Professional Documents
Culture Documents
ASCO Adjuvant Intravesical BCG
ASCO Adjuvant Intravesical BCG
Uploaded by
Chirac OanaCopyright:
Available Formats
You might also like
- This Study Resource Was Shared ViaDocument4 pagesThis Study Resource Was Shared ViaKyuSheen100% (1)
- Combinatorial Test Design (CTD) : IBM Haifa Research LaboratoryDocument7 pagesCombinatorial Test Design (CTD) : IBM Haifa Research LaboratoryChirac OanaNo ratings yet
- Compassionate Sciences - RedactedDocument184 pagesCompassionate Sciences - RedactedNew Jersey marijuana documentsNo ratings yet
- Conceptual Framework SampleDocument2 pagesConceptual Framework SampleReYa Buenaventura100% (1)
- The Short Textbook of Pediatrics PDFDocument38 pagesThe Short Textbook of Pediatrics PDFGolla manoharNo ratings yet
- Sfakianos 2015Document7 pagesSfakianos 2015nimaelhajjiNo ratings yet
- Synchronous Bilateral Breast CancersDocument4 pagesSynchronous Bilateral Breast CancersEnrico GaharaNo ratings yet
- MedicineDocument5 pagesMedicinepriyanka hermawanNo ratings yet
- Jasirwan 2019Document11 pagesJasirwan 2019MuliaNo ratings yet
- Prognostic Value of C Reactive Protein - AlbuminDocument8 pagesPrognostic Value of C Reactive Protein - AlbuminfernandallmagalhaesNo ratings yet
- Synchronous Bilateral Breast Cancers: Abst TDocument4 pagesSynchronous Bilateral Breast Cancers: Abst TLastrii HillaryNo ratings yet
- 8424365Document8 pages8424365Melody CyyNo ratings yet
- Theoncologist 15440Document8 pagesTheoncologist 15440nimaelhajjiNo ratings yet
- COGNITION A Prospective Precision Oncology TrialDocument12 pagesCOGNITION A Prospective Precision Oncology Trialveaceslav coscodanNo ratings yet
- Achenbach, 2015Document10 pagesAchenbach, 2015Leonardo Arévalo MoraNo ratings yet
- Impact of Comorbidity On Colorectal Cancer Screening Cost-Effectiveness Study in Diabetic PopulationsDocument9 pagesImpact of Comorbidity On Colorectal Cancer Screening Cost-Effectiveness Study in Diabetic PopulationsAna MîndrilăNo ratings yet
- 00006Document6 pages00006carlangaslaraNo ratings yet
- 1475 2891 12 118Document8 pages1475 2891 12 118SunardiasihNo ratings yet
- Ca Colon 2Document19 pagesCa Colon 2Tob JurNo ratings yet
- Ijmr 1588 22 R3Document6 pagesIjmr 1588 22 R3Aditi GoyalNo ratings yet
- Local Recurrence After Breast-Conserving Therapy I - 240415 - 080523Document12 pagesLocal Recurrence After Breast-Conserving Therapy I - 240415 - 080523Khan ZareenNo ratings yet
- Interval Colorectal Cancers in Inflammatory Bowel Disease: The Grim Statistics and True StoriesDocument12 pagesInterval Colorectal Cancers in Inflammatory Bowel Disease: The Grim Statistics and True StoriespancholarpancholarNo ratings yet
- Xiaoli HuDocument12 pagesXiaoli HuYohanes AdhityaNo ratings yet
- BR Vs CHOPDocument8 pagesBR Vs CHOPabdullahNo ratings yet
- 1019 5298 1 PBDocument11 pages1019 5298 1 PBm907062008No ratings yet
- Beal 2020Document17 pagesBeal 2020Nikos SerifisNo ratings yet
- Articulo Cirgua Musinoso Nodulos NegtivDocument10 pagesArticulo Cirgua Musinoso Nodulos NegtivJorge VintimillaNo ratings yet
- Comprehensive Precision Medicine Study Protocol On The Heterogeneity of Taiwanese Breast Cancer PatientsDocument14 pagesComprehensive Precision Medicine Study Protocol On The Heterogeneity of Taiwanese Breast Cancer Patients郭竹瑩No ratings yet
- Colorectal Cancer Lynch Nyhan SyndromeDocument9 pagesColorectal Cancer Lynch Nyhan SyndromeSteffanio SebastianNo ratings yet
- 19#prognostic HCC 2021Document7 pages19#prognostic HCC 2021hitashiNo ratings yet
- s13027 020 00299 3Document10 pagess13027 020 00299 3Remona RemoraNo ratings yet
- 1540 1413 Article p1529 PDFDocument26 pages1540 1413 Article p1529 PDFEvelynππ θσυNo ratings yet
- Allen2021 Article ChemotherapyVersusChemotherapyDocument8 pagesAllen2021 Article ChemotherapyVersusChemotherapyXavier QuinteroNo ratings yet
- Arends 2016Document7 pagesArends 2016DavorIvanićNo ratings yet
- Risk Factors For Pelvic and Distant Recurrence in Locally AdvancedDocument7 pagesRisk Factors For Pelvic and Distant Recurrence in Locally AdvancedfernandallmagalhaesNo ratings yet
- Colorectal CancerDocument9 pagesColorectal CancerPatricia ClarineNo ratings yet
- 10.1245/s10434 018 6369 XDocument9 pages10.1245/s10434 018 6369 Xsayumiholic89No ratings yet
- Jcav 13 P 0051Document11 pagesJcav 13 P 0051hasna muhadzibNo ratings yet
- 10 1093@icvts@ivz140Document8 pages10 1093@icvts@ivz140PEDRO JESuS GUERRA CANCHARINo ratings yet
- Comparison of Radical Cystectomy With Conservative Treatment in Geriatric ( 80) Patients With Muscle-Invasive Bladder CancerDocument9 pagesComparison of Radical Cystectomy With Conservative Treatment in Geriatric ( 80) Patients With Muscle-Invasive Bladder CancerjustforuroNo ratings yet
- 1 s2.0 S2531043719302156 MainDocument9 pages1 s2.0 S2531043719302156 Mainpulmonologi UnsyiahNo ratings yet
- Mallappa Et Al-2013-Colorectal DiseaseDocument6 pagesMallappa Et Al-2013-Colorectal DiseaseDumitru RadulescuNo ratings yet
- 10 1097@mou 0b013e328356ac20Document6 pages10 1097@mou 0b013e328356ac20nimaelhajjiNo ratings yet
- Research Article: Clinical Characteristics in Patients With Triple Negative Breast CancerDocument6 pagesResearch Article: Clinical Characteristics in Patients With Triple Negative Breast Cancerlapkas donjuanNo ratings yet
- EeDocument8 pagesEeEstiPramestiningtyasNo ratings yet
- 1 s2.0 S001236922200575XDocument9 pages1 s2.0 S001236922200575XYulia Niswatul FauziyahNo ratings yet
- Extracellular Nucleic Acids and Cancer: Michael - Fleischhacker@uk-Halle - de Bernd - Schmidt@uk-Halle - deDocument55 pagesExtracellular Nucleic Acids and Cancer: Michael - Fleischhacker@uk-Halle - de Bernd - Schmidt@uk-Halle - deAirin LeonieNo ratings yet
- 3994 - Adjusting Cyclophosphamide Dose in Obese PatientsDocument4 pages3994 - Adjusting Cyclophosphamide Dose in Obese PatientsErnika SariNo ratings yet
- Prophylactic MastectomyDocument5 pagesProphylactic MastectomyMuhammad Darussalam DarwisNo ratings yet
- NGS de Panel para CCR - JCO 2015 - Costo-EfectividadDocument12 pagesNGS de Panel para CCR - JCO 2015 - Costo-EfectividadSebas Barrionuevo VediaNo ratings yet
- Lotan Et Al. Molecular Marker For Rec and Cancer Specific Survival Post Radical CystectomyDocument7 pagesLotan Et Al. Molecular Marker For Rec and Cancer Specific Survival Post Radical CystectomyyuenkeithNo ratings yet
- Patient Survival Report 1Document5 pagesPatient Survival Report 1Rabeya Bibi 193-15-13510No ratings yet
- MainDocument8 pagesMainIoana CucuNo ratings yet
- Vandenbosch 2011Document8 pagesVandenbosch 2011nimaelhajjiNo ratings yet
- EJGO2022054 Cervical CaDocument8 pagesEJGO2022054 Cervical CaRahmayantiYuliaNo ratings yet
- JournalReading ONKO JeffriSyaputraDocument17 pagesJournalReading ONKO JeffriSyaputraYarman War officialNo ratings yet
- Research Article: Prevalence of Cachexia in Cancer PatientsDocument9 pagesResearch Article: Prevalence of Cachexia in Cancer Patientsadri20121989No ratings yet
- Advanced Non-Small Cell Lung Cancer in Patients Aged 45 Years or Younger: Outcomes and Prognostic FactorsDocument8 pagesAdvanced Non-Small Cell Lung Cancer in Patients Aged 45 Years or Younger: Outcomes and Prognostic FactorsAnnisa DiendaNo ratings yet
- How I Treat Newly Diagnosed Chronic Phase CMLDocument9 pagesHow I Treat Newly Diagnosed Chronic Phase CMLDenisse SarabiaNo ratings yet
- Howard 2012Document5 pagesHoward 20121alexandra12No ratings yet
- Effect of More Vs Less Frequent Follow-Up Testing On Overall and Colorectal Cancer-Specific Mortality in Patients With Stage II or III Colorectal CancerDocument9 pagesEffect of More Vs Less Frequent Follow-Up Testing On Overall and Colorectal Cancer-Specific Mortality in Patients With Stage II or III Colorectal CancerMr. LNo ratings yet
- Local Control in Metastatic Neuroblastoma in Children Over 1 Year of AgeDocument8 pagesLocal Control in Metastatic Neuroblastoma in Children Over 1 Year of AgePutri ManurungNo ratings yet
- GastroDocument9 pagesGastroAnonymous plYGwXNo ratings yet
- Changes in Ki 67 in Residual Tumor and Outcome of Primary I - 2022 - Clinical BRDocument9 pagesChanges in Ki 67 in Residual Tumor and Outcome of Primary I - 2022 - Clinical BRAd AdrianaNo ratings yet
- Settipane 1981Document5 pagesSettipane 1981Chirac OanaNo ratings yet
- Martinez 2015Document1 pageMartinez 2015Chirac OanaNo ratings yet
- Temple 1981Document6 pagesTemple 1981Chirac OanaNo ratings yet
- AnatolJCardiol 7 2 27 30Document4 pagesAnatolJCardiol 7 2 27 30Chirac OanaNo ratings yet
- Decribing Places Buildings Successful Writing - Intermediate SBDocument6 pagesDecribing Places Buildings Successful Writing - Intermediate SBChirac OanaNo ratings yet
- Hofbauer 2015Document5 pagesHofbauer 2015Chirac OanaNo ratings yet
- WHOPIR BB NCIPD 11-13march2020Document15 pagesWHOPIR BB NCIPD 11-13march2020Chirac OanaNo ratings yet
- Reg Form - Farmacovigilenta - 21-23sep2020Document1 pageReg Form - Farmacovigilenta - 21-23sep2020Chirac OanaNo ratings yet
- Conflict of Interest Disclosures: Patient Case # 1Document28 pagesConflict of Interest Disclosures: Patient Case # 1Chirac OanaNo ratings yet
- Meropenem VenusDocument7 pagesMeropenem VenusChirac OanaNo ratings yet
- Information Technology, 19 (1), 94-115. Retrieved From: Resources - Perpusnas.go - Id:2057/docview/1951416783?accountid 25704Document2 pagesInformation Technology, 19 (1), 94-115. Retrieved From: Resources - Perpusnas.go - Id:2057/docview/1951416783?accountid 25704AnggiNo ratings yet
- Indonesian Guideline H Pylori Dyspepsia 2022Document19 pagesIndonesian Guideline H Pylori Dyspepsia 2022Daniel TariganNo ratings yet
- Forensic Medical Examination of Alive Persons: CCCCCCC CDocument7 pagesForensic Medical Examination of Alive Persons: CCCCCCC CDrGurjyot NandaNo ratings yet
- SeminarDocument34 pagesSeminarMuhammad Faiz Satria WibowoNo ratings yet
- IHOP - 09.13.39 - Humpty Dumpty Fall Assessment ScaleDocument1 pageIHOP - 09.13.39 - Humpty Dumpty Fall Assessment ScaleRomiko NersNo ratings yet
- Ebook Campbell Walsh Urology 12Th Edition Review 3E Mar 2 2020 - 0323639690 - Elsevier PDF Full Chapter PDFDocument68 pagesEbook Campbell Walsh Urology 12Th Edition Review 3E Mar 2 2020 - 0323639690 - Elsevier PDF Full Chapter PDFfrank.daniels751100% (29)
- Employee Benefits CGHSDocument3 pagesEmployee Benefits CGHSaruvindhuNo ratings yet
- Hospital ManagementDocument3 pagesHospital ManagementFebriciaKristinaNo ratings yet
- PQCNC NHPC LS3 Noel 2020 Workload Indicators 20200310.Document23 pagesPQCNC NHPC LS3 Noel 2020 Workload Indicators 20200310.kcochranNo ratings yet
- Adult Neurological Observation Chart Education PackageDocument101 pagesAdult Neurological Observation Chart Education PackageRajiNo ratings yet
- Magdy El-Masry Prof. of Cardiology Tanta UniversityDocument55 pagesMagdy El-Masry Prof. of Cardiology Tanta UniversityPrabJot SinGhNo ratings yet
- David Perlmutter Full Length InterviewDocument28 pagesDavid Perlmutter Full Length InterviewKalNo ratings yet
- MeaslesDocument11 pagesMeaslesMarivic DianoNo ratings yet
- History of Anaesthesia Oropharyngeal and Nasopharyngeal Airways: I (1880-1995)Document7 pagesHistory of Anaesthesia Oropharyngeal and Nasopharyngeal Airways: I (1880-1995)Lucille IlaganNo ratings yet
- ATS-ERS Statement On Respiratory Muscle TestingDocument107 pagesATS-ERS Statement On Respiratory Muscle TestingLuizaNo ratings yet
- PGDHMDocument36 pagesPGDHMAndy JadNo ratings yet
- Internship ReportDocument35 pagesInternship ReportSamu LuwagunNo ratings yet
- Role and ResponsibilitiesDocument17 pagesRole and Responsibilitiesprabha karanNo ratings yet
- College of Medical Technology Principle of Medical Laboratory Science 1 (MLS 037)Document14 pagesCollege of Medical Technology Principle of Medical Laboratory Science 1 (MLS 037)Cindy Mae A. PogoyNo ratings yet
- Bupa Global List OF Contracted Providers in Egypt - Nov 2020Document11 pagesBupa Global List OF Contracted Providers in Egypt - Nov 2020MahmoudAbdElGhaniNo ratings yet
- Health Information SystemDocument11 pagesHealth Information SystemVineeta Jose100% (1)
- Med Surg Chap QuestionsDocument9 pagesMed Surg Chap Questionslani0% (1)
- Hh2sgonzupzxf4gu1w1wym1fDocument1 pageHh2sgonzupzxf4gu1w1wym1fHarsh AryaNo ratings yet
- Chapter 30 Assessment and Management of Patients With Vascular Disorders and Problems of Peripheral CirculationDocument23 pagesChapter 30 Assessment and Management of Patients With Vascular Disorders and Problems of Peripheral CirculationAbel C. Idusma Jr.No ratings yet
- Community Mental Health ProgramDocument9 pagesCommunity Mental Health Programpreeti sharma100% (1)
- Disorders of The Blood and Neoplastic DisordersDocument72 pagesDisorders of The Blood and Neoplastic DisordersavisenicNo ratings yet
ASCO Adjuvant Intravesical BCG
ASCO Adjuvant Intravesical BCG
Uploaded by
Chirac OanaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
ASCO Adjuvant Intravesical BCG
ASCO Adjuvant Intravesical BCG
Uploaded by
Chirac OanaCopyright:
Available Formats
Health Care Delivery
Original Contribution
Adjuvant Intravesical Bacillus Calmette-Guérin Therapy and
Survival Among Elderly Patients With Non–Muscle-Invasive
Bladder Cancer
By Benjamin A. Spencer, MD, MPH, Russell B. McBride, MPH, Dawn L. Hershman, MD, MS,
Donna Buono, MS, Harry W. Herr, MD, Mitchell C. Benson, MD, Supriya Gupta-Mohile, MD, MS,
and Alfred I. Neugut, MD, PhD
Columbia University; Memorial Sloan-Kettering Cancer Center, New York; and University of Rochester, Rochester, NY
Abstract Results: Of 23,932 patients with NMIBC identified, 22% re-
Purpose: National guidelines recommend adjuvant intravesi- ceived adjuvant intravesical BCG. Predictors of receipt were
cal Bacillus Calmette-Guérin (BCG) therapy for higher-risk non– stages Tis and T1, higher grade, and urban residence. Age ⬎ 80
muscle-invasive bladder cancer (NMIBC). Although a survival years, fewer than two comorbidities, and not being married were
benefit has not been demonstrated, randomized trials have associated with decreased use. In the survival analysis, BCG use
shown reduced recurrence and delayed progression after its was associated with better OS (hazard ratio [HR], 0.87; 95% CI,
use. We investigated predictors of BCG receipt and its associa- 0.83 to 0.92) in the entire cohort and BCSS among higher-grade
tion with survival for older patients with NMIBC. cancers (poorly differentiated: HR, 0.78; 95% CI, 0.72 to 0.85;
undifferentiated: HR, 0.66; 95% CI, 0.56 to 0.77).
Patients and Methods: We identified individuals with
NMIBC registered in the Surveillance, Epidemiology, and End
Results–Medicare database from 1991 to 2003. We used logistic Conclusion: Despite guidelines recommending its use, BCG
regression to compare those treated with BCG within 6 months is administered to less than one quarter of eligible patients. This
of initial diagnosis with those not treated, adjusting for demo- large population-based study found improved OS and BCSS
graphic and clinical factors. Cox proportional hazards modeling were associated with use of adjuvant intravesical BCG among
was used to analyze the association between BCG and overall older patients with NMIBC. Better-designed clinical trials fo-
survival (OS) and bladder cancer–specific survival (BCSS) for the cusing on higher-grade cancers are needed to confirm these
entire cohort and within tumor grades. findings.
Introduction 85% and 70%, respectively.4 NMIBC has a high likelihood of
The management of non–muscle-invasive bladder cancer recurrence after treatment with TUR alone. For example, in
(NMIBC) remains a common and complex clinical challenge. one large cohort of T1 bladder tumors treated only with TUR,
Approximately 70,000 new cases of bladder cancer are diag- 75% and 90% recurred by 5 and 10 years of follow-up, respec-
nosed annually in the United States, with two thirds of cases tively.5 One third progressed to muscle invasion within 5
occurring in persons older than age 65 years.1,2 Three quarters years.6
of incident cases are considered superficial or non–muscle in- Intravesical therapy has been investigated in the adjuvant
vasive: stages Ta, T1, and Tis.3 The risk of recurrence and pro- setting after TUR in an attempt to improve the outcomes of
gression of NMIBC is influenced by tumor stage, grade, size, patients with NMIBC. Bacillus Calmette-Guérin (BCG) is an
number of tumors, and previous history of and length of time to immunotherapeutic agent that is effective in the treatment of
recurrence. Overall, 65% of non–muscle-invasive tumors will NMIBC. Several clinical trials have demonstrated statistically
recur, and 25% of these will progress to a higher stage or grade.3 significant reductions in short- and long-term recurrence rates
Ta lesions are usually low grade and rarely progress to a higher with adjuvant BCG treatment after complete TUR of Ta and
stage or grade. The clinical behavior of T1 cancers is heteroge- T1 lesions when compared with TUR alone or with intravesical
neous, with some being indolent and others more aggressive, chemotherapy.7-10 Adjuvant BCG is effective treatment for Tis,
with a tendency to recur and progress to muscle-invasive disease eradicating 80% of cases and improving disease-specific sur-
(T2). Tis (carcinoma in situ [CIS]) lesions carry a much higher vival.11 A single randomized trial of 86 patients with high-risk
risk of recurrence and progression to muscle-invasive disease. disease and 15-year follow-up demonstrated a survival advan-
Various options are available for management of NMIBC, tage for BCG in conjunction with TUR.4,12 Three meta-anal-
including transurethral resection (TUR), adjuvant intravesical yses concluded that BCG in conjunction with TUR reduced
therapy, and radical cystectomy. TUR is the initial step for the recurrence13-15 and progression16 of NMIBC but had no effect
diagnosis and management of NMIBC. After TUR, 10-year on overall (OS) or disease-specific survival.16 The inability to
disease-specific survival for persons with Ta and T1 tumors is demonstrate a survival advantage likely results from the major-
92 JOURNAL OF ONCOLOGY PRACTICE • V O L . 9, I S S U E 2 Copyright © 2012 by American Society of Clinical Oncology
Downloaded from ascopubs.org by 86.120.168.196 on December 2, 2021 from 086.120.168.196
Copyright © 2021 American Society of Clinical Oncology. All rights reserved.
Adjuvant BCG for Non–Muscle-Invasive Bladder Cancer
ity of studies having relatively short follow-up, given the pro- ical stage into equivalent TNM stages: extension codes 00 and
longed natural history of NMIBC and the low risk of 06 were considered CIS; 01, 03, 06, and 10 were considered Ta;
progression from non–muscle-invasive to invasive disease. and 15 was considered T1. Patients without an extension code
BCG is considered safe as an intravesical agent, with fewer than were considered AJCC stage I, not otherwise specified. Age at
5% of patients experiencing a major adverse event.17 diagnosis was categorized in pentads starting at 65 years. We
Thus, no consensus exists regarding the impact of adjuvant recoded the SEER marital status variable into married, not mar-
intravesical BCG on OS or disease-specific survival. Specifi- ried, and unknown. Area-based socioeconomic (SES) status was
cally, early treatment at first diagnosis of bladder cancer has not estimated using a composite of three different variables from
been consistently studied. Nevertheless, the National Compre- the 2000 census, using a method described previously by
hensive Cancer Network guideline currently recommends ad- Chamie et al.20 Individuals were ranked into quintiles on the
juvant BCG after TUR for all non–muscle-invasive tumors that basis of their census tract median household income, percent-
are high grade and/or stage Tis or T1.18 Using a large popula- age of persons age ⱖ 25 years with at least a high school educa-
tion-based database, we sought to determine the predictors of tion, and percentage of people below the poverty level. Each
receipt of intravesical therapy and investigate the influence of patient was assigned a composite SES score based on the average
intravesical BCG on survival in a large cohort of elderly patients of these three rankings.
with NMIBC.
Comorbid Disease
Patients and Methods We computed a comorbidity score for each patient using the
Data Source Klabunde adaptation of the Charlson comorbidity index.21,22
Medicare inpatient and outpatient claims were searched from
We analyzed data from the Surveillance, Epidemiology, and
365 days before to 120 days after the diagnosis of cancer for all
End Results (SEER) database linked with diagnostic and pro-
International Classification of Diseases, Ninth Revision, Clin-
cedural billing claims from Medicare.19 SEER, under the aus-
ical Modification (ICD-9-CM) diagnostic codes corresponding
pices of the National Cancer Institute, has collected tumor
to each of the following comorbid conditions: myocardial in-
registry data on selected populations across the United States,
farction, congestive heart failure, peripheral vascular disease,
representing approximately 26% of the population, since 2000.
cerebrovascular disease, dementia, chronic pulmonary disease,
SEER provides information on tumor histology, location, dis-
connective tissue disease, peptic ulcer disease, mild to severe
ease stage, treatment, and survival along with selected census
liver disease, diabetes with or without end-organ damage, hemi-
tract–level sociodemographic information. The Medicare data-
plegia, moderate or severe renal disease, and AIDS. Each disease
base includes Medicare A and B eligibility status, dates of en-
category was weighted based on the Charlson index, and pa-
rollment in health maintenance organizations (HMOs), and
tients were assigned a score of 0, 1, or ⬎ 1.
billed claims, including inpatient and outpatient services, pro-
cedures, and diagnoses.
Treatment Characteristics
Sample Selection We searched the Medicare physician claims files (National
We identified all individuals within the SEER-Medicare data- Claims History database), hospital outpatient claims files (Out-
base age ⱖ 65 years who received a pathologically confirmed pat), and Medicare provider review files (Medicare Provider
primary diagnosis of bladder cancer (SEER site of cancer, 58) Analysis and Review database) for procedural and treatment
from January 1, 1991, to December 31, 2002. We excluded codes related to adjuvant cancer therapy within the first 6
patients who were enrolled in an HMO from 12 months before months from diagnosis. Instances of intravesical chemotherapy
to 12 months after diagnosis and who were not covered by were identified on the basis of having claims for the following
Medicare Parts A or B over the same period, because those in codes: instillation of intravesical BCG, Level II Health Care
HMOs are not billed within Medicare only. We limited our Procedure Coding System J9031, and instillation of intravesical
sample to those with stage I (according to the American Joint anticarcinogenic agent, Current Procedural Terminology
Committee on Cancer) NMIBC (N ⫽ 24,982). We excluded 51720. Although the ability of SEER-Medicare claims data to
patients who died during the first 3 months after a diagnosis of reliably identify a wide-ranging set of cancer treatments has
NMIBC (n ⫽ 535), who had a claim for intravesical BCG or been described previously, the validity of intravesical chemo-
bladder cancer surgery more than 14 days before the date of therapy has not been evaluated.23,24
bladder cancer diagnosis (n ⫽ 353), who died on the date of
diagnosis (n ⫽ 1), and who had fewer than 30 days of follow-up Mortality and Survival
(n ⫽ 161). This resulted in a cohort of 23,932 patients. Survival was calculated in months from the date of bladder
cancer diagnosis to the date of death according to SEER. Sur-
Tumor and Patient Characteristics vival was censored as of the last Medicare coverage month when
Data on clinical stage, histologic grade, age, race/ethnicity, sex, patients were known to be alive or as of December 31, 2002.
marital status, type of hospital, and area of residence were taken Bladder cancer–specific mortality was assessed with ICD-9
from the SEER database. We recoded extension codes for clin- codes 188.0 to 188.9 for patients dying as a result of bladder
Copyright © 2012 by American Society of Clinical Oncology M A R C H 2013 • jop.ascopubs.org 93
Downloaded from ascopubs.org by 86.120.168.196 on December 2, 2021 from 086.120.168.196
Copyright © 2021 American Society of Clinical Oncology. All rights reserved.
Spencer et al
cancer from 1991 to 1998 and ICD-10 codes C67.0 to C67.9 therapy within 6 months of diagnosis of NMIBC. In a sub-
from 1999 to 2002. group analysis stratified by stage (data not shown), we found
that OS was improved in higher grades (poorly differentiated:
Statistical Analyses OR, 0.78; 95% CI, 0.72 to 0.85 and undifferentiated: OR,
We used the 2 test to compare the distributions of clinical and 0.66; 95% CI, 0.56 to 0.77) but not in well- or moderately
demographic characteristics (age at diagnosis, sex, year of diag- differentiated grades. Although there was only a trend toward a
nosis, race, stage, grade, marital status, comorbidity score, and survival advantage for BCSS in the entire cohort (OR, 0.90;
area SES quintile), comparing those who received adjuvant in- 95% CI, 0.80 to 1.01), adjuvant BCG conferred a significant
travesical BCG within 6 months with those who did not. We survival advantage among subsets of higher-grade cancers
used univariate and multivariate logistic regression models to (poorly differentiated: OR, 0.70; 95% CI, 0.59 to 0.84 and
identify predictors of receipt of BCG from among the measured undifferentiated: OR, 0.56; 95% CI, 0.41 to 0.77). OS was
clinical and demographic characteristics. We adjusted these worse among patients with well- and moderately differentiated
models for age, sex, year of diagnosis, race, marital status, co- tumors who received BCG. Older age, higher grade, stages T1
morbidity score, urban/rural location, and area SES quintile. and Tis, more comorbidities, and not being married were risk
Among patients who survived at least 12 weeks, we developed factors for both all-cause and bladder cancer–specific mortality.
Cox proportional hazards models to analyze the association of Male sex was associated with a greater likelihood of all-cause
BCG treatment with OS and bladder cancer–specific survival mortality, and black and Hispanic races were risk factors for
(BCSS). Finally, we generated adjusted Kaplan-Meier curves bladder cancer–specific mortality.
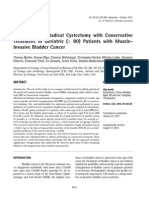
for each of the survival end points as well as curves stratified by Adjusted Kaplan-Meier survival curves comparing treat-
tumor grade. All statistical analyses were performed using SAS ment groups are shown for the entire cohort in Figure 1 and
Version 9.2 (SAS Institute, Cary, NC). The study protocol was stratified by tumor grade in Appendix Figures A1A to A1D
approved by the Columbia University Medical Center Institu- (online only). Those receiving adjuvant intravesical BCG expe-
tional Review Board. rienced a statistically significant survival advantage over the
10-year follow-up period compared with those not receiving
Results therapy (HR, 0.87; 95% CI, 0.83 to 0.92). The absolute sur-
The sample was predominantly male (74%), white (93%), mar- vival advantage at 5 years was approximately 4%. Median sur-
ried (63%), and without comorbidities (57%); most resided in vival was approximately 2 years greater in the BCG group. In
urban locales (91%); and the mean age was 77 years (Table 1). Figures A1A to A1D, OS stratified by histologic grade is plotted
Sixty-two percent of patients had stage Ta disease, and 64% had for the treatment groups. Statistically significant differences in
well- or moderately differentiated tumors. Differences between OS and disease-specific survival were seen among the poorly
the treated and untreated groups included younger age, more and undifferentiated groups but not in the well- or moderately
men, fewer blacks and other races, higher-grade tumors, stage differentiated groups.
CIS, married status, urban residence, and higher socioeco-
nomic status in the treated group. Discussion
Overall, 22% of patients received BCG within 6 months of Adjuvant intravesical BCG therapy has long been known to
being diagnosed with NMIBC. In multivariate analysis, the decrease the likelihood of bladder cancer recurrence and pro-
strongest predictors of receipt of BCG were grade: undifferen- gression rates, but it has never been convincingly shown in a
tiated (odds ratio [OR], 4.60; 95% CI, 3.97 to 5.32), poorly large randomized clinical trial to prolong OS or BCSS. Given
differentiated (OR, 4.07; 95% CI, 3.63 to 4.56), and moder- the prolonged natural history of NMIBC and the attendant
ately differentiated (OR, 1.85; 95% CI, 1.66 to 2.05) versus costs of a multiyear randomized clinical trial, the feasibility of a
well differentiated; stage: Tis (OR, 2.67; 95% CI, 2.37 to 3.02) prospective study investigating a survival benefit in this disease
and T1 (OR, 1.91; 95% CI, 1.77 to 2.05) versus Ta; age: 80 to may be limited. Thus, this observational study may represent
84 years (OR, 0.88; 95% CI, 0.79 to 0.98) and ⬎ 85 years (OR, the best we can do in a disease with late death. We found an
0.51; 95% CI, 0.45 to 0.58) versus 65 to 69 years; marital association with improved survival among elderly patients with
status: single or divorced (OR, 0.86; 95% CI, 0.80 to 0.92) high-grade bladder cancer. The overall effect was moderate,
versus married; and urban (OR, 1.16; 95% CI, 1.03 to 1.30) increased substantially with increasing grade, and persisted for
versus rural residence. 10 years of follow-up. Furthermore, we demonstrated that
Table 2 summarizes the results of Cox proportional hazards BCG use among patients with low-grade tumors was not asso-
models for OS and BCSS. A total of 10,598 patients (44% of ciated with survival.
the sample) died during the study period, including 2,303 who In their recent guidelines, the National Comprehensive
were treated with BCG and 8,295 who were not; 1,623 patients Cancer Network and American Urological Association both
(7%) died as a result of bladder cancer, of whom 443 received recommend the use of BCG and/or mitomycin C for adjuvant
BCG and 1,180 did not. After adjusting for demographic, SES, treatment after TUR for decreasing the risk of recurrence and
and clinical characteristics, we found that OS in the entire progression, but not for a survival advantage.18,25 Indications
cohort (hazard ratio [HR], 0.87; 95% CI, 0.83 to 0.92) was include high grade and stage Tis or T1 disease. Although we
improved among patients who received adjuvant intravesical found grade and stage to be the strongest predictors for receiv-
94 JOURNAL OF ONCOLOGY PRACTICE • V O L . 9, I S S U E 2 Copyright © 2012 by American Society of Clinical Oncology
Downloaded from ascopubs.org by 86.120.168.196 on December 2, 2021 from 086.120.168.196
Copyright © 2021 American Society of Clinical Oncology. All rights reserved.
Adjuvant BCG for Non–Muscle-Invasive Bladder Cancer
Table 1. Characteristics and Multivariate* Predictors of Receipt of Adjuvant Intravesical BCG Among Patients Diagnosed With NMIBC
Registered in the SEER-Medicare Database, 1991-2002 (N ⫽ 23,932)
Multivariate Predictors of
BCG (n ⴝ 5,885) No BCG (n ⴝ 18,047) Receipt of BCG
Category No. % No. % OR 95% CI
Age, years†
Mean 75.9 76.9
65-69 Referent
70-74 1.05 0.95 to 1.16
75-79 0.95 0.86 to 1.05
80-84 0.88 0.79 to 0.98
ⱖ 85 0.51 0.45 to 0.58
Sex†
Male 4,477 76 13,177 73 Referent
Female 1,408 24 4,870 27 0.99 0.92 to 1.07
Race/ethnicity†
White 5,434 92 16,904 94 Referent
Black 170 3 517 3 0.94 0.78 to 1.14
Hispanic 45 1 137 1 0.86 0.60 to 1.23
Other 223 4 438 22 1.42 1.20 to 1.68
Grade†
Well differentiated 505 9 4,111 23 Referent
Moderately differentiated 2,018 34 8,606 48 1.85 1.66 to 2.05
Poorly differentiated 1,993 34 3,363 19 4.07 3.63 to 4.56
Undifferentiated 659 11 847 5 4.60 3.97 to 5.32
Unknown 710 12 1,120 6 3.88 3.37 to 4.47
Stage†
Tis 679 12 862 5 Referent
Ta 2,706 46 12,178 67 2.67 2.37 to 3.02
T1 2,257 38 3,750 21 1.91 1.77 to 2.05
Other 243 4 1,257 7 0.76 0.66 to 0.89
No. of comorbidities
0 3,342 57 10,262 57 Referent
1 1,480 25 4,432 25 1.01 0.94 to 1.09
ⱖ2 1,063 18 3,353 19 0.94 0.86 to 1.02
Marital status†
Single/divorced 1,708 29 6,048 34 Referent
Married 3,941 67 11,242 62 0.86 0.80 to 0.92
Unknown 236 4 757 4 0.87 0.75 to 1.03
Residence†
Urban 5,390 92 16,331 90 1.16 1.03 to 1.30
Rural 495 8 1,716 10 Referent
SES quintile
1st 1,129 19 3,340 19 1.08 0.97 to 1.19
2nd 1,103 19 3,521 20 0.99 0.90 to 1.10
3rd 1,133 19 3,687 20 0.92 0.84 to 1.02
4th 1,213 21 3,694 20 0.98 0.89 to 1.08
5th 1,307 22 3,805 21 Referent
Abbreviations: BCG, Bacillus Calmette-Guérin; NMIBC, non–muscle-invasive bladder cancer; OR, odds ratio; SEER, Surveillance, Epidemiology, and End Results;
SES, socioeconomic.
* Adjusted for all other variables in the table and year of diagnosis.
† Statistically significant differences exist between BCG and no BCG groups for these variables (2 significance test).
Copyright © 2012 by American Society of Clinical Oncology M A R C H 2013 • jop.ascopubs.org 95
Downloaded from ascopubs.org by 86.120.168.196 on December 2, 2021 from 086.120.168.196
Copyright © 2021 American Society of Clinical Oncology. All rights reserved.
Spencer et al
Table 2. Estimates of Overall and Disease-Specific Survival Using Cox Proportional Hazards Models Among Patients Diagnosed With
NMIBC in the SEER-Medicare Database, 1991-2002 (N ⫽ 23,932)
Overall Survival Disease-Specific Survival
Category HR 95% CI HR 95% CI
BCG 0.87 0.83 to 0.92 0.90 0.80 to 1.01
Age, years
65-69 Referent Referent
70-74 1.41 1.31 to 1.52 1.16 0.97 to 1.39
75-79 1.89 1.76 to 2.03 1.47 1.23 to 1.76
80-84 2.77 2.57 to 2.98 1.82 1.51 to 2.19
ⱖ 85 4.53 4.21 to 4.89 3.10 2.58 to 3.73
Sex
Male Referent Referent
Female 0.74 0.71 to 0.78 1.07 0.95 to 1.20
Race
White Referent Referent
Black 1.08 0.97 to 1.21 1.57 1.26 to 1.96
Hispanic 1.14 0.92 to 1.43 1.94 1.26 to 2.99
Other 0.75 0.66 to 0.84 0.86 0.64 to 1.15
Grade
Well differentiated Referent Referent
Moderately differentiated 1.11 1.05 to 1.17 1.91 1.55 to 2.36
Poorly differentiated 1.41 1.32 to 1.50 4.21 3.40 to 5.23
Undifferentiated 1.72 1.57 to 1.89 5.91 4.62 to 7.56
Unknown 1.41 1.29 to 1.54 3.67 2.84 to 4.75
Stage
Ta Referent Referent
Tis 1.09 1.00 to 1.22 1.50 1.20 to 1.87
T1 1.25 1.19 to 1.31 2.18 1.94 to 2.46
Other 1.34 1.25 to 1.44 2.73 2.32 to 3.20
Year of diagnosis 0.97 0.96 to 0.98 0.93 0.92 to 0.95
No. of comorbidities
0 Referent Referent
1 1.39 1.33 to 1.46 1.02 0.90 to 1.15
ⱖ2 2.13 2.03 to 2.24 1.28 1.12 to 1.46
Marital status
Married Referent Referent
Single/divorced 1.26 1.20 to 1.31 1.21 1.08 to 1.35
Unknown 0.87 0.78 to 0.98 0.67 0.48 to 0.93
Residence
Urban 1.01 0.94 to 1.08 1.07 0.89 to 1.30
Rural Referent Referent
SES quintile
1st 1.23 1.15 to 1.31 1.20 1.02 to 1.41
2nd 1.17 1.10 to 1.24 1.13 0.96 to 1.33
3rd 1.05 0.99 to 1.12 1.01 0.86 to 1.18
4th 1.09 1.03 to 1.16 1.06 0.90 to 1.24
5th Referent Referent
Abbreviations: BCG, Bacillus Calmette-Guérin; HR, hazard ratio; NMIBC, non–muscle-invasive bladder cancer; SEER, Surveillance, Epidemiology, and End Results;
SES, socioeconomic.
96 JOURNAL OF ONCOLOGY PRACTICE • V O L . 9, I S S U E 2 Copyright © 2012 by American Society of Clinical Oncology
Downloaded from ascopubs.org by 86.120.168.196 on December 2, 2021 from 086.120.168.196
Copyright © 2021 American Society of Clinical Oncology. All rights reserved.
Adjuvant BCG for Non–Muscle-Invasive Bladder Cancer
There are several limitations to our study. Its retrospective
100 BCG observational nature prevents us from confirming a cause-and-
No BCG
effect relationship between BCG and improved survival; the
association with survival may have been related to confounders
Overall Survival (%)
75
rather than to the use of the drug itself. This Medicare claims–
based study was limited to those age ⱖ 65 years. Therefore, we
cannot generalize about the effectiveness of BCG in younger
50
patients. However, a recent study found that younger age was
associated with more favorable tumor characteristics,2 and the
25 risk of death as a result of bladder cancer increased with increas-
ing age.27 Patients with a nonspecific intravesical therapy claim
for Current Procedural Terminology code 51720 were in-
cluded with the BCG group, because more than 97% of adju-
0 10 20 30 40 50 60 70 80 90 100 110 120 vant intravesical therapy administered with a specified drug was
Time (months) for BCG. Only 3% received other drugs, including mitomycin
Month 0 24 48 72 96 120 C, thiotepa, or interferon. Therefore, we acknowledge that
No. at risk 23,932 19,959 12,050 7,159 4,444 2,367 there may have been some misclassification of patients in the
treatment groups. We did not have information regarding the
Figure 1. Adjusted Kaplan-Meier 10-year overall survival. BCG,
dose of intravesical therapy used, nor did we quantify the num-
Bacillus Calmette-Guérin.
ber of instillations administered. However, the most effective
dose of BCG remains unknown, with a recent randomized
ing BCG, only 39% of those with stage Tis or T1 and 27% of clinical trial demonstrating that one-third strength BCG was as
those with grades higher than well differentiated received BCG effective as the standard strength.28 SEER does not report the
within 6 months of diagnosis. Although the majority of Ta number or size of tumors nor concomitant Tis, which are im-
tumors are low grade, we chose not to eliminate this stage from portant risk factors for recurrence of NMIBC.29 We were also
the analysis to avoid biasing our results. In fact, when limiting unable to adjust for the completeness for the TUR of the blad-
the analysis to stages Tis and T1, we found that the protective der cancer, a factor that is important for adjuvant BCG to be
effect of BCG was strengthened, with an HR for OS of 0.79 effective.30 We found that the effect on OS was slightly greater
(95% CI, 0.74 to 0.84). than that on disease-specific survival, suggesting that a small
We also found that elderly patients and those with two or part of the survival benefit may represent unmeasured selection.
more comorbidities were less likely to undergo BCG treatment, Finally, a limitation of SEER is the inability to identify cancer
which would seem to be appropriate. However, we performed a recurrence. For our analysis, we assumed that patients who
survival analysis stratified by age and found that BCG was pro- received BCG more than 6 months after diagnosis (n ⫽ 3,148)
tective among those age ⱖ 80 years. Furthermore, a significant had suffered a recurrence, were treated with BCG as a salvage
interaction between age and receipt of BCG was present. Other therapy, and were therefore included in the comparison un-
studies have documented the appropriateness of treating octo- treated group. Our selection criteria attempted to avoid con-
genarians with muscle-invasive bladder cancer.20 Identifying founding by indication, which would have occurred if those
significant underuse of a guideline-recommended treatment, who were treated with BCG later than 6 months were included
we have documented a lapse in quality of care. Although many in the treated group and if the benefit of treatment was ascribed
of the untreated patients did receive BCG later in their disease to this group. Such cohort selection would have likely led to
courses, such treatment cannot be considered adjuvant therapy. much greater bias. Because 37% of those who received BCG at
This study suggests that early treatment is important. any time did so after 6 months, the potential beneficial effect of
Although this study and others suggest that the use of intra- BCG on survival was greatly attenuated and was a conservative
vesical BCG is increasing,26 the overall rate remains low. Ways estimate.
in which BCG use could be increased might include designat- To our knowledge, this is the first large population-based
ing adjuvant intravesical BCG as a measure of quality among study to suggest a survival advantage among patients with
younger patients newly diagnosed with high-grade NMIBC. NMIBC who receive adjuvant intravesical BCG. Although our
The Centers for Medicare and Medicaid Services Physician data are derived from a retrospective data set, this study may be
Quality Reporting Initiative ties the self-reporting of quality more indicative of the true effect of intravesical BCG because of
indicators to evidence-based practices and may represent an its large sample size, particularly of high-grade cancers, leading
intervention that could improve compliance with adjuvant in- to less dilution of the benefit of BCG, and longer follow-up
travesical therapy for NMIBC. Potential quality indicators period than previous clinical trials and meta-analyses. It also
might include not only the early use of BCG within 6 months of reflects its use and effectiveness in the community rather than in
diagnosis for high-grade tumors but also the absence of BCG highly selected trial patients.
use for low-grade tumors, thereby cost-effectively focusing
treatment on those most likely to benefit. Accepted for publication on April 12, 2012.
Copyright © 2012 by American Society of Clinical Oncology M A R C H 2013 • jop.ascopubs.org 97
Downloaded from ascopubs.org by 86.120.168.196 on December 2, 2021 from 086.120.168.196
Copyright © 2021 American Society of Clinical Oncology. All rights reserved.
Spencer et al
Acknowledgment Financial support: Mitchell C. Benson, Alfred I. Neugut
Supported by American Cancer Society Grants No. RSGHP PBP-
105710 and RSGT-01-024-04-CPHPS and National Cancer Institute Administrative support: Mitchell C. Benson
Grants No. CA95597, CA09529, and CA89155. Presented in part at Collection and assembly of data: Donna Buono
the 102nd Annual Meeting of the American Urological Association,
Anaheim, CA, May 19-24, 2007. We acknowledge the efforts of the Data analysis and interpretation: All authors
Applied Research Branch, Division of Cancer Prevention and Popula- Manuscript writing: All authors
tion Science, National Cancer Institute; Offices of Information Services
and Strategic Planning, Health Care Financing Administration; Informa- Final approval of manuscript: All authors
tion Management Services; and Surveillance, Epidemiology, and End
Results (SEER) Program tumor registries in the creation of the SEER- Corresponding author: Benjamin A. Spencer, Herbert Irving Compre-
Medicare database. hensive Cancer Center, 161 Fort Washington Avenue, New York, NY
10032; e-mail: bas10@columbia.edu.
Authors’ Disclosures of Potential Conflicts of Interest
The author(s) indicated no potential conflicts of interest.
Author Contributions
Conception and design: Benjamin A. Spencer, Dawn L. Hersh-
man, Harry W. Herr, Mitchell C. Benson, Supriya Gupta-Mohile, DOI: 10.1200/JOP.2011.000480; published online ahead of print
Alfred I. Neugut at jop.ascopubs.org on October 30, 2012.
References
1. American Cancer Society: What are the key statistics about bladder cancer? http:// A meta-analysis of the published results of randomized clinical trials. J Urol 168:
www.cancer.org/cancer/bladdercancer/detailedguide/bladder-cancer-key-statistics 1964-1970, 2002
2. Cho KS, Hwang TK, Kim BW, et al: Differences in tumor characteristics and 17. Lamm DL: Efficacy and safety of Bacille Calmette-Guérin immunotherapy in
prognosis in newly diagnosed Ta, T1 urothelial carcinoma of bladder according to superficial bladder cancer. Clin Infect Dis 31:S86-S90, 2000 (suppl 3)
patient age. Urology 73:828-832, 2009 18. National Comprehensive Cancer Network: NCCN clinical practice guidelines
3. Amling CL: Diagnosis and management of superficial bladder cancer. Curr in oncology: Bladder cancer including upper tract tumors and urothelial carci-
Probl Cancer 25:219-278, 2001 noma of the prostate, Volume 2, 2010. http://www.nccn.org/professionals/
physician_gls/f_guidelines.asp
4. Cookson MS, Herr HW, Zhang ZF, et al: The treated natural history of high risk
superficial bladder cancer: 15-year outcome. J Urol 158:62-67, 1997 19. Potosky AL, Riley GF, Lubitz JD, et al: Potential for cancer related health
services research using a linked Medicare-tumor registry database. Med Care
5. Herr HW: High-risk superficial bladder cancer: Transurethral resection alone in 31:732-748, 1993
selected patients with T1 tumor. Semin Urol Oncol 15:142-146, 1997
20. Chamie K, Hu B, Devere White RW, et al: Cystectomy in the elderly: Does the
6. Herr HW: Natural history of superficial bladder tumors: 10- to 20-year fol- survival benefit in younger patients translate to the octogenarians? BJU Int 102:
low-up of treated patients. World J Urol 15:84-88, 1997 284-290, 2008
7. Dalbagni G: The management of superficial bladder cancer. Nat Clin Pract 21. Klabunde CN, Potosky AL, Legler JM, et al: Development of a comorbidity
Urol 4:254-260, 2007 index using physician claims data. J Clin Epidemiol 53:1258-1267, 2000
8. Krege S, Giani G, Meyer R, et al: A randomized multicenter trial of adjuvant 22. Charlson ME, Pompei P, Ales KL, et al: A new method of classifying prog-
therapy in superficial bladder cancer: Transurethral resection only versus trans- nostic comorbidity in longitudinal studies: Development and validation. J Chronic
urethral resection plus mitomycin C versus transurethral resection plus bacillus Dis 40:373-383, 1987
Calmette-Guerin—Participating clinics. J Urol 156:962-966, 1996 23. Lamont EB, Lauderdale DS, Schilsky RL, et al: Construct validity of medicare
9. Herr HW: Intravesical BCG: Current results, natural history and implications for chemotherapy claims: The case of 5FU. Med Care 40:201-211, 2002
urothelial cancer prevention. J Cell Biochem Suppl 16I:112-119, 1992 24. Warren JL, Harlan LC, Fahey A, et al: Utility of the SEER-Medicare data to
10. Nadler RB, Catalona WJ, Hudson MA, et al: Durability of the tumor-free identify chemotherapy use. Med Care 40:IV-55-IV-61, 2002 (suppl 8)
response for intravesical bacillus Calmette-Guerin therapy. J Urol 152:367-373, 25. American Urological Association: Guideline for the management of nonmuscle in-
1994 vasive bladder cancer: Stage Ta, T1, Tis—2007 update. http://www.auanet.org/content/
11. Hudson MA, Herr HW: Carcinoma in situ of the bladder. J Urol 153:564-572, clinical-practice-guidelines/clinical-guidelines.cfm?sub⫽bc
1995 26. Strope SA, Ye Z, Hollingsworth JM, et al: Patterns of care for early stage
bladder cancer. Cancer 116: 2604-2611, 2010
12. Herr HW, Schwalb DM, Zhang ZF, et al: Intravesical bacillus Calmette-Guerin
therapy prevents tumor progression and death from superficial bladder cancer: 27. Huang GJ, Hamilton AS, Lo M, et al: Predictors of intravesical therapy for
Ten-year follow-up of a prospective randomized trial. J Clin Oncol 13:1404-1408, nonmuscle invasive bladder cancer: Results from the surveillance, epidemiology
1995 and end results program 2003 patterns of care project. J Urol 180:520-524,
2008; discussion 524
13. Han RF, Pan JG: Can intravesical bacillus Calmette-Guerin reduce recur-
rence in patients with superficial bladder cancer? A meta-analysis of randomized 28. Martı́nez-Piñeiro JA, Martı́nez-Piñeiro L, Solsona E, et al: Has a 3-fold de-
trials. Urology 67:1216-1223, 2006 creased dose of bacillus Calmette-Guerin the same efficacy against recurrences
and progression of T1G3 and Tis bladder tumors than the standard dose? Results
14. Shelley MD, Court JB, Kynaston H, et al: Intravesical Bacillus Calmette- of a prospective randomized trial. J Urol 174:1242-1247, 2005
Guerin in Ta and T1 bladder cancer. Cochrane Database Syst Rev 4:CD001986,
29. Orsola A, Cecchini L, Raventos CX, et al: Risk factors for positive findings in
2000
patients with high-grade T1 bladder cancer treated with transurethral resection of
15. Shelley MD, Kynaston H, Court J, et al: A systematic review of intravesical bladder tumour (TUR) and bacille Calmette-Guerin therapy and the decision for a
bacillus Calmette-Guerin plus transurethral resection vs transurethral resection repeat TUR. BJU Int 105:202-207, 2010
alone in Ta and T1 bladder cancer. BJU Int 88:209-216, 2001 30. Herr HW: Restaging transurethral resection of high risk superficial bladder
16. Sylvester RJ, van der Meijden AP, Lamm DL: Intravesical bacillus Calmette- cancer improves the initial response to bacillus Calmette-Guerin therapy. J Urol
Guerin reduces the risk of progression in patients with superficial bladder cancer: 174:2134-2137, 2005
98 JOURNAL OF ONCOLOGY PRACTICE • V O L . 9, I S S U E 2 Copyright © 2012 by American Society of Clinical Oncology
Downloaded from ascopubs.org by 86.120.168.196 on December 2, 2021 from 086.120.168.196
Copyright © 2021 American Society of Clinical Oncology. All rights reserved.
Appendix
A 100
B 100
BCG BCG
No BCG No BCG
Overall Survival (%)
Overall Survival (%)
75 75
50 50
25 25
0 10 20 30 40 50 60 70 80 90 100 110 120 0 10 20 30 40 50 60 70 80 90 100 110 120
Time (months) Time (months)
C 100
D 100
BCG BCG
No BCG No BCG
Overall Survival (%)
Overall Survival (%)
75 75
50 50
25 25
0 10 20 30 40 50 60 70 80 90 100 110 120 0 10 20 30 40 50 60 70 80 90 100 110 120
Time (months) Time (months)
Figure A1. Adjusted Kaplan-Meier 10-year overall survival by grade: (A) well differentiated; (B) moderately differentiated; (C) poorly differentiated; (D)
undifferentiated. BCG, Bacillus Calmette-Guérin.
Copyright © 2012 by American Society of Clinical Oncology M A R C H 2013 • jop.ascopubs.org
Downloaded from ascopubs.org by 86.120.168.196 on December 2, 2021 from 086.120.168.196
Copyright © 2021 American Society of Clinical Oncology. All rights reserved.
You might also like
- This Study Resource Was Shared ViaDocument4 pagesThis Study Resource Was Shared ViaKyuSheen100% (1)
- Combinatorial Test Design (CTD) : IBM Haifa Research LaboratoryDocument7 pagesCombinatorial Test Design (CTD) : IBM Haifa Research LaboratoryChirac OanaNo ratings yet
- Compassionate Sciences - RedactedDocument184 pagesCompassionate Sciences - RedactedNew Jersey marijuana documentsNo ratings yet
- Conceptual Framework SampleDocument2 pagesConceptual Framework SampleReYa Buenaventura100% (1)
- The Short Textbook of Pediatrics PDFDocument38 pagesThe Short Textbook of Pediatrics PDFGolla manoharNo ratings yet
- Sfakianos 2015Document7 pagesSfakianos 2015nimaelhajjiNo ratings yet
- Synchronous Bilateral Breast CancersDocument4 pagesSynchronous Bilateral Breast CancersEnrico GaharaNo ratings yet
- MedicineDocument5 pagesMedicinepriyanka hermawanNo ratings yet
- Jasirwan 2019Document11 pagesJasirwan 2019MuliaNo ratings yet
- Prognostic Value of C Reactive Protein - AlbuminDocument8 pagesPrognostic Value of C Reactive Protein - AlbuminfernandallmagalhaesNo ratings yet
- Synchronous Bilateral Breast Cancers: Abst TDocument4 pagesSynchronous Bilateral Breast Cancers: Abst TLastrii HillaryNo ratings yet
- 8424365Document8 pages8424365Melody CyyNo ratings yet
- Theoncologist 15440Document8 pagesTheoncologist 15440nimaelhajjiNo ratings yet
- COGNITION A Prospective Precision Oncology TrialDocument12 pagesCOGNITION A Prospective Precision Oncology Trialveaceslav coscodanNo ratings yet
- Achenbach, 2015Document10 pagesAchenbach, 2015Leonardo Arévalo MoraNo ratings yet
- Impact of Comorbidity On Colorectal Cancer Screening Cost-Effectiveness Study in Diabetic PopulationsDocument9 pagesImpact of Comorbidity On Colorectal Cancer Screening Cost-Effectiveness Study in Diabetic PopulationsAna MîndrilăNo ratings yet
- 00006Document6 pages00006carlangaslaraNo ratings yet
- 1475 2891 12 118Document8 pages1475 2891 12 118SunardiasihNo ratings yet
- Ca Colon 2Document19 pagesCa Colon 2Tob JurNo ratings yet
- Ijmr 1588 22 R3Document6 pagesIjmr 1588 22 R3Aditi GoyalNo ratings yet
- Local Recurrence After Breast-Conserving Therapy I - 240415 - 080523Document12 pagesLocal Recurrence After Breast-Conserving Therapy I - 240415 - 080523Khan ZareenNo ratings yet
- Interval Colorectal Cancers in Inflammatory Bowel Disease: The Grim Statistics and True StoriesDocument12 pagesInterval Colorectal Cancers in Inflammatory Bowel Disease: The Grim Statistics and True StoriespancholarpancholarNo ratings yet
- Xiaoli HuDocument12 pagesXiaoli HuYohanes AdhityaNo ratings yet
- BR Vs CHOPDocument8 pagesBR Vs CHOPabdullahNo ratings yet
- 1019 5298 1 PBDocument11 pages1019 5298 1 PBm907062008No ratings yet
- Beal 2020Document17 pagesBeal 2020Nikos SerifisNo ratings yet
- Articulo Cirgua Musinoso Nodulos NegtivDocument10 pagesArticulo Cirgua Musinoso Nodulos NegtivJorge VintimillaNo ratings yet
- Comprehensive Precision Medicine Study Protocol On The Heterogeneity of Taiwanese Breast Cancer PatientsDocument14 pagesComprehensive Precision Medicine Study Protocol On The Heterogeneity of Taiwanese Breast Cancer Patients郭竹瑩No ratings yet
- Colorectal Cancer Lynch Nyhan SyndromeDocument9 pagesColorectal Cancer Lynch Nyhan SyndromeSteffanio SebastianNo ratings yet
- 19#prognostic HCC 2021Document7 pages19#prognostic HCC 2021hitashiNo ratings yet
- s13027 020 00299 3Document10 pagess13027 020 00299 3Remona RemoraNo ratings yet
- 1540 1413 Article p1529 PDFDocument26 pages1540 1413 Article p1529 PDFEvelynππ θσυNo ratings yet
- Allen2021 Article ChemotherapyVersusChemotherapyDocument8 pagesAllen2021 Article ChemotherapyVersusChemotherapyXavier QuinteroNo ratings yet
- Arends 2016Document7 pagesArends 2016DavorIvanićNo ratings yet
- Risk Factors For Pelvic and Distant Recurrence in Locally AdvancedDocument7 pagesRisk Factors For Pelvic and Distant Recurrence in Locally AdvancedfernandallmagalhaesNo ratings yet
- Colorectal CancerDocument9 pagesColorectal CancerPatricia ClarineNo ratings yet
- 10.1245/s10434 018 6369 XDocument9 pages10.1245/s10434 018 6369 Xsayumiholic89No ratings yet
- Jcav 13 P 0051Document11 pagesJcav 13 P 0051hasna muhadzibNo ratings yet
- 10 1093@icvts@ivz140Document8 pages10 1093@icvts@ivz140PEDRO JESuS GUERRA CANCHARINo ratings yet
- Comparison of Radical Cystectomy With Conservative Treatment in Geriatric ( 80) Patients With Muscle-Invasive Bladder CancerDocument9 pagesComparison of Radical Cystectomy With Conservative Treatment in Geriatric ( 80) Patients With Muscle-Invasive Bladder CancerjustforuroNo ratings yet
- 1 s2.0 S2531043719302156 MainDocument9 pages1 s2.0 S2531043719302156 Mainpulmonologi UnsyiahNo ratings yet
- Mallappa Et Al-2013-Colorectal DiseaseDocument6 pagesMallappa Et Al-2013-Colorectal DiseaseDumitru RadulescuNo ratings yet
- 10 1097@mou 0b013e328356ac20Document6 pages10 1097@mou 0b013e328356ac20nimaelhajjiNo ratings yet
- Research Article: Clinical Characteristics in Patients With Triple Negative Breast CancerDocument6 pagesResearch Article: Clinical Characteristics in Patients With Triple Negative Breast Cancerlapkas donjuanNo ratings yet
- EeDocument8 pagesEeEstiPramestiningtyasNo ratings yet
- 1 s2.0 S001236922200575XDocument9 pages1 s2.0 S001236922200575XYulia Niswatul FauziyahNo ratings yet
- Extracellular Nucleic Acids and Cancer: Michael - Fleischhacker@uk-Halle - de Bernd - Schmidt@uk-Halle - deDocument55 pagesExtracellular Nucleic Acids and Cancer: Michael - Fleischhacker@uk-Halle - de Bernd - Schmidt@uk-Halle - deAirin LeonieNo ratings yet
- 3994 - Adjusting Cyclophosphamide Dose in Obese PatientsDocument4 pages3994 - Adjusting Cyclophosphamide Dose in Obese PatientsErnika SariNo ratings yet
- Prophylactic MastectomyDocument5 pagesProphylactic MastectomyMuhammad Darussalam DarwisNo ratings yet
- NGS de Panel para CCR - JCO 2015 - Costo-EfectividadDocument12 pagesNGS de Panel para CCR - JCO 2015 - Costo-EfectividadSebas Barrionuevo VediaNo ratings yet
- Lotan Et Al. Molecular Marker For Rec and Cancer Specific Survival Post Radical CystectomyDocument7 pagesLotan Et Al. Molecular Marker For Rec and Cancer Specific Survival Post Radical CystectomyyuenkeithNo ratings yet
- Patient Survival Report 1Document5 pagesPatient Survival Report 1Rabeya Bibi 193-15-13510No ratings yet
- MainDocument8 pagesMainIoana CucuNo ratings yet
- Vandenbosch 2011Document8 pagesVandenbosch 2011nimaelhajjiNo ratings yet
- EJGO2022054 Cervical CaDocument8 pagesEJGO2022054 Cervical CaRahmayantiYuliaNo ratings yet
- JournalReading ONKO JeffriSyaputraDocument17 pagesJournalReading ONKO JeffriSyaputraYarman War officialNo ratings yet
- Research Article: Prevalence of Cachexia in Cancer PatientsDocument9 pagesResearch Article: Prevalence of Cachexia in Cancer Patientsadri20121989No ratings yet
- Advanced Non-Small Cell Lung Cancer in Patients Aged 45 Years or Younger: Outcomes and Prognostic FactorsDocument8 pagesAdvanced Non-Small Cell Lung Cancer in Patients Aged 45 Years or Younger: Outcomes and Prognostic FactorsAnnisa DiendaNo ratings yet
- How I Treat Newly Diagnosed Chronic Phase CMLDocument9 pagesHow I Treat Newly Diagnosed Chronic Phase CMLDenisse SarabiaNo ratings yet
- Howard 2012Document5 pagesHoward 20121alexandra12No ratings yet
- Effect of More Vs Less Frequent Follow-Up Testing On Overall and Colorectal Cancer-Specific Mortality in Patients With Stage II or III Colorectal CancerDocument9 pagesEffect of More Vs Less Frequent Follow-Up Testing On Overall and Colorectal Cancer-Specific Mortality in Patients With Stage II or III Colorectal CancerMr. LNo ratings yet
- Local Control in Metastatic Neuroblastoma in Children Over 1 Year of AgeDocument8 pagesLocal Control in Metastatic Neuroblastoma in Children Over 1 Year of AgePutri ManurungNo ratings yet
- GastroDocument9 pagesGastroAnonymous plYGwXNo ratings yet
- Changes in Ki 67 in Residual Tumor and Outcome of Primary I - 2022 - Clinical BRDocument9 pagesChanges in Ki 67 in Residual Tumor and Outcome of Primary I - 2022 - Clinical BRAd AdrianaNo ratings yet
- Settipane 1981Document5 pagesSettipane 1981Chirac OanaNo ratings yet
- Martinez 2015Document1 pageMartinez 2015Chirac OanaNo ratings yet
- Temple 1981Document6 pagesTemple 1981Chirac OanaNo ratings yet
- AnatolJCardiol 7 2 27 30Document4 pagesAnatolJCardiol 7 2 27 30Chirac OanaNo ratings yet
- Decribing Places Buildings Successful Writing - Intermediate SBDocument6 pagesDecribing Places Buildings Successful Writing - Intermediate SBChirac OanaNo ratings yet
- Hofbauer 2015Document5 pagesHofbauer 2015Chirac OanaNo ratings yet
- WHOPIR BB NCIPD 11-13march2020Document15 pagesWHOPIR BB NCIPD 11-13march2020Chirac OanaNo ratings yet
- Reg Form - Farmacovigilenta - 21-23sep2020Document1 pageReg Form - Farmacovigilenta - 21-23sep2020Chirac OanaNo ratings yet
- Conflict of Interest Disclosures: Patient Case # 1Document28 pagesConflict of Interest Disclosures: Patient Case # 1Chirac OanaNo ratings yet
- Meropenem VenusDocument7 pagesMeropenem VenusChirac OanaNo ratings yet
- Information Technology, 19 (1), 94-115. Retrieved From: Resources - Perpusnas.go - Id:2057/docview/1951416783?accountid 25704Document2 pagesInformation Technology, 19 (1), 94-115. Retrieved From: Resources - Perpusnas.go - Id:2057/docview/1951416783?accountid 25704AnggiNo ratings yet
- Indonesian Guideline H Pylori Dyspepsia 2022Document19 pagesIndonesian Guideline H Pylori Dyspepsia 2022Daniel TariganNo ratings yet
- Forensic Medical Examination of Alive Persons: CCCCCCC CDocument7 pagesForensic Medical Examination of Alive Persons: CCCCCCC CDrGurjyot NandaNo ratings yet
- SeminarDocument34 pagesSeminarMuhammad Faiz Satria WibowoNo ratings yet
- IHOP - 09.13.39 - Humpty Dumpty Fall Assessment ScaleDocument1 pageIHOP - 09.13.39 - Humpty Dumpty Fall Assessment ScaleRomiko NersNo ratings yet
- Ebook Campbell Walsh Urology 12Th Edition Review 3E Mar 2 2020 - 0323639690 - Elsevier PDF Full Chapter PDFDocument68 pagesEbook Campbell Walsh Urology 12Th Edition Review 3E Mar 2 2020 - 0323639690 - Elsevier PDF Full Chapter PDFfrank.daniels751100% (29)
- Employee Benefits CGHSDocument3 pagesEmployee Benefits CGHSaruvindhuNo ratings yet
- Hospital ManagementDocument3 pagesHospital ManagementFebriciaKristinaNo ratings yet
- PQCNC NHPC LS3 Noel 2020 Workload Indicators 20200310.Document23 pagesPQCNC NHPC LS3 Noel 2020 Workload Indicators 20200310.kcochranNo ratings yet
- Adult Neurological Observation Chart Education PackageDocument101 pagesAdult Neurological Observation Chart Education PackageRajiNo ratings yet
- Magdy El-Masry Prof. of Cardiology Tanta UniversityDocument55 pagesMagdy El-Masry Prof. of Cardiology Tanta UniversityPrabJot SinGhNo ratings yet
- David Perlmutter Full Length InterviewDocument28 pagesDavid Perlmutter Full Length InterviewKalNo ratings yet
- MeaslesDocument11 pagesMeaslesMarivic DianoNo ratings yet
- History of Anaesthesia Oropharyngeal and Nasopharyngeal Airways: I (1880-1995)Document7 pagesHistory of Anaesthesia Oropharyngeal and Nasopharyngeal Airways: I (1880-1995)Lucille IlaganNo ratings yet
- ATS-ERS Statement On Respiratory Muscle TestingDocument107 pagesATS-ERS Statement On Respiratory Muscle TestingLuizaNo ratings yet
- PGDHMDocument36 pagesPGDHMAndy JadNo ratings yet
- Internship ReportDocument35 pagesInternship ReportSamu LuwagunNo ratings yet
- Role and ResponsibilitiesDocument17 pagesRole and Responsibilitiesprabha karanNo ratings yet
- College of Medical Technology Principle of Medical Laboratory Science 1 (MLS 037)Document14 pagesCollege of Medical Technology Principle of Medical Laboratory Science 1 (MLS 037)Cindy Mae A. PogoyNo ratings yet
- Bupa Global List OF Contracted Providers in Egypt - Nov 2020Document11 pagesBupa Global List OF Contracted Providers in Egypt - Nov 2020MahmoudAbdElGhaniNo ratings yet
- Health Information SystemDocument11 pagesHealth Information SystemVineeta Jose100% (1)
- Med Surg Chap QuestionsDocument9 pagesMed Surg Chap Questionslani0% (1)
- Hh2sgonzupzxf4gu1w1wym1fDocument1 pageHh2sgonzupzxf4gu1w1wym1fHarsh AryaNo ratings yet
- Chapter 30 Assessment and Management of Patients With Vascular Disorders and Problems of Peripheral CirculationDocument23 pagesChapter 30 Assessment and Management of Patients With Vascular Disorders and Problems of Peripheral CirculationAbel C. Idusma Jr.No ratings yet
- Community Mental Health ProgramDocument9 pagesCommunity Mental Health Programpreeti sharma100% (1)
- Disorders of The Blood and Neoplastic DisordersDocument72 pagesDisorders of The Blood and Neoplastic DisordersavisenicNo ratings yet