Professional Documents
Culture Documents
0 ratings0% found this document useful (0 votes)
47 viewsPerioperative Fluid Management in Children
Perioperative Fluid Management in Children
Uploaded by
Rashmi SahaThis document discusses perioperative fluid management in children. It covers physiology differences between children and adults related to total body water content. It also discusses different types of intravenous fluids including crystalloids and colloids. Guidelines are provided for calculating maintenance fluids, correcting preoperative deficits, and replacing intraoperative losses in children. Factors like higher metabolic rate, body surface area to weight ratio, and respiratory rate contribute to higher fluid requirements in children. Careful attention to fluid intake and losses is needed due to their limited margin of error. Monitoring of fluid therapy includes clinical examination as well as invasive measures like central venous pressure. An example calculation is provided for determining fluid needs during a 1 hour hernia surgery in a 25kg child.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You might also like
- DNP Dosing GuideDocument3 pagesDNP Dosing GuideManu KolaganiNo ratings yet
- DETAILED LESSON PLAN IN SCIENCE5 Loida EmanoDocument7 pagesDETAILED LESSON PLAN IN SCIENCE5 Loida EmanoVergiel Abellano88% (16)
- Pathophysiology of FractureDocument2 pagesPathophysiology of FractureAnne Lorraine Bringas93% (27)
- Genitourinary RadiologyDocument53 pagesGenitourinary RadiologyAnna Dixon100% (2)
- Blood Gas Analysis Ppt-3Document32 pagesBlood Gas Analysis Ppt-3Kresna Dharma SuryanaNo ratings yet
- Introduction To PharmacologyDocument26 pagesIntroduction To PharmacologyKaye Cor100% (3)
- Addison's DiseaseDocument15 pagesAddison's DiseaseRonald A. Ogania50% (4)
- Perioperative Fluid Management in Pediatrics: By: Karim Kamal, MDDocument33 pagesPerioperative Fluid Management in Pediatrics: By: Karim Kamal, MDMohammed AKNo ratings yet
- A Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsNo ratings yet
- Fetal, Transition and Neonatal Circulation: Divya Mishra Dept of PediatricsDocument37 pagesFetal, Transition and Neonatal Circulation: Divya Mishra Dept of PediatricsMathan KarthikNo ratings yet
- Pre Eclampsia ManualDocument48 pagesPre Eclampsia ManualFilipa Pimenta de MatosNo ratings yet
- Drugs in ObstetricsDocument95 pagesDrugs in ObstetricsPriya jNo ratings yet
- Newborn Respiratory Distress 11.28.2011Document41 pagesNewborn Respiratory Distress 11.28.2011Emily EresumaNo ratings yet
- A Comparative Study of Phenylephrine, Ephedrine and Mephentermine For Maintainance of Arterial Pressure During Spinal Anaesthesia in Caesarean SectionDocument6 pagesA Comparative Study of Phenylephrine, Ephedrine and Mephentermine For Maintainance of Arterial Pressure During Spinal Anaesthesia in Caesarean SectionInternational Organization of Scientific Research (IOSR)No ratings yet
- Diabetic Ketoacidosis Care GuidelineDocument5 pagesDiabetic Ketoacidosis Care GuidelineRahma DhNo ratings yet
- Fulminant Hepatic FailureDocument12 pagesFulminant Hepatic Failureafghansyah arfiantoNo ratings yet
- Water and Electrolyte ImbalanceDocument17 pagesWater and Electrolyte Imbalancemhairat6043100% (1)
- Neonatal Transition: Training of The Trainers Neonatal ResuscitationDocument36 pagesNeonatal Transition: Training of The Trainers Neonatal ResuscitationmitaNo ratings yet
- Posterior Urethral ValveDocument6 pagesPosterior Urethral ValveMustafa AadanNo ratings yet
- Anesthesia For Tracheoesophageal Fistula RepairDocument29 pagesAnesthesia For Tracheoesophageal Fistula RepairArop AkechNo ratings yet
- Intravenous Fluid Therapy in Adults in The HospitalDocument28 pagesIntravenous Fluid Therapy in Adults in The Hospitalushapadminivadivelswamy100% (2)
- Hemodynamic MonitoringDocument4 pagesHemodynamic Monitoringgurneet kourNo ratings yet
- Management of Emergencies in ChildrenDocument39 pagesManagement of Emergencies in ChildrensastroboyzNo ratings yet
- A Neonate With Acute Kidney Injury: Case PresentationDocument4 pagesA Neonate With Acute Kidney Injury: Case PresentationSahil DhamijaNo ratings yet
- Principles of Fluid Therapy On The Basis ofDocument29 pagesPrinciples of Fluid Therapy On The Basis ofhendrytzNo ratings yet
- Transposition of Great ArteriesDocument21 pagesTransposition of Great ArteriesAlusio Navosailagi VUNIIVI100% (1)
- Medical Surgical Nursing Suretech College of NursingDocument18 pagesMedical Surgical Nursing Suretech College of NursingSanket TelangNo ratings yet
- ICU TriageDocument27 pagesICU TriageAkmal FahrezzyNo ratings yet
- Classification of Obstetric Shock Diagnosis and MonitoringDocument3 pagesClassification of Obstetric Shock Diagnosis and MonitoringAryo PraditoNo ratings yet
- BASIC LIFE SUPPORT Basics IntroductionDocument27 pagesBASIC LIFE SUPPORT Basics IntroductionMUKESH SUNDARARAJANNo ratings yet
- Medical EthicsDocument4 pagesMedical EthicsANBU DINESHNo ratings yet
- ColloidDocument74 pagesColloidParvathy R NairNo ratings yet
- Physiologic Transition From Intrauterine To Extrauterine Life - UpToDateDocument7 pagesPhysiologic Transition From Intrauterine To Extrauterine Life - UpToDateGuilherme Kazuo OgawaNo ratings yet
- 8.the Atls ProtocolDocument57 pages8.the Atls ProtocolReuben DutiNo ratings yet
- Acute Hemodialysis PrescriptionDocument13 pagesAcute Hemodialysis PrescriptionR DNo ratings yet
- Bronchiectasis: Dr.K.M.LakshmanarajanDocument238 pagesBronchiectasis: Dr.K.M.LakshmanarajanKM Lakshmana Rajan0% (1)
- AHA For PregnancyDocument77 pagesAHA For PregnancyAndrew TimantaNo ratings yet
- InsulinDocument33 pagesInsulinSheikNo ratings yet
- Critical Care Update PDFDocument25 pagesCritical Care Update PDFHugo PozoNo ratings yet
- Plasma P Here SisDocument13 pagesPlasma P Here SisSampath GoudNo ratings yet
- 12.intraoperative Fluid ManagmentDocument54 pages12.intraoperative Fluid ManagmentyeabsraNo ratings yet
- Hypertensive EmergenciesDocument56 pagesHypertensive EmergenciesAdekunle JosephNo ratings yet
- Management of Hypovolemic Shock FinalDocument13 pagesManagement of Hypovolemic Shock FinalDrGarikipati Krishna VenuNo ratings yet
- Sedation Guidelines, Protocols, and Algorithms In.13Document8 pagesSedation Guidelines, Protocols, and Algorithms In.13Juan Pedro Alconada MaglianoNo ratings yet
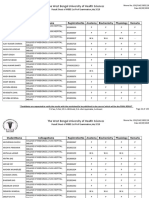
- The West Bengal University of Health SciencesDocument9 pagesThe West Bengal University of Health Sciencesbhaskar rayNo ratings yet
- Diagnosis of ShockDocument9 pagesDiagnosis of ShockRejina RavindranNo ratings yet
- Cad PamphletDocument2 pagesCad Pamphletapi-546509005No ratings yet
- Pediatric Newborn Medicine Clinical Practice GuidelinesDocument15 pagesPediatric Newborn Medicine Clinical Practice GuidelinesJosselle Sempio CalientaNo ratings yet
- Cardiopulmonary Cerebral ResuscitationDocument17 pagesCardiopulmonary Cerebral ResuscitationrizalNo ratings yet
- Mechanical Ventilation Practice Guidelines: 1. 2. Initial Settings - ModeDocument12 pagesMechanical Ventilation Practice Guidelines: 1. 2. Initial Settings - ModeGayathri RNo ratings yet
- 1 - Fetal Physiology and The Transition To Extrauterine LifeDocument13 pages1 - Fetal Physiology and The Transition To Extrauterine LifeRonaldo Pineda WieselbergNo ratings yet
- Initial Ventilator SettingsDocument22 pagesInitial Ventilator Settingsandi wija indrawanNo ratings yet
- Spinal Anaesthesia A Practical GuideDocument14 pagesSpinal Anaesthesia A Practical GuideNovita WulandariNo ratings yet
- Prognosis MGDocument7 pagesPrognosis MGPutri Cindy Claudia PandoyoNo ratings yet
- Abg Analysis and InterpretationDocument27 pagesAbg Analysis and InterpretationvaishnaviNo ratings yet
- 2020 ACHD For WebDocument108 pages2020 ACHD For WebRuslan RidcodubskiiNo ratings yet
- Ivc FilterDocument15 pagesIvc FilterashishNo ratings yet
- Hypovolemic ShockDocument25 pagesHypovolemic ShockManushi HenadeeraNo ratings yet
- Approach To Septic ShockDocument16 pagesApproach To Septic ShockRaja EllysyaNo ratings yet
- Cost EffectivenessDocument22 pagesCost EffectivenessEdalyn CapiliNo ratings yet
- Obstetric EmergenciesDocument15 pagesObstetric EmergenciesAndi SaputraNo ratings yet
- Sepsis Power Point Slide Presentation - The Guidelines - Implementation For The FutureDocument25 pagesSepsis Power Point Slide Presentation - The Guidelines - Implementation For The Futuremontie13No ratings yet
- Fetal ArrhythmiasDocument18 pagesFetal ArrhythmiasKarin Stefanny Muñoz CastilloNo ratings yet
- GIT Cirrhosis Liver in ChildrenDocument37 pagesGIT Cirrhosis Liver in ChildrenDr.P.NatarajanNo ratings yet
- Anem 2Document6 pagesAnem 2vamiqrasoolNo ratings yet
- Saponins and Their Potential Role in Diabetes MellitusDocument12 pagesSaponins and Their Potential Role in Diabetes MellitusArmenia Eka PutrianaNo ratings yet
- Last Min. PT2 Rev.Document22 pagesLast Min. PT2 Rev.sumedhasaha09No ratings yet
- Dispensary Investigation Details - Ramakrishna Math (Yogodyan)Document9 pagesDispensary Investigation Details - Ramakrishna Math (Yogodyan)HIMANSHU KUMAR CHOUDHARYNo ratings yet
- General Urine Examination (Urinalysis)Document24 pagesGeneral Urine Examination (Urinalysis)Ali RonaldoNo ratings yet
- Prattipati NIshant BRM RESREARCH PROJECTDocument12 pagesPrattipati NIshant BRM RESREARCH PROJECTPrattipati NishantNo ratings yet
- ES DX and TX Pituitary AIDocument26 pagesES DX and TX Pituitary AISybil Claudine LuyNo ratings yet
- Disease JaundiceDocument19 pagesDisease JaundiceMeena KoushalNo ratings yet
- Reproductive SystemDocument49 pagesReproductive SystemAyro Business CenterNo ratings yet
- Tapros - Leuprorelin Asetate - DKI9270700244A1 - 2015Document26 pagesTapros - Leuprorelin Asetate - DKI9270700244A1 - 2015Ananto PrasetyoNo ratings yet
- Digestive-SystemDocument93 pagesDigestive-SystemJulia Stefanel PerezNo ratings yet
- Gut Dysfunction and Non-Alcoholic Fatty Liver DiseaseDocument9 pagesGut Dysfunction and Non-Alcoholic Fatty Liver DiseaseAshwiniNo ratings yet
- Mithyantha2017 PDFDocument7 pagesMithyantha2017 PDFRifki Sanjaya PratamaNo ratings yet
- Chapter 12Document1 pageChapter 12Nona PeriarceNo ratings yet
- Cardiovascular Diseases and Risk Factors Among Diabetic Patients in Nablus District West Bank Palestine Case-Control StudyDocument155 pagesCardiovascular Diseases and Risk Factors Among Diabetic Patients in Nablus District West Bank Palestine Case-Control StudysaadNo ratings yet
- ACAD RESO 2020 01 DefermentDocument4 pagesACAD RESO 2020 01 DefermentJohn B BarbonioNo ratings yet
- How NAC and Glutathione Can Help To Heal Hashimoto's DiseaseDocument4 pagesHow NAC and Glutathione Can Help To Heal Hashimoto's Diseasemightyfever2973No ratings yet
- 10 - Monitoring Dan Evaluasi Enteral FormulaDocument23 pages10 - Monitoring Dan Evaluasi Enteral FormulaPaulinNo ratings yet
- Research Question: Does The Increasing Concentration of Natural Food Color Crocin (In Saffron)Document15 pagesResearch Question: Does The Increasing Concentration of Natural Food Color Crocin (In Saffron)RitikaFandaNo ratings yet
- Drug Used in Skin and Mucus MembraneDocument35 pagesDrug Used in Skin and Mucus MembraneMamta Yadav100% (1)
- Am J Clin Nutr 2007 85 4 967-71Document5 pagesAm J Clin Nutr 2007 85 4 967-71BALTAZAR OTTONELLONo ratings yet
- NCM 105 NotesDocument32 pagesNCM 105 NotesAubrey Justine GaleonNo ratings yet
- Thyroid GlandDocument59 pagesThyroid Glandbessan alfqeatNo ratings yet
- Diagnosis of Hyperthyroidism - UpToDateDocument24 pagesDiagnosis of Hyperthyroidism - UpToDateEfrain Coral PantojaNo ratings yet
Perioperative Fluid Management in Children
Perioperative Fluid Management in Children
Uploaded by
Rashmi Saha0 ratings0% found this document useful (0 votes)
47 views31 pagesThis document discusses perioperative fluid management in children. It covers physiology differences between children and adults related to total body water content. It also discusses different types of intravenous fluids including crystalloids and colloids. Guidelines are provided for calculating maintenance fluids, correcting preoperative deficits, and replacing intraoperative losses in children. Factors like higher metabolic rate, body surface area to weight ratio, and respiratory rate contribute to higher fluid requirements in children. Careful attention to fluid intake and losses is needed due to their limited margin of error. Monitoring of fluid therapy includes clinical examination as well as invasive measures like central venous pressure. An example calculation is provided for determining fluid needs during a 1 hour hernia surgery in a 25kg child.
Original Description:
Details discussion about preoperative fluid management in children
Original Title
perioperative fluid management in children-converted
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThis document discusses perioperative fluid management in children. It covers physiology differences between children and adults related to total body water content. It also discusses different types of intravenous fluids including crystalloids and colloids. Guidelines are provided for calculating maintenance fluids, correcting preoperative deficits, and replacing intraoperative losses in children. Factors like higher metabolic rate, body surface area to weight ratio, and respiratory rate contribute to higher fluid requirements in children. Careful attention to fluid intake and losses is needed due to their limited margin of error. Monitoring of fluid therapy includes clinical examination as well as invasive measures like central venous pressure. An example calculation is provided for determining fluid needs during a 1 hour hernia surgery in a 25kg child.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
0 ratings0% found this document useful (0 votes)
47 views31 pagesPerioperative Fluid Management in Children
Perioperative Fluid Management in Children
Uploaded by
Rashmi SahaThis document discusses perioperative fluid management in children. It covers physiology differences between children and adults related to total body water content. It also discusses different types of intravenous fluids including crystalloids and colloids. Guidelines are provided for calculating maintenance fluids, correcting preoperative deficits, and replacing intraoperative losses in children. Factors like higher metabolic rate, body surface area to weight ratio, and respiratory rate contribute to higher fluid requirements in children. Careful attention to fluid intake and losses is needed due to their limited margin of error. Monitoring of fluid therapy includes clinical examination as well as invasive measures like central venous pressure. An example calculation is provided for determining fluid needs during a 1 hour hernia surgery in a 25kg child.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
You are on page 1of 31
PERIOPERATIVE FLUID
MANAGEMENT IN CHILDREN
Presented By: Dr. Sourav Saha
(1st year PGT)
Moderated By: Dr. Ranjit Reang
(Asst. Proff)
Physiology:
Water is the most abundent single constituent of the
body.
Water accounts for about 60% of the weight in an
adult man and about 50% of the body weight in an
adult woman.
The difference is due to increased body fat reflecting
decreased water content in adipose tissue.
Body fluid are divided into intracellular and extracellular
compartments.
Approximately two-third of TBW constitute intracellular
fluid.
Rest one-third is extracellular fluid.
Extracellular fluid id divided into interstitial fluid and
intravascular fluid.
Most of the intestitial fluid is held in gel structure in
between the cells. Others are CSF, gastroistestinal fluid
and fluid in potential space(pleural fluid, pericardial fluid,
peritoneal fluid, synovial fluid)
Fluid physiology difference between adult
and children:
TBW is different in children from adult.
Total body water content changes drastically from
before birth until one year of age.
At 24 weeks gestational age, a baby’s total body
water content is close to 80% of total body weight.
This slowly decreases due to gradual increase in fat
and muscle mass until the child is around one year of
age, when total body water content is about 60% of
total body weight.
In addition to total body water differences, the
percent of body weight accounted for intracellular
and extracellular water also changes.
Newborn babies have more extracellular water—
45% of total body weight—compared with only 35%
of total body weight that is intracellular water.
These changes in total body fluid have important
implications for drug therapy, particularly for water
soluble drugs.
Drugs generally distribute into the
extracellular space, thus the larger
extracellular component of fluid in neonates
also contributes to the need for larger doses.
Different intravenous fluids:
Crystalloids:
1. They are aqueous solution of ion with or without
glucose considered as the initial resusitating fluid in
patients.
2. Mostly intraoperative fluids are isotonic crystaloid
solution like NS orbalanced electrolyte solution like
lactated ringer solution or plasmalyte.
3. NS in large volume can cause hyperchloramic metabolic
acidosis due to high Cl- content & lack of bicarbonate &
may lead to perioperative acute kidney injury.
4. An addition of 1–2.5% glucose in order to avoid
hypoglycaemia.
5. Many a time, neonates and infants present to
operating room with various paediatric solution
infusions (Isolyte P, D5%+ NS0.45%., etc.)
6. Their advantages include low cost, lack of effect on
coagulation, no risk of anaphylactic reaction and no
risk of transmission of any known or unknown
infectious agent.
Colloids:
1. They are osmotically active high molecular weight
substance.
2. Their intravascular half life is 3-6 hrs.
3. They are used in severe intravascular fluid deficit or
severe hypoproteinaemia.
4. They are derived from either plasma protein or
synthatic glucose polymer supplied in isotonic
electrolyte solution.
5. Synthetic colloids are gelatin or dextrose starch.
6. Gelatin are associated with histamine mediated
allergic reactions.
7. Albumin occurs naturally and is regarded as the
colloid “gold standard.” An albumin 5% solution is
osmotically equivalent to an equal volume of plasma,
whereas a 25% solution causes intravascular volume
expansion 3–5 times because of fluid translocation
from the interstitial compartment.
Intraoperative fluid therapy in children:
Pediatric patients have higher fluid requirement than
adults.
There are multiple reasons behind this-
1)First, the higher metabolic rate of children
requires a greater caloric expenditure, which
translates into higher fluid requirements.
2) Secondly, children, especially infants, have a much
higher body surface area to weight ratio, and this
translates into relatively more water loss from skin
compared with adults.
3) In addition, children, especially infants, have higher
respiratory rates, and this equates to higher
insensible losses from the respiratory tract.
4) Congenital abdominal wall defects such as
omphalocele and gastroschisis can lead to higher
evaporative losses before surgical correction, and
thus careful attention should be paid to fluid and
electrolyte balance.
So, meticulous attention to fluid intake and loss is
required in pediatric patient because they have
limited margin of error.
Fluid therapy can be divided into:-
a) maintainance
b) deficit correction
c) loss replacement
a) Maintainance:-
The basis for calculating maintainance fluid derived
from by Holliday and Segar.
They found that daily fluid requirements directly
depend on metabolic demand- specifically, that 100
ml of water is required for 100 cal of expanded
energy.
Relating this to weight produces hourly fluid
requirement of-
1) 4 ml/kg/hr upto 10 kg
2) 2ml/kg/hr for next 10 kg.
3) 1 ml/kg/hr above 20 kg.
A solution such as D5 + ½ NS with 20 mEq/L of
potassium chloride is preferable.
D5 + ¼ NS may be a better choice in neonates because
of their limited ability to handle sodium loads.
Children below 8 years require 6 mg/kg/min to maintain
euglycaemia and premature neonates require 6-8
mg/kg/min.
The original Holliday and Segar formula would be
problematic for children with acute illness or
signicant renal or cardiac dysfunction.
So, it is recommended to administer 20-40 ml/kg of
balanced salt solution during the course of the
anaesthesia. Postoperative fluid management should
be reduced to 2, 1, 0.5 rule with isotonic fluid. If after
12 hrs the child is unable to convert to oral intake,
than a standerd hypotonic solution is initiated at the
4-2-1 rule rate to avoid hypernatremia.
b) Deficit correction:
In addition to maintainance, any preoperative fluid
deficits must be replaced.
As a result of the fasting state, children are presumed
to develop preoperative fluid deficits secondary to
continuing insensible losses and urine output.
Preoperative fluid deficit administered with hourly
maintainance in a ratio of 50% in first hour and 25%
in second and third hour.
It is done with balanced salt slution. Glucose in
omitted to avoid hypoglycaemia.
Fasting guidelines for children:
Following fasting and sensible fluid loss child may
develop dehydration.
Estimation of degree of preoperative dehydration is
based on classical clinical signs.
The most important sign of normal hydration status
is kidney function. Thus, monitoring of urinary output
is essential for evaluating and treating any fluid
deficit.
Correction of 1% of dehydration requires about 10
ml/kg of fluids.
Rate of fluid administration depends on seriousness
and on rapidity of dehydration.
Clinical assessment for degree of
dehydration:
c) Loss replacement:
Blood loss:
a)It can be easily measured by amount of blood
collected in suction jar, guazes used and amount of
irrigation fluid used. A fully soaked (45×45cm) guaze
contains about 120-150 ml of blood.
b) For calculation of loss replacement, we need to
know Maximal Allowable Blood Loss(MABL) for a
child.
MABL= EBV ×{(starting hematocrit-target
hematocrit)÷starting hematocrit}
-EBV:- Estimated blood volume
-MABL would be replaced by 3 ml RL per ml of
blood loss or 1 ml colloid per ml of blood loss.
c) If blood loss is equal to or less than MABL, then no
need of blood transfusion.
d) If the child has reached the MABL and significant
more blood loss is expected during surgery, then
PRBC has to be transfused to make hematocrit in
20% to 25%.
Volume of PRBC to be transfused=
{(desired HCT-present HCT)×EBV}÷HCT of
PRBC(60%)
Third space loss:- they could not be measured
accurately. So they are replanished according to
surgical procedure like
a) minor procedure like herniotomy- 1 ml/kg/hr
b)major procedures like surgical repair of
gastroschisis- 15 ml/kg/hr
Monitoring of Fluid therapy:-
In pediatric patients monitering of fluid therapy is
very important as they have limited margin of error.
Clinical examination is the most imp measure, for
example-
a) Weight of the child
b) Urine output
c) periorbital edema
d) Bl Basal crepts in both lungs
For example:
A child of 25kg will be undergoing herniotomy. He
is on 6 hr fasting without any signs of dehydration.
Surgery expected to last for 1 hr with minimal
blood loss.
So maintainace fluid is 65 ml/hr
Deficit is (65×6)= 390 ml, out of which 195 ml to
be transfused in 1 hr rest in next 2 hr.
Loss replacement is 25ml/hr
So, during 1 hr of operation about 285 ml fluid to
be transfused.
Other invasive measures like:-
a) Central Venous pressure
b) Pulmonary artery pressure monitering
Non invasive fluid therapy guidence by arterial pulse
contour analysis and estimation of stroke volume by
using:-
a) Esophageal doppler
b) Transesophageal echocardiography
c) Transthoracic echocardiography.
Thank You
Next Topic:- Death in operation table-
How to resolve?
Date:22/11/19
presenter- Dr. Tapan Debbarma.
You might also like
- DNP Dosing GuideDocument3 pagesDNP Dosing GuideManu KolaganiNo ratings yet
- DETAILED LESSON PLAN IN SCIENCE5 Loida EmanoDocument7 pagesDETAILED LESSON PLAN IN SCIENCE5 Loida EmanoVergiel Abellano88% (16)
- Pathophysiology of FractureDocument2 pagesPathophysiology of FractureAnne Lorraine Bringas93% (27)
- Genitourinary RadiologyDocument53 pagesGenitourinary RadiologyAnna Dixon100% (2)
- Blood Gas Analysis Ppt-3Document32 pagesBlood Gas Analysis Ppt-3Kresna Dharma SuryanaNo ratings yet
- Introduction To PharmacologyDocument26 pagesIntroduction To PharmacologyKaye Cor100% (3)
- Addison's DiseaseDocument15 pagesAddison's DiseaseRonald A. Ogania50% (4)
- Perioperative Fluid Management in Pediatrics: By: Karim Kamal, MDDocument33 pagesPerioperative Fluid Management in Pediatrics: By: Karim Kamal, MDMohammed AKNo ratings yet
- A Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsNo ratings yet
- Fetal, Transition and Neonatal Circulation: Divya Mishra Dept of PediatricsDocument37 pagesFetal, Transition and Neonatal Circulation: Divya Mishra Dept of PediatricsMathan KarthikNo ratings yet
- Pre Eclampsia ManualDocument48 pagesPre Eclampsia ManualFilipa Pimenta de MatosNo ratings yet
- Drugs in ObstetricsDocument95 pagesDrugs in ObstetricsPriya jNo ratings yet
- Newborn Respiratory Distress 11.28.2011Document41 pagesNewborn Respiratory Distress 11.28.2011Emily EresumaNo ratings yet
- A Comparative Study of Phenylephrine, Ephedrine and Mephentermine For Maintainance of Arterial Pressure During Spinal Anaesthesia in Caesarean SectionDocument6 pagesA Comparative Study of Phenylephrine, Ephedrine and Mephentermine For Maintainance of Arterial Pressure During Spinal Anaesthesia in Caesarean SectionInternational Organization of Scientific Research (IOSR)No ratings yet
- Diabetic Ketoacidosis Care GuidelineDocument5 pagesDiabetic Ketoacidosis Care GuidelineRahma DhNo ratings yet
- Fulminant Hepatic FailureDocument12 pagesFulminant Hepatic Failureafghansyah arfiantoNo ratings yet
- Water and Electrolyte ImbalanceDocument17 pagesWater and Electrolyte Imbalancemhairat6043100% (1)
- Neonatal Transition: Training of The Trainers Neonatal ResuscitationDocument36 pagesNeonatal Transition: Training of The Trainers Neonatal ResuscitationmitaNo ratings yet
- Posterior Urethral ValveDocument6 pagesPosterior Urethral ValveMustafa AadanNo ratings yet
- Anesthesia For Tracheoesophageal Fistula RepairDocument29 pagesAnesthesia For Tracheoesophageal Fistula RepairArop AkechNo ratings yet
- Intravenous Fluid Therapy in Adults in The HospitalDocument28 pagesIntravenous Fluid Therapy in Adults in The Hospitalushapadminivadivelswamy100% (2)
- Hemodynamic MonitoringDocument4 pagesHemodynamic Monitoringgurneet kourNo ratings yet
- Management of Emergencies in ChildrenDocument39 pagesManagement of Emergencies in ChildrensastroboyzNo ratings yet
- A Neonate With Acute Kidney Injury: Case PresentationDocument4 pagesA Neonate With Acute Kidney Injury: Case PresentationSahil DhamijaNo ratings yet
- Principles of Fluid Therapy On The Basis ofDocument29 pagesPrinciples of Fluid Therapy On The Basis ofhendrytzNo ratings yet
- Transposition of Great ArteriesDocument21 pagesTransposition of Great ArteriesAlusio Navosailagi VUNIIVI100% (1)
- Medical Surgical Nursing Suretech College of NursingDocument18 pagesMedical Surgical Nursing Suretech College of NursingSanket TelangNo ratings yet
- ICU TriageDocument27 pagesICU TriageAkmal FahrezzyNo ratings yet
- Classification of Obstetric Shock Diagnosis and MonitoringDocument3 pagesClassification of Obstetric Shock Diagnosis and MonitoringAryo PraditoNo ratings yet
- BASIC LIFE SUPPORT Basics IntroductionDocument27 pagesBASIC LIFE SUPPORT Basics IntroductionMUKESH SUNDARARAJANNo ratings yet
- Medical EthicsDocument4 pagesMedical EthicsANBU DINESHNo ratings yet
- ColloidDocument74 pagesColloidParvathy R NairNo ratings yet
- Physiologic Transition From Intrauterine To Extrauterine Life - UpToDateDocument7 pagesPhysiologic Transition From Intrauterine To Extrauterine Life - UpToDateGuilherme Kazuo OgawaNo ratings yet
- 8.the Atls ProtocolDocument57 pages8.the Atls ProtocolReuben DutiNo ratings yet
- Acute Hemodialysis PrescriptionDocument13 pagesAcute Hemodialysis PrescriptionR DNo ratings yet
- Bronchiectasis: Dr.K.M.LakshmanarajanDocument238 pagesBronchiectasis: Dr.K.M.LakshmanarajanKM Lakshmana Rajan0% (1)
- AHA For PregnancyDocument77 pagesAHA For PregnancyAndrew TimantaNo ratings yet
- InsulinDocument33 pagesInsulinSheikNo ratings yet
- Critical Care Update PDFDocument25 pagesCritical Care Update PDFHugo PozoNo ratings yet
- Plasma P Here SisDocument13 pagesPlasma P Here SisSampath GoudNo ratings yet
- 12.intraoperative Fluid ManagmentDocument54 pages12.intraoperative Fluid ManagmentyeabsraNo ratings yet
- Hypertensive EmergenciesDocument56 pagesHypertensive EmergenciesAdekunle JosephNo ratings yet
- Management of Hypovolemic Shock FinalDocument13 pagesManagement of Hypovolemic Shock FinalDrGarikipati Krishna VenuNo ratings yet
- Sedation Guidelines, Protocols, and Algorithms In.13Document8 pagesSedation Guidelines, Protocols, and Algorithms In.13Juan Pedro Alconada MaglianoNo ratings yet
- The West Bengal University of Health SciencesDocument9 pagesThe West Bengal University of Health Sciencesbhaskar rayNo ratings yet
- Diagnosis of ShockDocument9 pagesDiagnosis of ShockRejina RavindranNo ratings yet
- Cad PamphletDocument2 pagesCad Pamphletapi-546509005No ratings yet
- Pediatric Newborn Medicine Clinical Practice GuidelinesDocument15 pagesPediatric Newborn Medicine Clinical Practice GuidelinesJosselle Sempio CalientaNo ratings yet
- Cardiopulmonary Cerebral ResuscitationDocument17 pagesCardiopulmonary Cerebral ResuscitationrizalNo ratings yet
- Mechanical Ventilation Practice Guidelines: 1. 2. Initial Settings - ModeDocument12 pagesMechanical Ventilation Practice Guidelines: 1. 2. Initial Settings - ModeGayathri RNo ratings yet
- 1 - Fetal Physiology and The Transition To Extrauterine LifeDocument13 pages1 - Fetal Physiology and The Transition To Extrauterine LifeRonaldo Pineda WieselbergNo ratings yet
- Initial Ventilator SettingsDocument22 pagesInitial Ventilator Settingsandi wija indrawanNo ratings yet
- Spinal Anaesthesia A Practical GuideDocument14 pagesSpinal Anaesthesia A Practical GuideNovita WulandariNo ratings yet
- Prognosis MGDocument7 pagesPrognosis MGPutri Cindy Claudia PandoyoNo ratings yet
- Abg Analysis and InterpretationDocument27 pagesAbg Analysis and InterpretationvaishnaviNo ratings yet
- 2020 ACHD For WebDocument108 pages2020 ACHD For WebRuslan RidcodubskiiNo ratings yet
- Ivc FilterDocument15 pagesIvc FilterashishNo ratings yet
- Hypovolemic ShockDocument25 pagesHypovolemic ShockManushi HenadeeraNo ratings yet
- Approach To Septic ShockDocument16 pagesApproach To Septic ShockRaja EllysyaNo ratings yet
- Cost EffectivenessDocument22 pagesCost EffectivenessEdalyn CapiliNo ratings yet
- Obstetric EmergenciesDocument15 pagesObstetric EmergenciesAndi SaputraNo ratings yet
- Sepsis Power Point Slide Presentation - The Guidelines - Implementation For The FutureDocument25 pagesSepsis Power Point Slide Presentation - The Guidelines - Implementation For The Futuremontie13No ratings yet
- Fetal ArrhythmiasDocument18 pagesFetal ArrhythmiasKarin Stefanny Muñoz CastilloNo ratings yet
- GIT Cirrhosis Liver in ChildrenDocument37 pagesGIT Cirrhosis Liver in ChildrenDr.P.NatarajanNo ratings yet
- Anem 2Document6 pagesAnem 2vamiqrasoolNo ratings yet
- Saponins and Their Potential Role in Diabetes MellitusDocument12 pagesSaponins and Their Potential Role in Diabetes MellitusArmenia Eka PutrianaNo ratings yet
- Last Min. PT2 Rev.Document22 pagesLast Min. PT2 Rev.sumedhasaha09No ratings yet
- Dispensary Investigation Details - Ramakrishna Math (Yogodyan)Document9 pagesDispensary Investigation Details - Ramakrishna Math (Yogodyan)HIMANSHU KUMAR CHOUDHARYNo ratings yet
- General Urine Examination (Urinalysis)Document24 pagesGeneral Urine Examination (Urinalysis)Ali RonaldoNo ratings yet
- Prattipati NIshant BRM RESREARCH PROJECTDocument12 pagesPrattipati NIshant BRM RESREARCH PROJECTPrattipati NishantNo ratings yet
- ES DX and TX Pituitary AIDocument26 pagesES DX and TX Pituitary AISybil Claudine LuyNo ratings yet
- Disease JaundiceDocument19 pagesDisease JaundiceMeena KoushalNo ratings yet
- Reproductive SystemDocument49 pagesReproductive SystemAyro Business CenterNo ratings yet
- Tapros - Leuprorelin Asetate - DKI9270700244A1 - 2015Document26 pagesTapros - Leuprorelin Asetate - DKI9270700244A1 - 2015Ananto PrasetyoNo ratings yet
- Digestive-SystemDocument93 pagesDigestive-SystemJulia Stefanel PerezNo ratings yet
- Gut Dysfunction and Non-Alcoholic Fatty Liver DiseaseDocument9 pagesGut Dysfunction and Non-Alcoholic Fatty Liver DiseaseAshwiniNo ratings yet
- Mithyantha2017 PDFDocument7 pagesMithyantha2017 PDFRifki Sanjaya PratamaNo ratings yet
- Chapter 12Document1 pageChapter 12Nona PeriarceNo ratings yet
- Cardiovascular Diseases and Risk Factors Among Diabetic Patients in Nablus District West Bank Palestine Case-Control StudyDocument155 pagesCardiovascular Diseases and Risk Factors Among Diabetic Patients in Nablus District West Bank Palestine Case-Control StudysaadNo ratings yet
- ACAD RESO 2020 01 DefermentDocument4 pagesACAD RESO 2020 01 DefermentJohn B BarbonioNo ratings yet
- How NAC and Glutathione Can Help To Heal Hashimoto's DiseaseDocument4 pagesHow NAC and Glutathione Can Help To Heal Hashimoto's Diseasemightyfever2973No ratings yet
- 10 - Monitoring Dan Evaluasi Enteral FormulaDocument23 pages10 - Monitoring Dan Evaluasi Enteral FormulaPaulinNo ratings yet
- Research Question: Does The Increasing Concentration of Natural Food Color Crocin (In Saffron)Document15 pagesResearch Question: Does The Increasing Concentration of Natural Food Color Crocin (In Saffron)RitikaFandaNo ratings yet
- Drug Used in Skin and Mucus MembraneDocument35 pagesDrug Used in Skin and Mucus MembraneMamta Yadav100% (1)
- Am J Clin Nutr 2007 85 4 967-71Document5 pagesAm J Clin Nutr 2007 85 4 967-71BALTAZAR OTTONELLONo ratings yet
- NCM 105 NotesDocument32 pagesNCM 105 NotesAubrey Justine GaleonNo ratings yet
- Thyroid GlandDocument59 pagesThyroid Glandbessan alfqeatNo ratings yet
- Diagnosis of Hyperthyroidism - UpToDateDocument24 pagesDiagnosis of Hyperthyroidism - UpToDateEfrain Coral PantojaNo ratings yet