Professional Documents
Culture Documents
Extra 1
Extra 1
Uploaded by
Jennifer LozanoCopyright:
Available Formats
You might also like
- Freshwater Aquarium ManualDocument32 pagesFreshwater Aquarium Manualhippong niswantoroNo ratings yet
- A View of The Cell Review PacketDocument7 pagesA View of The Cell Review Packetapi-259727482No ratings yet
- PA-1 Adjusments and Worksheet (Problems)Document5 pagesPA-1 Adjusments and Worksheet (Problems)Safira ChairunnisaNo ratings yet
- FGI Patient Handling and Mobility Assessments 191008Document476 pagesFGI Patient Handling and Mobility Assessments 191008morton1472100% (1)
- Effect of Mirror Therapy Combined With Somatosensory Stimulation On Motor Recovery and Daily Function in Stroke Patients: A Pilot StudyDocument7 pagesEffect of Mirror Therapy Combined With Somatosensory Stimulation On Motor Recovery and Daily Function in Stroke Patients: A Pilot StudyDedi Irawandi Angela NursisNo ratings yet
- Amasyali 2016Document6 pagesAmasyali 2016leandroNo ratings yet
- Effect of Mirror Therapy Combined With Somatosensory Stimulation On Motor Recovery and Daily Function in Stroke Patients: A Pilot StudyDocument7 pagesEffect of Mirror Therapy Combined With Somatosensory Stimulation On Motor Recovery and Daily Function in Stroke Patients: A Pilot Studywanda argeNo ratings yet
- NRC 1729Document9 pagesNRC 1729Laura Michell Carrero GómezNo ratings yet
- The Effectivity of Mirror Therapy On Arm Motoric Improvement in Acute Ischemic StrokeDocument7 pagesThe Effectivity of Mirror Therapy On Arm Motoric Improvement in Acute Ischemic StrokeilyasNo ratings yet
- Mirror Therapy For Motor Function of The Upper Extremity inDocument8 pagesMirror Therapy For Motor Function of The Upper Extremity inilyasNo ratings yet
- MPT Dissertation PPT CorrectedDocument30 pagesMPT Dissertation PPT CorrectedPradeep Kumar BhuvaneshwaranNo ratings yet
- Efficacy of Modified Constraint Induced Movement Therapy in The Treatment of Hemiparetic Upper Limb in Stroke Patients: A Randomized Controlled TrialDocument5 pagesEfficacy of Modified Constraint Induced Movement Therapy in The Treatment of Hemiparetic Upper Limb in Stroke Patients: A Randomized Controlled TrialHaveezhNo ratings yet
- Cerebal PalsyDocument10 pagesCerebal PalsySoffie FitriyahNo ratings yet
- Boake Et Al 2007 Constraint Induced Movement Therapy During Early Stroke RehabilitationDocument11 pagesBoake Et Al 2007 Constraint Induced Movement Therapy During Early Stroke RehabilitationoverhiitshopNo ratings yet
- E000514 FullDocument6 pagesE000514 FullRenan O. Pravatta PivettaNo ratings yet
- Morkisch 2019Document15 pagesMorkisch 2019David Morote VillaNo ratings yet
- Giray 2019Document13 pagesGiray 2019Felix LoaizaNo ratings yet
- Comparing Targeted Thrust Manipulation With General Thrust Manipulation in Patients With Low Back Pain. A General Approach Is As Effective As A Specific One. A Randomised Controlled TrialDocument6 pagesComparing Targeted Thrust Manipulation With General Thrust Manipulation in Patients With Low Back Pain. A General Approach Is As Effective As A Specific One. A Randomised Controlled TrialMilton Ricardo de Medeiros FernandesNo ratings yet
- SimonettiDocument14 pagesSimonettijuanNo ratings yet
- Cjim 11 163Document8 pagesCjim 11 163Nurul Annisa KamalNo ratings yet
- Dry Needling On Biomechanical 2021Document8 pagesDry Needling On Biomechanical 2021Fábio PedraNo ratings yet
- The Efficacy of Muscle Energy TechniquesDocument18 pagesThe Efficacy of Muscle Energy Techniquesmuhammad yaminNo ratings yet
- Dunning James Et AlDocument10 pagesDunning James Et Alapi-290796947No ratings yet
- Arthrogenic Muscle Inhibition After ACL Reconstruction A Scoping Review of The Efficacy of InterventionsDocument11 pagesArthrogenic Muscle Inhibition After ACL Reconstruction A Scoping Review of The Efficacy of InterventionsfilipecorsairNo ratings yet
- Constraint Induced Manual TherapyDocument165 pagesConstraint Induced Manual TherapyPrabhu Chinna Gounder100% (1)
- SHS EMG BiofeedbackDocument16 pagesSHS EMG BiofeedbackPraneeth KumarNo ratings yet
- FonteDocument12 pagesFontejuanNo ratings yet
- Cimt and NDT Proposal-2 AltDocument10 pagesCimt and NDT Proposal-2 Altapi-487111274No ratings yet
- Articulo MIRROR 1Document9 pagesArticulo MIRROR 1Jossie QueralesNo ratings yet
- Constraint Induced Movement TherapyDocument4 pagesConstraint Induced Movement TherapyNikka VentorilloNo ratings yet
- 12 Nadiah Zuhdi 18.0095.T JurnalCIMT StrokeDocument10 pages12 Nadiah Zuhdi 18.0095.T JurnalCIMT StrokeZuhdiNo ratings yet
- 10 Jpts 27 1455Document3 pages10 Jpts 27 1455mustafasacarNo ratings yet
- Mirror Therapy Enhances Motor Performance in The Paretic Upper Limb After Stroke: A Pilot Randomized Controlled TrialDocument6 pagesMirror Therapy Enhances Motor Performance in The Paretic Upper Limb After Stroke: A Pilot Randomized Controlled TrialScientifica EducacionalNo ratings yet
- BMC Neurology: Comparing Unilateral and Bilateral Upper Limb Training: The ULTRA-stroke Program DesignDocument14 pagesBMC Neurology: Comparing Unilateral and Bilateral Upper Limb Training: The ULTRA-stroke Program DesignDharam PandeyNo ratings yet
- The Effectiveness of Spinal Manipulation in Increasing Muscle Strength in Healthy Individuals A Systematic Review and Meta-AnalysisDocument11 pagesThe Effectiveness of Spinal Manipulation in Increasing Muscle Strength in Healthy Individuals A Systematic Review and Meta-Analysisdummyy1256No ratings yet
- Electromyography (EMG) Techniques For The Assessment and Rehabilitation of Motor Impairment Following StrokeDocument3 pagesElectromyography (EMG) Techniques For The Assessment and Rehabilitation of Motor Impairment Following StrokeNazhan HakeemNo ratings yet
- JMD 19083Document3 pagesJMD 19083anton MDNo ratings yet
- Effectiveness of Conventional Therapy & Mirror TherapyDocument4 pagesEffectiveness of Conventional Therapy & Mirror Therapyh4henryNo ratings yet
- CE (Ra1) F (SHU) PF1 (PAB) PN (SHU)Document4 pagesCE (Ra1) F (SHU) PF1 (PAB) PN (SHU)Rizky Meilynno CrisvantiknoNo ratings yet
- 10 3233@BMR-181135Document9 pages10 3233@BMR-181135Ayu SuprabawatiNo ratings yet
- Effects of Motor Imagery On Strength, Range of MotionDocument11 pagesEffects of Motor Imagery On Strength, Range of Motionseroxat2005No ratings yet
- Body Schema Casale2009Document6 pagesBody Schema Casale2009Carlos Esteban Lopez GocheNo ratings yet
- CimtDocument24 pagesCimtmadhu S MNo ratings yet
- Journal of Traditional and Complementary MedicineDocument6 pagesJournal of Traditional and Complementary MedicineLuana GomesNo ratings yet
- Effectiveness of Repetitive Magnetic Stimulation IDocument4 pagesEffectiveness of Repetitive Magnetic Stimulation I29kgcfgqw4No ratings yet
- Naclerio2019 Article EffectivenessOfCombiningMicrocDocument13 pagesNaclerio2019 Article EffectivenessOfCombiningMicrocAna SandovalNo ratings yet
- Effects of Constraint-Induced Therapy Versus Bilateral Arm Training On Motor Performance, Daily Functions, and Quality of Life in Stroke SurvivorsDocument8 pagesEffects of Constraint-Induced Therapy Versus Bilateral Arm Training On Motor Performance, Daily Functions, and Quality of Life in Stroke SurvivorswahyonoNo ratings yet
- MineDocument13 pagesMineZahra Faras SukmaNo ratings yet
- 2 Ijmtst0810098Document6 pages2 Ijmtst0810098Vijay MuniNo ratings yet
- The Effect of Somatosensory Input Byapplication of Kinesiotaping Over Wrist in Subacute and Chronic Stroke PatientsDocument3 pagesThe Effect of Somatosensory Input Byapplication of Kinesiotaping Over Wrist in Subacute and Chronic Stroke PatientsIJAR JOURNALNo ratings yet
- The Effect of Muscle Energy Technique On HeadacheDocument10 pagesThe Effect of Muscle Energy Technique On HeadacheDavid FehertyNo ratings yet
- Pagé-Descarreaux2019 Article EffectsOfSpinalMDocument14 pagesPagé-Descarreaux2019 Article EffectsOfSpinalMdavid ioanaNo ratings yet
- Fnbot 17 1161187Document13 pagesFnbot 17 1161187Anh HuyNo ratings yet
- TensDocument9 pagesTensRiri NandaNo ratings yet
- A Comparative Study of Thai Massage and Muscle Energy - 2021 - Journal of BodywoDocument7 pagesA Comparative Study of Thai Massage and Muscle Energy - 2021 - Journal of BodywoDmytro ChopovskyiNo ratings yet
- Terapia Do Espelho Na Fratura de RadioDocument11 pagesTerapia Do Espelho Na Fratura de RadiodanfisiofoxNo ratings yet
- 0308022620904339Document7 pages0308022620904339sebastian gallegosNo ratings yet
- 2ACLRehabilitationCitedRef4 09Document5 pages2ACLRehabilitationCitedRef4 09richy2hotNo ratings yet
- Rehabilitation of Arm Function After Stroke. Literature ReviewDocument25 pagesRehabilitation of Arm Function After Stroke. Literature ReviewMarius DomnicaNo ratings yet
- Journal of Yoga & Physical TherapyDocument4 pagesJournal of Yoga & Physical Therapykhadesakshi55No ratings yet
- Manual Therapy in The Treatment of Carpal Tunnel Syndrome in Diabetic Patients: A Randomized Clinical TrialDocument7 pagesManual Therapy in The Treatment of Carpal Tunnel Syndrome in Diabetic Patients: A Randomized Clinical TrialHerwanda PrasetyoNo ratings yet
- Manual of Vibration Exercise and Vibration TherapyFrom EverandManual of Vibration Exercise and Vibration TherapyJörn RittwegerNo ratings yet
- Atlas of Surgical Therapy for Migraine and Tension-Type HeadacheFrom EverandAtlas of Surgical Therapy for Migraine and Tension-Type HeadacheEdoardo RaposioNo ratings yet
- Man Overboard StoryDocument9 pagesMan Overboard StorySaud PathiranaNo ratings yet
- Rocks and Minerals WorksheetDocument4 pagesRocks and Minerals WorksheetPwiladNo ratings yet
- CP Form 1Document14 pagesCP Form 1HazelBitagaNo ratings yet
- BR StoCast Brick EN Web S909Document8 pagesBR StoCast Brick EN Web S909ivanbartoNo ratings yet
- Practical Guide To Dispersing AgentsDocument32 pagesPractical Guide To Dispersing AgentsGABRIEL ANGELO SANTOSNo ratings yet
- Gomco 6003 Maintenance and Service ManualDocument25 pagesGomco 6003 Maintenance and Service ManualBerenice CastellanosNo ratings yet
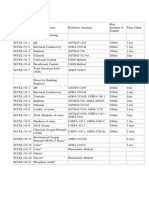
- Water, Soi & Aggregate Testing StandardsDocument2 pagesWater, Soi & Aggregate Testing StandardsSanjeewani Disna JayamaliNo ratings yet
- Danika Sanders Student Teacher ResumeDocument2 pagesDanika Sanders Student Teacher Resumeapi-496485131No ratings yet
- Itinerary Trip Korea-JapanDocument9 pagesItinerary Trip Korea-JapanDiana KamaliyahNo ratings yet
- Information Sheet 7.1-1 Regulations On Safety, Health and Hygiene - MergedDocument159 pagesInformation Sheet 7.1-1 Regulations On Safety, Health and Hygiene - MergedMæbēTh CuarterosNo ratings yet
- EEE 4227: Power Electronics: InvertersDocument52 pagesEEE 4227: Power Electronics: InvertersMd. Abu Hossain MahadyNo ratings yet
- 101 Negativity KillerDocument30 pages101 Negativity KillerAdeline FamousNo ratings yet
- Dropped Nucleus ManagementDocument32 pagesDropped Nucleus ManagementNiloy Basak100% (2)
- Vacuum and Pressure Gauges For Fire Proteccion System 2311Document24 pagesVacuum and Pressure Gauges For Fire Proteccion System 2311Anonymous 8RFzObvNo ratings yet
- New Inside Out Pre-Intermediate Unit 11 Test: Part ADocument5 pagesNew Inside Out Pre-Intermediate Unit 11 Test: Part ARadostina KatsarovaNo ratings yet
- Ijims 2017 105Document7 pagesIjims 2017 105Marcos HoilNo ratings yet
- Chufamix Recipe Book EngDocument100 pagesChufamix Recipe Book Eng600klaraNo ratings yet
- 10th STD FL English Notes 2021-22Document104 pages10th STD FL English Notes 2021-22Niharika knNo ratings yet
- User Manual: Easylogic™ Dm6000H / Dm6200H SeriesDocument50 pagesUser Manual: Easylogic™ Dm6000H / Dm6200H SeriesLucio SalesNo ratings yet
- Self-Learning Home Task (SLHT) : Nervous System As Well As Cognition. The Complexity of The Brain Is ExtremelyDocument7 pagesSelf-Learning Home Task (SLHT) : Nervous System As Well As Cognition. The Complexity of The Brain Is ExtremelySalagmaya ESNo ratings yet
- Tech-Venting HCL TanksDocument2 pagesTech-Venting HCL TanksDHAVALESH AMNo ratings yet
- A Study To Evaluate The Effectiveness of Patterned Breathing Technique On Pain During First Stage of Labour Among Primigravida Mothers Admitted in Selected Hospital at MoradabadDocument17 pagesA Study To Evaluate The Effectiveness of Patterned Breathing Technique On Pain During First Stage of Labour Among Primigravida Mothers Admitted in Selected Hospital at MoradabadEditor IJTSRDNo ratings yet
- Prescription WritingDocument26 pagesPrescription WritingShaHiL HuSsAinNo ratings yet
- White Coal: Best From Waste: W. K. Pokale, S. R. Warhate, H. R. Dhanbar, R. R. Sharma and G. P. DatirDocument4 pagesWhite Coal: Best From Waste: W. K. Pokale, S. R. Warhate, H. R. Dhanbar, R. R. Sharma and G. P. Datirsai kuberNo ratings yet
- MP CW2201SPF Boletin 665Document2 pagesMP CW2201SPF Boletin 665Juan Carlos De Leon CoradoNo ratings yet
- TVL Cookery - Q1 - M2Document16 pagesTVL Cookery - Q1 - M2Jovelyn AvilaNo ratings yet
Extra 1
Extra 1
Uploaded by
Jennifer LozanoOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Extra 1
Extra 1
Uploaded by
Jennifer LozanoCopyright:
Available Formats
CLINICAL TRIAL
published: 26 March 2019
doi: 10.3389/fneur.2019.00288
Comparison Between
Movement-Based and Task-Based
Mirror Therapies on Improving Upper
Limb Functions in Patients With
Stroke: A Pilot Randomized
Controlled Trial
Zhongfei Bai 1,2 , Jiaqi Zhang 3 , Ziwei Zhang 1 , Tian Shu 1 and Wenxin Niu 2*
1
Department of Occupational Therapy, Shanghai YangZhi Rehabilitation Hospital (Shanghai Sunshine Rehabilitation Center),
Tongji University School of Medicine, Shanghai, China, 2 Department of Rehabilitation Sciences, Tongji University School of
Medicine, Shanghai, China, 3 Department of Rehabilitation Sciences, The Hong Kong Polytechnic University, Kowloon, Hong
Kong
Edited by:
Nicola Smania, Objective: The aim of this trial was to compare the effect of movement-based mirror
University of Verona, Italy therapy (MMT) and task-based mirror therapy (TMT) on improving upper limb functions
Reviewed by: in patients with stroke.
Paolo Tonin,
Sant’Anna Institute, Italy Methods: A total of 34 patients with sub-acute stroke with mildly to moderately
Domenico Antonio Restivo,
impaired upper limb motor functions. The participants were randomly allocated to
Ospedale Garibaldi, Italy
one of three groups: MMT, TMT, and conventional treatment (CT). The MMT group
*Correspondence:
Wenxin Niu underwent movement-based mirror therapy for around 30 min/day, 5 days/week, for
niu@tongji.edu.cn 4 weeks, whereas the TMT group underwent dose-matched TMT. The CT group
underwent only conventional rehabilitation. The MMT and TMT groups underwent CT
Specialty section:
This article was submitted to in addition to their mirror therapy. Blinded assessments were administered at baseline
Neurorehabilitation, and immediately after the intervention. Upper limb motor functions, measured using
a section of the journal
Frontiers in Neurology
Fugl-Meyer Assessment-upper extremity (FMA-UE), Wolf Motor Function Test (WMFT),
and hand grip strength; upper limb spasticity, measured using the modified Ashworth
Received: 25 January 2019
Accepted: 05 March 2019 scale (MAS); and activities of daily living, measured using the modified Barthel index (MBI).
Published: 26 March 2019
Results: A significant time-by-group interaction effect was noted in FMA-UE. Post-hoc
Citation:
Bai Z, Zhang J, Zhang Z, Shu T and
analysis of change scores showed that MMT yielded a better effect on improving FMA-UE
Niu W (2019) Comparison Between than the other two therapies, at a marginally significant level (P = 0.050 and 0.022,
Movement-Based and Task-Based
respectively). No significant interaction effect was noted in WMFT, hand grip strength,
Mirror Therapies on Improving Upper
Limb Functions in Patients With MAS, and MBI.
Stroke: A Pilot Randomized Controlled
Trial. Front. Neurol. 10:288.
Conclusion: Both MMT and TMT are effective in improving the upper limb function of
doi: 10.3389/fneur.2019.00288 patients with mild to moderate hemiplegia due to stroke. Nevertheless, MMT seems to
Frontiers in Neurology | www.frontiersin.org 1 March 2019 | Volume 10 | Article 288
Bai et al. Movement- and Task-Based Mirror Therapies
be superior to TMT in improving hemiplegic upper extremity impairment. Further studies
with larger stroke cohorts are expected to be inspired by this pilot trial.
Trial registration number: No. ChiCTR1800019043 (http://www.chictr.org.cn/index.
aspx)
Keywords: mirror therapy, task-oriented training, upper limb, stroke, rehabilitation
INTRODUCTION a hybrid MT protocol (9, 10, 18). MMT and TMT were also
described as intransitive and transitive movements in some
Mirror therapy (MT) has been shown to be a useful intervention studies (9, 10). However, a sub-group meta-analysis comparing
for rehabilitation of upper limb functions following stroke, since MMT and TMT was not carried out in the meta-analysis
the first attempt by Altschuler et al. (1). The neural correlate of study (13).
MT remains under investigation. Three main theories explaining Initially, MMT was used for alleviating phantom pain after
the neural mechanism underlying the clinical efficacy of MT have amputation and for treating upper limb hemiplegia after stroke
been proposed (2). (1, 19). Subsequently, the effect of MMT in stroke upper limb
The first theory hypothesizes that the neural correlate of MT rehabilitation has been systematically investigated by many
is the mirror neuron system (MNS), which is defined as a class of clinical trials (14–16, 20). Arya et al. were the first to compare
neurons that fire during action observation and action execution the effects of TMT with those of conventional rehabilitation on
(3). It is assumed that the MNS can be triggered when people upper limb motor recovery after stroke, and they found a superior
are observing mirror visual feedback (MVF) generated in MT effect of TMT (12). The main rationale that Arya et al. mentioned
(4, 5). The affected cortical motor system can be accessed via was that the response of the MNS was better for object-directed
the MNS owing to their functional connections (6). The second actions than for non-object actions (12, 21). In a recent study
theory, supported by several studies with transcranial magnetic comparing the effects of action observation training and MT
stimulation (TMS), suggests that a potential neural mechanism on gait and balance in patients with stroke, the results showed
underlying the effect of MT can be the recruitment of the that action observation training had significantly better effects on
ipsilesional corticospinal pathway. Indeed, many TMS studies the improvement of balance functions than MT (22), indicating
have demonstrated the increment of motor-evoked potentials that action observation may be different from MT in terms of
of the ipsilesional primary motor cortex in participants with their neural mechanisms. In other studies in which TMT was
stroke when viewing MVF (7), which indicates a facilitatory introduced or combined with MMT, the authors did not explain
effect of MVF on the ipsilesional corticospinal pathway. The why they employed TMT (9–11).
last theory attributes the effect of MT to the compensation of Thus far, no RCT has systematically investigated the difference
restricted proprioception input from the affected limb and the between the effects of MMT and TMT. Therefore, we aimed to
enhancement of attention toward the paretic upper limb (8), conduct an RCT to directly compare the effect of MMT and TMT,
which may contribute to the reduction of the learned non-use in on improving hemiplegic upper limb motor functions, spasticity,
patients with stroke (1). and ADLs, in a group of patients with stroke.
A substantial number of randomized controlled trials (RCTs)
have demonstrated that MT is useful in improving upper limb
METHODS
functions after stroke (9–12). A recently published meta-analytic
review identified a moderate level of evidence supporting the Study Design and Procedure
effects of MT on improving upper limb motor functions (Hedges’ This study was designed as an assessor-blinded RCT. A computer
g = 0.47) and activities of daily living (ADLs) (Hedges’ g = random-number generator was used to generate the random
0.48) in patients with stroke (13). In the meta-analysis (13), sequence for group allocation. All participants were informed
the heterogeneity of conducting MT was obvious across studies. about the purpose and procedures of this study and provided
One major category of MT is movement-based MT (MMT), signed informed written consent before their participation. An
in which participants practice simple movements such as wrist investigator who was blinded to patient selection kept the
flexion and extension, or finger flexion and extension, with random sequence and allocated the participants to one of
their unaffected hands when viewing the MVF generated by three groups: MMT, TMT, or conventional treatment (CT), at
a physical mirror placed at their mid-sagittal plane (14–16). a 1:1:1 ratio. Three assessors and four occupational therapists
Another category of MT is task-based MT (TMT), in which who performed the outcome measurements and intervention,
participants perform specific motor tasks with their unaffected respectively, were trained by a senior occupational therapist in
hands, such as squeezing sponges, placing pegs in holes, and stroke rehabilitation before the study. The same assessor (one of
flipping a card, while they are viewing the MVF (12, 17). In some three) carried out the pre- and post-test assessments for the same
studies, researchers applied MMT in the first few sessions and participant. All assessors were blinded to the group allocation.
subsequently applied TMT in the following sessions, constituting Blinding of the occupational therapists providing interventions
Frontiers in Neurology | www.frontiersin.org 2 March 2019 | Volume 10 | Article 288
Bai et al. Movement- and Task-Based Mirror Therapies
and of the participants were impossible because of the nature of the reflective surface. Thereby, the participants were asked to
of MT. view the reflected upper limbs in the mirror instead of their real
The ethical application of this study was approved by upper limb.
the Research Committee of Shanghai YangZhi Rehabilitation Once the training started, the participants were asked to
Hospital (Shanghai Sunshine Rehabilitation Center, reference no. perform some simple movements with the affected upper limb,
YZ2016-021). This study was retrospectively registered in the such as (1) finger tapping, (2) griping and releasing, (3) wrist
Chinese Clinical Trial Registry (no. ChiCTR1800019043). ulnar and radial derivations, (4) wrist extension and flexion,
(5) forearm pronation and supination, (6) elbow extension and
Participant Recruitment flexion, (7) moving the affected arm from the middle position to
All participants were recruited from a rehabilitation hospital the lateral side, and (8) lifting the hand up and returning it to
between June 7, 2016, and April 11, 2018. The participants were the table.
referred for this study by their occupational therapists in charge. During the practices with the unaffected arm, the participants
A total of 95 post-stroke patients were screened. were instructed to move their affected arm synchronically while
Participants who met all of the following criteria were viewing the mirror. Each movement was repetitively performed
included: (1) a first-ever unilateral ischaemic or haemorrhagic for 3–4 min, with a total of 30 min for 1 MMT session. A 30-s
cerebrovascular accident with onset between 1 and 6 months; break was allowed intermittently when changing the movements.
(2) mild to moderate motor impairment, level 3 to 5 in the The task-oriented training for upper limb motor function and
Functional Test for the Hemiplegic Upper Extremity (23); (3) ADL training was conducted in the remaining 1 h, which was the
mild to moderate degree of spasticity in all joints of the same as that in the CT group.
affected upper limb; and (4) sufficient cognitive ability to follow The treatment dose of the MMT group was similar to that of
instructions (Mini-mental State Examination score >24). the CT group: 5 days/week, for a total of 4 weeks between the pre-
Patients who met any of the following criteria were excluded: test and post-test. After the post-test, the participants underwent
(1) participation in another drug or experimental project within the same training as the CT group until discharge.
3 months; (2) aphasia; (3) serious unilateral neglect (Star
Cancellation Test ≤ 44/54) or visual field deficiency; (4) any Interventions for the TMT Group
other comorbid neurological diseases except for stroke; and (5) All procedures and setup for the TMT training were the same
diagnosis of any other neuromuscular or orthopedic disease in as those for the MMT training. However, the upper limb
the upper extremities. movements performed in TMT were tasks instead of simple
movements. Six tasks were performed with the affected hand
Interventions for the CT Group during TMT, including (1) transferring small cubes from the
All patients in the CT group underwent multi-disciplinary middle position to the lateral side, (2) placing pegs in holes
rehabilitation training, including customary physiotherapy and and taking them out, (3) turning over paper cards, (4) placing
occupational therapy. The physiotherapy intervention, lasting for steel needles in holes, (5) stacking blocks, and (6) putting cups
1–2 h/day, focused on the patients’ lower limb motor function on a shelf. During performing the tasks with the unaffected
and ambulation. Usually, physiotherapists applied muscle hand, the participants were instructed to move their affected
stretching before active motor training. Moreover, intensive arm synchronically in the same way while viewing the mirror.
training for ambulation, consisting of dynamic walking balance Each task should be performed for at least 4 min, with a total of
and gait patterns, was provided for the included participants. For 30 min for one TMT session. The participants could have a 30-
occupational therapy intervention, the participants underwent s break intermittently when changing tasks. The training in the
1.5 h of training, including customary upper limb functional remaining 1 h and the dose were the same as those in the CT
training and ADL training. In customary upper limb functional group, 5 days per week, for a total of 4 weeks between the pre-
training, the primary principle was to apply individual task- test and post-test. After the post-test, the participants underwent
oriented training for the affected arms to enhance muscle the same training as the CT group until discharge.
strength, endurance, coordination, and functional use.
All participants underwent the interventions 5 days/week, Outcome Measures
for a total of 4 weeks between the pre-test and post-test. After Pre-tests were conducted 1 day before the initiation of
the post-intervention assessment, they underwent CT as usual interventions, and post-tests were conducted 1 day after the
until discharge. completion of all intervention sessions. The primary outcomes
were upper limb motor impairment, measured using the Fugl-
Interventions for the MMT Group Meyer Assessment-upper extremity (FMA-UE), and upper limb
Participants in the MMT group underwent the same motor functional performance, measured using the Wolf Motor
physiotherapy as that in the CT group. During the MMT Function Test (WMFT). The FMA-UE includes 33 items
training, the participants were instructed to sit on a chair in front assessing movement, coordination, and reflex actions of the
of a table. A mirror on the table was positioned perpendicular shoulder, elbow, forearm, wrist, and hand joints of the paretic
to the participants. All jewelleries were removed from the arm. Each item consists of a 3-point scale (0, 1, and 2), with a total
unaffected arms, and the affected hand was positioned behind maximum score of 66. The FMA-UE has excellent inter-rater
the mirror, whereas the unaffected hand was placed in the front reliability (intra-class correlation coefficient [ICC] > 0.95) and
Frontiers in Neurology | www.frontiersin.org 3 March 2019 | Volume 10 | Article 288
Bai et al. Movement- and Task-Based Mirror Therapies
test-retest reliability (ICC > 0.95) (24). The minimal clinically muscle tone during passive soft-tissue stretching, with moderate
important difference (MCID) of FMA-UE is 5.25 (25). The inter-rater (kappa = 0.51) and intra-rater (kappa = 0.60)
WMFT is a tool for evaluating the functional performance of reliabilities (27). The MBI consists of 10 common daily activities,
the hemiplegic upper limb in given tasks. The assessors rated including feeding, bathing, grooming, dressing, bowel control,
the quality of performance by using a 6-point functional ability bladder control, toileting, chair transfer, ambulation, and stair
scale, and the total score was obtained by summing the individual climbing, with excellent inter-rater reliability (kappa > 0.80)
scores of each item. The total score of the WMFT has excellent (28) and concurrent validity (Functional Independence Measure,
inter-rater reliability (ICC = 0.88) and test-retest reliability (ICC r = 0.92) (29).
= 0.95) (26). The grip strength of the affected hand was assessed
with a calibrated Jamar hydraulic hand dynamometer (model Sample Size Calculation
SH5001; Saehan Corp, Masan, Korea). As no study comparing MMT and TMT has been performed, we
The secondary outcomes included the muscle tone of the cannot set an estimated effect size for our sample size calculation.
affected arm (i.e., biceps) and hand (i.e., wrist flexor) and We reviewed all published clinical trials on MT, and the sample
ADLs, measured using the modified Ashworth scale (MAS) and size of most studies ranged from 10 to 20 patients in each group.
modified Barthel index (MBI), respectively. The MAS measures Therefore, we planned to recruit 15 patients in each group for
FIGURE 1 | Flowchart of the study. MMT, movement-based mirror therapy; TMT, task-based mirror therapy; CT, conventional treatment.
Frontiers in Neurology | www.frontiersin.org 4 March 2019 | Volume 10 | Article 288
Bai et al. Movement- and Task-Based Mirror Therapies
this pilot RCT considering the exploratory nature of the present recruit the expected number of patients owing to the limited time
preliminary study. of this trial. The mean age of participants in MMT, TMT, and
CT were 56.08 ± 13.61, 54.36 ± 11.56, and 58.27 ± 15.44 years,
Statistical Analysis respectively. Higher percentage of male patients than female
Data analysis was conducted using SPSS version 23.0 (SPSS Inc., patients were enrolled in all groups, 75.00% for MMT, 90.90% for
Madison, WI, USA). Demographic characteristics and pre-test TMT, and 54.55% for CT. For the type of stroke, ischaemic stroke
scores were compared using analysis of variance (ANOVA) for is more common than haemorrhagic stroke, 75.00% for MMT,
continuous and ordinal data, or Fisher’s exact test for categorical 63.64% for TMT, 81.81% for CT. The time after stroke onset
data. Two-way repeated-measures ANOVA, with time effect, in CT group is higher than MMT and TMT, but the statistical
group effect, and time-by-group interaction effect, was used analysis was not significant (P = 0.19). More comparisons of the
to assess within-group and between-group differences. If any demographic characteristics and pre-test scores are presented in
significant difference was noted in the pre-test score of any Table 1. There were no significant differences among the three
dependent variable, one-way analysis of covariance with the groups in demographic characteristics and baseline assessments.
pre-test score as covariate was employed instead. The level of Table 2 shows the descriptive data and statistical analysis of
significance was set at P < 0.05 (2-tailed). Post-hoc analysis the patients’ functional outcomes. With respect to our primary
was performed when any significant interaction effect was noted outcomes, all patients showed significant improvement in FMA-
in two-way repeated ANOVA, by comparing all pairs of mean UE (F = 44.85, P < 0.001), WMFT (F = 40.69, P < 0.001),
change scores between groups by using one-way ANOVA with and grip strength (F = 13.22, P = 0.001), as indicated by
pairwise comparisons. Bonferroni correction was used in post- the significant time effects. Only 1 significant time-by-group
hoc analysis to avoid the inflation of type I errors. The level of interaction effect was noted in FMA-UE (F = 3.44, P = 0.045).
significance was set at P < 0.017 (0.05/3; 3 = number of paired Post-hoc analysis showed that the change score of FMA-UE in
comparisons) after Bonferroni correction. the MMT group was significantly higher than that in the TMT
and CT groups (P = 0.050 and 0.022, respectively). However,
RESULTS they did not survive a Bonferroni correction at a significance
level of 0.017 (Figure 2). The number of participants who
The patient recruitment process is presented in Figure 1. From a exceeded the MCID of FMA-UE was 10 (83.3%), 5 (45.5%), and
pool of 95 patients with sub-acute stroke, a total of 34 inpatients 4 (36.3%) in the MMT, TMT, and CT groups, respectively. Both
(MMT = 12, TMT = 11, and CT = 11) were included in the the MMT and TMT groups tended to yield a higher change
present study. No patient dropped out from this trial. We cannot score of WMFT than the CT group. However, post-hoc analysis
TABLE 1 | Comparisons of demographic characteristics and baseline assessments.
MMT (n = 12) TMT (n = 11) CT (n = 11) F or X2 P-value
DEMOGRAPHICS
Age (years) 56.08 (13.61) 54.36 (11.56) 58.27 (15.44) 0.23 0.80
Male sex, n (%) 9 (75.00%) 10 (90.90%) 6 (54.55%) 3.54 0.17
STROKE CHARACTERISTICS
Time after stroke (days) 61.92 (35.35) 60.00 (44.41) 93.45 (59.75) 1.76 0.19
Side of hemiplegia
Left, n (%) 6 (50.00%) 3 (27.27%) 6 (54.55%) 1.91 0.47
Right, n (%) 6 (50.00%) 8 (72.72%) 5 (45.45%)
TYPE OF STROKE
Ischaemic, n (%) 9 (75.00%) 7 (63.64%) 9 (81.81%) 0.99 0.72
Haemorrhagic, n (%) 3 (25.00%) 4 (36.36%) 2 (18.18%)
Brunnstrom stage (arm) 3.25 (0.62) 3.55 (1.04) 3.00 (0.45) 1.50 0.24
Brunnstrom stage (hand) 3.42 (1.24) 3.64 (1.75) 4.09 (0.94) 0.74 0.49
FMA-UE 34.25 (12.21) 37.55 (14.19) 35.36 (10.62) 0.21 0.81
WMFT 29.08 (7.38) 34.55 (9.45) 26.09 (9.72) 2.56 0.09
Grip strength 4.30 (3.43) 5.37 (5.93) 4.59 (5.46) 0.14 0.87
MBI 66.25 (17.73) 60.45 (18.36) 62.27 (16.49) 0.33 0.72
MAS (arm) 1.29 (0.26) 1.18 (0.50) 1.05 (0.61) 0.76 0.48
MAS (hand) 1.04 (0.58) 0.86 (0.60) 1.00 (0.59) 0.28 0.76
Values are represented as n (%) or mean (standard deviation). MMT, movement-based mirror therapy; TMT, task-based mirror therapy; CT, conventional treatment; FMA-UE, Fugl-Meyer
Assessment-upper extremity; WMFT, Wolf Motor Function Test; MBI, modified Barthel index; MAS: modified Ashworth scale.
Frontiers in Neurology | www.frontiersin.org 5 March 2019 | Volume 10 | Article 288
Bai et al. Movement- and Task-Based Mirror Therapies
Between-group interaction
showed that the comparisons were not significant (P = 0.246 and
Values are represented as mean (standard deviation). MMT, movement-based mirror therapy; TMT, task-based mirror therapy; CT, conventional treatment; FMA-UE, Fugl-Meyer Assessment-upper extremity; WMFT, wolf motor function
P-value
0.045#
0.086, respectively).
0.213
0.428
0.090
0.316
0.901
All groups showed significant improvement in MBI, as
indicated by a significant time effect (F = 57.29, P < 0.001);
however, there was an insignificant time-by-group interaction
effect (F = 2.61, P = 0.090). A significant time effect was noted
F-value
0.104
3.44
1.63
0.87
2.61
1.20
in MAS (hand) (F = 5.64, P = 0.024) but not in MAS (arm)
(F= 0.14, P = 0.714). However, no significant time-by-group
interaction effect was noted in MAS (arm).
Mean difference
−0.18 (0.51)
4.36 (3.44)
4.73 (4.90)
1.65 (4.81)
8.18 (8.15)
0.18 (0.68)
DISCUSSION
CT (n = 11)
The current pilot RCT is the first study to systematically
39.73 (11.79)
30.82 (12.71)
70.45 (19.93)
6.25 (9.42)
1.23 (0.68)
0.81 (0.68)
Post-test
investigate the differential effects of MMT and TMT on
improving motor impairment and functional performance in
patients with sub-acute stroke. Upper limb motor impairments
refer to problems in upper limb motor function and structure,
35.36 (10.62)
62.27 (16.49)
such as limited upper limb movement, whereas upper limb
26.09 (9.72)
4.59 (5.46)
1.05 (0.61)
1.00 (0.59)
Pre-test
functional performance is defined as the ability to perform a
task or action with the upper limbs (30). Our results suggested
that MMT seemed to be better than TMT in terms of improving
hemiplegic upper limb motor impairment, as indicated by
Mean difference
the FMA-UE, among patients with sub-acute stroke. A higher
18.18 (11.46)
−0.09 (0.62)
−0.27 (0.85)
10.00 (6.50)
5.27 (4.69)
4.04 (3.13)
proportion of participants who exceeded the MCID of FMA-
UE were noted in the MMT group (83.3%) than in the TMT
(45.5%) and CT (36.3%) groups. However, upper limb motor
functional performance, grip strength, ADL, and upper limb
TMT (n = 11)
spasticity changed at similar rates across all groups. The effects
42.82 (13.48)
44.55 (14.17)
78.64 (12.06)
9.41 (7.16)
1.09 (0.63)
0.59 (0.58)
Post-test
of TMT were not significantly different from those of CT, which
was against our expectation. We found that TMT tended to gain
a higher change score of the WMFT than the CT group indicated
by a very low P-value (P = 0.086). The potential reason for
TABLE 2 | Difference in outcome measurements between groups at pre- and post-test.
37.55 (14.19)
60.45 (18.36)
34.55 (9.54)
not finding significance was our small sample size. Our sample
5.37 (5.93)
1.18 (0.51)
0.86 (0.60)
Pre-test
size calculation for a future study indicated that 23 patients in
each group are required to gain a significant difference between
TMT and CT in the WMFT at a Bonferroni corrected α error
Test; MBI, modified Barthel index; MAS, modified Ashworth Scale. # P < 0.05.
probability of 0.017 and a power of 0.8.
Mean difference
13.75 (10.90)
Our results of MMT were line with early studies examining the
−0.21 (0.54)
−0.29 (0.40)
10.17 (7.88)
8.17 (8.76)
2.41 (4.77)
effects of MMT in patients with stroke. Previous researchers did
not propose the concepts of TMT and MMT, but we can classify
them into MMT or TMT according to the concepts we proposed.
In early studies (15, 16), their MMT protocols were shown
MMT (n = 12)
effective in motor impairment which was in line with our results.
44.42 (12.89)
37.25 (10.91)
80.00 (13.48)
6.71 (5.19)
1.08 (0.56)
0.75 (0.45)
Post-test
Particularly, in the study by Lee et al. (15), the characteristics
of participants, sample size and treatment protocols of both
experimental and control groups were consistent with ours.
Although our results supported the superior effects of MMT in
34.25 (12.21)
66.25 (17.73)
29.08 (7.38)
4.30 (3.43)
1.29 (0.26)
1.00 (0.59)
improving motor impairment, these did not support the effects
Pre-test
of MMT in improving functional performance. A previous study
found that MMT was also more effective than sham MT in
improving functional performance in patients with acute stroke,
<1 month since stroke onset (16). Because of the heterogenicity
Grip strength
MAS (hand)
MAS (arm)
of participants and treatment protocol of control group across
FMA-UE
WMFT
studies (16), we cannot draw a firm conclusion about the effects
MBI
of MMT in functional performance.
Frontiers in Neurology | www.frontiersin.org 6 March 2019 | Volume 10 | Article 288
Bai et al. Movement- and Task-Based Mirror Therapies
FIGURE 2 | The comparisons in all outcome measures across the three groups. MMT, movement-based mirror therapy; TMT, task-based mirror therapy; CT,
conventional treatment; FMA-UE, Fugl-Meyer Assessment-upper extremity; WMFT, wolf motor function test; MBI, modified Barthel index; MAS, modified Ashworth
Scale.
For the effects of TMT in motor impairment, our result did functional performance (i.e., WMFT) in patients with sub-acute
not support its superior effects compared to CT, which was not stroke. However, further clinical studies are needed to confirm
consistent with other two studies (12, 17). In these two studies, the preliminary findings.
they recruited patients with stroke more than 6 months since When interpreting the differential effects of MMT and TMT in
onset, while our study included participants in sub-acute stage. stroke rehabilitation, the nature of these two MT protocols needs
Therefore, we may postulate that the time since stroke is an to be considered. The reasons to recommend the application of
essential mediator for the effects of TMT in improving motor TMT may include the functional preference of the assumed MNS.
impairment. In addition, although 4-week interventions were Previous evidence has shown that the assumed MNS responds
used in most of the previous MT studies (31), Arya et al. (12) more intensively to object-directed action observation than to
implemented the TMT protocol for 8 weeks. Therefore, a longer non-object action observation (21), because more information
intervention may reveal the potential benefits of TMT on upper from objects for action recognition can be derived by the observer
limb motor impairment, in the case that patients become adapted (32, 33). Therefore, it can be hypothesized that TMT may have a
to mirror-based motor practice. Moreover, participants in Arya superior effect to MMT in triggering the assumed MNS, thereby
et al. (12) had more severe hemiplegia (mean of FMA-UE: 19.71) facilitating the cortical motor system of patients with stroke.
than ours (mean of FMA-UE: 37.55). Therefore, we cannot draw In our study, we observed a phenomenon during TMT, which
a firm conclusion of TMT in motor impairment due to these is illustrated in Figure 3. During the training, the participants
heterogeneities. Meanwhile, although we only observed the effect continuously exhibited the process of “fault and correction”
favoring MMT over TMT in terms of improving upper limb owing to the increased complexity when performing the tasks
motor impairment (i.e., FMA-UE), we cannot underestimate the in MT. The source of the increased complexity was mainly
effect of TMT. We found that TMT, but not MMT, tended to the mirrored spatial location. In the mirrored space, the spatial
yield a superior effect to that of CT on enhancing upper limb relationship among objects is opposite relative to real objects.
Frontiers in Neurology | www.frontiersin.org 7 March 2019 | Volume 10 | Article 288
Bai et al. Movement- and Task-Based Mirror Therapies
FIGURE 3 | An example of the process of “fault and correction.” The given task is that participants are required to transfer an object placed in the No. 3 hole (in
orange color) to the No. 2 hole (Step 1). However, participants usually move the object to the No. 4 hole when they are viewing the mirror reflection (Step 2). Then,
participants realize the fault and transfer the object it to the No. 2 hole (Steps 3, 4).
Therefore, the increased complexity requires patients with stroke results may be difficult to generalize to other stroke cohorts, such
to manipulate their healthy hands carefully and may be the as community-dwelling stroke survivors. Third, we were not able
source of differential effects in motor impairment and functional to conduct follow-up assessment to observe the durability of the
performance. We must acknowledge that, based on the present training effect, as the length of hospitalization in our medical unit
clinical study, it remains difficult to explain the differential neural was limited.
mechanisms underlying MMT and TMT. Further neuroscientific
investigations are needed to elucidate the potential differential
effect of MMT and TMT on modulating the cortical activity of the CONCLUSIONS
motor areas and the potential lateralization change of activation
pattern between the left and right hemispheres when receiving Both MMT and TMT are effective in improving the upper
different forms of MVF. limb function of patients with mild to moderate hemiplegia due
to stroke. Nevertheless, MMT seems to be superior to TMT
in improving hemiplegic upper extremity motor impairment.
LIMITATIONS Further studies with larger stroke cohorts are expected to be
inspired by this pilot trial.
Our study is not free of limitations. First, our recruited sample
did not reach our expected size. The marginally significant
results may have resulted from the limited power. Further studies DATA AVAILABILITY
with larger sample sizes are needed to confirm our preliminary
findings. Second, as our participants were limited to hospitalized All datasets generated for this study are included in the
patients with stroke with mild to moderate hemiplegia, our manuscript and/or the supplementary files.
Frontiers in Neurology | www.frontiersin.org 8 March 2019 | Volume 10 | Article 288
Bai et al. Movement- and Task-Based Mirror Therapies
AUTHOR CONTRIBUTIONS FUNDING
All authors were involved in drafting the article or revising This work was supported by the Fundamental Research Funds for
it critically for important intellectual content, and all authors the Central Universities (No. 22120180401) and Research Project
approved the final version for submission. ZB was responsible of Shanghai Disabled Person’ Federation (2016).
for the conception, organization of the research project, drafting
the manuscript, and critically reviewing the statistical analysis. ACKNOWLEDGMENTS
JZ was responsible for drafting the manuscript, statistical
analysis, and interpretation. ZZ and TS were responsible for The authors would like to thank all patients with stroke who
the organization and execution. WN was also responsible for participated in this study. We also would like to thank Minxia
study design, statistical analysis, and critically reviewing for Jin, Feifei Zhu, Xiaojin Xu, and Ting He who were responsible
the manuscript. for the assessments and intervention in this study.
REFERENCES controlled trial. Neurorehabil Neural Repair. (2009) 23:209–17.
doi: 10.1177/1545968308324786
1. Altschuler EL, Wisdom SB, Stone L, Foster C, Galasko D, Llewellyn DM, 15. Lee MM, Cho HY, Song CH. The mirror therapy program enhances
et al. Rehabilitation of hemiparesis after stroke with a mirror. Lancet. (1999) upper-limb motor recovery and motor function in acute stroke
353:2035–6. doi: 10.1016/S0140-6736(99)00920-4 patients. Am J Phys Med Rehabil. (2012) 91:689–96; quiz: 697–700.
2. Shih TY, Wu CY, Lin KC, Cheng CH, Hsieh YW, Chen CL, et al. Effects of doi: 10.1097/PHM.0b013e31824fa86d
action observation therapy and mirror therapy after stroke on rehabilitation 16. Yavuzer G, Selles R, Sezer N, Sütbeyaz S, Bussmann JB, Köseoglu F,
outcomes and neural mechanisms by MEG: study protocol for a randomized et al. Mirror therapy improves hand function in subacute stroke: a
controlled trial. Trials. (2017) 18:459. doi: 10.1186/s13063-017-2205-z randomized controlled trial. Arch Phys Med Rehabil. (2008) 89:393–8.
3. Brunner IC, Skouen JS, Ersland L, Grüner R. Plasticity and response to doi: 10.1016/j.apmr.2007.08.162
action observation: a longitudinal FMRI study of potential mirror neurons in 17. Kim K, Lee S, Kim D, Lee K, Kim Y. Effects of mirror therapy combined with
patients with subacute stroke. Neurorehabil Neural Repair. (2014) 28:874–84. motor tasks on upper extremity function and activities daily living of stroke
doi: 10.1177/1545968314527350 patients. J Phys Ther Sci. (2016) 28:483–7. doi: 10.1589/jpts.28.483
4. Bartur G, Pratt H, Dickstein R, Frenkel-Toledo S, Geva A, 18. Thieme H, Bayn M, Wurg M, Zange C, Pohl M, Behrens J. Mirror
Soroker N. Electrophysiological manifestations of mirror visual therapy for patients with severe arm paresis after stroke–a randomized
feedback during manual movement. Brain Res. (2015) 1606:113–24. controlled trial. Clin Rehabil. (2013) 27:314–24. doi: 10.1177/026921551
doi: 10.1016/j.brainres.2015.02.029 2455651
5. Bartur G, Pratt H, Frenkel-Toledo S, Soroker N. Neurophysiological effects of 19. Ramachandran VS, Rogersramachandran D, Cobb S. Touching the phantom
mirror visual feedback in stroke patients with unilateral hemispheric damage. limb. Nature. (1995) 377:489–90. doi: 10.1038/377489a0
Brain Res. (2018) 1700:170–80. doi: 10.1016/j.brainres.2018.09.003 20. Michielsen ME, Selles RW, van der Geest JN, Eckhardt M, Yavuzer G, Stam
6. Sharma N, Pomeroy VM, Baron JC. Motor imagery: a backdoor HJ, et al. Motor recovery and cortical reorganization after mirror therapy in
to the motor system after stroke? Stroke. (2006) 37:1941–52. chronic stroke patients: a phase II randomized controlled trial. Neurorehabil
doi: 10.1161/01.STR.0000226902.43357.fc Neural Repair. (2011) 25:223–33. doi: 10.1177/1545968310385127
7. Kang YJ, Park HK, Kim HJ, Lim T, Ku J, Cho S, et al. Upper 21. Agnew ZK, Wise RJ, Leech R. Dissociating object directed and non-
extremity rehabilitation of stroke: facilitation of corticospinal excitability object directed action in the human mirror system; implications
using virtual mirror paradigm. J Neuroeng Rehabil. (2012) 9:71. for theories of motor simulation. PLoS ONE. (2012) 7:e32517.
doi: 10.1186/1743-0003-9-71 doi: 10.1371/journal.pone.0032517
8. Michielsen ME, Smits M, Ribbers GM, Stam HJ, van der Geest JN, Bussmann 22. Lee HJ, Kim YM, Lee DK. The effects of action observation training and
JB, et al. The neuronal correlates of mirror therapy: an fMRI study on mirror mirror therapy on gait and balance in stroke patients. J Phys Ther Sci. (2017)
induced visual illusions in patients with stroke. J Neurol Neurosurg Psychiatry. 29:523–6. doi: 10.1589/jpts.29.523
(2011) 82:393–8. doi: 10.1136/jnnp.2009.194134 23. Fong K, Ng B, Chan D, Chan E, Ma D, Au B, et al. Development of
9. Wu CY, Huang PC, Chen YT, Lin KC, Yang HW. Effects of mirror therapy on the Hong Kong version of the functional test for the hemiplegic upper
motor and sensory recovery in chronic stroke: a randomized controlled trial. extremity (FTHUE-HK). Hong Kong J Occupat Ther. (2004) 14:21–9.
Arch Phys Med Rehabil. (2013) 94:1023–30. doi: 10.1016/j.apmr.2013.02.007 doi: 10.1016/S1569-1861(09)70025-7
10. Lin KC, Huang PC, Chen YT, Wu CY, Huang WI. Combining afferent 24. Platz T, Pinkowski C, van Wijck F, Kim IH, di Bella P, Johnson G.
stimulation and mirror therapy for rehabilitating motor function, motor Reliability and validity of arm function assessment with standardized
control, ambulation, and daily functions after stroke. Neurorehabil Neural guidelines for the Fugl-Meyer Test, Action Research Arm Test and Box
Repair. (2014) 28:153–62. doi: 10.1177/1545968313508468 and Block Test: a multicentre study. Clin Rehabil. (2005) 19:404–11.
11. Samuelkamaleshkumar S, Reethajanetsureka S, Pauljebaraj P, Benshamir B, doi: 10.1191/0269215505cr832oa
Padankatti SM, David JA. Mirror therapy enhances motor performance in the 25. Page SJ, Fulk GD, Boyne P. Clinically important differences for the upper-
paretic upper limb after stroke: a pilot randomized controlled trial. Arch Phys extremity Fugl-Meyer Scale in people with minimal to moderate impairment
Med Rehabil. (2014) 95:2000–5. doi: 10.1016/j.apmr.2014.06.020 due to chronic stroke. Phys Ther. (2012) 92:791–8. doi: 10.2522/ptj.
12. Arya KN, Pandian S, Kumar D, Puri V. Task-based mirror therapy 20110009
augmenting motor recovery in poststroke hemiparesis: a randomized 26. Morris DM, Uswatte G, Crago JE, Cook EW III, Taub E. The reliability
controlled trial. J Stroke Cerebrovasc Dis. (2015) 24:1738–48. of the wolf motor function test for assessing upper extremity function
doi: 10.1016/j.jstrokecerebrovasdis.2015.03.026 after stroke. Arch Phys Med Rehabil. (2001) 82:750–5. doi: 10.1053/apmr.
13. Thieme H, Morkisch N, Mehrholz J, Pohl M, Behrens J, Borgetto B, et al. 2001.23183
Mirror therapy for improving motor function after stroke. Cochrane Database 27. Ansari NN, Naghdi S, Arab TK, Jalaie S. The interrater and intrarater
Syst Rev. (2018) 7:Cd008449. doi: 10.1002/14651858.CD008449.pub3 reliability of the Modified Ashworth Scale in the assessment of
14. Dohle C, Pullen J, Nakaten A, Kust J, Rietz C, Karbe H. Mirror muscle spasticity: limb and muscle group effect. NeuroRehabilitation.
therapy promotes recovery from severe hemiparesis: a randomized (2008) 23:231–7.
Frontiers in Neurology | www.frontiersin.org 9 March 2019 | Volume 10 | Article 288
Bai et al. Movement- and Task-Based Mirror Therapies
28. Leung SO, Chan CC, Shah S. Development of a Chinese version of the action knowledge during action observation in fMRI. Front Psychol. (2014)
Modified Barthel Index– validity and reliability. Clin Rehabil. (2007) 21:912– 5:636. doi: 10.3389/fpsyg.2014.00636
22. doi: 10.1177/0269215507077286 33. Chen W, Ye Q, Ji X, Zhang S, Yang X, Zhou Q, et al. Mirror neuron
29. Hsueh IP, Lin JH, Jeng JS, Hsieh CL. Comparison of the psychometric system based therapy for aphasia rehabilitation. Front Psychol. (2015) 6:1665.
characteristics of the functional independence measure, 5 item Barthel index, doi: 10.3389/fpsyg.2015.01665
and 10 item Barthel index in patients with stroke. J Neurol Neurosurg
Psychiatry. (2002) 73:188–90. doi: 10.1136/jnnp.73.2.188 Conflict of Interest Statement: The authors declare that the research was
30. Santisteban L, Térémetz M, Bleton JP, Baron JC, Maier MA, Lindberg conducted in the absence of any commercial or financial relationships that could
PG. Upper limb outcome measures used in stroke rehabilitation be construed as a potential conflict of interest.
studies: a systematic literature review. PLoS ONE. (2016) 11:e0154792.
doi: 10.1371/journal.pone.0154792 Copyright © 2019 Bai, Zhang, Zhang, Shu and Niu. This is an open-access article
31. Perez-Cruzado D, Merchan-Baeza JA, Gonzalez-Sanchez M, Cuesta-Vargas distributed under the terms of the Creative Commons Attribution License (CC BY).
AI. Systematic review of mirror therapy compared with conventional The use, distribution or reproduction in other forums is permitted, provided the
rehabilitation in upper extremity function in stroke survivors. Aust Occup original author(s) and the copyright owner(s) are credited and that the original
Ther J. (2017) 64:91–112. doi: 10.1111/1440-1630.12342 publication in this journal is cited, in accordance with accepted academic practice.
32. Schubotz RI, Wurm MF, Wittmann MK, von Cramon DY. Objects tell us what No use, distribution or reproduction is permitted which does not comply with these
action we can expect: dissociating brain areas for retrieval and exploitation of terms.
Frontiers in Neurology | www.frontiersin.org 10 March 2019 | Volume 10 | Article 288
You might also like
- Freshwater Aquarium ManualDocument32 pagesFreshwater Aquarium Manualhippong niswantoroNo ratings yet
- A View of The Cell Review PacketDocument7 pagesA View of The Cell Review Packetapi-259727482No ratings yet
- PA-1 Adjusments and Worksheet (Problems)Document5 pagesPA-1 Adjusments and Worksheet (Problems)Safira ChairunnisaNo ratings yet
- FGI Patient Handling and Mobility Assessments 191008Document476 pagesFGI Patient Handling and Mobility Assessments 191008morton1472100% (1)
- Effect of Mirror Therapy Combined With Somatosensory Stimulation On Motor Recovery and Daily Function in Stroke Patients: A Pilot StudyDocument7 pagesEffect of Mirror Therapy Combined With Somatosensory Stimulation On Motor Recovery and Daily Function in Stroke Patients: A Pilot StudyDedi Irawandi Angela NursisNo ratings yet
- Amasyali 2016Document6 pagesAmasyali 2016leandroNo ratings yet
- Effect of Mirror Therapy Combined With Somatosensory Stimulation On Motor Recovery and Daily Function in Stroke Patients: A Pilot StudyDocument7 pagesEffect of Mirror Therapy Combined With Somatosensory Stimulation On Motor Recovery and Daily Function in Stroke Patients: A Pilot Studywanda argeNo ratings yet
- NRC 1729Document9 pagesNRC 1729Laura Michell Carrero GómezNo ratings yet
- The Effectivity of Mirror Therapy On Arm Motoric Improvement in Acute Ischemic StrokeDocument7 pagesThe Effectivity of Mirror Therapy On Arm Motoric Improvement in Acute Ischemic StrokeilyasNo ratings yet
- Mirror Therapy For Motor Function of The Upper Extremity inDocument8 pagesMirror Therapy For Motor Function of The Upper Extremity inilyasNo ratings yet
- MPT Dissertation PPT CorrectedDocument30 pagesMPT Dissertation PPT CorrectedPradeep Kumar BhuvaneshwaranNo ratings yet
- Efficacy of Modified Constraint Induced Movement Therapy in The Treatment of Hemiparetic Upper Limb in Stroke Patients: A Randomized Controlled TrialDocument5 pagesEfficacy of Modified Constraint Induced Movement Therapy in The Treatment of Hemiparetic Upper Limb in Stroke Patients: A Randomized Controlled TrialHaveezhNo ratings yet
- Cerebal PalsyDocument10 pagesCerebal PalsySoffie FitriyahNo ratings yet
- Boake Et Al 2007 Constraint Induced Movement Therapy During Early Stroke RehabilitationDocument11 pagesBoake Et Al 2007 Constraint Induced Movement Therapy During Early Stroke RehabilitationoverhiitshopNo ratings yet
- E000514 FullDocument6 pagesE000514 FullRenan O. Pravatta PivettaNo ratings yet
- Morkisch 2019Document15 pagesMorkisch 2019David Morote VillaNo ratings yet
- Giray 2019Document13 pagesGiray 2019Felix LoaizaNo ratings yet
- Comparing Targeted Thrust Manipulation With General Thrust Manipulation in Patients With Low Back Pain. A General Approach Is As Effective As A Specific One. A Randomised Controlled TrialDocument6 pagesComparing Targeted Thrust Manipulation With General Thrust Manipulation in Patients With Low Back Pain. A General Approach Is As Effective As A Specific One. A Randomised Controlled TrialMilton Ricardo de Medeiros FernandesNo ratings yet
- SimonettiDocument14 pagesSimonettijuanNo ratings yet
- Cjim 11 163Document8 pagesCjim 11 163Nurul Annisa KamalNo ratings yet
- Dry Needling On Biomechanical 2021Document8 pagesDry Needling On Biomechanical 2021Fábio PedraNo ratings yet
- The Efficacy of Muscle Energy TechniquesDocument18 pagesThe Efficacy of Muscle Energy Techniquesmuhammad yaminNo ratings yet
- Dunning James Et AlDocument10 pagesDunning James Et Alapi-290796947No ratings yet
- Arthrogenic Muscle Inhibition After ACL Reconstruction A Scoping Review of The Efficacy of InterventionsDocument11 pagesArthrogenic Muscle Inhibition After ACL Reconstruction A Scoping Review of The Efficacy of InterventionsfilipecorsairNo ratings yet
- Constraint Induced Manual TherapyDocument165 pagesConstraint Induced Manual TherapyPrabhu Chinna Gounder100% (1)
- SHS EMG BiofeedbackDocument16 pagesSHS EMG BiofeedbackPraneeth KumarNo ratings yet
- FonteDocument12 pagesFontejuanNo ratings yet
- Cimt and NDT Proposal-2 AltDocument10 pagesCimt and NDT Proposal-2 Altapi-487111274No ratings yet
- Articulo MIRROR 1Document9 pagesArticulo MIRROR 1Jossie QueralesNo ratings yet
- Constraint Induced Movement TherapyDocument4 pagesConstraint Induced Movement TherapyNikka VentorilloNo ratings yet
- 12 Nadiah Zuhdi 18.0095.T JurnalCIMT StrokeDocument10 pages12 Nadiah Zuhdi 18.0095.T JurnalCIMT StrokeZuhdiNo ratings yet
- 10 Jpts 27 1455Document3 pages10 Jpts 27 1455mustafasacarNo ratings yet
- Mirror Therapy Enhances Motor Performance in The Paretic Upper Limb After Stroke: A Pilot Randomized Controlled TrialDocument6 pagesMirror Therapy Enhances Motor Performance in The Paretic Upper Limb After Stroke: A Pilot Randomized Controlled TrialScientifica EducacionalNo ratings yet
- BMC Neurology: Comparing Unilateral and Bilateral Upper Limb Training: The ULTRA-stroke Program DesignDocument14 pagesBMC Neurology: Comparing Unilateral and Bilateral Upper Limb Training: The ULTRA-stroke Program DesignDharam PandeyNo ratings yet
- The Effectiveness of Spinal Manipulation in Increasing Muscle Strength in Healthy Individuals A Systematic Review and Meta-AnalysisDocument11 pagesThe Effectiveness of Spinal Manipulation in Increasing Muscle Strength in Healthy Individuals A Systematic Review and Meta-Analysisdummyy1256No ratings yet
- Electromyography (EMG) Techniques For The Assessment and Rehabilitation of Motor Impairment Following StrokeDocument3 pagesElectromyography (EMG) Techniques For The Assessment and Rehabilitation of Motor Impairment Following StrokeNazhan HakeemNo ratings yet
- JMD 19083Document3 pagesJMD 19083anton MDNo ratings yet
- Effectiveness of Conventional Therapy & Mirror TherapyDocument4 pagesEffectiveness of Conventional Therapy & Mirror Therapyh4henryNo ratings yet
- CE (Ra1) F (SHU) PF1 (PAB) PN (SHU)Document4 pagesCE (Ra1) F (SHU) PF1 (PAB) PN (SHU)Rizky Meilynno CrisvantiknoNo ratings yet
- 10 3233@BMR-181135Document9 pages10 3233@BMR-181135Ayu SuprabawatiNo ratings yet
- Effects of Motor Imagery On Strength, Range of MotionDocument11 pagesEffects of Motor Imagery On Strength, Range of Motionseroxat2005No ratings yet
- Body Schema Casale2009Document6 pagesBody Schema Casale2009Carlos Esteban Lopez GocheNo ratings yet
- CimtDocument24 pagesCimtmadhu S MNo ratings yet
- Journal of Traditional and Complementary MedicineDocument6 pagesJournal of Traditional and Complementary MedicineLuana GomesNo ratings yet
- Effectiveness of Repetitive Magnetic Stimulation IDocument4 pagesEffectiveness of Repetitive Magnetic Stimulation I29kgcfgqw4No ratings yet
- Naclerio2019 Article EffectivenessOfCombiningMicrocDocument13 pagesNaclerio2019 Article EffectivenessOfCombiningMicrocAna SandovalNo ratings yet
- Effects of Constraint-Induced Therapy Versus Bilateral Arm Training On Motor Performance, Daily Functions, and Quality of Life in Stroke SurvivorsDocument8 pagesEffects of Constraint-Induced Therapy Versus Bilateral Arm Training On Motor Performance, Daily Functions, and Quality of Life in Stroke SurvivorswahyonoNo ratings yet
- MineDocument13 pagesMineZahra Faras SukmaNo ratings yet
- 2 Ijmtst0810098Document6 pages2 Ijmtst0810098Vijay MuniNo ratings yet
- The Effect of Somatosensory Input Byapplication of Kinesiotaping Over Wrist in Subacute and Chronic Stroke PatientsDocument3 pagesThe Effect of Somatosensory Input Byapplication of Kinesiotaping Over Wrist in Subacute and Chronic Stroke PatientsIJAR JOURNALNo ratings yet
- The Effect of Muscle Energy Technique On HeadacheDocument10 pagesThe Effect of Muscle Energy Technique On HeadacheDavid FehertyNo ratings yet
- Pagé-Descarreaux2019 Article EffectsOfSpinalMDocument14 pagesPagé-Descarreaux2019 Article EffectsOfSpinalMdavid ioanaNo ratings yet
- Fnbot 17 1161187Document13 pagesFnbot 17 1161187Anh HuyNo ratings yet
- TensDocument9 pagesTensRiri NandaNo ratings yet
- A Comparative Study of Thai Massage and Muscle Energy - 2021 - Journal of BodywoDocument7 pagesA Comparative Study of Thai Massage and Muscle Energy - 2021 - Journal of BodywoDmytro ChopovskyiNo ratings yet
- Terapia Do Espelho Na Fratura de RadioDocument11 pagesTerapia Do Espelho Na Fratura de RadiodanfisiofoxNo ratings yet
- 0308022620904339Document7 pages0308022620904339sebastian gallegosNo ratings yet
- 2ACLRehabilitationCitedRef4 09Document5 pages2ACLRehabilitationCitedRef4 09richy2hotNo ratings yet
- Rehabilitation of Arm Function After Stroke. Literature ReviewDocument25 pagesRehabilitation of Arm Function After Stroke. Literature ReviewMarius DomnicaNo ratings yet
- Journal of Yoga & Physical TherapyDocument4 pagesJournal of Yoga & Physical Therapykhadesakshi55No ratings yet
- Manual Therapy in The Treatment of Carpal Tunnel Syndrome in Diabetic Patients: A Randomized Clinical TrialDocument7 pagesManual Therapy in The Treatment of Carpal Tunnel Syndrome in Diabetic Patients: A Randomized Clinical TrialHerwanda PrasetyoNo ratings yet
- Manual of Vibration Exercise and Vibration TherapyFrom EverandManual of Vibration Exercise and Vibration TherapyJörn RittwegerNo ratings yet
- Atlas of Surgical Therapy for Migraine and Tension-Type HeadacheFrom EverandAtlas of Surgical Therapy for Migraine and Tension-Type HeadacheEdoardo RaposioNo ratings yet
- Man Overboard StoryDocument9 pagesMan Overboard StorySaud PathiranaNo ratings yet
- Rocks and Minerals WorksheetDocument4 pagesRocks and Minerals WorksheetPwiladNo ratings yet
- CP Form 1Document14 pagesCP Form 1HazelBitagaNo ratings yet
- BR StoCast Brick EN Web S909Document8 pagesBR StoCast Brick EN Web S909ivanbartoNo ratings yet
- Practical Guide To Dispersing AgentsDocument32 pagesPractical Guide To Dispersing AgentsGABRIEL ANGELO SANTOSNo ratings yet
- Gomco 6003 Maintenance and Service ManualDocument25 pagesGomco 6003 Maintenance and Service ManualBerenice CastellanosNo ratings yet
- Water, Soi & Aggregate Testing StandardsDocument2 pagesWater, Soi & Aggregate Testing StandardsSanjeewani Disna JayamaliNo ratings yet
- Danika Sanders Student Teacher ResumeDocument2 pagesDanika Sanders Student Teacher Resumeapi-496485131No ratings yet
- Itinerary Trip Korea-JapanDocument9 pagesItinerary Trip Korea-JapanDiana KamaliyahNo ratings yet
- Information Sheet 7.1-1 Regulations On Safety, Health and Hygiene - MergedDocument159 pagesInformation Sheet 7.1-1 Regulations On Safety, Health and Hygiene - MergedMæbēTh CuarterosNo ratings yet
- EEE 4227: Power Electronics: InvertersDocument52 pagesEEE 4227: Power Electronics: InvertersMd. Abu Hossain MahadyNo ratings yet
- 101 Negativity KillerDocument30 pages101 Negativity KillerAdeline FamousNo ratings yet
- Dropped Nucleus ManagementDocument32 pagesDropped Nucleus ManagementNiloy Basak100% (2)
- Vacuum and Pressure Gauges For Fire Proteccion System 2311Document24 pagesVacuum and Pressure Gauges For Fire Proteccion System 2311Anonymous 8RFzObvNo ratings yet
- New Inside Out Pre-Intermediate Unit 11 Test: Part ADocument5 pagesNew Inside Out Pre-Intermediate Unit 11 Test: Part ARadostina KatsarovaNo ratings yet
- Ijims 2017 105Document7 pagesIjims 2017 105Marcos HoilNo ratings yet
- Chufamix Recipe Book EngDocument100 pagesChufamix Recipe Book Eng600klaraNo ratings yet
- 10th STD FL English Notes 2021-22Document104 pages10th STD FL English Notes 2021-22Niharika knNo ratings yet
- User Manual: Easylogic™ Dm6000H / Dm6200H SeriesDocument50 pagesUser Manual: Easylogic™ Dm6000H / Dm6200H SeriesLucio SalesNo ratings yet
- Self-Learning Home Task (SLHT) : Nervous System As Well As Cognition. The Complexity of The Brain Is ExtremelyDocument7 pagesSelf-Learning Home Task (SLHT) : Nervous System As Well As Cognition. The Complexity of The Brain Is ExtremelySalagmaya ESNo ratings yet
- Tech-Venting HCL TanksDocument2 pagesTech-Venting HCL TanksDHAVALESH AMNo ratings yet
- A Study To Evaluate The Effectiveness of Patterned Breathing Technique On Pain During First Stage of Labour Among Primigravida Mothers Admitted in Selected Hospital at MoradabadDocument17 pagesA Study To Evaluate The Effectiveness of Patterned Breathing Technique On Pain During First Stage of Labour Among Primigravida Mothers Admitted in Selected Hospital at MoradabadEditor IJTSRDNo ratings yet
- Prescription WritingDocument26 pagesPrescription WritingShaHiL HuSsAinNo ratings yet
- White Coal: Best From Waste: W. K. Pokale, S. R. Warhate, H. R. Dhanbar, R. R. Sharma and G. P. DatirDocument4 pagesWhite Coal: Best From Waste: W. K. Pokale, S. R. Warhate, H. R. Dhanbar, R. R. Sharma and G. P. Datirsai kuberNo ratings yet
- MP CW2201SPF Boletin 665Document2 pagesMP CW2201SPF Boletin 665Juan Carlos De Leon CoradoNo ratings yet
- TVL Cookery - Q1 - M2Document16 pagesTVL Cookery - Q1 - M2Jovelyn AvilaNo ratings yet