Professional Documents
Culture Documents
Chapter 37: Bronchodilators: B) Therapeutic
Chapter 37: Bronchodilators: B) Therapeutic
Uploaded by
skuladilzOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Chapter 37: Bronchodilators: B) Therapeutic
Chapter 37: Bronchodilators: B) Therapeutic
Uploaded by
skuladilzCopyright:
Available Formats
Chapter 37: Bronchodilators
1. The nurse evaluates a theophylline level of 14 mcg/mL as
A) subtherapeutic.
B) therapeutic.
C) toxic.
D) life-threatening.
The therapeutic theopylline level is 10 to 20 mcg/mL.
2. Discharge teaching to a patient receiving a beta-agonist bronchodilator should
emphasize reporting which side effect?
A) Tachycardia
B) Nonproductive cough
C) Hypoglycemia
D) Sedation
A beta-agonist bronchodilator stimulates the beta receptors of the sympathetic
nervous system, resulting in tachycardia, bronchodilation, hyperglycemia, and
increased alertness.
3. Which over-the-counter product, when taken with theophylline, can decrease
theophylline’s serum drug levels?
A) Caffeine
B) Diphenhydramine
C) St. John’s wort
D) Echinacea
St. John’s wort has been shown to enhance the rate of theophylline metabolism, thus
decreasing serum levels.
4. Nonselective adrenergic agonist bronchodilators should be used cautiously in
patients with
A) coronary artery disease.
B) COPD.
C) hyperkalemia.
D) premature labor.
Nonselective adrenergic agonist bronchodilators stimulate beta1 receptors in the
heart and beta2 receptors in the lungs. Stimulation of beta1 receptors can increase
heart rate and contractility, increasing oxygen demand. This increased oxygen
demand may lead to angina or myocardial ischemia in patients with coronary artery
disease.
5. The advantage of salmeterol (Serevent) over other beta2 agonists such as
albuterol (Proventil) is:
A) shorter onset of action.
B) better side effect profile.
C) quicker peak action.
D) longer duration of action.
Salmeterol has a longer duration of action, requiring the patient to use it only twice
a day instead of four times a day with albuterol.
6. Patient teaching regarding the use of antileukotriene drugs such as zafirlukast
(Accolate) should include which statement?
A) “Take the medication as soon as you begin wheezing.”
B) “It will take about 3 weeks before you notice a therapeutic effect.”
C) “This medication works by preventing the inflammation that causes your
asthma attack.”
D) “Increase fiber and fluid in your diet to prevent the common side effect of
constipation.”
Antileukotriene drugs block the inflammatory response of leukotrienes and thus the
trigger for asthma attacks. Response to these drugs is usually noticed within 1 week.
They are not used to treat an acute asthma attack.
7. Which respiratory medication is an antileukotriene drug?
A) Flunisolide (Aerobid)
B) Epinephrine (Adrenalin)
C) Cromolyn sodium (Intal)
D) Montelukast (Singulair)
Montelukast is an antileukotriene drug. Epinephrine is an adrenergic agonist.
Cromolyn is a mast cell stabilizer. Flunisolide is a corticosteroid.
8. Corticosteroids are useful in the treatment of acute respiratory disorders
secondary to their ability to
A) stimulate the immune system.
B) directly dilate the bronchi.
C) increase gas exchange in the alveoli.
D) decrease inflammation.
Corticosteroids suppress the immune system. They do not directly affect
bronchodilation but rather prevent bronchoconstriction as a response to
inflammation.
9. A patient demonstrates understanding of flunisolide (AeroBid) by stating
A) “I will take two puffs to treat an acute asthma attack.”
B) “I will rinse my mouth with water after each use.”
C) “I will immediately stop taking my oral prednisone as soon as I start using the
AeroBid.”
D) “I will not use my albuterol inhaler while I am taking AeroBid.”
Flunisolide is an inhaled corticosteroid. Rinsing the mouth will help prevent oral
candidal infections. It is not used to treat an acute asthma attack and should be
taken with the patient’s bronchodilator medications. If the patient is taking oral
prednisone, it needs to be tapered off in order to prevent acute adrenal crisis since
flunisolide is minimally absorbed systemically.
10. Mast cell stabilizers are most effective in treating bronchoconstriction
associated with which condition?
A) Emphysema
B) Exposure to cold
C) Allergens
D) Infection
Mast cell stabilizers work by preventing the release of chemical mediators that
cause bronchospasm and are most effective in preventing asthma caused by
extrinsic factors such as allergens or exercise.
11.A patient is prescribed albuterol for treatment of an electrolyte imbalance.
Which disorder would the nurse assess this patient for?
A) Hyperkalemia
B) Hypocalcemia
C) Hypernatremia
D) Hyperphosphatemia
Beta2 agonists are thought to stimulate the Na+-K+ adenosinetriphosphatase
(ATPase) ion pump contained within cell membranes. This facilitates a temporary
shift of potassium ions from the bloodstream into the cells, resulting in a temporary
decrease in serum potassium levels. This makes these drugs also useful in treating
patients with acute hyperkalemia.
12. The physician orders ipratropium bromide (Atrovent), albuterol (Proventil),
and beclomethasone (Beclovent) inhalers for your patient. Which action will the
nurse take?
A) Question the order; three inhalers should not be given at one time.
B) Administer the bronchodilator first, wait a few minutes, and then administer
the anticholinergic followed by the corticosteroid several minutes later.
C) Administer each inhaler at 30-minute intervals.
D) Administer the beclomethasone first, followed by ipratropium and albuterol 5
minutes later.
Administering the bronchodilator first allows the other drugs to reach deeper into
the lungs as the bronchioles dilate. Anticholinergics also help bronchodilate but to a
lesser extent. Steroids do not dilate and are therefore given last.
13. Which statement would be included when teaching a patient about the proper
use of metered-dose inhalers?
A) “After you inhale the medication once, repeat until you obtain relief.”
B) “Make sure that you puff out air repeatedly after you inhale the medication.”
C) “Hold your breath for 10 seconds if you can after you inhale the medication.”
D) “Hold the inhaler in your mouth, take a deep breath, and then compress the
inhaler.”
Holding the breath for 10 seconds allows the medication to be absorbed in the
bronchial tree rather than being immediately exhaled.
14. The nurse knows that teaching has been successful if the patient, who is using
the anticholinergic inhaler ipratropium bromide (Atrovent) states
A) “I will increase my intake of caffeine.”
B) “I may gain weight as a result of taking this medication.”
C) “Nausea and vomiting are common adverse effects of this medication, so I will
always take it with meals.”
D) “This inhaler is not to be used alone to treat an acute asthma attack.”
Feedback: INCORRECT
Although ipratropium works to prevent bronchoconstriction and thus secondarily
leads to bronchodilation, a direct-acting bronchodilator is needed to treat an acute
asthma attack.
15. Prior to administering an antileukotriene medication, the nurse would assess
the patient for allergies to which substance? (Select all that apply.)
A) lactose
B) povidone
C) cellulose
D) chlorhexedine
Allergy to povidone, lactose, titanium dioxide, or cellulose derivatives is important
to note because these are inactive ingredients in antileukotriene drugs.
16. Which laboratory value should the nurse assess prior to administering
zafirlukast to a patient?
A) Liver enzymes
B) Cardiac enzymes
C) Renal function tests
D) Complete blood count
Since zafirlukast may lead to liver dysfunction, liver enzyme levels should be
monitored regularly, especially early in the course of therapy.
You might also like
- Fear and Loathing in FaerûnDocument84 pagesFear and Loathing in FaerûnDavide Gobbi100% (1)
- Nbme Step 1 PharmacologyDocument20 pagesNbme Step 1 PharmacologyIshani Patel100% (1)
- CardioVascular and Endocrin ExercisesDocument6 pagesCardioVascular and Endocrin ExercisesBogartNo ratings yet
- RPN - Pharmacology (A)Document12 pagesRPN - Pharmacology (A)Ana BienneNo ratings yet
- Chapter 55 - Drugs Acting On The Lower Respiratory TractDocument13 pagesChapter 55 - Drugs Acting On The Lower Respiratory TractJonathonNo ratings yet
- Oxygenation Test Key AsthmaDocument6 pagesOxygenation Test Key Asthmamelodia gandezaNo ratings yet
- Sample Question Pharma2Document12 pagesSample Question Pharma2Ali ZezoNo ratings yet
- bIOLOGIC cRISIS FINAL QUIZ pHARMACOCHENETICSDocument35 pagesbIOLOGIC cRISIS FINAL QUIZ pHARMACOCHENETICSSusan MaglaquiNo ratings yet
- Pharm 28 29 30 ExamDocument3 pagesPharm 28 29 30 Examkay belloNo ratings yet
- QuestionsDocument61 pagesQuestionsTop MusicNo ratings yet
- Chapter 54 - Drugs Acting On The Upper Respiratory TractDocument13 pagesChapter 54 - Drugs Acting On The Upper Respiratory TractJonathonNo ratings yet
- Pharmacology QuizesDocument30 pagesPharmacology QuizesRM DemetilloNo ratings yet
- Practice ExamDocument15 pagesPractice ExamShay Ann CharltonNo ratings yet
- QuestionsDocument61 pagesQuestionsTop MusicNo ratings yet
- Nclex Review Pneumonia COPD AsDocument11 pagesNclex Review Pneumonia COPD Asmj078No ratings yet
- Pharma Nest HDocument92 pagesPharma Nest HAvner TolentinoNo ratings yet
- Pedia HandoutsDocument15 pagesPedia Handoutskobegsantos24No ratings yet
- 2020 Cholinergic Drugs QuizDocument4 pages2020 Cholinergic Drugs QuizKiller VNo ratings yet
- Vocabulary Test Practice On Pharmacology.Document21 pagesVocabulary Test Practice On Pharmacology.illia1028No ratings yet
- Drugs Affecting Neurologic SystemDocument5 pagesDrugs Affecting Neurologic SystemjustineGREATNo ratings yet
- Medical EmergenciesDocument23 pagesMedical Emergenciesanish mahlawatNo ratings yet
- Pharmacology McqsDocument7 pagesPharmacology McqsAshraf AboNo ratings yet
- Chapter 59 - Antiemetic AgentsDocument11 pagesChapter 59 - Antiemetic AgentsJonathonNo ratings yet
- More Nclex From Evolve ResourcesDocument18 pagesMore Nclex From Evolve ResourcesKristin Bienvenu100% (1)
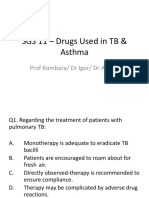
- Sgs 11 - TB & Asthma4Document13 pagesSgs 11 - TB & Asthma4Gx NavinNo ratings yet
- PHARMADocument8 pagesPHARMARegine Dela peñaNo ratings yet
- Pneumonia & TB NCLEX Practice Questions Med SurgDocument20 pagesPneumonia & TB NCLEX Practice Questions Med SurgKirsten ChavezNo ratings yet
- Respiratory System DrugsDocument64 pagesRespiratory System DrugsArlyn MendenillaNo ratings yet
- # CLINICAL PHARMA FINALS MCQs 2021-1-30Document30 pages# CLINICAL PHARMA FINALS MCQs 2021-1-30Pavan chowdaryNo ratings yet
- Quiz 3 Study QuestionsDocument20 pagesQuiz 3 Study QuestionsJessie AllisonNo ratings yet
- Study QuestionsDocument5 pagesStudy QuestionsasemNo ratings yet
- RPN Pharmacology Test (Questions)Document12 pagesRPN Pharmacology Test (Questions)jyselle domingoNo ratings yet
- Question Bank For Pharmacology - WJP AnsweredDocument55 pagesQuestion Bank For Pharmacology - WJP AnsweredGeorge MoshiNo ratings yet
- Eval ExamDocument11 pagesEval ExamKristian Karl Bautista Kiw-isNo ratings yet
- Nonsteroidal Anti-Inflammatory Drugs, Acetaminophen, & Drugs Used in GoutDocument4 pagesNonsteroidal Anti-Inflammatory Drugs, Acetaminophen, & Drugs Used in GoutMahesh ShankarNo ratings yet
- Q - A PharmacologyDocument9 pagesQ - A PharmacologyYuuki Chitose (tai-kun)No ratings yet
- Pharmacology FINALLLpdfDocument223 pagesPharmacology FINALLLpdfRitika NigamNo ratings yet
- PRE Test 1Document15 pagesPRE Test 1Naomi VirtudazoNo ratings yet
- 2 QE Competency 2 MOCK Test May 2014 QADocument46 pages2 QE Competency 2 MOCK Test May 2014 QAAndrew MeNo ratings yet
- CH 46 Part IIquizDocument4 pagesCH 46 Part IIquiznkr59No ratings yet
- Respiratory SystemDocument61 pagesRespiratory SystemJASTINE NICOLE SABORNIDONo ratings yet
- Pharmacology QuestionsDocument33 pagesPharmacology QuestionsPurnimaNo ratings yet
- BOOST Pharm Exam 2 Review - BLANKDocument20 pagesBOOST Pharm Exam 2 Review - BLANKHwi GNDCNo ratings yet
- QUESTIONS ForDocument13 pagesQUESTIONS ForJobelie R. BodionganNo ratings yet
- Dosages and SolutionDocument68 pagesDosages and SolutionRuan MarchessaNo ratings yet
- Pharma Long Quiz KeyDocument3 pagesPharma Long Quiz KeyBiatch NebturaNo ratings yet
- Q & A Random Selection #3Document5 pagesQ & A Random Selection #3Yuuki Chitose (tai-kun)No ratings yet
- UntitledDocument5 pagesUntitledZandile Angeline DhlomonseleNo ratings yet
- Pharm Exam 5 BOOST - BlankDocument2 pagesPharm Exam 5 BOOST - BlankHwi GNDCNo ratings yet
- RS 6 Qs QuizDocument14 pagesRS 6 Qs QuizXajepoxNo ratings yet
- Focus On Nursing Pharmacology 6th Edition Karch Test BankDocument38 pagesFocus On Nursing Pharmacology 6th Edition Karch Test Bankgenericparaxialb41vmq100% (19)
- Focus On Nursing Pharmacology 6Th Edition Karch Test Bank Full Chapter PDFDocument36 pagesFocus On Nursing Pharmacology 6Th Edition Karch Test Bank Full Chapter PDFfionaalexandrahukc100% (13)
- LPN Jan 1Document49 pagesLPN Jan 1wltnz0418No ratings yet
- Prelim Exam NCM 103Document10 pagesPrelim Exam NCM 103Zhyraine Iraj D. CaluzaNo ratings yet
- Prelim Exam NCM 103Document10 pagesPrelim Exam NCM 103Zhyraine Iraj D. CaluzaNo ratings yet
- Nursing Exam Questions 2023 Part 3Document6 pagesNursing Exam Questions 2023 Part 3Lejo SunnyNo ratings yet
- E - Cart DrugsDocument18 pagesE - Cart Drugs'SheenMarkReal'100% (2)
- General Pharma Mcqs 2Document11 pagesGeneral Pharma Mcqs 2hassan qureshiNo ratings yet
- Reviewer Med Surg PT 2Document22 pagesReviewer Med Surg PT 2Lance SilvaNo ratings yet
- NCLEX: Pharmacology for Nurses: 100 Practice Questions with Rationales to help you Pass the NCLEX!From EverandNCLEX: Pharmacology for Nurses: 100 Practice Questions with Rationales to help you Pass the NCLEX!Rating: 5 out of 5 stars5/5 (4)
- Philippine Pharmacy ActDocument63 pagesPhilippine Pharmacy ActpsyarjavierNo ratings yet
- 3rd Newsletter FinalDocument14 pages3rd Newsletter FinalBhavish RamroopNo ratings yet
- Add Risk Min MeasDocument12 pagesAdd Risk Min MeasVladimir KostovskiNo ratings yet
- Ucsp TelDocument14 pagesUcsp TelVincent Ocon PaduaNo ratings yet
- 1 s2.0 S0379073823002256 MainDocument10 pages1 s2.0 S0379073823002256 MainRodeo CrabNo ratings yet
- Borderline Between Cosmetics and Medicinal, Biocidal and Other Types of ProductsDocument37 pagesBorderline Between Cosmetics and Medicinal, Biocidal and Other Types of ProductsTatjana BrankovićNo ratings yet
- Herbal Medicines Usage Among Patients With Chronic Conditions: Case StudyDocument6 pagesHerbal Medicines Usage Among Patients With Chronic Conditions: Case StudyDimas PratamaNo ratings yet
- IBSD Antiviral CompendiumDocument501 pagesIBSD Antiviral Compendiumbharath s100% (1)
- Current Trends in PharmacovigilanceDocument5 pagesCurrent Trends in PharmacovigilanceSutirtho MukherjiNo ratings yet
- Natures CandyDocument19 pagesNatures CandyFanejegNo ratings yet
- 1000 English CollocationsDocument126 pages1000 English CollocationsblindreptileNo ratings yet
- Gemsical Cap (Menrik Biomerge PVT LTD)Document3 pagesGemsical Cap (Menrik Biomerge PVT LTD)Nani GangNo ratings yet
- AccurioLabel400 - PRODUCT - GUIDE v1.3 - ENDocument46 pagesAccurioLabel400 - PRODUCT - GUIDE v1.3 - ENDiego LanderosNo ratings yet
- Essential Medicine List (Updated) (Medex - Com.bd)Document5 pagesEssential Medicine List (Updated) (Medex - Com.bd)Daak ChattalaNo ratings yet
- Use of Market DataDocument214 pagesUse of Market Datamodava-2No ratings yet
- Pellet and Pelletization - Extrusion - Tablet (Pharmacy)Document1 pagePellet and Pelletization - Extrusion - Tablet (Pharmacy)Pragnesh ParmarNo ratings yet
- Drug Registration Guidance Document DRGD - Second Edition Revised - July 2019Document710 pagesDrug Registration Guidance Document DRGD - Second Edition Revised - July 2019Revathy ThandapaniNo ratings yet
- MYRESUMEDocument1 pageMYRESUMELaila JaneNo ratings yet
- Colors of BiotechnologyDocument66 pagesColors of Biotechnologyasdfgh0% (1)
- Class Xii Business Studies Planning: Reason-Based, Evaluation & HotsDocument8 pagesClass Xii Business Studies Planning: Reason-Based, Evaluation & HotsAnshuman SajwanNo ratings yet
- Administration Errors in SEADocument7 pagesAdministration Errors in SEAFrancis NgNo ratings yet
- Dr. Trupti Laxmi SwainDocument107 pagesDr. Trupti Laxmi SwainAnca GligorNo ratings yet
- Patient Information Booklet ST VincentsDocument16 pagesPatient Information Booklet ST VincentsFahad KhanNo ratings yet
- NLE ReviewerDocument247 pagesNLE ReviewerDiana Rose DC0% (1)
- Dossier Structure enDocument29 pagesDossier Structure enKarim HefnyNo ratings yet
- The Drugs and Cosmetics Act, 1940 and Rules, 1945Document177 pagesThe Drugs and Cosmetics Act, 1940 and Rules, 1945Bhaskar Chaurasia100% (3)
- Bib 7fa2d53233d8.p001 PDFDocument4 pagesBib 7fa2d53233d8.p001 PDFИрина ДубовскаяNo ratings yet
- Drugs of Biological OriginDocument4 pagesDrugs of Biological OriginIdenyi Daniel Ewa EdeNo ratings yet
- In Vitro Anticoagulant Activity of Papaya (Carica Papaya) Ethanolic Leaves ExtractDocument14 pagesIn Vitro Anticoagulant Activity of Papaya (Carica Papaya) Ethanolic Leaves ExtractKaye MontildeNo ratings yet