Professional Documents
Culture Documents
Resin - Resin Bonding - A New Adhesive - Technology
Resin - Resin Bonding - A New Adhesive - Technology
Uploaded by
ComarzzoOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Resin - Resin Bonding - A New Adhesive - Technology
Resin - Resin Bonding - A New Adhesive - Technology
Uploaded by
ComarzzoCopyright:
Available Formats
Resin/Resin Bonding: A New Adhesive
Technology
Ralf Jandaa/Jean-François Rouletb/Michael Wulfc/Hans-Jürgen Tillerd
Purpose: Evaluation of a new surface treatment method to obtain a good bond strength between a luting
composite and (1) a light-cured, (2) a heat-cured and (3) a thermoplastic resin.
Materials and Methods: Specimens were prepared and tests conducted according to ISO 10477,
Amend. 1. The surfaces of Targis (light cured), SR Isosit (heat cured), and Dental D (thermoplastic) were
ground under water cooling with 400-grit grinding paper, polished with 800-grit paper and air dried. Each
resin material was divided into 3 groups of 10 specimens each. Group 1 was flame treated with a Py-
rosilPen for 5 s/2 cm2, group 2 for 10 s/2 cm2, and group 3 for 20 s/2 cm2. Subsequently, a methacryl
silane was applied, followed by a luting composite. Prior to measuring shear bond strength, the speci-
mens were thermocycled 5000 times in a water bath between 5°C and 55°C. SEM, FTIR investigations,
and fracture analysis were also done. Etched and silanized Empress II – the gold standard – was used
as a control.
Results: The following shear bond strengths were found: treatment time 5 s/2 cm2, Targis 25 (±12)
MPa, SR Isosit 17 (±11) MPa; treatment time 10 s/2 cm2, Targis 23 (±12) MPa, SR Isosit 26 (±8) MPa;
treatment time 20 s/2 cm2, Targis 29 (±5) MPa, SR Isosit 26 (±9) MPa. All Dental D specimens failed
completely so that shear bond strength could not be measured. The control achieved 27 (±6) MPa. No
significant differences were found between the materials or the flaming times. On all flamed surfaces,
Si was detected by FTIR. SEM showed that no heat destruction occurred at a flaming time of 5 s/2 cm2,
a slight change at 10 s/2 cm2, and a significant change at 20 s/2 cm2.
Conclusion: This new bonding technology is an effective method for surface-treating polymerized com-
posite resin materials to obtain good bonding to luting composites. The method fails on thermoplastic
resins.
J Adhes Dent 2002; 4: 299–308. Submitted for publication: 27.08.01; accepted for publication: 06.09.02.
t is very problematic to bond resins to other,
a Associate Professor, Dept. of Operative and Preventive Dentistry
and Endodontics, Faculty of Medicine (Charité), Humboldt Universi-
I already cured and highly crosslinked resins. In
practice, this problem always arises when indi-
ty, Berlin, Germany.
b Professor, Dept. of Operative and Preventive Dentistry and Endo- rectly luting manufactured composite inlays, on-
dontics, Faculty of Medicine (Charité), Humboldt University, Berlin, lays, crowns, or bridges to hard dental tis-
Germany.
sues.11-14,24,29,33,36,40,42,43,50 Although in vitro in-
c Graduate Student, Dept. of Operative and Preventive Dentistry and
Endodontics, Faculty of Medicine (Charité), Humboldt University,
vestigations show that light-cured composite inlays
Berlin, Germany. bond better to luting composites than do
d President of Innovent eV, Technology Development, Jena, Germany. heat-cured composites, the bond is still not opti-
mal.2 Furthermore, it must be noted that other
studies have proven that an optimized curing pro-
cess (heat curing, laboratory light curing, or light
Reprint requests: PD Dr. R. Janda, Dept. of Operative and Preventive curing followed by heat treatment) results in a high-
Dentistry and Endodontics, Faculty of Medicine (Charité), Humboldt
University, Augustenburger Platz 1, 13353 Berlin, Germany. Fax: er conversion rate and thus in superior composite
+49-30-450-56-29-61. e-mail: rjanda1108@aol.com properties.26,27 However, the higher conversion
Vol 4, No 4, 2002 299
Janda et al
Fig 2 Layers created by the Silicoater technique.
Fig 1 PyrosilPen.
rate might negatively affect the bond strength to The present study investigates a new surface
the luting composite. Recently, new fiber-rein- treatment method called the PyrosilPen technique
forced composite materials for manufacturing (SurA Instruments, Jena, Germany). The PyrosilPen
crowns and bridges have been introduced and in- (Fig 1) is a very special, small hand-held lighter con-
vestigated. It is recommended that these restora- taining a mixture of butane gas and a silane (tetra-
tions also be luted with an appropriate luting com- ethoxy silane). The flame is lit by a piezo element.
posite.7,21,28,30,41,49 The substrate surfaces are flame treated for only a
To obtain an acceptable bond strength between few seconds. Then SurALink (SurA Instruments), a
the luting composite and the cured composite res- proprietary solution of 3-methacryloyl oxypropyl tri-
toration, various surface pretreatment methods methoxy silane in an organic solvent, is brushed on
have been tested in vitro, such as sandblasting, the surface. Finally, the composite material is ap-
hydrofluoric acid etching, phosphoric acid etching, plied.
roughening with burs, silicating and silanizing, or The PyrosilPen technique is based on the Sili-
combinations thereof.1,6,16,29,33,36,43,44,50 Howev- coater technique (Heraeus-Kulzer, Hanau, Germa-
er, the reported results are not uniform and some- ny) developed in 1984.17,18,20,22,32,35,37-39,45 For
times even contradictory. Stokes et al43 reported the first time, this system allowed a very strong and
shear bond strength values of 19 MPa, Haller et long-lasting adhesive bond to be created between
al12 10 to 50 MPa, and Ludwig33 21 to 24 MPa. resins and precious as well as nonprecious met-
Krämer et al,29 who used a different test method, als.10,23-25,48 More recently, this technique has
obtained bond strength values of approximately also been used to bond luting composites to zirco-
48 MPa. The reported in vitro tests are complicat- nia and alumina ceramics.9,13 The Silicoater is a
ed. Moreover, it is also very difficult to compare lab device for flame-treating metal or ceramic. The
the results of the in vitro tests mentioned, since fuel gas is butane, which is burned with atmospher-
each one of the authors used a different test pro- ic oxygen. Prior to lighting the gas, it is guided over
cedure. a container filled with tetraethoxy silane. After light-
In addition, clinical investigations have been ing, this silane decomposes in the flame, and
conducted comparing composite inlays that had SiOx-C fragments are created. Objects put in the
undergone different pretreatments prior to inser- flame are covered by a layer of these SiOx-C frag-
tion with adhesively (etched and silanized) insert- ments that bond adhesively (van der Waals forces)
ed ceramic inlays.3,16,34,47 These tests proved onto the substrate surfaces.38,45 This extremely
that marginal integrity of composite inlays was not thin layer (ca 0.1 µm)38,45 has glasslike properties
as good as the adhesively inserted ceramic inlays. and can be silanized with 3-methacryloyl oxypropyl
Based on these results, it seems to be appropriate trimethoxy silane, which polymerizes with acrylic or
to look for a more reliable, simpler technique to methacrylic groups. Figure 2 schematically shows
bond already cured composite inlays to a luting the single layers created by the Silicoater tech-
composite. nique. However, the Silicoater technique was rather
300 The Journal of Adhesive Dentistry
Janda et al
complicated, expensive, susceptible to difficulties,
and could not be applied chairside.
The PyrosilPen is based on the same technology
but is much easier to use, even chairside, less sus-
ceptible to difficulties, and much more cost effec-
tive. Furthermore, this technique is expected to be
applicable for all types of composite materials.
Therefore, it was the purpose of this study to eval-
uate whether this new bonding technique leads to
optimal adhesion between various polymerized Fig 3 Device to measure shear bond strength according
composite materials and a luting composite in ISO 10477 Amendment 1.
comparison to the clinically well-proven etched and
silanized ceramic/luting-composite bond. The null
hypothesis was that the PyrosilPen does not per-
form as well as the etched and silanized ceram-
ic/luting-composite method.
with sharp edges, was put onto the composite
specimens. Heliobond (Ivoclar/Vivadent) was ap-
MATERIALS AND METHODS plied through this hole with a brush in an extremely
thin layer. Then the bore of the mold was filled with
The following composites were used: the light-curing component of Variolink II. The sur-
face of Variolink II was covered with a microscopic
• Targis, light-curing hybrid composite (Ivoclar/Vi- slide mount. Light curing was done for 40 s with a
vadent, Schaan, Liechtenstein) Translux light unit (Heraeus-Kulzer, Hanau, Germa-
• SR Isosit, heat-curing microfilled composite (Ivo- ny). After polymerization, the polyoxymethylene
clar/Vivadent) mold was carefully removed and the Variolink II
• Dental D, polyacetale thermoplastic resin composite cylinder remained on the composite sur-
(Shera, Lemförde, Germany) face. After 24 h dry storage according to ISO
10477 Amendment 1, all specimens were ther-
Variolink II (Ivoclar/Vivadent) was used as the mocycled 5000 times in water between +5 and
luting composite. +55°C. The dwell time at each temperature was
In accordance with ISO 10477 Amendment 1, 30 s. Prior to measuring shear bond strength, the
rectangular specimens with the dimensions 20 specimens were brought to room temperature in a
(±1) x 10 (±1) x 2 (±0.5) mm were provided by the water bath.
respective manufacturing company. The resin spec- As a control, Empress II frame ceramic was
imens were ground under water cooling with used. Etching was performed with Vita Ceramics
400-grit grinding paper and afterwards polished Etch (Vita Zahnfabrik, Bad Säckingen, Germany)
with 800-grit paper and air dried. Each group was for 60 s. The etching gel was sprayed off com-
divided into three subgroups of ten specimens pletely with water and the ceramic surface was
each: subgroup 1 was flamed for 5 s/2 cm2, sub- dried with oil-free air. The silane solution Mono-
group 2 for 10 s/2 cm2, and subgroup 3 for 20 s/2 bond-S (Vivadent/Ivoclar) was applied, and after
cm2. To avoid thermal destruction due to flame 60 s, the solvent was removed under an oil-free
treatment times of more than 5 s/2cm2, the resin air stream. Heliobond and Variolink II applications
specimens were flamed stepwise for 2 s until the as well as thermocycling were done as described
final treatment time was obtained. After flame above. The shear test was carried out according to
treatment, the specimens were cooled down to ISO 10477 Amendment 1. The specimens were
room temperature for 3 min and the silane solution fixed in a special apparatus for testing the shear
SurALink was brushed on. The organic solvent bond strength (Fig 3). The whole assembly was
evaporated within a few seconds. Next, a polyoxy- placed in a Universal Testing Machine (Zwick, Ulm,
methylene mold having a slightly conical hole with Germany). The cylinder formed by the luting com-
a large diameter of 5 ± 0.1 mm, a small diameter posite was loaded with a constant crosshead
of 4.9 ± 0.1 mm, and a height of 2.0 ± 0.05 mm speed of 1 (± 0.3) mm/min. The load at breaking
Vol 4, No 4, 2002 301
Janda et al
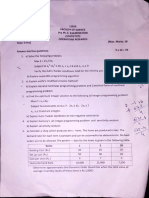
Table 1 Shear bond strengths (SBS) of Variolink II on a light-curing
and a heat-curing composite material
Material mean SBS (SD) in MPa
Flame treatment time
5 s / 2 cm2 10 s / 2 cm2 20 s / 2 cm2
Light curing (Targis ) 25 (12) 23 (12) 29 (5) ns
Heat curing (SR Isosit) 17 (11) 26 (8) 26 (9) ns
ns ns ns
Empress II, etched, silanized (control): 27 (6)
ns = not significant
was recorded and the bond strength B was calcu- RESULTS
lated in MPa using the formula B = F/S, in which F
is the load in N at breaking and S is the bonded Means and standard deviations of shear test re-
area of the cylinder of luting composite in mm2. sults are given in Table 1. No statistical difference
The data of shear bond tests were statistically could be observed between Targis and SR Isosit.
analyzed by two-way ANOVA and the Bonferroni post However, Dental D failed totally, so that no mea-
hoc test (p < 0.05) to investigate the influence of surements could be taken after thermocycling. Sta-
material and flame treatment time. The recorded tistical analysis did not reveal any significant differ-
data follow a normal distribution. One-way ANOVA ences between the flame treatment times of 5, 10,
and the Bonferroni post hoc test (p < 0.05) was and 20 s/2 cm2 for each resin (p > 0.05) and the
used to compare the test groups with the control. control.
To investigate whether the flame-treated surfac- FTIR difference (Fig 4) spectra clearly indicated
es were covered with silicon atoms, they were ex- that all flame-treated surfaces were covered with
amined using a Fourier-transform infrared spectro- silicon atoms (strong absorption band at 1230 to
photometer (FTIR) (Biorad Laboratory, Hempstead, 1259 cm-1). This effect was already reported with
UK). First, a reference spectrum of the non-sur- the Silicoater technique,17,18,20,22,32,35,38,39,45 in-
face-treated specimen was scanned and stored by dicating that the PyrosilPen functions similarly.
the computer. Then the flame-treated specimen SEM investigation of the Dental D (thermoplastic
was scanned, and the computer calculated the dif- resin) specimens after polishing with 800-grit sand-
ference spectrum. Therefore, the finally recorded paper but before flaming showed a severe destruc-
spectrum only represents the treatment effect. tion of the surface. The surface of the specimen
SEM (1810 Scanning Electron Microscope, Am- was rough with projecting resin tags. This is entirely
ray, Bedford, MA, USA) investigations of the speci- different with Targis and SR Isosit after polishing
men surfaces were carried out after polishing as and before flaming. SEM reveals that after polish-
well as after the different flaming times, in order to ing with 800-grit sandpaper, Targis and SR Isosit
evaluate the polished surfaces and whether the had very smooth surfaces. No microretentive pat-
heat occurring during the flame treatment with the tern could be detected (Fig 5).
PyrosilPen influences or even destroys the charac- SEM investigation was also carried out on the
teristic of the composite surfaces. polished and flame-treated specimens. The results
Finally, a fracture analysis was carried out by vi- are shown in Fig 6. Regarding Targis and SR Isosit,
sual inspection to determine the type of failure (co- no destruction was detected after a treatment time
hesive and/or adhesive). of 5 s/2 cm2. The surfaces started to show a slight
302 The Journal of Adhesive Dentistry
Janda et al
Fig 4 FTIR difference spectrum of flamed polymerized composite surface.
Fig 5 SEM image of the speci-
mens polished with 800-grit sand-
paper. No microretentive pattern or
destruction can be seen on Targis
and SR Isosit. Surface destruction
can be detected on Dental D
(340X). Targis (a), SR Isosit (b),
Dental D (c).
change after being flamed for 10 s/2 cm2 and a se- Furthermore, a fracture analysis to determine
vere destruction after 20 s/2 cm2. Therefore, flam- cohesive and adhesive failures was conducted. In
ing times longer than 5 s/2 cm2 were done step- reference to the control, only cohesive failures
wise in periods of 2 s. SEM revealed that this pro- could be observed in the Empress II ceramic. Con-
cedure did not damage composite surfaces. The be- cerning Targis and SR Isosit, the following failure
havior of the thermoplastic resin Dental D was again characteristics were observed: At a treatment time
different. The resin tags projecting from the surface of 5 s/2 cm2, Targis showed 10% adhesive failure
after polishing were molten after flaming, and loose- and 90% cohesive in the Targis material; SR Isosit
ly cover the surface in an overlapping manner. displayed 30% adhesive failure and 70% cohesive
Vol 4, No 4, 2002 303
Janda et al
Targis SR Isosit Dental D
5s
20s
(10×2s)
20s
(continuously)
Fig 6 SEM images of the specimens after different flaming times (1000X).
in the SR Isosit material. At a treatment time of DISCUSSION
10 s/2 cm2, Targis showed 20% adhesive and 80%
cohesive failure in the Targis material. At the same The shear bond strength of a luting composite on
treatment time, SR Isosit exhibited 50% adhesive different resin materials was investigated in this
failure and 50% cohesive in the SR Isosit material. study after using a new bonding technique called
At a treatment time of 20 s/2 cm2, Targis showed PyrosilPen. None of the investigators in the report-
100% cohesive failure in the Targis material and SR ed literature used a standardized method to evalu-
Isosit showed 20% adhesive and 80% cohesive fail- ate bond strength between the cured composite
ure in the SR Isosit material. and the luting composite. For this reason, it is very
The results indicate that 50% to 80% of all fail- difficult to compare the various reported in vitro re-
ures are cohesive in the SR Isosit composite and sults. The present investigation followed dental
80% to 100% in the Targis composite. This explains standard ISO 10477 Amendment 1 – developed to
the high standard deviation calculated (Table 1), investigate bond strength between metal and resin
since the bond strength is higher than the inherent – to measure shear bond strength. Although it is
strength of the tested composites. usually normal procedure, the composite surfaces
304 The Journal of Adhesive Dentistry
Janda et al
were not sandblasted or roughened to avoid the in- times in water between 5°C and 55°C), in addition
fluence of microretentions on the bond strength. to a significantly better performance by the
The only intention of this study was to investigate light-cured composites (approximately 50 MPa).
the performance of the Pyrosil technique. Sandblasting did not significantly influence shear
Furthermore, Empress II frame ceramic was used bond strength of the tested materials. Without sand-
as the control. This is justified by the fact that nu- blasting, the heat-cured composite did not bond at
merous clinical investigations16,36,44 have shown all (shear bond strength ca 0.4 MPa). The sand-
that there is no completely optimal bond between a blasted samples achieved approximately 10 MPa.
polymerized composite and luting composite. How- Ludwig33 measured shear bond strength of a
ever, the procedure of etched and silanized ceram- heat-cured microfilled composite to a dual-curing
ic/luting composite is clinically well known, proven, luting composite. The microfilled composite speci-
and established, and is considered to be the gold mens were conditioned by different methods. After
standard. To guarantee that optimal conditions thermocycling (1000 cycles between 15°C and
were available for this system, the manufacturer’s 65°C), lower values were obtained as compared to
instructions for use were followed. A further reason the 24 h values. The conditioning methods sand-
why none of the methods described by other blasting and cleaning with hydrofluoric acid etching
authors1,6,16,29,33,36,43,44,50 was used in this gel, sandblasting and cleaning with hydrofluoric
study, was that sandblasting – commonly the first acid etching gel followed by an application of a spe-
step of surface conditioning – had to be avoided in cial MMA-containing bonder, and sandblasting and
the present study for the reasons mentioned above. cleaning with hydrofluoric acid etching gel followed
If the PyrosilPen is expected to compete, it by 5 min of etching in an ultrasound bath with 10%
needs to be seen as a truly innovative and promis- hydrofluoric acid, showed the best results with
ing technique. Composite inlays and onlays are of shear bond strength values between approximately
increasing interest in restorative dentistry. There- 21 and 24 MPa. The conditioning method sand-
fore, the question of how to adhesively bond al- blasting and cleaning with hydrofluoric acid etching
ready cured composite restorations to hard dental gel followed by 5 min of etching in an ultrasound
tissues has been discussed by several investiga- bath with 40% hydrofluoric acid achieved a signifi-
tors.1,7,12,16,29,31,33,36,43,44,50 cantly lower bond strength of ca 15 MPa.
With respect to the present investigation, the Krämer et al29 investigated bond strength be-
most important literature shall be reviewed in more tween a light-cured hybrid composite and a dual-cur-
detail, since it shows the difficulties of achieving a ing luting composite. A completely different test
good bond between a cured composite and a luting method was used by preparing standardized cavi-
composite. ties in light-cured hybrid composite specimens in
Stokes et al43 investigated shear bond strength such a way that they formed holes. The inlays were
between a heat-cured hybrid composite and a du- directly shaped and cured in these cavities. After
al-curing luting composite. The specimens were removing the inlays of the cavities, the inner surfac-
conditioned by sandblasting, hydrofluoric acid etch- es of the cavities were sandblasted by a standard-
ing, and/or silanizing. Next, the dual-curing luting ized process. The inlay surfaces were conditioned
composite was applied in the form of cylinders. Pri- by the following methods:
or to measuring shear bond strength, the speci-
mens were stored in water at 37°C for 7 days. For 1. no conditioning
all conditioning methods, shear bond strength val- 2. silanizing
ues around 19 MPa were measured. Stokes et al 3. etching and silanizing
considered these values as sufficient for an accept- 4. sandblasting
able clinical performance. 5. roughening with rotating instruments
Haller et al12 tested the shear bond strength of 6. roughening with rotating instruments, etching
three light-cured inlay composite materials as well and silanizing
as one heat cured and the respective dual-curing lut- 7. using Rocatector -Intraoral
ing composite. The surfaces were pretreated by sev-
eral methods. As a general conclusion, the results Then the hybrid composite inlays were inserted
showed a significant difference between the non- into the hybrid composite cavities after the respec-
thermocycled and the thermocycled group (1440 tive surface treatment by using the dual-curing lut-
Vol 4, No 4, 2002 305
Janda et al
ing composite. Bond strength was measured by tem works according to almost the same principle
pushing the inlays through the cavities after 24 h as the PyrosilPen. By a blasting process, a silicon
storage in water followed by 1440 thermocycles in dioxide is fixed on the composite surface. In a fol-
water between 5°C and 55°C. Bond strength values lowing step, a silane coupling agent is applied, cre-
increased from conditioning method No. 1 (ca ating the bond to the luting composite. However, the
28 MPa) to method No. 7 (ca 48 MPa). Condition- first step of this system, too, is a sandblasting pro-
ing method No. 7 significantly achieved the best cedure.
performance. As already stated above, none of the results pro-
Shear bond strength was also investigated by vided by the literature can be compared directly
Latta et al31 between a cured composite inlay ma- with ours, since each author used a different test
terial and a luting composite. The surface of the procedure. Only the test by Stokes et al22 is similar
composite inlay material was treated by several to the one used in the present study. He recorded
methods. Microabrasion achieved the best results. bonding values in optimal cases of 19 MPa, which
Mehl et al,36 Hannig,16 and Zuellig-Singer et al50 he considered to be sufficiently high. The present
investigated marginal gap formation of adhesively in- investigation proves that the PyrosilPen technique
serted composite and ceramic inlays after in vitro is a further method which enables light- and
and in vivo service of the inlays. After testing adhe- heat-cured composites to bond to luting compos-
sively restored extracted teeth in a chewing simula- ites with very good shear bond strength. However,
tion device, Mehl et al36 proved that the marginal the flaming time needs to be considered, since
quality of ceramic inlays was superior to that of flaming periods longer than 10 s/2 cm2 will destroy
light-cured hybrid composite. Zuellig-Singer et al50 the resin surfaces. This time seems to be optimal,
investigated marginal integrity of light-cured hybrid and values of approximately 23 to 26 MPa were
composite inlays and ceramic inlays. The inlays man- achieved with SR Isosit and Targis, which are iden-
ufactured of each material were inserted adhesively. tical to the bond strength of the clinically well-prov-
The restored teeth were exposed to a chewing sim- en system of etched and silanized ceramic/luting
ulation test. Zuellig-Singer et al reported no change composite. It was also observed that the majority
in the marginal quality after the chewing simulation of the fractures occurred in the polymerized com-
was conducted. In contrast to this study, Thordrup posite material, which is a further indication of the
et al44 found a tendency of less microleakage for ce- strength of the bond.
ramic inlays compared to composite inlays. Nevertheless, bonding to the thermoplastic res-
Clinical tests proved that marginal integrity of in Dental D (polyacetale) seems to be problematic.
composite inlays was not as good as that of adhe- Pretesting of this material has shown that a shear
sively inserted ceramic inlays. Hannig16 has report- bond strength of ca 10 MPa could be achieved with
ed 67.6% marginal imperfections of heat-cured nonthermocycled specimens. After thermocycling,
composite inlays in Class I and 54.9% in Class II all specimens failed totally, suggesting that the lut-
cavities after a clinical service of seven years. ing composite and the polyacetale separated in the
As described above, the literature reports numer- thermocycling bath. When the nonthermocycled
ous, sometimes very complicated procedures for specimens were examined with SEM after conduct-
adhesively bonding polymerized composite restora- ing the shear bond test, it was observed that the
tions.1,7,12,16,29,31,33,35,43,44,50 The general state- polyacetale resin showed a flaky surface. These
ment can be made that light-cured composites bond scales are considered to be the residues of the
significantly better to luting composites than do tags that had been observed after the polishing
heat-cured.12 Heat-cured composite restorations process and prior to flaming (Fig 5). It is assumed
achieve an acceptable shear bond strength after that the luting composite only bonds to these tags
sandblasting and etching with hydrofluoric acid.33 It and not to the “actual” surface. This indicates that
is very interesting that without sandblasting, no the luting composite had bonded to a loose surface
bond at all could be achieved with heat-cured com- that separated during thermocycling under the in-
posites.12 However, Rocatector-Intraoral (3M Espe, fluence of water from the firm, “actual” surface.
Seefeld, Germany) seems to be a very innovative Whether or not this is true can only be confirmed
and effective bonding technology, which Krämer et by a further investigation using a surface treatment
al29 have reported as achieving the best perfor- method other than polishing, that does not destroy
mance among all other tested methods. This sys- the surface of the polyacetale resin.
306 The Journal of Adhesive Dentistry
Janda et al
CONCLUSIONS 16. Hannig M. Das Randschlussverhalten von Kompositinlays
aus SR-Isosit. Dtsch Zahnärztl Z 1996;51:595-597.
The new bonding technology investigated here, the 17. Hansson O, Moberg LE. Evaluation of three silicoating meth-
ods for resin-bonded protheses. Scand J Dent Res 1993;
PyrosilPen, is considered to be a very helpful and 101:243-251.
effective tool for chairside surface treatment of po- 18. Hansson O. Strength of bond with with Comspan Opaque to
lymerized composite resins to obtain good bonding three silicoated alloys and titanium. Scand J Dent Res 1990;
to luting composites. Further investigations are re- 98:248-256.
quired to determine whether it is possible to effec- 19. Hasegawa EA, Boyer DB, Chan DCN. Microleakage of indirect
composite inlay. Dent Mat 1989;5:388-391.
tively apply this technique to other resin types.
20. Hero H, Ruyter IE, Waarli ML, Huitquist G. Adhesion of resins
to Ag-Pd alloy by means of the silicoating technique. J Dent
Res 1987;66:1380-1385.
REFERENCES 21. Hornbrook DS. Placement protocol for an anterior fiber-rein-
forced composite restoration. Pract Periodontics Aesthet
Dent 1997;9:1-5.
1. Behr M, Rosentritt M, Rosentritt A, Schneider-Feyrer S, Han- 22. Hummel SK, Pace LL, Marker VA. A comparison of two sili-
del G. In-vitro study of fracture strength and marginal adap- coating techniques. J Prosthodont 1994;3:108-113.
tation of fiber-reinforced adhesive fixed partial inlay den-
23. Janda R. Kleben und Klebetechniken. dental-labor 1992;40:
tures. J Dent 1999;27:163-168.
409-415 / 615-628.
2. De Shepper EJ, Tate WH, Powers JM. Bond strength of resin
24. Kappert HF, Schüren M, Fritsch F. Dauerfestigkeitsprüfung
cement to microfilled composites. Am J Dent 1993;6:
des Metall-Kunststoff-Verbundes unter dem Einfluss von
235-238.
Temperaturlastwechseln Quintessenz Zahntech 1996;22:
3. Donly KJ, Jensen ME, Triolo P, Chan D. A clinical comparison 293-307.
of resin composite inlay and onlay posterior restorations and
25. Kern M, Simon MHP, Strub JR. Clinical evaluation of all-ce-
cast-gold restorations at 7 years. Quintessence Int 1999;30:
ramic zirconia posts. A pilot study [abstract 2234]. J Dent
163-168.
Res 1997;76:293.
4. Ebert J, Kunzelmann KH, Krämer N, Pelka M. Schadensan-
26. Kilda KK, Ruyter IE. How different curing methods affect
alyse bei Adhäsivinlays am Beispiel VisioGem. Dtsch Zah-
mechanical properties of composites for inlays when test-
närztl Z 1994;49:932-936.
ed in dry and wet conditions. Eur J Oral Sci 1997;105:353-
5. Ernst CP, Muche A, Willershausen-Zönnchen B, Hickel R. In-vit- 361.
ro-Untersuchung zur Oberflächenbehandlung von Komposit-
27. Kildal KK, Ruyter IE. How different curing methods affect the
inlay-Innenseiten. Dtsch Zahnärztl Z 1994;49:273-275.
degree of conversion of resin-based inlay/onlay materials.
6. Feinman RA, Smidt A. A combination/porcelainfiber-rein- Acta Odontol Scand 1994;52:315-322.
forced composite: a case report. Pract Periodontics Aesthet
28. Koczarski MJ. Utilization of ceromer inlays/onlays for re-
Dent 1997;9:925-929.
placement of amalgam restorations. Pract Periodontics Aes-
7. Frankenberger R, Strobel WO, Baresel J, Trapper T, Kramer thet Dent 1998;10:405-412.
N, Petschelt A. Effect of surface treatment on fatigue behav-
29. Krämer N, Popp S, Sindel J, Frankenberger R. Einfluß der Vor-
iour between Tetric Ceram inlays and Variolink luting com-
behandlung von Kompositinlays auf die Verbundfestigkeit.
posite. Clin Oral Investig 2001;5:260-265.
Dtsch Zahnärztl Z 1996;51:598-601.
8. Giordano R. Fiber-reinforced composite resin systems. Gen
30. Krecji I, Boretti R, Giezzendanner P, Lutz F. Adhesive crowns
Dent 2000;48:244-249.
and fixed partial dentures fabricated of Ceromer/FRC: clini-
9. Göbel R, Luthardt R, Welker D. Experimentelle Untersuchun- cal and laboratory procedures. Pract Periodontics Aesthet
gen zur Befestigung von Restaurationen aus Zirkonoxid und Dent 1998;10:487-498.
Titan. Dtsch Zahnärztl Z 1998;53:295-298.
31. Latta MA, Barkmeier WW. Bond strength of a resin cement
10. Göbel R, Welker, D. Etablierte und neuentwickelte Met- to a cured composite inlay material. J Prosthet Dent 1994;
all-Kunststoff-Verbundverfahren im experimentellen Ver- 71:189-193.
gleich. Dtsch Zahnärtzl Z 1999;54: 644-647.
32. Leinfelder KF, Lacefield WR, Bell W. Effectiveness of a meth-
11. Haller B, Klaiber B, Secknus A. Randschluß zervikaler Kom- od used in bonding resins to metal. J Prosthet Dent 1990;
positinlays in vitro. Dtsch Zahnärztl Z 1990;45:296-299. 64:37-41.
12. Haller B, Klaiber B, Tarenz O, Hofmann N. Zur Verbundfes- 33. Ludwig K. Untersuchungen zur Verbundfestigkeit von Com-
tigkeit zwischen Kompositinlay und Befestigungskomposit. posite und Dualzement. dental-labor 1992;40:2103-2107.
Dtsch Zahnärztl Z 1990;45:669-672.
34. Manhart J, Chen HY, Meuerer P, Scheibenbogen-Fuchsbrun-
13. Hannig M, Albers HK, Prieshoff T, Weinle S. REM-Untersu- ner A, Hickel R. Three-year clinical evaluation of composite
chungen zur Nacharbeitung der Befestigungskompositfuge and ceramic inlays. Am J Dent 2001;14:95-99.
adhäsiv zementierter Kompositinlays. Dtsch Zahnärztl Z
35. Mazurat RD, Pesun S. Resin-metal bonding systems: a review
1990;45:672-675.
of the Silicoating and Kevloc systems. J Can Dent Assoc
14. Hannig M, Albers KH. Kompositinlays aus SR-Isosit im 1998;64:503-507.
klinischen Kurzzeittest. Dtsch Zahnärztl Z 1990;45:236- 239.
36. Mehl A, Godescha P, Kunzelmann KH, Hickel R. Randspal-
15. Hannig M, Weinle S, Albers HK. Der Einfluß modifizierter Prä- tverhalten von Komposit- und Keramikinlays bei ausgedehnt-
parationsformen auf die Randqualität on Kompositinlays aus en Kavitäten. Dtsch Zahnärztl Z 1996;51:701-704.
SR-Isosit. Dtsch Zahnärztl Z 1991;46:609-611.
Vol 4, No 4, 2002 307
Janda et al
37. Musil R, Tiller, HJ. Das Silicoater Verfahren nach fünfjähriger 45. US Patent 4,600,390. Apparatus and method for applying a
klinischer Bewährung. Zahnärztl Praxis 1989;4:124-128. silicon oxide-containing adhesion-promoting layer on metallic
38. Musil R, Tiller, HJ. Der Kunststoff-Metall-Verbund Silicoater- dental prostheses, Kulzer, Wehrheim, Germany.
verfahren. Heidelberg: Hüthig, 1989. 46. Vojvodic D, Predanic-Gasparac H, Brkic H, Celebic A. The
39. Nord RS. Kulzer’s Silicoater: a new technique for bonding bond strength of polymers and metal surfaces using the sil-
methacrylates to metal. Trends Tech Contemp Dent Lab icoater technique. J Oral Rehabil 1995;22:493-499.
1986;3:32-46. 47. Wendt SL, Leinfelder KF. Clinical evaluation of a heat-treated
40. Reinhardt 18KJ. Seitenzahnrestauration mit Composite-Fül- resin composite inlay: 3-year results. Am J dent 1992;5;258-
lung oder Inlay. Phillip J 1994;11:465-472. 262.
41. Rosenthal L, Trinkner T, Pescatore C. A new system for pos- 48. Wirz J, Schmidli F. Neue Kunststoff-Metall-Verbundsysteme
terior restorations: a combination of ceramic optimized poly- und ihre legierungsabhängige Haftqualität. Quintessenz
mer and fiber-reinforced composite. Pract Periodontics Aes- 1996;47:1231-1240.
thet Dent 1997;9:6-10. 49. Zanghellini G. Fiber-reinforced framework and Ceromer res-
42. Sindel J, Ebert J. Einfluß von Befestigungskompositen und torations: a technical review. Signature 1997;4:1-5.
Haftvermittler auf die biaxiale Biegefestigkeit sandgestrahl- 50. Zuellig-Singer R, Krejci I, Lutz F. Effects of cement-curing
ter Komposite. Dtsch Zahnärztl Z 1995;50:459-462. modes on dentin bonding of inlays. J Dent Res 1992;71:
43. Stokes AN, Tay WM, Pereira P B. Shear bond of resin cement 1842-1846.
to post-cured hybrid composites. Dent Mat 1993;9:370-374.
44. Thordrup M, Isidor F, Horsted-Bindslev P. Comparison of mar-
ginal fit and microleakage of ceramic and composite inlays:
an in vitro study. J Dent 1994;22:147-153.
308 The Journal of Adhesive Dentistry
You might also like
- Accelerated Fatigue Resistance of Thick CAD/CAM Composite Resin Overlays Bonded With Light - and Dual-Polymerizing Luting ResinsDocument8 pagesAccelerated Fatigue Resistance of Thick CAD/CAM Composite Resin Overlays Bonded With Light - and Dual-Polymerizing Luting ResinsTiago SpeziaNo ratings yet
- Progress in Materials Science and EngineeringDocument203 pagesProgress in Materials Science and Engineeringjdavidospina100% (1)
- 2011 The - Impact - of - in - Vitro - Aging - On - The - MechDocument13 pages2011 The - Impact - of - in - Vitro - Aging - On - The - MechGeorgi AnaNo ratings yet
- Adhesion ZRDocument4 pagesAdhesion ZRDaniela OliverosNo ratings yet
- Bonding Performance of Self-Adhesive Flowable Composites To Enamel, Dentin and A Nano-Hybrid CompositeDocument10 pagesBonding Performance of Self-Adhesive Flowable Composites To Enamel, Dentin and A Nano-Hybrid CompositeSoraya BouchammaNo ratings yet
- Za Chris Son 1996Document11 pagesZa Chris Son 1996Paola LoloNo ratings yet
- Resin Composite Blocks Via High-Pressure High-Temperature PolymerizationDocument6 pagesResin Composite Blocks Via High-Pressure High-Temperature PolymerizationWilver MuñozNo ratings yet
- Pisani Proenca2006Document6 pagesPisani Proenca2006Fer TorresNo ratings yet
- Long-Term Resin Bond Strength To Zirconia Ceramic: Stefan M. Wegnera/Matthias KernDocument10 pagesLong-Term Resin Bond Strength To Zirconia Ceramic: Stefan M. Wegnera/Matthias KernAnılNo ratings yet
- Silica-Based Nano-Coating On Zirconia Surfaces Using Reactive Magnetron Sputtering: Effect On Chemical Adhesion of Resin CementsDocument9 pagesSilica-Based Nano-Coating On Zirconia Surfaces Using Reactive Magnetron Sputtering: Effect On Chemical Adhesion of Resin CementsFrontiersNo ratings yet
- Cold Gas Spray Titanium Coatings Onto A Biocompatible PolymerDocument3 pagesCold Gas Spray Titanium Coatings Onto A Biocompatible Polymeranwalker123No ratings yet
- J Dental 2015 08 013Document2 pagesJ Dental 2015 08 013OLIVIER JuniorNo ratings yet
- Comparative Study of Impact Strength of Six Acrylic Denture ResinsDocument3 pagesComparative Study of Impact Strength of Six Acrylic Denture Resinsdrmezzo68No ratings yet
- Adhesion To Zirconia Used For Dental Restorations: A Systematic Review and Meta-AnalysisDocument20 pagesAdhesion To Zirconia Used For Dental Restorations: A Systematic Review and Meta-AnalysisPablo Andrés ErazoNo ratings yet
- Cementacion de DisilicatoDocument8 pagesCementacion de DisilicatoAngel Humberto Bermudez ParraNo ratings yet
- JBM A 31162 PDFDocument9 pagesJBM A 31162 PDFAndrew makramNo ratings yet
- Degree of Conversion of Three Composite PDFDocument6 pagesDegree of Conversion of Three Composite PDFFreddy GarciaNo ratings yet
- D - Arcangelo 2007Document8 pagesD - Arcangelo 2007valperlunNo ratings yet
- Magne 2006Document8 pagesMagne 2006valperlunNo ratings yet
- Effect of Polydopamine Coating On AdhesiDocument6 pagesEffect of Polydopamine Coating On AdhesiDoctor JackNo ratings yet
- Bulk Fill Resin Composites Polymerization Properties and Extended Light CuringDocument9 pagesBulk Fill Resin Composites Polymerization Properties and Extended Light Curingmaroun ghalebNo ratings yet
- De Souza Et Al 2014Document9 pagesDe Souza Et Al 2014Daniela Zenteno HeiseNo ratings yet
- AbstractsDocument146 pagesAbstractsAnibal RodriguezNo ratings yet
- An Alternative Method For Thermal Cycling Test - Effect On The Marginal Microleakage and Bond Strength of Dental Polymer Bonded To Dentin PDFDocument5 pagesAn Alternative Method For Thermal Cycling Test - Effect On The Marginal Microleakage and Bond Strength of Dental Polymer Bonded To Dentin PDFilich sevillaNo ratings yet
- 112 Water SorptionDocument8 pages112 Water Sorptioncut nurulNo ratings yet
- Efficacy of Different Surface Treatments For Intraoral Repair of Veneered Zirconia FrameworksDocument8 pagesEfficacy of Different Surface Treatments For Intraoral Repair of Veneered Zirconia FrameworksJulio Torres OrtodonciaNo ratings yet
- Fracture Load and Failure Types of Different Veneered Polyetheretherketone Fixed Dental ProsthesesDocument8 pagesFracture Load and Failure Types of Different Veneered Polyetheretherketone Fixed Dental ProsthesesNelson BarakatNo ratings yet
- Effects of Thermocycling On The Bond Strength of A Resin-Modified Glass Ionomer Cement An in Vitro Comparative Study PDFDocument5 pagesEffects of Thermocycling On The Bond Strength of A Resin-Modified Glass Ionomer Cement An in Vitro Comparative Study PDFKamal ShantoNo ratings yet
- Supragingival Relocation of Subgingivally Located Margins For Adhesive Inlays/Onlays With Different MaterialsDocument7 pagesSupragingival Relocation of Subgingivally Located Margins For Adhesive Inlays/Onlays With Different MaterialsAli Al-QaysiNo ratings yet
- Feldspathic AdhesionDocument5 pagesFeldspathic AdhesionDaniela OliverosNo ratings yet
- Characteristics of Micro-Glass bead/PLA Porous Composite Prepared by ElectrospinningDocument12 pagesCharacteristics of Micro-Glass bead/PLA Porous Composite Prepared by ElectrospinningNounaNo ratings yet
- Cuspal Deflection of Bulk Fill Versus LaDocument7 pagesCuspal Deflection of Bulk Fill Versus LaComarzzoNo ratings yet
- Meerten 2015Document7 pagesMeerten 2015Sourabh GaikwadNo ratings yet
- Self-Adhesive Resin Cements - Adhesive Performance To Indirect Restorative CeramicsDocument7 pagesSelf-Adhesive Resin Cements - Adhesive Performance To Indirect Restorative CeramicsAna Massiel NarváezNo ratings yet
- 1 s2.0 S2666539523000019 MainDocument10 pages1 s2.0 S2666539523000019 MainArunNo ratings yet
- TMP 39 F4Document5 pagesTMP 39 F4FrontiersNo ratings yet
- Effect of Surface Conditioning Techniques On The Resistance of Resin Composite Core Materiais On Titanium PostsDocument6 pagesEffect of Surface Conditioning Techniques On The Resistance of Resin Composite Core Materiais On Titanium PostsFrontiersNo ratings yet
- Improvements of Physical and Mechanical Properties of Electron Beam Irradiation-Crosslinked EVA FoamsDocument6 pagesImprovements of Physical and Mechanical Properties of Electron Beam Irradiation-Crosslinked EVA FoamsAroop Ratan SenNo ratings yet
- Effect of Different Finishing Techniques For Restorative Materials On Surface Roughness and Bacterial AdhesionDocument7 pagesEffect of Different Finishing Techniques For Restorative Materials On Surface Roughness and Bacterial AdhesionsahahhussNo ratings yet
- Does The CO Laser Reduce Bond Strength in Different Types of Ceramic Brackets?Document6 pagesDoes The CO Laser Reduce Bond Strength in Different Types of Ceramic Brackets?megaparamitaNo ratings yet
- Microsoft Word Document NouDocument14 pagesMicrosoft Word Document NouRodica IlincaNo ratings yet
- TMP 6782Document8 pagesTMP 6782FrontiersNo ratings yet
- Influence of Different Surface Treatments On Two-Body Wear and Fracture Load of Monolithic CAD/CAM CeramicsDocument12 pagesInfluence of Different Surface Treatments On Two-Body Wear and Fracture Load of Monolithic CAD/CAM CeramicsLuis Alberto Carpio MorenoNo ratings yet
- TMP 9 DFADocument7 pagesTMP 9 DFAFrontiersNo ratings yet
- Stokes Griffin Et Al 2013 Thermal Modelling of The Laser Assisted Thermoplastic Tape Placement ProcessDocument18 pagesStokes Griffin Et Al 2013 Thermal Modelling of The Laser Assisted Thermoplastic Tape Placement Process1711076053No ratings yet
- 2021 Impact of The Microstructure of CADCAM Blocks On The Bonding Strength and The Bonded InterfaceDocument7 pages2021 Impact of The Microstructure of CADCAM Blocks On The Bonding Strength and The Bonded Interface蔡依芸No ratings yet
- TMP BB85Document8 pagesTMP BB85FrontiersNo ratings yet
- Mitchell 1994Document5 pagesMitchell 1994NAHLA ELKHOLYNo ratings yet
- Applied Surface Science: Ting Zhou, Xudong Cheng, Yuelei Pan, Congcong Li, Lunlun Gong, Heping ZhangDocument8 pagesApplied Surface Science: Ting Zhou, Xudong Cheng, Yuelei Pan, Congcong Li, Lunlun Gong, Heping ZhangSaba GheniNo ratings yet
- !!!Two-Year Evaluation of A New NanoDocument6 pages!!!Two-Year Evaluation of A New NanoHande Dalgar KemaloğluNo ratings yet
- Cip DentalDocument7 pagesCip DentalRicardo CintraNo ratings yet
- JAD 2699 Cengiz 1pr SCREEN-mWMDocument7 pagesJAD 2699 Cengiz 1pr SCREEN-mWMNaji Z. ArandiNo ratings yet
- 1-5 Sisteme AdeziveDocument10 pages1-5 Sisteme AdezivestuparusamiNo ratings yet
- Influence of Curing Time, Overlay Material and Thickness On Three Light-Curing Composites Used For Luting Indirect Composite RestorationsDocument8 pagesInfluence of Curing Time, Overlay Material and Thickness On Three Light-Curing Composites Used For Luting Indirect Composite RestorationsAbhishek Isaac MathewNo ratings yet
- Evaluation of Different Light-Curing Lamps HalogenDocument7 pagesEvaluation of Different Light-Curing Lamps HalogenKenny Rafael Iglesias AlvarezNo ratings yet
- Acondicionamiento Del ZirconioDocument8 pagesAcondicionamiento Del ZirconioVíctor RodríguezNo ratings yet
- Composite Resin Fillings and Inlays. An 11-Year Evaluation: OriginalarticleDocument10 pagesComposite Resin Fillings and Inlays. An 11-Year Evaluation: OriginalarticleMira AnggrianiNo ratings yet
- TMP 1 BBDocument8 pagesTMP 1 BBFrontiersNo ratings yet
- Effect of Resin Thickness, and Curing Time On The Micro-Hardness of Bulk-Fill Resin CompositesDocument6 pagesEffect of Resin Thickness, and Curing Time On The Micro-Hardness of Bulk-Fill Resin CompositesrespikNo ratings yet
- A Comparative Study of Mechanical Properties of Zinc Acrylate Epoxy nanocomposites Reinforced by AL2O3 and Cloisite®30B and Their Mixture: Tensile Strength and Fracture Toughness: A Comparative Study of Mechanical Properties of Zinc Acrylate Epoxy nanocomposites Reinforced by AL2O3 and Cloisite®30B and Their Mixture: Tensile Strength and Fracture ToughnessFrom EverandA Comparative Study of Mechanical Properties of Zinc Acrylate Epoxy nanocomposites Reinforced by AL2O3 and Cloisite®30B and Their Mixture: Tensile Strength and Fracture Toughness: A Comparative Study of Mechanical Properties of Zinc Acrylate Epoxy nanocomposites Reinforced by AL2O3 and Cloisite®30B and Their Mixture: Tensile Strength and Fracture ToughnessNo ratings yet
- Junji Tagami BioDocument2 pagesJunji Tagami BioComarzzoNo ratings yet
- AAR Course M2 Edudentinternational D Dietschi 2019Document1 pageAAR Course M2 Edudentinternational D Dietschi 2019ComarzzoNo ratings yet
- Zucchelli Masterclass Course Program 2020Document11 pagesZucchelli Masterclass Course Program 2020ComarzzoNo ratings yet
- Unige 85011 Attachment01Document12 pagesUnige 85011 Attachment01ComarzzoNo ratings yet
- Fly - Mos 13.01.15Document1 pageFly - Mos 13.01.15ComarzzoNo ratings yet
- Unige 109773 Attachment01Document7 pagesUnige 109773 Attachment01ComarzzoNo ratings yet
- Proximal Box Elevation With Resin Composite and The Dogma of Biological Width: Clinical R2-Technique and Critical ReviewDocument10 pagesProximal Box Elevation With Resin Composite and The Dogma of Biological Width: Clinical R2-Technique and Critical ReviewComarzzoNo ratings yet
- Microleakage in Class II Composite Resin - Restorations - Total Bonding and Open - Sandwich TechniqueDocument8 pagesMicroleakage in Class II Composite Resin - Restorations - Total Bonding and Open - Sandwich TechniqueComarzzoNo ratings yet
- 2 One Week Flyer Oman Academy Program 29 Sept. To 3 October 2018Document8 pages2 One Week Flyer Oman Academy Program 29 Sept. To 3 October 2018ComarzzoNo ratings yet
- Dental Adhesion Review Aging and StabiliDocument12 pagesDental Adhesion Review Aging and StabiliComarzzoNo ratings yet
- Sato Dentin 2017Document7 pagesSato Dentin 2017ComarzzoNo ratings yet
- Cuspal Deflection of Bulk Fill Versus LaDocument7 pagesCuspal Deflection of Bulk Fill Versus LaComarzzoNo ratings yet
- The Acid Base Resistant Zone in Three deDocument5 pagesThe Acid Base Resistant Zone in Three deComarzzoNo ratings yet
- 2017 Sato Dentin Bonding Durability of Two-Step Self-Etch Adhesives With Improved of Degree of Conversion of Adhesive ResinsDocument7 pages2017 Sato Dentin Bonding Durability of Two-Step Self-Etch Adhesives With Improved of Degree of Conversion of Adhesive ResinsComarzzoNo ratings yet
- Post Operative Sensitivity On Direct ResDocument12 pagesPost Operative Sensitivity On Direct ResComarzzoNo ratings yet
- 1 Introduction To Anatomy For Medical StudentDocument13 pages1 Introduction To Anatomy For Medical StudentOroAsle ManNo ratings yet
- Prof - Ed Part 13Document6 pagesProf - Ed Part 13Akmad Ali AbdulNo ratings yet
- Test Bank For Canadian Organizational Behaviour 7th Edition McshaneDocument44 pagesTest Bank For Canadian Organizational Behaviour 7th Edition Mcshanearieldonald6kp7rhNo ratings yet
- J. J. Thomson and The Electron: 1897-1899 An IntroductionDocument42 pagesJ. J. Thomson and The Electron: 1897-1899 An IntroductionJBNo ratings yet
- Alan Freeman - Booms Depressions and The Rate of ProfitDocument22 pagesAlan Freeman - Booms Depressions and The Rate of ProfithajimenozakiNo ratings yet
- Heat Treating of Titanium and Titanium Alloys: Charles Carson, Fort Wayne Wire Die, Inc., RetiredDocument24 pagesHeat Treating of Titanium and Titanium Alloys: Charles Carson, Fort Wayne Wire Die, Inc., RetiredAmin AminiNo ratings yet
- Statistics or Paper Pre PHD 2022Document2 pagesStatistics or Paper Pre PHD 2022muragesh mathNo ratings yet
- Reading Diary 211Document3 pagesReading Diary 211phongdz201205No ratings yet
- Implementation of The Contensou-Erismann Model ofDocument12 pagesImplementation of The Contensou-Erismann Model ofJarek PlaszczycaNo ratings yet
- MC OpenmpDocument10 pagesMC OpenmpBui Khoa Nguyen DangNo ratings yet
- Sample Toposheet Practice 1Document5 pagesSample Toposheet Practice 1Shalini AravindanNo ratings yet
- Geo Notes FinalDocument65 pagesGeo Notes FinalSachi Rain LiccudNo ratings yet
- Week 9Document33 pagesWeek 9notabc gamerNo ratings yet
- Ce343 Software EngineeringDocument55 pagesCe343 Software EngineeringD20CE183 HIREN SHYAM RUGHANINo ratings yet
- Quiz - Lab Safety and ApparatusDocument1 pageQuiz - Lab Safety and ApparatusJohn Kristoffer RoblezaNo ratings yet
- Tai Lieu Toefl Stucture Bank Part 11Document10 pagesTai Lieu Toefl Stucture Bank Part 11Hà NguyễnNo ratings yet
- AE ProductCatalog Semiconductors EN 202207Document40 pagesAE ProductCatalog Semiconductors EN 202207Clayse RalphNo ratings yet
- Grounding SystemDocument186 pagesGrounding Systemjerry TomasNo ratings yet
- Pi2094 00 - en UsDocument4 pagesPi2094 00 - en UsMauro GonzalezNo ratings yet
- İzmir Ekonomi Üniversitesi Hazırlık Atlama Pie Sample WebDocument28 pagesİzmir Ekonomi Üniversitesi Hazırlık Atlama Pie Sample WebMustafa KutanNo ratings yet
- Material 1 (Writing Good Upwork Proposals)Document3 pagesMaterial 1 (Writing Good Upwork Proposals)OvercomerNo ratings yet
- Testing Requirements of API 5CRA - Rev2Document2 pagesTesting Requirements of API 5CRA - Rev2ganis supriadiNo ratings yet
- 2019 11A MAM Test 2 SolutionsDocument11 pages2019 11A MAM Test 2 SolutionsRaghav GanaNo ratings yet
- The Book of Genesis Is An Essential Source For Reflection On Creation and Its Place in GodDocument3 pagesThe Book of Genesis Is An Essential Source For Reflection On Creation and Its Place in GodroshelleNo ratings yet
- Clase 2 Ingles TecnicoDocument6 pagesClase 2 Ingles TecnicoGiselle FigueroaNo ratings yet
- ECSA-book - of - Abstracts - Ecsa2016 (1) (Trascinato)Document2 pagesECSA-book - of - Abstracts - Ecsa2016 (1) (Trascinato)Alessio VovlasNo ratings yet
- NUSC AY2024 Admissions Short Answer QuestionsDocument1 pageNUSC AY2024 Admissions Short Answer Questions20210021493No ratings yet
- Psa CepDocument1 pagePsa CepEisha AzizNo ratings yet
- Methodology Workshop Concept NoteDocument2 pagesMethodology Workshop Concept NoteIma AriateNo ratings yet