Professional Documents
Culture Documents
Antitubercular Agent
Antitubercular Agent
Uploaded by
Elizabeth IdananCopyright:
Available Formats
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5835)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (903)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (541)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (350)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (824)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (405)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Motivation LetterDocument2 pagesMotivation LetterAjit AntonyNo ratings yet
- NOTES ON OB NursingDocument19 pagesNOTES ON OB NursingElizabeth Idanan100% (1)
- Antenatal Corticosteroids: Essential Inrapartum and Newborn Care (Einc) Policy ObjectiveDocument7 pagesAntenatal Corticosteroids: Essential Inrapartum and Newborn Care (Einc) Policy ObjectiveElizabeth IdananNo ratings yet
- Antifungal Drugs: Side Effects and Adverse Reactions of Amphotericin BDocument23 pagesAntifungal Drugs: Side Effects and Adverse Reactions of Amphotericin BElizabeth IdananNo ratings yet
- APGARDocument1 pageAPGARElizabeth IdananNo ratings yet
- Nursing Family AssessmentDocument5 pagesNursing Family AssessmentElizabeth IdananNo ratings yet
- Records in Family Health Nursing PracticeDocument2 pagesRecords in Family Health Nursing PracticeElizabeth IdananNo ratings yet
- Family Nursing Care PlanDocument5 pagesFamily Nursing Care PlanElizabeth Idanan100% (1)
- Phases of Nursing Research ReviewerDocument6 pagesPhases of Nursing Research ReviewerElizabeth IdananNo ratings yet
- Acute Viral Hepatitis: Jonathan WalaDocument49 pagesAcute Viral Hepatitis: Jonathan WalaAntony WaithakaNo ratings yet
- Torch InfectionsDocument13 pagesTorch InfectionsOmeNo ratings yet
- 2 PidDocument31 pages2 PidNatif BoteNo ratings yet
- Introduction MicroparaDocument30 pagesIntroduction MicroparaAlessandro MadrigalNo ratings yet
- Unit 11&12 TestDocument3 pagesUnit 11&12 TestBùi Mỹ HươngNo ratings yet
- Microbiology HistoryDocument10 pagesMicrobiology HistoryUsman WaheedNo ratings yet
- EnterobacteriaceaeDocument13 pagesEnterobacteriaceaejemarmiraquelNo ratings yet
- The Event 201: October 2019Document5 pagesThe Event 201: October 2019Allen BurroughsNo ratings yet
- RET 1024 Mod 3.0 Infection Control ADocument26 pagesRET 1024 Mod 3.0 Infection Control AmichellegruenbergNo ratings yet
- Jl. Pulo Mas Timur K No.2 RT4/RW.14, Kayu Pu H, Kec. Pulo Gadung, Kota Jakarta Timur, Daerah Khusus Ibukota Jakarta 13210Document1 pageJl. Pulo Mas Timur K No.2 RT4/RW.14, Kayu Pu H, Kec. Pulo Gadung, Kota Jakarta Timur, Daerah Khusus Ibukota Jakarta 13210suherman paleleNo ratings yet
- Bio-Controlling Capability of Probiotic Strain Lactobacillus Foodborne Pathogens in YoghurtDocument16 pagesBio-Controlling Capability of Probiotic Strain Lactobacillus Foodborne Pathogens in YoghurtLola Ayu IstifianiNo ratings yet
- Gradien, 10 (2), Pp. 992-995Document3 pagesGradien, 10 (2), Pp. 992-995Riza Ma'rufinNo ratings yet
- YersiniaDocument16 pagesYersiniaAlexandra Ançã PiresNo ratings yet
- Arbovirus Flash CardsDocument11 pagesArbovirus Flash CardsmfabzakNo ratings yet
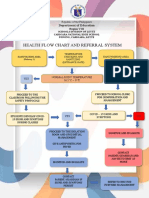
- Health Flow Chart and Referral System: Department of EducationDocument2 pagesHealth Flow Chart and Referral System: Department of EducationWendy TablaNo ratings yet
- Parasitic DiseaseDocument21 pagesParasitic DiseaseRakib HossainNo ratings yet
- KBMC Covid-19 RT-PCR Molecular Biology Laboratory: Ranjan Society, Near MSEB Office, Badlapur (West), Thane - 421503Document2 pagesKBMC Covid-19 RT-PCR Molecular Biology Laboratory: Ranjan Society, Near MSEB Office, Badlapur (West), Thane - 421503Sandeep VishwakarmaNo ratings yet
- 14th International Iranian Congress of MicrobiologyDocument1,130 pages14th International Iranian Congress of MicrobiologynavidsalamiNo ratings yet
- Macconkey Broth M: Art. No. 02-118Document2 pagesMacconkey Broth M: Art. No. 02-118junkyNo ratings yet
- MicrobesDocument1 pageMicrobesHartford CourantNo ratings yet
- Clinical Efficacy of Fosfomycin For The Treatment of Complicated Lower Tract and Uncomplicated Urinary Tract InfectionsDocument7 pagesClinical Efficacy of Fosfomycin For The Treatment of Complicated Lower Tract and Uncomplicated Urinary Tract InfectionsInternational Medical PublisherNo ratings yet
- Policies and Procedures Manual Infection Control in General Nursing UnitDocument9 pagesPolicies and Procedures Manual Infection Control in General Nursing UnitDerick RanaNo ratings yet
- What Is NorovirusDocument1 pageWhat Is NorovirusHunter GeiselNo ratings yet
- Kurdistan Regional Government - Iraq1Document4 pagesKurdistan Regional Government - Iraq1azarakam15No ratings yet
- SBI Reporting Forms New 2019 1Document7 pagesSBI Reporting Forms New 2019 1Salagmaya ES100% (1)
- ArvindbhaiDocument1 pageArvindbhaiJ D PatelNo ratings yet
- A Case of Warts Treated With Thuja OccidentalisDocument4 pagesA Case of Warts Treated With Thuja OccidentalisHomoeopathic PulseNo ratings yet
- Science of MicrobiologyDocument11 pagesScience of MicrobiologyJamaica M DanguecanNo ratings yet
- Exposé Sur L - Ebola en AnglaisDocument6 pagesExposé Sur L - Ebola en AnglaisMahama GbaneNo ratings yet
Antitubercular Agent
Antitubercular Agent
Uploaded by
Elizabeth IdananOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Antitubercular Agent
Antitubercular Agent
Uploaded by
Elizabeth IdananCopyright:
Available Formats
Anti-infective Agents Antitubercular
Antifungals
Anti-infective
Antivirals
Is a general term for any medication that is Antiprotozoal
effective against pathogens. Anthelminthics
Although antibiotic is more frequently used, this
term refers only to natural substances produced by Antitubercular drugs
microorganism that can kill another microorganism Tuberculosis
Bactericidal/bactericidal Is caused by the acid-fast bacillus Mycobacterium
Medications that accomplish this goal by killing the tuberculosis or tubercle bacillus.
bacteria One of the world’s major health problems, killing
one person than any other infectious disease,
Bacteriostatic including acquired immunodeficiency syndrome
(AIDS)-immune dis order characterized by
This drug will not kill the bacteria but instead slow opportunistic diseases
their growth, depending on the body's natural
defense to dispose microorganism Tubercles- slow growing mycobacterium usually
Growth slowing drugs become dormant, existing inside cavities
Mutation or errors in genetic code Antitubercular drugs
Microorganism have the ability to replicate Agents that treat tuberculosis
extremely rapidly.
Occur spontaneously and randomly throughout the Streptomycin
bacterial chromosomes. The first drug used to treat TB, ands given
Acquired resistance parenteral antibiotic
Clients develops an infection that is resistant to Isoniazid (INH)
conventional drug therapy. Was the first oral drug preparation effective
Broad spectrum antibiotic against the tubercle bacillus and was
discovered in 1952.
are effective against many different species of A bactericidal drug that inhibits tubercle cell
pathogens wall synthesis and blocks pyridoxine (Vit.B6),
which is used for intracellular enzyme
Narrow spectrum antibiotic production.
Effective against only one or a restricted group of Note: Drug therapy of TB differs from that of most other
microorganisms infections. Mycobacteria have a cell wall that is resistant to
Culture and sensitivity test penetration by antibiotic.
Process of growing the pathogen and identifying o 6 to 12 months medications to reach the isolated
the most effective antibiotic microorganism in the tubercles.
o 24 months is needed when the clients develop
Superinfection multidrug resistant
o 6 to 24 months-different combinations of drugs
Appearance of secondary infection
Occur when microorganisms normally present in may be used. At least 2 and sometimes 4 or more
the body are destroyed antibiotics is administered Concurrently
Host flora 2 Broad Categories of Antitubercular Drugs
Normal microorganism, inhabit the skin, upper 1. First line drugs
respiratory, genitourinary and intestinal tract Are safer and generally the most effective
o Ethambutol (Myambutol)
Note: The primary goal of antibiotic therapy is to kill o Isoniazid (INH) Pyrazinamide (PZA)
enough bacteria, of to slow the growth of the infection, o Rifampin (Rifadin, Rimactane)
so that natural body defenses can overcome the o Rifapentine (Priftin)
invading agent. o Rifater: combination of PZA with INH and
rifampin.
o Streptomycin
ANTITUBERCULAR AGENT
(adverse effect on book p. 507)
Anti-infective Agent
2. Second line drugs Should not be taken with alcohol will increase the
More toxic and less effective than the first line incidence of peripheral neuropathy
drugs Antacids decreases isoniazid absorption
Used when resistance develops. If phenytoin is taken with isoniazid, the effect of
o Amikacin (Amikin) phenytoin will decrease
o Capreomycin (Capastat Sulfate)
Side Effects and Adverse Effects
o Ciprofloxacin (Cipro)
o Cycloserine (Seromycin) Isoniazid – peripheral neuropathy
o Ethionamide (Trecator-SC) INH, Rifampin, Streptomycin – hepatotoxicity
o Kanamycin (Kantrex) patient may develop headache, blood dyscrasias,
o Ofloxacin (Floxin) paresthesia, GI distress and ocular toxicity
Rifampin – turns body fluid orange
Combination of INH and PZA Ethambutol – may develop dizziness, confusion,
Is approved for tuberculosis prophylaxis ih HIV hallucination and joint pains
positive patients for a short-term therapy of 2 Streptomycin – ototoxicity, optic nerve toxicity,
months. encephalopathy, angioedema, CNS and respiratory
Rifampin and PZA depression nephrotoxicity and ototoxicity
Recommended to HIV positive patient with Nursing Consideration:
positive TB skin test as prophylactic for 2 months 1. Assess for the presence of or history of a positive
Isoniazid tuberculin skin test, positive sputum culture, or a
close contact to a person recently infected with TB
The primary antitubercular drug used and may 2. Assess the patient for a history of alcohol abuse,
cause isoniazid-induced liver damage AIDS, liver disease, or kidney disease because
Must be taken with Pyridoxine (Vit B6) to avoid many antituberculosis drugs are contraindicated in
deficiency and peripheral neuropathy. those conditions
3. Assess for concomitant use of immunosuppressant
2 Types of Mycobacteria Infects Humans
drugs
1. Mycobacterium Leprae 4. Use caution in clients with renal dysfunction,
Responsible for leprosy pregnancy and lactation
Treated with multiple drugs, usually 5. Use caution to a client with history of convulsion
beginning with rifampin disorder
2. Mycobacterium Avium Complex (MAC) 6. Use caution with in clients having chronic liver
Causes infection of the lungs, most disease or alcoholism because of the risk of hepatic
commonly observed in AIDS. injury due to the production of toxic levels of drugs
metabolites.
Macrolides Azithromycin (Zithromax) and 7. Ethambutol ((Myambutol) is contraindicated in
Clarithromycin (Biaxin) clients with optic neuritis
8. Antituberculosis drugs interact with oral
Effective drugs against MAC
contraceptives and decrease their effectiveness,
Multi Drugs Therapy female clients with childbearing potential should
use an alternative form of birth control
o Isoniazid and Rifampin
o Isoniazid, Rifampin and Ethambutol Client Teaching:
o Isoniazid, Rifampin and Pyrazinamide 1. Immediately report yellow eye and skin, loss of
Pharmacokinetics appetite, dark urine or unusual tiredness
2. Take supplemental vitamin B^ as ordered to reduce
UNH – well absorbed in the GI tract risk of adverse effects
Administered IM 3. If taking isoniazid, avoid food containing tyramine,
Has low protein binding rate (10%) such as age cheese, smoked and pickled fish, beer,
Half-life: 1-4 hours and red wine, bananas and chocolate
Isoniazid is metabolized in the liver and 4. Wash hands frequently and cover the mouth when
75% of the drug excreted in the urine coughing, or sneezing. Properly dispose of soiled
tissues
Pharmacodynamic
5. If taking oral contraceptives, use an alternative
Inhibits cell wall synthesis of the tubercle bacillus form of birth control during antitubercular drug
Peripheral neuropathy is an adverse reaction to therapy
isoniazid, so pyridoxine (vitamin B6) is usually 6. Complete the full course of treatment
taken to decrease probability of neuropathy
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5835)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (903)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (541)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (350)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (824)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (405)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Motivation LetterDocument2 pagesMotivation LetterAjit AntonyNo ratings yet
- NOTES ON OB NursingDocument19 pagesNOTES ON OB NursingElizabeth Idanan100% (1)
- Antenatal Corticosteroids: Essential Inrapartum and Newborn Care (Einc) Policy ObjectiveDocument7 pagesAntenatal Corticosteroids: Essential Inrapartum and Newborn Care (Einc) Policy ObjectiveElizabeth IdananNo ratings yet
- Antifungal Drugs: Side Effects and Adverse Reactions of Amphotericin BDocument23 pagesAntifungal Drugs: Side Effects and Adverse Reactions of Amphotericin BElizabeth IdananNo ratings yet
- APGARDocument1 pageAPGARElizabeth IdananNo ratings yet
- Nursing Family AssessmentDocument5 pagesNursing Family AssessmentElizabeth IdananNo ratings yet
- Records in Family Health Nursing PracticeDocument2 pagesRecords in Family Health Nursing PracticeElizabeth IdananNo ratings yet
- Family Nursing Care PlanDocument5 pagesFamily Nursing Care PlanElizabeth Idanan100% (1)
- Phases of Nursing Research ReviewerDocument6 pagesPhases of Nursing Research ReviewerElizabeth IdananNo ratings yet
- Acute Viral Hepatitis: Jonathan WalaDocument49 pagesAcute Viral Hepatitis: Jonathan WalaAntony WaithakaNo ratings yet
- Torch InfectionsDocument13 pagesTorch InfectionsOmeNo ratings yet
- 2 PidDocument31 pages2 PidNatif BoteNo ratings yet
- Introduction MicroparaDocument30 pagesIntroduction MicroparaAlessandro MadrigalNo ratings yet
- Unit 11&12 TestDocument3 pagesUnit 11&12 TestBùi Mỹ HươngNo ratings yet
- Microbiology HistoryDocument10 pagesMicrobiology HistoryUsman WaheedNo ratings yet
- EnterobacteriaceaeDocument13 pagesEnterobacteriaceaejemarmiraquelNo ratings yet
- The Event 201: October 2019Document5 pagesThe Event 201: October 2019Allen BurroughsNo ratings yet
- RET 1024 Mod 3.0 Infection Control ADocument26 pagesRET 1024 Mod 3.0 Infection Control AmichellegruenbergNo ratings yet
- Jl. Pulo Mas Timur K No.2 RT4/RW.14, Kayu Pu H, Kec. Pulo Gadung, Kota Jakarta Timur, Daerah Khusus Ibukota Jakarta 13210Document1 pageJl. Pulo Mas Timur K No.2 RT4/RW.14, Kayu Pu H, Kec. Pulo Gadung, Kota Jakarta Timur, Daerah Khusus Ibukota Jakarta 13210suherman paleleNo ratings yet
- Bio-Controlling Capability of Probiotic Strain Lactobacillus Foodborne Pathogens in YoghurtDocument16 pagesBio-Controlling Capability of Probiotic Strain Lactobacillus Foodborne Pathogens in YoghurtLola Ayu IstifianiNo ratings yet
- Gradien, 10 (2), Pp. 992-995Document3 pagesGradien, 10 (2), Pp. 992-995Riza Ma'rufinNo ratings yet
- YersiniaDocument16 pagesYersiniaAlexandra Ançã PiresNo ratings yet
- Arbovirus Flash CardsDocument11 pagesArbovirus Flash CardsmfabzakNo ratings yet
- Health Flow Chart and Referral System: Department of EducationDocument2 pagesHealth Flow Chart and Referral System: Department of EducationWendy TablaNo ratings yet
- Parasitic DiseaseDocument21 pagesParasitic DiseaseRakib HossainNo ratings yet
- KBMC Covid-19 RT-PCR Molecular Biology Laboratory: Ranjan Society, Near MSEB Office, Badlapur (West), Thane - 421503Document2 pagesKBMC Covid-19 RT-PCR Molecular Biology Laboratory: Ranjan Society, Near MSEB Office, Badlapur (West), Thane - 421503Sandeep VishwakarmaNo ratings yet
- 14th International Iranian Congress of MicrobiologyDocument1,130 pages14th International Iranian Congress of MicrobiologynavidsalamiNo ratings yet
- Macconkey Broth M: Art. No. 02-118Document2 pagesMacconkey Broth M: Art. No. 02-118junkyNo ratings yet
- MicrobesDocument1 pageMicrobesHartford CourantNo ratings yet
- Clinical Efficacy of Fosfomycin For The Treatment of Complicated Lower Tract and Uncomplicated Urinary Tract InfectionsDocument7 pagesClinical Efficacy of Fosfomycin For The Treatment of Complicated Lower Tract and Uncomplicated Urinary Tract InfectionsInternational Medical PublisherNo ratings yet
- Policies and Procedures Manual Infection Control in General Nursing UnitDocument9 pagesPolicies and Procedures Manual Infection Control in General Nursing UnitDerick RanaNo ratings yet
- What Is NorovirusDocument1 pageWhat Is NorovirusHunter GeiselNo ratings yet
- Kurdistan Regional Government - Iraq1Document4 pagesKurdistan Regional Government - Iraq1azarakam15No ratings yet
- SBI Reporting Forms New 2019 1Document7 pagesSBI Reporting Forms New 2019 1Salagmaya ES100% (1)
- ArvindbhaiDocument1 pageArvindbhaiJ D PatelNo ratings yet
- A Case of Warts Treated With Thuja OccidentalisDocument4 pagesA Case of Warts Treated With Thuja OccidentalisHomoeopathic PulseNo ratings yet
- Science of MicrobiologyDocument11 pagesScience of MicrobiologyJamaica M DanguecanNo ratings yet
- Exposé Sur L - Ebola en AnglaisDocument6 pagesExposé Sur L - Ebola en AnglaisMahama GbaneNo ratings yet