Professional Documents
Culture Documents
Intermittent Hemodialysis For Managing Metabolic Acidosis During Resuscitation of Septic Shock: A Descriptive Study
Intermittent Hemodialysis For Managing Metabolic Acidosis During Resuscitation of Septic Shock: A Descriptive Study
Uploaded by
ilham masdarCopyright:
Available Formats
You might also like
- Case Chrons For ReadingsDocument4 pagesCase Chrons For Readingsskyemacdonald23No ratings yet
- ERS Handbook of Paediatric Respiratory Medicine - E. Eber, F MidullaDocument750 pagesERS Handbook of Paediatric Respiratory Medicine - E. Eber, F MidullaOlga Cîrstea100% (1)
- BSM M104 Curriculum OutlineDocument3 pagesBSM M104 Curriculum OutlineDamaris Pandora Songcal0% (1)
- Qi Project PaperDocument8 pagesQi Project Paperapi-380333919No ratings yet
- Consultation Handbook - Bill BevingtonDocument37 pagesConsultation Handbook - Bill BevingtonAnny Aun50% (2)
- Cardiology An Illustrated Textbook (Jaypee) PDFDocument2,136 pagesCardiology An Illustrated Textbook (Jaypee) PDFSarital Boron100% (3)
- 14 - Mazandarani2012Document7 pages14 - Mazandarani2012TandeanTommyNovenantoNo ratings yet
- Prittie-2006-Journal of Veterinary Emergency and Critical CareDocument11 pagesPrittie-2006-Journal of Veterinary Emergency and Critical Carejose fdoNo ratings yet
- Aneurysm Brain and Hyperbaric Chamber AIT - Art - 37989-10Document7 pagesAneurysm Brain and Hyperbaric Chamber AIT - Art - 37989-10cooleraid884No ratings yet
- Non Analgesic BenefitDocument11 pagesNon Analgesic Benefitajay kumarNo ratings yet
- Impact of Remote Ischaemic Preconditioning On Cerebral Oxygenation During Total Knee ArthroplastyDocument8 pagesImpact of Remote Ischaemic Preconditioning On Cerebral Oxygenation During Total Knee ArthroplastySanti ParambangNo ratings yet
- SINPHONIDocument11 pagesSINPHONIvistamaniacNo ratings yet
- SLED Vs CRRT PDFDocument9 pagesSLED Vs CRRT PDFquilino2012No ratings yet
- Early Versus Delayed Administration of Norepinephrine in Patients With Septic ShockDocument8 pagesEarly Versus Delayed Administration of Norepinephrine in Patients With Septic ShockNanda SusiloNo ratings yet
- dainty2011Document7 pagesdainty20110172488336No ratings yet
- 4 Phases of IV Fluid Therapy FinalDocument29 pages4 Phases of IV Fluid Therapy FinalLuqmanul Hakim Junaidden100% (1)
- Medi 101 E31671Document6 pagesMedi 101 E31671302895No ratings yet
- Sumber Tabel Kriteria JMHWDocument10 pagesSumber Tabel Kriteria JMHWDwika AudiyanandaNo ratings yet
- Ali - 2019 - J. - Phys. - Conf. - Ser. - 1246 - 012002Document6 pagesAli - 2019 - J. - Phys. - Conf. - Ser. - 1246 - 012002priyaNo ratings yet
- Echocardiography in Hemodynamic MonitoringDocument5 pagesEchocardiography in Hemodynamic MonitoringDr.Biswajit jenaNo ratings yet
- 2a.330-Removal of Humoral Mediators and The Effect On The Survival of Septic Patients by Hemoperfusion With Neutral Microporous Resin ColumnDocument7 pages2a.330-Removal of Humoral Mediators and The Effect On The Survival of Septic Patients by Hemoperfusion With Neutral Microporous Resin Columngmejiar5237No ratings yet
- Year in Review 2012: Critical Care - CardiologyDocument6 pagesYear in Review 2012: Critical Care - CardiologyUdrea NicolaeNo ratings yet
- Pi Is 0007091223002052Document8 pagesPi Is 0007091223002052aieyha hamkaNo ratings yet
- Park2019 Article RecoveryFromAcuteKidneyInjuryADocument11 pagesPark2019 Article RecoveryFromAcuteKidneyInjuryALeandro NogueiraNo ratings yet
- Niknam 2019Document8 pagesNiknam 2019Valdir ReisNo ratings yet
- Medi 96 E6490Document4 pagesMedi 96 E6490TheEdgeNo ratings yet
- Special Article: Department of Medicine, Faculty of Medicine, Siriraj Hospital, Mahidol University, Bangkok, ThailandDocument7 pagesSpecial Article: Department of Medicine, Faculty of Medicine, Siriraj Hospital, Mahidol University, Bangkok, ThailanddefriNo ratings yet
- Maximum Norepinephrine Dosage Within 24 Hours As An Indicator of Refractory Septic Shock: A Retrospective StudyDocument5 pagesMaximum Norepinephrine Dosage Within 24 Hours As An Indicator of Refractory Septic Shock: A Retrospective StudyLuis Miguel VillanuevaNo ratings yet
- s13019 020 1084 7Document10 pagess13019 020 1084 7Shalva BasharuliNo ratings yet
- Lee 2015 Yonsei Med JDocument8 pagesLee 2015 Yonsei Med JCamilaNo ratings yet
- Goal-Directed Fluid Restriction During Brain Surgery: A Prospective Randomized Controlled TrialDocument7 pagesGoal-Directed Fluid Restriction During Brain Surgery: A Prospective Randomized Controlled TrialkenjiNo ratings yet
- Clinical Significance of Urinary L-FABP in The Emergency DepartmentDocument7 pagesClinical Significance of Urinary L-FABP in The Emergency DepartmentmentariNo ratings yet
- 2052 0492 2 6 PDFDocument4 pages2052 0492 2 6 PDFLina LatanzaNo ratings yet
- Extracorporeal Cardiopulmonary Resuscitation With Therapeutic Hypothermia For Prolonged Refractory In-Hospital Cardiac ArrestDocument10 pagesExtracorporeal Cardiopulmonary Resuscitation With Therapeutic Hypothermia For Prolonged Refractory In-Hospital Cardiac Arrestika nur annisaNo ratings yet
- Kumar Et Al 2004 Extended Daily Dialysis Vs Continuous Hemodialysis For Icu Patients With Acute Renal Failure A TwoDocument9 pagesKumar Et Al 2004 Extended Daily Dialysis Vs Continuous Hemodialysis For Icu Patients With Acute Renal Failure A TwoAmanda SantosNo ratings yet
- Comparative Study Between Cardioprotective Effects of Intermitternt Antegrade Blood Cardioplegia With Terminal Warm Blood Reperfusion (Hot Shot) vs Intermittent Antegrade Blood Cardioplegia in PediatricDocument18 pagesComparative Study Between Cardioprotective Effects of Intermitternt Antegrade Blood Cardioplegia With Terminal Warm Blood Reperfusion (Hot Shot) vs Intermittent Antegrade Blood Cardioplegia in PediatricalbadroeNo ratings yet
- Epinephrine During Resuscitation of Traumatic Cardiac Arrest and Increased Mortality: A Post Hoc Analysis of Prospective Observational StudyDocument9 pagesEpinephrine During Resuscitation of Traumatic Cardiac Arrest and Increased Mortality: A Post Hoc Analysis of Prospective Observational StudymaithilicharanNo ratings yet
- 4 Preliminary Guideline - and Pathophysiology - Base Protocols For Neurological CareDocument9 pages4 Preliminary Guideline - and Pathophysiology - Base Protocols For Neurological CareehuaniNo ratings yet
- Sinkovi 2018Document8 pagesSinkovi 2018EviNo ratings yet
- O LiguriaDocument8 pagesO LiguriaMartin SchickNo ratings yet
- Impact of Intravenous Lidocaine On Myocardial InjuDocument7 pagesImpact of Intravenous Lidocaine On Myocardial InjuRENAULTNo ratings yet
- Oral Rehydration Therapy For Preoperative Fluid and Electrolyte Man-AgementDocument9 pagesOral Rehydration Therapy For Preoperative Fluid and Electrolyte Man-AgementSasmira JamalNo ratings yet
- Anesthetic Management During Cardiopulmonary Bypass A SystematicDocument21 pagesAnesthetic Management During Cardiopulmonary Bypass A SystematicFabio MeloNo ratings yet
- Pi Is 2590059522000863Document4 pagesPi Is 2590059522000863nina2911No ratings yet
- Background - : Original ResearchDocument10 pagesBackground - : Original ResearchDAHLIANo ratings yet
- Use of Hyperoncotic Human Albumin Solution in Severe Traumatic Brain Injury Revisited-A Narrative Review and Meta-AnalysisDocument10 pagesUse of Hyperoncotic Human Albumin Solution in Severe Traumatic Brain Injury Revisited-A Narrative Review and Meta-Analysisjose luis iribarrenNo ratings yet
- PGDT Protocol Summary ReferenceDocument32 pagesPGDT Protocol Summary Referenceghg sddNo ratings yet
- Intraoperative Fluid Management in Open Gastro-Intestinal Surgery: Goal-Directed Versus RestrictiveDocument7 pagesIntraoperative Fluid Management in Open Gastro-Intestinal Surgery: Goal-Directed Versus Restrictiveade_liaNo ratings yet
- Preoperative Evaluation Before NoncardiacDocument16 pagesPreoperative Evaluation Before NoncardiacHercilioNo ratings yet
- What's New in Cardiopulmonary BypassDocument31 pagesWhat's New in Cardiopulmonary Bypass凌晓敏No ratings yet
- A High Mean Arterial PressureDocument8 pagesA High Mean Arterial Pressureadek07No ratings yet
- Jiang 2022Document9 pagesJiang 2022Olivia LimNo ratings yet
- En V29n2a08Document5 pagesEn V29n2a08Iago DjavanNo ratings yet
- Preoperative Evaluation Before Noncardiac Surgery.Document16 pagesPreoperative Evaluation Before Noncardiac Surgery.Paloma AcostaNo ratings yet
- Intraoperative Cardiac ArrestDocument7 pagesIntraoperative Cardiac ArrestdefitranandaNo ratings yet
- Robba Et Al-2024-Intensive Care MedicineDocument13 pagesRobba Et Al-2024-Intensive Care MedicineLeiniker NavarroNo ratings yet
- AnnCardAnaesth9144-7552051 020552Document5 pagesAnnCardAnaesth9144-7552051 020552Imanuel Far-FarNo ratings yet
- Clinical and Experimental Emergency MedicineDocument56 pagesClinical and Experimental Emergency MedicineAlfonso Ga MaNo ratings yet
- PIRRDocument8 pagesPIRRcursointensivoenamNo ratings yet
- Brain Injury Resuscitation 2009Document8 pagesBrain Injury Resuscitation 2009Dandy Azmi AzwirNo ratings yet
- Bivalirudin Anticoagulant1Document6 pagesBivalirudin Anticoagulant1walid hassanNo ratings yet
- Isovolume Hypertonic Solutes Sodium ChloDocument5 pagesIsovolume Hypertonic Solutes Sodium Chlodai leNo ratings yet
- Capillary Refill Time Variation Induced by Passive Leg Raising Predicts Capillary Refill Time Response To Volume ExpansionDocument11 pagesCapillary Refill Time Variation Induced by Passive Leg Raising Predicts Capillary Refill Time Response To Volume ExpansionLarissa BianchiniNo ratings yet
- Hyperbaric Oxygenation Therapy: Molecular Mechanisms and Clinical ApplicationsFrom EverandHyperbaric Oxygenation Therapy: Molecular Mechanisms and Clinical ApplicationsNariyoshi ShinomiyaNo ratings yet
- Top Trials in Gastroenterology & HepatologyFrom EverandTop Trials in Gastroenterology & HepatologyRating: 4.5 out of 5 stars4.5/5 (7)
- Confirmed COVID-19 Confirmed COVID-19Document5 pagesConfirmed COVID-19 Confirmed COVID-19ilham masdarNo ratings yet
- Batu Ren, Batu Ureter Dan Onko NewDocument29 pagesBatu Ren, Batu Ureter Dan Onko Newilham masdarNo ratings yet
- Maret PelayananDocument31 pagesMaret Pelayananilham masdarNo ratings yet
- TrialDocument3 pagesTrialilham masdarNo ratings yet
- Absen Masker N95, Surgical Mask Maret 2022Document2 pagesAbsen Masker N95, Surgical Mask Maret 2022ilham masdarNo ratings yet
- Quantification (Popq) Terhadap KualitasDocument9 pagesQuantification (Popq) Terhadap Kualitasilham masdarNo ratings yet
- NCP Kenezo, Female 17Document2 pagesNCP Kenezo, Female 17labanesstephanyNo ratings yet
- Herbal - Medicines - in - The - Treatment of Mental IllnessesDocument12 pagesHerbal - Medicines - in - The - Treatment of Mental IllnessesFarash farshiNo ratings yet
- Ophthalmology STR eDocument2 pagesOphthalmology STR ekevinzhu11111No ratings yet
- Susannah Brewton - ResumeDocument2 pagesSusannah Brewton - Resumeapi-318876563No ratings yet
- Mental Health in ConnecticutDocument60 pagesMental Health in ConnecticutHelen BennettNo ratings yet
- PNA 2012 National Convention LectureDocument60 pagesPNA 2012 National Convention LectureHarby Ongbay AbellanosaNo ratings yet
- PDF Midwifery Final Test 1Document7 pagesPDF Midwifery Final Test 1DianeNo ratings yet
- 0eriodontology: 5pdate - AYDocument6 pages0eriodontology: 5pdate - AYFatima AliNo ratings yet
- AAOHNS MembershipApplicationDocument4 pagesAAOHNS MembershipApplicationAnonymous AuJncFVWvNo ratings yet
- Sample Complaints LettersDocument4 pagesSample Complaints LettersZdenka PetroskyNo ratings yet
- MEHT130423 - Information For Screening For Retinopathy of Prematurity 1.0Document4 pagesMEHT130423 - Information For Screening For Retinopathy of Prematurity 1.0Rohit BharadwajNo ratings yet
- ICM Essential Competencies For Basic Midwifery Practice 2010, Revised 2013 PDFDocument19 pagesICM Essential Competencies For Basic Midwifery Practice 2010, Revised 2013 PDFKuurniiaa PraweestiiNo ratings yet
- Tamil Nadu ReportDocument116 pagesTamil Nadu ReportVenkatasubramaniyanNo ratings yet
- PGH 101 v2018Document10 pagesPGH 101 v2018Ian Phillip PaclibareNo ratings yet
- SABA Reliance Questionnaire (SRQ) FulltextDocument34 pagesSABA Reliance Questionnaire (SRQ) FulltextPhụng KimNo ratings yet
- Final Announcement Liver UpdateDocument13 pagesFinal Announcement Liver Updatenerissa arvianaNo ratings yet
- 2023 Updated-Nursing Skills ChecklistDocument7 pages2023 Updated-Nursing Skills Checklistapi-652071746No ratings yet
- Application Form For Punjab Residency Program (Level - Iv) TrainingDocument6 pagesApplication Form For Punjab Residency Program (Level - Iv) TrainingFatima Habib JajjaNo ratings yet
- First AidDocument10 pagesFirst AidArslan Shaukat100% (1)
- Trade and Health:: Towards Building A National StrategyDocument149 pagesTrade and Health:: Towards Building A National Strategymanjusri lalNo ratings yet
- 17th HXMDP - AIIMS New DelhiDocument12 pages17th HXMDP - AIIMS New Delhiars_del0% (1)
- John Hoberman-Testosterone Dreams, Rejuvenation, Aphrodisia, Doping PDFDocument390 pagesJohn Hoberman-Testosterone Dreams, Rejuvenation, Aphrodisia, Doping PDFjpcmanso100% (3)
- Chapter 01 - Health Care Delivery and Evidence-Based Nursing PracticeDocument9 pagesChapter 01 - Health Care Delivery and Evidence-Based Nursing PracticePrince K. TaileyNo ratings yet
- Endorsement FormDocument12 pagesEndorsement Formferraterkimdaniel25No ratings yet
Intermittent Hemodialysis For Managing Metabolic Acidosis During Resuscitation of Septic Shock: A Descriptive Study
Intermittent Hemodialysis For Managing Metabolic Acidosis During Resuscitation of Septic Shock: A Descriptive Study
Uploaded by
ilham masdarOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Intermittent Hemodialysis For Managing Metabolic Acidosis During Resuscitation of Septic Shock: A Descriptive Study
Intermittent Hemodialysis For Managing Metabolic Acidosis During Resuscitation of Septic Shock: A Descriptive Study
Uploaded by
ilham masdarCopyright:
Available Formats
Critical Care
Observational Study Explorations
Intermittent Hemodialysis for Managing
Metabolic Acidosis During Resuscitation of
Septic Shock: A Descriptive Study
Kazutaka Nogi, MD1,2; Atsushi Shiraishi, MD, PhD3; Ryohei Yamamoto, MD1; Mikio Sasano, MD1,4;
Takashi Matsumoto, MD1,4; Toshiyuki Karumai, MD1; Yoshiro Hayashi, MD, PhD1
Objectives: Septic shock is often complicated by severe metabolic 6–13; p < 0.001), decreased minute ventilatory volume (–2.0 L/min;
acidosis, for which renal replacement therapy may be considered. 95% CI, –3.3 to 0.8; p = 0.002), decreased norepinephrine require-
However, little is known about the use of intermittent hemodialysis to ment (–0.07 µg/kg/min; 95% CI, –0.12 to –0.02; p = 0.009), increased
manage this condition. The aim of this study was to compare physio- bicarbonate level (+7.2 mmol/L; 95% CI, 6.1–8.3; p < 0.001), and
logic and biochemical variables and vasopressor requirements before increased pH (+0.17; 95% CI, 0.13–0.21; p < 0.001) were observed
and after intermittent hemodialysis among patients who received in comparison to those before intermittent hemodialysis.
intermittent hemodialysis to manage metabolic acidosis during resus- Conclusions: In conclusion, intermittent hemodialysis appeared to be
citation of septic shock. feasible and to stabilize hemodynamic and respiratory conditions in
Design: This retrospective, cross-sectional study was conducted patients with septic shock complicated by metabolic acidosis during
between April 2014 and September 2015. resuscitation.
Settings: The ICU of a non-university-affiliated teaching hospital. Key Words: acute kidney injury; hemodialysis; intensive care;
Patients: Patients who were admitted to the ICU with septic shock metabolic acidosis; renal replacement therapy; septic shock
and underwent intermittent hemodialysis to manage metabolic acido-
sis within 48 hours after the diagnosis of septic shock.
S
Measurements and Main Results: The main outcomes were mean arte-
rial pressure, minute ventilator volume, norepinephrine requirement,
eptic shock is often complicated by severe metabolic acidosis.
bicarbonate and pH before and after intermittent hemodialysis. Of
Therapeutic intervention to correct metabolic acidosis may
1,190 patients screened, 34 were included, and 33 accomplished a
be considered when hemodynamic and respiratory deterio-
planned session of intermittent hemodialysis. After intermittent hemo-
ration rapidly progress (1, 2). In general, continuous renal replace-
dialysis, an increased mean arterial pressure (+9.0 mm Hg; 95% CI,
ment therapy (CRRT) is the preferred mode of renal replacement
therapy (RRT) in hemodynamically unstable critically ill patients
with regard to hemodynamic stability (1, 3, 4). However, intermit-
1
Department of Intensive Care Medicine, Kameda Medical Center, Kamogawa,
Chiba, Japan. tent hemodialysis (IHD) may have potential advantages for those
2
Department of Cardiovascular Medicine, Nara Medical University, Nara, requiring RRT to manage clinically significant metabolic acido-
Japan. sis during resuscitation of septic shock in that IHD more rapidly
3
Emergency and Trauma Center, Kameda Medical Center, Kamogawa, Chiba, removes low molecular weight solutes than CRRT (4). Currently,
Japan. little is known about the use of IHD to manage this condition (5).
4
Department of Intensive Care Medicine, Nakagami Hospital, Okinawa, Japan. IHD rather than CRRT may be employed as a mode of RRT even
The authors have disclosed that they do not have any potential conflicts of for hemodynamically unstable patients for various reasons such as
interest.
cost and limited access to CRRT. For example, in our ICU, 24/7 CRRT
For information regarding this article, E-mail: yoshi.icu@gmail.com
service was not available. In addition, CRRT is performed with very
Copyright © 2019 The Authors. Published by Wolters Kluwer Health, Inc.
on behalf of the Society of Critical Care Medicine. This is an open-access low intensity (12–16 mL/kg/hr) in Japan because of a daily maximum
article distributed under the terms of the Creative Commons Attribution-Non dose limitation of CRRT solution products covered by public health
Commercial-No Derivatives License 4.0 (CCBY-NC-ND), where it is permis- insurance (6). Although CRRT with an intensity of greater than or
sible to download and share the work provided it is properly cited. The work
cannot be changed in any way or used commercially without permission from equal to 35 mL/kg/hr has been demonstrated to have no benefit as
the journal. compared with that with an intensity of 20–25 mL/kg/hr (7–9), one
Crit Care Expl 2019; 1:e0065 may be concerned about providing CRRT with a very low intensity in
DOI: 10.1097/CCE.0000000000000065 such conditions as rapid solute removal is thought to be ideal.
Critical Care Explorations www.ccejournal.org 1
Nogi et al
The aim of this study was to compare respiratory physiology inserted into either the internal jugular or femoral vein. A DBB-
and acid-base biochemistry and vasopressor requirements before 100NX dialysis machine (NIKKISO, Tokyo, Japan) and either a
and after IHD among patients who had metabolic acidosis during KF12 or KF15 synthetic hydrophilic membrane (Asahi Kasei
resuscitation of septic shock. Medical, Tokyo, Japan) was used. Blood and dialysate flow were
200 mL/min and 500 mL/min, respectively. The duration of one
IHD session was 4 hours but extended up to 6 hours if deemed
MATERIALS AND METHODS
necessary. Unfractionated heparin or nafamostat mesilate (Torii
Study Design and Setting Pharmaceutical, Tokyo, Japan) was administered for anticoagula-
This retrospective, cross-sectional study was conducted at an ICU in tion during IHD. For those with bleeding or high risk of bleeding,
Kameda Medical Center between April 2014 and September 2015. IHD was performed without anticoagulation.
Kameda Medical Center is a non-university-affiliated teaching hos-
pital with 917 beds. The ICU was a medical-surgical ICU with a Study Variables
closed-ICU policy and approximately 1,000 annual admissions. Physiologic variables included systolic blood pressure (SBP), mean
arterial pressure (MAP), heart rate (HR), and measured minute
Ethics ventilatory volume (MV). Biochemical variables included pH,
The institutional review boards of the hospital approved the study biocarbonate (Hco3–), Paco2, base excess, and lactate and were
protocol (approval number: 15-071). Requirement to obtain obtained from arterial blood gas analysis. These data were collected
informed consent was waived by them.
TABLE 1.Baseline Characteristics of the Study
Patients Patients (n = 34)
Septic shock patients who received IHD in the ICU for the man-
Characteristic Value
agement of metabolic acidosis within 48 hours after the diagnosis
of septic shock were included. Septic shock was defined based on Age, yr 75 (66–81)
the 2001 International Sepsis Definitions (10). Decision to per- Female, n (%) 11 (32)
form IHD for the correction of metabolic acidosis was made by
each treating intensivist. Those who did not complete a session of Sequential Organ Failure Assessment 13 (10–15)
IHD were excluded from the analysis of physiologic and biochem- Acute Physiology and Chronic Health 28 (23–33)
ical parameters but included in the analysis of clinical outcomes. Evaluation II
Simplified Acute Physiology Score II 69 (54–80)
Intermittent Hemodialysis
IHD was performed via a double-lumen hemodialysis catheter Serum creatinine, mg/dL 2.16 (1.34–2.83)
(12F, Gentle Cath; Medtronic, Dublin, Ireland) percutaneously Serum potassium, mM 4.6 (4.0–5.1)
Pre IHD total fluid volume, mL 4,700 (3,200–6,600)
Time to IHD after ICU admission, hr 3 (1.4–17.8)
Mechanical ventilation, n (%) 27 (79)
Use of norepinephrine, n (%) 34 (100)
Use of steroids, n (%) 25 (74)
Use of vasopressin, n (%) 13 (38)
Admission route, n (%)
Emergency department 18 (53)
Ward 10 (29)
Operating theater 6 (18)
Primary source of infection, n (%)
Respiratory 10 (29)
Urinary tract infection 7 (21)
Intra-abdominal sepsis 4 (12)
Bloodstream 5 (15)
Others 8 (23)
IHD = intermittent hemodialysis.
Quantitative variables are displayed as medians and interquartile ranges and
Figure 1. Flow chart of the study cohort. IHD = intermittent hemodialysis. categorical variables are displayed as counts and percentages.
2 www.ccejournal.org 2019 • Volume 1 • e0065
Observational Study
from the electronic medical records. Clinical outcome data, such as (Table 2). All patients completed the 90-day follow-up after the
ICU mortality, in-hospital mortality, 28-day and 90-day mortality, initiation of IHD. ICU mortality, in-hospital mortality, 28-day
ICU-free days and alive, RRT-free days and alive, ventilator-free and 90-day mortality were 15 (44%), 17 (50%), 12 (35%), and 16
days and alive at the 28th day were also retrieved from the elec- (47%), respectively. ICU-free days and alive, RRT-free days and
tronic medical records. alive, and ventilator-free days and alive on the 28th day were 8
(5–12), 10 (0–26), 15 (0–25), respectively (Table 3).
Statistical Analysis
Data were analyzed descriptively. Continuous or categorical vari-
DISCUSSION
ables were described as medians and interquartile ranges (25–
In this study, it was observed that IHD in patients who had meta-
75th) or as counts and percentages, respectively.
bolic acidosis during resuscitation of septic shock was associated
It was not assumed that the continuous study variables were nor-
with improvement not only in biochemical parameters but also
mally distributed; bootstrapping methods were used to estimate the
in respiratory and circulatory physiology with decreased norepi-
means and CIs for differences in these variables before and after IHD.
nephrine requirement as compared with pre-IHD status.
All statistical analyses were performed using R 3.4.1 (R Core Team
Our findings raise a question regarding the consensus that IHD
2017; R Foundation for Statistical Computing, Vienna, Austria.).
should be avoided for hemodynamically unstable patients including
those who suffer from septic shock complicated by clinically signifi-
RESULTS cant metabolic acidosis. When providing RRT in hemodynamically
A total of 1,190 patients admitted to the ICU were screened for unstable patients, the current common understanding is in favor of
study eligibility. A total of 34 patients fulfilled the study inclusion CRRT rather than IHD for fear of further deterioration of hemody-
criteria (Fig. 1). The baseline characteristics of the study popula- namics (12–17). A randomized controlled trial comparing IHD and
tion are shown in Table 1. Two patients (5.9%) had 1,000 mL of CRRT in patients with septic shock complicated by acute kidney
fluid removal. Only one patient (2.9%), who was an 81-year-old injury (AKI) showed an increase in SBP 2 hours after the initiation
female with septic shock of unknown origin, failed to complete a of CRRT, whereas a decrease in SBP at 0.5 hours and 2 hours after
planned session of IHD due to a decision to withdraw, which was the initiation of IHD (5). However, the study population and the
made during IHD, followed by her immediate death. aim of RRT in the study were different from those of our study, in
Regarding the physiologic parameters, an increase in MAP which IHD was performed in order to manage metabolic acidosis in
and a decrease in MV were observed after IHD. In contrast, there patients with septic shock while being resuscitated.
was no significant difference in HR before and after IHD. For bio- Serum lactate level after IHD in the study population decreased
chemical parameters, increases in Hco3– and pH were observed slightly, although it remained at a high level. In a previous study, lac-
after IHD (Table 2 and Fig. 2A–D). In addition, the noradrena- tate clearance was inversely associated with increased risk of death
line requirement and inotropic score (11) decreased after IHD over the first 6 hours after ICU admission (18). However, data on
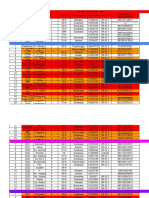
TABLE 2. Comparison of Variables Before and After Intermittent Hemodialysis (n = 33)
Before IHD, After IHD, Bootstrap Difference,
Variables Mean (sd) Mean (sd) Mean (95% CI) Bootstrap p
Norepinephrine (µg/kg/min) 0.28 (0.20) 0.21 (0.18) –0.07 (–0.12 to –0.02) 0.009
Inotropic score 30 (23) 23 (20) –7 (–12 to –1) 0.012
Physiologic
Systolic blood pressure (mm Hg) 101 (13) 115 (21) 15 (9–21) < 0.001
Mean arterial pressure (mm Hg) 69 (8) 79 (11) 9 (6–13) < 0.001
Heart rate (/min) 99 (21) 100 (23) 1 (–3 to 5) 0.532
Minute volume (L/min) 14.1 (4.3) 12.0 (3.7) –2.0 (–3.3 to –0.8) 0.002
Biochemical
pH 7.22 (0.12) 7.40 (0.09) 0.17 (0.13–0.21) < 0.001
Bicarbonate (mmol/L) 12.6 (3.4) 19.7 (2.7) 7.2 (6.1–8.3) < 0.001
Paco2 (mm Hg) 31.5 (10.0) 33.6 (9.5) 2.1 (–0.2 to 4.5) 0.079
Base excess (mmol/L) –13.7 (4.0) –4.4 (2.8) 9.3 (7.9–10.8) < 0.001
Lactate (mmol/L) 6.9 (4.7) 6.2 (3.7) –0.9 (–1.7 to –0.3) 0.010
IHD = intermittent hemodialysis.
Differences were estimated by bootstrapping and described as mean and 95% CIs.
Critical Care Explorations www.ccejournal.org 3
Nogi et al
Figure 2. Changes in mean arterial pressure (MAP), heart rate (HR), measured minute ventilatory volume (MV), and norepinephrine (NE) over time after the start
of intermittent hemodialysis (IHD).
lactate clearance by RRT are limited and conflicting (19). Some to IHD. Current AKI guidelines recommend delivering CRRT at
researchers suggest that increased lactate clearance may be the an effluent volume of 20–25 mL/kg/hr in patients with AKI (4).
improved endogenous acid-base and metabolic status achieved dur- In Japan, however, CRRT is generally delivered at a lower inten-
ing RRT rather than the removal of large amounts of lactate by RRT sity (12–16 mL/kg/hr, up to 800 mL/hr) than the recommended
(20). We assumed that improvement of circulation was associated intensity because of limited daily maximum use of CRRT solu-
with a slightly decreased lactate level and IHD may contributed to tions covered by public health insurance (6). In addition, our ICU
hemodynamic stabilization. Significant acidosis is associated with had limited access to CRRT during the study period. Although
catecholamine-refractory hypotension through a mechanism that these rare environments forced us to use IHD to manage clinically
involves a decreased number of β adrenergic receptors and decreased significant metabolic acidosis during septic shock resuscitation, in
myocardial contractility (21, 22). In contrast, improvement of meta- our observation, IHD is a feasible and even beneficial therapeu-
bolic acidosis is associated with an enhanced effect of catecholamines tic option to manage this condition. As the typical dose of IHD
and an alleviated effort for respiratory compensation. (500 mL/min = 30,000 mL/hr) is much higher than that of CRRT,
To artificially compensate metabolic acidosis in hemodynami- comparison to CRRT is of particular interest. Other potential ben-
cally unstable septic shock patients, CRRT is generally preferred efits of IHD as compared with CRRT include earlier mobilization
4 www.ccejournal.org 2019 • Volume 1 • e0065
Observational Study
TABLE 3. Clinical Outcomes of Study Patients REFERENCES
1. Rhodes A, Evans LE, Alhazzani W, et al: Surviving sepsis campaign:
(n = 34) International guidelines for management of sepsis and septic shock: 2016.
Outcomes Value Intensive Care Med 2017; 43:304–377
2. Jentzer JC, Vallabhajosyula S, Khanna AK, et al: Management of refrac-
ICU-day, median (IQR) 8 (5–12) tory vasodilatory shock. Chest 2018; 154:416–426
3. Uchino S, Kellum JA, Bellomo R, et al; Beginning and Ending Supportive
28-d ICU-free survival day, median (IQR) 8 (5–12)
Therapy for the Kidney (BEST Kidney) Investigators: Acute renal failure
28-d renal replacement therapy-free 10 (0–26) in critically ill patients: A multinational, multicenter study. JAMA 2005;
survival day, median (IQR) 294:813–818
4. Khwaja A: KDIGO clinical practice guidelines for acute kidney injury.
28-d ventilator-free survival day, median (IQR) 15 (0–25) Nephron Clin Pract 2012; 120:c179–c184
ICU death, n (%) 15 (44) 5. John S, Griesbach D, Baumgärtel M, et al: Effects of continuous haemo-
filtration vs intermittent haemodialysis on systemic haemodynamics and
In-hospital death, n (%) 17 (50) splanchnic regional perfusion in septic shock patients: A prospective,
randomized clinical trial. Nephrol Dial Transplant 2001; 16:320–327
28-d death, n (%) 12 (35)
6. Uchino S, Toki N, Takeda K, et al; Japanese Society for Physicians and
90-d death, n (%) 16 (47) Trainees in Intensive Care (JSEPTIC) Clinical Trial Group: Validity of
low-intensity continuous renal replacement therapy*. Crit Care Med
IQR = interquartile range (25–75th). 2013; 41:2584–2591
Quantitative variables are displayed as medians and IQRs and categorical
variables are displayed as counts and percentages. 7. Kellum JA, Angus DC, Johnson JP, et al: Continuous versus intermittent renal
replacement therapy: A meta-analysis. Intensive Care Med 2002; 28:29–37
8. Rabindranath K, Adams J, Macleod AM, et al: Intermittent versus contin-
of patients, less staff-time requirements to provide RRT, simpler uous renal replacement therapy for acute renal failure in adults. Cochrane
antibiotic dosing, shorter and less exposure to anticoagulants, and Database Syst Rev 2007; 3:CD003773
lower costs associated with RRT. 9. Bagshaw SM, Berthiaume LR, Delaney A, et al: Continuous versus inter-
Little is known about the safety and efficacy of IHD use in mittent renal replacement therapy for critically ill patients with acute kid-
hemodynamically unstable patients with septic shock. This study ney injury: A meta-analysis. Crit Care Med 2008; 36:610–617
described changes in physiologic and biochemical parameters and 10. Levy MM, Fink MP, Marshall JC, et al; International Sepsis Definitions
Conference: 2001 SCCM/ESICM/ACCP/ATS/SIS international sepsis
decreased norepinephrine requirement before and after IHD, and definitions conference. Intensive Care Med 2003; 29:530–538
major clinical outcomes such as mortality and event-free days, in 11. Cruz DN, Antonelli M, Fumagalli R, et al: Early use of polymyxin B
patients who received IHD for the management of severe meta- hemoperfusion in abdominal septic shock: The EUPHAS randomized
bolic acidosis while resuscitation of septic shock. controlled trial. JAMA 2009; 301:2445–2452
Our study has several limitations. First, our study was a single- 12. Pannu N, Klarenbach S, Wiebe N, et al; Alberta Kidney Disease Network:
Renal replacement therapy in patients with acute renal failure: A system-
center retrospective study that described within group, before IHD atic review. JAMA 2008; 299:793–805
and after IHD changes in regard to physiologic and biochemical 13. Friedrich JO, Wald R, Bagshaw SM, et al: Hemofiltration compared to
parameters without a control group. Second, decisions to initiate hemodialysis for acute kidney injury: Systematic review and meta-analy-
IHD for metabolic acidosis correction were made by attending sis. Crit Care 2012; 16:R146
intensivists without any formal objective criteria. Third, our study 14. Schneider AG, Bellomo R, Bagshaw SM, et al: Choice of renal replacement
therapy modality and dialysis dependence after acute kidney injury: A sys-
population was limited to very old Japanese patients (median age, tematic review and meta-analysis. Intensive Care Med 2013; 39:987–997
75 yr) who lived in a rural area. This may limit the generalizabil- 15. Augustine JJ, Sandy D, Seifert TH, et al: A randomized controlled trial
ity of the study interpretation. Fourth, one patient, who withdrew comparing intermittent with continuous dialysis in patients with ARF.
during IHD followed by immediate death, was excluded for the Am J Kidney Dis 2004; 44:1000–1007
analysis of physiologic and biochemical variables. This potentially 16. Schefold JC, von Haehling S, Pschowski R, et al: The effect of continuous
versus intermittent renal replacement therapy on the outcome of criti-
caused selective bias toward favorable effects of our practice. Fifth, cally ill patients with acute renal failure (CONVINT): A prospective ran-
IHD efficiently removes most of the commonly used antibiotics domized controlled trial. Crit Care 2014; 18:R11
such as β-lactams, potentially resulting in therapeutic underdose, 17. Truche AS, Darmon M, Bailly S, et al; OUTCOMEREA Study Group:
although special attention to this issue was always paid in our ICU. Continuous renal replacement therapy versus intermittent hemodialy-
sis in intensive care patients: Impact on mortality and renal recovery.
Intensive Care Med 2016; 42:1408–1417
CONCLUSIONS 18. Nichol A, Bailey M, Egi M, et al: Dynamic lactate indices as predictors of
Favorable changes in physiologic and biochemical variables and outcome in critically ill patients. Crit Care 2011; 15:R242
norepinephrine dependency were observed after IHD in patients 19. De Corte W, Vuylsteke S, De Waele JJ, et al: Severe lactic acidosis in criti-
with septic shock complicated by metabolic acidosis during resus- cally ill patients with acute kidney injury treated with renal replacement
therapy. J Crit Care 2014; 29:650–655
citation. Further studies are needed to show feasibility and benefit
20. Briglia AE: The current state of nonuremic applications for extracorpo-
of IHD for this purpose. real blood purification. Semin Dial 2005; 18:380–390
21. Marsh JD, Margolis TI, Kim D: Mechanism of diminished contractile
response to catecholamines during acidosis. Am J Physiol 1988; 254:H20–H27
ACKNOWLEDGMENTS 22. Orchard CH, Hamilton DL, Astles P, et al: The effect of acidosis on the
We thank Kosuke Sekine for his support with the data collection relationship between Ca2+ and force in isolated ferret cardiac muscle. J
process and useful discussions. Physiol 1991; 436:559–578
Critical Care Explorations www.ccejournal.org 5
You might also like
- Case Chrons For ReadingsDocument4 pagesCase Chrons For Readingsskyemacdonald23No ratings yet
- ERS Handbook of Paediatric Respiratory Medicine - E. Eber, F MidullaDocument750 pagesERS Handbook of Paediatric Respiratory Medicine - E. Eber, F MidullaOlga Cîrstea100% (1)
- BSM M104 Curriculum OutlineDocument3 pagesBSM M104 Curriculum OutlineDamaris Pandora Songcal0% (1)
- Qi Project PaperDocument8 pagesQi Project Paperapi-380333919No ratings yet
- Consultation Handbook - Bill BevingtonDocument37 pagesConsultation Handbook - Bill BevingtonAnny Aun50% (2)
- Cardiology An Illustrated Textbook (Jaypee) PDFDocument2,136 pagesCardiology An Illustrated Textbook (Jaypee) PDFSarital Boron100% (3)
- 14 - Mazandarani2012Document7 pages14 - Mazandarani2012TandeanTommyNovenantoNo ratings yet
- Prittie-2006-Journal of Veterinary Emergency and Critical CareDocument11 pagesPrittie-2006-Journal of Veterinary Emergency and Critical Carejose fdoNo ratings yet
- Aneurysm Brain and Hyperbaric Chamber AIT - Art - 37989-10Document7 pagesAneurysm Brain and Hyperbaric Chamber AIT - Art - 37989-10cooleraid884No ratings yet
- Non Analgesic BenefitDocument11 pagesNon Analgesic Benefitajay kumarNo ratings yet
- Impact of Remote Ischaemic Preconditioning On Cerebral Oxygenation During Total Knee ArthroplastyDocument8 pagesImpact of Remote Ischaemic Preconditioning On Cerebral Oxygenation During Total Knee ArthroplastySanti ParambangNo ratings yet
- SINPHONIDocument11 pagesSINPHONIvistamaniacNo ratings yet
- SLED Vs CRRT PDFDocument9 pagesSLED Vs CRRT PDFquilino2012No ratings yet
- Early Versus Delayed Administration of Norepinephrine in Patients With Septic ShockDocument8 pagesEarly Versus Delayed Administration of Norepinephrine in Patients With Septic ShockNanda SusiloNo ratings yet
- dainty2011Document7 pagesdainty20110172488336No ratings yet
- 4 Phases of IV Fluid Therapy FinalDocument29 pages4 Phases of IV Fluid Therapy FinalLuqmanul Hakim Junaidden100% (1)
- Medi 101 E31671Document6 pagesMedi 101 E31671302895No ratings yet
- Sumber Tabel Kriteria JMHWDocument10 pagesSumber Tabel Kriteria JMHWDwika AudiyanandaNo ratings yet
- Ali - 2019 - J. - Phys. - Conf. - Ser. - 1246 - 012002Document6 pagesAli - 2019 - J. - Phys. - Conf. - Ser. - 1246 - 012002priyaNo ratings yet
- Echocardiography in Hemodynamic MonitoringDocument5 pagesEchocardiography in Hemodynamic MonitoringDr.Biswajit jenaNo ratings yet
- 2a.330-Removal of Humoral Mediators and The Effect On The Survival of Septic Patients by Hemoperfusion With Neutral Microporous Resin ColumnDocument7 pages2a.330-Removal of Humoral Mediators and The Effect On The Survival of Septic Patients by Hemoperfusion With Neutral Microporous Resin Columngmejiar5237No ratings yet
- Year in Review 2012: Critical Care - CardiologyDocument6 pagesYear in Review 2012: Critical Care - CardiologyUdrea NicolaeNo ratings yet
- Pi Is 0007091223002052Document8 pagesPi Is 0007091223002052aieyha hamkaNo ratings yet
- Park2019 Article RecoveryFromAcuteKidneyInjuryADocument11 pagesPark2019 Article RecoveryFromAcuteKidneyInjuryALeandro NogueiraNo ratings yet
- Niknam 2019Document8 pagesNiknam 2019Valdir ReisNo ratings yet
- Medi 96 E6490Document4 pagesMedi 96 E6490TheEdgeNo ratings yet
- Special Article: Department of Medicine, Faculty of Medicine, Siriraj Hospital, Mahidol University, Bangkok, ThailandDocument7 pagesSpecial Article: Department of Medicine, Faculty of Medicine, Siriraj Hospital, Mahidol University, Bangkok, ThailanddefriNo ratings yet
- Maximum Norepinephrine Dosage Within 24 Hours As An Indicator of Refractory Septic Shock: A Retrospective StudyDocument5 pagesMaximum Norepinephrine Dosage Within 24 Hours As An Indicator of Refractory Septic Shock: A Retrospective StudyLuis Miguel VillanuevaNo ratings yet
- s13019 020 1084 7Document10 pagess13019 020 1084 7Shalva BasharuliNo ratings yet
- Lee 2015 Yonsei Med JDocument8 pagesLee 2015 Yonsei Med JCamilaNo ratings yet
- Goal-Directed Fluid Restriction During Brain Surgery: A Prospective Randomized Controlled TrialDocument7 pagesGoal-Directed Fluid Restriction During Brain Surgery: A Prospective Randomized Controlled TrialkenjiNo ratings yet
- Clinical Significance of Urinary L-FABP in The Emergency DepartmentDocument7 pagesClinical Significance of Urinary L-FABP in The Emergency DepartmentmentariNo ratings yet
- 2052 0492 2 6 PDFDocument4 pages2052 0492 2 6 PDFLina LatanzaNo ratings yet
- Extracorporeal Cardiopulmonary Resuscitation With Therapeutic Hypothermia For Prolonged Refractory In-Hospital Cardiac ArrestDocument10 pagesExtracorporeal Cardiopulmonary Resuscitation With Therapeutic Hypothermia For Prolonged Refractory In-Hospital Cardiac Arrestika nur annisaNo ratings yet
- Kumar Et Al 2004 Extended Daily Dialysis Vs Continuous Hemodialysis For Icu Patients With Acute Renal Failure A TwoDocument9 pagesKumar Et Al 2004 Extended Daily Dialysis Vs Continuous Hemodialysis For Icu Patients With Acute Renal Failure A TwoAmanda SantosNo ratings yet
- Comparative Study Between Cardioprotective Effects of Intermitternt Antegrade Blood Cardioplegia With Terminal Warm Blood Reperfusion (Hot Shot) vs Intermittent Antegrade Blood Cardioplegia in PediatricDocument18 pagesComparative Study Between Cardioprotective Effects of Intermitternt Antegrade Blood Cardioplegia With Terminal Warm Blood Reperfusion (Hot Shot) vs Intermittent Antegrade Blood Cardioplegia in PediatricalbadroeNo ratings yet
- Epinephrine During Resuscitation of Traumatic Cardiac Arrest and Increased Mortality: A Post Hoc Analysis of Prospective Observational StudyDocument9 pagesEpinephrine During Resuscitation of Traumatic Cardiac Arrest and Increased Mortality: A Post Hoc Analysis of Prospective Observational StudymaithilicharanNo ratings yet
- 4 Preliminary Guideline - and Pathophysiology - Base Protocols For Neurological CareDocument9 pages4 Preliminary Guideline - and Pathophysiology - Base Protocols For Neurological CareehuaniNo ratings yet
- Sinkovi 2018Document8 pagesSinkovi 2018EviNo ratings yet
- O LiguriaDocument8 pagesO LiguriaMartin SchickNo ratings yet
- Impact of Intravenous Lidocaine On Myocardial InjuDocument7 pagesImpact of Intravenous Lidocaine On Myocardial InjuRENAULTNo ratings yet
- Oral Rehydration Therapy For Preoperative Fluid and Electrolyte Man-AgementDocument9 pagesOral Rehydration Therapy For Preoperative Fluid and Electrolyte Man-AgementSasmira JamalNo ratings yet
- Anesthetic Management During Cardiopulmonary Bypass A SystematicDocument21 pagesAnesthetic Management During Cardiopulmonary Bypass A SystematicFabio MeloNo ratings yet
- Pi Is 2590059522000863Document4 pagesPi Is 2590059522000863nina2911No ratings yet
- Background - : Original ResearchDocument10 pagesBackground - : Original ResearchDAHLIANo ratings yet
- Use of Hyperoncotic Human Albumin Solution in Severe Traumatic Brain Injury Revisited-A Narrative Review and Meta-AnalysisDocument10 pagesUse of Hyperoncotic Human Albumin Solution in Severe Traumatic Brain Injury Revisited-A Narrative Review and Meta-Analysisjose luis iribarrenNo ratings yet
- PGDT Protocol Summary ReferenceDocument32 pagesPGDT Protocol Summary Referenceghg sddNo ratings yet
- Intraoperative Fluid Management in Open Gastro-Intestinal Surgery: Goal-Directed Versus RestrictiveDocument7 pagesIntraoperative Fluid Management in Open Gastro-Intestinal Surgery: Goal-Directed Versus Restrictiveade_liaNo ratings yet
- Preoperative Evaluation Before NoncardiacDocument16 pagesPreoperative Evaluation Before NoncardiacHercilioNo ratings yet
- What's New in Cardiopulmonary BypassDocument31 pagesWhat's New in Cardiopulmonary Bypass凌晓敏No ratings yet
- A High Mean Arterial PressureDocument8 pagesA High Mean Arterial Pressureadek07No ratings yet
- Jiang 2022Document9 pagesJiang 2022Olivia LimNo ratings yet
- En V29n2a08Document5 pagesEn V29n2a08Iago DjavanNo ratings yet
- Preoperative Evaluation Before Noncardiac Surgery.Document16 pagesPreoperative Evaluation Before Noncardiac Surgery.Paloma AcostaNo ratings yet
- Intraoperative Cardiac ArrestDocument7 pagesIntraoperative Cardiac ArrestdefitranandaNo ratings yet
- Robba Et Al-2024-Intensive Care MedicineDocument13 pagesRobba Et Al-2024-Intensive Care MedicineLeiniker NavarroNo ratings yet
- AnnCardAnaesth9144-7552051 020552Document5 pagesAnnCardAnaesth9144-7552051 020552Imanuel Far-FarNo ratings yet
- Clinical and Experimental Emergency MedicineDocument56 pagesClinical and Experimental Emergency MedicineAlfonso Ga MaNo ratings yet
- PIRRDocument8 pagesPIRRcursointensivoenamNo ratings yet
- Brain Injury Resuscitation 2009Document8 pagesBrain Injury Resuscitation 2009Dandy Azmi AzwirNo ratings yet
- Bivalirudin Anticoagulant1Document6 pagesBivalirudin Anticoagulant1walid hassanNo ratings yet
- Isovolume Hypertonic Solutes Sodium ChloDocument5 pagesIsovolume Hypertonic Solutes Sodium Chlodai leNo ratings yet
- Capillary Refill Time Variation Induced by Passive Leg Raising Predicts Capillary Refill Time Response To Volume ExpansionDocument11 pagesCapillary Refill Time Variation Induced by Passive Leg Raising Predicts Capillary Refill Time Response To Volume ExpansionLarissa BianchiniNo ratings yet
- Hyperbaric Oxygenation Therapy: Molecular Mechanisms and Clinical ApplicationsFrom EverandHyperbaric Oxygenation Therapy: Molecular Mechanisms and Clinical ApplicationsNariyoshi ShinomiyaNo ratings yet
- Top Trials in Gastroenterology & HepatologyFrom EverandTop Trials in Gastroenterology & HepatologyRating: 4.5 out of 5 stars4.5/5 (7)
- Confirmed COVID-19 Confirmed COVID-19Document5 pagesConfirmed COVID-19 Confirmed COVID-19ilham masdarNo ratings yet
- Batu Ren, Batu Ureter Dan Onko NewDocument29 pagesBatu Ren, Batu Ureter Dan Onko Newilham masdarNo ratings yet
- Maret PelayananDocument31 pagesMaret Pelayananilham masdarNo ratings yet
- TrialDocument3 pagesTrialilham masdarNo ratings yet
- Absen Masker N95, Surgical Mask Maret 2022Document2 pagesAbsen Masker N95, Surgical Mask Maret 2022ilham masdarNo ratings yet
- Quantification (Popq) Terhadap KualitasDocument9 pagesQuantification (Popq) Terhadap Kualitasilham masdarNo ratings yet
- NCP Kenezo, Female 17Document2 pagesNCP Kenezo, Female 17labanesstephanyNo ratings yet
- Herbal - Medicines - in - The - Treatment of Mental IllnessesDocument12 pagesHerbal - Medicines - in - The - Treatment of Mental IllnessesFarash farshiNo ratings yet
- Ophthalmology STR eDocument2 pagesOphthalmology STR ekevinzhu11111No ratings yet
- Susannah Brewton - ResumeDocument2 pagesSusannah Brewton - Resumeapi-318876563No ratings yet
- Mental Health in ConnecticutDocument60 pagesMental Health in ConnecticutHelen BennettNo ratings yet
- PNA 2012 National Convention LectureDocument60 pagesPNA 2012 National Convention LectureHarby Ongbay AbellanosaNo ratings yet
- PDF Midwifery Final Test 1Document7 pagesPDF Midwifery Final Test 1DianeNo ratings yet
- 0eriodontology: 5pdate - AYDocument6 pages0eriodontology: 5pdate - AYFatima AliNo ratings yet
- AAOHNS MembershipApplicationDocument4 pagesAAOHNS MembershipApplicationAnonymous AuJncFVWvNo ratings yet
- Sample Complaints LettersDocument4 pagesSample Complaints LettersZdenka PetroskyNo ratings yet
- MEHT130423 - Information For Screening For Retinopathy of Prematurity 1.0Document4 pagesMEHT130423 - Information For Screening For Retinopathy of Prematurity 1.0Rohit BharadwajNo ratings yet
- ICM Essential Competencies For Basic Midwifery Practice 2010, Revised 2013 PDFDocument19 pagesICM Essential Competencies For Basic Midwifery Practice 2010, Revised 2013 PDFKuurniiaa PraweestiiNo ratings yet
- Tamil Nadu ReportDocument116 pagesTamil Nadu ReportVenkatasubramaniyanNo ratings yet
- PGH 101 v2018Document10 pagesPGH 101 v2018Ian Phillip PaclibareNo ratings yet
- SABA Reliance Questionnaire (SRQ) FulltextDocument34 pagesSABA Reliance Questionnaire (SRQ) FulltextPhụng KimNo ratings yet
- Final Announcement Liver UpdateDocument13 pagesFinal Announcement Liver Updatenerissa arvianaNo ratings yet
- 2023 Updated-Nursing Skills ChecklistDocument7 pages2023 Updated-Nursing Skills Checklistapi-652071746No ratings yet
- Application Form For Punjab Residency Program (Level - Iv) TrainingDocument6 pagesApplication Form For Punjab Residency Program (Level - Iv) TrainingFatima Habib JajjaNo ratings yet
- First AidDocument10 pagesFirst AidArslan Shaukat100% (1)
- Trade and Health:: Towards Building A National StrategyDocument149 pagesTrade and Health:: Towards Building A National Strategymanjusri lalNo ratings yet
- 17th HXMDP - AIIMS New DelhiDocument12 pages17th HXMDP - AIIMS New Delhiars_del0% (1)
- John Hoberman-Testosterone Dreams, Rejuvenation, Aphrodisia, Doping PDFDocument390 pagesJohn Hoberman-Testosterone Dreams, Rejuvenation, Aphrodisia, Doping PDFjpcmanso100% (3)
- Chapter 01 - Health Care Delivery and Evidence-Based Nursing PracticeDocument9 pagesChapter 01 - Health Care Delivery and Evidence-Based Nursing PracticePrince K. TaileyNo ratings yet
- Endorsement FormDocument12 pagesEndorsement Formferraterkimdaniel25No ratings yet