Professional Documents
Culture Documents
How To Implement Systematic Ethics Work in Nursing Homes?: Georg Bollig, Jan Henrik Rosland, Andreas Heller
How To Implement Systematic Ethics Work in Nursing Homes?: Georg Bollig, Jan Henrik Rosland, Andreas Heller
Uploaded by
Noname NotavailableOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
How To Implement Systematic Ethics Work in Nursing Homes?: Georg Bollig, Jan Henrik Rosland, Andreas Heller
How To Implement Systematic Ethics Work in Nursing Homes?: Georg Bollig, Jan Henrik Rosland, Andreas Heller
Uploaded by
Noname NotavailableCopyright:
Available Formats
How to implement systematic ethics work in nursing homes?
Georg Bollig 1,2,3*, Jan Henrik Rosland 1,2, Andreas Heller 4
1 Department of Clinical Medicine, University of Bergen, Norway 2 Sunnica centre for Palliative Care, Department of Internal Medicine,
Haraldsplass Deaconess Hospital Bergen, Norway 3 Department of Anesthesiology, Intensive Care, Palliative Medicine and Pain
Medicine, HELIOS Klinikum Schleswig, Germany 4 Institute of Palliative Care and Organizational Ethics, IFF (Faculty for
Interdisciplinary Research and Further Education), Faculty of University Klagenfurt, Vienna, Graz
Abstract
Systematic ethics work and ethics discussions may help practitioners handle the many ethical challenges and
dilemmas that have been described in the scientific literature pertaining to nursing homes. This review is based
on a selective literature search of relevant publications retrieved from PubMed and CINAHL. In addition,
relevant articles from the Internet or reference lists of articles and books, and other sources were included.
Several methods and ways of approaching the discussion of ethics, and the implementation of ethics work in
nursing homes, were identified. Frequently used methods and models to address ethical challenges were ethics
peer groups, ethics consultation, or ethics committees. In conclusion, systematic ethics work in nursing homes is
needed. The implementation should be individualized to meet different needs, as well as geographical and
cultural conditions.
Citation: Bollig G, Rosland JH, Heller A (2016) How to implement systematic ethics work in nursing homes? Advances in Medical
Ethics 3:1. doi:10.12715/ame.2016.3.1
Received: April 2, 2015; Accepted: November 29, 2015; Published: January 1, 2016
Copyright: © 2016 Bollig et al. This is an open access article distributed under the terms of the Creative Commons Attribution License,
which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Competing interests: The authors have declared that no competing interests exist.
Sources of funding: GB´s PhD-project on ethical challenges and decision-making in nursing homes has been financially supported by the
Norwegian Extra Foundation for Health and Rehabilitation through EXTRA funds (grant no. 2008/2/0208).
*
Email: bollig.georg@gmx.de
Introduction increasing. In advanced dementia, residents can no
longer make their own decisions, so physicians,
“Respect for individual persons is the ethical thread nurses and relatives have to make them on the
that runs through the care of nursing home residents’ behalf. Often, these decisions are made
residents.” [1] without knowing the resident’s true wishes because of
There are many ethical challenges in nursing homes, a lack of advanced care planning (ACP), and
for example a lack of resources, coercion, autonomy, inadequate preparatory conversations about their
decision-making for residents without capacity, and wishes and preferences for the end-of-life [14,15].
end-of-life care issues [2-11]. Modern medicine has However, decisions to withhold or withdraw life-
led to complex ethical challenges because of a greater sustaining therapy cannot be based on medical fact
number of people living with chronic illnesses, and alone, but must respect the patient’s own values and
the possibility to extend life using continually wishes. In people with advanced dementia, ACP,
invasive therapies such as tube feeding, dialysis and ethics consultation or ethics committees can be useful
respiratory therapy – even at home [12]. As the decision-making tools [16,17]. Daily, systematic
population of elderly and people suffering with ethics work in nursing homes is needed, yet is not
dementia is increasing worldwide [13] the need for standard in many nursing homes [5,11]. The term
surrogate decision-making in nursing homes is also ‘systematic ethics work’ has been defined as “the
www.ame-journal.com 1 Bollig et al. 2016 | 3:1
organization’s systematic use of different measures, making in patients with cognitive impairment,
tools and places to enhance ethics discussions and communication, shared decision-making with
ways to handle ethically difficult situations and relatives, and issues about end-of-life care are often
choices in nursing homes, e.g. ethics education, described in the literature as ethical challenges
ethical deliberation, different arenas for ethics [2,5,10]. Whereas “everyday ethical issues” are
discussions, ethics consultants and ethics important and need attention, the case discussions of
committees.” [11]. ethics committees and ethics consultant teams mostly
deal with “big ethical issues” such as withdrawal of
The aim of this article is to provide an overview of
life-sustaining treatment [2,21]. Staff members often
different approaches to implement systematic ethics
describe end-of-life issues, lack of resources and
work in nursing homes. Challenges and obstacles in
coercion as frequent ethical challenges in nursing
the implementation of systematic ethics work will also
homes [9,11]. A recent study has shown that everyday
be addressed.
ethical challenges seem to be most important from the
residents’ point of view [22]. Another problem is the
fact that in many Central European long term
Methods facilities, it is general practitioners who selectively
Using the databases PubMed and CINAHL, a provide medical expertise and treatment; some
selective literature search was carried out with a countries e.g. the Netherlands and Norway, are an
combination of the search terms: ‘nursing homes’, exception to this in that they have specialized nursing
‘long-term care facilities’, ‘implementation’ and home physicians. In many European long-term
‘ethics’. In addition, relevant articles from the facilities, day-to-day treatment is mostly provided by
Internet, or from reference lists of articles and books caregivers and non-medically trained staff. These
or articles found via other sources as lectures or circumstances suggest that different methods of
personal communications were included. Reflections ethical communication are needed, other than the one
on own experiences with implementation and research commonly practiced in hospitals.
on systematic ethics work in nursing homes were also
used to describe and discuss the topic.
Strategies to handle ethical challenges in nursing
homes
Results Places for both staff and patients to engage in
Ethical challenges and dilemmas in nursing homes discussion of ethical challenges should be established
throughout primary care sites [23]; such discussions
Ethical problems in nursing homes are often more require inter-professional collaboration of all staff
complex than those in hospitals [7,18,19]. There are members, relatives and residents. Healthcare
two major groups of ethical issues in nursing homes. professionals should remember that the choice of
The first group can be described as “everyday ethical treatment should be guided by what the resident
issues”, such as autonomy-related problems, informed would want and not what they would want for
consent, use of restraints, offensive behavior, or themselves [24]. Therefore, one important factor is to
refusing medication, food and bathing [6,8,10,11,20]. recognize, reconstruct and consider the wishes and
The second group consists of “big ethical issues”, values of the resident. In addition relatives’ views
mostly dealing with life-or-death matters, such as should be heard and taken into account. More timely
decisions to withhold or withdraw life-sustaining and effective discussions about planning for the end-
treatment, including artificial nutrition and hydration of-life should be routine in nursing homes [14,15].
[2,3,9,10,11,14,15]. According to Reitinger et al. [20] Planning for the end-of-life should be a process
ethical issues can arise from situations such as including continued discussions, rather than a single
admission to the nursing home, running away, meeting where all future decisions are made at once.
bathing, conflicts with relatives, admission to hospital, ACP should be the result of a series of such
treatment with nutrition and fluids, dying with discussions [25]. Continuity of ethical
dementia, or bereavement. Competence in decision-
www.ame-journal.com 2 Bollig et al. 2016 | 3:1
communications involving the parties concerned is admissions. Reflection groups (ethics peer groups)
therefore crucial. Strategies for enhancing end-of-life and moral case deliberation (ethics reflection groups
discussions are most productively linked to the with an ethicist as facilitator) with colleagues or a
physicians’ interpersonal communication skills, a multidisciplinary team are used in some nursing
patient-centered model of care, a focus on the quality homes, e.g. in Norway and the Netherlands [28–31].
of remaining life, and innovative clinical models for Staff from community health and elderly care services
implementing these discussions earlier in the care appreciate reflection groups as means to discuss
process [25]. ethical challenges, and the use of reflection groups can
improve daily practice [28,30,31]. Use of an ethics
consultant or a team of ethics specialists, who give
Methods and ways of organizing systematic ethics advice or help with immediate consultations on a
work ward, is rarely used in nursing homes. The team can
consist of members from the disciplines of social
Several methods and ways of organizing systematic
ethics work are used or proposed to handle ethical work, nursing, medicine and administration [21]. In
general, nursing home ethics committees fulfill the
problems in nursing homes (Box 1).
same tasks as hospital ethics committees, even though
they are often made up differently and known for
Box 1. Methods to handle ethical problems in nursing homes being less attached to specific hospital ethics
committees. Their tasks are education, case review
(In)formal discussions
and analysis, and policy development [2,7,18,24,32–
Reflection-groups (ethics peer groups) 34]. A survey of nursing home ethics committees in
Moral case deliberation the USA revealed that, of the 29% who responded,
few (8%) had established ethics committees. Their
Ethics consultant/ethics team
tasks were policy review (in 81%), advisory case
Ethics committee review (67%) and education (45%) [18]. Ethics cafés
Ethics café [35,36] aim at discussing ethical issues with different
Ethics rounds
groups (physicians, nurses, residents and relatives).
The discussion is usually led by a moderator, often a
Gaming/role play professional ethicist, who encourages the discussion.
Advance care planning (as a tool to improve This approach is called “Mäeutik” [35]. Ethics rounds
resident autonomy) [37] are meetings for healthcare professionals,
residents and relatives, which aim at encouraging a
dialogue across disciplines, education, and discussion
A systematic review on ethics support mechanisms of ethical issues for a broad range of people. Gaming
concluded that ethics support is often connected to and role-play have been used as educational tools for
local contexts [26]. In present nursing home practice, health care professionals and other nursing home staff.
informal or formal discussions between healthcare By acting out different roles, one may enhance the
professionals (nurses and physicians) alone or with understanding of others’ values and positions,
the resident and/or his relatives are often used [11]. including the difficulties and dilemmas involved in
Hayley et al. [1] suggested that most ethical issues in decision-making related to long-term care and care for
the nursing home could be resolved in an open the elderly [38].
discussion between the resident, relevant family
members, legal advisors, the physician, and nursing
home staff members. ACP and preparatory Development in Norway
conversations [15,17,27] between residents, relatives,
physicians and nursing home staff about the resident’s In 2007 the Norwegian Association of Local and
wishes and views about different treatment options Regional Authorities (Kommunesektorens
and acceptable outcomes can be useful to avoid organisasjon, KS) started a series of projects to raise
unnecessary life-prolonging treatments and hospital competence in ethics, and to implement reflection on
www.ame-journal.com 3 Bollig et al. 2016 | 3:1
ethics or ethics committees in nursing homes [39]. Obstacles of implementing ethics work in nursing
Examples of ethical tools used in these projects are an homes
ethics handbook [40], and simple methods as the
Organizational change is always a challenge and is
“traffic light approach” or “take a card” to discuss
accompanied by many obstacles. There will always be
ethical challenges in a group. Furthermore an e-
people who are afraid of change, and who will use a
learning program for learning and discussing ethics in
variety of arguments against systematic ethics work.
a peer group has been developed [39]. An evaluation
Some of the most frequently used arguments against
of this Norwegian project showed that there is a need
ethics consultation are [43]:
for competence in ethics and systematic reflection
beside support from the municipality [29]. • “There is not enough time.”
Indeed, sufficient time is needed to establish
systematic ethics work. However, discussions about
Challenges of implementation of ethics work in
ethics are likely to help save time since conflicts that
nursing homes
are not properly addressed may cost yet more time
The first step in dealing with ethical dilemmas is to be and lead to communication problems, burn-out, etc.
aware of the ethical aspects of a given situation and to
recognize a problem as an ethical one: “…critical • “Disturbance of the trustful relationship between
appraisal in ethics needs training in ‘you don’t physician and patient.”
perceive what you don’t perceive.’” [23]. Another Physicians might be afraid of others making “their
challenge is that situations which do not necessitate decisions”; however, a multidisciplinary discussion
immediate medical action are not considered ethically helps to ensure that different points of view are taken
relevant. Examples might be the staff situation, the into account. Ethics consultation can lead to a
great lack of time, or the implementation of processes recommendation based on ethical deliberation. The
according to mere economic standards, which often physicians are still responsible for their decisions, but
means a direct contrast of caregiving standards. they can then be based on a thorough investigation of
Issues concerning organizational ethics usually need all aspects of the case.
to be dealt with in a different context, where • “More unnecessary bureaucracy.”
leadership should also be involved. Organizational
ethics is the ethics of the whole organization and is Many healthcare professionals are afraid of more
interdependent with the organization’s culture [41]. paperwork and more meetings instead of working
To implement systematic ethics work in nursing with patients. Ethics consultation can be offered and
homes it is paramount to sensitize and educate the used voluntarily. The needs of patients, relatives and
whole nursing home staff (including those working in health care professionals shall be at the center of
administration, technical personnel, and others who do ethics consultation, which should be a tool in make
not work at the bedside), but probably also residents, good decisions. Information from the staff, patients
relatives and the public, about the importance of and relatives can be used to clarify the aims and the
ethical issues in the care of the elderly. To reach that process of ethics consultation.
many people will involve a huge effort, since teaching • “Something that only the management wants.”
and education is a challenge in terms of resources,
time, and organization. One of the many obstacles in If a top-down model of implementation is used then
the implementation of systematic ethics work in employees might get the impression that ethics
nursing is a lack of resources. To implement ethics consultation is something desired only by
education and ethical reflection in nursing homes, management. A combined top-down and bottom-up
time and financial support is needed. In times of cost approach can help to include all employees in the
effectiveness and economical restraints one should implementation process. Joint efforts between the
remember that: “Ethics cost, whether you have them management and interested employees have a greater
or not” [42]. chance of leading to sustainable changes within an
organization. Presumptions for ethics consultation
www.ame-journal.com 4 Bollig et al. 2016 | 3:1
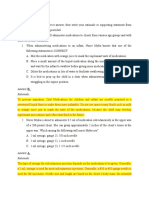
should be trustworthiness, acceptance, competence Based on a review of the literature and the authors’
and independence. experiences, our suggestion is a three-step approach to
ethical decision-making in nursing homes (Figure 1,
Another obstacle may occur if healthcare personnel
modified and adapted from [10]). The steps can be
are afraid to highlight a case with ethical problems
individualized to meet different needs as well as
because of a fear that this could lead to negative
geographical conditions. For a small rural nursing
consequences for themselves or their organization. A
home, education and open discussions might be a
common misunderstanding is that an ethics committee
good start, whereas large institutions in big cities
is a court that makes decisions in case of conflicts; i.e.
might need their own ethics committee or ethics
it is often misinterpreted as an attempt to sue
consultation team. It is possible to use all three steps
someone. To avoid such misunderstandings,
in one nursing home. A model of good practice for
information is needed about the work of ethics
systematic ethics works, which includes all three steps
committees to reassure staff that they do not make
shown in Figure 1, is the Caritas Socialis (CS) in
decisions; rather they reflect on ethical aspects of
Vienna, Austria, which has nursing homes, palliative
possible decisions, and give advice to the ones who
care and home care services [44, p. 146–150]. The CS
have to make those decisions, e.g. physicians and
has successfully included systematic ethics work
residents.
throughout the whole organization since 2007, and
frequently uses ethics meetings with residents to aid
decision-making for frail residents [11,44]. In Norway
Discussion in 2006, Bergen Red Cross Nursing Home established
Many methods to handle ethical problems, and ways its own ethics guidelines [45].
to organize ethics work in nursing homes, are
described in the literature. These are introduced in the
Results section and an overview is shown in Box 1.
Different methods and approaches to systematic ethics
work
A combination of different approaches to systematic
ethics work is likely to be most useful, for example,
discussion groups on the wards, and ethics committees
where people are able to transfer certain problems to a
higher level of ethics competence, or to reflect with a
broader perspective. Systematic ethics work may be
implemented using different measures, tools and
places to enhance ethics discussions and ways to
handle ethically difficult situations and choices in Figure 1. A three-step approach to ethical deliberation and
nursing homes [11]. There is evidence that different decision-making in nursing homes
methods, for example ethics reflection groups, or
moral case deliberation to discuss and reflect on
ethical challenges can be useful in nursing homes Planning the implementation of systematic ethics work
[2,7,9–11,18,19,21,26,28–32]. If ethical challenges in nursing homes
are complex and local ethics discussion does not lead
The organization of ethics consultation should be
to a consensus about a certain case, it could be helpful
clarified before its implementation in the nursing
to have an ethics committee to discuss the case
home. It is necessary to discuss the following
[18,32]. The best option must be adapted to suit local
questions [43, p. 71–-75]:
needs.
www.ame-journal.com 5 Bollig et al. 2016 | 3:1
• Who shall be able to ask for an ethics Internet, and – importantly – ensures that groups can
consultation (staff, resident, relatives, others)? have a dialogue. Use of Internet platforms in ethics
discussions may become more frequent in the future.
• Who will be the secretary and coordinator for the An obstacle against the use of the Internet is that
meetings? many of the staff in Norwegian nursing homes at
• Who decides if the issue is relevant to be present are not familiar with the Internet as an
discussed in an ethics consultation, or if it should educational tool.
be discussed elsewhere?
• Who shall participate in case reflections? Factors for successful implementation
• Which method shall be used for ethics reflection? An essential factor for the successful implementation
• How shall the results be documented? of systematic ethics work is that the management
encourages and supports the work [29,30]. If a project
These considerations underline that there is much starts from a bottom-up approach, one must try to
work to do before one can start ethical case involve the management at as early a stage as
discussions. The usual tasks (education, development possible. In our opinion, the combination of a top-
of guidelines and case review) should be defined, and down and bottom-up approach, with assignment and
a decision made as to whether they will be performed support from management and inclusion of the
within the organization, or if there might be a need to employees, is the best option to make implementation
collaborate with others. In other words, Step 1 and and organizational change possible and durable.
Step 2 of the three-step approach (Figure 1) may be Ethics must become a part of the everyday life of the
used in small nursing homes, whereas to implement organization, and will lead to change the organization
Step 3 might mean establishing a joint ethics as a whole. Some authors use the term ‘organizational
committee together with other nursing homes. This ethics’ for this type of common ethics within an
approach has been used in Oslo, Norway, and in organization such as a nursing home or hospital [41].
Frankfurt, Germany [46,47]. To ensure a change and a common concept of
organizational ethics within ones own institution,
discussion about values and ethics education are
Views of the residents, relatives and nursing home cornerstones of the implementation process. Residents
staff and their relatives should be encouraged to participate
Before implementing an ethics process it may be wise in ethics discussions whenever possible. A recent
to explore the views and needs of the staff, the study from our group has shown that relatives
residents, and their next of kin. But what do leaders participate in ethics meetings, whereas the residents
and nursing home/homecare services staff want? Staff themselves usually do not [11]. To our knowledge, the
members and leaders from Norwegian nursing homes residents are often excluded from ethics meetings.
and primary care services want ethics education for Reasons for that may be that staff members are afraid
health care personnel and administrators, meeting that the experience might be harmful or irritating for
places, and time to discuss ethical problems in order the residents. One major challenge for the future will
to improve systematic ethics work [5,9,11]. A recent therefore be to include both relatives and residents in
study found that only 18% of nursing home staff ethics discussions and ethical decision-making in
members consider internet-based learning a nursing homes [11].
meaningful option in ethics education [11]. This is in
contrast to the finding that internet-based learning is
growing and is included in university ethics courses. Summary and suggestions for the implementation of
One approach used in Norway is an Internet-based systematic ethics work in nursing homes
course that can be used by groups of healthcare In summary, implementation of ethics in nursing
personnel to facilitate ethics education and discussion homes is both needed and possible, as Weston et al.
[48]. This option likely spreads education using the [2] have already shown. The implementation of
www.ame-journal.com 6 Bollig et al. 2016 | 3:1
systematic ethics work can help to ascertain the
resident’s wishes, and enable the physician, staff and
others to discuss ethical problems in the course of
decision-making. Hopefully this could lead to a
reduction of conflicts between the resident, their
relatives, care staff and the physician, and greater
complicity with the resident’s wishes regarding their
treatment and care. Possible outcome measures could
be the number of cases in which consent could be
reached with ethical deliberation, or the percentage of
people who perceive that they have reached a “good
decision”. Good decisions may be reached more often
if options and ethical issues are discussed openly
before making a decision. Experiences from Austria
have shown that consensus about a practical solution Figure 2. Key factors for the implementation of systematic ethics
was reached in each of 29 cases in which a resident work
ethics meeting was held [11]. As there is not, as yet, a
gold standard protocol for the implementation of
systematic ethics work and ethical deliberation in • Receive an assignment and support from the
nursing homes, research must be an essential part of management (e.g., resources, time)
the process. Different approaches in different regions • Use a combination of a top-down and bottom-up
should be investigated in order to learn more about the model
topic. Surveys from nursing homes should be
combined with qualitative, in-depth interviews in • Define tasks and the structure of systematic
order to evaluate the different approaches, such as ethics work:
ethics peer groups/reflection groups, ethics o Usual tasks are education, case
consultation services, and ethics committees. review, and development of
Interviews with nursing home residents and relatives guidelines
help us to learn more about their views and wishes
regarding ethical challenges and decision-making in o A combination of education and case
nursing homes [15,22]. Nursing home residents are review might be reasonable in the
most concerned about “everyday ethical issues” [22]. initial phase
From our point of view there are three key factors for • Raise awareness about ethics: education for all,
the implementation of systematic ethics work, which including all personnel, patients, relatives and
are the same as those described for the other interested parties from the community
implementation of palliative care in nursing homes
(Figure 2 modified from [49]). These include: 1) • Provide information about ethics and the local
education and qualification of the whole staff; 2) to structures to staff, patients and relatives:
receive an assignment and support from the
o Is an ethics consultant or ethics
management; and 3) a change in the organization’s committee available?
culture. These key factors must be taken care of to
ensure a smooth process and sustainable success. o Who can be contacted?
Suggestions for the implementation of systematic o Information folder?
ethics work in nursing homes, and methods to handle • Include residents and their next of kin
the described challenges and obstacles that arise
during the course of the implementation process are • To ask questions has to be acceptable within the
to: organization
www.ame-journal.com 7 Bollig et al. 2016 | 3:1
o Ethics can be viewed as the question 8. Powers BA. Ethnographic analysis of everyday ethics in
about what is best for those involved the care of nursing home residents with dementia: a
taxonomy. Nurs Res. 2001;50:332–39.
and affected
9. Gjerberg E, Førde R, Pedersen R, Bollig G. Ethical
• Conduct research as part of the implementation challenges in the provision of end of life care in
process Norwegian nursing homes. Soc Sci Med. 2010;71:677–
84.
10. Bollig G. Ethical decision-making in nursing homes – a
literature study. In: Schildmann J, Gordon JS, Vollmann
Conclusions J, editors. Clinical Ethics Consultation – Theories and
Methods, Implementation, Evaluation. Farnham:
Many ethical problems occur in nursing homes, where Ashgate; 2010. p. 189–201.
there is a lack of systematic work in the field of ethics. 11. Bollig G, Schmidt G, Rosland JH, Heller A. Ethical
Ethics peer groups, ethics consultation, or ethics challenges in nursing homes – staff’s opinions and
committees could help to solve many ethical experiences with systematic ethics meetings with
participation of residents’ relatives. Scand J Caring Sci.
dilemmas in this setting. A broader inclusion of the 2015;29(4):810–823.
residents’ and relatives’ perspectives, and open 12. Loewy EH, Springer Loewy R. The ethics of terminal
discussions about “everyday ethical issues” (e.g. the care – orchestrating the end of life. New York: Kluwer
use of restraints) as well as “big ethical issues” (e.g. Academic; 2000.
decision-making in end-of-life care) are needed. The 13. Ferri CP, Prince M, Brayne C, Brodaty H, Fratiglioni L,
implementation should be individualized to meet Ganguli M, et al. Global prevalence of dementia: a
different needs, as well as geographical and cultural Delphi consensus study. Lancet. 2015;366(9503):2112–
2117.
conditions. A three-step approach to ethical decision-
14. Gjerberg E, Lillemoen L, Førde R, Pedersen R. End-of-
making in nursing homes has been proposed, and
life care communications and shared decision-making in
suggestions for the implementation process are given. Norwegian nursing homes – experiences and
As there is currently no gold standard for systematic perspectives of patients and relatives. BMC Geriatr.
ethics work in nursing homes, research should be an 2015;15:103
integral part of its implementation. 15. Bollig G, Gjengedal E, Rosland JH. They know! - Do
they? A qualitative study of residents and relatives
views on advance care planning, end-of-life care, and
decision-making in nursing homes. Palliat Med. 2015.
References [Forthcoming]
16. Gerhard C, Bollig G. Palliative care für Patienten mit
fortgeschrittener Demenz. Palliativmedizin. 2007;8:69–
1. Hayley DC, Cassel CK, Snyder L, Rudberg MA. Ethical
72. [German]
and legal issues in nursing home care. Arch Int Med.
1996;156:249–256. 17. Vandervoort A, Houttekier D, Vander Stichele R, van
der Steen JT, Van den Block L. Quality of dying in
2. Weston CM, O’Brien LA, Goldfarb NI, Roumm AR,
nursing home residents dying with dementia: Does
Isele WP, Hirschfeld K. The NJ SEED Project:
advanced care planning matter? A nationwide
evaluation of an innovative initiative for ethics training
postmortem study. PLoS One. 2014;9(3):e91130.
in nursing homes. J Am Med Dir Assoc. 2005;6:68–75.
18. Glasser G, Zweibel NR, Cassel CK. The ethics
3. Schaffer MA. Ethical problems in end-of-life decisions
committee in the nursing home. Results of a national
for elderly Norwegians. Nurs Ethics. 2007;14:242–57.
survey. J Am Geriatr Soc. 1988;36:150–156.
4. Slettebo A, Bunch EH. Solving ethically difficult care
19. Libow LS, Olson E, Neufeld RR, Martico-Greenfield T,
situations in nursing homes. Nurs Ethics. 2004;11:543–
Meyers H, Gordon N, et al. Ethics rounds at the nursing
52.
home: An alternative to an ethics committee. J Am
5. Bollig G, Pedersen R, Førde R. Etikk i sykehjem og Geriatr Soc. 1992;40(1):95–97.
hjemmetjenester. Sykepleien forskning. 2009;4:186–96.
20. Reitinger E, Wegleitner K, Heimerl K, editors.
[Norwegian]
Geschichten, die uns betroffen machen – Lernen aus
6. Reitinger E, Heller A, Heimerl K. Ethische ethischen Herausforderungen in der Altenbetreuung.
entscheidungen in der altenpflege. BtPrax. 2007;2:58– IFF-Palliative Care und OrganisationsEthik Eigenverlag,
62. [German] Vienna; 2007.
7. Sansone P. The evolution of a long-term care ethics
committee. HEC Forum. 1996;8:44–51.
www.ame-journal.com 8 Bollig et al. 2016 | 3:1
21. Chichin ER, Olson E. An ethics consult team in geriatric 37. Olson E, Chichin ER, Libow LS, Martico-Greenfield T,
long-term care. Camb Q Healthc Ethics. 1995;4:178– Neufeld RR, Mulvihill M. A center on ethics in long-
184. term care. Gerontologist. 1993; 33(2):269–274.
22. Bollig G, Gjengedal E, Rosland JH. Nothing to 38. Wilson CC, Netting FE, Henderson SK. Gaming as a
complain about? Residents’ and relatives’ views on a method for learning to resolve ethical dilemmas in long-
“good life” and ethical challenges in nursing homes. term care. Health Educ. 1988;19(1):42–44.
Nurs Ethics. 2014 0969733014557719. [Forthcoming] 39. KS.no [Internet]. Norwegian Association of Local and
23. Peile, E. Supporting primary care with ethics advice and Regional Authorities. Samarbeid om etisk
education. BMJ. 2001;323:3–4. kompetanseheving. (Kommunesektorens organisasjon,
24. Hogstel MO, Curry LC, Burns PG. Ethics committees in KS). [cited 2016 January 4]. Available from:
long-term care facilities. Geriatr Nurs. 2004;25:364– http://www.ks.no/fagomrader/helse-og-velferd/etisk-
369. kompetanseheving/.
25. Larson DG. Tobin DR. End-of-life conversations. 40. Eide T, Aadland E. Etikkhåndboka. Kommuneforlaget
Evolving practice and theory. JAMA. 2000;284:1573– AS: Oslo; 2008.
1578. 41. Heller A, Krobath T, editors. Ethik organisieren:
26. Van der Dam S, Molewijk B, Widdershoven GA, Abma Handbuch der Organisationsethik Lambertus-Verlag:
TA. Ethics support in institutional elderly care: a review Freiburg; 2010. [German]
of the literature. J Med Ethics 2014; 40(9):625–631. 42. Harvey J. Ethics cost, whether you have them or not.
27. Husebø S, Husebø BS. Omsorg ved livets slutt eller BMJ. 2001;232:936.
aktiv dødshjelp? Tidsskrift for den Norske 43. Dörries A, Neitzke G, Simon A, Vollmann J, editors.
Lægeforening. 2005;125:1848–1849. [Norwegian] Klinische Ethikberatung. Kohlhammer: Stuttgart; 2008.
28. Van der Dam S, Abma TA, Kardol MJ, Widdershoven [German]
GA. “Here’s my dilemma”. Moral case deliberation as a 44. Hallwirth-Spörk C, Heller A, Weiler K, editors.
platform for discussing everyday ethics in elderly care. Hospizkultur und Mäeutik: Offen sein für Leben und
Health Care Anal 2012;20(3):250–267. Sterben. Lambertus-Verlag: Freiburg; 2009. [German]
29. Gjerberg E, Lillemoen L, Dreyer A, Pedersen R, Førde 45. Husebø S. De døende gamle: Retningslinjer for etiske
R. Etisk kompetanseheving i norske kommuner – hva er avgjørelser om avslutning av livsforlengende
gjort, og hva har vært levedyktig over tid? Etikk I behandlingstiltak. Omsorg. 2006;4:43–45. [Norwegian]
praksis. 2014;8(2):31–49.
46. Oslo kommune Sykehjemsetaten
30. Lillemoen L, Pedersen R. Ethics reflection groups in Undervisningssykehjemmet. KEKK. Klinisk etikk-
community health services: an evaluation study. BMC komité i kommunehelsetjenesten. [cited 2015 March 1].
Med Ethics 2015;16:25. Available from:
31. Lillemoen L, Pedersen R. Ethical challenges and how to http://ush.custompublish.com/getfile.php/1595309.1875.
develop ethics support in primary health care. Nurs uurquusxbf/Brosjyre+om+Klinisk+etikkkomit%C3%A9
Ethics. 2012;20(1):96–108. +i+kommunehelsetjenesten(KEKK).pdf.
32. Bockenheimer-Lucius G, May AT. Ethikberatung – 47. EthikNetzwerk-Atenpflege.de [Internet]. Frankfurter
Ethik-Komitee in Einrichtungen der stationären Netzwerk Ethik in der Altenpflege. [cited 2015 March
Altenhilfe (EKA). Ethik in der Medizin. 2007;19:331– 1]. Available from:
339. [German]
http://www.ethiknetzwerk-altenpflege.de/index.php.
33. Brown BA, Miles SH, Aroskar MA. The prevalence and
design of ethics committees in nursing homes. J Am 48. KS.no [Internet]. "Etisk refleksjon"- et e-læringsprogram
for å heve den etiske kompetansen. [cited 2016 January
Geriatr Soc. 1987;35(11):1028–1033.
4]. Available from:
34. Osborne T, Lacy NL, Potter JF, Crabtree BF, American
Health Care Association. The prevalence, composition, http://www.ks.no/fagomrader/helse-og-velferd/etisk-
and function of ethics committees in nursing facilities: kompetanseheving/verktoy-metoder-og-
fagmateriell/etisk-refleksjon--et-e-laringsprogram-for-a-
results of a random, national survey of American Health
Care Association members. J Am Med Dir Assoc. heve-den-etiske-kompetansen/
2000;1(2):51–57. 49. Bollig, G. Palliative Care für alte und demente
35. Bachmann A, Rippe KP. Ethik-Cafés – Idee, Konzept Menschen lernen und lehren. LIT-Verlag: Berlin; 2010.
und Praxis. Pflegezeitschrift. 2004;57(12):868–869.
[German]
36. Maier M, Kälin S. Ethik-Cafés in der geriatrischen
Langzeitpflege: halten sie, was sie versprechen? Ethik
Med. 2015:1–13.
www.ame-journal.com 9 Bollig et al. 2016 | 3:1
You might also like
- Manuel - Reflection Paper - Cmca2Document1 pageManuel - Reflection Paper - Cmca2Shawn ManuelNo ratings yet
- Lecture Notes On Basic NursingDocument126 pagesLecture Notes On Basic NursingHarriet GyamfuaaNo ratings yet
- Introduction To Nursing EthicsDocument23 pagesIntroduction To Nursing EthicsAzra Baloch67% (3)
- + Rhodes - A Systematic Approach To Clinical Moral Reasoning (Clinical Ethics 2007)Document6 pages+ Rhodes - A Systematic Approach To Clinical Moral Reasoning (Clinical Ethics 2007)Mercea AlexNo ratings yet
- Nursing Care PlanDocument7 pagesNursing Care Planmcd7r883% (6)
- CHED MEMORANDUM ORDER (CMO) No. 14 Series of 2009Document129 pagesCHED MEMORANDUM ORDER (CMO) No. 14 Series of 2009lylesantos86% (49)
- Nur 300 Nursing PhilosophyDocument12 pagesNur 300 Nursing Philosophyapi-375928224No ratings yet
- Etic of CareDocument13 pagesEtic of CaredikiNo ratings yet
- 1 s2.0 S0738399110003150 Main PDFDocument5 pages1 s2.0 S0738399110003150 Main PDFkhai2646No ratings yet
- Developing Health Care Ethics ProgramDocument3 pagesDeveloping Health Care Ethics ProgramCasyl QuindorNo ratings yet
- Principles of Clinical Ethics and Their Application To PracticeDocument12 pagesPrinciples of Clinical Ethics and Their Application To PracticeHarshNo ratings yet
- 03 Dilemma & 04 Biomedical Ethics Discorse (Prof Hakimi)Document54 pages03 Dilemma & 04 Biomedical Ethics Discorse (Prof Hakimi)Zuzu FinusNo ratings yet
- Ijerph 17 04442Document13 pagesIjerph 17 04442JAMES PATRICK MONTEMAYORNo ratings yet
- Practice of Moral Case Deliberation Teaching Ethics in The Clinic. The Theory andDocument6 pagesPractice of Moral Case Deliberation Teaching Ethics in The Clinic. The Theory andQuarteto ArcadaNo ratings yet
- Research Ethics in The Intensive Care Unit: Current and Future ChallengesDocument2 pagesResearch Ethics in The Intensive Care Unit: Current and Future ChallengesJV BernNo ratings yet
- Ethics in Dentistry - A ReviewDocument7 pagesEthics in Dentistry - A ReviewNabielaNo ratings yet
- English in Medicine: Subject: Medical EthicsDocument18 pagesEnglish in Medicine: Subject: Medical Ethics060149612No ratings yet
- Ethical Problems in Nursing Management - A Cross-Sectional Survey About Solving ProblemsDocument11 pagesEthical Problems in Nursing Management - A Cross-Sectional Survey About Solving ProblemsSri RahmawatiNo ratings yet
- Jocn 14542Document16 pagesJocn 14542millionNo ratings yet
- Medical Ethics and A Ethical Dilema SDocument10 pagesMedical Ethics and A Ethical Dilema SRyukoNo ratings yet
- BioethicsDocument1 pageBioethicsKate strangeNo ratings yet
- HHS Public Access: Implementing Evidence-Based Practice in Residential Care - How Far Have We Come?Document19 pagesHHS Public Access: Implementing Evidence-Based Practice in Residential Care - How Far Have We Come?André MatosNo ratings yet
- Does Participation in Ethics Discussions Have An Impact On EthicsDocument9 pagesDoes Participation in Ethics Discussions Have An Impact On EthicsFaridRivaiNo ratings yet
- Care For Elderly PDFDocument10 pagesCare For Elderly PDFDzulfiqarNo ratings yet
- Kontio Ethical AlternativesDocument13 pagesKontio Ethical AlternativesAlina CiabucaNo ratings yet
- Sources:: A A Aa A A A ADocument7 pagesSources:: A A Aa A A A AKimmie Dadula DenayaNo ratings yet
- Journal Sharing: Veronica I. BaptistaDocument24 pagesJournal Sharing: Veronica I. BaptistaAnika GonzagaNo ratings yet
- Teaching 7 Principles For Public Health EthicsDocument10 pagesTeaching 7 Principles For Public Health Ethicsapi-491280545No ratings yet
- Rabe 1 1Document78 pagesRabe 1 1Samantha Nicole MendozaNo ratings yet
- Plano Terapeutico IHIDocument29 pagesPlano Terapeutico IHIAna Karine Girão LimaNo ratings yet
- Ethical Decision Making in Critical CareDocument5 pagesEthical Decision Making in Critical CarePALMA , JULIA A.No ratings yet
- Report of 255 Clinical Ethics ConsultatiDocument6 pagesReport of 255 Clinical Ethics ConsultatimghaseghNo ratings yet
- The Role of EthicistDocument19 pagesThe Role of EthicistZuzu FinusNo ratings yet
- Bioetihics in Clinicl LaboraoryDocument3 pagesBioetihics in Clinicl Laboraoryhira jamilNo ratings yet
- NCM108 Module1 Topic A 1stsem20-21Document4 pagesNCM108 Module1 Topic A 1stsem20-21mirai desuNo ratings yet
- Ethics HWDocument8 pagesEthics HWhelloaNo ratings yet
- Ethical Problems in Intensive Medicine: Ústav Sociálneho Lekárstva A Lekárskej EtikyDocument4 pagesEthical Problems in Intensive Medicine: Ústav Sociálneho Lekárstva A Lekárskej EtikyAlexandros LazarouNo ratings yet
- Ethical Decision Making in Clinical PracticeDocument50 pagesEthical Decision Making in Clinical PracticesafiraNo ratings yet
- Medical Ethics: A Physician's Guide to Clinical MedicineFrom EverandMedical Ethics: A Physician's Guide to Clinical MedicineNo ratings yet
- Health Care Ethics Programs in U.S. Hospitals: Results From A National SurveyDocument14 pagesHealth Care Ethics Programs in U.S. Hospitals: Results From A National SurveySNo ratings yet
- Ethical Final EssayDocument6 pagesEthical Final EssayTitus KoechNo ratings yet
- Moodule 12Document14 pagesMoodule 12camille nina jane navarroNo ratings yet
- BioethicsDocument1 pageBioethicsNica Mariz Dela CruzNo ratings yet
- Values and EthicsDocument21 pagesValues and EthicsPaulo Xander Corpin Basa100% (1)
- International Journal of Medical Informatics: Sara Atanasova, Tanja Kamin, Gregor Petri CDocument9 pagesInternational Journal of Medical Informatics: Sara Atanasova, Tanja Kamin, Gregor Petri Cmlee5638valNo ratings yet
- Ethical Dilemmas of End of Life Care in Intensive Care Unit: A Literature ReviewDocument9 pagesEthical Dilemmas of End of Life Care in Intensive Care Unit: A Literature ReviewEviNo ratings yet
- Ethical Considerations in Emergency Care: Kenneth V. Iserson, MD, MBA, FacepDocument8 pagesEthical Considerations in Emergency Care: Kenneth V. Iserson, MD, MBA, FacepJenry Reyes TrispaNo ratings yet
- America College Physicians Ethics Manual 2011Document32 pagesAmerica College Physicians Ethics Manual 2011juan lopezNo ratings yet
- EthicsDocument14 pagesEthicsP QqNo ratings yet
- Hes Sas 2 - Ponce, Kristel Mae o PDFDocument12 pagesHes Sas 2 - Ponce, Kristel Mae o PDFPonce Kristel Mae ONo ratings yet
- Health Social Care Comm - 2011 - Lucock - Self Care in Mental Health Services A Narrative ReviewDocument15 pagesHealth Social Care Comm - 2011 - Lucock - Self Care in Mental Health Services A Narrative ReviewDina NabilaNo ratings yet
- Hes Sas 2 - Ponce, Kristel Mae oDocument12 pagesHes Sas 2 - Ponce, Kristel Mae oPonce Kristel Mae ONo ratings yet
- Microethics The Ethics of Everyday CliniDocument7 pagesMicroethics The Ethics of Everyday ClinimghaseghNo ratings yet
- A Practical Approach To Ethical Decision MakingDocument5 pagesA Practical Approach To Ethical Decision MakingEmmy IsaNo ratings yet
- EditKaidah Dasar Bioetik &Document49 pagesEditKaidah Dasar Bioetik &Chimul Lavigne 'L'No ratings yet
- Session 10 - NGU6400Document20 pagesSession 10 - NGU6400s9664960No ratings yet
- KD BN Prima Facie 2013Document60 pagesKD BN Prima Facie 2013Aldo HamkaNo ratings yet
- Etika Profesi Dan Hukum Kesehatan: Fikri Mourly WahyudiDocument23 pagesEtika Profesi Dan Hukum Kesehatan: Fikri Mourly WahyudiArya MuhammadNo ratings yet
- Telerobots ArticulosDocument9 pagesTelerobots ArticulosDanilo Carvajal MarinNo ratings yet
- Ethics in Community Health NursingDocument22 pagesEthics in Community Health NursingAbdelrahman SwilamNo ratings yet
- Medical Ethics Dissertation TopicsDocument8 pagesMedical Ethics Dissertation TopicsThesisPaperHelpCanada100% (1)
- What Matters Most For End-Of-Life Care? Perspectives From Community-Based Palliative Care Providers and AdministratorsDocument8 pagesWhat Matters Most For End-Of-Life Care? Perspectives From Community-Based Palliative Care Providers and AdministratorsPutri Tamara DasantosNo ratings yet
- NURS3001 NotesDocument40 pagesNURS3001 NotesjamestouffinNo ratings yet
- The Four Topics Chart:: A Tool For Clinical Ethics Case AnalysisDocument25 pagesThe Four Topics Chart:: A Tool For Clinical Ethics Case AnalysisZuzu FinusNo ratings yet
- Legal Aspects of NursingDocument9 pagesLegal Aspects of NursingleslyjoyNo ratings yet
- Application of Informatics in AdministrationDocument30 pagesApplication of Informatics in Administrationmagdaashaaban100% (1)
- BS BuzzDocument10 pagesBS BuzzBS Central, Inc. "The Buzz"No ratings yet
- Construct Validation of The Nurse Cultural Competence Scale: A Hierarchy of AbilitiesDocument7 pagesConstruct Validation of The Nurse Cultural Competence Scale: A Hierarchy of Abilitiesandriaeypreel1224No ratings yet
- Profilel (Delhi Institute of Paramedical Science)Document9 pagesProfilel (Delhi Institute of Paramedical Science)Crib DelhiNo ratings yet
- Patient SafetyDocument18 pagesPatient SafetySuhatman AhNo ratings yet
- Week 10 WorksheetDocument13 pagesWeek 10 WorksheetAb Staholic BoiiNo ratings yet
- EPN I New Book Chapter 1-3Document19 pagesEPN I New Book Chapter 1-3iyanNo ratings yet
- Your Pre-Application ChecklistDocument3 pagesYour Pre-Application ChecklistAbdeljalil ER-RAKIBINo ratings yet
- Prof. Joseph Bahian Abang,: Ahse, BSN, RN, Man (C)Document67 pagesProf. Joseph Bahian Abang,: Ahse, BSN, RN, Man (C)Yucef Bahian-AbangNo ratings yet
- Compre Exam Review - Hospital Planning, Infrastructure., Design and MaintenanceDocument2 pagesCompre Exam Review - Hospital Planning, Infrastructure., Design and MaintenancePatricia PagsolinganNo ratings yet
- Nursing Practice IIDocument18 pagesNursing Practice IIstuffednurseNo ratings yet
- 1 Client Records 1Document15 pages1 Client Records 1Grape JuiceNo ratings yet
- QUESTIONNAIREDocument3 pagesQUESTIONNAIREKatherine Aplacador100% (4)
- Lecture of NCM 100Document123 pagesLecture of NCM 100karendelarosa06277100% (1)
- IV-Year Model Question Paper - 2016-SchemeDocument4 pagesIV-Year Model Question Paper - 2016-SchemeJeyachithra83% (6)
- Nursing Bylaws 2009Document30 pagesNursing Bylaws 2009Silviana FassicaNo ratings yet
- Kualitas Pelayanan Keperawatan Di Rumah Sakit Umum Daerah (Rsud) Kota BaubauDocument10 pagesKualitas Pelayanan Keperawatan Di Rumah Sakit Umum Daerah (Rsud) Kota BaubauAmaNo ratings yet
- Neonatal Nurse Thesis StatementDocument8 pagesNeonatal Nurse Thesis StatementjenniferontiveroskansascityNo ratings yet
- NCP UreteroDocument1 pageNCP UreteroCerie Anne OlayNo ratings yet
- NCPDocument3 pagesNCPDelaine Mae MierNo ratings yet
- ST Johns Newsletter Issue 3Document5 pagesST Johns Newsletter Issue 3Parish MagazineNo ratings yet
- Bahasa InggrisDocument2 pagesBahasa InggrisAde Muliana LestariNo ratings yet
- Nursing LeadershipDocument152 pagesNursing LeadershipBSN4C2010No ratings yet
- A Mixed-Method Research On Stress Among Government Workers: Analysis Using The Health and Safety Executive Management StandardsDocument8 pagesA Mixed-Method Research On Stress Among Government Workers: Analysis Using The Health and Safety Executive Management StandardsPsychology and Education: A Multidisciplinary JournalNo ratings yet