Professional Documents
Culture Documents
Hmo Msa Overview
Hmo Msa Overview
Uploaded by
mamatha mamtaCopyright:
Available Formats
You might also like
- Alberta Pension Plan - Analysis of Costs, Benefits, Risks and ConsiderationsDocument95 pagesAlberta Pension Plan - Analysis of Costs, Benefits, Risks and Considerationsedmontonjournal100% (3)
- SBFR Project Document MarchDocument37 pagesSBFR Project Document MarchAbdi Tofik91% (11)
- Clinic Feasibility StudyDocument20 pagesClinic Feasibility StudyJeff Bergosh100% (3)
- University of Virginia Health System-The LongTerm Acute Care Hospital ProjectDocument4 pagesUniversity of Virginia Health System-The LongTerm Acute Care Hospital ProjectAde Ade100% (1)
- Health PDFDocument25 pagesHealth PDFShurieUNo ratings yet
- Projected Medicare Expenditures Under An Illustrative Scenario With Alternative Payment Updates To Medicare ProvidersDocument18 pagesProjected Medicare Expenditures Under An Illustrative Scenario With Alternative Payment Updates To Medicare ProvidersTed OkonNo ratings yet
- 2018 Medicare Physician Fee Schedule SLPDocument14 pages2018 Medicare Physician Fee Schedule SLPAnonymous WpMUZCb935No ratings yet
- Cost ReportDocument48 pagesCost ReportdptNo ratings yet
- 2009 UdsreportingmanualDocument108 pages2009 Udsreportingmanualrtfm216No ratings yet
- ASH 2014 Medicare Physician Fee Schedule Final Rule SummaryDocument10 pagesASH 2014 Medicare Physician Fee Schedule Final Rule SummaryLiza GeorgeNo ratings yet
- PH AccountingDocument542 pagesPH Accountingolayinkaaliu38No ratings yet
- Below Is What Every Hospital Administrator Should Know About Health Care ReformDocument4 pagesBelow Is What Every Hospital Administrator Should Know About Health Care ReformMatthew TaberNo ratings yet
- IntroductionDocument8 pagesIntroductionRashiden MadjalesNo ratings yet
- IG ReportDocument44 pagesIG ReportDaniel BentleyNo ratings yet
- Multiple Choice Questions 1 The Aicpa Audit and Accounting Guide HealthDocument2 pagesMultiple Choice Questions 1 The Aicpa Audit and Accounting Guide HealthMuhammad ShahidNo ratings yet
- 2022 NCCI Manual Complete Final 1.1.2022Document275 pages2022 NCCI Manual Complete Final 1.1.2022agnaveenanNo ratings yet
- 01 Introduction Final 1.1.2021Document9 pages01 Introduction Final 1.1.2021agnaveenanNo ratings yet
- 23-25NHSPS - NHS Provider Payment Mechanisms - 23-25NHSPS - NHS-provider-payment-mechanisms - v1.1Document32 pages23-25NHSPS - NHS Provider Payment Mechanisms - 23-25NHSPS - NHS-provider-payment-mechanisms - v1.1andry budiarjoNo ratings yet
- FinalDocument26 pagesFinalitssupercindy100% (7)
- 2023 Medicare Fee Schedule For SlpsDocument23 pages2023 Medicare Fee Schedule For SlpsLeon DaleyNo ratings yet
- Concepts Statement No 8 Amended August 2018Document12 pagesConcepts Statement No 8 Amended August 2018Adham AghaNo ratings yet
- Coursework 1Document10 pagesCoursework 1Coey HoNo ratings yet
- CalPERS ReportDocument63 pagesCalPERS Reportnchc-scribdNo ratings yet
- Conceptual Framework For Financial Reporting Objectives of Financial ReportingDocument31 pagesConceptual Framework For Financial Reporting Objectives of Financial ReportingteryNo ratings yet
- PWC Utilities Power 2013Document683 pagesPWC Utilities Power 2013Iskandar HamonanganNo ratings yet
- Updated: April 2010Document30 pagesUpdated: April 2010basithalNo ratings yet
- ClaimsAdjudicationRulesV2011 Q2Document26 pagesClaimsAdjudicationRulesV2011 Q2timvrghs123No ratings yet
- 2019 Hospital Outpatient and Ambulatory Surgery Payment Systems (OPPS) Proposed Rule SummaryDocument13 pages2019 Hospital Outpatient and Ambulatory Surgery Payment Systems (OPPS) Proposed Rule SummarysundararajanNo ratings yet
- OHRS Chapter 7 v7 0 Q2 FINALDocument86 pagesOHRS Chapter 7 v7 0 Q2 FINALjanNo ratings yet
- IAS 34 Part 2Document61 pagesIAS 34 Part 2anjali sharmaNo ratings yet
- FY23 Program Guide - Vnov2021Document28 pagesFY23 Program Guide - Vnov2021stallioncode5009No ratings yet
- Getpdf 3Document76 pagesGetpdf 3WilliamNo ratings yet
- No. 2016-14 August 2016: Not-for-Profit Entities (Topic 958)Document270 pagesNo. 2016-14 August 2016: Not-for-Profit Entities (Topic 958)dinis irikaNo ratings yet
- Smi68292 ch03 064-092Document29 pagesSmi68292 ch03 064-092Beeboy CroSel100% (1)
- Chapter 7 Surgery Urinary - Male Genital - Female Genital - Maternity Care and Delivery Systems CPT Codes 50000 - 59999Document16 pagesChapter 7 Surgery Urinary - Male Genital - Female Genital - Maternity Care and Delivery Systems CPT Codes 50000 - 59999Rashiden MadjalesNo ratings yet
- SFAC No.8Document42 pagesSFAC No.8Rizky Ar100% (1)
- Proposed Statement of The Governmental Accounting Standards Board: Plain-Language SupplementDocument20 pagesProposed Statement of The Governmental Accounting Standards Board: Plain-Language SupplementGerrie SchipskeNo ratings yet
- Final Project Submission - Edited.editedDocument15 pagesFinal Project Submission - Edited.editedSammy DeeNo ratings yet
- Pde GuidanceDocument94 pagesPde GuidancerajsundarsNo ratings yet
- Summary of 2020 Changes To The Medicare Physician Fee Schedule, Quality Payment Program, and Other Federal ProgramsDocument25 pagesSummary of 2020 Changes To The Medicare Physician Fee Schedule, Quality Payment Program, and Other Federal ProgramsJared DeraneyNo ratings yet
- Embargoed Alberta Pension Plan ReportDocument95 pagesEmbargoed Alberta Pension Plan ReportCTV CalgaryNo ratings yet
- Sa1 Pu 15 PDFDocument78 pagesSa1 Pu 15 PDFPolelarNo ratings yet
- Dokumen - Tips Finance Management ManualDocument17 pagesDokumen - Tips Finance Management ManualZubair GhaznaviNo ratings yet
- Millman 2016 Analysis of Medicare IndustryDocument25 pagesMillman 2016 Analysis of Medicare Industrykhyati123No ratings yet
- Chapter 6 Surgery Digestive System CPT Codes 40000 - 49999Document16 pagesChapter 6 Surgery Digestive System CPT Codes 40000 - 49999Rashiden MadjalesNo ratings yet
- IPSAS 1 For 2022 SeptDocument5 pagesIPSAS 1 For 2022 SeptWilson Mugenyi KasendwaNo ratings yet
- Asian Development Bank QBS-TA-APP3 Prep of Financial ProposalDocument20 pagesAsian Development Bank QBS-TA-APP3 Prep of Financial Proposalrodval77No ratings yet
- ActmemosmgrpDocument3 pagesActmemosmgrpapi-373105184No ratings yet
- Final Project Submission - Edited.editedDocument15 pagesFinal Project Submission - Edited.editedSammy DeeNo ratings yet
- UTSW Internal Audit of Billing Compliance 2010Document13 pagesUTSW Internal Audit of Billing Compliance 2010reesedunklinNo ratings yet
- Conceptual Framework - DiscussionDocument7 pagesConceptual Framework - DiscussionAi MelNo ratings yet
- No. 2010-20 July 2010: Receivables (Topic 310)Document92 pagesNo. 2010-20 July 2010: Receivables (Topic 310)LexuzDyNo ratings yet
- Financial Forecasting in The Budget Preparation ProcessDocument7 pagesFinancial Forecasting in The Budget Preparation Processnmsusarla888No ratings yet
- Announcement2019 PDFDocument270 pagesAnnouncement2019 PDFHarsha VipinNo ratings yet
- Wiley GAAP for Governments 2012: Interpretation and Application of Generally Accepted Accounting Principles for State and Local GovernmentsFrom EverandWiley GAAP for Governments 2012: Interpretation and Application of Generally Accepted Accounting Principles for State and Local GovernmentsNo ratings yet
- Textbook of Urgent Care Management: Chapter 12, Pro Forma Financial StatementsFrom EverandTextbook of Urgent Care Management: Chapter 12, Pro Forma Financial StatementsNo ratings yet
- Audit Risk Alert: General Accounting and Auditing Developments, 2017/18From EverandAudit Risk Alert: General Accounting and Auditing Developments, 2017/18No ratings yet
- Implementing Results-Based Budget Management Frameworks: An Assessment of Progress in Selected CountriesFrom EverandImplementing Results-Based Budget Management Frameworks: An Assessment of Progress in Selected CountriesNo ratings yet
- OpTransactionHistory03 12 2019Document2 pagesOpTransactionHistory03 12 2019mamatha mamtaNo ratings yet
- This Is A System Generated Payslip and Does Not Require SignatureDocument1 pageThis Is A System Generated Payslip and Does Not Require Signaturemamatha mamtaNo ratings yet
- APCS494 - May 2020Document1 pageAPCS494 - May 2020mamatha mamtaNo ratings yet
- The 'S of CSW BillingDocument2 pagesThe 'S of CSW Billingmamatha mamtaNo ratings yet
- OpTransactionHistory26 01 2020Document2 pagesOpTransactionHistory26 01 2020mamatha mamtaNo ratings yet
- The Medicare Appeals Process: Five Levels To Protect Providers, Physicians, and Other SuppliersDocument3 pagesThe Medicare Appeals Process: Five Levels To Protect Providers, Physicians, and Other Suppliersmamatha mamtaNo ratings yet
- This Is A System Generated Payslip and Does Not Require SignatureDocument1 pageThis Is A System Generated Payslip and Does Not Require Signaturemamatha mamtaNo ratings yet
- Certificate For COVID-19 Vaccination: Beneficiary DetailsDocument1 pageCertificate For COVID-19 Vaccination: Beneficiary Detailsmamatha mamtaNo ratings yet
- This Is A System Generated Payslip and Does Not Require SignatureDocument1 pageThis Is A System Generated Payslip and Does Not Require Signaturemamatha mamtaNo ratings yet
- COVID-19 Vaccination Appointment Details: Center Preferred Time SlotDocument1 pageCOVID-19 Vaccination Appointment Details: Center Preferred Time Slotmamatha mamtaNo ratings yet
- July Operations Exempt Town Hall - FINALDocument31 pagesJuly Operations Exempt Town Hall - FINALmamatha mamtaNo ratings yet
- Dvanceceipt2021 07 10 13 46 46Document3 pagesDvanceceipt2021 07 10 13 46 46mamatha mamtaNo ratings yet
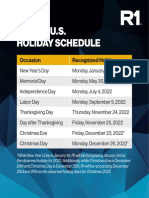
- 2022 US Holiday ScheduleDocument1 page2022 US Holiday Schedulemamatha mamtaNo ratings yet
- AdvanceReceipt2021 07 117 15Document6 pagesAdvanceReceipt2021 07 117 15mamatha mamtaNo ratings yet
- Certificate For COVID-19 Vaccination: Beneficiary DetailsDocument1 pageCertificate For COVID-19 Vaccination: Beneficiary Detailsmamatha mamtaNo ratings yet
- COVID-19 Vaccination Appointment Details: Center Date Time Preferred Time SlotDocument1 pageCOVID-19 Vaccination Appointment Details: Center Date Time Preferred Time Slotmamatha mamtaNo ratings yet
- Tax Invoice: Name Address State Gstin State Code Description AmountDocument1 pageTax Invoice: Name Address State Gstin State Code Description Amountmamatha mamtaNo ratings yet
- 2022 US Holiday ScheduleDocument1 page2022 US Holiday Schedulemamatha mamtaNo ratings yet
- D M E (DME) : Urable Edical QuipmentDocument30 pagesD M E (DME) : Urable Edical Quipmentmamatha mamtaNo ratings yet
- Laptop Policy - CernerDocument2 pagesLaptop Policy - Cernermamatha mamtaNo ratings yet
- Name: Manjushree G: B.E, Information Science and EngineeringDocument3 pagesName: Manjushree G: B.E, Information Science and Engineeringmamatha mamtaNo ratings yet
- Constipation:: Drug Therapy For Constipation & DiarroheaDocument8 pagesConstipation:: Drug Therapy For Constipation & DiarroheaDevi Prasanna 42.No ratings yet
- Generic Structure Language FeatureDocument11 pagesGeneric Structure Language FeatureAina NisaNo ratings yet
- BPT3 RD YearDocument17 pagesBPT3 RD YearKhushNo ratings yet
- Immune System AssignmentDocument2 pagesImmune System AssignmentZura KotaroNo ratings yet
- Intestinal Diseases in Cattle 2023Document30 pagesIntestinal Diseases in Cattle 2023Krystyna WędrychowskaNo ratings yet
- Aki To CKDDocument22 pagesAki To CKDSrinivas PingaliNo ratings yet
- Pathology of Nervous System2020Document33 pagesPathology of Nervous System2020AITUNRChoirul OktavianNo ratings yet
- Daftar Pustaka Bab IIDocument7 pagesDaftar Pustaka Bab IIWantoroNo ratings yet
- Curriculum Vitae: Education & Working ExperienceDocument2 pagesCurriculum Vitae: Education & Working Experienceapotek hegarNo ratings yet
- Wa0008.Document8 pagesWa0008.Dany MorBenNo ratings yet
- Pharmacology: Drugs Acting On The Endocrine SystemDocument20 pagesPharmacology: Drugs Acting On The Endocrine SystemShun Reigh SumilangNo ratings yet
- Thyroid Disorders Part I Hyperthyroidism Little 2006Document9 pagesThyroid Disorders Part I Hyperthyroidism Little 2006Jing XueNo ratings yet
- Factors Affecting The Activity of Health Caders in The Discovery of Tuberculosis Cases in Kelurahan Sonorejo SukoharjoDocument7 pagesFactors Affecting The Activity of Health Caders in The Discovery of Tuberculosis Cases in Kelurahan Sonorejo SukoharjoIntan AyuNo ratings yet
- Essay 3 BrionesDocument7 pagesEssay 3 Brionesapi-704703402No ratings yet
- AUVON AS8016 5languages Sms V1.0 211014 80x130mmDocument205 pagesAUVON AS8016 5languages Sms V1.0 211014 80x130mmjuanNo ratings yet
- Thesis Statement For Bipolar Disorder Research PaperDocument7 pagesThesis Statement For Bipolar Disorder Research Paperfvja66n5No ratings yet
- HSCP - A Brief History of Hepatitis CDocument8 pagesHSCP - A Brief History of Hepatitis CA WeaverNo ratings yet
- Basics of Knee Arthroscopy: For The BeginnersDocument40 pagesBasics of Knee Arthroscopy: For The BeginnersPedro Zambrano100% (1)
- DSM Comparison ChartDocument6 pagesDSM Comparison ChartAJ commsNo ratings yet
- NEBOSH Occupational Health Hazards by Terry RobsonDocument62 pagesNEBOSH Occupational Health Hazards by Terry RobsonAhsan HasanNo ratings yet
- Rough Draft Research Paper 11Document14 pagesRough Draft Research Paper 11api-549217680No ratings yet
- Case of TuberculosisDocument5 pagesCase of TuberculosisSheryhan Tahir BayleNo ratings yet
- Artificial Intelligence For Neurological Disorders Abraham Full ChapterDocument51 pagesArtificial Intelligence For Neurological Disorders Abraham Full Chapteralice.chao451100% (6)
- Clinically Relevant Complications Related To Pedicle Screw Placement in Thoracolumbar Surgery and Their ManagementDocument9 pagesClinically Relevant Complications Related To Pedicle Screw Placement in Thoracolumbar Surgery and Their ManagementjoshbakhNo ratings yet
- Trigger Finger-An Overview of The Treatment OptionsDocument5 pagesTrigger Finger-An Overview of The Treatment OptionsSatrya DitaNo ratings yet
- Adult Post-Cardiac Arrest Care Algorithm: o Co Io o CoDocument1 pageAdult Post-Cardiac Arrest Care Algorithm: o Co Io o CoKavya ShreeNo ratings yet
- Pemphigus Vegetans of Neumann: A Case Report of A Rare Variant of Pemphigus VulgarisDocument3 pagesPemphigus Vegetans of Neumann: A Case Report of A Rare Variant of Pemphigus VulgarisIJAR JOURNALNo ratings yet
- Introduction HmoleDocument32 pagesIntroduction HmoleBrian Montales BaggayanNo ratings yet
- MR-13 LampropoulosBLHealth2003Document19 pagesMR-13 LampropoulosBLHealth2003BillalNo ratings yet
- Herrero Vanrell2014Document17 pagesHerrero Vanrell2014Fer RodriguezNo ratings yet
Hmo Msa Overview
Hmo Msa Overview
Uploaded by
mamatha mamtaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Hmo Msa Overview
Hmo Msa Overview
Uploaded by
mamatha mamtaCopyright:
Available Formats
HMO Medical Service Agreement Overview
Medical Service Agreement (MSA) Highlights .......................................................................2
Submission Grid.......................................................................................................................7
Sample Report Formats ...........................................................................................................8
2010 Behavioral Health Referral Request Log................................................................ 8
2010 Denial/Appeal Log.................................................................................................. 9
2010 Admission Log ..................................................................................................... 10
2010 Out of Network Referral Request Log .................................................................. 11
2010 Inpatient Physician Advisor Referral Log ............................................................. 12
2010 Referral Inquiry Log ............................................................................................. 13
2010 CMF Oversight Report ......................................................................................... 14
2010 Member Complaints............................................................................................. 15
Member Complaint/Inquiry Categories.......................................................................... 17
2010 Capitated Employed Encounter Date Report Overview ....................................... 18
2010 Capitated Employed Encounter Data Report Example ........................................ 19
2010 Sample Welcome Letter Format .......................................................................... 20
HMOI/BA HMO Quarterly Income Statement and Balance Sheet Report Format ........ 23
2010 Directions for Complex Case Management Log................................................... 24
2010 Complex Case Management Case Log ............................................................... 25
IPA Attestation .............................................................................................................. 26
IPA Standards for Emergency Services ...............................................................................28
A Division of Health Care Service Corporation, a Mutual Legal Reserve Company, an Independent Licensee of the Blue Cross and Blue Shield Association
BCBSIL Provider Manual—Rev 6/10 1
HMO Medical Service Agreement Overview
Medical Service Agreement (MSA) Highlights
This is not intended to be an all-inclusive listing of changes - please refer to the actual Medical Service
Agreement for all details.
Appendix C is now the Capitation Fee Schedules. Appendix E is now the sample of Office Based Surgery
Procedures.
On page 6, definitions have been added for Office Based Surgery and Outpatient procedures to differentiate
those procedures that are in Appendix E from those in Appendix B.
On page 18, b, 1, the reference to Preadmission testing claims has been removed from the business associate
use paragraph.
Language has been added to quantify that the IPA must notify the HMO within five (5) business days if any of
the actions have occurred against the IPA or one of the IPA’s physicians.
Language has been added on page 30 to reflect the name change for the Quality Site Visit Standards. In
addition, allergies being noted in a prominent location for each medical record have been added as a chart
requirement.
Page 33 has been updated to reflect that the IPA’s Utilization Management plan must meet IDPH requirements
as well as URAC. The requirement to notify the IPA physicians regarding how to obtain the IPA UM plan and
medical criteria for decision making has also been added.
Page 43 reflects a new item F – all PAT language has been removed and Office based surgery has been
added. Appendix E has been created and is a sample of potential Office Based Surgeries. It is separate and
unique from Appendix B. Procedures in Appendix B do not qualify for reimbursement under the Office Based
Surgery provision.
Additional information clarifying the MSA language: Appendix E is attached to the January 2010 Agenda.
This is a sample of surgeries that may be able to be performed in an office. This list is only to serve as a sample
as the standard of care may change over time. The HMO will reimburse the IPA $200 per case for every surgery
that met the following criteria:
1. The surgery would have otherwise been HMO risk, performed in a Hospital Based Surgery
Center or free standing Ambulatory Surgery Center
2. he HMO did not pay a facility fee
3. he provider was accredited by: Joint Commission on Accreditation of Healthcare Organizations
(JCAHO), Accreditation Association for Ambulatory Health Care (AAAHC) or American
Association for Accreditation of Ambulatory Surgical Facilities (AAAASF)
The HMO will reimburse the IPA annually, at the same time that it calculates Utilization Management Fund
earnings and payments. The IPA will continue to receive payment for assumed but unutilized Unit associated
with these surgeries.
Language revision that the IPA shall not re-insure any of the first $14,000 of costs. Other re-insurance
thresholds have also been adjusted (page 49). Language has also been added to ensure that any
changes to the Provider Manual or any other contractual revision that changes the IPA’s financial
responsibility or liability would not become effective until the subsequent Agreement Year.
The amount payable to the IPA for each assumed but unutilized Unit for the Utilization Management Fund
has been increased to $760.00. If the IPA has implemented a hospitalist program, the unit value has been
increased to $790.00 or $840.00 as described on page 50.
Page 53 reflects a new timeline for the payment of the Utilization Management Fund – will now be paid on
or about 8 months following the end of the sixth month and the end of the calendar year.
Refer directly to the MSA (pages 54-65) for the details of the Quality Improvement Fund revisions. As
distributed in the Cover letter sent with the 2010 MSA, the following summarizes the changes to the
Quality Improvement Fund.
BCBSIL Provider Manual—Rev 6/10 2
HMO Medical Service Agreement Overview
Medical Service Agreement (MSA) Highlights (cont)
1. Semi-annual Payment
The total amount of the semi annual payment (2.0% of Capitation Fees) did not change but the payment was
divided into two components. One percent of Capitation Fees is available based upon the IPA meeting the
first five criteria, and one percent of Capitation Fees is available to IPAs that submit complete encounter data.
Specific criteria have been added as a minimum definition of “complete” encounter data. Most IPAs are
already meeting these criteria. Note that for most IPAs, rates will be much higher than these minimums.
IPAs are required to submit documentation of all encounters
An Evaluation & Management visit rate of at least 2.5 visits per member per year
A laboratory services rate of at least 2.5 per member per year
Confirmation that all claim and encounter data has been submitted by all IPA providers
Also note that IPAs that do not meet these criteria for submission of complete encounter data are not eligible
to participate in those QI Fund projects for which the denominator requires complete encounters:
Controlling High Blood Pressure
Pediatric Wellness and Prevention
Adult Wellness and Prevention
BCBSIL will begin to provide IPAs with periodic reports on their status with respect to these indicators of
encounter data completeness.
Additional information clarifying the MSA language regarding complete encounter data:
The "Evaluation & Management visits" rate includes all E&M codes (CPT codes 99201-99499).
The "lab services" rate includes all CPT codes in the "Pathology and Laboratory" section of the CPT book (CPT
codes 80047-89356).
Starting in the first quarter of 2010, BCBSIL will provide quarterly reports summarizing the IPA encounter data
rates for Evaluation & Management visits and lab services. Please note that the MSA requires that IPA encounter
data be complete, including, for example, all physician visits and all laboratory, radiology and other diagnostic
services provided by or through the IPA. Consistent submission of the specialty of the physician providing a
service is also important. IPA encounter data must include only services that were actually provided and must
reflect the dates of services on which the services were rendered. Encounter data should not include services
that are ordered but not provided or services for which a referral was issued but for which the member did not
actually have the service.
2. Annual Payments
The overall annual payment available to IPAs has increased by 0.25%.
3. Special HEDIS Payments
In 2010, BCBSIL will be collecting data on several new HEDIS measures that involve medical record review.
Some of the new measures include more than one indicator to be assessed for each sampled member.
Through 2008, the Special HEDIS Payment was $1100 per numerator event. In 2009, the payment was
reduced to $550 per numerator event for the diabetes measures, for which several indicators were being
reported for each sampled member. For 2010, BCBSIL considered a two or three tier payment methodology
for the new indicators. However, to reduce complexity, a decision was made to reduce the payment to $750
per numerator event and use the same payment amount for all indicators, regardless of whether BCBSIL is
requesting data for one indicator or several indicators for a given member.
Overall, with the new HEDIS measures for 2010 that involve medical record review, it is likely that most IPAs
will have the opportunity to earn a larger Special HEDIS Payment in 2010 than in 2009.
BCBSIL Provider Manual—Rev 6/10 3
HMO Medical Service Agreement Overview
Medical Service Agreement (MSA) Highlights (cont)
4. Seasonal Influenza Vaccination Project
1. The QI Fund project was renamed to reflect that it includes only seasonal influenza vaccination, not H1N1
vaccination.
2. Payment thresholds were not changed from 2009.
3. The 2010 Seasonal Influenza Vaccination Project will include members with asthma, diabetes,
cardiovascular disease and members age 50 and older. While the Advisory Committee on Immunization
Practices has recommended for several years that all persons age 50 and older receive a flu shot,
inclusion in the project of members age 50-64 is new. [Previously, members age 65 and older were
included along with younger members with one of the specified conditions.]
As previously communicated to IPAs, because of this change in the age range, in 2010 BCBSIL will
calculate the IPA influenza vaccination rate two ways (including and excluding members identified solely
on the basis of being age 50-64) and IPAs will be paid on the basis of the better of the two rates.
d. An outreach component was added to the project. This payment will be based upon outreach to high risk
members in the fall of 2010.
5. Cervical Cancer Screening Project
For the 2009 QI Fund, the payment thresholds were set very low as BCBSIL did not have baseline data
on which to estimate results. For 2010, the payment thresholds were adjusted in accordance with
HEDIS results and 2009 project performance. Note that this project incorporates administrative data
only; medical record data will not be accepted for this project.
6. Asthma
a. In 2009, payments were based upon the percentage of members who both receive a written asthma
action plan and have an assessment of asthma control. For 2010, these components have been
separated. One payment will be based upon the IPA asthma action plan rate and a second payment
will be based upon the IPA assessment of asthma control rate.
b. A new component of the asthma project for 2010 is payment based upon the percentage of
asthmatic members meeting NAEPP criteria for having Well Controlled asthma. Asthma control
must be assessed using a standardized tool for the member to be considered Well Controlled for this
portion of the payment.
7. Diabetes
a. Payment thresholds were adjusted in accordance with 2008 results.
b. The criteria for Overall Diabetes Preventive Care were changed. In 2009, a member had to
meet four of four criteria (HbA1c<8.0%, LDL-C<100 mg/dL, dilated retinal exam and receipt of
medical attention for nephropathy) for the member to meet criteria for Overall Diabetes
Preventive Care. For 2010, the member must meet at least four of five criteria (HbA1c<8.0%,
LDL-C<100 mg/dL, BP<140/90, dilated retinal exam and receipt of medical attention for
nephropathy) to meet criteria for Overall Diabetes Preventive Care.
8. Follow-Up After Hospitalization for Mental Illness
Payment thresholds were adjusted in accordance with 2008 results.
9. Childhood Immunization
a. Payment thresholds were adjusted in accordance with 2008 results.
b. As discussed at the QI Forum in 2009, the 2010 QI Fund includes a new payment based upon
the percentage of two year old children who received at least two doses of rotavirus vaccine.
BCBSIL Provider Manual—Rev 6/10 4
HMO Medical Service Agreement Overview
Medical Service Agreement (MSA) Highlights (cont)
10. Management of Members with Cardiovascular Conditions
a. An additional payment was added to the project. There are now two payment tiers for LDL-C
control.
b. Payment thresholds were adjusted in accordance with 2008 results.
c. Advice to quit smoking will be counted only when there is documentation that smokers have received
face to face advice to quit smoking during the one year timeframe for the project.
d. A change was made in the methodology for calculating the Advice to Quit Smoking rate. For most
IPAs, few identified members smoke so the denominator for this measure can be quite small.
Therefore, to reduce variation in results due to small numbers, the Advice to Quit Smoking rate will
be a two year rate. [The denominator for this indicator will be all members included in the
denominator for the 2009 project plus all members included in the denominator for the 2010 project.
The numerator will be all members included in the numerator for the 2009 project plus all members
included in the numerator for the 2010 project. Members included in the project both years will be
counted twice, once for each year.] In 2010, the Advice to Quit Smoking rate will be calculated as
both a one year rate and a two year rate, and IPAs will receive credit for the better of the two rates.
11. Breast Cancer Screening
Payment thresholds were adjusted in accordance with 2009 project results. As in previous years, this
project incorporates administrative data only; medical record data will not be accepted for this project.
12. Colorectal Cancer Screening
Payment thresholds were adjusted in accordance with 2009 project results.
13. Controlling High Blood Pressure
a. Payment thresholds were adjusted in accordance with 2009 project results.
b. Criteria for assessing the completeness of encounter data were updated for consistency
throughout the MSA.
14. Pediatric Wellness and Prevention
a. The Wellness and Prevention project was divided into pediatric and adult components.
b. For children, IPAs can earn two payments: one based upon the percentage of children who
have had an assessment of BMI percentile in 2009 and one based upon the percentage of
children who received counseling for both physical activity and nutrition in 2009.
c. Numerator and denominator criteria were revised in accordance with HEDIS specifications.
BCBSIL Provider Manual—Rev 6/10 5
HMO Medical Service Agreement Overview
Medical Service Agreement (MSA) Highlights (cont)
15. Adult Wellness and Prevention
a. The Wellness and Prevention project was divided into pediatric and adult components.
b. For adults, IPAs can earn two payments: one based upon the percentage of adults who had an
assessment of BMI in 2008 or 2009 and one based upon Advice to Quit Smoking and Screening for
Problem Drinking.
c. Payment for the Advice to Quit Smoking and Screening for Problem Drinking measure will be based
upon the percentage of identified members who meet the following four criteria:
i. Smoking status is documented.
ii. If the member is a smoker, the member received advice to quit smoking in 2008 or 2009.
iii. The member has had an assessment of alcohol use
iv. If the member uses alcohol, the member was screened for problem drinking using a
standardized assessment tool in 2008 or 2009.
d. Numerator and denominator criteria were revised in accordance with HEDIS specifications.
16. Patient Safety Physician Education Project
This program was removed from the MSA for 2010.
• The Prescription Drug Management Fund thresholds have been revised. Refer directly to page 65 for the
details. Please note that there may be two typographical errors in this section. The first is in the
description of the top tier. Eleven percent (11 %) is available for reaching at least seventy-six percent of
all prescriptions for members enrolled in the IPA are generic. The second is tier four percent tier is from
sixty to sixty-three point nine-nine percent (60.00% - 63.99%). Also note that the HMO now provides a
report on the top 150 prescribers for the IPA instead of the 25 that was previously available. In addition,
the Prescription Drug Fund will now be paid on or about five (5) months after the end of the calendar
year.
BCBSIL Provider Manual—Rev 6/10 6
HMO Medical Service Agreement Overview
Submission Grid
HMOs* of Blue Cross Blue Shield of Illinois
2010 Submission Grid
Annual - 150
10th of days after the
Due each 1st qtr 2nd qtr 3rd qtr 4th qtr 4th qtr end of the IPA's
Date: Month 2/15/2010 05/01/2010 1st qtr 05/31/2010 07/31/2010 2nd qtr 08/31/2010 10/31/2010 3rd qtr 11/30/2010 01/31/2011 02/28/2011 fiscal year
Annual
Financial
Capitated/ Statement (incl
Employed balance sheet)
Denial/Appe IPA/CMF Capitated/Employed IPA/CMF Capitated/ IPA/CMF Capitated/ IPA/CMF Provider (audited or
al Log & Oversight report Provider Encounter Oversight report Employed Provider Oversight report (if Employed Provider Oversight report Encounter independently
Files UM Plan (if applicable) Report (if applicable) Encounter Report applicable) Encounter Report (if applicable) Report prepared)
Case Mngmt Income and
Report due
Expense
the 10th of
Income and Income and Income and Report,
the month
after the Expense Report, Expense Report, Expense Report, electronically
quarter ends electronically BH telephone electronically BH telephone electronically BH telephone submitted,
(April 10, July submitted, YTD, Access standards submitted, YTD, Access standards submitted, YTD, Access standards YTD, cash
10, Oct 10, cash basis, contract report - if cash basis, contract report - if cash basis, contract report - if basis, contract
January 10) IPA attestation specific applicable specific applicable specific applicable specific
IPA Provider
Roster
Spreadsheet
electronically
submitted
Welcome letter - (if
not already submitted
with UM plan)
CMF Service
Agreement +
Oversight Plan,
incl. Beh. Health
Care CMFs, if
appl.
BH telephone
Access standards
report - if
applicable
Upon HMO
Request: 1. Behavioral Health Referral Request Log 2. Complaint Report 3. Out of Network Referral Log 4. Inpt. Phys. Advisor Referral Log 5. Admission Log 6. Complex Case Mngmt Log
Revised 1/10 * HMO Illinois and Blue Advantage HMO
All submissions should be sent to: Ernestine Brown - Browne@BCBSIL.com or fax - 312-540-8206.
BCBSIL Provider Manual—Rev 6/10 7
HMO Medical Service Agreement Overview
Sample Report Formats
2010 Behavioral Health Referral Request Log
IPA #/Name:_______________________________ Month: ______________
# of Visits Approved
Name of PCP Requesting Date Referral Date Referral Date PCP
Member ID #: ICD - 9 Code (Include Initial
Referral Received Approved Notified
Assessments)
* HMO Illinois and Blue Advantage HMO If Referral is approved record on this form.
If denied, record on the Denial/Appeal Log. 11/09
BCBSIL Provider Manual—Rev 6/10 8
HMO Medical Service Agreement Overview
2010 Denial/Appeal Log
MG/IPA #/Name:______________________________________ Product: HMOI [ ] BA HMO [ ] Month: _________
For questions regarding log:
Contact Name: ______________________________ Phone: ________________________
*Type of Denial Reason Date of
Date of Date of
Date Referral Service Codes: 1 Medical Necessity; Date of Appeal
Member Group # Member ID # Member Physician
Received Denial Code 2 Out of Network; Denial (date or
Letter Letter
(1-8) 3 Noncovered Benefit N/A)
*HMO Illinois and BlueAdvantage HMO
Nov-09
Type of Service Denial Codes:
1 - Inpatient days 2 - Specialist Referral 3 - Outpatient Surgery 4 - Labs/Diagnostic Testing 5 - DME/Medical Equipment 6 - Drugs 7- Investigational Treatment 8 -
Other
BCBSIL Provider Manual—Rev 6/10 9
HMO Medical Service Agreement Overview
2010 Admission Log
IPA #/Name:
______________________________________________________ Month: _________________________________
Member Name and ID: Facility Diagnosis/Procedures Performed PCP or Admitting Physician Admit Date Discharge Date
*HMO Illinois and BlueAdvantage HMO
11/09
BCBSIL Provider Manual—Rev 6/10 10
HMO Medical Service Agreement Overview
2010 Out of Network Referral Request Log
_____________
IPA #/Name:___________________________ Month: _
Name of PCP Date
Out of Network Service Date Referral Date PCP/MBR
Member ID #: Requesting Referral Notified
Requested Requested
Referral Approved
No. of Referrals for ALL Medical Specialties ________ *HMO Illinois, BlueAdvantage HMO
No. of Referrals for Behavioral Health _________ Reviewed 11/09
BCBSIL Provider Manual—Rev 6/10 11
HMO Medical Service Agreement Overview
2010 Inpatient Physician Advisor Referral Log
IPA #/Name: ______________________________________________________ Month: ______
Date of Referral to
Member ID #: Admit Date Reason for Referral Approved Denied
PA
*HMO Illinois, BlueAdvantage HMO
Reviewed 11/09
BCBSIL Provider Manual—Rev 6/10 12
HMO Medical Service Agreement Overview
2010 Referral Inquiry Log
IPA #/Name______________________________________________ Month: ____________________
Date Inquiry
Date Inquiry Referral Inquiry Outcome
Case Identifier Service Requested Discussed with PCP
Initiated Deny/Approve
and/or Attending
*HMO Illinois, BlueAdvantage HMO
11/09
BCBSIL Provider Manual—Rev 6/10 13
HMO Medical Service Agreement Overview
2010 CMF Oversight Report
HMOs* of Blue Cross Blue Shield of Illinois
2010 CMF Oversight Report
Quarterly Submission Schedule
st
1 Quarter 2nd Quarter 3rd Quarter 4th Quarter
Due at HMO on April 30 July 31 October 31 January 31
IPA #: __________________________ Quarter : 1st 2nd 3rd 4th
IPA Name:______________________________ Product: HMO Illinois
(9Check One) BA HMO
List all services delegated to CMF
[] Claims [] Utilization Management
[] Membership/Eligibility [] Quality Review
[] Customer Service [] MSA/Contracting
[] Credentialing
List dates and attendance of meetings where IPA personnel reviewed CMF activities:
List name of report and date of review/approval for all reports provided to the IPA by the CMF for oversight
purposes:
List date of review and approval of CMF Quality Plan (annually):
Were any of the complaints submitted to the HMO related to the CMF activities? If so, list the complaints, the
resolution of the complaints, and the IPA action addressing the CMF’s process that may have resulted in the
complaint. (What action was taken to prevent reoccurrence of the complaint?)
Revised 12/09 *HMO Illinois and Blue Advantage HMO
BCBSIL Provider Manual—Rev 6/10 14
HMO Medical Service Agreement Overview
2010 Member Complaints
HMOs* of Blue Cross Blue Shield of Illinois
2010 Member Complaints
Cover Sheet --Submit Upon HMO Request Only
Instructions
1. Use separate submission covers for HMOI and Blue Advantage HMO products & for individual IPA sites.
2. Assign ONE category per complaint: Choose the type that best fits the description.
3. Attach (staple or bind) all relevant documentation behind this submission cover sheet for each HMO product.
4. If no complaints were submitted, please indicate “0” in appropriate boxes.
5. Submit complaints only. NO inquiries please.
6. Please submit data to your Network Consultant by the dates outlined below, IF REQUESTED.
Quarterly Submission Schedule
IF REQUESTED, 1st Quarter 2nd Quarter 3rd Quarter 4th Quarter
due at HMO on April 30 July 31 October 31 January 31
IPA #: __________________________ Quarter : 1st 2nd 3rd 4th
IPA Name:______________________________ Product: HMO Illinois
(9Check One) BA HMO
Month 1 Month 2 Month 3 Total Complaints
by Type
Name of Month __________ __________ _________ (Add three months
of data per category)
Complaint Category:
ADM
ACC
QOC
OTH
Total Complaints per Quarter
Complaint Category Descriptions:
ADM R B ACC C QOC OTH
Administrative Referral Benefit Access Claims Quality of Care Other 11/09
BCBSIL Provider Manual—Rev 6/10 15
HMO Medical Service Agreement Overview
2010 Member Complaint Log Report
HMOs* of Blue Cross Blue Shield of Illinois
2010 Member Complaint Log Report-Submit Upon Request Only
Complaint: an expression of dissatisfaction, oral or written. All complaints must be resolved within 30 days of
receipt. All complaints must be discussed in monthly QR/UM meetings.
Quarterly Submission Schedule
st
IF REQUESTED 1 Quarter 2nd Quarter 3rd Quarter 4th Quarter
due at HMO on April 30 July 31 October 31 January 31
IPA #: __________________________ Quarter : 1st 2nd 3rd 4th
IPA Name:______________________________ Product: HMO Illinois
(9Check One) BA HMO
Member Name: Group & ID #:
Category of Complaint: ADM R B ACC C QOC OTH
PCP/Provider Name: License #:
Receipt Date: Date of Incident: Resolution Date: Date letter sent to UM Mtg. Review Date:
member:
Problem:
Findings of Investigation:
Recommendation of UM/QR Committee:
Resolution and follow-up:
HMO Illinois and Blue Advantage HMO
Revised 11/08
BCBSIL Provider Manual—Rev 6/10 16
HMO Medical Service Agreement Overview
Member Complaint/Inquiry Categories
Complaint: An expression of dissatisfaction, oral or written
Inquiry: A request for information or a request for investigation of a potential problem
ADM = Administrative
Member inquiring about an administrative issue. For example:
member complains of rudeness, attitude, or inattentive staff
clerical, facility issues
management issues
membership/eligibility/ID card issues
provider related concerns not related to Quality of Care
ACC = Access
Member inquiring about access issues such as:
availability/timeliness/appropriateness of appointments
difficult access to PCP and/or support staff by telephone
answering service issues
insufficient PCPs to cover geographic location
reduced access to PCP and medical services because patient is an HMO member
R = Referrals
Any referral related issues. For example:
availability/timeliness/appropriateness/processing
denied access to a specialist
C = Claims
Member inquiring about any claim issues. For example:
unpaid claim
claim payment amount
B = Benefits
Member dissatisfied with HMO benefits or benefit coverage.
QOC = Quality of Care
Member inquiring about the quality of medical care received through HMO providers. This may include:
provider prescribed the wrong medication
member feels illness was misdiagnosed or not properly treated
OTH = Other
Member inquiring about any other problems that require investigation that does not fit into the other categories.
HMO Illinois and Blue Advantage HMO
Revised 11/09
BCBSIL Provider Manual—Rev 6/10 17
HMO Medical Service Agreement Overview
2010 Capitated Employed Encounter Date Report Overview
PCP report (all PCPs should be included)
Create a spreadsheet that contains the following columns:
- PCP name
- PCP specialty
- Average current membership assigned to this PCP
- Number of claims received in the quarter.
- Average number of claims adjudicated in the quarter.
- Average number of claims received divided by the average current PCP membership will give us
the average number of claims received/adjudicated by capitated/employed PCP.
The Average number of claims adjudicated for each PCP should look similar to the other PCPs in that
specialty. If the data for a particular PCP does not look within the range of the other values, then the
IPA should investigate whether the PCP is not submitting complete claim/encounter data and document
the IPA’s action plan for obtaining complete claim/encounter data. (with follow up reports on action
items in subsequent quarters)
Specialist/Ancillary provider report
Create a spreadsheet that contains the following columns:
- Specialty/Ancillary provider/provider group name
- IPA average current membership
- Number of claims received
- Average number of claims received in the quarter divided by Average current membership will give
us the average number of claims received/adjudicated by capitated/employed Specialist and
capitated Ancillary facility.
The Average number of claims adjudicated or allowed charges received for each Specialty/Ancillary
Group should be within the range of the other values established for that Specialty/Ancillary Group or
the PMPM value should approximate the PMPM subcapitated amount paid to the Specialty/Ancillary
Group. If this is not the case, then the IPA should investigate whether the Specialty/Ancillary Group is
not submitting complete claim/encounter data and document the IPA’s action plan for obtaining
complete claim/encounter data. (with follow up reports on action items in subsequent quarters).
Revised 12/09
BCBSIL Provider Manual—Rev 6/10 18
HMO Medical Service Agreement Overview
2010 Capitated Employed Encounter Data Report Example
HMOI/BA 1ST QTR PCP REPORT
PCP SPEC AVG MBR #CLM RCV AVG # CLM ADJ
###### 1 PEDIATRIC 82 24 0.29
###### 2 FAMILY PRAC 297 233 0.78
###### 3 FAMILY PRAC 104 60 0.58
###### 4 FAMILY PRAC 156 56 0.36
###### 5 PEDIATRIC 48 25 0.52
###### 6 INTERNAL MED 18 7 0.39
###### 7 INTERNAL MED 224 131 0.58
###### 8 PEDIATRIC 55 43 0.78
###### 9 PEDIATRIC 0 0 0.00
###### 10 INTERNAL MED 70 81 1.16
###### 11 INTERNAL MED 35 0 0.00
HMOI/BA SPECIALIST and ANCILLARY PROVIDER REPORT
1ST QUARTER
SPECIALTY GRP NAME AVG MBR #CLM RCV AVG # CLM ADJ
RADIOLOGY ####### 127 67 0.53
1st QUARTER
ANCILLARY FACILITY AVG MBR #CLM RCV AVG # CLM ADJ
Radiology Facility ######## 123 76 0.62
BCBSIL Provider Manual—Rev 6/10 19
HMO Medical Service Agreement Overview
2010 Sample Welcome Letter Format
IPA Name
Address
City State Zip
Phone Number
Dear Managed Care Member:
On behalf of the physicians and staff of , I would like to thank you for selecting us as your
managed care provider. (Short description of IPA.)
As you may know, a major factor of your managed care plan is the active role of your Primary Care Physician
(PCP). Your Primary Care Physician will be responsible for directing all of your health care needs. Be sure to
contact your Primary Care Physician whenever you need to seek health care services. Services rendered
outside of may not be covered if prior authorization has not been obtained.
This plan provides for preventive services intended to help maintain your health and to promote early detection of
disease. We strongly encourage you and the enrolled members of your family to work with your personal Primary
Care Physicians to obtain general physicals.
Your IPA has the ability to provide case management services if your condition warrants. If you think you
might be a candidate for these services, you or you PCP may contact us at_____________
It is important that each member selects a Primary Care Physician and knows how to reach him or her. To further
assist you in understanding your health care coverage, our staff has prepared the enclosed reference sheet. If
you have any questions, please feel free to call us at . We look forward to a long and healthy
relationship.
Sincerely,
Rev 12/09
BCBSIL Provider Manual—Rev 6/10 20
HMO Medical Service Agreement Overview
MAKE YOUR HMO WORK FOR YOU
FOLLOW THESE EASY STEPS:
Choosing or changing your Primary Care Physician (PCP) from the enclosed list
Please make sure the PCP you have selected is on the enclosed list.
Select or change your PCP by contacting our office at .
Choosing or changing your Woman’s Principal Health Care Provider (WPHCP)
A Woman’s Principal Health Care Provider (WPHCP) is an Obstetrician/Gynecologist (OB/GYNE) who has
been selected to be directly accessible for treating and coordinating a female Member's health care needs.
The WPHCP must have a referral arrangement with the female Member's PCP.
Please make sure the WPHCP you have selected is on the enclosed list.
Select or change your WPHCP by contacting our office at _________________________.
Call your Primary Care Physician and WPHCP for a get acquainted visit
Have your HMO Identification Card with you.
Please be aware that co-payment amounts vary by HMO plan and are payable at the time of the visit.
Behavioral Health Care Services
If you are in need of Behavior Health Care services, you should______________. (outline how member should
access care)
Chemical Dependency Services
Benefits are available through the HMO Illinois Chemical Dependency Network for the treatment of Substance
Abuse whether or not the Covered Services rendered have been ordered by your Primary Care Physician or
Woman’s Principal Health Care Provider. To obtain benefits for Substance Abuse Treatment, you must call the
HMO Illinois Chemical Dependency Hotline at 1 (800) 346-3986.
Medical Records and Patient Confidentiality
If you have medical records that need to be transferred to this facility, please have those records transferred as
soon as possible.
If you need a copy of your medical record, you must _________________.
Medical Records are held in strict confidence.
Emergency Services
Prior to seeking care in an emergency room, we recommend that you call your PCP for treatment advice.
In situations where you feel you can't call your PCP, such as when you think you may be having a heart attack
or a stroke, go directly to the to the nearest hospital emergency room. Notify your PCP as soon as possible of
any treatment you receive.
To contact your PCP call _________________.
A referral for services not directly provided by your PCP may be required
Your PCP will coordinate your overall health care and determine the need for specialty care referrals for
medically necessary services.
All referrals undergo a review process.
If a referral is denied, the reason for the denial, the alternative treatment, a telephone number for questions,
and the mechanism for appeal will be communicated to you in writing.
Be sure to verify the date and type of referral you receive.
BCBSIL Provider Manual—Rev 6/10 21
HMO Medical Service Agreement Overview
Utilization Management Process
Pre-Admission Certification and Concurrent Review are two programs established to ensure that you receive
the most appropriate and cost effective health care.
Your PCP must obtain approval from your Participating IPA prior to inpatient hospital admission other than
emergency situations.
Your participating IPA may recommend other courses of treatment that could help you avoid an Inpatient stay.
It is your responsibility to cooperate with the recommendations made by your PCP.
Concurrent Review ensures that your length of stay is appropriate given your diagnosis and treatment.
You may contact us to discuss the Utilization Management Process or any issues regarding it by calling our toll
free phone number _____________ or by calling ____________collect.
Appeal Process
Communication with your physician is an important part of your health care. If you do not understand any
course of your care, please discuss this with your PCP.
You can also contact our Patient Advocate at _________________. The role of the Patient Advocate is to help
with Member issues or concerns that cannot be resolved through normal channels.
As an HMO member, you have the right to appeal any payment or denial of covered services by contacting our
HMO office at _____________________ or in writing at _____________ or this can be initiated by contact the
HMOs of Blue Cross Blue Shield of Illinois at 312-653-6600 or in writing at:
HMO Appeal Committee
300 East Randolph
Chicago Il 60601
Following an adverse determination for a clinical service, procedure or treatment that is not reviewed as
medically necessary, any involved party may request an external independent review.
Rev 12/09
BCBSIL Provider Manual—Rev 6/10 22
HMO Medical Service Agreement Overview
HMOI/BA HMO Quarterly Income Statement and Balance Sheet Report Format
This report is only available electronically. Contact your Provider Network Consultant to obtain the
report.
BCBSIL Provider Manual—Rev 6/10 23
HMO Medical Service Agreement Overview
2010 Directions for Complex Case Management Log
The case management log does not need to be sent in quarterly. The log will be requested prior to the
case management audit. The case management audit cases will be chosen at least two weeks prior to
the audit. The HMO log is a sample log, but any IPA log must have all the elements that are requested.
1. Patient ID/ Name – can be any number that enables the IPA to find the patient. Name or initials
should also be included.
2. Date Opened - the date the case was opened as a complex case managed case.
3. Identified by – how the case was identified as a complex case management case. Use the
sources identified in the HMO UM Plan.
4. Diagnosis – this should be the diagnosis that is associated with the case managed case.
5. Guidelines used – this is not a Yes or No. This column should be completed with the name of
the guideline the IPA has adopted.
6. Date closed - this column will remain blank until the patient is no longer being case managed.
Cases should be chosen from this log for audit (AT LEAST 1). Try to choose cases that
encompass the different methods of case identification.
BCBSIL Provider Manual—Rev 6/10 24
HMO Medical Service Agreement Overview
2010 Complex Case Management Case Log
SAMPLE LOG
IPA # and NAME: _______________________________________________________
Patient ID/ Date Opened Identified by Diagnosis Guidelines used to Date Closed
Name (code 1) manage case
1
10
11
12
1. Identification codes: A. Claims data
B. Hospital discharge data
C. Pharmacy data
D. Data collected through UM process
E. D2 Hawkeye report
12/09
BCBSIL Provider Manual—Rev 6/10 25
HMO Medical Service Agreement Overview
IPA Attestation
Hospital Affiliation(s): ____________________ site number(s): _________________
IPA attests that it has written agreement with all IPA Physicians or other providers of professional or
ancillary services (“Provider”) that render care to Blue Cross and Blue Shield of Illinois (“BCBSIL”) HMO
Members. A list of Providers that the IPA has written agreements with is attached hereto as Exhibit A).
This list includes but is not limited to: PCPs, specialists, facilities, ancillary providers, sub-specialists
and hospital based physicians, and includes any and all agreements in place for the provision of care to
BCBSIL HMO Members. IPA further attests that the IPA’s written agreements with each of its
Providers contain, at a minimum, the following:
a) Provider’s responsibilities;
b) Provider’s compensation;
c) Agreement to seek compensation not from HMO or Member but solely from the IPA for services
provided to Members;
d) Agreement to participate in quality of care review activities as requested by the IPA, including
allowing access to medical records for HEDIS reporting and other HMO quality improvement
initiatives;
e) Professional liability insurance coverage – each Provider shall maintain a valid current policy (or
policies) of insurance with a solvent insurer of national reputation covering professional liability of
each Provider, his/her agents and employees, which is in an amount not less than $1,000,000 per
claim and $3,000,000 annual aggregate coverage. Each Provider shall carry such other insurance
as shall be necessary to insure each Provider, his/her agents and employees against any and all
damages arising from each Provider’s various duties and obligations;
f) Agreement to preserve patient confidentiality;
g) Agreement not to charge any Provider that has a contractual or other affiliation with another
Participating IPA more than the BlueCross BlueShield of Illinois PPO Schedule of Maximum
Allowances for referred or Emergency services, provided to Members of such Participating IPA, if
such bills are paid within 30 days of the Participating IPA’s receipt of such bills; and
h) Agreement that IPA Physicians and/or IPA are solely responsible for the provision of all healthcare
services to Members. All decisions regarding Member treatment and care are the sole
responsibility of IPA Physicians and such decisions are neither directed nor controlled by HMO.
And, except as to the amount and manner of payment, the Agreement shall in no way affect the
usual physician/patient relationship. The IPA and IPA Physicians shall provide services to
Members in the same manner and quality as those services that are provided to other patients of
the IPA/IPA Physicians that are not HMO Members.
BCBSIL Provider Manual—Rev 6/10 26
HMO Medical Service Agreement Overview
1) _________ IPA attests that the above listed terms and conditions are in the current written
agreements between the IPA and IPA Physicians and Providers (provide copies of each
written agreement)
2) _________ IPA attests that it has obtained a written Addendum from all contracting IPA Physicians
and providers which includes the information set forth in (a) – (h) above (provide copies
of each executed Addendum)
3) _________ IPA has communicated the above listed terms and conditions to IPA Physicians and
Providers in some other manner as set forth in the attachment hereto , that is legally
binding, acceptable to the HMO and ensures that IPA Physicians and Providers
acknowledge and agree with the above listed terms and conditions. IPA agrees to hold
harmless and indemnify HMO for the failure of any IPA Physician or Provider to adhere
to the above listed terms and conditions set forth in (a) – (h) above.
_________________________________ _____________________________
“IPA” Authorized Signature Title
________________________________
Print name
_____________________________
Date
BCBSIL Provider Manual—Rev 6/10 27
HMO Medical Service Agreement Overview
IPA Standards for Emergency Services
All IPAs participating in the HMO Network must meet the following minimum standards for emergency
services:
1. The IPA is required to have a 24-hour answering service available every day including weekends
and holidays to handle emergency calls. The IPA must also assure that each PCP and WPHCP
provides a 24-hour answering arrangement, including a 24-hour on call PCP arrangement.
2. The IPA must provide the answering service with written guidelines and procedures that include, at
a minimum, the following information:
An updated schedule of the physician on call, depending on the specific schedule of the IPA.
A complete list of Primary Care Physicians
Written procedures for handling emergency calls which include keeping a documented log with
the following information:
Patient’s name and age
Caller’s name
Date of call
Patient’s symptoms
Physician contacted and time of such contact
Instructions given by service to patient (caller)
3. The answering service should send this log to the IPA at a minimum, weekly, to facilitate the IPA’s
ability to confirm phone contact from members. Each PCP, WPHCP and Behavior Health
Practitioner should maintain an answering service log.
4. The IPA should review the answering service log for any discrepancies and problems. The Medical
Director or Quality Review Committee should review any discrepancies or identified problems.
5. The IPA should maintain the log in their files for at least one year.
6. Those IPAs in heavily ethnic areas (e.g., Spanish) should provide an answering service that speaks
the particular language of the population served.
The HMO reserves the right to survey IPA’s answering service to assure compliance with these
standards.
Each HMO member is instructed through the Marketing Account Executive, product brochures,
literature, newsletters and the IPA administration to call his/her IPA when an emergency situation
arises.
BCBSIL Provider Manual—Rev 6/10 28
You might also like
- Alberta Pension Plan - Analysis of Costs, Benefits, Risks and ConsiderationsDocument95 pagesAlberta Pension Plan - Analysis of Costs, Benefits, Risks and Considerationsedmontonjournal100% (3)
- SBFR Project Document MarchDocument37 pagesSBFR Project Document MarchAbdi Tofik91% (11)
- Clinic Feasibility StudyDocument20 pagesClinic Feasibility StudyJeff Bergosh100% (3)
- University of Virginia Health System-The LongTerm Acute Care Hospital ProjectDocument4 pagesUniversity of Virginia Health System-The LongTerm Acute Care Hospital ProjectAde Ade100% (1)
- Health PDFDocument25 pagesHealth PDFShurieUNo ratings yet
- Projected Medicare Expenditures Under An Illustrative Scenario With Alternative Payment Updates To Medicare ProvidersDocument18 pagesProjected Medicare Expenditures Under An Illustrative Scenario With Alternative Payment Updates To Medicare ProvidersTed OkonNo ratings yet
- 2018 Medicare Physician Fee Schedule SLPDocument14 pages2018 Medicare Physician Fee Schedule SLPAnonymous WpMUZCb935No ratings yet
- Cost ReportDocument48 pagesCost ReportdptNo ratings yet
- 2009 UdsreportingmanualDocument108 pages2009 Udsreportingmanualrtfm216No ratings yet
- ASH 2014 Medicare Physician Fee Schedule Final Rule SummaryDocument10 pagesASH 2014 Medicare Physician Fee Schedule Final Rule SummaryLiza GeorgeNo ratings yet
- PH AccountingDocument542 pagesPH Accountingolayinkaaliu38No ratings yet
- Below Is What Every Hospital Administrator Should Know About Health Care ReformDocument4 pagesBelow Is What Every Hospital Administrator Should Know About Health Care ReformMatthew TaberNo ratings yet
- IntroductionDocument8 pagesIntroductionRashiden MadjalesNo ratings yet
- IG ReportDocument44 pagesIG ReportDaniel BentleyNo ratings yet
- Multiple Choice Questions 1 The Aicpa Audit and Accounting Guide HealthDocument2 pagesMultiple Choice Questions 1 The Aicpa Audit and Accounting Guide HealthMuhammad ShahidNo ratings yet
- 2022 NCCI Manual Complete Final 1.1.2022Document275 pages2022 NCCI Manual Complete Final 1.1.2022agnaveenanNo ratings yet
- 01 Introduction Final 1.1.2021Document9 pages01 Introduction Final 1.1.2021agnaveenanNo ratings yet
- 23-25NHSPS - NHS Provider Payment Mechanisms - 23-25NHSPS - NHS-provider-payment-mechanisms - v1.1Document32 pages23-25NHSPS - NHS Provider Payment Mechanisms - 23-25NHSPS - NHS-provider-payment-mechanisms - v1.1andry budiarjoNo ratings yet
- FinalDocument26 pagesFinalitssupercindy100% (7)
- 2023 Medicare Fee Schedule For SlpsDocument23 pages2023 Medicare Fee Schedule For SlpsLeon DaleyNo ratings yet
- Concepts Statement No 8 Amended August 2018Document12 pagesConcepts Statement No 8 Amended August 2018Adham AghaNo ratings yet
- Coursework 1Document10 pagesCoursework 1Coey HoNo ratings yet
- CalPERS ReportDocument63 pagesCalPERS Reportnchc-scribdNo ratings yet
- Conceptual Framework For Financial Reporting Objectives of Financial ReportingDocument31 pagesConceptual Framework For Financial Reporting Objectives of Financial ReportingteryNo ratings yet
- PWC Utilities Power 2013Document683 pagesPWC Utilities Power 2013Iskandar HamonanganNo ratings yet
- Updated: April 2010Document30 pagesUpdated: April 2010basithalNo ratings yet
- ClaimsAdjudicationRulesV2011 Q2Document26 pagesClaimsAdjudicationRulesV2011 Q2timvrghs123No ratings yet
- 2019 Hospital Outpatient and Ambulatory Surgery Payment Systems (OPPS) Proposed Rule SummaryDocument13 pages2019 Hospital Outpatient and Ambulatory Surgery Payment Systems (OPPS) Proposed Rule SummarysundararajanNo ratings yet
- OHRS Chapter 7 v7 0 Q2 FINALDocument86 pagesOHRS Chapter 7 v7 0 Q2 FINALjanNo ratings yet
- IAS 34 Part 2Document61 pagesIAS 34 Part 2anjali sharmaNo ratings yet
- FY23 Program Guide - Vnov2021Document28 pagesFY23 Program Guide - Vnov2021stallioncode5009No ratings yet
- Getpdf 3Document76 pagesGetpdf 3WilliamNo ratings yet
- No. 2016-14 August 2016: Not-for-Profit Entities (Topic 958)Document270 pagesNo. 2016-14 August 2016: Not-for-Profit Entities (Topic 958)dinis irikaNo ratings yet
- Smi68292 ch03 064-092Document29 pagesSmi68292 ch03 064-092Beeboy CroSel100% (1)
- Chapter 7 Surgery Urinary - Male Genital - Female Genital - Maternity Care and Delivery Systems CPT Codes 50000 - 59999Document16 pagesChapter 7 Surgery Urinary - Male Genital - Female Genital - Maternity Care and Delivery Systems CPT Codes 50000 - 59999Rashiden MadjalesNo ratings yet
- SFAC No.8Document42 pagesSFAC No.8Rizky Ar100% (1)
- Proposed Statement of The Governmental Accounting Standards Board: Plain-Language SupplementDocument20 pagesProposed Statement of The Governmental Accounting Standards Board: Plain-Language SupplementGerrie SchipskeNo ratings yet
- Final Project Submission - Edited.editedDocument15 pagesFinal Project Submission - Edited.editedSammy DeeNo ratings yet
- Pde GuidanceDocument94 pagesPde GuidancerajsundarsNo ratings yet
- Summary of 2020 Changes To The Medicare Physician Fee Schedule, Quality Payment Program, and Other Federal ProgramsDocument25 pagesSummary of 2020 Changes To The Medicare Physician Fee Schedule, Quality Payment Program, and Other Federal ProgramsJared DeraneyNo ratings yet
- Embargoed Alberta Pension Plan ReportDocument95 pagesEmbargoed Alberta Pension Plan ReportCTV CalgaryNo ratings yet
- Sa1 Pu 15 PDFDocument78 pagesSa1 Pu 15 PDFPolelarNo ratings yet
- Dokumen - Tips Finance Management ManualDocument17 pagesDokumen - Tips Finance Management ManualZubair GhaznaviNo ratings yet
- Millman 2016 Analysis of Medicare IndustryDocument25 pagesMillman 2016 Analysis of Medicare Industrykhyati123No ratings yet
- Chapter 6 Surgery Digestive System CPT Codes 40000 - 49999Document16 pagesChapter 6 Surgery Digestive System CPT Codes 40000 - 49999Rashiden MadjalesNo ratings yet
- IPSAS 1 For 2022 SeptDocument5 pagesIPSAS 1 For 2022 SeptWilson Mugenyi KasendwaNo ratings yet
- Asian Development Bank QBS-TA-APP3 Prep of Financial ProposalDocument20 pagesAsian Development Bank QBS-TA-APP3 Prep of Financial Proposalrodval77No ratings yet
- ActmemosmgrpDocument3 pagesActmemosmgrpapi-373105184No ratings yet
- Final Project Submission - Edited.editedDocument15 pagesFinal Project Submission - Edited.editedSammy DeeNo ratings yet
- UTSW Internal Audit of Billing Compliance 2010Document13 pagesUTSW Internal Audit of Billing Compliance 2010reesedunklinNo ratings yet
- Conceptual Framework - DiscussionDocument7 pagesConceptual Framework - DiscussionAi MelNo ratings yet
- No. 2010-20 July 2010: Receivables (Topic 310)Document92 pagesNo. 2010-20 July 2010: Receivables (Topic 310)LexuzDyNo ratings yet
- Financial Forecasting in The Budget Preparation ProcessDocument7 pagesFinancial Forecasting in The Budget Preparation Processnmsusarla888No ratings yet
- Announcement2019 PDFDocument270 pagesAnnouncement2019 PDFHarsha VipinNo ratings yet
- Wiley GAAP for Governments 2012: Interpretation and Application of Generally Accepted Accounting Principles for State and Local GovernmentsFrom EverandWiley GAAP for Governments 2012: Interpretation and Application of Generally Accepted Accounting Principles for State and Local GovernmentsNo ratings yet
- Textbook of Urgent Care Management: Chapter 12, Pro Forma Financial StatementsFrom EverandTextbook of Urgent Care Management: Chapter 12, Pro Forma Financial StatementsNo ratings yet
- Audit Risk Alert: General Accounting and Auditing Developments, 2017/18From EverandAudit Risk Alert: General Accounting and Auditing Developments, 2017/18No ratings yet
- Implementing Results-Based Budget Management Frameworks: An Assessment of Progress in Selected CountriesFrom EverandImplementing Results-Based Budget Management Frameworks: An Assessment of Progress in Selected CountriesNo ratings yet
- OpTransactionHistory03 12 2019Document2 pagesOpTransactionHistory03 12 2019mamatha mamtaNo ratings yet
- This Is A System Generated Payslip and Does Not Require SignatureDocument1 pageThis Is A System Generated Payslip and Does Not Require Signaturemamatha mamtaNo ratings yet
- APCS494 - May 2020Document1 pageAPCS494 - May 2020mamatha mamtaNo ratings yet
- The 'S of CSW BillingDocument2 pagesThe 'S of CSW Billingmamatha mamtaNo ratings yet
- OpTransactionHistory26 01 2020Document2 pagesOpTransactionHistory26 01 2020mamatha mamtaNo ratings yet
- The Medicare Appeals Process: Five Levels To Protect Providers, Physicians, and Other SuppliersDocument3 pagesThe Medicare Appeals Process: Five Levels To Protect Providers, Physicians, and Other Suppliersmamatha mamtaNo ratings yet
- This Is A System Generated Payslip and Does Not Require SignatureDocument1 pageThis Is A System Generated Payslip and Does Not Require Signaturemamatha mamtaNo ratings yet
- Certificate For COVID-19 Vaccination: Beneficiary DetailsDocument1 pageCertificate For COVID-19 Vaccination: Beneficiary Detailsmamatha mamtaNo ratings yet
- This Is A System Generated Payslip and Does Not Require SignatureDocument1 pageThis Is A System Generated Payslip and Does Not Require Signaturemamatha mamtaNo ratings yet
- COVID-19 Vaccination Appointment Details: Center Preferred Time SlotDocument1 pageCOVID-19 Vaccination Appointment Details: Center Preferred Time Slotmamatha mamtaNo ratings yet
- July Operations Exempt Town Hall - FINALDocument31 pagesJuly Operations Exempt Town Hall - FINALmamatha mamtaNo ratings yet
- Dvanceceipt2021 07 10 13 46 46Document3 pagesDvanceceipt2021 07 10 13 46 46mamatha mamtaNo ratings yet
- 2022 US Holiday ScheduleDocument1 page2022 US Holiday Schedulemamatha mamtaNo ratings yet
- AdvanceReceipt2021 07 117 15Document6 pagesAdvanceReceipt2021 07 117 15mamatha mamtaNo ratings yet
- Certificate For COVID-19 Vaccination: Beneficiary DetailsDocument1 pageCertificate For COVID-19 Vaccination: Beneficiary Detailsmamatha mamtaNo ratings yet
- COVID-19 Vaccination Appointment Details: Center Date Time Preferred Time SlotDocument1 pageCOVID-19 Vaccination Appointment Details: Center Date Time Preferred Time Slotmamatha mamtaNo ratings yet
- Tax Invoice: Name Address State Gstin State Code Description AmountDocument1 pageTax Invoice: Name Address State Gstin State Code Description Amountmamatha mamtaNo ratings yet
- 2022 US Holiday ScheduleDocument1 page2022 US Holiday Schedulemamatha mamtaNo ratings yet
- D M E (DME) : Urable Edical QuipmentDocument30 pagesD M E (DME) : Urable Edical Quipmentmamatha mamtaNo ratings yet
- Laptop Policy - CernerDocument2 pagesLaptop Policy - Cernermamatha mamtaNo ratings yet
- Name: Manjushree G: B.E, Information Science and EngineeringDocument3 pagesName: Manjushree G: B.E, Information Science and Engineeringmamatha mamtaNo ratings yet
- Constipation:: Drug Therapy For Constipation & DiarroheaDocument8 pagesConstipation:: Drug Therapy For Constipation & DiarroheaDevi Prasanna 42.No ratings yet
- Generic Structure Language FeatureDocument11 pagesGeneric Structure Language FeatureAina NisaNo ratings yet
- BPT3 RD YearDocument17 pagesBPT3 RD YearKhushNo ratings yet
- Immune System AssignmentDocument2 pagesImmune System AssignmentZura KotaroNo ratings yet
- Intestinal Diseases in Cattle 2023Document30 pagesIntestinal Diseases in Cattle 2023Krystyna WędrychowskaNo ratings yet
- Aki To CKDDocument22 pagesAki To CKDSrinivas PingaliNo ratings yet
- Pathology of Nervous System2020Document33 pagesPathology of Nervous System2020AITUNRChoirul OktavianNo ratings yet
- Daftar Pustaka Bab IIDocument7 pagesDaftar Pustaka Bab IIWantoroNo ratings yet
- Curriculum Vitae: Education & Working ExperienceDocument2 pagesCurriculum Vitae: Education & Working Experienceapotek hegarNo ratings yet
- Wa0008.Document8 pagesWa0008.Dany MorBenNo ratings yet
- Pharmacology: Drugs Acting On The Endocrine SystemDocument20 pagesPharmacology: Drugs Acting On The Endocrine SystemShun Reigh SumilangNo ratings yet
- Thyroid Disorders Part I Hyperthyroidism Little 2006Document9 pagesThyroid Disorders Part I Hyperthyroidism Little 2006Jing XueNo ratings yet
- Factors Affecting The Activity of Health Caders in The Discovery of Tuberculosis Cases in Kelurahan Sonorejo SukoharjoDocument7 pagesFactors Affecting The Activity of Health Caders in The Discovery of Tuberculosis Cases in Kelurahan Sonorejo SukoharjoIntan AyuNo ratings yet
- Essay 3 BrionesDocument7 pagesEssay 3 Brionesapi-704703402No ratings yet
- AUVON AS8016 5languages Sms V1.0 211014 80x130mmDocument205 pagesAUVON AS8016 5languages Sms V1.0 211014 80x130mmjuanNo ratings yet
- Thesis Statement For Bipolar Disorder Research PaperDocument7 pagesThesis Statement For Bipolar Disorder Research Paperfvja66n5No ratings yet
- HSCP - A Brief History of Hepatitis CDocument8 pagesHSCP - A Brief History of Hepatitis CA WeaverNo ratings yet
- Basics of Knee Arthroscopy: For The BeginnersDocument40 pagesBasics of Knee Arthroscopy: For The BeginnersPedro Zambrano100% (1)
- DSM Comparison ChartDocument6 pagesDSM Comparison ChartAJ commsNo ratings yet
- NEBOSH Occupational Health Hazards by Terry RobsonDocument62 pagesNEBOSH Occupational Health Hazards by Terry RobsonAhsan HasanNo ratings yet
- Rough Draft Research Paper 11Document14 pagesRough Draft Research Paper 11api-549217680No ratings yet
- Case of TuberculosisDocument5 pagesCase of TuberculosisSheryhan Tahir BayleNo ratings yet
- Artificial Intelligence For Neurological Disorders Abraham Full ChapterDocument51 pagesArtificial Intelligence For Neurological Disorders Abraham Full Chapteralice.chao451100% (6)
- Clinically Relevant Complications Related To Pedicle Screw Placement in Thoracolumbar Surgery and Their ManagementDocument9 pagesClinically Relevant Complications Related To Pedicle Screw Placement in Thoracolumbar Surgery and Their ManagementjoshbakhNo ratings yet
- Trigger Finger-An Overview of The Treatment OptionsDocument5 pagesTrigger Finger-An Overview of The Treatment OptionsSatrya DitaNo ratings yet
- Adult Post-Cardiac Arrest Care Algorithm: o Co Io o CoDocument1 pageAdult Post-Cardiac Arrest Care Algorithm: o Co Io o CoKavya ShreeNo ratings yet
- Pemphigus Vegetans of Neumann: A Case Report of A Rare Variant of Pemphigus VulgarisDocument3 pagesPemphigus Vegetans of Neumann: A Case Report of A Rare Variant of Pemphigus VulgarisIJAR JOURNALNo ratings yet
- Introduction HmoleDocument32 pagesIntroduction HmoleBrian Montales BaggayanNo ratings yet
- MR-13 LampropoulosBLHealth2003Document19 pagesMR-13 LampropoulosBLHealth2003BillalNo ratings yet
- Herrero Vanrell2014Document17 pagesHerrero Vanrell2014Fer RodriguezNo ratings yet