Professional Documents
Culture Documents
Surface Modification of Polymers For Biomedical Applications
Surface Modification of Polymers For Biomedical Applications
Uploaded by
pcnferreiraOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Surface Modification of Polymers For Biomedical Applications
Surface Modification of Polymers For Biomedical Applications
Uploaded by
pcnferreiraCopyright:
Available Formats
Surface modification of polymers for
biomedical applications
P Alves, P Ferreira and M H Gil
Chemical Engineering Department, University of Coimbra, Portugal
O
ne of the more frequent, expensive
and serious problems facing human Outlines
healthcare is the loss or failure of
organs or tissues. It is in providing solutions l A large number of different materials are used in a wide range of biomedical
to such problems that coating technologies applications for which biocompatibility is essential. In order to combine this with
have much to offer. The medical need for the desired bulk structural properties, it is frequently desirable to apply some form
tissue and organ substitutes can arise from of coating or other surface modification.
trauma, infections, inherited or age-related l Factors involved in the interactions between the body and implants are discussed.
diseases and organ failure.1 The process of cell attachment to surfaces is complex and takes place in several
The theme of biomaterials embraces a stages. Depending on the application, this attachment may be essential or highly
wide range of materials and their undesirable.
applications. Polymers have been l Surface modification may be based on physical methods such as flame treatment,
extensively used as coatings in biomedical corona discharge, UV radiation exposure or laser ablation. Chemical methods include
devices and in the devices themselves, such etching, surface oxidation, hydrolysis, chemical grafting and surface coating. Various
as catheters, heart valves and dialysis aspects and applications of these technologies are considered.
membranes. Many of these polymers were l Surface modification is a very important aspect of the creation of medically viable
originally developed for industrial polymeric and non-polymeric biomaterials and thus the use of coating techniques in
applications but were then adapted for use the creation of biomaterials has been growing over recent decades as they can
as biomaterials, based on their favourable improve the application properties of materials in end uses ranging from catheters
characteristics.2 to endoprostheses and cardiac valves.
The performance of a material in a
biological environment is mainly mediated commonly used as implants, as coatings Surface modification aims to tailor the
by its surface properties and by the and as bulk materials. Their surface surface characteristics of a material for a
combination of physical and mechanical chemical properties are a major factor in specific application without detrimentally
properties required for a specific determining the adhesion of proteins in ‘in affecting the bulk properties. This approach
application, often achieved by appropriate vivo’ systems. This behaviour is directly provides a basis for increasing the success
coating treatments. Among the surface related to the subsequent cellular of implant applications by increasing their
properties that can be achieved by the interactions with the coating/polymer and, service lifetime.
judicious use of coatings, and of utmost therefore, to the material’s
importance with respect to the biocompatibility.
performance, are surface chemical Also, it has to be recognised that if the Surfaces and cell adhesion
structure (such as inherent hydrophilicity), coating is inappropriately chosen,
the presence of functional groups on the When a biomaterial is implanted in a living
pathological microorganisms may easily
surface, (that could initiate organism, several types of interactions are
adhere to the surfaces, causing infection.
interaction/reaction with biological established between the host tissue and the
The incidence of such infections varies
systems, in biological media) and the material and, more specifically, with its
from 1% for hip prostheses up to 100% for
surface morphology (the distribution and surface. These interactions, although
urinary tract catheters and up to 50% in
abundance of specified classified as being normal, may lead, if not
aortic vascular graft infections.4
hydrophilic/hydrophobic regions and the properly controlled, to a failure of the
An infection involves three major steps. implant and in the worst case scenario to
presence of crystalline/amorphous phases) These are microbial adhesion, microbial
and the overall surface topography.3 the host’s death.
proliferation and the formation of a
In order to understand, predict and avoid
bacterial film. To overcome this problem,
such effects, it is important to remember
Factors affecting the choice the surface modification (coating and
that it is not only the effect of the implant
surface deactivation) of the material
of materials on the host’s tissues that should be
substrate has, in the recent past, been one
considered. Another very important factor
of the more widely used and studied
Many polymers, such as the polyolefins, the involved in this tissue-coated biomaterial
approaches to resolving biofouling issues.
polysiloxanes and the polyurethanes are interface is the effect of the host on the
Surface Coatings International Issue 2013/3 1
material and the consequences that such
an interaction might bring about. Several Table 1: Interactions commonly established between a coated biomaterial and a host tissue
effects arising from biomaterial-tissue Local effects Systemic/distant effects
interactions have been reported, and some
are detailed in Table 1. 1. Blood-material interactions (eg protein adsorption, 1. Embolisation (eg thrombus formation, …)
Immediately after implantation of a coagulation, haemolysis, platelet or 2. Hypersensitivity
leukocyte activation, …) 3. Mutagenicity
biomaterial, coated or otherwise,
adsorption of proteins to its surface takes 2. Toxicity 4. Teratogenicity
place. Among these proteins are usually the 3. Inhibition of normal healing (eg encapsulation,
immunoglobulins vitronectin, fibrinogen, foreign body reaction)
and fibronectin. This adsorption 4. Infection
phenomenon is due to the high abundance 5. Carcinogenesis
of these proteins in plasma as well as their
considerable mobility. Protein adsorption to
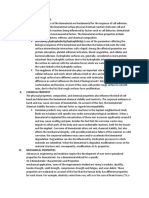
a surface is a highly complex and dynamic Figure 1: Representation of the Vroman effect: after exposure to the physiological medium, small and
process. In fact, with time, the initially abundant proteins (protein A) adsorb and interact with the polymeric surface. These weakly surface-active
adsorbed proteins are displaced by others proteins are subsequently displaced by other larger proteins having a greater affinity with the coated
that are larger and less motile, but have a material.7
more pronounced affinity for the material’s Protein A
surface. This phenomenon is commonly
known as the Vroman effect5 (see Figure 1).
The nature of the proteins’ adherence to
the coated biomaterial surface is a major
factor in influencing the attachment of
posterior cells and their behaviour, such as
the attachment and the activation of
neutrophils (white blood cells),
macrophages and other inflammatory cells.6
Protein adhesion initiates cell Exposure time
adhesion
Once attached to the material, a complex Protein B
Protein
system of communication, initiated by the
displacement
proteins, begins to take place, involving the
release of signals, the attraction of cells
and, finally, the adherence of these cells to
the surface.
The process of cell attachment to a
surface (coated or otherwise) occurs in
three consecutive stages:
l Attachment,
l Spreading and growth, Following this process, filaments of actin in the case of the development of materials
(a protein capable of polymerisation) are for use in tissue engineering), in other
l The formation of focal adhesions and
formed and the cells spread, enhancing cases such processes will result in implant
stress fibres.8
their surface contact area (second stage). failure and the need for removal and
Each of these stages can be recognised in Finally, strong points of attachment, named replacement.
the development of interaction between focal adhesions, are formed. These sites
most non-biological coatings and their work as linkage spots between the fibres of Biofilm formation
substrate. actin and the extracellular medium, via the The most obvious example of undesirable
In the process of cell attachment, the first transmembrane integrins. At the end of this cell adhesion to a material is the case of
stage is initiated by the contact between process, the cell is tightly attached to the bacterial attachment. Bacterial attachment
those integrins (trans-membranar proteins coated surface (see Figure 2). and subsequent spreading on biomaterials
composed of an (alpha) sub-unit and a When coated biomaterials are used, cell (commonly known as infection), results in
(beta) subunit) and the proteins that are on adhesion may come either as an advantage the formation of a secondary coating, a
the coated surface. This phase will result in or as a shortcoming, depending on the biofilm, which is frequently associated with
the integrins becoming activated, a circumstances. While for some applications the failure of implants, as in the case of
phenomenon that includes their clustering it is vital that cells become attached, joint prostheses, heart valves, vascular
and the increase of their affinity towards spread and even divide on the surface, (as catheters and contact lenses.10
the coated surface.9
2 Surface Coatings International Issue 2013/3
which works as an enclosing structure. The
Figure 2: Stages of cell adhesion to a coated surface: attachment, spreading and formation of focal adhesions
spreading of the resultant coating biofilm
and stress fibres9
is mainly due to the release of some
Stage 1 Stage 2 Stage 3 bacteria from the cluster structures, which
Cell attachment Cell spreading Focal adhesion then adhere to the coating surface and
Stress fibres start a new cycle.11
Integrin Actin filaments
Studies concerning the mechanisms of
bacterial adhesion, leading to an
understanding of how to avoid this
drawback, are constantly being updated.
However, the complexity of such processes
and all the factors of relevance (eg material
properties, bacterial strain type and patient
Strength of adhesion condition), makes it a difficult task to
accomplish.
Figure 3: Stages of biofilm development: (1) bacterial attachment to the coated surface; (2) synthesis of As previously mentioned, cell attachment
extracellular matrix; (3) formation of bacterial microcolonies; (4) maturation of biofilm architecture; (5) and consequent cell behaviour involves a
dispersion of bacteria complex set of occurrences which, in turn,
involve processes such as protein
adsorption and intercellular signalling that
Dispersion of bacteria
occur externally to the material. However,
these are fundamentally related to the
properties of the material. In fact, the
surface of the biomaterial is a key factor
determining the biological response and,
Beginning therefore, the biocompatibility, since most
of new biological reactions occur at the surfaces
cycle and interfaces.12
Properties such as the wettability,
chemical composition, porosity,
softness/stiffness, roughness and the
surface charge of the biomaterial, are
highly influential with respect to the effect
1 2 3 4 5 on the physiological environment (see
Figure 4).13 For such reasons, when
designing a biomaterial, all of these factors
Figure 4: Examples of key features of the material’s surface (coated or otherwise) that determine cell must be taken into consideration when
adhesion and spreading, following coating attempting to optimise features that are
related to the overall biocompatibility and
consequences of coating.
Charge Softness Two major strategies have been used by
researchers to increase the overall extent of
biocompatibility of coating compositions.
Wettability Chemical One involves the synthesis of new materials
composition and the other concerns the modification of
the surface of pre-existing materials, for
example by the use of appropriate coating
technologies and pretreatments. Here, some
of the available techniques that are used to
Roughness Porosity enhance biocompatibility are described and
Surface
properties examples of their application are given.
Enhancing biocompatibility
Biofilm formation occurs through several proliferation. Finally, cells begin to Surface modifications
consecutive stages (see Figure 3), starting accumulate in multilayer clusters and to
with the attachment of bacteria to the produce an extracellular matrix (mainly In biomaterials, the surface and bulk
surface, followed by cell-cell adhesion and composed of polysaccharidic species), properties of the coated devices are
Surface Coatings International Issue 2013/3 3
responsible for the success or failure of the
Figure 5: Schematic representation of surface modification methods (adapted from references 16 and 17)
device. For a specific medical application,
the desired characteristic for the implant
must be known prior to its implantation. Original surface Surface active bulk additive
Therefore, the implanted devices (coated or H H H CH3 CH3 CH3
otherwise), need to present specific bulk Overcoat O O O O O O
and surface characteristics if they are to be – Solvent coating
– Grafted surface layer Surface chemical reaction
recognised and accepted by the medium in
which they are placed.
Usually a material is chosen according to Surface gradient
its bulk properties, such as the stiffness, the – Graft
– Interpenetrating network Etching and roughening
polymer type, conductivity, optical
properties, degradation and strength.14,15
For most biomedical applications, the two treatment, plasma treatment, ultra-violet treatments. These include fast reaction
properties of greatest importance are the (UV) radiation exposure, laser ablation rates, the low cost of such processing, the
strength (based on mechanical attributes) treatment, gamma irradiation and x-ray availability of relatively simple formulations
and the surface reactivity and ease of treatments. and equipment, relatively facile
coating (based on chemical attributes). The second class includes surface development on an industrial scale and,
Some synthetic materials have suitable bulk modification by using ‘chemical methods’ probably most importantly, the distribution
properties. However, most such surfaces and incorporation of functional groups, of the grafted chains is limited to the
have to be modified by coating, if they are such as etching, surface oxidation, surface of the material.26
not to be recognised as a foreign material. hydrolysis, chemical grafting and surface Such grafting can be viewed as a
Thus, surface modification (coating) plays coating. Some of the common surface controlled coating option. Surface
an important role in the biomedical field modification techniques include plasma modification by the photo-grafting of
since this technique can be used to adapt techniques followed by polymerisation, coating formulations provides another basis
the surface to the desired characteristics sputter coating and etching, spray coating, for the modification of the surface
without compromising the bulk properties. dip coating, graft copolymerisation at the properties without interfering with the
Surface modification techniques are used surface, UV, gamma radiation and laser bulk material.
in several distinct types of application, such treatment, biomolecule attachment and the The first work on photografting
as biomedical polymers, textile materials, use of self-assembling coatings.16 polymerisation that was initiated by UV
microelectronics components and food Over the years, several surface radiation was published in the 1950s by
industry products. Thus, any successful modification methods have been Oster and Shibata.27 Surface graft
surface coatings related modification developed. Some of these are summarised polymerisation after coating, by using
method that is used will have been tried here: simultaneous UV radiation
and tested in a variety of fields, relevant to induction/initiation, is usually performed in
different final applications of the material. l The physical deposition of active
the presence of a photoinitiator or a
This reality gives confidence in the compounds to the surface by coating;18
photosensitiser.
appropriateness of the coating materials l The covalent immobilisation of polymer
This photoinitiator (after its
and the modification techniques that are chains onto a surface by chemical
photodecomposition), along with
available. reactions, taking place after the
monomers can induce the formation of
As previously mentioned, in the coating has been applied;19
monomer radicals, leading to subsequent
biomedical field, one of the major causes of l The grafting of polymer chains on the atom abstraction processes, (usually
device failure is biological response to the surface, during/after plasma involving H-atoms), resulting in radicals on
implanted material. Therefore, it is crucial treatment;20,21 by corona
to control the bio-interaction (if any) that discharge,22,23 and by grafting that has Figure 6: Schematic representation of surface graft
occurs between the modified (coated) been initiated by radiation pre- polymerisation by UV irradiation
device and its surroundings. treatment.24,25
Several methods for tailoring surfaces to
suit specific applications have been Surface modification by ultraviolet
radiation UV irradiation
reported. Biological methods, chemical
methods, physical methods and/or Monomer
Some of the surface modification methods
physicochemical methods can be used for that have been previously mentioned might Initiator
these purposes. Some of these methods are not give rise to a ‘permanent’ change and
schematically illustrated in Figure 5. Surface graft
the benefits might also considerably impair
Consequently, two major classes of polymerisation
the required bulk properties of the
surface modification techniques can be material. Surface graft polymerisation with
considered. The first concerns surface ultraviolet (UV) irradiation induced
modification by physical methods, which initiation (see Figure 6) has been proven to
include flame treatment, corona discharge offer some advantages over alternative
4 Surface Coatings International Issue 2013/3
the backbone of the substrate surface, Surface modification by plasma modification, coating, grafting and film
thereby initiating graft treatment deposition (plasma polymerisation).40
photopolymerisation through the usual
routes of propagation and eventual chain Nowadays, plasma technologies are being How plasma treatment functions
termination.28–30 widely used to tailor the surface properties The surface treatment of polymers is widely
of polymers without affecting their bulk achieved by using gases such as argon,
Benzophenone (BP), thioxanthones,
properties. The hydrophilicity, chemical helium, nitrogen and oxygen, among
chlorinated acetophenones and their
structure and roughness are some of the others. This treatment leads to the
derivatives are among the more common
surface properties that can be modified by formation of free radicals at the surface of
photoinitiators that are used in this
plasma treatment in order to adapt a the polymer. These radicals are, under
context. These allow the initiation of the
material for a specific application. Plasma appropriate circumstances, able to react
grafting process by inducing radical
treatment can also be used to clean with the excited species in the plasmas.
formation. The radical produced may be
polymer surfaces from organic Therefore, treatment with O2, N2 or inert
symmetrical or asymmetrical, depending on
contamination.37 gases leads to the formation of
the molecular structure of the initiator.
Thus, frequently used photoinitiators, such A plasma is a mixture of highly excited functionalities containing oxygen atoms,
as the isopropylthioxanthone, xanthone, electrons, negatively charged particles and such as hydroxyl groups, carbonyl groups
anthraquinone, 2,2-azo-bisisobutyronitrile positively charged particles, neutral atoms and, in some cases carboxylic groups.
and Irgacure 2959, among others, are used and molecules. For this reason, the plasma In the biomedical field, plasma surface
for non-aqueous media.26 state is sometimes referred to as the fourth modifications are mostly used to improve
state of matter. adhesion, increase surface wettability and
Water-soluble derivatives of these
initiator types are used when aqueous- Plasma polymerisation has been studied induce surface roughness. Thus, plasma
based formulations are required, the water intensively since the 1950s and especially surface modifications include:37
solubility being provided by the use of the in the 1960s. Over the years, it has gained
importance as a surface modification l removing surface contaminants such as
appropriate quaternary salt or sulphonic air pollutants or fingerprints;
acid salt. The curing reaction time and the technique and nowadays is a well-
recognised method38, especially in the l etching, leading to an increase of the
wavelength of the radiation that is used in
biomedical field. This is because it is a surface roughness by selective removal
the reaction are determined by the chosen
relatively economical and effective of surface material by chemical
photoinitiator and the spectral output of
technique for the processing of polymeric reaction and/or physical sputtering;
the radiation source.
materials. Table 2 lists some of the common l substitution of chemical groups on the
1-[4-(2-hydroxyethoxy)-phenyl]-2-
research areas and applications in which surface by other groups or
hydroxy-2-methyl-1-propane-1-one
plasma treatment is used for the creation functionalities that might allow
(Irgacure 2959), is a highly efficient non-
of more effective coated biomaterials.39 covalent bonding, by the modification
yellowing radical photoinitiator that is used
As previously mentioned, a plasma can be of the surface characteristics with
for the UV curing of systems comprising of
used for cleaning, for activation and for reactive gases.
unsaturated monomers and pre-polymers.
This photoinitiator has been very much the etching of a surface (metal, ceramics,
glass and plastics) as well as for coating by Plasma grafting/coating
used since Williams et al31 studied its
biocompatibility, along with that of other plasma polymerisation. The various effects Plasma grafting is a two-step incorporation
photoinitiators. In their study, Irgacure of the plasma treatment of a polymer process whereby functional groups and
2959 gave the best results in terms of surface may be categorised as surface reactive sites can be created on the
cytocompatibility.
Other applications of UV in the field Table 2: Common research areas and applications of plasma treatment in biomaterials, adapted from
reference 39
Despite the main application of UV
radiation in the biomaterial field being Areas Applications
targeted towards the modification of
Blood-containing surfaces Vascular grafts, catheters, stents, heart valves,
surfaces, in some cases, such as in the
membranes (haemodialysis), filters (blood cell
improvement of biocompatibility and
separation)
haemocompatibility, UV irradiation can be
also used to modify the bulk properties and Non-fouling surfaces Intraocular lenses, contact lenses, wound healing,
catheters, biosensors
composition of the material. Moreover,
cross-linked materials and cell Tissue engineering and cell culture Cell growth, antibody production, essays, vascular
immobilisation systems,32,33 anti-fouling grafts
surfaces34 and bio-scaffolds for tissue Sterilisation of surgical tools and devices Cutting tools of surgeons, tweezers
engineering35,36 can be prepared by UV Biosensors Biomolecules immobilised on surfaces
irradiation-based techniques. Barrier coatings Drug-release, gas-exchange membranes, device
protection, corrosion protection, reduction of leaching
(many of these involving the correct use of additives
and plasticisers)
Surface Coatings International Issue 2013/3 5
polymer surface. Using inert gas plasmas, acrylic acid being the plasma monomer. The with blood and thus minimise surface-
free radicals can be formed on the surface. authors concluded that the coated thin induced platelet activation. Albumin
To generate a grafted/coated polymer on film was formed was chemically similar to reduces both the number of adherent
this surface, a monomer solution is poly(acrylic acid). platelets and the extent of platelet
introduced into the reaction chamber, activation on the albumin-adsorbed
allowing the monomer to react with the surface.50
surface free radicals, resulting in a Biomolecule attachment Poly-D-lysine (PDL) is a synthetic
grafted/coated surface treatment (Inagaki, polypeptide that is used as a culture
As mentioned previously, the
1996).40 substrate to enhance cell attachment, after
adsorption/desorption behaviour of blood
Alves et al41 have introduced carboxylic coating on plastic and on glass surfaces.
proteins and the adhesion and proliferation
groups onto a thermoplastic polyurethane PDL is also widely used with a wide variety
of different types of cells on polymeric
substrate using the plasma method. In this of cell cultures, particularly neurons, glial
materials depends mainly on surface
way, the authors graft/coated acrylic acid cells and transfected cells. In addition, PDL
characteristics such as the wettability, the
and methacrylic acid onto the surface of coated surfaces are often used to reduce
degree of hydrophilicity/hydrophobicity, the
the polymeric substrate to improve cell detachment that might otherwise
bulk chemistry, the surface charge, the
wettability and reduce cell adhesion. occur during the multiple washing steps
surface charge distribution and the surface
Poly(dimethyl siloxane) surfaces can be that are associated with cell assays.50,51
roughness44 In order to accommodate
modified by low pressure plasmas in order these issues, the surface modification of
to improve their characteristics for biomaterials, using proteins to control cell
biomedical applications. Pluronic F-68 (a Conclusions
adhesion and the subsequent cellular
surfactant) and poly(ethylene glycol) response to material surfaces, has been The modification of surfaces is a very
methyl methacrylate can be grafted to reported.44–48 important aspect of the creation of
poly(dimethyl siloxane) surfaces to improve
For this purpose, molecules such as medically viable polymeric and non-
the wettability of the surface and reduce
laminin, fibronectin, collagen, and the polymeric biomaterials (metals, ceramics).
bacterial adhesion.42
Arg–Gly–Asp (RGD) peptide can be used. The use of coating techniques in the
These surface modification findings allow Some studies have shown that by creation of biomaterials field has been
these kinds of materials (polyurethanes and modifying the biomaterial surface with growing over recent decades due to the
poly(dimethyl siloxane)) to be used as molecules that induce cell adhesion, such developed abilities to improve the
medical devices (eg catheters, vascular as fibronectin, an improvement of the application properties of such materials
grafts and voice prostheses) without cellular response and of tissue repair can be when they are used in several biomedical
leading to a biofouling mechanism. achieved. applications, such as catheters, artificial
Some serum proteins, such as fibronectin veins, endoprostheses, cardiac valves and
Plasma Polymerisation
and vitronectin, show a preferential voice prostheses.
Plasma polymerisation leads to the
adsorption onto moderately wettable The efforts of researchers towards
formation of a thin coating film that can
surfaces. These proteins are also known as reaching ideal, designed surface
possess unique chemical properties and
cell-adhesive proteins. Thus, if a surface modifications are converging towards the
physical properties. In order for the
offers the ideal hydrophilicity, these introduction of desired functional
polymerisation process to occur, radicals
proteins can adhere on the surface and properties without leading to irregular
can be formed in the presence of a gas in
consequently can improve cell adhesion, etching or producing significant hazardous
which a monomer is usually mixed. Then, as
spreading, and growth.44 Thus if a surface wastes. At the same time, it is
the molecular weight of the polymer in the
is tailored to have the ideal hydrophilicity recognised/proposed that the nature of
chamber increases, the polymer is deposited
the cellular response can be controlled. these functional properties must be
as a coating on the surface of the
The RGD peptide sequence is known as a provided by species that are as close to
substrate.
cell recognition site for numerous adhesive being a monolayer as possible.
The deposition of the polymers is mainly
proteins that are present in the From all the methods available for surface
mediated by the geometry of the plasma
extracellular matrix (ECM) and in blood. modification, the radiation treated-
system, the working gas pressure, the
Surface-immobilised RGD groups are chemical related (ultraviolet and gamma
power and frequency of the signal, the
known to enhance cell attachment, while radiation-plasma systems) have been shown
temperature of the substrate and the flow
RGD components that are present in to be among the simpler, faster and more
rate and reactivity of the monomer. This
solution can inhibit cell attachment by effective methods. One of the more
technique leads to coated thin films that
competing with endogenous ligands for the important characteristics of the UV
are highly cross-linked and are strongly
same recognition site).49 irradiation or plasma methods is that their
bound to the surface.37,40
Bovine serum albumin (BSA) protein has action takes place only on thin surface
Vilani et al43 studied the influence of the layers, permitting the bulk of the sample to
different responses to different interfacial
parameters associated with the plasma remain unchanged, the modified material
environments. BSA is often used to coat
treatment during the use of acrylic acid on being thus able to retain its mechanical
biomedical devices. Albumin is often used
polysiloxane and polyurethane substrates. properties.
for the coating of vascular grafts to
They treated both surfaces using a RF
passivate those surfaces that are in contact
(radio frequency), low-pressure plasma with
6 Surface Coatings International Issue 2013/3
References and of techniques used in estimating onto polysulphone membranes’, J App
bacteria-material interactions’, Polym Sci, 78, 979–85, 2007
European Cells and Materials, 8,
1. Bottaro D P and M A 22. Lei J, Q Li, G He and X Lin, ‘Surface
37–57, 2004
Heidaran,.‘Engineered extracellular graft copolymerisation of acrylic
matrices: A biological solution for 11. Lasa I, ‘Towards the identification of amide onto BOPP film through
tissue repair, regeneration and the common features of bacterial corona discharge’, Acta Chim Sin, 58,
replacement’, The J Regen Med, 2, 9- biofilm development’, International 598–600, 2000
12, 2001 Microbiology, 9, 21–28, 2006
23. Lei J, M Shi and J Zhang, ‘Surface graft
2. This was listed as Ho, 1997 in the 12. JiaoY-P and F-Z Cui, ‘Surface copolymerisation of hydrogen silicon
text but details have not been modification of polyester biomaterials fluid onto fabric through corona
provided for tissue engineering’, Biomed Mater, discharge and water repellency of
2, (R24), 2007 grafted fabric’, Eur Polym J, 36,
3. Vadgama P, ‘Surface biocompatibility’, 1277–81, 2000
Royal Society of Chemistry, Annual 13. Carré A and V Lacarrière, ‘How
Reports Section ‘C’ (Physical substrate properties control cell 24. Bucio E, E Arenas and G Burillo,
Chemistry), 101, 14–52, 2005 adhesion: A physical-chemical ‘Radiation grafting of n-
approach’, Journal of Adhesion Science isopropylacrylamide onto
4. Furno F and R Bayston, and Technology, 24, 815–30, 2010 polypropylene films by pre-irradiation
‘Antimicrobial/antibiotic (infection method’, Mol Cryst Liq Cryst, 447,
resistance) materials’, Encyclopedia of 14. Goddard J and J Hotchkiss, ‘Polymer
203–13, 2006
Biomaterials and Biomedical surface modification for the
Engineering, 1, Marcel Dekker Inc, attachment of bioactive compounds’, 25. Mok S, D Worsfold, A Founda and T
2004 Prog Polym Sci, 32, 698–725, 2007 Matsuura, ‘Surface modification of
polyethersulphone hollow-fibre
5. Jung S-Y, S-M Lim, F Albertorio, G 15. Hu S, X Ren, M Bachman and C Sims,
membranes by gamma-ray
Kim, M C Gurau, R D Yang, M A ‘Tailoring the surface properties of
irradiation’, J App Polym Sci, 51, 193–9,
Holden and P S Cremer, ‘The Vroman poly(dimethylsiloxane) microfluidic
1994
effect: A molecular level description devices’ Langmuir,
of fibrinogen displacement’, J Am 20:5569–5574,2004 26. Deng J, L Wang, L Liua, and W Yang,
Chem Soc, 42, 12782–6, 2003 ‘Developments and new applications
16. McArthur S and K McLean, ‘Surface
of UV-induced surface graft
6. Chang H-I and Y Wang, ‘Cell modification’, Encyclopedia of
polymerisations’, Prog Polym Sci, 34,
responses to surface and architecture Biomaterials and Biomedical
156–93, 2009
of tissue engineering scaffolds’, Engineering, 2, Marcel Dekker Inc,
Regenerative Medicine and Tissue 2004 27. Oster G and O Shibata, ‘Graft
Engineering – Cells and Biomaterials, copolymer of polyacrylamide and
17. Ratner B, A Hoffman, F Schoen and J
(ed D Eberli), InTech Publisher, natural rubber produced by means of
Lemons, Biomaterials Science: An
Croatia, ISBN: 978–953–307–663–8 ultraviolet light’, J Polym Sci, 26, 233–4,
Introduction to Materials in Medicine,
1957
7. Palacio M L B, S R Schricker and B (2nd edition), Elsevier Publishers,
Bhushan, ‘Bioadhesion of various 2004 28. Ebara M, J Hoffman, P Stayton and A
proteins on random, diblock and Hoffman, ‘Surface modification of
18. Ozdemir M., C Yurteri and H
triblock copolymer surfaces and the microfluidic channels by UV-mediated
Sadikoglu, ‘Physical polymer surface
effect of pH conditions’, J R Soc graft polymerisation of non-fouling
modification methods and
Interface: and smart polymers’, Radiat Phys
applications in food packaging
rsif.2010.0557v1–rsif20100557, 2010 Chem, 76, 1409–13, 2007
polymers’, Crit Rev. Food Sci. Nutr.,
8. Greenwood J A, A B Theibert, G D 39:457–477, 1999 29. Guan J, C Gao, L Feng and J Shen,
Prestwich and J E Murphy-Ullrich, ‘Surface modification of polyurethane
19. Jia Z, S Du and G Tian, ‘Surface
‘Restructuring of focal adhesion for promotion of cell adhesion and
modification of acrylic fiber by
plaques by PI 3-Kinase: Regulation by growth 1: Surface photo-grafting with
grafting of casein’, J Macromol Sci, Part
PtdIns (3,4,5)-P3 binding to -Actinin’, N,N-dimethylaminoethyl
A, 44, 299–304, 2007
The Journal of Cell Biology, 150, methacrylate and cytocompatibility of
627–41, 2000 20. Suzuki M, A Kishida, H Iwata and Y modified surface’, J Mater Med, 12,
Ikada, ‘Graft copolymerisation of 447–52, 2001
9. Murphy-Ullrich J E, ‘The de-adhesive acrylamide onto a polyethylene
activity of matricellular proteins: is 30. Masson F, C Decker, S Andre and X
surface pretreated with a glow
intermediate cell adhesion an Andrieu, ‘UV-curable formulations for
discharge’ Macromolecules, 19,
adaptive state?’ The Journal of Clinical UV-transparent optical fibre coatings
1804–8, 1986
Investigation, 107, 785–90, 2001 I. Acrylic resins’, Prog Org Coat, 49,
21. Song Y, J Sheng, M Wei and X Yuan, 1–12, 2004
10. Katsikogianni M and Y-F Missirlis, ‘Surface modification of polysulphone
‘Concise review of mechanisms of 31. Williams G, A Malik, T Kim, P Manson
membranes by low-temperature
bacterial adhesion to biomaterials and J Elisseeff, ‘Variable
plasma-graft poly(ethylene glycol)
Surface Coatings International Issue 2013/3 7
cytocompatibility of six cell lines with 42. Pinto S, P Alves, C M Matos, A C Bibliography
photoinitiators used for polymerising Santos, L R Rodrigues, J A Teixeira
hydrogels and cell encapsulation’, and M H Gil, ‘Poly(dimethyl siloxane)
Biomaterials, 26, 1211–8m, 2005 surface modification by low pressure 1. DienerElectronics, Plasma Technology.
plasma to improve its characteristics Diener Electronics GmbH + Co KG,
32. Hipler U, P Elsner and J Fluhr, 2007
towards biomedical applications’,
‘Antifungal and antibacterial
Colloids Surfaces B, 81, 20–26, 2010 2. Egitto F and L Matienzo, ‘Plasma
properties of a silver-loaded cellulosic
fibre’, J Biomed Mater Res, Part B: Appl 43. Vilani C, D Weibel, R Zamora, A modification of polymer surfaces for
Biomater, 77B, 156–63, 2006 Habert and C Achete, ‘Study of the adhesion improvement’, J Res
influence of the acrylic acid plasma Develop, 38, 423–9, 1994
33. Jayakumar R, N Nwe, S Tokura and H
parameters on silicon and
Tamura, ‘Sulphated chitin and chitosan
polyurethane substrates using XPS and
as novel biomaterials’, Int J Biol
AFM’, Appl Surf Sci, 254,131–4, 2007
Macromol, 40, 175–81, 2007
44. Lee H B, G Khang and J Lee,
34. Pinto S, P Alves, A C Santos, C M
‘Polymeric biomaterials’, Biomaterials:
Matos, B Oliveiros, S Gonçalves, E
Principles and Applications, CRC Press
Gudiña, L R Rodrigues, J A Teixeira
LLC, 2003
and M H Gil, ‘Poly(dimethyl siloxane)
surface modification with 45. Ohya Y, H Matsunami, E Yamabe and
biosurfactants isolated from probiotic T Ouchi, ‘Cell attachment and growth
strains’, J Biomed Mater Res, 98A, on films prepared from
535–43, 2011 poly(depsipeptide-co-lactide) having
various functional groups’, J Biomed
35. Janorkar A, J Fritz, K Burg, A Metters
Mater Res, 65A, 79–88, 2003
and D Hirt, ‘Grafting amine-
terminated branched architectures 46. Wan Y, J Yang, J Yang, J Bei and S
frompoly(l-lactide) film surfaces for Wang, ‘Cell adhesion on gaseous
improved cell attachment’, J Biomed plasma modified poly-(L-lactide)
Mater Res, Part B: Appl Biomater, surface under shear stress field’,
81B,142–52, 2007 Biomaterials, 24, 3757–64, 2003
36. Thom V, G Altankov, T Groth, K 47. Garcia A, M Vega and D Boettiger,
Jankova, G Jonsson and M Ulbricht, ‘Modulation of cell proliferation and
‘Optimising cell–surface interactions differentiation through substrate-
by photografting of poly(ethylene dependent changes in fibronectin
glycol)’, Langmuir, 16, 2756–65, 2000 conformation’, Mol Biol Cell, 1910,
785–98, 1999
37. Gomathi N, S Neogi and A
Sureshkumar, ‘RF plasma-treated 48. Lee I-C and T-H Young, ‘Preparation
polymers for biomedical applications’, of PLLA membranes with different
Curr Sci, 94, 1478–86, 2008 morphologies for culture of ligament
cells’, Biomedical Engineering:
38. Biederman H and D Slavínská, ‘Plasma
Applications, Basis, Communications,
polymer films and their future
18, 185–9, 2006
prospects’, Surf Coat Tech, 125, 371–6,
2000 49. Armstrong J, H Salacinski, Q Mu, A
Seifalian, L Peel, N Freeman, C Holt
39. Chu P, J Chen, L Wang and N Huang,
and J Lu, ‘Interfacial adsorption of
‘Plasma-surface modification of
fibrinogen and its inhibition by RGD
biomaterials’, Mat Sci Eng R, 36,
peptide: A combined physical study’, J
143–206, 2002
Phys: Condens Matter, 16, S2483–91,
40. Inagaki N, Plasma Surface Modification 2004
and Plasma Polymerisation, Technomic
50. Maalej N, R Albrecht, J Loscalzo and J
Publishing Co Inc,1996
Folts, ‘The potent platelet inhibitory
41. Alves P, S Pinto, J-P Kaiser, A Bruinink, effects of S-nitrosated albumin
H C Sousa and M H Gil, ‘Surface coating of artificial surfaces’, J Am Coll
grafting of a thermoplastic Cardiol, 33, 1408–14, 1999
polyurethane with methacrylic acid
51. Harnett E, J Alderman and T Wood,
by previous plasma surface activation
‘The surface energy of various
and by ultraviolet Irradiation to
biomaterials coated with adhesion
reduce cell adhesion’, Colloids Surfaces
molecules used in cell culture’, Colloid
B, 82, 371–7, 2011
Surface B, 55, 90–97, 2006
8 Surface Coatings International Issue 2013/3
You might also like
- Identification of Minerals & RocksDocument45 pagesIdentification of Minerals & RocksShayhaq Baloch0% (1)
- Tang 2008Document12 pagesTang 2008pmayaNo ratings yet
- Mammalian Cell Behavior On Hydrophobic Substrates Influence of Surface PropertiesDocument16 pagesMammalian Cell Behavior On Hydrophobic Substrates Influence of Surface PropertiesManoj Kumar pandreNo ratings yet
- WilliamDocument25 pagesWilliamGuilherme RomeroNo ratings yet
- 1 s2.0 S1350417713001193 MainDocument8 pages1 s2.0 S1350417713001193 MainIITRANANDJADHAVNo ratings yet
- Bioceramics For Hard Tissue Engineering Applications: A ReviewDocument9 pagesBioceramics For Hard Tissue Engineering Applications: A ReviewAjanth PraveenNo ratings yet
- Kishen - Haapasalo - 2010 - Biofilm Models and Methods of Biofilm AssessmentDocument21 pagesKishen - Haapasalo - 2010 - Biofilm Models and Methods of Biofilm AssessmentdrchanyccNo ratings yet
- Force Fields For Simulating The Interaction of Surfaces With Biological MoleculesDocument10 pagesForce Fields For Simulating The Interaction of Surfaces With Biological Moleculesmateo ojedaNo ratings yet
- Surface ChemistryDocument15 pagesSurface ChemistryHajime HikariNo ratings yet
- Biofilm Formation: A Clinically Relevant Microbiological ProcessDocument6 pagesBiofilm Formation: A Clinically Relevant Microbiological ProcessGian RabagoNo ratings yet
- Bacteria Adhesion CoatingDocument11 pagesBacteria Adhesion CoatingWilliam VenegasNo ratings yet
- Nghien CuuDocument9 pagesNghien CuuNguyen GiaoNo ratings yet
- Bio Medical Surface Science Foundations To FrontiersDocument33 pagesBio Medical Surface Science Foundations To FrontiersRoxana StoicaNo ratings yet
- Recent Advance in Surface Modification For Regulating Cell Adhesion and BehaviorsDocument19 pagesRecent Advance in Surface Modification For Regulating Cell Adhesion and BehaviorssivaNo ratings yet
- Review Molecular Interactions in BiofilmsDocument13 pagesReview Molecular Interactions in Biofilmsnaima aminaNo ratings yet
- Biomaterials and BiocompatibiltDocument34 pagesBiomaterials and Biocompatibiltsindy mNo ratings yet
- Biofilms: Microbial Life On Surfaces: Rodney M. DonlanDocument10 pagesBiofilms: Microbial Life On Surfaces: Rodney M. DonlanKapil JhajhariaNo ratings yet
- InTech-Scanning Electron Microscopy Sem and Environmental Sem Suitable Tools For Study of Adhesion Stage and Biofilm FormationDocument15 pagesInTech-Scanning Electron Microscopy Sem and Environmental Sem Suitable Tools For Study of Adhesion Stage and Biofilm FormationJose Manuel Oliveira PereiraNo ratings yet
- Biofilms in Endodontic InfectionsDocument10 pagesBiofilms in Endodontic InfectionsValderrama Cisneros José LuisNo ratings yet
- Final Paper On TdiDocument17 pagesFinal Paper On Tdisujitpra058No ratings yet
- Review BifolmDocument16 pagesReview BifolmpcnferreiraNo ratings yet
- Biological Fixed Film: Md. Shahinoor Islam, Geelsu Hwang, Yang LiuDocument33 pagesBiological Fixed Film: Md. Shahinoor Islam, Geelsu Hwang, Yang Liusong1088No ratings yet
- Content ServerDocument10 pagesContent ServerAdit VekariaNo ratings yet
- Bharti2017 Phototrophic BiofilmsDocument16 pagesBharti2017 Phototrophic BiofilmsSacra PsyntergiaNo ratings yet
- Lecture 3 Charecteristics of BiomaterialsDocument11 pagesLecture 3 Charecteristics of BiomaterialsDivs TNo ratings yet
- Pubb 9 Recent - Advances - in - Functionalized - Electrospun - MembDocument24 pagesPubb 9 Recent - Advances - in - Functionalized - Electrospun - Membmarcofriuli2No ratings yet
- Surfactants in The Treatment of Chronic Wounds and Biofilm Management PLUS SnapShot JCNDocument8 pagesSurfactants in The Treatment of Chronic Wounds and Biofilm Management PLUS SnapShot JCNjcastNo ratings yet
- Cuticle Penetration3Document13 pagesCuticle Penetration3dainiusjNo ratings yet
- Mechanisms of Action of DisinfectantsDocument8 pagesMechanisms of Action of DisinfectantsAlagu SolaimalaiNo ratings yet
- Biofilm Susceptibility To Antimicrobials: Abstract-Microbial Biofilms, Where Organisms AreDocument8 pagesBiofilm Susceptibility To Antimicrobials: Abstract-Microbial Biofilms, Where Organisms AresiribabummtNo ratings yet
- Biofilm Models and Methods ofDocument21 pagesBiofilm Models and Methods ofVerghese George MNo ratings yet
- Effects of Material Characteristics and Surface Topograapy On Biofilm DevelopmentDocument14 pagesEffects of Material Characteristics and Surface Topograapy On Biofilm Development. .No ratings yet
- Marine Ecotoxicology-Chapter 5 - Biomarkers and Effects 2016Document45 pagesMarine Ecotoxicology-Chapter 5 - Biomarkers and Effects 2016Andrea LagomarsinoNo ratings yet
- Silk Fibroinchitosanalginate Multilayer Membranes As A System For Controlled Drug Release in Wound HealingDocument9 pagesSilk Fibroinchitosanalginate Multilayer Membranes As A System For Controlled Drug Release in Wound HealingвикторNo ratings yet
- Ni Hms 935462Document42 pagesNi Hms 935462Rin ChanNo ratings yet
- 1.3.proteins, Platelets, and Blood Coagulation at Biomaterial, Xu (2014)Document54 pages1.3.proteins, Platelets, and Blood Coagulation at Biomaterial, Xu (2014)LUCERONo ratings yet
- The Role of Bacterial Biofilms in Device-Associated InfectionDocument10 pagesThe Role of Bacterial Biofilms in Device-Associated InfectionLorena Bellan DomicianoNo ratings yet
- I. Physical PropertiesDocument2 pagesI. Physical PropertiesRegine GarciaNo ratings yet
- Biofilm 3 TypesDocument14 pagesBiofilm 3 TypesRin ChanNo ratings yet
- Example ChapterDocument5 pagesExample Chapterapi-375199340No ratings yet
- Bacterial Biofilm Under Flow First A Physical Struggle To Stay, Then A Matter of BreathingDocument24 pagesBacterial Biofilm Under Flow First A Physical Struggle To Stay, Then A Matter of BreathingWhite SpireNo ratings yet
- Pintelon 2011Document12 pagesPintelon 2011Adriana GomezNo ratings yet
- Biofilms in Treatment of Waste Water 2Document15 pagesBiofilms in Treatment of Waste Water 2anishapradhan.studNo ratings yet
- 1 s2.0 S2666138121000074 MainDocument5 pages1 s2.0 S2666138121000074 MainTejas krishnakanthNo ratings yet
- Reviews: Design of Biodegradable, Implantable Devices Towards Clinical TranslationDocument21 pagesReviews: Design of Biodegradable, Implantable Devices Towards Clinical Translation363331272No ratings yet
- Biofilms and Their Advantages/Disadvantages in Food IndustryDocument7 pagesBiofilms and Their Advantages/Disadvantages in Food IndustryUmarNo ratings yet
- Antibiotic Incorporation in Jet Sprayed Nanofibril - 2017 - International JournaDocument11 pagesAntibiotic Incorporation in Jet Sprayed Nanofibril - 2017 - International JournaMadhu Kiran DhondalayNo ratings yet
- Textbook Chapter1Document11 pagesTextbook Chapter1Denisse DominguezNo ratings yet
- Focal Adhesions in Osteoneogenesis: Special Issue Paper 1441Document13 pagesFocal Adhesions in Osteoneogenesis: Special Issue Paper 1441dupuytrenNo ratings yet
- Content 9080Document7 pagesContent 9080Andreea MicuNo ratings yet
- How Do Bacteria Know They Are On A Surface and Regulate Their Response To An Adhering State?Document3 pagesHow Do Bacteria Know They Are On A Surface and Regulate Their Response To An Adhering State?shargunan11No ratings yet
- Resistance of Bacterial Biofilms To Disinfectants A ReviewDocument17 pagesResistance of Bacterial Biofilms To Disinfectants A ReviewGianinna Zegarra QuevedoNo ratings yet
- Biofilms in Food IndustryDocument11 pagesBiofilms in Food IndustryKaleem UllahNo ratings yet
- Prevention of Biofilm Formation by Quorum QuenchingDocument11 pagesPrevention of Biofilm Formation by Quorum QuenchingJulio César Castillo HernándezNo ratings yet
- 10 1016@j Cellsig 2020 109867Document34 pages10 1016@j Cellsig 2020 109867VivianKlembergNo ratings yet
- The Impact of Contact Angle On The BiocoDocument13 pagesThe Impact of Contact Angle On The Biocowhiplash527No ratings yet
- Physiological Methods To Study Biofilm DisinfectionDocument6 pagesPhysiological Methods To Study Biofilm DisinfectionCharlie AbagonNo ratings yet
- New Insights Into The Structure and Function of Phyllosphere Microbiota Through High-Throughput Molecular ApproachesDocument10 pagesNew Insights Into The Structure and Function of Phyllosphere Microbiota Through High-Throughput Molecular ApproachesindahdwirahNo ratings yet
- Pbiomes 05 17 0019 RVWDocument13 pagesPbiomes 05 17 0019 RVWJessNo ratings yet
- Applications of Protein Resistant Polymer and Hydrogel Coatings On Biosensors and BiomaterialsDocument8 pagesApplications of Protein Resistant Polymer and Hydrogel Coatings On Biosensors and BiomaterialsPaul HartingNo ratings yet
- Polyurethane: Material For The Next Generation of Heart Valve Prostheses?Document9 pagesPolyurethane: Material For The Next Generation of Heart Valve Prostheses?pcnferreiraNo ratings yet
- Review BifolmDocument16 pagesReview BifolmpcnferreiraNo ratings yet
- Laser GraftingDocument5 pagesLaser GraftingpcnferreiraNo ratings yet
- Colloids and Surfaces B: BiointerfacesDocument7 pagesColloids and Surfaces B: BiointerfacespcnferreiraNo ratings yet
- PDMS Surface Modification Methods ReviewDocument16 pagesPDMS Surface Modification Methods ReviewpcnferreiraNo ratings yet
- Fabrication of Long-Term Hydrophilic Surfaces of Poly (Dimethyl Siloxane) Using 2-Hydroxy Ethyl MethacrylateDocument5 pagesFabrication of Long-Term Hydrophilic Surfaces of Poly (Dimethyl Siloxane) Using 2-Hydroxy Ethyl MethacrylatepcnferreiraNo ratings yet
- Paper PublicadoDocument9 pagesPaper PublicadopcnferreiraNo ratings yet
- ChemicalEngineering Che January-2024Document45 pagesChemicalEngineering Che January-2024Cem DursunoğluNo ratings yet
- Tutorial 4, 5 & 6 CHM361Document4 pagesTutorial 4, 5 & 6 CHM3612021819542No ratings yet
- SDS - SOLB - ARCTIC 3x3% ATC Foam Concentrate OSHA WHMIS GHS - 2019-07-26 - EN (26676)Document6 pagesSDS - SOLB - ARCTIC 3x3% ATC Foam Concentrate OSHA WHMIS GHS - 2019-07-26 - EN (26676)Luis Alberto Serrano MesaNo ratings yet
- Enhancement Activity/Outcome (Lesson 1) : No Answers YetDocument3 pagesEnhancement Activity/Outcome (Lesson 1) : No Answers YetWinxPink 17No ratings yet
- CHE 005 Lec SAS Days 15 - 16Document14 pagesCHE 005 Lec SAS Days 15 - 16johairah merphaNo ratings yet
- Using Composites As Rocket Motor Thermal InsulationDocument14 pagesUsing Composites As Rocket Motor Thermal InsulationguxxtavobarbattoNo ratings yet
- Major Classification of Indian SoilsDocument4 pagesMajor Classification of Indian SoilsALABANI MANGANo ratings yet
- Balancing Chemical Equations GizmoDocument3 pagesBalancing Chemical Equations GizmoSean HarleyNo ratings yet
- Advances in Geological and Geotechnical Engineering Research - Vol.4, Iss.1 January 2022Document55 pagesAdvances in Geological and Geotechnical Engineering Research - Vol.4, Iss.1 January 2022Bilingual PublishingNo ratings yet
- Feasibility and Need of Use of Waste Marble Powder in Concrete ProductionDocument4 pagesFeasibility and Need of Use of Waste Marble Powder in Concrete ProductionAjithNo ratings yet
- Atomic Structure & The Periodic Table (Multiple Choice) 1 QPDocument15 pagesAtomic Structure & The Periodic Table (Multiple Choice) 1 QPrayaNo ratings yet
- CPT Rasi Xi Che NeetDocument5 pagesCPT Rasi Xi Che NeetDeena chemistNo ratings yet
- Chemical Bonding II: Molecular Geometry and Hybridization of Atomic OrbitalsDocument86 pagesChemical Bonding II: Molecular Geometry and Hybridization of Atomic OrbitalsAsudeNo ratings yet
- Keerthi M.Nair, Vignesh Kumaravel, Suresh C Pillai Carbonaceous Cathode Materials For Electro-Fenton TechnologyDocument142 pagesKeerthi M.Nair, Vignesh Kumaravel, Suresh C Pillai Carbonaceous Cathode Materials For Electro-Fenton TechnologyVăn Thành MaiNo ratings yet
- Audit Report-AHL Rev.01Document12 pagesAudit Report-AHL Rev.01Osama AhmedNo ratings yet
- 4.06 - 4.07 Aromatic Chemistry and Amines MSDocument20 pages4.06 - 4.07 Aromatic Chemistry and Amines MSAdnan ChowdhuryNo ratings yet
- PDF Introduction To General Organic and Biochemistry 12Th Edition Frederick Ebook Full ChapterDocument53 pagesPDF Introduction To General Organic and Biochemistry 12Th Edition Frederick Ebook Full Chapterlynne.finney723100% (3)
- Coligative Properties - MUT PowerPoint PresentationDocument29 pagesColigative Properties - MUT PowerPoint PresentationYonelaNo ratings yet
- Safety Data Sheet: Texclad 2Document7 pagesSafety Data Sheet: Texclad 2Om Prakash RajNo ratings yet
- Candle Holder ReportDocument7 pagesCandle Holder ReportSHARIFAH AZIAH SYED RIDHUANNo ratings yet
- HaloalkanesDocument12 pagesHaloalkanescoding727treeNo ratings yet
- Principles of Biochemistry 5Th Edition Moran Test Bank Full Chapter PDFDocument38 pagesPrinciples of Biochemistry 5Th Edition Moran Test Bank Full Chapter PDFyuyen1ty6100% (9)
- Fabrication and Characteristics of Aluminium Metal Matrix CompositesDocument8 pagesFabrication and Characteristics of Aluminium Metal Matrix CompositesKonduru NaniNo ratings yet
- Separating Mixtures Answer KeyDocument1 pageSeparating Mixtures Answer KeyNtando Nkunzimanikina XimbaNo ratings yet
- Clax Build Lite 12A1 MsdsDocument10 pagesClax Build Lite 12A1 Msdsayman2015samirNo ratings yet
- C15 Notes CH5 States of MatterDocument9 pagesC15 Notes CH5 States of MatterArnieNo ratings yet
- 2.1 Cell Structure and FunctionDocument39 pages2.1 Cell Structure and Functionforyourhonour wongNo ratings yet
- Análisis de Diseño de Mexclas de Un Producto CosméticoDocument28 pagesAnálisis de Diseño de Mexclas de Un Producto CosméticoMaria Jose Moncayo PastasNo ratings yet
- 8 Plastering PDFDocument26 pages8 Plastering PDFZayedur RahmanNo ratings yet