area Chamber of CommerceNo ratings yet
- IIFL Multicap PMS TermsheetDocument4 pagesIIFL Multicap PMS TermsheetRanjithNo ratings yet
- Nutanix: NCP-MCI-5.15 ExamDocument7 pagesNutanix: NCP-MCI-5.15 ExamAlvin BosqueNo ratings yet
- 501 20B PDFDocument16 pages501 20B PDFTuan TranNo ratings yet
- Proprietary & Confidential: This Is A Static Sensitive Device. Handle & Store Appropriately To Prevent Esd DamageDocument2 pagesProprietary & Confidential: This Is A Static Sensitive Device. Handle & Store Appropriately To Prevent Esd DamagePawan PalNo ratings yet
- GST Accounting EntriesDocument24 pagesGST Accounting EntriesRamesh KumarNo ratings yet
- DentinDocument133 pagesDentinMohammed hisham khan100% (3)
- Avanti Service Lift Pegasus - A Safe Investment: DesignDocument2 pagesAvanti Service Lift Pegasus - A Safe Investment: DesignFrancisco GarciaNo ratings yet
- Nanofiltration - WikipediaDocument7 pagesNanofiltration - WikipediaSrinivas DsNo ratings yet
- WaveLight Allegretto Wave Eye-Q - User Manual PDFDocument232 pagesWaveLight Allegretto Wave Eye-Q - User Manual PDFcmsepulveda100% (2)
- System Software and Microprocessor LabmanualDocument130 pagesSystem Software and Microprocessor LabmanualananthuclashNo ratings yet
- Iygb Gce: Core Mathematics C2 Advanced SubsidiaryDocument5 pagesIygb Gce: Core Mathematics C2 Advanced SubsidiaryssmithNo ratings yet
- Ap4na1r4cmt ADocument6 pagesAp4na1r4cmt AMar GaoNo ratings yet