Professional Documents
Culture Documents
Clinical Chemistry Notes With Blanks
Clinical Chemistry Notes With Blanks
Uploaded by
epson printerOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Clinical Chemistry Notes With Blanks
Clinical Chemistry Notes With Blanks
Uploaded by
epson printerCopyright:
Available Formats
CLINICAL CHEMISTRY MTAP
BY: GEORGE VINCENT GELLENA, RMT
Remedios Trinidad Romualdez Medical Foundation
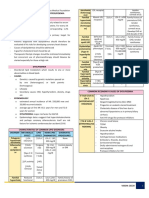
CONTENTS: Table 1. – Types of Error
1 Quality Management Random Error Systematic Error
2 Automation Description
4 Carbohydrates
7 Lipids
10 Proteins
12 Enzymes
16 Non-Protein Nitrogens
18 Liver Function Tests Examples
20 Electrolytes
23 Acid-Base Balance
24 Endocrinology
30 Therapeutic Drug Monitoring
32 Toxicology
QUALITY MANAGEMENT
___________________ - Is a system of ensuring accuracy
Statistics
& precision in the laboratory by including quality control
____________________ – measure of central tendency;
reagents in every series of measurements
measure of accuracy; AVERAGE
___________________- is a systematic action necessary
____________________ – measure of dispersion of
to provide adequate confidence that laboratory services
values from the mean; measure of precision; most
will satisfy the given medical needs for patient care
frequently used measure of variation
___________________ – material of known
____________________ - index of precision; percentile
concentration used in developing a standard curve
expression of the mean
and/or instrument calibration
____________________ - measure of variability
___________________ – sample of known quantity with
____________________ - determines whether there is a
several analytes present
statistically significant difference between the standard
Parameters
deviations of two groups of data
___________________ - Is the Ability of an analytical
____________________ - determines whether there is a
method to measure the smallest concentration of the
statistically significant difference between the means of
analyte of interest
two groups of data
___________________ - Is the Ability of an analytical
____________________ - MIDPOINT of the distribution;
method to measure ONLY the analyte of Interest
value of the observation that divides the observation into
___________________ - Is the Nearness or Closeness of
two equal groups of data
the Assayed value to the true or target value
____________________ – most FREQUENT observation
___________________- The ability of an analytical
____________________ - is the difference between the
method to give repeated results on the same sample that
highest and lowest score in data
agree with one another
___________________ - The degree by w/c a method is Quality Control Charts
____________________ - data element are centered
easily repeated.
___________________ - The ability of an analytical around the mean with most elements close to the mean
method to maintain accuracy & precision over an ____________________ - provides the earliest
extended period of time during w/c equipment, indication of systematic error (trend); requires computer
reagents, & personnel may change implementation
___________________ - The Ability of an analytical ____________________ – compare results obtained on
method to detect the proportion of individuals with the a high and low control serum from different laboratories
disease. (Screening tests require high sensitivity) ___________________________ – most widely used QC
___________________ - The Ability of an analytical chart in the clinical laboratory; allows laboratorians to
method to detect the proportion of individuals without apply multiple rules without the aid of computer;
the disease. (Confirmatory tests require high specificity) identifies both random and systematic error
___________________ – highest frequency occurs with Table 2. Errors observed in LJ Chart
the use of handwritten labels and request forms TREND SHIFT
COLLEGE OF MEDICAL LABORATORY SCIENCE | 1 | 34
Clinical Chemistry
7. __________________ – Displays output of the detection
system
SINGLE BEAM SPECTROPHOTOMETER
Simplest Type; Designed to make one measurement at a
time at one specified wavelength
Westgard Errors on LJ Chart
Table 3. Westgard Control Rules
Random Errors Systematic Errors
_______ – 1 control value _______ – 2 consecutive
exceeds ±2SD; rejection or control values exceed Components of a single-beam spectrophotometer.
warning rule either ±2SD A, Exciter lamp; B, entrance slit; C, monochromator; D,
_______ – 1 control value _______ – 4 consecutive exit slit; E, cuvet; F, photodetector; G, light-emitting
exceeds ±3SD control values exceed ±1SD diode (LED) display
_______ – Range/ _______ – 10 consecutive DOUBLE BEAM SPECTROPHOTOMETER
difference between the control values fall on 1 side Splits monochromatic light into two components: one
highest and lowest control or the other side of the beam passes through the sample and the other through
result within an analytical mean a reference solution or blank
run is 4SD 1. ___________________________ – 2 photodetectors
AUTOMATION
Automation
Wavelength – distance between two successive peaks
400-700 nm – visible spectrum
<400 nm – ultraviolet region (UV)
>700 nm – infrared region
Didymium or holmium oxide filter is used to check
wavelength accuracy
Neutral density filters and dichromate solution verify _______________________. A, Exciter lamp; B,
absorbance accuracy mirror; C, entrance slits; D, monochromators; E, exit
Beer-Lambert’s law slits; F, cuvets; G, photodetectors; H, light-emitting
A = abc = 2 – log%T diode (LED).
o A: molar absorptivity 2. ____________________________ – 1 photodetector
o B: length of light through the solution and 1 chopper or rotating sector mirror
o C: concentration of absorbing molecules
o T: transmittance
One-point calcuation or calibration
𝐶𝑜𝑛. 𝑜𝑓 𝑆𝑡𝑎𝑛𝑑𝑎𝑟𝑑 (𝐶𝑠) 𝐶𝑜𝑛𝑐. 𝑜𝑓 𝑢𝑛𝑘𝑛𝑜𝑤𝑛 (𝐶𝑢)
=
𝐴𝑏𝑠. 𝑜𝑓 𝑆𝑡𝑎𝑛𝑑𝑎𝑟𝑑 (𝐴𝑠) 𝐴𝑏𝑠. 𝑜𝑓 𝑢𝑛𝑘𝑛𝑜𝑤𝑛 (𝐴𝑢)
SPECTROPHOTOMETRY
Measurement of light transmitted by a solution to
determine the concentration
PARTS OF A SPECTROPHOTOMETER
1. __________________ – Provide Polychromatic light
___________________________
2. __________________- Minimizes unwanted or stray
light; prevents entrance of scattered light
3. __________________ – Isolates specific or individual
wavelength of light Excitation of electrons from lower to higher energy state
4. __________________– Controls the width of light beam Measures light emitted by single atom burned in flame;
(bandpass) measures excited ions (Na+ and K+)
5. __________________ – Holds the solution whose
concentration is to be measured
6. __________________ – Detects and converts transmitted Element is not excited but merely dissociated from its
light into photoelectric energy chemical bond and placed in an unionized, unexcited
ground state
COLLEGE OF MEDICAL LABORATORY SCIENCE | 2 | 34
Clinical Chemistry
Measures light absorbed by atoms dissociated by heat; GAS CHROMATOGRAPHY
measures unexcited trace metals (Ca2+ and Mg2+) for naturally volatile compounds or easily converted to
volatile form
___________________ – based on fragmentation
and ionization of molecules using a suitable energy
Unknown sample is made to react with known solution
source
in the presence of an indicator _______________ – gold standard for drug testing
Schales and Schales (Chloride) _______________________ – detects 20 inborn
EDTA titration (Calcium) errors of metabolism from a single blood spot
LIQUID CHROMATOGRAPHY
TURBIDIMETRY
based on distribution of solutes between a liquid mobile
Determines the amount of light blocked by a particulate
phase and a stationary phase
matter in a turbid solution
High performance liquid chromatography (HPLC) –
Used in measuring proteins and bacterial suspensions used in rapid HbA1c testing
Liquid chromatography-Mass Spectroscopy (LC-MS)
NEPHELOMETRY – used in detecting non-volatile substances;
complementary to GC-MS
Determines amount of scattered light by a particulate
matter in a turbid solution FLUOROMETRY/MOLECULAR LUMINESCENCE
Used in measuring antigen-antibody complexes SPECTROPHOTOMETRY
Determines the amount of light emitted by a molecule
after excitation by electromagnetic radiation
Uses 2 monochromators; measures amount of light
intensity present over a zero background; affected by
quenching
Optical Arrangements of Nephelometry and
Turbidimetry
ELECTROPHORESIS
Migration of charged particles in an electric field
Separates proteins on the basis of electrical charge;
Buffer: Veronal/Barbital (pH 8.6) Components of a Fluorometer
DENSITOMETRY
Measures absorbance of stain Chemical reaction yields electronically excited
Scans and quantitates electrophoretic pattern; compound that emits light as it returns to its ground
measures concentration of dye and protein fraction state
Emission of light is created from a chemical or
ISOELECTRIC FOCUSING electrochemical reaction; usually used in immunoassays
Migration through a pH gradient
*pH gradient – created by adding acid to anodic area OSMOMETRY
and base to the cathode area
Based on measuring changes in colligative properties of
Ideal for separating proteins of identical sizes but with solutions
different net charges; detects CSF oligoclonal banding
Freezing-point depression osmometry – most commonly
used method
CHROMATOGRAPHY
Separation of soluble components based on physical
and chemical characteristics
COLLEGE OF MEDICAL LABORATORY SCIENCE | 3 | 34
Clinical Chemistry
ELECTROCHEMISTRY TECHNIQUES CARBOHYDRATES
GLUCOSE
Glucose is the principal and almost exclusive
Measurement of electrical potential due to free ion
carbohydrate circulating in the blood
activity
Glucose is the central, pivotal point of carbohydrate
Use: _______________________
metabolism
____________ is the most important glucose consumer.
Measurement of electricity (Coulombs) at fixed
CNS consumes about 50% of glucose used by the body
potential
Glucose can be derived from (1) diet, (2) from body
Use: _______________________
stores like glycogen, and (3) from endogenous synthesis
from proteins or glycerol of triglycerides.
Measurement of current flow produced by oxidation
reaction
REGULATION OF BLOOD GLUCOSE
Use: _______________________ CONCENTRATION
PROCESSES INVOLVED IN CARBOHYDRATE METABOLISM
Measurement of differences in current at constant 1.
voltage Metabolism of glucose molecule to pyruvate or
Use: Specific for pO 2 and glucose lactate to energy
Decreases blood glucose since glucose is consumed
Measurement of current after which a potential is to produce lactate/pyruvate
applied to an electromechanical cell 2.
Lead and iron testing (anodic stripping voltammetry) Formation of glucose-6-phosphate from non-
carbohydrate sources
THREE BASIC APPROACHES Increases blood glucose; new glucoses are formed
from other sources
3.
Samples flow through a common reaction vessel; uses a
Breakdown of glycogen to glucose for use as energy
system of continuous tubing; ____________________
Increases glucose due to glycogen degradation
Mixing of Sample and Reagent: Glass coil inserted into
4.
the flow path Conversion of glucose to glycogen for storage
Decreases gluceose since excess glucoses in the
Uses acceleration and deceleration of rotor to transfer body is stored in the liver and skeletal muscle as
reagents and sample from one chamber to another; glycogen
___________________________ 5.
Mixing of Sample and Reagent: Conversion of carbohydrates to fatty acids
____________________________________________ Decreases glucose since carbohydrates are
converted into fatty acids and stored as fats
Uses syringe pipettes (positive-liquid displacement) to 6.
aspirate and dispense samples; most versatile and most Breakdown of fats; fats are used as energy
popular; ___________________________________ HORMONES INVOLVED
Mixing of Sample and Reagent: Magnetic driven Teflon 1. Hyperglycemic hormones
stirring bar, etc Glucagon, Epinephrine, Cortisol, Growth hormone,
____________________________ – all samples are Thyroxine
loaded at the same time and a single test is conducted 2. Hypoglycemic hormone
on each sample
Insulin
____________________________ – more than one test
is analyzed concurrently on a given clinical specimen 3. Regulator hormone
____________________________ – any test can be Somatostatin – inhibits release of growth hormone,
performed on any sample in any sequence insulin, and glucagon
____________________________ – multiple tests are
analyzed one after another on a given specimen
____________________________ – a system other SPECIMEN FOR GLUCOSE DETERMINATION
than the manufacturer’s reagents can be utilized for Standard clinical specimen is ______________________
measurement Fasting Blood Sugar should be obtained after
____________________________ – a system where the _____________________________________
operator can only use the manufacturer’s reagent
Venous blood has lower glucose levels compared to
arterial blood
COLLEGE OF MEDICAL LABORATORY SCIENCE | 4 | 34
Clinical Chemistry
Capillary blood has higher glucose levels compared to Table 4. Comparison Between Type 1 and Type 2
venous blood DM
Whole blood gives approximately 10 – 15 % LOWER TYPE 1 DM TYPE 2 DM
glucose levels than serum or plasma Pathogenesis
To convert whole blood glucose into serum or plasma
level, multiply value by 1.15 Incidence rate 5-10% 90-95%
A serum specimen is appropriate for glucose analysis if Onset Any; most Any; most
serum is separated from the cells within 30 – 60 minutes common to common with
Glucose is metabolized at room temperature at a rate of childhood/teens advancing age,
____________________ race/ethnicity,
At 4°C, glucose decreases by approximately hypertension,
____________________ dyslipidemia,
10% contamination with 5% dextrose will increase polycystic
glucose by 500mg/dL or more ovarian
CSF glucose concentration is approximately syndrome
______________________ that of plasma concentration Risk Factors Genetic, auto- Genetic, obesity,
Blood glucose should be obtained 1 – 2 hours before the immune sedentary
spinal tap lifestyle,
CSF for glucose analysis should be performed polycystic
immediately. If delay in measurement is unavoidable, the ovarian
sample must be centrifuged and stored at 4°C or at -20°C syndrome,
dyslipidemia and
CLINICAL SIGNIFICANCE OF GLUCOSE RESULTS hypertension
HYPOGLYCEMIA C-peptide levels
Glycemic factors such as glucagon are released when
Pre-diabetes
glucose levels reach ___________________________
Observable signs and symptoms of hypoglycemia appear
Symptomatology Symptoms Symptoms
when glucose levels reach ________________________
develop abruptly develop
Critical value for glucose is _________________;
gradually (some
excessively low glucose values can cause severe CNS
patients are
dysfunction especially if blood glucose value drops to 20
asymptomatic)
– 30 mg/dL
Ketosis
Whipple’s Triad: low blood glucose concentration, typical
symptoms and symptoms alleviated by glucose
Medication Insulin absolute Oral agents
administration
HYPERGLYCEMIA
GESTATIONAL DIABETES MELLITUS
Laboratory Finidngs in Hyperglycemia
A disorder characterized by impaired ability to
1. Increase glucose in plasma and urine
metabolize carbohydrate usually caused by a deficiency
2. Increase in urine specific gravity
3. Ketones in serum and urine of insulin, metabolic or hormonal changes
4. Decreased blood and urine pH (acidosis) It occurs during pregnancy and disappears after delivery
5. Electrolyte imbalance (decrease Na+ and HCO3+, Screening should be performed between 24-28 weeks of
increase K+) gestation
DIABETES MELLITUS (DM) Screening and diagnostic test: 2-hour OGTT using 75g
glucose load
Group of metabolic disorders characterized by
hyperglycemia resulting from defects in insulin secretion, Infants born to diabetic mother are at increased risk for
insulin receptors or both respiratory distress syndrome, hypocalcemia and
hyperbilirubinemia
Fasting plasma glucose concentration ≥126 mg/dl on
more than one testing is diagnostic of hypoglycemia After giving birth, women with GDM should be evaluated
6-12 weeks postpartum
Glucosuria occurs when the plasma glucose levels exceed
________________________ with normal renal function GDM converts to DM within 10 years in 30-40% of cases
Severe DM, the ratio of β-hydroxybutyrate to Diagnostic Criteria for GDM
acetoacetate is 6:1 1. FBS - ≥92 mg/dL
2. 1-hour OGTT = ≥180 mg/dL
3. 2-hour OGTT = ≥153 mg/dL
COLLEGE OF MEDICAL LABORATORY SCIENCE | 5 | 34
Clinical Chemistry
GLUCOSE METHODOLOGIES Guidelines for OGTT
CHEMICAL METHODS o Patient is aked to consume a normal to high
carbohydrate intake (150g carbs per day) for 3
OXIDATION REDUCTION METHOD
days prior to the test
1. _____________________________ – reduction of
cupric to cuprous ions forming cuprous oxide in hot o Patient is asked to fast overnight and to avoid
alkaline solution excessive physical activity. Patient should fast at
Folin Wu Method least ____________ but not greater than 16 hrs
Nelson Somogyi Method o OGT testing should be performed on the
Neocuproine Method morning to prevent hormonal diurnal effect on
Benedict’s Method (Modified Folin Wu) – glucose.
uses citrate or tartrate as stabilizing agent o Patient should be _______________________.
2. ________________________________ - reduction of Patient should refrain from exercise, eating, or
yellow ferricyanide to colorless ferricyanide (inverse drinking (except water) and smoking
colorimetry) o FBS is measured before giving the glucose load;
CONDENSATION METHOD if the FBS is greater than 140, test should be
AKA Ortho-toluidine/Dubowski method terminated; if the FBS is <140 mg/dL, glucose
load should be given to the patient.
ENZYMATIC METHODS o Glucose load for an adult is ____ and the patient
should finish drinking it within ______________
o Patient should not vomit, if they vomit,
measures ___________________________; also
discontinue the test
measures glucose in CSF and urine; presence of bleach
o Blood Glucose is taken every 30 minutes for 2
can cause a false increase in glucose
hrs
Colorimetric (Saifer Gernstenfield) - enzymes used:
Intravenous Glucose Tolerance Test (IVGTT)
glucose oxidase, peroxidase
o Used for patients with GI disorders (eg.
Polarographic - measures the rate of oxygen
Malabsorption)
consumption which is proportional to glucose
o 0.5 g of glucose/kg body weight (given w/in 3
concentration using an oxygen-sensing electrode;
mins) is administered intravenously
enzymes used: glucose oxidase, catalase
o Second blood collection is 5 minutes after
infusion
Most specific glucose method; reference method; uses
2-HRS POSTPRANDIAL BLOOD SUGAR (2HPPBS)
__________________________________ which is the
measures how well the used in the diagnosis of GDM
most specific enzyme/reagent in glucose measurement;
FBS is measured initially, patient is then given glucose
not affected by ascorbic acid or uric acid
load (75g) and plasma glucose is determeined after 2 hrs
enzymes used: _________________________________
Normally, blood glucose levels should be back near the
________________
reference limits approximately 2 hrs post load
GLUCOSE DEHYDROGENASE
GLYCOSYLATED HEMOGLOBIN (HbA1c)
glucose is reduced to a chromophore that is measured
Reliable method in monitoring long-term glucose control
spectrophotometrically
Reflects average blood glucose level over the previous 2-
Mutarotase: shorten time necessary to reach equilibrium
4 months
enzymes used: glucose dehydrogenase and diaphorase
Specimen: __________________________
Methods: Electrophoresis, Immunoassay, HPLC, and
LABORATORY TESTS
Affinity Chromatography
For every _____________ change in HbA1c, 35 mg/dL is
Blood Glucose taken any time of the day and without any
added to plasma glucose
fasting
Table 5. Glucose Test Categories in mg/dL
Requested during insulin shock and hyperglycemic
NORMAL IMPAIRED/ DIAGNOSTIC
ketonic coma
HIGH RISK FOR DM
FBS
Measure of over-all glucose homeostasis
OGTT
Requirement: non-per orem (NPO) at least 8 hours
HbA1c (%)
before the test
Short term glucose control (3 – 6 weeks)
determines how well the body metabolizes glucose; used
in the diagnosis of GDM Monitoring DM individuals with Chronic Hemolytic
Anemia and Hb variants
COLLEGE OF MEDICAL LABORATORY SCIENCE | 6 | 34
Clinical Chemistry
VALUES TO REMEMBER o Catalyzes the esterification of cholesterol (HDL)
Fasting Plasma Glucose: resulting in the formation of lysolecithin and
Glycosylated Hgb: 4-6% (Henry’s); 4.5-8% (Bishop) cholesterol ester
Conversion Factor: ____________________________ (30%)
Critical Values: <40 mg/dL and >500 mg/dL Found in plasma, serum and rbcs
Free cholesterol and phospholipids are found on the
LIPIDS surface of lipoproteins
Are insoluble in blood and water but soluble in organic
solvents (chloroform and ether) TRIGLYCERIDE (TAG)
FORMS OF LIPIDS Contains 3 molecules of fatty acid and one molecule of
FATTY ACID glycerol by ester bonds; main storage lipid in man
Linear chains of carbon-hydrogen bonds that terminate Very hydrophobic and water insoluble – does not contain
with a carboxyl group charged or hydrophilic groups
Mostly found as constituents of phospholipids or Evaluates suspected atherosclerosis and measure’s the
triglycerides body’s ability to metabolize fat
Only a small amount is present in the plasma (free TAG and cholesterol are the most important lipids in the
unesterified form), most is bound to albumin management of coronary artery disease
Very important sources of energy Prior to venipuncture, ideally patients should undergo
Provide the substance for conversion to glucose fasting for ________________________
(gluconeogenesis)
LIPOPROTEINS
PHOSPHOLIPID Are large macromolecular complexes of lipids with
Most abundant lipid derived from phosphatidic acid specialized proteins known as apolipoproteins
Amphipathic: with polar hydrophilic (water-loving) head Main purpose: transport TAG and cholesterol to sites of
groups and nonpolar hydrophobic (water-fearing) fatty energy storage and utilization
acid side chains Apolipoprotein: helps keep the lipids in solution during
Similar in structure in triglycerides, except they contain circulation through the blood stream; contain a
two fatty acids structural motif called an “amphiphatic helix”
PHOSPHOLIPIDS IN THE BODY MAJOR LIPOPROTEINS
Phosphatidylcholine (70 – 75%) 1.
Sphingomyelin (18 – 20%) Largest and lightest among the lipoproteins;
Phosphatidylserine, Phosphatidylethanolamine (3 – lipoprotein with LDL
6%) 80-95% TAG by weight
Transports _________________________
Lysophosphatidylcholine (4 – 9%)
Causes non-fasting lipemia
No charge; remains in the origin during
CHOLESTEROL electrophoresis
Found on the surface of lipid layers and synthesized in 2.
the liver Pre-beta Lipoprotein
Transports __________________________
Precursor of 5 major classes of steroids: progestins,
3.
glucocorticoids, mineralocortocoids, androgens and
AKA as the bad cholesterol; beta lipoprotein
estrogens
Transports cholesterol from
Evaluates the risk for atherosclerosis, myocardial and __________________________________________
coronary artery occlusions Transport majority (75%) of the cholesterol
Direct relationship between elevated serum cholesterol Directly proportional to the risk of atherosclerosis
and myocardial infarction and coronary heart disease (CHD); higher LDL means
FORMS OF CHOLESTEROL higher risk
_________________________________ (70%) 4.
Found in plasma and serum; cholesterol bound in Smallest and heaviest among the lipoproteins
Fastest towards the anode; alpha lipoprotein; good
fatty acid
cholesterol
Neutral lipid: located at center of lipid drops
Inversely proportional to the risk of atherosclerosis
Undergoes esterification by lcat
and CHD; lower HDL means higher risk
Lecithin-Cholesterol Acyl Transferase (LCAT) Responsible for reverse cholesterol transport;
transports cholesterol ________________________
COLLEGE OF MEDICAL LABORATORY SCIENCE | 7 | 34
Clinical Chemistry
MINOR LIPOPROTEINS ENZYMATIC METHODS
1. Most common method of quantifying the cholesterol
Product of VLDL catabolism – VLDL remnant; oxidase reaction is to measure the amount of hydrogen
“subclass of LDL” peroxide produced
Major apolipoprotein: 1. Cholesterol Oxidase Method (Spectrophotometric)
Density: 1.006-1.019 kg/L = floats on the 1.063 Enzymes used: Cholesterol esterase, Cholesterol
density potassium bromide solution oxidase, Peroxidase
2. TRIGYLCERIDE
Known as ________________________________
due to electrophoretic mobility same as VLDL but CHEMICAL METHODS
density like LDL 1.
LDL-like particles that have a molecule of Apo (a) Uses chromotrophic acid
linked to Apo B-100 by a disulfide bond End product: Blue colored compound
Independent risk factor for atherosclerosis __________________________________________
Density: 1.045-1.080 kg/L (CDC Reference method)
o alkaline hydrolysis (saponification) using
ABNORMAL LIPOPROTEINS alcoholic KOH, solvent extraction with
1. chloroform and the extract is treated with silicic
Abnormal lipoprotein found in obstructive jaundice acid (chromatography) to isolate TAG and a
and LCAT deficiency color reaction with chromotropic acid giving rise
A specific and sensitive indicator of cholestasis to a pink end color
Lipid content is mostly phospholipid and free 2.
cholesterol (90%); contains ApoC and albumin Uses diacetyl acetone and ammonia
2. End product: Diacetyl lutidine compound
Known as “___________________________ – ENZYMATIC METHODS
density of VLDL during ltracentrifugation but Specific, Rapid, and easy to use
migrates with LDL in the β-region during Major Interference: Endogenous Glycerol
electrophoresis
Glycerol Kinase
Found in type 3 hyperlipoproteinemia or
Reaction A - lipase, glycerol kinase, pyruvate kinase
dysbetalipoproteinemia
and LDH
Also known as VLDL rich in cholesterol due to
Reaction B - lipase, glycerol kinase, glycerol PO 4
defective catabolism of VLDL
dehydrogenase, diaphorase
METHODOLOGIES LIPOPROTEIN
CHOLESTEROL 1. Ultracentrifugation
CHEMICAL METHODS Reference method for quantification of lipoproteins
Based on protein and triglyceride contents of
PRINCIPLE: Dehydration and oxidation of cholesterol to
lipoproteins
form a colored compound
Expressed on svedverg units
1.
________________________ – end product: Reagent: potassium bromide solution (1.063)
Cholestadienyl monosulfonic acid (green end color) 2. Electrophoresis
2. ________________________ - end product: Electrophoretic pattern (from origin): Chylomicrons,
cholestadienly disulfonic acid (red end color) LDL, VLDL, HDL
Color Developer Mixture (Liebermann Burchardt Preferred supporting medium: agarose gel
reagent) Lipid staining dyes: Oil red O, Fat red 7B, Sudan Black
Glacial acetic acid B
Acetic Anhydride 3. Chemical Precipitation
Concentrated H2SO4 a. HDL
Table 6. General Methods o Uses dextran sulfate (synthetic heparin) with
METHOD STEPS OTHER NAME magnesium (precipitants)
Pearson, Stern o CDC reference method: ultracentrifugation,
One-step Colorimetry
and MacGavack heparin manganese precipitation and Abell-
Two-step Extraction + Colorimetry Bloors Kendall assay
Saponification + o Homogeneous assays are the most popular
Three-step Abell-Kendall method for measuring HDL-C
Extraction + Colorimetry
Saponification + b. LDL
Schoenheimer i. β-quantification
Four-step Extraction + Colorimetry
Sperry o EDTA plasma is the preferred sample
+ Precipitation
COLLEGE OF MEDICAL LABORATORY SCIENCE | 8 | 34
Clinical Chemistry
o Plasma is centrifuged for at least 18 IIb (Familial Combined High LDL & VLDL (High
hours; VLDL and CM accumulate as Hyperlipidemia) Cholesterol & TAG)
floating layer, leaving predominantly LDL III (Familial Presence of β-VLDL, High
and HDL in solution Dysbetalipoproteinemia) Cholesterol & TAG)
ii. Homogeneous Direct LDL-C method IV (Familial Hight VLDL (High TAG)
o First reagent: selectively removes non- Hypertriglyceridemia)
LDL lipoproteins High VLDL and Presence of
o Second reagent: releases cholesterol V CM (High Cholesterol and
from LDL so that it can be measured TAG)
enzymatically LIPID STORAGE DISEASES
4. Chromatographic methods
Table 8. Lipid Storage Diseases
Uses either Gel Chromatography or Affinity
Chromatography Lipid Storage Disease Enzyme Deficient
5. Immunochemical methods Fabry’s disease Alpha galactosidase
Uses antibodies specific to epitopes on the GM-1 Gangliosidosis Beta galactosidase
apolipoproteins Gaucher Beta glucosidase
6. Immunoassay or Immunonephelometry Krabbe Cerebroside beta galactosidase
Based on the measurement of the turbidity created Niemann Pick Sphingomyelinase
by apolipoprotein-antibody complexes
Metachromatic Arylsulfatase A
Lp(a) is measured by immunoturbidimetric assay
leukodystrophy
Sandhoff Total Hexosamindase (A & B)
CLINICAL SIGNIFICANCE
Tay Sach Hexosaminidase
ARTERIOSCLEROSIS VS ATHEROSCLEROSIS
VALUES TO REMEMBER
Arteriosclerosis – general term for the thickening and ATP III CLASSIFICATION FOR LDL, TOTAL & HDL
hardening of arteries CHOLESTEROL & TAG VALUES
Atherosclerosis – Type of arteriosclerosis; Hardening of
Table 9. LDL CHOLESTEROL
the arteries caused by plaques (made up ofCholesterol,
< 100 mg/dL Optimal
Fatty substances, Cellular Waste products, Calcium and
100 – 129 mg/dL Near Optimal/Above Optimal
Fibrin) that build up inside the arteries
130 – 159 mg/dL Borderline High
CORONARY HEART DISEASE (CHD)
160 – 189 mg/dL High
Broad spectrum of Heart disease resulting from Imparied ≥ 190 mg/dL Very High
coronary blood flow
Table 10. HDL CHOLESTEROL
Clinical (Non-Laboratory) Risk factors for CHD < 40 mg/dL Low
Cigarette Smoking
≥ 60 mg/dL High
Hypertension (BP >140/90 mmHg)
Table 11. TOTAL CHOLESTEROL
Family history of premature CHD
< 200 mg/dL Desirable
Age (Men > 45 years; Women > 55 years)
200 – 239 mg/dL Borderline High
Obesity
≥ 240 mg/dL High
Diabetes Mellitus
Table 12. TRIGLYCERIDE
Sedentary lifestyle
< 150 mg/dL Normal
ANALPHALIPOPROTEINEMIA
150 – 199 mg/dL Borderline high
Aka Tangier Disease; HDL deficiency
200 – 499 mg.dL High
ABETALIPOPROTEINEMIA
≥ 500 mg/dL Very High
Aka Bassen-Kornzweig syndrome; Deficiency of apoB REFERENCE RANGES
(B48 and B100); notable acanthocytes in peripheral
Total Cholesterol – 140 – 200 mg/dL
blood smear
HDL Cholesterol – (M) 29 – 60 mg/dL; (F) 38 – 75 mg/dL
FREDRICKSON AND LEVY’S HYPERLIPOPROTEINEMIA
LDL Cholesterol – 57 – 130 mg/dL
PHENOTYPES
Triglycerides – 67 – 157 mg/dL
Table 7. Fredrickson Classification of
CONVERSION FACTORS
Hyperlipoproteinemia
TYPE LPP PATTERN Cholesterol (mg/dL to mmol/L) – _________________
I (Familial LPL deficiency) High CM (High TAG) Triglyceride (mg/dL to mmol/L) – _________________
IIa (Familial High LDL (High Cholesterol) FORMULA FOR LDL-C
Hypercholesterolemia) LDL-C = _______________________________________
COLLEGE OF MEDICAL LABORATORY SCIENCE | 9 | 34
Clinical Chemistry
Friedewald Method (Indirect)
VLDL (mmol/L) = ____________________________ most abundant protein in fetal serum
VLDL (mg/dL) = ____________________________ detectable in maternal blood up to the 7th or 8th month
De Long Method (Indirect) of pregnancy
VLDL (mmol/L) = ____________________________ increased (maternal blood):
VLDL (mg/dL) = ____________________________ ______________________________________________
tumor marker for _______________________________
PROTEINS α1 ACID GLYCOPROTEIN/OROSOMUCOID (AAG)
Are synthesized in the liver and secreted by the greatest affinity for progesterone
hepatocyte into the circulation except immunoglobulins useful diagnostic tool in neonates with bacterial
(plasma cells) infections
Amphoteric: can bear positive and negative charges α1 ANTI – CHYMOTRYPSIN
because of their acid and basic amino acid compositions binds and inactivates prostate specific antigen (PSA)
PLASMA PROTEINS major form of PSA found in human sera; associated with
FRACTION SPECIFIC PROTEINS
Alzheimer’s disease
Prealbumin Prealbumin
GROUP-SPECIFIC COMPONENT (Gc) GLOBULIN
Albumin Albumin
exhibits affinity with vitamin D and actin
α1-Globulin α1antitrypsin, α fetoprotein, α lipoprotein,
method: radial immunodiffusion
α1 acid glycoprotein, α1 antichymotrypsin,
ALPHA 2 – GLOBULIN
inter α-trypsin inhibitor, Gc globulin
α2-Globulin Ceruloplasmin, Haptoglobin, α2
macroglobulin largest major non-immunoglobulin in plasma
β-Globulin Transferrin, Hemopexin, β2 microglobulin, increases 10x in ______________________
Complement, Fibrinogen, LDL, VLDL, CRP found principally in the intravascular spaces
γ-Globulin Immunoglobulin, CRP (In some books)
PREALBUMIN (TRANSTHYRETIN) copper-binding glycoprotein; imparts blue color to
protein
Transport protein for ____________________________
marker for Wilson’s disease: deposition of copper in skin,
Used to detect malnutrition
liver, brain and cornea (Kayser Fleisher rings)
Landmark to confirm that the specimen is really CSF
decreased: Wilson’s disease, Menkes’ kinky-hair
syndrome
Protein present in highest concentration in the plasma
General transport protein; maintains osmotic pressure binds free hemoglobin by its α chain
Sensitive and highly prognostic marker in cases of cystic prevents the loss of hemoglobin and its constituent iron
fibrosis into the urine
“_____________________________________” BETA - GLOBULIN
Normal life span in circulation is 15 – 19 days
β2 - MICROGLOBULIN
High serum albumin levels are more often associated
light chain component of the major human leukocyte
with dehydration or prolonged tourniquet application or
antigen (HLA)
specimen evaporation
found on surface of most nucleated cells; needed in the
Low serum albumin levels can be related to:
production of CD8 cells
Inflammation, Hepatic disease, Urinary loss,
Gastrointestinal loss, Protein-Calorie malnutrition,
Burn injury, Edema, and Ascites Major Component of the β2 globulin fraction
TERMS: transports iron to its storage sites
Analbuminemia – absence of albumin increased: hemochromatosis (bronze-skin) and IDA
Bisalbuminemia – presence of 2 bands in the COMPLEMENT
albumin region one of the natural defense mechanisms that protects the
Hypoalbuminemia – decreased levels of albumin human body from infection
ΑLPHA 1 - GLOBULIN Complement C3: most abundant form in serum
binds heme released by degradation of hemoglobin;
Major inhibitor of protease activity
helps in diagnosis of early hemolysis
Deficiency: emphysematous pulmonary disease and
juvenile hepatic cirrhosis
COLLEGE OF MEDICAL LABORATORY SCIENCE | 10 | 34
Clinical Chemistry
BETWEEN BETA AND GAMMA Can be used to determine if a certain body fluid is a
transudate or an exudate
FIBRINOGEN
No to lipemia and hemolysis
most abundant of all the coagulation factors
METHODOLOGIES
serve as long term marker for prognosis of cardiovascular
disease
GAMMA GLOBULIN reference method but not routinely used
based on the measurement of the nitrogen content of
IMMUNOGLOBULIN
protein (1g of nitrogen=6.54g of protein)
synthesized in the plasma cells
uses serum treated with tungstic acid to form a protein
IgG: most abundant in plasma and lymph
free filtrate
IgA: main antibody found in secretions
reagent: H2SO4
IgM: first antibody that appears in response to antigenic
end product: ammonia
stimulation
IgD: present mostly on the surface of B cells
IgE: antibody associated with allergic and anaphylactic most widely used method
reactions requires at least 2 peptide bonds and an alkaline medium
Reagents:
general scavenger molecule; binds to the C- ______________________________________________
polysaccharide of the pneumococcus Principle: Cupric ions complex the group involved in the
cardiac marker: early warning for persons at risk for peptide bond forming a violet-colored chelate which is
coronary artery disease proportional to the number of peptide bonds present
inflammatory marker: reflect severity of CHD and reflects the total protein level at 545nm.
FOLIN – CIOCALTEU (LOWRY)
rapid test for presumptive diagnosis of bacterial versus
viral infection has the highest analytical sensitivity
MISCELLANEOUS PROTEINS Principle: Oxidation of phenolic compounds such as
tyrosine, tryptophan, and histidine to give a deep blue
small heme protein found in skeletal and cardiac muscles color
that transports and stores oxygen from hemoglobin to Main reagent: Phosphotungstic molybdic acid or phenol
intracellular respiratory enzymes of contractile cells reagent
higher affinity for oxygen than does hemoglobin Color enhancer: Biuret reagent
marker for chest pain (angina) and early detection of ULTRAVIOLET ABSORPTION
acute myorcardial infarction (AMI) Principle: The absorbance of proteins at 210nm due to
Rises at 1 – 3 hrs; Peaks at 5 – 12 hrs; Returns to normal the absorbance of peptide bonds at that specific
in 18 – 30 hrs wavelength
TROPONINS All proteins have absorbance at 210 except tryptophan,
are regulators of actin and myosin tyrosine and phenylalanine (280nm)
most important marker for cardiac injury REFRACTOMETRY
alternative test to chemical analysis of serum proteins
useful for assessment of early and late AMI SALT FRACTIONATION
sensitive marker for the diagnosis of unstable angina
Globulins can be separated from albumin by salting-out
Rises within 3 – 4 hrs; Peak in 10 – 24 hrs; Remains
procedures using sodium salts
elevated for up to 10 – 14 days
Reagent: sodium sulfate salts
Table 13. Solubility Property of Proteins
only found in myocardium, greater cardiac specificity
than TnT; highly specific for AMI PROTEIN SOLUBLE INSOLUBLE
Rises within 3 – 6 hrs; Peak in 14 – 20 hrs; Returns to Albumin Water Saturated Salt Soln
normal in 5 – 10 days Conc. Salt Soln Highly conc salt soln
Hydrocarbon solvents
Globulin Weak Salt Soln Water
A cardiac marker; diagnostic for congestive heart failure
Hydrocarbon solvents Saturated Salt soln
SPECIMEN CONSIDERATIONS AND PATIENT PREP Conc salt soln
Serum is preferred; 24-hr urine and serous fluids can also
be used
Protein in CSF is ________________________ compared
to Plasma Protein
COLLEGE OF MEDICAL LABORATORY SCIENCE | 11 | 34
Clinical Chemistry
SERUM PROTEIN ELECTROPHORESIS when the substrate concentration reaches a
maximal value, higher concentration of substrate no
The single most significant clinical application of SPE is
longer result in increased rate of reaction
for the identification of monoclonal spike of
3. Cofactors
immunoglobulins and differentiating them from
nonprotein entities that bind to enzymes before a
polyclonal hypergammaglobulinemia
reaction occurs
“blip” in the late α2 or early β zone region: free
Coenzymes – is an organic compound, which when
hemoglobin
increased in concentration, will result to an increase
small spikes in the β region: iron deficiency anemia
in velocity of the reaction
(transferrin)
Activators – organic ions that alter the spatial
polyclonal gammopathy: rheumatoid arthritis and
configuration of the enzyme for proper substrate
malignancy
binding
ABNORMAL SPE PATTERNS
Metalloenzymes – an organic ion attached to a
1. Gamma Spike – ___________________________ molecule
2. β-γ bridging – ___________________________
4. Inhibitors
3. α2 globulin spike – ___________________________
4. α1 globulin flat curve – ___________________________
o Physically binds to the active site of an enzyme
5. α1, α2 and β globulin spikes - ______________________
and competes with the substrate for that active
site
o The effect of the inhibitor can be counteracted
by adding excess substrate to bind the enzyme
o does not compete with the substrate but look
for areas other than the active site (allosteric
site)
o increasing substrate concentration does not
Abnormal SPE Patterns
reverse the inhibition
DYES
1. ___________________________ – most sensitive, o binds to the enzyme substrate complex
specific, and precise among the dye-binding assays o increasing substrate concentration results to
2. ___________________________ – most commonly increased inhibition
used, measure absorbance 5. Isoenzymes - have the same catalytic reactions but
3. Tetrabromphenol blue – used in urine reagent strip, slightly different molecular structures
sensitive to albumin 6. Temperature
4. Ninhydrin – for amino acids enzymes are active at 25°C, 30°C or 37°C
5. Methyl orange
37°C = optimum temperature
6. Hydroxybenzeneazobenzoic acid (HABA)
45-50°C = enzyme start to denature
7. Coomassie Brilliant Blue
60-65°C = inactivation of enzymes
8. Pyrogallol Red – used for analysis of fluids with lower
protein concentrations such as urine and CSF 7. pH - most physiologic reactions occur in the pH range of
7 to 8.
VALUES TO REMEMBER
8. Storage - low temperatures (refrigeration/freezing)
Reference Range:
render enzymes visibly inactive
Total Protein: 6.5 – 8.3 g/dL
2° to 8°C = ideal storage temperature for substrates
Albumin: 3.5 – 5.5 g/dL
and coenzymes
Globulin = Total Protein – Albumin
-20°C = preservation for longer periods of time
Conversion Factor: g/dL to g/L = 10
room temperature = ideal storage for LDH (LD4 and
LD5)
ENZYMES 9. Hemolysis - most increases enzyme concentration
FACTORS AFFECTING ENZYMATIC REACTIONS 10. Lactescence or Milky serum - decreases enzyme
1. Enzyme Concentration concentration
The higher the enzyme concentration, the faster is ENZYME NOMENCLATURE
the reaction 1st digit = classification
2. Substrate concentration 2nd and 3rd digits = subclass
with the amount of enzyme exceeding the amount 4th and 5th digits = serial number
of substrate, the reaction rate steadily increases as
more substrate is added
COLLEGE OF MEDICAL LABORATORY SCIENCE | 12 | 34
Clinical Chemistry
Table 14. Classification of Enzymes
CLASS FUNCTION EXAMPLE ENZYMATIC REACTION
Oxidoreductases Catalyze the LDH, MDH, 1. _____________________________ – reaction rate
(-dehydrogenase) removal or addition ICD, G6PD depends only on enzyme concentration
of electrons 2. _____________________________ – reaction rate is
Transferases Catalyze the CK, AST, ALT, directly proportional to substrate concentration
(-transferase, transfer of chemical OCT GENERAL METHODS TO MEASURE ENZYMATIC
-kinase) group other than REACTIONS
hydrogen from one 1. Fixed time/endpoint – reaction proceeds for a
substrate to another designated time, the reaction is stopped and a
Hydrolases Catalyze hydrolysis Esterases – measurement is made.
or splitting of a bond ACP, ALP, CHS, 2. Continuous Monitoring/ kinetic assay – multiple
LPS measurements are made during the reaction; preferred
by the addition of
Peptidases –
water (hydrolytic than fixed-time
Trypsin,
reactions) pepsin, LAP ALKALINE PHOSPHATASE (ALP)
Glycosidase – CHARACTERISTICS
AMS, Catalyzes hydrolysis of phosphomonoesters (or organic
galactosidases phosphate esters) into alcohol and phosphate at an
Lyase Catalyze removal of Glulatamate alkaline pH (9.0 – 10.0)
(-decarboxylase) groups from decarboxylase, Requires activator zinc
substrates without pyruvate ISOENZYMES
hydrolysis decarboxylase,
tryptophan Normal Isoenzymes: Intestinal, Placental, Bone, and Liver
decarboxylase, Liver and Bone ALP are the most predominant fractions
aldolase Can be differentiated using electrophoresis, heat
Isomerase Catalyze the Glucose denaturation, and chemical inhibition
intramolecular phosphate Carcinoplacental isoenzymes include Regan, Nagao, and
arrangement of the isomerase, Kasahara. They are usually found in patients with
substrate ribose malignancy and their characteristics resemble that of
compound phosphate placental ALP
isomerase ELECTROPHORESIS
Ligase Catalyze the joining Synthase Origin towards anode:
of two substrate
molecules, coupled Liver and bone fractions are difficult to resolve during
with breaking of the electrophoresis
pyrophosphate To improve separation of bone and liver forms, use
bond in ATP or neuraminidase & wheat germ lectin
similar compounds HEAT DENATURATION
GENERAL PROPERTIES OF ENZYMES
Most Heat Stable to Most Heat Labile
1. Active site - is a water-free activity, where the substrate
interacts with particular charged amino acid residues
Heat stability is determined by heating serum at 56C for
2. Allosteric site - is a cavity other than the active site
10 – 15 minutes
When bound tightly to the enzyme, the coenzyme is
___________________________ – most heat stable of
called a prosthetic groups
all the normal ALP isoenzymes
Apoenzyme (enzyme portion) and coenzyme forms
Regan ALP – most heat stable among all the types of ALP
a complete and active system known as holoenzyme
CHEMICAL INHIBITION
(apoenzyme + prosthetic group = holoenzyme)
Digestive enzyme in its inactive form originally Placental and intestinal ALPs are inhibited by
secreted from the organ of production is called a phenylalanine reagent and 3M urea inhibits bone ALP
proenzyme or zymogen Levamisole inhibits both liver and bone ALP
ENZYME THEORY
1. Emil Fisher’s (Lock and Key Theory) – the shape of the
key (substrate) must fit into the lock (enzyme)
2. Kochland’s (Induced Fit Theory) – based on the substrate
binding to the active site of the enzyme
COLLEGE OF MEDICAL LABORATORY SCIENCE | 13 | 34
Clinical Chemistry
METHODOLOGIES Table 16. Summary of ACP Methods
METHODS SUBSTRATE END
Table 15. Summary of ALP Methods
PRODUCTS
METHODS SUBSTRATE END
Gutman & Phenyl PO4 Inorganic PO4
PRODUCTS
Gutman
Bodansky
Inorganic Shinowara PNPP p-nitrophenol
Shinowara β-
phosphate + Babson, Read, & α-naphthol α-naphthol
Jones glycerophosphate
glycerol Philips phosphate
Reinhart
Roy & Hillman Thymolphthalein Free
King &
Phenylphosphate Phenol MonoPO4 thymolphthalein
Armstrong
CLINICAL SIGNIFICANCE
Bessy, Lowry, P-nitrophenol or
& Brock Yellow Elevated in patients with prostatic CA, however it is not
Bowers & Nitrophenoxide specific since it can also be elevated in prostatic
PNPP
McComb Iron hyperplasia and prostatic surgery
Huggins & Phenolphthalein Phenolphthalein Prostatic ACP (PAP) is used together with prostate
Talalay disphosphate Red specific antigen (PSA) to monitor recurrence of prostatic
α-naphthol cancer
Moss α-naphthol
phosphate Useful in forensic clinical chemistry – especially in medico
Buffered legal evaluation of rape
Klein, Babson, Free
phenolphthalein ACP may also be elevated in bone diseases due to
& Read Phenolphthalein
phosphate osteoclastic activity, as well as in Gaucher disease
CLINICAL SIGNIFICANCE ASPARTATE AMINOTRANSFERASE (AST)
CHARACTERISTICS
Often used in evaluation of Hepatobilliary (obstructive
conditions) and Bone disorders (Osteoblast involvement) Aka __________________________________________
Highest elevation of ALP is seen in: Paget’s disease Involved in the transfer of an amino group between
(Osteitis deformans) aspartate and α-keto acids with the formation of
Increased in: Hyperparathyroidism, rickets & oxaloacetate and glutamate.
osteomalacia, fractures, and Malignant tumors 2 isoenzymes: cytoplasmic (predominant form in serum)
Cirrhosis and Hepatitis produce only slight elevations and mitochondrial
Biliary obstruction (Cholestasis) – 3 -10 times elevation Major tissue source: cardiac tissue, liver and skeletal
Physiologic elevation of ALP can be seen in growing muscle
children due to osteoblastic activity CLINICAL SIGNIFICANCE
ACID PHOSPHATASE (ACP) used in the evaluation of myocardial infarction,
CHARACTERISTICS hepatocellular disorders and skeletal muscle
catalyzes the same reaction made by ALP, except that it involvement
is active at pH 5.0 Often used in conjunction with ALT for hepatocellular
tissue sources: __________________ (major source), disorders
RBCs, platelets, liver and bone SPECIMEN CONSIDERATION
ISOENZYMES Hemolysis should be avoided because it can dramatically
Electrophoretic Separation increase serum AST concentration
____________________ remains in Origin METHODOLOGIES
___________________ migrates with great mobility _______________ – (pH 7.5) uses malate dehydrogenase
Chemical Inhibition (MD) and monitors the change in absorbance at 340nm
___________________ is inhibited by L-tartrate ALANINE AMINOTRANSFERASE (ALT)
___________________ is inhibited by 2% CHARACTERISTIC
formaldehyde and 1mM cupric sulfate solution
catalyzes the transfer of an amino group from alanine to
METHODOLOGIES
α-ketoglutarate with the formation of glutamate and
______________________________ = specific pyruvate
substrate; for endpoint reaction
Major tissue source: _____________________________
______________________________ = preferred for
continuous monitoring CLINICAL SIGNIFICANCE
If not assayed immediately, serum should be frozen to a
Highest elevation is found in
pH lower than 6.5. With acidification, ACP will be stable
______________________________________________
for 2 days
COLLEGE OF MEDICAL LABORATORY SCIENCE | 14 | 34
Clinical Chemistry
ALT is slightly increased in obstructive jaundice but METHODOLOGIES
markedly increased in necrotic jaundice
uses ________________________ as the substrate
METHODOLOGIES
Triolein (purer form of TAG) is also used as a substrate
Couple Enzymatic reaction: ALT + Lactate for LPS assay
dehydrogenase; pH 7.5, reading at 340nm Table 19. Methods for Lipase
Table 17. Differentiating AST and ALT Determination
AST ALT Methods Principle
Major Organ Cherry Reference method; substrate – 50% olive oil
Affected Crandal Hydrolysis of olive oil after incubation for 24
Substrate hours at 37°C and titration of fatty acids using
NaOH
End products Tietz &
Fiereck
Color developer 2,4 DNPH 2,4 DNPH Peroxidase Most commonly used; do not use 50% olive
Color intensifier 0.4 N NaOH 0.4 N NaOH Coupling oil
Methods Reitman & Reitman & Table 20. Acute Pancreatitis Markers
Frankel Frankel Onset of Peak Duration of
Marker
AMYLASE (AMS) Elevation Activity Elevation
CHARACTERISTICS Amylase 2 – 12 hrs 24 hrs 3 – 5 days
Lipase 6 hrs 24 hrs 7 days
catalyzes the breakdown of starch and glycogen
LACTATE DEHYDROGENASE
Isoenzymes: ___________________________________
CHARACTERISTIC
Major tissue source: _____________________________
______________________________________________ catalyzes the interconversion of lactic and pyruvic acid
CLINICAL SIGNIFICANCE enzyme virtually found in all cells of the body
uses NAD+ (nicotinamide dinucleotide) as coenzyme
____________________________________________
__________________ is the major isoenzyme
Three-fold amylase increase with normal 24 hours urine
LD-1 is relatively abundant in cardiac muscle; LD-5 is
amylase – repeat serum AMS after polyethylene glycol
more abundant in skeletal muscles
precipitation
__________________ - alcohol dehydrogenase enzyme;
METHODOLOGIES
responsible for the metabolic conversion of methanol
STARCH – Substrate for all methods and ethylene glycol
Table 18. Methods for AMS Determination Conc in Serum: LD-2 > LD-1 > LD-3 > LD-4 > LD-5
Method Principle Table 21. LDH Tissue Sources
Saccharogenic Classic Reference Method; Measures the Isoenzyme Chain Composition Tissue Sources
amount of reducing sugars produced by the LD1 & LD 2
hydrolysis of starch
Amyloclastic Measures AMS activity following the LD3
decrease in substrate concentration
Chromogenic Measures AMS activity by the increase in LD4 & LD5
color intensity of the soluble dye-substrate
solution CLINICAL SIGNIFICANCE
Couple- Measures AMS activity by continuous
highest serum levels: pernicious anemia and hemolytic
enzyme monitoring technique; Enzymes used: AMS,
disorders
Glucosidase, Hexokinase, G6PD
10-fold increase in hepatic carcinoma and toxic hepatitis
LIPASE (LPS)
LD-1 > LD-2 (“flipped pattern”) = seen in myocardial
CHARACTERISTIC
infarction and hemolytic anemia
hydrolyzes ester linkages of fats to produce alcohol and METHODOLOGIES
fatty acid
Method Principle
major tissue source: ____________________________
Most commonly used; pH 8.8;
CLINICAL SIGNIFICANCE
absorbance measured at 340 nm
____________________________________ – secreted
exclusively in the pancreas Preferred method;
rises more slowly compared to amylase
COLLEGE OF MEDICAL LABORATORY SCIENCE | 15 | 34
Clinical Chemistry
Table 22. Methods for LDH Determination increased: skeletal muscle disease, leukemia, hemolytic
CREATINE KINASE (CK) anemia and hepatic cancer
CHARACTERISTIC Highest level in progressive muscular dystrophy
catalyzes the transfer of a phosphate group between OTHER CLINICALLY SIGNIFICANT ENZYMES
creatine phosphate and adenosine diphosphate 5’ NUCLEOTIDASE (5’N)
found in high concentrations only in muscle and brain marker for hepatobiliary disease and infiltrative lesions
major tissue sources: brain, smooth and skeletal muscle in the liver
and cardiac muscle
___________ – (BB) most anodal and labile isoenzyme;
catalyzes the transfer of glutamyl groups between
most dominant isoenzyme found in the brain, intestine
peptides or amino acids through linkage at a gamma
and smooth muscle
carboxyl group
_________ (20%) – (MB) present only in the myocardium
useful in differentiating the increase in ALP
_________ – (MM) least anodal; major isoenzyme (94-
elevated in _________________________________ –
100%)
______________________________
CLINICAL SIGNIFICANCE
sensitive indicator of _________________ – most
a very sensitive indicator of acute myocardial infarction sensitive marker of ____________________________
(AMI) and Duchenne disorder PSEUDOCHOLINESTERASE (PCHE)
highest elevation of total CK is seen in Duchenne’s
marker for insecticide/pesticide poisoning
muscular dystrophy (50x)
(organophosphate poisoning) – low serum PchE
Table 23. Acute Myocardial Infarction
monitor the effect of muscle relaxants (succinylcholine)
Markers
after surgery
Marker Onset of Peak Duration of
ANGIOTENSIN-CONVERTING ENZYME (ACE)
Elevation activity elevation
Myoglobin 1 – 3 hrs 5 -12 hrs 18 – 30 hrs also known as peptidyldipeptidase A or kininase II
Troponin T 3 -4 hrs 10 – 24 hrs 10 - 14 days possible indicator of neuronal dysfunction (Alzheimer’s
Troponin I 3 – 6 hrs 12 – 18 hrs 5 – 10 days disease – CSF)
CK – MB 4 – 6 hrs 12 – 24 hrs 48 – 72 hrs for the diagnosis and monitoring of sarcoidosis
AST 6 – 8 hrs 24 hrs 5 days CERULOPLASMIN
LDH 12 – 24 hrs 48 – 72 hrs 10 – 14 days marker for Wilson’s disease (hepatolenticular disease)
METHODOLOGIES ORNITHINE CARBAMOYL TRANSFERASE (OCT)
Adenylate kinase released after red cell lysis interferes marker for hepatobiliary disease
with CK assay particularly with hemolysis
Cleland’s reagent and glutathione – partially restore lost NON-PROTEIN NITROGENS
activity of CK UREA
Table 24. Methods for CK Determination CHARACTERISTICS
Methods Principle
major end product of protein catabolism
pH 9.0; 340 nm
Enzymes used: CK, pyruvate kinase, constitutes to 45% of the total NPN
lactate dehydrogenase synthesized in the liver via the Kreb’s Henseleit cycle
first metabolite to elevate in kidney disease
Blood Urea Nitrogen (BUN) – pertains to the nitrogen
Most commonly used; pH 6.8; 340 nm
Enzymes used: CK, hexokinase, G-6-PD content only of urea. This value is often obtained using
indirect methods
Urea Concentration – concentration of urea as a whole
molecule, not just the nitrogen portion. This value is
ALDOLASE
often obtained using the direct methods.
CHARACTERISTIC
METHODOLOGIES
splits fructose-1,6-diphosphate aldolase into 2 triose
DIRECT METHOD
phosphate molecules in the metabolism of glucose
1.
ISOENZYMES
Aka Fearon reaction
Aldolase A – Skeletal Muscle
Inexpensive, Lacks specificity
Aldolase B – WBC, Liver, Kidney
End product: Yellow Diazine Derivative
Aldolase C – Brain tissue
2. O-phthaldehyde
CLINICAL SIGNIFICANCE
End product: Colored product
COLLEGE OF MEDICAL LABORATORY SCIENCE | 16 | 34
Clinical Chemistry
INDIRECT METHOD Normal BUN to Creatinine Ration = _________________
Measures urea by converting it first into ammonium ions METHODOLOGIES
using urease; ammonium ions formed from urea are then
CHEMICAL (DIRECT JAFFE)
measured
1.
Initial Reaction: Urease (derived from jack bean meal) Sensitive but non-specific method
converts urea to ammonium ions and carbonate ions 2. Lloyd or Fuller’s Earth Method
Secondary Reactions: Quantifies ammonium ions that Adsorbent:
form after the initial reaction o ________________ – sodium aluminum silicate
o ________________ – aluminum magnesium
o Reagents: KI, HgI silicate
o Products measured: Yellow-orange colloid
(Ammonium dimercuric iodide) Principle: Serum is mixed with alkaline picrate solution
and the rate of change in absorbance is measured
o Reagents: NaOCl, phenol, sodium nitroprusside between 2 points
o NaOCl chlorinates ammonia into Jaffe Reagent: Satd picric acid & 10% NaOH
monochloramine; monochloramine reacts with
popular, inexpensive, rapid and easy to perform
phenol to form indophenol (blue or green)
ENZYMATIC METHOD
o Reaction is maintained at alkaline pH (>10.0)
1. Creatinine aminohydrolase – CK
with sodium nitroprusside acting as catalyst
enzymes used: creatinine aminohydrolase,
o Product measured: indophenol at 630 – 660 nm
creatinine kinase, pyruvate kinase and lactate
dehydrogenase
o Ammonia + 2-oxoglutarate + NADH + GLDH ->
2. Creatinase – Hydrogen peroxide method
NAD + Glutamate + Water potential to replace Jaffe method (specific than Jaffe
o Measurement of decrease in absorbance at 340 method)
nm enzymes: Creatininase (creatinine aminohydrolase),
creatinase, sarcosine oxidase, peroxidase
o Conversion of unionized urea into ammonium CLINICAL SIGNIFICANCE
and bicarbonate ion; measure increase in
conductivity rate AZOTEMIA
1. Pre-Renal
diminished glomerular filtration with normal renal
o Color change; used in dry reagent strips
function
CLINICAL SIGNIFICANCE
cause: dehydration, shock, congestive heart failure
DECREASED BUN LEVELS 2. Renal
Decreased protein intake damaged within the kidneys
Liver disease acute/chronic renal disease, glomerulonephritis
Vomiting and Diarrhea 3. Post-Renal
Pregnancy usually the result of urinary tract obstruction
UREMIA VS AZOTEMIA VALUES TO REMEMBER
___________________________ – refers to increase Reference Value: M = 0.6 – 1.2 mg/dL; F = 0.5 – 1.1 mg/dL
NPNs, particularly urea in blood Conversion factor: (mg/dL to mmol/L) =
___________________________ – increase in NPNs in URIC ACID
blood; defined as increase in NPNs with symptoms of CHARACTERISTIC
organ involvement such as renal failure
major end product of purine catabolism
VALUES TO REMEMBER
final breakdown of nucleic acid catabolism in humans
Reference Value: 7 – 18 mg/dL formed from xanthine by the action of xanthine oxidase
Conversion Factor: mg/dL to mmol/L = ____________ in the liver and intestine
Urea Concentration: BUN x ______________ filtered by the glomerulus but 40% of uric acid is
CREATININE reabsorbed in the kidneys
CHARACTERISTIC METHODOLOGIES
end product of muscle catabolism CHEMICAL (CARAWAY/HENRY METHOD)
not affected by protein diet; not easily removed by Reagent: Phosphotungstic acid (PTA)
dialysis Reaction: Uric Acid + PTA -> Tungsten blue + Allantoin
__________________________________; used to
evaluate fetal lung maturity
COLLEGE OF MEDICAL LABORATORY SCIENCE | 17 | 34
Clinical Chemistry
Sodium Cyanide is used to increase color and inhibit Right lobe is 6x larger than the left lobe
fading 1.2 – 1.5 kg in weight
Sodium carbonate may be used instead Smallest functional unit of the liver is known as the
ENZYMATIC hepatic lobule
_____________________ is the enzyme used Blood is supplied from two sources: hepatic artery and
Principle: ______________________________________ portal vein
______________________________________________ FUNCTIONS OF THE LIVER
Uric acid has a UV absorbance peak at 293 nm Table 25. Functions of the Liver
CLINICAL SIGNIFICANCE Function
HYPERURICEMIA Synthesis Plasma proteins, carbohydrates, lipid,
Gout – associated with pain and inflammation of the lipoproteins, clotting factors, ketone
joints; (+) birefringent crystals in the synovial fluid bodies, enzymes
Increased nuclear metabolism – seen in leukemia, Conjugation Bilirubin
lymphoma, multiple myeloma or polycythemia, Detoxification Toxic substances absorbed in the
hemolytic and megaloblastic anemias and Drug intestine and by-products of metabolism
Chronic renal disease – due to decreased GFR and metabolism
tubular secretion Excretion and Bile acids or salts, bile pigments,
______________________ – deficiency in hypoxanthine Secretion cholesterol
guanine phosphoribosyl transferase (HGPT) Storage Fat and water soluble vitamins, glycogen
HYPOURICEMIA Table 26. Liver Function Tests
Liver disease, defective reabsorption of uric acid by Function Tests
kidneys (i.e. Fanconi Syndrome) Synthesis
VALUES TO REMEMBER
Conjugation
Reference Value: M = 3.5 – 7.2 mg/dL; F = 2.6 – 6.0 mg/dL
& Excretion
Conversion Factor: mg/dL to umol/L = ____________
Detoxification
AMMONIA
CHARACTERISTIC
BILIRUBIN
arises from the deamination of amino acids CHARACTERISTIC
preferred specimen: arterial blood
end product of hemoglobin metabolism and principal
METHODOLOGIES
pigment in bile
Digestion (Kjeldahl) method – nitrogen ion in a protein- also formed from destruction of heme-containing
free filtrate of the specimen is converted to ammonia proteins such as myoglobin, catalase and cytochrome
using hot concentrated H2SO4 in the presence of catalyst oxidase
Measurement of ammonia Table 27. Comparison between Conjugated
Nesslerization reaction – uses Gum Ghatti reagent and Unconjugated Bilirubin
Berthelot reaction – uses sodium nitroprusside Bilirubin 1 (B1) Bilirubin 2 (B2)
Glutamate dehydrogenase
CLINICAL SIGNIFICANCE
used in the diagnosis of hepatic failure (hepatic coma)
and Reye’s syndrome
elevated levels of ammonia are neurotoxic and are often
associated with encephalopathy
VALUES TO REMEMBER
Reference Range: 19 – 60 ug/dL
Conversion Factor: ug/dL to umol/L = _________
BILIRUBIN METABOLISM AND EXCRETION
1. When RBCs are destroyed in the spleen, hemoglobin is
LIVER FUNCTION TESTS
released
LIVER
2. Hemoglobin is broken down into heme and globin
ANATOMY OF THE LIVER
3. Globin is recycled while heme is divided into iron and the
Largest and the most versatile organ in the body protoporphyrin ring
Has two main lobes, separated from each other by 4. Iron is transported into the bone marrow to be used for
falciform ligament RBC sythesis
COLLEGE OF MEDICAL LABORATORY SCIENCE | 18 | 34
Clinical Chemistry
5. Protoporphyrin is broken down into biliverdin, and then Diazo Reagents
further broken down into bilirubin, specifically the Diazo A = 0.1% sulfanilic acid + HCl
unconjugated form Diazo B = 0.5% sodium nitrite
6. Unconjugated bilirubin (UB) is transported by albumin Diazo blank = 1.5% HCl
towards the site of conjugation, the liver
Principle: Diazo reaction is diazotization of bilirubin to
7. In the liver cells, UB is converted into Conjugated
produce azobilirubin
bilirubin (CB) through the action of the enzyme uridyl
Table 28. Main Bilirubin Methodologies
diphosphate glucoronyl transferase (UDPGT). The
process occurs in the smooth ER of the liver cells. Evelyn Malloy Jendrassik-Grof
8. Conjugated bilirubin goes out of the liver, down to the Accelerator
biliary tree (bile duct) and emptied into the intestine.
9. In the intestine, conjugated bilirubin is converted into pH
urobilinogen. Urobilinogen is a colorless substance Final
formed in the intestine reaction
10. Urobilinogen is converted into urobilin, an orange brown
Maximum
pigment responsible for the natural brown color of the
absorbance
stool. It is then excreted through the stool out of the
body. CLINICAL SIGNIFICANCE
11. Some of the urobilinogen from the intestine is
reabsorbed back into the blood, only to be excreted by conjugated bilirubin tightly bound to albumin; has longer
the kidneys into the urine.
half-life than other bilirubin
formed due to prolonged elevation of conjugated
bilirubin in biliary obstruction
helps in monitoring the decline of serum bilirubin
following surgical removal of gallstones
JAUNDICE
also called icterus or hyperbilirubinemia; characterized
by yellow discoloration of the skin, sclera and mucous
membranes
clinically evident when bilirubin levels exceeds 2mg/dl
Table 29. Classifications of Jaundice
Schematic summary of the pathway of bilirubin Urine Urine
(Bili, in brown circles) transport and metabolism Jaundice B1 B2
urobilinogen bilirubin
METHODOLOGIES Pre-Hepatic
Hemolysis will cause increase bilirubin while lipemia can (Hemolytic
cause decrease bilirubin Anemia)
Visible icterisia occurs when bilirubin is ______________ Hepatic
Bilirubin standard solution is usually made up of (Liver
unconjugated bilirubin diseases)
Conjugated bilirubin produces color in aqueous Post
solution. Hepatic
Unconjugated bilirubin produces color only after the (Bile duct
addition of alcohol obstruction)
Total bilirubin is measured 15 minutes after adding DERANGEMNTS IN BILIRUBIN METABOLISM
methanol or caffeine solution 1. _________________________ – Bilirubin transport
Caffeine-benzoate is preferred over methanol deficit
because the latter promotes protein precipitation characterized by impaired cellular uptake in
and increases turbidity bilirubin; elevated B1
_______________________ – most commonly used 2. _____________________________ – Conjugation deficit
method; more sensitive and not affected by hemoglobin infants are treated with phototherapy; elevated B1
_______________________
Sodium acetate = maintains alkalinity
o deficiency of the enzyme UDPGT resulting to
Sodium tartrate = provides alkalinity total absence of B2
Ascorbic acid = terminates initial reaction and o (+) kernicterus
destroys excess diazo reagent _______________________
o partial deficiency of UDPGT
o small amount of B2 is produced
COLLEGE OF MEDICAL LABORATORY SCIENCE | 19 | 34
Clinical Chemistry
3. _________________________________ – Bilirubin Diarrhea, Excess fluid loss
excretion deficit SIADH, Excess water intake
blockade of the excretion of bilirubin into the Adrenal insufficiency
canaliculi caused by hepatocyte membrane defect Reset osmostat
elevated B2 and total bilirubin
Acute or Chronic renal failure
4. __________________________ – Conjugation inhibition
Nephrotic syndrome, Hepatic cirrhosis, Congestive heart
familial form of unconjugated bilirubinemia caused
failure
by circulating inhibitor of bilirubin conjugation
Pseudohyponatremia (hyperglycemia, hyperlipidemia,
elevated B1
hyperproteinemia)
VALUES TO REMEMBER
VALUES TO REMEMBER
Total Bilirubin – Direct Bilirubin = Indirect Bilirubin
Reference Value: 135 – 145 mmol/L
Reference Values:
Threshold Critical Value
Total Bilirubin: 0.2 – 1.0 mg/dL
Hypernatremia: _________________
Direct Bilirubin: 0 – 0.2 mg/dL
Hyponatremia: ________________
Indirect Bilirubin: 0.2 – 0.8 mg/dL
Conversion Factor: mEq/L to mmol/L = __________
Conversion Factor: mg/dL to umol/L = ____________
POTASSIUM
Critical Value for Bilirubin: > 18 mg/dL
CHARACTERISTIC
otherwise known as “kalium”
ELECTROLYTES
SODIUM major intracellular cation – only 2% of the body’s total
CHARACTERISTIC potassium circulates in plasma
Functions: heart contraction, neuromuscular excitability,
also known as “natrium”
ICF volume regulation and hydrogen ion concentration
major extracellular anion hence the major contributor of
METHODOLOGIES
osmolality
principal osmotic pressure outside the cell; depends 1. Ion selective electrode (Valinomycin gel)
greatly on the intake of excretion of water 2. Flame emission photometry (Violet)
3. Atomic absorption spectrophotometry
HORMONES AFFECTING SODIUM LEVELS
4. Colorimetry (Lockhead & Purcell)
1.
CLINICAL SIGNIFICANCE
major electro-regulating hormone
promotes sodium retention and potassium CAUSES OF HYPERKALEMIA
excretion 1. Decreased Renal Excretion
2. Acute or Chronic Renal Failure
endogenous antihypertensive agent; promotes Hypoaldosteronism; Addison’s disease
natriuresis Diuretics
blocks aldosterone and renin secretion and inhibits 2. Increased Intake
the action of angiotensin II and vasopressin Oral or IV potassium replacement therapy
METHODOLOGIES 3. Cellular Shift
Acidosis, Muscle/Cellular injury
1. Ion selective electrode (Glass aluminum silicate) – most
Chemotherapy
commonly used method
Leukemia (Increased WBC)
2. Flame emission photometry (Yellow)
Hemolysis
3. Atomic absorption spectrophotometry
4. Increased Intake
4. Colorimetry (Albanese Lein)
Sample hemolysis, Thrombocytosis
CLINICAL SIGNIFICANCE
Prolonged tourniquet use or excessive fist clenching
CAUSES OF HYPERNATREMIA CAUSES OF HYPOKALEMIA
Diabetes Insipidus 1. GI Loss
Osmotic dieresis Vomiting, Diarrhea, Gastric suction, Intestinal
Loss of thirst tumor, Malabsorption
Insensible loss of water Cancer therapy
Gastrointestinal loss of hypotonic fluid Large doses of laxatives
Excess intake of sodium 2. Decreased Intake
CAUSES OF HYPONATREMIA 3. Renal Loss
Diuretics, Potassium depletion Diuretics – thiazides, mineralocorticoids
Aldosterone deficiency, Ketonuria Nephritis, Renal tubular acidosis,
Hyperaldosteronism; Cushing’s syndrome
Salt-losing nephropathy, Vomiting
COLLEGE OF MEDICAL LABORATORY SCIENCE | 20 | 34
Clinical Chemistry
Hypomagnesemia CALCIUM
Acute leukemia CHARACTERISITC
4. Cellular Shift
present almost exclusively in the plasma
Alkalosis, Insulin overdose
involved in blood coagulation, enzyme activity,
VALUES TO REMEMBER
excitability of skeletal and cardiac muscles and
Reference Value: 3.5 – 5.2 mmol/L maintenance of blood pressure
Threshold Critical Value 99% is part of the bones and 1% is in the blood and ECF
Hyperkalemia: _________________ FORMS OF CALCIUM
Hypokalemia: ________________ Ionized (active) calcium - 50%
Conversion Factor: mEq/L to mmol/L = _________ Protein-bound calcium - 40%
EFFECTS OF POTASSIUM TO CARDIAC MUSCLES Complexed with anions - 10%
8mmol/L – lack of muscle excitability FACTORS AFFECTING SERUM CALCIUM LEVELS
6-7mmol/L – may alter ECG
10mmol/L – fatal (cardiac arrest) increases intestinal reabsorption of calcium
3.0-3.4mmol/L – arrhythmia & paralysis increases reabsorption in the kidneys
CHLORIDE
CHARACTERISTIC activates the process of bone resorption
major extracellular anion – chief counterion of sodium stimulates the conversion of inactive vit. D to active
promotes maintenance of water balance and osmotic vit. D3
pressure in conjunction with sodium
only anion to serve as enzyme activator secreted by the parafollicular/C cells of the thyroid
Functions: maintains osmolality, blood volume and gland
electric neutrality hypocalcemic hormone – inhibits PTH and vit. D3
inhibits bone resorption
Responsible for Chloride shift – an exchange mechanism
between chloride and bicarbonate across the membrane METHODOLOGIES
of RBCs 1. Precipitation and Redox Titration
METHODOLOGIES
o end product: oxalic acid (violet color)
Interferences: bromide, cyanide, and cysteine
Mercurimetric Titration (Schales & Schales)
o end product: chloranilic acid (violet)
indicator: Diphenylcarbazone
2. Ortho-Cresolpthalein Complexone dyes
endproduct: Mercuric chloride (blue violet)
Dye: Arzeno III
Spectrophotometric method
3. EDTA titration method (Bachra, Dawer & Sobel)
Mercuric thiocyanate (Whitehorn titration) 4. Ion selective electrode (Liquid-membrane)
Ferric perchlorate 5. Flame emission photometry
Colorimetric amperometric titration – Cotlove CLINICAL SIGNIFICANCE
Chloridometer
HYPERCALCEMIA
____________________ – most commonly used method
Primary Hyperparathyroidism (Most Common PTH –
CLINICAL SIGNIFICANCE
mediated hypercalcemia)
HYPERCHLOREMIA Familial hypocalciuric hypercalcemia
Excess loss of bicarbonate Ectopic secretion of PTH by neoplasms
Renal tubular acidosis Malignancy associated (most common non PTH
Metabolic acidosis mediated hypercalcemia)
HYPOCHLOREMIA Vitamin D intoxication, Thyrotoxicosis
Prolonged vomiting, Diabetic ketoacidosis, Aldosterone Hypoadrenalism, Immobilization with increased bone
deficiency turnover, Milk-alkali syndrome, Sarcoidosis, Multiple
Salt-losing renal disease (eg Pyelonephritis) Myeloma
High serum bicarbonate (eg compensated respiratory HYPOCALCEMIA
acidosis or metabolic acidosis) Primary hypoparathyroidism
VALUES TO REMEMBER Severe hypomagnesemia
Longstanding hypercalcemia
Reference Values: 98 – 107 mmol/L
Pseudohypoparathyroidism
Conversion Factor: mEq/L to mmol/L = _________
Vitamin D deficiency, Chronic renal failure
Renal tubulopathies, Fanconi’s syndrome
COLLEGE OF MEDICAL LABORATORY SCIENCE | 21 | 34
Clinical Chemistry
Mutations of Vitamin D receptor MAGNESIUM
Hypoalbuminemia, Acute pancreatitis CHARACTERISTIC
Rhabdomyolysis intracellular cation second abundance to potassium; also
Tetany an enzyme activator
VALUES TO REMEMBER majority is stored in bones (53%)
Reference Values: life threatening symptoms occur if the serum levels
Total Calcium: 2.15 – 2.5 mmol/L reaches 5mmol/L
Ionized Calcium: 1.16 – 1.32 mmol/L FORMS OF MAGNESIUM
Conversion Factor: mg/dL to mmol/L = 2+
Free Mg /Ionized form – 55%
INORGANIC PHOSPHOROUS Protein-bound Mg2+ - 30%
CHARACTERISTIC Complexed with ions – 15%
______________________ related to calcium; maximally FACTORS AFFECTING MAGNESIUM LEVELS IN BLOOD
absorbed in the _________________________ __________________________________ - increases
organic phosphorous exists as: renal and intestinal reabsorption of magnesium
Organic phosphate – principal anion within cells __________________________________ - increases
Inorganic phosphate – part of the blood buffer renal excretion of magnesium
Only inorganic phosphate is measured in clinical METHODOLOGIES
laboratory Colorimetric methods
FORMS OF PHOSPHOROUS Calmagite
1. Free/Unbound form – 55% Formazen Dye
2. Complexes with ions – 35% Magnesium thymol blue
3. Protein-bound – 10% __________________________________ – reference
FACTOS AFFECTING PHOSPHATE CONCENTRATIONS method
1. PTH – decreases phosphate by renal excretion Dye Lake method – Titan yellow dye (Clayton/Thiazole
2. Calcitonin – inhibits bone resorption
yellow)
3. Growth hormone – increase phosphate renal
CLINICAL SIGNIFICANCE
reabsorption
METHODOLOGIES HYPERMAGNESEMIA
Acute or Chronic Renal Failure
most commonly used method to measure inorganic Hypothyroidism
phosphate Hypoaldosteronism
most common reducing agent: pictol Hypopituitarism
other reducing agents: elon, ascorbic acid and Antacids
senidine Enemas
endproduct: ammonium-molybdate complex Cathartics
CLINICAL SIGNIFICANCE Dehydration
Bone carcinoma/Bone metastasis
HYPERPHOSPHATEMIA
HYPOMAGNESEMIA
Renal Failure
Poor diet; Prolonged magnesium-deficient IV therapy,
Increased breakdown of cells (eg Intravascular
Chronic alcoholsim
hemolysis)
Pancreatitis, Vomiting, Diarrhea
Neoplastic disorders (eg Lymphoblastic leukemia)
Laxative abuse, Hyperparathyroidism,
Intensive exercise, Severe infections
Hyperaldosteronism, Hyperthyroidism
HYPOPHOSPHATEMIA
Hypercalcemia, Diabetic ketoacidosis
Infusion of dextrose solution
Diuretics, Excess lactation
Use of antacids
Pregnancy
Alcohol withdrawal
Tubular disorders, Glomerulonephritis, Pyelonephritis
Poor diet
Tetany
Vomiting
VALUES TO REMEMBER
Ketoacidosis
VALUES TO REMEMBER Reference Value: 0.63 – 1.0 mmol/L
Conversion factor: mEq/L to mmol/L = ____________
Reference Values: 0.87 – 1.45 mmol/L
Conversion Factor: mg/dL to mmol/L = _________
COLLEGE OF MEDICAL LABORATORY SCIENCE | 22 | 34
Clinical Chemistry
ANION GAP the pH decreases by 0.015/each Celsius above 37°C
is the difference between the unmeasured cations
(sodium and potassium) and unmeasured anions
Evaluate ventilation by lungs
(chloride and bicarbonate)
is an index or efficiency of gas exchange and not a
form of quality control for the analyzer used to measure
measure of CO2 concentration in the blood
these analytes
Increased: renal failure/uremia, ketoacidosis (starvation
or diabetes), poisoning by methanol, ethanol, ethylene Evaluate metabolic process
glycol or salicylate, lactic acidosis, hypernatremia and the kidneys regulate pH by excreting acid and
instrument error reabsorption of HCO 3 from the glomerular filtrate
Decreased: hypoalbuminemia, hypercalcemia,
hyperlipidemia and elevated myeloma proteins Evaluate degree of oxygenation
FORMULA: reflects the availability of the gas in blood but not its
AG = __________________________________ content
o RV: 8 – 16 mmol/L
Table 30. Levels of Hypoxemia
AG = __________________________________
pO2
o RV: 10 – 20 mmol/L
Mild 61 – 80 mmHg
Moderate 41 – 60 mmHg
ACID – BASE BALANCE, & VITAMINS Severe ≤ 40 mmHg
ORGANS ASSOCIATED WITH ACID-BASE
CLINIAL SIGNIFICANCE
BALANCE MAINTENANCE
RESPIRATORY ACIDOSIS
LUNGS
Help maintain acid-base balance through gas pH: Decreased; HCO3: Decreased
exchange or respiration Organ Defective: Lungs
Rapid or short term compensation Primary Cause: Hypoventilation
Analyte(s) controlled: O 2 & CO2 Organ to Compensate: Kidneys
KIDNEYS Primary Compensation: Bicarbonate Reabsorption
Help maintain acid-base balance through Example: ______________________________________
reabsorption or excretion of bicarbonate _____________________________________________
Slow but long term compensation RESPIRATORY ALKALOSIS
Analye controlled: Bicarbonate (HCO3-)
pH: Increased; HCO3: Increased
BLOOD BUFFERS
Organ Defective: Lungs
1. Bicarbonate and carbonic acid – major extracellular
Primary Cause: Hyperventilation
blood buffer
2. Plasma proteins Organ to Compensate: Kidneys
3. Hemoglobin Primary Compensation: Bicarbonate Excretion
4. Inorganic phosphate Example: ______________________________________
HENDERSON-HASSELBACH EQUATION METABOLIC ACIDOSIS
𝑐𝑜𝑛𝑗𝑢𝑔𝑎𝑡𝑒 𝑏𝑎𝑠𝑒
pH = pKa + log pH: Decreased; HCO3: Decreased
𝑤𝑒𝑎𝑘 𝑎𝑐𝑖𝑑
Organ Defective: Kidneys
Primary Cause: Bicarbonate Excretion
Where
pKa = 6.1 Organ to Compensate: Lungs
conjugate base = bicarbonate (HCO 3-) Primary Compensation: Hyperventilation
weak acid = carbonic acid (H2CO3) Example: ______________________________________
METABOLIC ALKALOSIS
𝐻𝐶𝑂3−
pH = 6.1 + log total CO2 = 𝐻𝐶𝑂3− + 𝐻2 𝐶𝑂3
𝐻2 𝐶𝑂3 pH: Increased; HCO3: Increased
𝐻𝐶𝑂3− = total CO2 - 𝐻2 𝐶𝑂3 𝐻2 𝐶𝑂3 = 0.03 x pCO2
Organ Defective: Kidneys
PARAMETERS Primary Cause: Bicarbonate Reabsorption
PH Organ to Compensate: Lungs
pH of 7.40 is the optimum level for arterial blood Primary Compensation: Hypoventilation
the reference range for arterial blood (7.35-7.45) is only Example: ______________________________________
0.03 pH unit lower for venous blood owing to the SPECIMEN COLLECTION
buffering effects of hemoglobin known as chloride specimen: arterial blood
isohydric shift anticoagulant: 0.05ml heparin/ml of blood
COLLEGE OF MEDICAL LABORATORY SCIENCE | 23 | 34
Clinical Chemistry
syringe and needle for arterial blood must be Table 33. Water Soluble Vitamins
preheparinized Chemical Name Deficiency
use of butterfly infusion sets is not recommended Vitamin B1 Thiamine Infants: Dyspnea,
liquid form of heparin is not recommended cyanosis, diarrhea,
vomiting
Samples should be analyzed immediately (<30mins) Adults: Beri-beri,
SPECIMEN CONSIDERATIONS Wernicke-Korsakoff
On standing: ___________________________________
syndrome (apathy, ataxia
______________________________________________
and visual problems)
Exposure to air: _________________________________
Vitamin B2 Riboflavin Angular stomatitis,
______________________________________________
dermatitis, photophobia
Blood samples should be chilled
Vitamin B3 Panthothenic acid Depressed immune
Glycolysis results to _____________________________ system, muscle weakness
METHODOLOGIES Vitamin B6 Pyridoxine, Infants: Irritability,
GASOMETER seizures, anemia
Pyridoxal
Adult: facial seborrhea
Van Slyke
Vitamin B12 Cyanocobalamin Megaloblastic anemia,
Natelson
Neurologic abnormalities
mercury – to produce vacuum
Vitamin C Ascorbic Acid Scurvy
caprylic alcohol – anti-foam reagent
lactic acid Folic Acid Pterolyglutamic Megaloblastic anemia
NaOH and NaHSO3 acid
ELECTRODES Niacin Nicotinic Pellagra (dermatitis,
acid/Nicotinamide disorientation, weight
pH (potentiomentry) loss)
________________________________________ –
internal reference electrode
ENDOCRINOLOGY
________________________________________ –
Endocrine System: network of ductless glands that
external reference electrode
secrete hormones directly into the blood; regulatory
pO2 – ________________ (polarography-amperometry)
system of blood
pCO2 – __________________________ (potentiometry)
Hormones: are chemical signals produced by specialized
VALUES TO REMEMBER
cells secreted into the blood stream and carried to target
Table 31. Normal Values
tissue; Major function: to maintain the constancy of
Normal Value
chemical composition of extracellular and intracellular
pH
fluids and control metabolism, growth, fertility and
pO2
responses to stress.
pCO2
FEEDBACK MECHANISMS
HCO3- Positive feedback mechanism –an increase in the
Total CO2 (arterial) product results to elevation of the activity of the system
Total CO2 (venous) and the production rate.
Negative feedback mechanism –an increase in the
VITAMINS product results to decreased activity of the system and
Table 32. Fat Soluble Vitamins the production rate.
Chemical Name Deficiency CLASSIFICATION OF HORMONES
Vitamin A Retinol Night blindness, growth Table 34. Classification of Hormones
retardation, abnormal Proteins/ Glycoprotein Steroids Amino acid
taste response, Peptides derivative
dermatitis GHRH, CRH, TSH, LH, FSH, Cortisol, Melatonin,
Vitamin E Tocopherols Mild hemolytic anemia TRH, GnRH, hCG, EPO Aldosterone, Serotonin,
(newborn), RBC fragility, Somatostatin, Estrogen, T3, T4,
ataxia PRF, ADH, Progesterone, Epinephrine,
Vitamin D Calciferol Rickets and Osteomalacia oxytocin, GH, Testosterone, Nor-
Vitamin K Phylloquinones, Bleeding disorder, ACTH, PRL, Vitamin D epinephrine
Menaquinones Hemorrhage Calcitonin,
hPL, PTH,
Insulin,
Glucagon
COLLEGE OF MEDICAL LABORATORY SCIENCE | 24 | 34
Clinical Chemistry
HYPOTHALAMUS GONADOTROPINS (FSH – FOLLICLE STIMULATING
above the pituitary gland and is connected to the HORMONE/LH – LUTEINIZING HORMONE)
posterior pituitary by the infundibulum (pituitary stalk) important markers in diagnosing fertility and menstrual
supraoptic and paraventricular nuclei produce cycle disorders
vasopressin and oxytocin ___________________ aids in spermatogenesis in males
HYPOTHALAMIC HORMONES ____________________________ helps Leydig cells to
1. Thyrotropin-releasing hormone (TRH) produce testosterone (male) and for female, it is
2. Gonadotropin-releasing hormone (GnRH) necessary for ovulation and the final follicular growth
3. Somatostatin/Growth hormone-inhibiting hormone (GH- _________________________ also acts on thecal cells to
IH) cause synthesis of androgens
4. Growth hormone-releasing hormone (GH-RH) THYROID STIMULATING HORMONE (TSH)
5. Prolactin-inhibiting factor (PIF) also known as thyrotropin
6. Vasopressin (supraoptic)
main stimulus for the uptake of iodide
7. Oxytocin (paraventricular nuclei)
stimulates thyroid hormone synthesis
PINEAL GLAND
ADRENOCORTICOTROPIC HORMONE (ACTH)
secretes ____________________________________
that decreases pigmentation of the skin produced in response to low serum cortisol
PITUITARY GLAND highest levels is between 6:00am to 8:00am; lowest level
also known as the “master gland” is between 6:00pm to 11:00pm
located in a small cavity called the sella turcica or Turkish increased: Addison’s disease, ectopic tumors, after
saddle protein-rich meals
All pituitary hormones have circadian rhythms best time for collecting specimen: 8:00am to 10:00am
ADENOHYPOPHYSEAL CELLS PROLACTIN (PRL)
functions in the initiation and maintenance of lactation
1. ________________________ – secrete growth hormone
2. ______________________________ – secrete prolactin major inhibitor: _______________________________
3. __________________________________ – secretes TSH consequence of prolactin excess: hypogonadism
4. ____________________________ – secretes LH and FSH specimen requirement: blood should be collected 3-4
5. _________________ – secretes proopiomelanocortin hours after the individual has awakened; fasting sample
(cleaved to produce ACTH, β-endorphin and β-lipotropin) POSTERIOR PITUITARY GLAND
ANTERIOR PITUITARY GLAND (ADENOHYPOPHYSIS)
capable of releasing hormones’ oxytocin and vasopressin
GROWTH HORMONE (GH/SOMATOTROPIN) but not capable of producing it
most abundant of all pituitary hormones OXYTOCIN
controlled by GH-RH (the amount released) and stimulates contraction of the gravid uterus at term –
somatostatin (governs the frequency and duration of “Fergusson reflex”
secretory pulse) ANTI-DIURETIC HORMONE (ADH)/ARGININE VASOPRESSIN
major stimulus: ________________________________ (AVP)
Disorders: acts on the distal convoluted tubule and collecting duct
Idiopathic GH deficiency – most common cause of major function: maintain osmotic homeostasis by
pituitary dwarfism in children regulating water balance
Pituitary adenoma – most common etiology in promotes reabsorption of water by the renal tubules –
adult-onset GH deficiency maintains water homeostasis
Acromegaly – due to overproduction of GH DIABETES INSIPIDUS (DI) is deficiency of ADH; results in
Table 35. Diagnostic Test for Growth severe polyuria
Hormone Clinical Picture for Diabetes Insipidus
Screening Tests Confirmatory Tests o Normoglycemia, Polyuria with low SG,
GH deficiency Physical activity Insulin tolerance Polydipsia, Polyphagia
(Exercise) test test (gold standard)
__________________________________________
Arginine stimulation
__________________________________________
test (2nd
o deficiency of ADH with normal ADH receptor
confirmatory test)
__________________________________________
Acromegaly Somatomedin-C or Glucose suppression
o normal ADH but abnormal ADH receptor – renal
Insulin-like growth test – OGTT (75g
resistance to ADH action
factor glucose)
o failure of the kidneys to respond to normal or
elevated ADH levels
COLLEGE OF MEDICAL LABORATORY SCIENCE | 25 | 34
Clinical Chemistry
Diagnostic test for DI – REIDEL’S THYROIDITIS
__________________________________________ thyroid turns into a woody or stony-hard mass
THYROID GLAND SUBCLINICAL HYPERTHYROIDISM
also known as the “butterfly-shaped’ gland shows no clinical symptom but TSH is low and FT 3 and FT4
consist of two lobes connected by the isthmus located at are normal
the lower part of the neck
follicle is the fundamental unit of the thyroid gland
2 types of cells: follicular cells (T3 and T4) and associated with neck pain, low grade fever and swings in
parafollicular cells/C cells (Calcitonin) thyroid function test
________________________________ is a glycoprotein HYPOTHYROIDISM
stored in the follicular colloid of the thyroid gland
Signs and symptoms: bradycardia, weight gain,
____________________________ is the most important
coarsened skin, cold intolerance and mental dullness
element in the biosynthesis of thyroid hormones
PRIMARY HYPOTHYROIDISM
MAJOR THYROID HORMONES
primarily due to deficiency in elemental iodine
TRIIODOTHYRONINE (T3) also caused by destruction or ablation of the thyroid
______________________________________________ gland
principal application of this hormone is in the diagnosis
of T3 thyrotoxicosis most common cause of primary hypothyroidism
______________________________________________ characterized by thyroid replaced by a nest of
an increase in the plasma level of T 3 is the first lymphoid tissue
abnormality seen in cases of hyperthyroidism lab result: high TSH and positive TPO antibody
TETROIODOTHYRONINE (T4) Myxedema
______________________________________________ myxedema coma is the severe form of primary
major fraction of organic iodine hypothyroidism
the amount of serum T 4 is a good indicator of thyroid peculiar non-pitting swelling of the skin
secretory rate clinical features: “puffy” face, weight gain, slow
THYROID-HORMONE BINDING PROTEINS speech, eyebrow thinned, dry and yellow skin and
1. anemia
transports majority of T3 (affinity for T3 is lower than Table 36. Autoimmune Disorders of the
T4) Thyroid Hormone
transport 70-75% of total T4 Hashimoto’s Thyroiditis Grave’s Disease
2. Thyroxine-binding prealbumin (transthyretin)
transports 15-20% of total T4
T3 has no affinity for prealbumin
3. Thyroxine-binding albumin
transports T3 and 10% of T4
HYPERTHYROIDISM
Signs and symptoms: tachycardia, tremors, weight loss, SECONDARY HYPOTHYROIDISM
heat intolerance, emotional lability and menstrual due to pituitary destruction or pituitary adenoma
changes TERTIARY HYPOTHYROIDISM
THYROTOXICOSIS
due to hypothalamic disease
high levels of free thyroid hormones in the circulation
CONGENITAL HYPOTHYROIDISM
T3 thyrotoxicosis/Plummer’s disease: FT3 increased but
defect in the development or function of the gland
FT4 normal with low TSH
symptoms: retarded physical and mental development
T4 thyrotoxicosis: T3 normal or low but T4 is increased
of the child
with low TSH
Table 37. Clinical Presentation of Patients
with Hypothyroidism & Hyperthyroidism
most common cause of thyrotoxicosis
Hypothyroidism Hyperthyroidism
antibodies are produced which are active against the TSH
Basal metabolic
receptor
rate
features: exophthalmos (bulging eyes) and pretibial
Sympathetic
myxedema
response
diagnostic test: TSH receptor antibody test
Weight
COLLEGE OF MEDICAL LABORATORY SCIENCE | 26 | 34
Clinical Chemistry
Temperature inversely related to TBG – decreased T3 uptake results to
tolerance elevated TBG result
THYROXINE-BINDING GLOBULIN (TBG)
GI function used to confirm results of FT 3 and FT4 or abnormalities in
the relationship of the total thyroxine (TT4) and THBR test
useful in distinguishing between hyperthyroidism
Cardiovascular (elevated T4 + N TBG) and euthyroidism (elevated T 4 +
function elevated TBG)
Table 38. Thyroid Gland Disturbances
T3 & T4 TSH
Respiratory Primary Hypothyroidism
function Secondary Hypothyroidism
General Primary Hyperthyroidism
appearance Secondary Hyperthyroidism
Table 39. Secondary vs Tertiary
Hypothyroidism
General behavior Mental Hypothyroidism Secondary Tertiary
Restlessness
retardation; T3 & T4
Irritability
Mental & TSH
Anxiety
Physical
Hyperkinesis TRH
sluggishness
Wakefulness TRH Stimulation/ TSH before TSH before
Somnolence
Administration administration: administration:
Others Increased Test
Cholesterol & Increased ALP
TSH after TSH after
TAG administration: administration:
THYROID FUNCTION TESTS
TRH STIMULATION TEST PARATHYROID GLAND
used to differentiate euthyroid and hyperthyroid located on or near the thyroid capsule; most people have
patients who both had undetectable TSH levels 4 parathyroid hormones
used to confirm borderline cases and euthyroid Grave’s smallest endocrine gland; secretes parathyroid hormone
disease – hypercalcemic hormone
PARATHYROID HORMONE
most important thyroid function test – best method for to prevent hypocalcemia (regulates blood calcium)
detecting clinically significant thyroid dysfunction preserve calcium and phosphate within normal range
most clinically sensitive assay in the detection of primary promotes bone resorption – release calcium in the
bloodstream
thyroid disorders
increases renal calcium reabsorption
REVERSE T3 (rT3) stimulates conversion of inactive vitamin D to activated
formed from the removal of one iodine from the inner vitamin D3
ring of T4 HYPERPARATHYROIDISM
rd
3 major circulating thyroid hormone
Primary Hyperparathyroidism
FREE THYROXINE INDEX (FTI OR T 7)
physiologic defect lies within the parathyroid gland
indirectly assesses the level of T 4 in the blood most common cause of hypercalcemia
FTI = TT4 x THBR due to the presence of a functioning parathyroid
𝑇3 𝑈 (%)
FTI = TT4 x 100 adenoma
TOTAL T3 (TT3), FREE T3 (FT3) AND FREE T4 (FT4) Secondary hyperparathyroidism
used to differentiate drug-induced TSH elevation and develops in response to decreased calcium
hypothyroidism diffuse hyperplasia of all 4 glands
the value of TT3 or FT3 is in confirming hyperthyroidism Tertiary hyperparathyroidism
T3 UPTAKE phosphate levels are normal to high; calcium
measures the number of available binding sites of the phosphates precipitate in soft tissues
thyroxine-binding proteins (TBG)
does not measure the level of T 3 in serum but it reflects
the serum level of TBG
COLLEGE OF MEDICAL LABORATORY SCIENCE | 27 | 34
Clinical Chemistry
Table 40. Hyperparathyroidism Levels signs and symptoms: obesity but with thin extremities
Primary Secondary (“buffalo hump”), hirsutism, hyperglycemia, thinning of
Serum Calcium the skin, poor wound healing, hypertension,
Serum hypercholesterolemia, low WBC count (lymphocytes)
Phosphate ________________________________ – current
PTH reference method for measuring urinary free cortisol
Urine Calcium ________________________________ – most sensitive
Urine Phosphate and screening test
VALUES TO REMEMBER Table 43. Diagnostic Tests for Cushing’s
Syndrome
Calcium level ________________________ = laryngeal
Screening Tests Confirmatory Tests
stridor and tonic clonic seizures
Calcium level ________________________ = tetany and 24-hour urinary free Low dose dexamethasone
cortisol test suppression test
altered neuromuscular activity
Overnight dexamethasone Midnight plasma cortisol
ADRENAL GLAND suppression test Corticotropin-releasing
has pyramid-like shape located above the kidneys Midnight salivary cortisol hormone (CRH) stimulation
composed of distinct but conjoined glands, the outer test test
adrenal cortex (yellow) and inner adrenal medulla (dark
HYPOCORTISOLISM
mahogany)
screening test: _________________________________
ADRENAL CORTEX
_____________________________________________
major site of steroid hormone production confirmatory test: Insulin tolerance test
Table 41. Adrenal Cortex Layers _______________________________ – gold standard
Layer Function for secondary and tertiary hypocortisolism
Zona glomerulosa (Outer Overnight metyrapone test – alternative diagnostic or
10%) confirmatory test for seconda
Zona fasciculata (Middle ry or tertiary adrenal insufficiency
75%) Primary hypocorticolism (primary adrenal insufficiency)
Zona reticularis (Inner 10%) due to decreased cortisol production – 90%
destruction of adrenal cortex
disorder: Addison’s disease – hypotension,
CORTISOL hyponatremia, hyperkalemia, weight loss,
hyperpigmentation
is the principal glucocorticoid
Secondary hypocorticolism (secondary adrenal
mostly bound to glycoprotein – transcortin
insufficiency)
stimulates gluconeogenesis in the liver resulting in
due to hypothalamic-pituitary insufficiency with loss
hyperglycemia
of ACTH
is the only adrenal hormone that inhibits the secretion of
absence of hyperpigmentation
ACTH
highest level ___________________________ and
results in the deficiency of enzymes necessary for the
lowest at night ____________________________
synthesis of cholesterol which will result to decreased
specimen: serum (red top), urine; blood sample should
plasma cortisol and increased ACTH and androgen levels
be drawn at 8:00 AM
definitive tests:
urine free cortisol levels are sensitive indicators of
17-OHP measurement in amniotic fluid
adrenal hyperfunction (endogenous hypecorticolism) –
Genotyping cells from chorionic villous sampling –
24 hour urine collection
preferred
Table 42. Cortisol Urinary Metabolites
ALDOSTERONE
Method Reagent
17- Phenylhydrazine most potent mineralocorticoid (electro-regulating
hydroxycorticosteroid in H2SO4 + hormone)
alcohol helps regulate water and electrolytes (sodium, chloride
17-ketogenic steroids Meta- and potassium) and blood pressure
dinitrobenzene acts on renal tubular epithelium to increase retention of
Na+ and Cl- and excretion of K+ and H+
Hypercortisolism (Cushing’s syndrome) method: RIA and chromatography
caused primarily by excessive production of cortisol and
ACTH but decreased aldosterone and renin
COLLEGE OF MEDICAL LABORATORY SCIENCE | 28 | 34
Clinical Chemistry
PRIMARY HYPERALDOSTERONISM (CONN’S DISEASE) EPINEPHRINE (ADRENALINE/SECONDARY AMINE)
caused by aldosterone-secreting adrenal adenoma most abundant medullary hormone
associated with elevated plasma aldosterone and low produced from norepinephrine and only from the
plasma renin adrenal gland
Table 44. Tests for Conn’s Disease
called the “flight or fight” hormone: release in response
Screening Test Confirmatory Test to physiologic (injuries) or psychologic (stress, anxiety)
Plasma aldosterone Saline suppression test threats
concentration/plasma Oral sodium loading test
Fludrocortisone major metabolite: __________________________:
renin activity ratio major (60%) catecholamine metabolite in the urine
suppression test
>30 ratio: __________ Captopril challenge test minor metabolites: metanephrine, normetanephrine
___________________
and homovanillic acid
___________________
DOPAMINE (PRIMARY AMINE)
>60 ratio: __________
___________________ catecholamine produced via the decarboxylation of 3,4-
___________________ dihydroxyphenylalanine
SECONDARY HYPERALDOSTERONISM major intact catecholamine in the urine
occurs as a result of excessive renin production major metabolite: ___________________________
accompanied by elevated plasma levels of aldosterone PHEOCHROMOCYTOMA
and renin tumor of the adrenal medulla or sympathetic ganglia
associated disorders: Liddle’s syndrome due to the overproduction of catecholamine
(pseudohypoaldosteronism), Barterr’s syndrome screening test: plasma metanephrines and
(bumetanide-sensitive chloride channel mutation), normetanephrines by HPLC (four-fold increase)
Gitelman’s syndrome (thiazide-sensitive transporter diagnostic test: 24-hour urinary excretion of
mutation) metanephrines and normetanephrine
HYPOALDOSTERONISM pharmacologic test: clonidine test and glucagon
due to the destruction of the adrenal glands and stimulation test
deficiency of glucocorticoid Patient preparation in the diagnosis of Pheochromocytoma
also associated with 21-hydroxylase deficiency Avoid caffeine, nicotine, alcohol and acetaminophen,
Tests for hypoaldosteronism monoamine oxidase inhibitors and tricyclic
Furosemide stimulation test or upright posture antidepressants for at least 5 days before testing
Saline suppression test
NEUROBLASTOMA
WEAK ANDROGENS
fatal malignant condition in children resulting to
serve as precursors for the production of more potent excessive production of norepinephrine
androgen and estrogen in tissues
(+) high urinary excretion of HVA or VMA or both and
example: dehydroepiandrosterone (DHEA) and dopamine
androstenedione
METHODOLOGIES
______________________________: principal adrenal
androgen; converted into estrone Specimen: _____________________________________
excessive production of androgens results in virilization Patient preparation:
(pseudohermaphroditism) Patient should undergo overnight fasting
Avoid smoking or drinking coffee at least 4 hours
ADRENAL MEDULLA
prior to blood collection
composed primarily of chromaffin cells that secrete Blood is collected on pre-chilled EDTA tubes
catecholamines Specimen considerations:
L-tyrosine is the precursor of catecholamines Catheterization is the preferred method of blood
ratio of norepinephrine to epinephrine is 9:1 collection
NOREPINEPHRINE (PRIMARY AMINE) Urine is preserved with 10ml of 6N HCl
produced by the sympathetic ganglia 1. Chromatography – HPLC or GC-MS (VMA and
highest concentration is in the brain (CNS) metanephrines)
major metabolite in CNS is MHPG 2. Radioimmunoassay – sensitive screening test for total
MAJOR METABOLITES OF NOREPINEPHRINE plasma catecholamines
>2000pg/ml of plasma catecholamines: diagnostic
3-methoxy-4-hydroxyphenylglycol (MHPG) – CSF and
for pheochromocytoma
urine
vanillylmandelic acid
COLLEGE OF MEDICAL LABORATORY SCIENCE | 29 | 34
Clinical Chemistry
REPRODUCTIVE HORMONES prime secretory product of the ovary
testes and ovaries produce sex steroids such as single best hormone to determine whether ovulation
androgens and estrogens from cholesterol has occurred
major transport proteins: sex-hormone binding globulin deficiency: failure of implantation of embryo
metabolites: pregnanediols (most easily measured
(SHBG), corticosteroid-binding globulin (CBG) and
metabolite), pregnanediones, pregnanalones
albumin
HUMAN CHORIONIC GONADOTROPIN (HCG)
TESTOSTERONE
produced by the trophoblast cells of the placenta during
principal androgen hormone in the blood – most potent
pregnancy
male androgen
same α-subunit as LH, FSH and TSH; similar β-subunit to
synthesized by the Leydig cells of the testis of the male;
LH – “LH-like” hormone
controlled primarily by the FSH and LH
intact HCG (α and β) is the predominant form throughout
function: growth and development of the reproductive
pregnancy
system, prostate and external ganglia
method: immunometric (sandwich) method – serum and
tests for male fertility: semen analysis, testosterone, FSH
urine samples
and LH
INHIBIN A
transport proteins: SHBG (60%) and albumin (40%)
Table 45. Types of Testicular Infertility Reproductive hormone which inhibits FSH activity
(Hypogonadism) METHODOLOGIES
Testos- FSH & Description/ other
Porter-Silber – for 17-OHCS
terone LH information
Zimmerman – steroids with 17-keto structure
Pre-
Due to hypothalamic Pisano – quantitating metanephrines and
testicular
or pituitary lesions normetanephrines
(Secondary)
Kober – estrogen
May be congenital
TESTS FOR MENSTRUAL CYCLE DYSFUNCTION
(e.g. Klinefelter’s
Testicular
syndrome) or
(Primary) TESTS FOR FEMALE INFERTILITY
acquired (e.g.
varicocele)
MARKERS FOR DOWN SYNDROME
Disorders of sperm
Post- Increased: _____________________________________
transport and
testicular Decreased: ____________________________________
function
DEHYDROEPIANDROSTERONE (DHEA) GASTRIN
peptide secreted by the G cells of the antrum of the
principal androgen formed by the adrenal cortex; weak stomach
androgen causes secretion of the HCl by parietal cells in the
ESTROGEN stomach
functions: promotion of breast development, diagnostic marker for Zollinger-Ellison syndrome (islet-
maturation of the external genitalia, deposition of body cell tumor)
fat and termination of linear growth (secondary sexual SEROTONIN (5-HYDROXYTRYPTAMINE)
characteristics in the female) derived from the hydroxylation and decarboxylation of
precursor: acetate, cholesterol, progesterone and tryptophan
testosterone synthesize by argentaffin cells, primarily in the GI tract
FORMS OF ESTROGEN diagnostic marker for carcinoid tumor
1. _________________ – most abundant estrogen in post- tests: Ehrlich’s aldehyde test – (+) purple color
menopausal women
2. _________________ – most potent estrogen; major THERAPEUTIC DRUG MONITORING
estrogen a quantitative procedure performed for drugs with
most abundant estrogen in pre-menopausal women narrow therapeutic index
transport proteins: albumin (60%), SHBG (38%) the half-life of the drug determines the time to reach the
3. _________________ – estrogen found in maternal urine steady-state or average concentration
major estrogen secreted by the placenta during Mixed Function Oxidase (MFO) system: biochemical
pregnancy pathway responsible for the greatest portion of drug
PROGESTERONE metabolism
produced mainly by the granulose (lutein) cells of the
corpus luteum in the female
COLLEGE OF MEDICAL LABORATORY SCIENCE | 30 | 34
Clinical Chemistry
PHARMACOLOGICAL PARAMETERS THAT ANTIBIOTICS
DETERMINE DRUG CONCENTRATION
1. Liberation – release of the drug
2. Absorption – transport of the drug from the site of Gentamicin, tobramycin, amikacin, kanamycin,
neomycin, streptomycin
administration to the blood
3. Distribution – delivery of the drug to the tissues Used for treatment of Gram-negative bacterial infection
4. Metabolism – process of chemical modification of the Toxic effects: nephrotoxocity and ototoxicity
drug by cells
5. Excretion – process by which the drug and its Used against Gram-positive bacilli and cocci
metabolites are excreted from the body Toxic effects: “______________________________”,
TERMINOLOGIES nephrotoxicity, ototoxicity
1. Bioavailable fraction (f) – fraction of the dose that CHLORAMPHENICOL
reaches the blood Toxic effects: blood dyscrasia, cytoplasmic vacuolation
2. First pass hepatic metabolism – drugs that are (erythroid and myeloid cells)
transported to the liver lost a fraction of its bioavailability ANTI-EPILEPTIC DRUGS
before the drug reaches the general circulation
3. Half-life (t1/2) – time required to reduce a drug level to
Long acting barbiturate that controls grand-mal tonic
half its original value
clonic seizures and focal epilepsies
4. _____________________________ – highest
concentration of a drug obtained in the dosing interval
5. _____________________________ – lowest Controls tonic-clonic, simple partial seizures; a short
concentration of a drug obtained in the dosing interval term prophylactic agent in brain injury
6. _____________________________ – relationship
between the drug concentration at the target site and Treatment of petit mal (absence seizures), atomic seizure
response of the tissues and grand mal
7. ______________________ – mathematical expression of
the relationship between drug dose and drug blood level Effective for grand mal seizures and treating seizures
8. Pharmacogenomics – study of genes that affect the accompanied by pain
performance of a drug in an individual ETHOSUXIMIDE
THERAPEUTIC DRUGS Drug of choice in controlling petit mal (absence) seizure
CARDIOACTIVE DRUGS
Class I – rapid Na+ blockers Chemically similar to neurotransmitter gamma
Class II – beta receptor blockers aminobutyric acid
Class III – K+ channel blockers Adverse effects: dizziness, ataxia, fatigue and nystagmus
Class IV – Ca2+ channel blockers PSYCHOACTIVE DRUGS
DIGOXIN LITHIUM
Treatment of atrial arrhythmia and congestive heart Used for treatment of manic-depressive bipolar
failure (CHF) disorders
LIDOCAINE (XYLOCAINE) TRICYCLIC ANTI-DEPRESSANTS
Correct ventricular arrhythmia and treatment of MI Used for treatment of depression, insomnia and extreme
QUINIDINE apathy
Treatment of arrhythmia Major metabolite: desipramine
FLUOXETINE (PROZAC)
Treatment of ventricular arrhythmia Treatment of obsessive-compulsive disorders
Toxic effects: reversible lupus-like- syndrome BRONCHODILATOR
DISOPYRAMIDE
Has anti-cholinergic effects – dry mouth and constipation
Treatment of asthma and chronic obstructive pulmonary
PROPANOLOL
disease
Used in treatment of thyrotoxicosis
IMMUNOSUPPRESIVE DRUGS
AMIODARONE
Iodine-containing drug which can cause hypo or CYCLOSPORINE
hyperthyroidism For suppression of acute graft-versus-host disease
VERAPAMIL (GVHD)
Treatment of angina, hypertension and supraventricular Specimen of choice: whole blood
arrhythmia
COLLEGE OF MEDICAL LABORATORY SCIENCE | 31 | 34
Clinical Chemistry
TACROLIMUS Peak concentrations are drawn one hour after an orally
100x more powerful than cyclosporine administered dose and immediately after infusion for an
Toxic effects: thrombus formation, nephrotoxicity, IV administered drug; best specimen
neurotoxicity COLORIMETRY
RAPAMYCIN Acetaminophen in urine is detected by boiling to form p-
Similar to tacrolimus with major side effects of amphenol which then reacts with o-cresol to form
thrombocytopenia and lipid abnormalities indophenol blue
MYCOPHENOLATE MOFETIL Trinder assay for salicylate using ferric nitrate forming a
Decreases renal allograft rejection colored complex
LEFLUNOMIDE (LFM) IMMUNOASSAY METHODS
Inhibits lymphocyte proliferation; treatment of RA
can detect drug levels in nanomolar range; sensitive and
ANTINEOPLASTIC DRUGS
specific methods
METHOTREXATE Enzyme-mediated (multiplied) immunologic technique
Inhibits DNA synthesis in all cells (EMIT)
Leucovorin rescue: reverse action of methotrexate Fluorescence polarization immunoassay (FPIA)
BUSULFAN CHROMATOGRAPHIC METHODS
Treatment of leukemias and lymphomas prior to best specimen: ____________________________
bone marrow transplantation
ANTI-INFLAMMATORY/ANALGESICS quantitatively identifies drugs by means of their Rf
values
Commonly used analgesic, anti-pyretic and anti- extraction of drugs is pH dependent – acidic drugs at
inflammatory drug pH 4.5 and alkaline drugs at pH 9.0
Has anticoagulant property by inhibiting _____________
Acute aspirin intoxication: common cause of fatal drug ideal for separation of tricyclic antidepressants and
poisoning in children its metabolites
Method: Trinder assay, HPLC, EMIT, Enzymatic assay ____________________________________________ –
gold standard
Commonly used analgesic and anti-pyretic drug
Over dosage leads to hepatotoxicity TOXICOLOGY
Method: HPLC ALCOHOLS
ETHANOL (GRAIN ALCOHOL)
Lower risk of toxicities than salicylates and most common abused drug
acetaminophen antidote for chronic intoxication: diazepam (for
NEUROLEPTICS (ANTI-PSYCHOTIC MAJOR alcoholic mania)
TRANQUILIZERS) specimen: serum (capillary and arterial blood are
preferred)
Block the action of dopamine and serotonin in the limbic
system methods for testing: enzymatic, gas-liquid
chromatography and electrochemical oxidation
Used in the treatment of acute schizophrenia
preferred method: enzymatic using alcohol
2 classes: phenothiazines (chlorpromazine) and
dehydrogenase reagent
butyrophenones (haloperidol)
Examples: risoperdal, olanzapine, quetiapine, ____________________________ = symptoms of
aripiprazole alcohol intoxication begin to manifest
___________________________ = legally intoxicated
METHODOLOGIES FOR TDM
SPECIMEN CONSIDERATIONS ___________________________ = presumptive
evidence of driving under influence of alcohol
Specimen of choice: serum or plasma
Table 46. Stages of Ethanol Impairment
Whole blood EDTA sample is required for cyclosporine
Alcohol (%, w/v) SxS
and
0.01 – 0.05 No obvious impairment, some changes
tacrolimus test
observable on performance testing
Timing of the specimen collection is the single most
0.03 – 0.12 Mild euphoria, decreased inhibitions,
important factor in TDM
some impairment of motor skills
Trough concentrations are drawn immediately or 30
minutes before the next dose; lowest level of drug in
blood
COLLEGE OF MEDICAL LABORATORY SCIENCE | 32 | 34
Clinical Chemistry
0.09 – 0.25 Decreased inhibitions, loss of critical MERCURY
judgment, memory impairment, inhibits catecholamine-0-methytransferase
diminished reaction time has the ability to “amalgamate” – mix or merge with
0.18 – 0.30 Mental confusion, dizziness, strongly other substances
impaired motor skills (staggering, forms of mercury: elemental/metallic mercury,
slurred speech) mercurous, mercuric and alkyl mercury
0.27 – 0.40 Unable to stand or walk, vomiting, major toxic effect of elemental mercury: ____________
impaired consciousness ______________________________________________
0.35 – 0.50 Coma and possible death major toxic effect of alkyl mercury: congenital Minimata
METHANOL (WOOD ALCOHOL) disease
samples: whole blood and 24-hour urine
commonly used solvent and a contaminant of
method: ________________________
homemade liquors
LEAD
Symptoms of intoxication: frank blindness (ocular
blocks ________________________________________
toxicity) and metabolic acidosis
______________________________________________
screening test: computation of osmolal gap
______________________________________________
preferred method: GC-MS
source: paints and gasoline
ISOPROPANOL (RUBBING ALCOHOL)
indications of toxicity: urinary aminolevulinic acid, free
metabolized by hepatic alcohol dehydrogenase into RBC proporphyrin and presence of
acetone ________________________________________ in RBC
preferred method: gas chromatography lead chelators: EDTA and dimercaptosuccinic acid (DMA)
antidote: activated charcoal characteristic “wrist drop” or “foot drop” manifestation
ETHYLENE GLYCOL (1,2 – ETHANEDIOL) (peripheral neuropathy)
common constituent of hydraulic fluid and anti-freeze samples: whole blood (quantitative testing), urine
(recent lead exposure), hair
converted to oxalic acid and glycolic acid by hepatic
alcohol dehydrogenase LABORATORY TESTS FOR LEAD
indication of toxicity: deposition of calcium oxalate 1. Screening test - Zinc protoporphyrin test
crystals in renal tubules (Fluorometric) δ-ALA dehydratase test (sensitive)
major metabolite: glycolic acid (cause of acute toxicity 2. In-vivo x-ray fluorescence of bones
and death) 3. Atomic absorption spectrophotometry
preferred method: HPLC 4. Inductively couples plasma emission spectrophotometry
SPECIMEN PRECAUTION 5. Anodic stripping voltammetry
DRUGS OF ABUSE
Specimen must be capped at all times to avoid alcohol
Designer drugs – are modified forms of established drugs
evaporation
of abuse
prior to collection, alcohol-free skin cleanser must be
used instead of isopropanol
CARBON MONOXIDE therapeutically used for the treatment of narcolepsy and
is a colorless, odorless, tasteless gas; very toxic substance attentional deficit disorder
binds with heme proteins: cytochromes, hemoglobin and cause the release of dopamine from brain leading to
myoglobin “pleasant feeling” or “high” among users
higher affinity for hemoglobin that does oxygen (200x 3,4-methylenedioxymethamphetamine (MDMA or
faster than oxygen) ‘ecstasy’) – a derivative of methamphetamine, is a
indication of acute toxicity: “________” color of the face popular recreational abused drug
sample for testing: EDTA whole blood cause of false positive reaction: presence of
definitive method: ___________________________ antihistamine
(carboxyhemoglobin measurement) ANNABOLIC STEROIDS
CYANIDE chemically related to testosterone; improves athletic
super toxic substance (fast acting toxin) and death may performance by increasing muscle mass
occur in less than an hour CANNABINOIDS
inhibits cellular respiration, electron transport and ATP
formation naturally-occurring cannabinoids: marijuana and
hashish
indication of toxicity: “___________________________”
breath and altered mental status __________________________________ : most potent
component or the psychoactive substance of marijuana;
antidote: sodium thiosulfate, amyl and sodium
lipophilic
COLLEGE OF MEDICAL LABORATORY SCIENCE | 33 | 34
Clinical Chemistry
THC-COOH can be detected in urine for 3-5 days; up to 4
weeks for chronic users METHODS FOR IDENTIFYING AND MEASURING
urinary metabolite: 11-nor-deltatetrahydrocannabinol ABUSED DRUGS
(THC-COOH) 1. Enzymatic – alcohol is measured from blood using
COCAINE (CRACK) alcohol dehydrogenase as reagent
used as _______________________________________ 2. Capillary electrophoresis – different analyte selectivity is
derived from coca plant (Erythroxylon) and used as based on different physicochemical principles of
additive to some foods separation without changes in instrumental hardware.
inhibitor: Prozac 3. Homogenous immunoassay – assay is done in one
solution without separation
treatment for cocaine addiction: Benzodiazepine
Enzyme mediated immunologic technique (EMIT) –
urine metabolite: ______________________________
uses enzyme-labeled drug that competes with the
not considered as an addictive drug – does not reflect
drug in sample
true dependence
4. Chromatographic methods
easily passes the placenta and mammary glands resulting
Thin layer chromatography – uses serum, urine or
to mental retardation, slow mental development and
gastric fluid for analysis
drug dependence in newborns
Liquid chromatography-Mass spectroscopy (LC-MS)
can cause sudden death due to direct toxicity in
– used to confirm positive test results from a
myocardium (cardiac toxicity)
screening assay
OPIATES
High performance liquid chromatography (HPLC) –
capable of analgesia, sedation and anesthesia used as an alternative to GC-MS in definitive
derived chemically from opium poppy identification of drugs
naturally occurring opiates: opium, morphine and Gas chromatography
codeine o Gas liquid chromatography (GLC) – legally
chemically modified opiates: heroine, hydormorphone accepted method for ethanol testing
and oxycodone o GC with infrared spectroscopy – detection of
commonly tested opiates: _______________________ amphetamines
major metabolites of heroine: N-acetylmorphine o Gas chromatography-Mass spectroscopy – gold
(heroin) and morphine standard for confirmation of screening tests;
antagonist for opiate overdose: naloxone (narcan) allows for detection of low levels of drugs
Codeine is ________________________________.
Morphine is a metabolite of heroin used in the treatment REFERENCES
of congestive heart failure. Rodriguez, Maria Teresa. Clinical Chemistry Handbook for
Heroin is highly addictive (true physical dependence) medical technologists. Cattleya Star Copy Center and
PHENCYCLIDINE Book Binding, 2014
Coderes, Errol. March 2018 Medical Technology Board
physiologic effects: analgesia and anesthesia
Exam Final Coaching Notes. Pioneer Educational Review
major metabolite: phencyclidine HCl
Center, Manila, 2018
mode of treatment: isolation (kept in quiet, dark room)
Policarpio, Judea Marie. March 2018 Medical Technology
SEDATIVE HYPNOTICS
Board Exam Final Coaching Notes. ACTS Review Center,
examples: barbiturates and benzodiazepines Manila, 2018
Commonly abused barbiturates: secobarbital, Plaza, Xenia. March 2019 Medical Technology Board
pentobarbital, phenobarbital and thiopental Exam Clinical Chemstry Review Notes. Remedios Trinidad
commonly abused benzodiazepines: diazepam (valium), Romualdez Medical Foundation, 2019
chlordiazepoxide (Librium) and lorezepam (Ativan)
major metabolite: secobarbital (barbiturates)
barbiturate chemoadsorbent: activated charcoal
LYSERGIC ACID DIETHYLAMIDE (LSD, LYSERGIDE)
one of the most potent pharmacologic materials known
most common adverse reaction: panic reaction - “bad
trip”
toxic effects: blurred/ “undulating” vision and
synesthesia
COLLEGE OF MEDICAL LABORATORY SCIENCE | 34 | 34
You might also like
- Rodak Questions CompilationDocument40 pagesRodak Questions CompilationGertrudeshane IletoNo ratings yet
- Glanela Manaloto: Clinical ChemistryDocument48 pagesGlanela Manaloto: Clinical ChemistryGlanela M. BenjaminNo ratings yet
- Clinical Chemistry Notes - AbiDocument34 pagesClinical Chemistry Notes - AbiAnya Ignacio100% (1)
- Clinical Chemistry Notes Without Blanks LegitDocument43 pagesClinical Chemistry Notes Without Blanks LegitPearl Isabelle SudarioNo ratings yet
- University of The Immaculate Conception: ProteinDocument13 pagesUniversity of The Immaculate Conception: ProteinDams ZainalNo ratings yet
- Clinical MicrosDocument37 pagesClinical MicrosMarie Llanes100% (1)
- MUST To KNOW in Clinical ChemistryDocument53 pagesMUST To KNOW in Clinical ChemistryMonkey LuffyNo ratings yet
- St. Paul University Philippines: College of Medical TechnologyDocument14 pagesSt. Paul University Philippines: College of Medical TechnologyJulius FrondaNo ratings yet
- Clinical Chemistry Notes (Blanked) - ABI PDFDocument34 pagesClinical Chemistry Notes (Blanked) - ABI PDFAnya IgnacioNo ratings yet
- ISBB Aaaaa PDFDocument55 pagesISBB Aaaaa PDFSelena de LimaNo ratings yet
- Group 1 - Analysis of Urine and Other Body FluidsDocument11 pagesGroup 1 - Analysis of Urine and Other Body Fluidsjulo_05100% (4)
- Histopath ReviewerDocument43 pagesHistopath ReviewerMika De VeraNo ratings yet
- CHEM 2 CH 29 Review QuestionsDocument2 pagesCHEM 2 CH 29 Review QuestionsthrowawyNo ratings yet
- Ereviewer. Mtlaws. Prelims and Midterms PDFDocument8 pagesEreviewer. Mtlaws. Prelims and Midterms PDFCatlyn RivalNo ratings yet
- HistopathDocument23 pagesHistopathElla SalesNo ratings yet
- Immunology and Serology TestsDocument2 pagesImmunology and Serology TestsPearlregine Cianne MirandaNo ratings yet
- AUBF QuetionsDocument34 pagesAUBF QuetionsAprille Patol100% (1)
- Clinical Microscopy ExamDocument3 pagesClinical Microscopy ExamKarla GiorlaNo ratings yet
- Clinical ChemistryDocument10 pagesClinical ChemistryKristine Jamella Maris Narag100% (1)
- Clinical Chemistry KeyNotes For Board ExaminationDocument12 pagesClinical Chemistry KeyNotes For Board ExaminationPrincess Alen Aguilar100% (2)
- Immunology Serology ReviewDocument211 pagesImmunology Serology ReviewRachel Marie M. Gania100% (1)
- Histopathology ReviewerDocument6 pagesHistopathology ReviewerDiamante MhayaleneNo ratings yet
- Mls 419: Aubf Lab Semen Analysis 5% Spermatozoa 60-70% Seminal Fluid 20-30% Prostate FluidDocument24 pagesMls 419: Aubf Lab Semen Analysis 5% Spermatozoa 60-70% Seminal Fluid 20-30% Prostate FluidLyra Dennise LlidoNo ratings yet
- Hematology ReviewerDocument10 pagesHematology ReviewerAldren BeliberNo ratings yet
- MUST To KNOW in BacteriologyDocument35 pagesMUST To KNOW in BacteriologyJohn TamayoNo ratings yet
- Chapter 13 Rodaks HematologyDocument10 pagesChapter 13 Rodaks HematologyRALPH JAN T. RIONo ratings yet
- Pre and Post Analytical Procedures: Subtopic: Receiving, Accessioning, & Releasing of ResultsDocument29 pagesPre and Post Analytical Procedures: Subtopic: Receiving, Accessioning, & Releasing of ResultsShara AboNo ratings yet
- MTAP - HematologyDocument13 pagesMTAP - HematologyKassandra CordetaNo ratings yet
- Clinical ChemistryDocument8 pagesClinical Chemistryleizej29No ratings yet
- Aubf LabDocument99 pagesAubf Labhinata shoyoNo ratings yet
- Group 4 - General Pathology, Logic and Cytologic TechniquesDocument11 pagesGroup 4 - General Pathology, Logic and Cytologic Techniquesjulo_05No ratings yet
- Clinical Chemistry RTP 1Document9 pagesClinical Chemistry RTP 1Reham Que100% (1)
- Clinical Chemistry 1 Basic PrinciplesDocument2 pagesClinical Chemistry 1 Basic PrinciplesJorella Marisol MarquezNo ratings yet
- CM Handouts Clinical MicrosDocument33 pagesCM Handouts Clinical Microsrenato renato100% (1)
- Must To Know HemaDocument44 pagesMust To Know HemaKaycee Gretz LorescaNo ratings yet
- Clinical Chemistry NotesDocument24 pagesClinical Chemistry Notesclower112100% (3)
- Recalls Sept 2018 PDFDocument12 pagesRecalls Sept 2018 PDFRomina LacsonNo ratings yet
- MTAP ISBB - Sir JJ (Merged)Document9 pagesMTAP ISBB - Sir JJ (Merged)Nathan DrakeNo ratings yet
- Recalls of Compilation of Clinical ChemistryDocument10 pagesRecalls of Compilation of Clinical ChemistryDeniel BusiNo ratings yet
- MT Laws Reviewer MidtermsDocument6 pagesMT Laws Reviewer MidtermsKyaru Fuentes100% (1)
- Is RecallsDocument15 pagesIs RecallskthmntsNo ratings yet
- Aubf Review UermDocument18 pagesAubf Review UermZhiddah Japzon0% (1)
- Clinical Chemistry Notes - ABIDocument32 pagesClinical Chemistry Notes - ABIAnya Ignacio100% (1)
- Aubf Questions With AnswersDocument16 pagesAubf Questions With AnswersFenyl Isis GuigayomaNo ratings yet
- Clinical Chemistry 2Document22 pagesClinical Chemistry 2Rubenne Miles ElagasNo ratings yet
- Must To Know MTLDocument15 pagesMust To Know MTLMae MacalandaNo ratings yet
- Hematology Recall QuestionsDocument4 pagesHematology Recall QuestionsMai RodrigoNo ratings yet
- In House Review On MTLE PDFDocument46 pagesIn House Review On MTLE PDFYukiNo ratings yet
- SerologyDocument84 pagesSerologyngsusannasuisum100% (2)
- Immunoserology: Medical Technology Assessment Progam 1 Discussed By: Mr. Mark MendrosDocument8 pagesImmunoserology: Medical Technology Assessment Progam 1 Discussed By: Mr. Mark MendrosLea Juan100% (1)
- Clinical Microscopy ReviewerDocument31 pagesClinical Microscopy Reviewerbokbokbok100% (1)
- LAB MAN REVIEWER by Darcee QTDocument8 pagesLAB MAN REVIEWER by Darcee QTJhona Mae CortesNo ratings yet
- Histopath MTLDocument6 pagesHistopath MTLElla Sales100% (1)
- Clinical Chemistry (Lecture) - PrelimsDocument12 pagesClinical Chemistry (Lecture) - Prelimsisprikitik3100% (1)
- Micro Lab Prac - PDCR PDFDocument10 pagesMicro Lab Prac - PDCR PDFPatti Danielle Referente50% (2)
- Clinical Chemistry Board ReviewDocument14 pagesClinical Chemistry Board ReviewWellaBaylasNo ratings yet
- 2nd Sem - Hema1 - An Overview of Clinical Laboratory HematologyDocument3 pages2nd Sem - Hema1 - An Overview of Clinical Laboratory HematologyAisle Malibiran PalerNo ratings yet
- Hemodynamic Hemodynamic Monitoring I Monitoring IDocument8 pagesHemodynamic Hemodynamic Monitoring I Monitoring Ifernn88No ratings yet
- Glasswares and EquipmentDocument2 pagesGlasswares and EquipmentCharlyn Dela CruzNo ratings yet
- Handout CCDocument39 pagesHandout CCmaikkadoriaNo ratings yet
- LAQ 2104 Lambton Handout1 .DotxDocument11 pagesLAQ 2104 Lambton Handout1 .Dotxamit kashyapNo ratings yet
- The Efficacy of Cucurbitane Type Triterpenoids GlyDocument13 pagesThe Efficacy of Cucurbitane Type Triterpenoids GlyVenny SandjajaNo ratings yet
- Lipid and Glucose Methodology PDFDocument16 pagesLipid and Glucose Methodology PDFJezzah Mae CañeteNo ratings yet
- Plasma Lipoproteins - METABOLISM PDFDocument4 pagesPlasma Lipoproteins - METABOLISM PDFRishabhNo ratings yet
- Biokimia LipidDocument6 pagesBiokimia Lipiddimensi warnaNo ratings yet
- Lipoprotein MetabolismDocument60 pagesLipoprotein MetabolismI MADE MIARTA YASA100% (1)
- Effects of Exercise On Lipoproteins and Hemostatic FactorsDocument11 pagesEffects of Exercise On Lipoproteins and Hemostatic FactorsJessica BarcelonaNo ratings yet
- Clinical Biochemistry - Fifth YearDocument176 pagesClinical Biochemistry - Fifth YearBayan AlsaadiNo ratings yet
- Ch15 Metabolism of Dietary LipidsDocument37 pagesCh15 Metabolism of Dietary LipidsWahab KhaniNo ratings yet
- ReportDocument16 pagesReportprachiNo ratings yet
- Bandeali-Farmer2012 Article High-DensityLipoproteinAndAtheDocument7 pagesBandeali-Farmer2012 Article High-DensityLipoproteinAndAtheDainius JakubauskasNo ratings yet
- Fat PTC8Document52 pagesFat PTC8vNo ratings yet
- Reagents Brochure LT314 MAR20Document80 pagesReagents Brochure LT314 MAR20Yousra ZeidanNo ratings yet
- Therapeutic Efficacy of Centella Asiatica PDFDocument9 pagesTherapeutic Efficacy of Centella Asiatica PDFJ C Torres FormalabNo ratings yet
- L16 - LipidsDocument15 pagesL16 - LipidsBobbyNo ratings yet
- The Effect of Ginger (Zingiber Officinale) As An Ancient Medicinal Plant On Improving Blood LipidsDocument5 pagesThe Effect of Ginger (Zingiber Officinale) As An Ancient Medicinal Plant On Improving Blood LipidsShania Astanti SimanjuntakNo ratings yet
- Al., 2008. American Heart Association American Stroke AssociationDocument6 pagesAl., 2008. American Heart Association American Stroke AssociationPuput mopanggaNo ratings yet
- Apoe in LipoproteinDocument12 pagesApoe in LipoproteinHoàng Linh VươngNo ratings yet
- Roche Cobas E411 Tests MenuDocument4 pagesRoche Cobas E411 Tests Menuمصطفى علي0% (1)
- A Fully Automated Clinical Chemistry Analyser With Unrivalled PerformanceDocument16 pagesA Fully Automated Clinical Chemistry Analyser With Unrivalled PerformanceBadmus AdeyemiNo ratings yet
- Tenp DPT Biochemistry: DR Pius KiptemburDocument13 pagesTenp DPT Biochemistry: DR Pius KiptemburGerald Limo Arap ChebiiNo ratings yet
- Compendium of Selected Recent Publications Cell and Molecular Biology ResearchDocument16 pagesCompendium of Selected Recent Publications Cell and Molecular Biology ResearchXyza Kim OlivaNo ratings yet
- 2016 ESC/EAS Guidelines For The Management of DyslipidaemiasDocument72 pages2016 ESC/EAS Guidelines For The Management of DyslipidaemiasStăncescu OvidiuNo ratings yet
- Far Eastern University - Nicanor Reyes Medical FoundationDocument7 pagesFar Eastern University - Nicanor Reyes Medical FoundationMaf B100% (1)
- Pharmacotherapy - 2023 - Alhomoud - Role of Lipoprotein A in Atherosclerotic Cardiovascular Disease A Review of CurrentDocument13 pagesPharmacotherapy - 2023 - Alhomoud - Role of Lipoprotein A in Atherosclerotic Cardiovascular Disease A Review of CurrentOana MihaelaNo ratings yet
- Reagents Brochure LT314 JULY 16 LOW RESDocument72 pagesReagents Brochure LT314 JULY 16 LOW RESSivaNo ratings yet
- Nejmp 038171Document3 pagesNejmp 038171Rifki Effendi SuyonoNo ratings yet
- Clinical Chemistry Notes - ABIDocument32 pagesClinical Chemistry Notes - ABIAnya Ignacio100% (1)
- Lipoproteins in Diabetes Mellitus: Alicia J. Jenkins Peter P. Toth Timothy J. Lyons EditorsDocument468 pagesLipoproteins in Diabetes Mellitus: Alicia J. Jenkins Peter P. Toth Timothy J. Lyons EditorsFELEL100% (1)