Professional Documents
Culture Documents
Telemedicine and Orthopaedic Surgery: The COVID-19 Pandemic and Our New Normal
Telemedicine and Orthopaedic Surgery: The COVID-19 Pandemic and Our New Normal
Uploaded by
Alecjohn FortoOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Telemedicine and Orthopaedic Surgery: The COVID-19 Pandemic and Our New Normal
Telemedicine and Orthopaedic Surgery: The COVID-19 Pandemic and Our New Normal
Uploaded by
Alecjohn FortoCopyright:
Available Formats
|
Telemedicine and Orthopaedic Surgery
The COVID-19 Pandemic and Our New Normal
Nathan S. Lanham, MD Abstract
» Telemedicine can serve as a medium for patient evaluation,
Kyle J. Bockelman, DO
monitoring, and interpretation of diagnostic imaging and other tests.
Brendan J. McCriskin, MD
» Advantages of telemedicine include improved access to care, cost-
Downloaded from http://journals.lww.com/jbjsreviews by BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AWnYQp/IlQrHD3i3D0OdRyi7TvSFl4Cf3VC4/OAVpDDa8KKGKV0Ymy+78= on 01/19/2021
effectiveness, and efficiency.
Investigation performed at Martin
» Challenges remain regarding more widespread adoption of tele-
Army Community Hospital, Fort
Benning, Georgia medicine and involve reimbursement as well as regulatory support.
» The coronavirus disease 2019 (COVID-19) pandemic has led to a
paradigm shift in telemedicine that is here to stay.
» Patient satisfaction is a key component of telemedicine and will drive
its evolution.
O
ver the past several decades, and negative findings in the literature per-
there has been a rapid taining to telemedicine and orthopaedic
emergence of technological surgery, and provide a few pragmatic steps
advances that have facili- that can be taken to begin implementing
tated health-care delivery at a distance1. telemedicine in a practice.
Multiple forms of telemedicine have
enabled providers to evaluate patients, Defining Telemedicine
monitor follow-up, and interpret diagnos- Telemedicine has been defined as patient
tic imaging and other tests. This has led to care that is provided at a distance using
improved access to care, cost-effectiveness, information technology, including cell
and efficiency. The coronavirus disease phones, computers, or other electronic
2019 (COVID-19) pandemic and the devices1. The U.S. Centers for Medicare &
response that it has engendered have dis- Medicaid Services (CMS) defines tele-
rupted health-care systems around the medicine, or telehealth and related terms, as
world. Initiatives such as telemedicine have the exchange of medical information from
been encouraged and employed in order to 1 site to another through electronic com-
limit this disruption and combat the spread munication to improve a patient’s health.
of COVID-192. This electronic communication must
Orthopaedic surgery is a dynamic include an audio and a video component
multifaceted specialty that is high-volume in order to be considered a telehealth
and technology-dependent. Therefore, encounter by CMS. More broadly, the
efforts to improve efficiency and leverage World Health Organization (WHO)
technology through telemedicine could defines telemedicine as the delivery of
benefit patients and providers in the field of health-care services at a distance, using
Written work prepared by employees of the orthopaedic surgery under any circum- electronic means for the diagnosis, the
Federal Government as part of their official stances. This review article is intended to treatment, and the prevention of disease
duties is, under the United States Copyright
define and provide a framework for tele- and injury, as well as for research and eval-
Act, a ‘work of the United States Government’
forwhichcopyrightprotectionunderthatActis medicine classification, summarize positive uation and the education of health-care
not available. As such, copyright protection
does not extend to the contributions of Disclosure: The authors indicated that no external funding was received for any aspect of this work.
employees of the Federal Government The Disclosure of Potential Conflicts of Interest forms are provided with the online version of the
prepared as part of their employment. article (http://links.lww.com/JBJSREV/A621).
JBJS REVIEWS 2020;8(7):e20.00083 · http://dx.doi.org/10.2106/JBJS.RVW.20.00083 1
| Te l e m e d i c i n e a n d O r t h o p a e d i c S u r g e r y
providers in order to improve the health reported when the billing practice has an phone on their electronic device are
of their patients1. established relationship with the patient. functioning appropriately prior to the
The patient must generate the initial encounter. Specific tools that can aid
Classification inquiry, and communication can occur virtual physical examination include
Telemedicine may be classified accord- over a 7-day period. This 7-day period web-based goniometers, which have
ing to the nature of the interaction and may involve multiple messages between been noted to be compatible with most
the type of information that is being the patient and the provider and is billed telemedicine applications7. In addition,
transmitted3. Synchronous and asyn- according to the amount of time that is some physical examination tests that
chronous telemedicine are the 2 major required to satisfy the patient’s inquiry5. require manual resistance can be simu-
classifications that characterize tele- lated by having the patient grasp an
medicine as it relates to the timing of the Telemedicine Encounters object of a known size and weight.
provider-patient interaction. Synchro- Prior to the initiation of a telemedicine Additional evaluation of strength and
nous telemedicine, often called real-time encounter, the staff or the provider neurologic status can be achieved with
telemedicine, employs videoconferenc- should inform and educate the patient patient-demonstrated activities, such as
ing and other technologies to facilitate about the nature of the telemedicine having patients sit back in a chair and
provider-patient interaction. Asynchro- service compared with in-person care. then rise without using their arms for
nous telemedicine, often called store- This information can be presented in assistance. In the absence of provocative
and-forward telemedicine, involves writing or verbally and should include a testing, discrete palpation, and stability
generating images or data and trans- discussion of record-keeping, schedul- testing, some authors have advocated for
mitting them electronically for later ing, privacy and security, potential risks, increased utilization of advanced imag-
review4. mandatory reporting, follow-up, and ing studies such as magnetic resonance
The CMS recognizes 3 types of contingencies if the encounter is dis- imaging (MRI)7.
telemedicine services that can be pro- rupted6. Each of these items may be Following each patient encounter,
vided to patients: telehealth visits, vir- included in an all-encompassing documentation should be provided and
tual check-ins, and electronic (E)-visits. waiver consent form that may be maintained in a secure Health Insurance
Telehealth visits are considered virtual electronically signed. Most impor- Portability and Accountability Act
encounters between the provider and tantly, patient-specific concerns about (HIPAA)-compliant form and location.
the patient for services that usually occur the telemedicine encounter should be This includes assessment and discussion
in-person at a clinic or a hospital. The addressed accordingly. with the patient about pertinent diag-
provider must use an interactive audio The patient encounter should nostic tests, imaging or laboratory
and video telecommunications system reflect the level of assessment that is results, and treatment options6.
that permits real-time communication required to manage a patient, taking into
between the distant site and the patient consideration the information that can Advantages
at home for the encounter to be recog- be elicited remotely. Audio-based eval- The purported advantages of tele-
nized and reimbursed as a telehealth uation may be used solely for consulta- medicine include cost-effectiveness,
visit5. tion if the evaluation, the diagnosis, and improved access to care, patient satis-
The CMS also reimburses virtual the treatment can be reliably made with faction, and efficiency. Buvik et al.
check-ins, or brief communications a complete medical history and is con- performed an economic evaluation
with technology-based services, which sistent with established standards of care based on a randomized controlled trial
allow for patients to communicate with and state and federal laws and regula- of 389 patients who had been referred
their providers and avoid unnecessary tions, especially as they relate to the for an orthopaedic outpatient consul-
trips to their provider’s office or hospital. prescribing of medications. tation8. One group was randomized to
These virtual check-ins are intended for Preparing and standardizing the receive a video-assisted remote con-
patients who have an established rela- conditions of the virtual physical exam- sultation, while the control group
tionship with a provider and when the ination can help to optimize the quality received standard care with an outpa-
communication is not related to a and efficiency of the telemedicine tient consultation at the hospital. The
medical visit that has occurred within encounter. As part of this preparation, remote consultation involved trained
the previous 7 days and does not lead to a patients can be sent a pre-encounter nurses who set up the videoconfer-
medical visit within the next 24 hours5. checklist containing certain positives encing at the remote site. The nurses
Lastly, established patients may and negatives that are relevant to the assisted during the consultation and
have non-face-to-face patient-initiated chief concern, in addition to diagrams performed physical tasks, such as
communications, or E-visits, with their for the localization of pain and sensory changing casts or removing stitches.
providers by using online patient por- abnormalities. Patients also should Digital radiographs also were made at
tals. This E-visit service only can be confirm that the camera and the micro- the remote sites if needed and were
2 JULY 2020 · VOLUME 8, ISSUE 7 · e 20.00083
Te l e m e d i c i n e a n d O r t h o p a e d i c S u r g e r y |
shown to patients during consulta- patient and the provider were approxi- decrease patient wait times for clinical
tions with the orthopaedic provider to mately 240 km apart13. Two-thirds of evaluation. Clegg et al. found that real-
help inform patients about their the patients who were evaluated with time telemedicine reduced the wait time
pathology. The authors found that the videoconferencing were afforded defin- for wound-care consultations in rural
video-assisted orthopaedic consulta- itive treatment, and the videoconfer- locations from 48 hours to ,24 hours
tions were cost-effective provided that encing obviated the need for these when compared with in-person consul-
the number of consultations per- patients to travel for an in-person tations18. Another study found that tel-
formed per year was .1838. Another appointment13. A randomized trial eradiology for remote orthopaedic
study evaluating cost data obtained comparing telemedicine with standard consultation diminished the need for in-
from a randomized controlled trial outpatient appointments found that hospital consultation and reduced the
showed that telemedicine was less patients in the telemedicine group were average time for decision-making by
costly than conventional care if the offered a follow-up appointment more more than half19.
number of evaluated patients was .80 often. In addition, telemedicine led to Gamus et al. evaluated the remote
per year; however, if the distance to fewer tests being ordered and increased care of lower-extremity ulcers over a
specialist care was reduced from patient satisfaction when compared with 12-month period and compared tele-
160 km to 80 km, the number of standard outpatient consultation14. medicine with face-to-face consulta-
patients needed in order to realize Buvik et al. performed a randomized tions20. The telemedicine evaluation
the same cost benefit increased to controlled trial comparing video-assisted was performed with synchronous vid-
approximately 200 per year9. remote orthopaedic consultations and eoconferencing, and a nurse-assisted
Harno et al. prospectively evalu- standard outpatient consultations in an setting was implemented during all
ated the costs of videoconferencing and orthopaedic clinic for patients living in treatment sessions for both groups. No
outpatient clinic appointments for 225 remote locations15. The telemedicine difference in healing was found between
patients who had been referred to consultations were rated as “good” or “very the groups, and the telemedicine group
orthopaedic surgeons and found that the good” in 98% of cases and were found to had a substantially reduced number of
use of telemedicine reduced direct costs be non-inferior to the standard in-person visits (4.36) when compared with those
by 45% and was cost-effective10. In evaluations15. who had face-to-face care (6.32)20.
another study, first-time telemedicine The United States Army found Similarly, another study evaluated the
appointments with orthopaedic oncol- that its telemedicine program, which efficiency and orthopaedic surgery spe-
ogy specialists for patients with sus- consisted of email consultations from cialty care wait times of patients in remote
pected bone tumors were found to health-care providers in austere settings locations using telemedicine. The authors
decrease health-care costs between 12% of deployment to subspecialty ortho- found that nearly 70% of patient consul-
and 72% when compared with con- paedic consultants, limited the number tations were resolved after 2 telemedicine
ventional face-to-face appointments. of unnecessary medical evacuations16. evaluations, and wait times for referrals to
The cost analysis performed by the Rogers et al. equipped 4 rural hospital orthopaedic subspecialty care decreased
authors considered the cost of trans- emergency departments with real-time from 201 to 40 days21.
portation as the primary variable that videoconference technology to facilitate
was responsible for telemedicine’s cost- consultation with 3 trauma surgeons at Challenges and Barriers
savings11. level-I trauma centers17. Telemedicine Despite multiple studies demonstrating
Despite the evidence in support of consultations in the study were with telemedicine’s efficacy, widespread im-
telemedicine’s cost-effectiveness, other more severely injured patients than the plementation faces multiple barriers,
authors have identified weaknesses and general trauma population that was including regulatory support, reim-
have recommended additional studies to admitted to the level-I trauma center. bursement, liability, and the technology
consider alternative economic evalua- These findings were attributed to the itself.
tions12. Some of these include how increase in capability of the rural hospi- Establishing a patient-provider
studies define costs, which can involve tals, which leveraged the level-I trauma relationship using telemedicine subjects
1 or a combination of factors that are not surgeons’ expertise to perform patient the provider and the practice to all of the
uniform across all studies and therefore care. More than 80% of the rural refer- usual regulatory considerations. The
make cost comparisons difficult11. ring providers believed that telemedi- provider needs to be licensed at the site
Multiple studies have found that cine improved trauma care and was of origin, and the video and medical
telemedicine increases access to care for lifesaving on multiple occasions17. record transmission should be HIPAA-
patients in remote locations. Aarnio Not only has telemedicine been compliant1. Although many state licen-
et al. prospectively evaluated orthopae- shown to decrease cost and improve sure statutes have provisions for inter-
dic telemedicine consultations that were access to care, it has also been shown state consultations and have enacted
performed in which the locations of the to improve provider efficiency and special “telemedicine licenses,” these are
JULY 2020 · VOLUME 8, ISSUE 7 · e20.00083 3
| Te l e m e d i c i n e a n d O r t h o p a e d i c S u r g e r y
not uniformly present in all states. their telemedicine system, such as orders maintenance or service subscription
In addition, The Joint Commission and progress notes that were not inserted fees, which can add additional costs.
requires that physicians practicing with into the chart after the consultation had Telemedicine encounters that are re-
telemedicine technologies be creden- been completed18. Similar challenges corded and archived as part of the per-
tialed in the hospital where they are were noted by Rogers et al.17. On mul- manent medical record necessitate large
transmitting17. Additionally, the Ryan tiple occasions, the hospital and the data storage capability, which also can
Haight Act prohibits the prescribing of trauma surgeon were not able to connect increase costs.
controlled substances without a valid using the videoconferencing system. Nevertheless, there are lower-cost
prescription and requires at least 1 in- Additional technical failures included alternatives in the form of videoconfer-
person evaluation. Although there are loss of remote camera control and non- encing software and mobile applications
exemptions granted for telemedicine, functional audio17. (apps) that can be easily downloaded
providers must meet specific criteria, Baruffaldi et al. compared asyn- onto computers, tablets, and smart-
and these vary from state to state. The chronous and synchronous real-time phones. Zoom for Healthcare, GoTo-
current public health emergency is 1 of teleconsulting for orthopaedic second Meeting, and Skype for Business are a
the exemptions to the Ryan Haight Act opinions24. The authors found that few examples of the products that pur-
and was granted by the U.S. Drug asynchronous teleconsulting was pre- port HIPAA-compliant videoconfer-
Enforcement Administration (DEA) in ferred in the majority of cases, although encing capability26. The WhatsApp
March 2020 to help curtail the spread of there were issues with the lack of infor- Messenger is another example of a
COVID-1922. mation or the low quality of the infor- relatively inexpensive nonmedical
The next challenge is reimburse- mation that had been received from the mobile app that has been shown to
ment. Medicare only pays for video referring sites. The authors found that effectively facilitate orthopaedic care in
consultation if the patient lives in a clinicians’ confidence in their diagnosis multiple clinical settings27,28. The cost-
designated rural Health Professional was lower in asynchronous consulta- effectiveness and ubiquitous presence of
Shortage Area, and reimbursement by tions, and clinical complexity and orga- these technologies should be balanced
private payers varies5. Thus, under the nizational requirements were noted to against their requirements of patient
current payment models, reimburse- be the main factors affecting the choice resources and fluency with technology.
ment is limited. However, during the of the consulting procedure24. Although Presuming that all patients possess the
COVID-19 pandemic, several insur- videoconferencing has been found to be necessary technology and understand-
ance companies as well as the CMS, with feasible for the examination of ortho- ing of this technology to effectively
the support of multiple regulatory bod- paedic outpatients when randomized to leverage it for telemedicine may disen-
ies, made necessary changes to their telemedicine, there have been problems franchise certain groups of patients.
policies that enabled providers to engage examining these patients. There are Therefore, consideration of lower-cost
patients with telemedicine and bill for instances where the diagnosis and sub- alternative forms of telemedicine cannot
their services5. sequent treatment are contingent on ignore the patient factors that may
Malpractice insurance and liability specific physical examination findings or compromise their efficacy.
for providers who are engaged in tele- inspection can be impeded with poor-
medicine also have raised concerns17,18,23. quality audio-video or imaging tech- Implementation
Some institutions have attempted to nology. Therefore, some authors Despite multiple challenges and bar-
resolve these concerns by covering endorse the remote evaluation of riers, telemedicine possesses several
providers in the same fashion as an in- orthopaedic patients only when reliable advantages and can serve as a valuable
person visit, and they require the use and high-quality audio-video or imaging tool to reduce costs, increase access, and
of a separate consent form for tele- technology is not critical for developing improve patient satisfaction and effi-
medicine encounters 17 . In addition, a treatment plan25. ciency. Providers who are interested in
each telemedicine encounter is vid- Finally, the costs of implementation developing a telemedicine service-line in
eotaped and kept as part of the per- and maintenance have been cited as their practice should set clear goals that
manent medical record for each barriers to the widespread adoption of reflect the needs of their patient popu-
patient encounter 23 . Other liability telemedicine. The cost of installing the lation and practice. This begins with
concerns have been raised in which required surveillance equipment to determining which telemedicine plat-
a referring provider could be held complete remote wound consults form capabilities would enable effective
liable for not obtaining a telemed- through videoconferencing has been telemedicine consultations. Some of
icine consult if the service was noted to be substantial18. This finding these platform capabilities include, but
available 17 . has been echoed in other studies, with are not limited to, the ability to screen
Clegg et al. noted technological starting costs ranging from $10,000 to share and review imaging with patients
difficulties with the implementation of $17,0008,17. These costs do not include while also simultaneously maintaining
4 JULY 2020 · VOLUME 8, ISSUE 7 · e 20.00083
Te l e m e d i c i n e a n d O r t h o p a e d i c S u r g e r y |
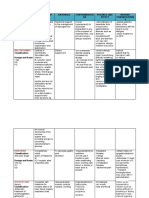
TABLE I Telemedicine Resources
Resource Description
Center for Connected Health Nonprofit organization originally established by the California Health Care
Policy (CCHP)* Foundation
Serves as the National Telehealth Policy Resource Center
Resources dedicated to national and state-specific telehealth policy
National Consortium of Federally funded with charter from the Office for the Advancement of
Telehealth Resource Centers Telehealth
(TRC)† Provides assistance, education, and information to individuals and
organizations interested in providing health care at a distance
Regional telehealth resource center hub
National Telehealth Technology Grant funded with support from the Office for the Advancement of Telehealth,
Assessment Resource Center Health Resources and Services Administration, U.S. Department of Health and
(TTAC)‡ Human Services (HHS)
Based out of the Alaska Native Tribal Health Consortium (ANTHC)
Offers a variety of services in the areas of technology assessment and selection
for providers
American Telemedicine Nonprofit association that is headquartered in Washington, DC
Association (ATA)§ Seeks to accelerate the adoption of telehealth
Promotes policy and provides education and resources to include
telemedicine clinical practice guidelines
*cchpca.org. †telehealthresourcecenter.org. ‡telehealthtechnology.org. §americantelemed.org.
videoconferencing. Other examples Additionally, there must be an health information should then follow
include audio-only platforms and analysis of the projected cost impact (Table II). Many of the larger elec-
asynchronous texting or emailing. and a review of state regulations to tronic medical record (EMR) compa-
While patient satisfaction has been ensure that a patient-provider rela- nies provide telemedicine options
demonstrated in both synchronous tionship can occur using telemedicine. that interface with their EMR. Thus,
and asynchronous telemedicine The Center for Connected Health providers currently using an EMR
platforms, studies citing patient sat- Policy (CCHP) is 1 of many resources system should consider engaging
isfaction with asynchronous tele- that can help providers understand their EMR’s representatives. Lastly,
medicine have primarily involved many of the policies and regulations verifying state licensure rules and
older patient populations 29. There- pertaining to telemedicine (Table I). policy compliance along with re-
fore, the capability to deliver multi- Reviewing telemedicine vendors and viewing malpractice considerations
modal telemedicine services allows for options in addition to ensuring HI- with your malpractice insurance
a more efficacious patient-centered PAA compliance with secured en- carrier can mitigate medicolegal
approach. crypted transmissions for personal liability.
TABLE II Telemedicine Vendor Considerations*
Determine upfront and maintenance/subscription cost(s)
Assess platform capabilities (screen sharing, uploading outside images)
System compliance with HIPAA and medical boards
Type of services provided (synchronous “real-time” videoconferencing versus asynchronous “store-and-forward”)
24/7 service and technical support
Integration with current practice and electronic health record
Support for insurance claims/billing
*https://www.aaos.org/quality/practice-management/telemedicine/. HIPAA 5 Health Insurance Portability and Accountability
Act.
JULY 2020 · VOLUME 8, ISSUE 7 · e20.00083 5
| Te l e m e d i c i n e a n d O r t h o p a e d i c S u r g e r y
Future Directions icymakers will be necessary if telemedi- 3. Brebner EM, Seymour DG. Telemedicine and
the older patient. Age Ageing. 2001 May;30(3):
The use of telemedicine is likely to cine is to continue to grow in practice 183-4.
increase in the United States. A 2017 and scope. 4. Buvik A, Bugge E, Knutsen G, Småbrekke A,
survey of 184 health-care executives Wilsgaard T. Patient reported outcomes
with remote orthopaedic consultations by
conducted by the American Telemedi- Overview telemedicine: a randomised controlled trial. J
cine Association found that 88% of the Telemedicine is a multidimensional Telemed Telecare. 2019 Sep;25(8):451-9. Epub
2018 Jul 4.
executives believed that they would rapidly evolving modality that is capable
5. Centers for Medicare & Medicaid Services.
invest in telemedicine in the near future, of improving access to quality cost- Medicare telemedicine healthcare provider fact
and 98% believed that it offered a efficient health care for patients needing sheet. 2020 Mar 17. Accessed 2020 Apr 1.
https://www.cms.gov/newsroom/fact-sheets/
competitive advantage. However, 71% orthopaedic specialty services. The medicare-telemedicine-health-care-provider-
believed that lack of coverage and pay- fact-sheet
COVID-19 pandemic has compelled
ments were barriers to implementation1. 6. ATA practice guidelines for live, on-demand
providers to negotiate a myriad of chal- primary and urgent care. Accessed 2020 Jun 23.
A more recent survey of .800 physi- lenges that have brought telemedicine to http://www.medicalinfo.ch/images/articles/
cians in the U.S. found that 48% are ATA-Practice-Guidelines-for-Live-On-Demand-
the forefront of health care. With the Primary-and-Urgent-Care.pdf
now using telemedicine in their prac- support of the CMS and other insurance 7. Tanaka MJ, Oh LS, Martin SD, Berkson EM.
tices as a consequence of COVID-19, carriers, telemedicine initiatives were Telemedicine in the era of COVID-19: the virtual
orthopaedic examination. J Bone Joint Surg
which is up from 18% in a similar survey quickly supported and enacted in order Am. 2020 Jun 17;102(12):e57.
that had been conducted in 201830. to continue providing health care to 8. Buvik A, Bergmo TS, Bugge E, Smaabrekke A,
Another survey of .600 private prac- patients during the pandemic. Patient Wilsgaard T, Olsen JA. Cost-effectiveness
of telemedicine in remote orthopedic
tices and 140 billing companies found a satisfaction is a key component of tele- consultations: randomized controlled trial. J
35% decline in patient volume during medicine and will drive its evolution. Med Internet Res. 2019 Feb 19;21(2):e11330.
March 2020. The survey also found that 9. Ohinmaa A, Vuolio S, Haukipuro K, Winblad I.
Beyond the COVID-19 pandemic, A cost-minimization analysis of orthopaedic
41% of respondents had begun offering telemedicine will undoubtedly serve an consultations using videoconferencing in
telemedicine options to patients, up comparison with conventional consulting. J
increasing role as our new normal in Telemed Telecare. 2002;8(5):283-9.
from 22% in a previous 2018 survey31. orthopaedic surgery. 10. Harno K, Arajärvi E, Paavola T, Carlson C,
Despite telemedicine’s tremen- Viikinkoski P. Clinical effectiveness and cost
dous upside, traditional research analysis of patient referral by videoconferencing in
Nathan S. Lanham, MD1,
orthopaedics. J Telemed Telecare. 2001;7(4):
methods may be challenging with tele- Kyle J. Bockelman, DO2, 219-25.
medicine, given the rapidly increasing Brendan J. McCriskin, MD1 11. Aponte-Tinao LA, Farfalli GL, Albergo JI,
utilization of health technology among Plazzotta F, Sommer J, Luna D, de Quirós FGB.
1Department of Orthopaedic Surgery, Face to face appointment vs. telemedicine in
patients and health-care systems, espe- Martin Army Community Hospital, first time appointment orthopedic oncology
cially during the COVID-19 pandemic. patients: a cost analysis. Stud Health Technol
Fort Benning, Georgia Inform. 2019 Aug 21;264:512-5.
Thus, the traditional methods of ran- 12. Mair FS, Haycox A, May C, Williams T. A
2Department of Orthopaedic Surgery,
domized controlled trials to evaluate the review of telemedicine cost-effectiveness
efficacy of an intervention or a change in William Beaumont Army Medical Center, studies. J Telemed Telecare. 2000;6(Suppl 1):
El Paso, Texas S38-40.
care delivery may not be feasible. Some 13. Aarnio P, Lamminen H, Lepistö J, Alho A. A
authors have instead suggested more Email address for K.J. Bockelman: prospective study of teleconferencing for
orthopaedic consultations. J Telemed Telecare.
pragmatic methods that balance the kbockelman@gmail.com 1999;5(1):62-6.
traditional research paradigms and the 14. Wallace P, Haines A, Harrison R, Barber J,
ever-changing landscape of telemedicine ORCID iD for N.S. Lanham: Thompson S, Jacklin P, Roberts J, Lewis L,
0000-0003-3641-9367 Wainwright P; Virtual Outreach Project Group.
and its many facets32. In addition, future Joint teleconsultations (virtual outreach) versus
ORCID iD for K.J. Bockelman:
research regarding telemedicine must standard outpatient appointments for patients
0000-0002-5627-3695 referred by their general practitioner for a
more clearly and uniformly define cost ORCID iD for B.J. McCriskin: specialist opinion: a randomised trial. Lancet.
analysis and cost savings in order to 0000-0003-2941-9983 2002 Jun 8;359(9322):1961-8.
enable comparison among studies. Bar- 15. Buvik A, Bugge E, Knutsen G, Småbrekke A,
Wilsgaard T. Quality of care for remote
riers to regulatory support and reim- References orthopaedic consultations using telemedicine:
bursement that have required specialty 1. Serper M, Volk ML. Current and future a randomised controlled trial. BMC Health Serv
applications of telemedicine to optimize the Res. 2016 Sep 8;16:483.
society involvement in the form of delivery of care in chronic liver disease. Clin 16. Blank E, Lappan C, Belmont PJ Jr, Machen
evidence-based practice guidelines and Gastroenterol Hepatol. 2018 Feb;16(2): MS, Ficke J, Pope R, Owens BD. Early analysis of
157-161.e8. the United States Army’s telemedicine
political advocacy have largely been
2. Ohannessian R, Duong TA, Odone A. Global orthopaedic consultation program. J Surg
eliminated during the COVID-19 Telemedicine implementation and Orthop Adv. 2011 Spring;20(1):50-5.
pandemic. Nevertheless, sustained integration within health systems to fight the 17. Rogers FB, Ricci M, Caputo M, Shackford S,
COVID-19 pandemic: a call to action. JMIR Sartorelli K, Callas P, Dewell J, Daye S. The use of
coordinated efforts among providers, Public Health Surveill. 2020 Apr 2;6(2): telemedicine for real-time video consultation
researchers, insurance carriers, and pol- e18810. between trauma center and community
6 JULY 2020 · VOLUME 8, ISSUE 7 · e 20.00083
Te l e m e d i c i n e a n d O r t h o p a e d i c S u r g e r y |
hospital in a rural setting improves early trauma 23. Karp WB, Grigsby RK, McSwiggan-Hardin M, 28. Khanna V, Sambandam SN, Gul A,
care: preliminary results. J Trauma. 2001 Dec; Pursley-Crotteau S, Adams LN, Bell W, Stachura Mounasamy V. “WhatsApp”ening in orthopedic
51(6):1037-41. ME, Kanto WP. Use of telemedicine for children care: a concise report from a 300-bedded
18. Clegg A, Brown T, Engels D, Griffin P, with special health care needs. Pediatrics. 2000 tertiary care teaching center. Eur J Orthop Surg
Simonds D. Telemedicine in a rural community Apr;105(4 Pt 1):843-7. Traumatol. 2015 Jul;25(5):821-6. Epub 2015 Jan
hospital for remote wound care consultations. J 24. Baruffaldi F, Gualdrini G, Toni A. 30.
Wound Ostomy Continence Nurs. 2011 May- Comparison of asynchronous and realtime 29. Kruse CS, Krowski N, Rodriguez B, Tran L,
Jun;38(3):301-4. teleconsulting for orthopaedic second Vela J, Brooks M. Telehealth and patient
19. Zennaro F, Grosso D, Fascetta R, Marini M, opinions. J Telemed Telecare. 2002;8(5): satisfaction: a systematic review and narrative
Odoni L, Di Carlo V, Dibello D, Vittoria F, 297-301. analysis. BMJ Open. 2017 Aug 3;7(8):e016242.
Lazzerini M. Teleradiology for remote 25. Haukipuro K, Ohinmaa A, Winblad I, Linden 30. Merritt Hawkins. Survey: physician
consultation using iPad improves the use of T, Vuolio S. The feasibility of telemedicine for practice patterns changing as a result of
health system human resources for paediatric orthopaedic outpatient clinics—a randomized
fractures: prospective controlled study in a COVID-19. 2020. Accessed 2020 May 17. https://
controlled trial. J Telemed Telecare. 2000;6(4):
tertiary care hospital in Italy. BMC Health Serv www.merritthawkins.com/news-and-insights/
193-8.
Res. 2014 Jul 28;14:327. media-room/press/-Physician-Practice-
26. U.S. Department of Health and Human Patterns-Changing-as-a-Result-of-COVID-19/.
20. Gamus A, Kaufman H, Chodick G. Remote care Services. Notification of enforcement discretion
of lower extremities ulcers: an observational pilot for telehealth remote communications during
31. Kareo. Independent medical practices
study. Isr Med Assoc J. 2019 Apr;21(4):265-8. the COVID-19 nationwide public health emer- rapidly deploying telemedicine to offset steep
drop in patient office visits due to “stay at
21. Prada C, Izquierdo N, Traipe R, Figueroa C. gency. 2020. Accessed 2020 May 17. https://
www.hhs.gov/hipaa/for-professionals/special- home” orders. 2020. Accessed 2020 May 17.
Results of a new telemedicine strategy in
traumatology and orthopedics. Telemed J E topics/emergency-preparedness/notification- https://www.kareo.com/newsroom/press/
Health. 2020 May;26(5):665-70. Epub 2019 Jul 9. enforcement-discretion-telehealth/index.html kareo-survey-reveals-coronavirus-pandemic-
impact-independent-medical-practices
22. Drug Enforcement Administration. How to 27. Giordano V, Koch HA, Mendes CH,
prescribe controlled substances to patients Bergamin A, de Souza FS, do Amaral NP. 32. Proctor E, Silmere H, Raghavan R, Hovmand
during the COVID-19 public health emergency. WhatsApp Messenger is useful and P, Aarons G, Bunger A, Griffey R, Hensley M.
Accessed 2020 May 17. https://www. reproducible in the assessment of tibial plateau Outcomes for implementation research:
deadiversion.usdoj.gov/GDP/(DEA-DC- fractures: inter- and intra-observer agreement conceptual distinctions, measurement
023)(DEA075)Decision_Tree_(Final)_33120_ study. Int J Med Inform. 2015 Feb;84(2):141-8. challenges, and research agenda. Adm
2007.pdf Epub 2014 Nov 11. Policy Ment Health. 2011 Mar;38(2):65-76.
JULY 2020 · VOLUME 8, ISSUE 7 · e20.00083 7
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5834)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (903)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (541)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (823)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (405)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Case Reflection FormatDocument9 pagesCase Reflection Formatanusarannya100% (5)
- Pandora's Box FinalDocument45 pagesPandora's Box FinalPraveen CrNo ratings yet
- DodgeballDocument5 pagesDodgeballapi-514548596No ratings yet
- Cetak Stop Opname - AlkesDocument22 pagesCetak Stop Opname - AlkesOkto YutubNo ratings yet
- Assessing The Current State of Cognitive Frailty: Measurement PropertiesDocument9 pagesAssessing The Current State of Cognitive Frailty: Measurement PropertiesCarlos CarrilloNo ratings yet
- Hepatic EncelopathyDocument10 pagesHepatic EncelopathyWinny WullurNo ratings yet
- Zoll AED PlusDocument5 pagesZoll AED PlusNurul FathiaNo ratings yet
- Physiotherapy in CancerDocument5 pagesPhysiotherapy in CancerSofia Adão da FonsecaNo ratings yet
- Administration of Oxygen Retdem NotesDocument2 pagesAdministration of Oxygen Retdem NotesJhayneNo ratings yet
- Acute Bronchitis - StatPearls - NCBI BookshelfDocument1 pageAcute Bronchitis - StatPearls - NCBI BookshelfJulian Muhammad YasinNo ratings yet
- Lucas v. TuanoDocument25 pagesLucas v. TuanojNo ratings yet
- BHS Lec 1Document55 pagesBHS Lec 1AtiaNo ratings yet
- Brazilian Version of The Mattis Dementia Rating ScaleDocument7 pagesBrazilian Version of The Mattis Dementia Rating ScaleCaio PereiraNo ratings yet
- Complex Regional Pain SyndromesDocument16 pagesComplex Regional Pain SyndromesroooNo ratings yet
- Use Your Brain To Change Your Age by Daniel G. Amen - ExcerptDocument38 pagesUse Your Brain To Change Your Age by Daniel G. Amen - ExcerptCrown Publishing Group89% (9)
- Neonatal Mortality, Risk Factors and Causes - A Prospective Population-Based Cohort Study in Urban PakistanDocument7 pagesNeonatal Mortality, Risk Factors and Causes - A Prospective Population-Based Cohort Study in Urban PakistanDavid OlarinloyeNo ratings yet
- Aha GuidlineDocument7 pagesAha GuidlineMidyan AjiarsoNo ratings yet
- 2 Pharma ModuleDocument227 pages2 Pharma ModuleCielina BatangNo ratings yet
- DVDGGDocument10 pagesDVDGGSilviNo ratings yet
- Hitā HitāDocument25 pagesHitā HitāAnamaria IvančićNo ratings yet
- Cdc-Guideline For Disinfection and Sterilization in Health-Care Facilities-2008Document158 pagesCdc-Guideline For Disinfection and Sterilization in Health-Care Facilities-2008fuentenatura100% (1)
- Kaufman Cerina RDRDocument3 pagesKaufman Cerina RDRapi-730043203No ratings yet
- HEPATITIS A DRUG STUDY FinalDocument3 pagesHEPATITIS A DRUG STUDY FinalJordz PlaciNo ratings yet
- Indirect Calorimetry in Critical Illness A New.3Document10 pagesIndirect Calorimetry in Critical Illness A New.3gjk5q24qrqNo ratings yet
- Pem PresenataionDocument38 pagesPem PresenataionBhawna PandhuNo ratings yet
- Worksheet #3 VOCABULARYDocument2 pagesWorksheet #3 VOCABULARYAngel Angeleri-priftis.No ratings yet
- Hba 1 CDocument2 pagesHba 1 CManoj MishraNo ratings yet
- Final NCP AppendicitisDocument4 pagesFinal NCP AppendicitisCha Ry100% (1)
- MCQ3FULLDocument153 pagesMCQ3FULLtheintrov100% (4)
- Health - Grade-10 - Module 3Document21 pagesHealth - Grade-10 - Module 3Christine Faith DimoNo ratings yet