Professional Documents
Culture Documents
Drug Study (Mod7)
Drug Study (Mod7)
Uploaded by
Ma. Kaile Shyla LlacarOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Drug Study (Mod7)
Drug Study (Mod7)
Uploaded by
Ma. Kaile Shyla LlacarCopyright:
Available Formats
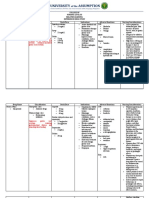
Pharmacology (C-NCM106)
DRUG STUDY
DRUG NAME CLASSIFICATION MECHANISM OF ACTION THERAPEUTICS EFFECTS NURSING CONSIDERATIONS
a.) Metoclopramide GI Stimulants/ Dopamine MOA: Stimulates motility of upper GI tract, Indications: Side Effects: restless, drowsy, tired, lack Assessment & Drug Effects:
Generic Name: Metoclopramide Antagonists increases lower esophageal sphincter To prevent or reduce: of energy, nausea, vomiting headache, Monitor bowel sounds.
Brand Name: Metonia, Reglan tone, and blocks dopamine receptors at nausea and vomiting from confusion, insomnia. Safety and effectiveness of drug
Appearance: the chemoreceptor trigger zone emetogenic cancer chemotherapy haven't been established for
Injection: 5mg/mL Postoperative nausea and Adverse Effects: anxiety, drowsiness, therapy lasting longer than 12
vomiting dystonic re actions, fatigue, lassitude, weeks.
restlessness, seizures, suicidal ideation, Drug may cause tardive
To facilitate small-bowel akathisia, confusion, depression, dyskinesia, parkinsonian
intubation dizziness, extrapyramidal symptoms, symptoms, and motor rest-
fever, hallucinations, headache, insomnia, lessness.
To aid in radiologic exam tardive dyskinesia, bradycardia, Monitor patient for involuntary
Delayed gastric emptying supraventricular tachycardia, movements of face, tongue, and
secondary to diabetic hypotension, transient HTN, HF, bowel extremities, which may indicate
gastroparesis disorders, diarrhea, nausea, incontinence, tardive dyskinesia or other
GERD urinary frequency, erectile dysfunction, extrapyramidal adverse effects.
agranulocytosis, neutropenia, rash, Monitor patient for fever, CNS
Contraindications: urticarial, loss of libido, prolactin symptoms, irregular pulse,
Oral Solutions: 5mg/mL Patients hypersensitive to drug secretion, gynecomastia, amenorrhea. cardiac arrhythmias, or ab normal
and in those with BP, which may indicate NMS.
pheochromocytoma or other Monitor patient for dizziness,
catecholamine-releasing headache, or nervousness after
paragangliomas, tardive metoclopramide is stopped; these
dyskinesia, or seizure disorders. may indicate withdrawal.
Patients for whom stimulation of Diphenhydramine or benztropine
GI motility might be dangerous may be used to counteract
(with hemorrhage, obstruction, extrapyramidal adverse effects
or perforation) from high doses.
Patient & Family Education
Tablets: 5mg, 10mg Instruct patient to take ODTs 30
minutes before food and at
bedtime and not to repeat dose if
inadvertently taken with food.
Tell patient taking ODTs to open
blister pack with dry hands and
immediately place tablet on
tongue, let it melt completely, and
then swallow. (Taking it with
water isn't nec essary.) If tablet
breaks or crumbles, advise
patient to throw it away and take
a new tablet out of the blister
pack.
Tell patient to avoid activities
that require alertness for 2 hours
after doses. Urge patient to report
persistent or serious adverse
reactions promptly.
Teach patient signs and
symptoms of tar dive dyskinesia,
other extrapyramidal signs and
symptoms, and NMS.
Advise patients to discontinue
drug and to seek immediate
medical attention if such signs
and symptoms occur.
Advise patient not to drink
alcohol during therapy.
DRUG NAME CLASSIFFICATION MECHANISM OF ACTION THERAPEUTICS EFFECTS NURSING CONSIDERATION
b.) Loperamide Antidiarrheal agents MOA: Loperamide acts by slowing Indications: Side Effects: dizziness, drowsiness, Patients should be advised to
Generic Name: Loperamide intestinal motility and by affecting water For the control and symptomatic tiredness, constipation, skin rash, itching check with their physician if their
Brand Name: Imodium, Diatabs and electrolyte movement through the relief of acute nonspecific diarrhea does not improve in 48
Appearance: bowel. Loperamide inhibits peristaltic diarrhea and chronic diarrhea Adverse Effects: severe constipation, hours or if they note blood in
Capsule: 2mg activity by a direct effect on the circular associated with inflammatory nausea, vomiting, abdominal pain, their stools, develop a fever or
and longitudinal muscles of the intestinal bowel disease. uncomfortable fullness of stomach, develop abdominal distention.
wall. It is a non-selective calcium channel For reducing the volume of irregular heartbeat, severe dizziness, Tiredness, dizziness, or
blocker and binds to opioid mu-receptors. discharge from ileostomies. fainting, rash, pruritus, urticaria, drowsiness may occur in the
Evidence also suggests that at higher angioedema, anaphylactic shock, dry setting of diarrheal syndromes
concentrations it binds to calmodulin. Contraindications: mouth, flatulence, dyspepsia, paralytic treated with IMODIUM
Patients with abdominal pain in ileus, megacolon, toxic megacolon, (loperamide hcl). Therefore, it is
absence of diarrhea. urinary retention. advisable to use caution when
Infants below 24 months old driving a car or operating
Patients with acute dysentery, machinery.
which is characterized by blood
in stools and high fever.
Patients with acute ulcerative
colitis.
Patients with bacterial
enterocolitis caused by invasive
organisms including Salmonella,
Shigella, and Campylobacter.
Patients with
Pseudomembranous colitis
associated with the use of broad-
spectrum antibiotics.
DRUG NAME CLASSIFICATION MECHANISM OF ACTION THERAPEUTICS EFFERCTS NURSING CONSIDERATIONS
c.) Simethicone Miscellaneous GI Agents MOA: Simethicone is a surfactant that Indications: Side Effects: nausea, constipation, Assess patient for abdominal
Generic Name: Simethicone decreases the surface tension of gas To treat symptoms of too much diarrhea, headache. pain, distention, and bowel
Brand Name: Alka-seltzer, Anti- bubbles in the gastrointestinal tract, more stomach acid such as stomach sounds prior to and periodically
Gas, Bicarsim Forte, Gas Aide, easily allowing gas to exit the body. upset, heartburn, and acid Adverse Effects: dizziness, fainting, throughout course of therapy.
Gas-X, Little Tummys, Mi-Acid indigestion. black/tarry stools, slow/shallow Frequency of belching and
Gas Relief, Mylanta Gas To relieve symptoms of extra gas breathing, irregular heartbeat, mood passage of flatus should also be
Maximum Strength, Mylicon, such as belching, bloating, and changes, deep sleep, pain with urination, assessed.
Phazyme, SimePed feelings of pressure/discomfort in abdominal pain, rash, itching, swelling Explain to patient the importance
Appearance: the stomach or gut. (tongue, face, throat), severe dizziness. of diet and exercise in the
Capsule: 125mg, 180mg, prevention of gas. Also explain
250mg Contraindications: that this medication does not
Patients with hypersensitivity to prevent the formation of gas.
simethicone or any component of Advise patient to notify health
the inactive ingredients. care professional if symptoms are
Lactating patients persistent
Pregnant patients
Patients with phenylketonuria
Tablet (Chewable):
125mg, 80mg
Oral
Liquid:
40mg/0.6mL
Oral Suspension:
20mg/0.3mL
DRUG NAME CLASSIFICATION MECHANISM OF ACTION THERAPEUTICS EFFERCTS NURSING CONSIDERATIONS
c.) Esomeprazole Antiulcer Drugs/ Proton Pump MOA: Esomeprazole exerts its stomach Indications: Side Effects: headache, flatulence, Assessment & Drug Effects:
Generic Name: Esomeprazole Inhibitors acid-suppressing effects by preventing the GERD; To heal erosive esophagitis indigestion, nausea, abdominal pain, Antacids can be used while taking
Brand Name: Nexium final step in gastric acid production by Symptomatic GERD diarrhea, constipation, drowsiness, drug, unless otherwise directed
Appearance: covalently binding to sulfhydryl groups of Erosive esophagitis due to acid itching, rash, nervousness. by prescriber.
Capsules: 20mg, 40mg cysteines found on the (H+, K+)-ATPase mediated GERD Monitor patient for rash or signs
enzyme at the secretory surface of gastric Shor-term treatment of GERD in Adverse Effects: headache, dizziness, and symptoms of
parietal cells. This effect leads to patients with history off erosive abdominal pain, constipation, diarrhea, hypersensitivity.
inhibition of both basal and stimulated esophagitis who can’t take drug dry mouth, flatulence, nausea, vomiting, Monitor GI symptoms for
gastric acid secretion, irrespective of the orally pruritus, agranulocytosis, pancytopenia, improvement or worsening.
stimulus. As the binding of esomeprazole To reduce the risk of gastric blurred vision, pancreatitis, stomatitis, Monitor LFTs, especially in
to the (H+, K+)-ATPase enzyme is ulcers in patients receiving microscopic colitis, liver failure, hepatitis, patients with preexisting hepatic
irreversible and new enzyme needs to be continuous NSAIDs therapy anaphylactic shock, GI candidiasis, disease.
expressed in order to resume acid Long-term treatment of hypomagnesemia, muscular weakness, Prolonged use may cause low
Tablets: 20mg secretion, esomeprazole's duration of pathologic hypersecretory muscle pain, bone fracture, hepatic magnesium levels that require
antisecretory effect that persists longer conditions encephalopathy, taste disturbance, magnesium supplementation and
than 24 hours. To eliminate Helicobacter Pylori aggression, agitation, depression, possibly discontinuation of drug.
Reduction of risk of rebleeding of hallucination, intestinal nephritis, Monitor magnesium level before
gastric or duodenal ulcers after bronchospasm, hair loss, erythema treatment and periodically during
therapeutic endoscopy multifome, hyperhidrosis, treatment.
Contraindications: photosensitivity, toxic epidermal Monitor patient for signs and
Patients hypersensitive to drug or necroysis symptoms of low magnesium
components of esomeprazole or level, such as abnormal HR or
omeprazole. heart rhythm, palpitations,
muscle de spasms, tremor, and
seizures. In children, abnormal
HR may present as fatigue, upset
Suspension: 2.5mg, 5mg,
stomach, dizziness, and light-
10mg, 20mg, 40mg
headedness.
May increase risk of CDAD.
Evaluate for CDAD in patients
who develop diarrhea that
doesn't improve.
Prolonged treatment (at least 3
years or more) may lead to
vitamin B12 malabsorption and
subsequent vitamin B12
deficiency, which is dose-related
and more severe in women and
those younger than age 30;
prevalence decreases after
Injection: 20mg, 40mg
discontinuation of therapy.
Patient & Family Education
Instruct patient to take drug
exactly as 17 prescribed.
Tell patient to take drug at least 1
hour before a meal.
Advice patient that antacids can
be used f while taking drug unless
otherwise directed by prescriber.
Warn patient not to chew or
crush drugs pellets because this
inactivates the drug.
Tell patient who has difficulty
swallowing capsule to mix
contents of capsule with 10
tablespoon of soft applesauce and
swallow immediately.
Advice patient to store capsules
at room temperature in a tight
container.
Tell patient to inform prescriber
of worsening signs and
symptoms, pain, or diarrhea that
doesn't improve.
Instruct patient to alert
prescriber if rash or other signs
and symptoms of allergy occur.
Warn patient to immediately
report symptoms of low
magnesium level, such as
involuntary muscle movements
or seizures.
DRUG NAME CLASSIFICATION MECHANISM OF ACTION THERAPEUTICS EFFERCTS NURSING CONSIDERATIONS
c.) Sucralfate GI Agents MOA: Sucralfate exerts its action locally Indications: Side Effects: back pain, constipation, Encourage the patient to:
Generic Name: Sucralfate rather than systemically and its effect on Treatment of: diarrhea, dizziness, drowsiness, Tell the doctor and pharmacist if
Brand Name: Carafate gastric acid is negligible with a low acid- Duodenal Ulcer insomnia, vertigo, abdominal pain, upset you are allergic to sucralfate, any
Appearance: neutralizing capacity (14—16 mEq/dose). Dyspepsia stomach, other medications, or any of the
Tablet: 1g Sucralfate reacts with hydrochloric acid in Epithelial wounds ingredients in sucralfate tablets
the stomach to form an adherent, paste- Chemotherapy-induced mucositis Adverse Effects: diarrhea, dizziness, dry or liquid. Ask your pharmacist for
like substance capable of acting as an acid Radiation proctitis mouth, flatulence, headache, indigestion, a list of the ingredients.
buffer. Subsequently, sucralfate adheres Prevention of: insomnia, nausea, vertigo, vomiting, Tell the doctor and pharmacist
electrostatically to proteins on the surface Ulceration bezoars formation, GI discomfort, hives, what other prescription and
of an ulcer, such as albumin and Stress ulcer prophylaxis in rash, itching, difficulty of breathing or nonprescription medications,
fibrinogen, forming insoluble, stable ventilated patiens swallowing, swelling (face, throat, vitamins, nutritional
complexes. These ulcer-bound complexes Behcet Disease tongue, lips), angioedema, aluminum supplements, and herbal products
act as a protective barrier at the ulcer site, Contraindications: toxicity you are taking or plan to take. Be
which facilitates recovery by shielding the Patients with hypersensitivity to sure to mention anticoagulants
ulcer from the ulcerogenic properties of sucralfate or any ingredients ('blood thinners') such as
pepsin, acid, and bile. Sucralfate contained in the drug. warfarin (Coumadin); cimetidine
Oral Suspension: predominantly binds to damaged GI
Patients with end-stage renal (Tagamet); cinoxacin (Cinobac);
1g/10mL mucosa, although binding to normal
disease ciprofloxacin (Cipro); digoxin
mucosa occurs to a minimal extent. This (Lanoxin); enoxacin (Penetrex);
Patients with uncontrolled
agent also inhibits back-diffusion of ketoconazole (Nizoral);
diabetes mellitus with
hydrogen ions, and adsorbs both pepsin levofloxacin (Levaquin);
hyperglycemia
and bile acids. In vivo, recommended levothyroxine (Levothroid,
Patients with impaired
doses of sucralfate inhibit pepsin activity Levoxyl, Synthroid); lomefloxacin
swallowing or gag reflex
in gastric juice by 32%. Recent data (Maxaquin); nalidixic acid
indicate that production of prostaglandin (NegGram); norfloxacin
E2 and gastric mucus may be increased. (Noroxin); ofloxacin (Floxin);
Sucralfate also absorbs bile salts in vitro. phenytoin (Dilantin, Phenytek);
quinidine; ranitidine (Zantac);
sparfloxacin (Zagam);
tetracycline; and theophylline
(Theo-24) If the patient is taking
any of these medicines, take them
at least 2 hours before taking
sucralfate. The assigned doctor
also may need to change the
doses of the patient’s medications
or monitor you carefully for side
effects.
Tell the patient who’s taking
antacids, to take them at least 30
minutes before or after sucralfate.
REFERENCES:
https://www.rxlist.com/imodium-drug.htm#side_effects
https://go.drugbank.com/drugs/DB00836
https://go.drugbank.com/drugs/DB09512https://www.webmd.com/drugs/2/drug-56526/antacid-simethicone-oral/details
https://www.webmd.com/drugs/2/drug-56526/antacid-simethicone-oral/details#:~:text=This%20medication%20can%20cause%20nausea,become%20severe%2C%20notify%20your%20doctor.
https://www.pdr.net/drug-summary/Gas-X-simethicone-2675
https://www.coursehero.com/file/23036643/Simethicone/
https://www.rxlist.com/consumer_esomeprazole_nexium/drugs-condition.htm
https://www.medicinenet.com/esomeprazole/article.htm#what_brand_names_are_available_for_esomeprazole4
https://www.mims.com/philippines/drug/info/sucralfate?mtype=generic
https://pubchem.ncbi.nlm.nih.gov/compound/Sucralfate#section=Mechanism-of-Action
https://www.rxlist.com/consumer_sucralfate__carafate/drugs-condition.htm
https://medlineplus.gov/druginfo/meds/a681049.html
https://www.ncbi.nlm.nih.gov/books/NBK551527/
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5824)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (903)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (541)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (823)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (403)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Orthodontic Contract and Consent Form PDFDocument6 pagesOrthodontic Contract and Consent Form PDFjack100% (1)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- OKU 5 Orthopaedic Knowledge Update SpineDocument45 pagesOKU 5 Orthopaedic Knowledge Update SpinePubMed77100% (1)
- FDAR TemplateDocument1 pageFDAR TemplateMa. Kaile Shyla LlacarNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- S. Connolly Mini Guide Astral Temple ModifiedDocument31 pagesS. Connolly Mini Guide Astral Temple Modifiedbuddaofdestruction100% (10)
- Reading Review TOEFL Exercise (Skill 1 - 7)Document2 pagesReading Review TOEFL Exercise (Skill 1 - 7)LussyAlbayinnah100% (1)
- Drug StudyDocument4 pagesDrug StudyMa. Kaile Shyla LlacarNo ratings yet
- HEMAnotesDocument1 pageHEMAnotesMa. Kaile Shyla LlacarNo ratings yet
- Drug StudyDocument2 pagesDrug StudyMa. Kaile Shyla LlacarNo ratings yet
- Diazepam-Gentamicin DrugstudyDocument3 pagesDiazepam-Gentamicin DrugstudyMa. Kaile Shyla LlacarNo ratings yet
- NCP Increased ICPDocument3 pagesNCP Increased ICPMa. Kaile Shyla LlacarNo ratings yet
- Alternative and Herbal MedicineDocument2 pagesAlternative and Herbal MedicineMa. Kaile Shyla LlacarNo ratings yet
- Drug Study and Case Analysis (Salbutamol and Montelukast)Document4 pagesDrug Study and Case Analysis (Salbutamol and Montelukast)Ma. Kaile Shyla LlacarNo ratings yet
- Drug Study and Case Analysis (Salbutamol and Montelukast)Document4 pagesDrug Study and Case Analysis (Salbutamol and Montelukast)Ma. Kaile Shyla LlacarNo ratings yet
- Drug Study and Concept MapDocument3 pagesDrug Study and Concept MapMa. Kaile Shyla LlacarNo ratings yet
- DRUG STUDY (Ivermectin, Remdesivir, Lianhua)Document4 pagesDRUG STUDY (Ivermectin, Remdesivir, Lianhua)Ma. Kaile Shyla Llacar100% (1)
- DRUG STUDY and CASE ANALYSISDocument6 pagesDRUG STUDY and CASE ANALYSISMa. Kaile Shyla LlacarNo ratings yet
- Periodontal Manifestations of Hematological Diseases - A ReviewDocument4 pagesPeriodontal Manifestations of Hematological Diseases - A ReviewInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Arrhythmia CBLDocument7 pagesArrhythmia CBLRyuuzakiDNNo ratings yet
- Anatomy Syllabus 2013-14Document13 pagesAnatomy Syllabus 2013-14احمد كرمNo ratings yet
- Mcintyre, John 04/13/1990 Patient ReportDocument7 pagesMcintyre, John 04/13/1990 Patient ReportJohn McIntyreNo ratings yet
- Lecture 2 Block 1.1 Introduction To EpidemiologyDocument27 pagesLecture 2 Block 1.1 Introduction To EpidemiologyANAN ALSURAYYINo ratings yet
- Butadiene: Material Safety Data SheetDocument39 pagesButadiene: Material Safety Data Sheethyde2520015754No ratings yet
- Practical PhysiologyDocument436 pagesPractical Physiologyaastha212002100% (1)
- Basis For Review of Related LiteratureDocument3 pagesBasis For Review of Related LiteratureNader AbdurasadNo ratings yet
- Balantidium ColiDocument12 pagesBalantidium ColiSalsabila Putri AmrilNo ratings yet
- Fulltext - Jda v3 Id1087Document5 pagesFulltext - Jda v3 Id1087Caterina PatrauceanNo ratings yet
- Bipolar Disorder: SeminarDocument7 pagesBipolar Disorder: SeminarZhi Wu BhâvaNo ratings yet
- Gynae FCPS 1 Guide-1Document24 pagesGynae FCPS 1 Guide-1Lubna MushtaqNo ratings yet
- A Case of Mitral StenosisDocument29 pagesA Case of Mitral StenosisShadab KamalNo ratings yet
- Biotechnology Old Question PaperDocument10 pagesBiotechnology Old Question PaperHarshitNo ratings yet
- Anatomy of The SkinDocument28 pagesAnatomy of The Skinay254No ratings yet
- Custodial Death Pgp1Document16 pagesCustodial Death Pgp1Guru PrasadNo ratings yet
- 2018 Chapter 3-1 2018 Introduction To Industrial Higiene & Occupational Health PDFDocument59 pages2018 Chapter 3-1 2018 Introduction To Industrial Higiene & Occupational Health PDFLove StrikeNo ratings yet
- Who Has The Flu Pre Lab InformationDocument18 pagesWho Has The Flu Pre Lab InformationAnvitha EllankiNo ratings yet
- Full Chapter 1Document7 pagesFull Chapter 1Afif AzharNo ratings yet
- PBSDocument72 pagesPBSKavi KaviNo ratings yet
- Booklet Blood Culture 2018Document19 pagesBooklet Blood Culture 2018Karmass JallalNo ratings yet
- SGH Cervical Screening Colposcopy PathwaysDocument13 pagesSGH Cervical Screening Colposcopy PathwaysAbraham ChiuNo ratings yet
- Liu 2016Document34 pagesLiu 2016Arina AndriesNo ratings yet
- Virus, Monera and ProtistaDocument42 pagesVirus, Monera and ProtistaGigih Putra100% (3)
- Pre-And Postnatal Risk Factors in The Pathogenesis of BPD: The Role of InfectionsDocument35 pagesPre-And Postnatal Risk Factors in The Pathogenesis of BPD: The Role of InfectionslordofthewebNo ratings yet
- Preoperative Assessment of The Patient With Heart Disease Case FileDocument2 pagesPreoperative Assessment of The Patient With Heart Disease Case Filehttps://medical-phd.blogspot.comNo ratings yet