Professional Documents
Culture Documents
Time Kinetics of Viral Clearance and Resolution of Symptoms in Novel Coronavirus Infection
Time Kinetics of Viral Clearance and Resolution of Symptoms in Novel Coronavirus Infection
Uploaded by
Bharat GouripurCopyright:
Available Formats
You might also like
- Why You Need To Quit Drinking Soda PersuasiveDocument3 pagesWhy You Need To Quit Drinking Soda PersuasiveEdcel Abustan100% (1)
- Smoking Stinks Lesson PlanDocument3 pagesSmoking Stinks Lesson PlanNatalia Soledad RojasNo ratings yet
- PIIS0140673620306334Document2 pagesPIIS0140673620306334Dina sofianaNo ratings yet
- Preliminary Study To Identify Severe From Moderate Cases of COVID-19 Using Combined Hematology ParametersDocument15 pagesPreliminary Study To Identify Severe From Moderate Cases of COVID-19 Using Combined Hematology Parameterstrisna amijayaNo ratings yet
- Piis0923753420363833 PDFDocument26 pagesPiis0923753420363833 PDFSyed HossainNo ratings yet
- COVID-19: Towards Controlling of A Pandemic: CommentDocument4 pagesCOVID-19: Towards Controlling of A Pandemic: CommentEugenNo ratings yet
- 10.5811@westjem.2020.6.47919 (2) 81105Document7 pages10.5811@westjem.2020.6.47919 (2) 81105Giovan GaulNo ratings yet
- Journal Pre-Proof: Journal of Clinical VirologyDocument18 pagesJournal Pre-Proof: Journal of Clinical VirologyOkki Wahyu AtikasariNo ratings yet
- Association of Procalcitonin Levels With The Progression and Prognosis of Hospitalized Patients With COVID-19Document9 pagesAssociation of Procalcitonin Levels With The Progression and Prognosis of Hospitalized Patients With COVID-19Dian Putri NingsihNo ratings yet
- Reduction and Functional Exhaustion of T Cells inDocument14 pagesReduction and Functional Exhaustion of T Cells inChavdarNo ratings yet
- Clinical Characteristics of Children With Coronavirus Disease 2019 in Hubei, ChinaDocument6 pagesClinical Characteristics of Children With Coronavirus Disease 2019 in Hubei, ChinaBobanBisercicNo ratings yet
- Rccm.202002 0445oc Clinics ChineseDocument53 pagesRccm.202002 0445oc Clinics ChineseAlex Escobar GavilánNo ratings yet
- A Novel Severity Score To Predict Inpatient Mortality in COVID 19 PatientsDocument8 pagesA Novel Severity Score To Predict Inpatient Mortality in COVID 19 PatientsanscstNo ratings yet
- 1 s2.0 S0272638620306120 ManinDocument10 pages1 s2.0 S0272638620306120 ManinrezaNo ratings yet
- Sars-Cov-2 Viral Load in Clinical Samples of Critically Ill PatientsDocument15 pagesSars-Cov-2 Viral Load in Clinical Samples of Critically Ill Patientsrahma_husna_1No ratings yet
- UK Estimates of The Severity of COVID-19 DiseaseDocument32 pagesUK Estimates of The Severity of COVID-19 DiseaseRogueNo ratings yet
- 4) Komorbid Dan Usia (Rebecca) 10.1002@art.41456Document25 pages4) Komorbid Dan Usia (Rebecca) 10.1002@art.41456Mastifa HanasitaNo ratings yet
- Clinical Characteristics of Imported Cases of COVID-19 in Jiangsu Province A Multicenter Descriptive StudyDocument23 pagesClinical Characteristics of Imported Cases of COVID-19 in Jiangsu Province A Multicenter Descriptive StudyAna Maria Romero IbagonNo ratings yet
- Journal Pre-Proof: International Journal of Infectious DiseasesDocument18 pagesJournal Pre-Proof: International Journal of Infectious DiseasesKenya EspinozaNo ratings yet
- Coagulation Disorder PDFDocument4 pagesCoagulation Disorder PDFBrownell TraciNo ratings yet
- 1 LRDocument12 pages1 LRaoonNo ratings yet
- A Case Series Describing The Epidemiology and Clinical Characteristics of COVID-19 Infection in Jilin ProvinceDocument4 pagesA Case Series Describing The Epidemiology and Clinical Characteristics of COVID-19 Infection in Jilin Provinceabeer alrofaeyNo ratings yet
- Asymptomatic and Human To Human Transmission of SARS COV 2Document3 pagesAsymptomatic and Human To Human Transmission of SARS COV 2belinda thaniaNo ratings yet
- Covid-19 in Critically Ill Patients in The Seattle Region - Case SeriesDocument18 pagesCovid-19 in Critically Ill Patients in The Seattle Region - Case SeriesZelgi PutraNo ratings yet
- Journal Pre-Proof: Journal of Cardiothoracic and Vascular AnesthesiaDocument21 pagesJournal Pre-Proof: Journal of Cardiothoracic and Vascular AnesthesiaJuan Esteban Paez MolinaNo ratings yet
- Covid Er ArticleDocument6 pagesCovid Er ArticleReeb BukhariNo ratings yet
- Pathological Evidence of Pulmonary Thrombotic Phenomena in Severe COVID 19Document5 pagesPathological Evidence of Pulmonary Thrombotic Phenomena in Severe COVID 19Victor AugustoNo ratings yet
- Coagulation Disorders in Coronavirus Infected PatientsDocument6 pagesCoagulation Disorders in Coronavirus Infected PatientsQuang TrầnNo ratings yet
- Journal Pre-Proof: International Journal of Infectious DiseasesDocument14 pagesJournal Pre-Proof: International Journal of Infectious DiseasesKenya EspinozaNo ratings yet
- Clinical Characteristics and Durations of Hospitalized Patients With COVID-19 in BeijingDocument18 pagesClinical Characteristics and Durations of Hospitalized Patients With COVID-19 in BeijingTOMMYNo ratings yet
- An Epidemiological Study of Laboratory Confirmed COVID-19 Cases Admitted in Dhaka Medical College HospitalDocument7 pagesAn Epidemiological Study of Laboratory Confirmed COVID-19 Cases Admitted in Dhaka Medical College HospitalPranto BaraiNo ratings yet
- Seminario CovidDocument17 pagesSeminario CovidGonzalo Ccahuana YanqueNo ratings yet
- Multisystem Inflammatory Syndrome in Children and Adolescents With COVID-19Document3 pagesMultisystem Inflammatory Syndrome in Children and Adolescents With COVID-19Maria BriceñoNo ratings yet
- Jurnal Chen Et AlDocument31 pagesJurnal Chen Et AlUtami MNo ratings yet
- Fimmu 11 00827Document7 pagesFimmu 11 00827yangxiao9511No ratings yet
- Epidemiological and Clinical Characteristics of 671 COVID-19 Patients in Henan Province, ChinaDocument11 pagesEpidemiological and Clinical Characteristics of 671 COVID-19 Patients in Henan Province, ChinaOrlando JúniorNo ratings yet
- Title Authors:: Snarain@northwell - EduDocument17 pagesTitle Authors:: Snarain@northwell - EduPaola A. Zeña HuancasNo ratings yet
- Clinical Immunology: Koichi Yuki, Miho Fujiogi, Sophia Koutsogiannaki TDocument7 pagesClinical Immunology: Koichi Yuki, Miho Fujiogi, Sophia Koutsogiannaki TishmahNo ratings yet
- Coccidioidomycosis in Patients With HIV-1 Infection in The Era of Potent Antiretroviral TherapyDocument7 pagesCoccidioidomycosis in Patients With HIV-1 Infection in The Era of Potent Antiretroviral Therapydata32No ratings yet
- Ciaa242 2 PDFDocument8 pagesCiaa242 2 PDFHesbon MomanyiNo ratings yet
- Estudo DiabetesDocument9 pagesEstudo DiabetesFulano de TalNo ratings yet
- Analysis Clinical Features of COVID-19 Infection IDocument6 pagesAnalysis Clinical Features of COVID-19 Infection Imohamed atefNo ratings yet
- Ciaa 414Document7 pagesCiaa 414Kev Jose Ruiz RojasNo ratings yet
- Us Chest CT Findings in Coronavirus Disease PDFDocument7 pagesUs Chest CT Findings in Coronavirus Disease PDFRomit JainNo ratings yet
- Clinical Features of Patients Infected With 2019 Novel Coronavirus in Wuhan China Chaolin Huang 2 Full Chapter PDFDocument34 pagesClinical Features of Patients Infected With 2019 Novel Coronavirus in Wuhan China Chaolin Huang 2 Full Chapter PDFhassidcaraza100% (8)
- Dong J - Prediction For Progression Risk in Patients With COVID - 19 Pneumonia The CALL ScoreDocument7 pagesDong J - Prediction For Progression Risk in Patients With COVID - 19 Pneumonia The CALL ScoreMercedes Ah CardenasNo ratings yet
- Aksungar 2007Document10 pagesAksungar 2007twarrenNo ratings yet
- PIIS0140673622003270Document7 pagesPIIS0140673622003270chaivat kNo ratings yet
- Clinical Features of Patients Infected With 2019 Novel Coronavirus in Wuhan China Chaolin Huang Full Chapter PDFDocument34 pagesClinical Features of Patients Infected With 2019 Novel Coronavirus in Wuhan China Chaolin Huang Full Chapter PDFhassidcaraza100% (8)
- Pages From WhuDocument2 pagesPages From Whurahat879No ratings yet
- Coronavirus Disease 2019 (COVID-19) A Perspective From ChinaDocument29 pagesCoronavirus Disease 2019 (COVID-19) A Perspective From ChinabackupNo ratings yet
- CCDCW220132Document7 pagesCCDCW220132Lin ZhouNo ratings yet
- Preprint corticoidesNeuminiaCOVIDDocument16 pagesPreprint corticoidesNeuminiaCOVIDJorgelina BernetNo ratings yet
- Journal Pre-Proof: Clinical ImmunologyDocument23 pagesJournal Pre-Proof: Clinical ImmunologypqrsehunNo ratings yet
- Clinical Characteristics of Covid-19 in China: CorrespondenceDocument3 pagesClinical Characteristics of Covid-19 in China: CorrespondenceSofia VidalNo ratings yet
- New Insights of Emerging Sars-Cov-2: Epidemiology, Etiology, Clinical Features, Clinical Treatment, and PreventionDocument22 pagesNew Insights of Emerging Sars-Cov-2: Epidemiology, Etiology, Clinical Features, Clinical Treatment, and PreventionWendi IochNo ratings yet
- Liu2020 Article ClinicalAndBiochemicalIndexesFDocument11 pagesLiu2020 Article ClinicalAndBiochemicalIndexesFGabriel Ibarra TrujilloNo ratings yet
- Gender Differences in Patients With COVID-19: Focus On Severity and MortalityDocument18 pagesGender Differences in Patients With COVID-19: Focus On Severity and MortalityYogi drNo ratings yet
- Analysis of Mortality in Covid 19 Patients - A Study in A District Covid Hospital in Andhra Pradesh During The First WaveDocument6 pagesAnalysis of Mortality in Covid 19 Patients - A Study in A District Covid Hospital in Andhra Pradesh During The First WaveIJAR JOURNALNo ratings yet
- Dengue How ClassifyDocument5 pagesDengue How ClassifyErlin IrawatiNo ratings yet
- COVID-19 Mortality Review in Malaysia & Updates on Clinical Management of COVID-19From EverandCOVID-19 Mortality Review in Malaysia & Updates on Clinical Management of COVID-19No ratings yet
- Facing COVID-19 with the benefits of medical cannabisFrom EverandFacing COVID-19 with the benefits of medical cannabisNo ratings yet
- Aluminium Glass Shutter Profile 2Document2 pagesAluminium Glass Shutter Profile 2Bharat GouripurNo ratings yet
- 1Document40 pages1Bharat GouripurNo ratings yet
- GROHE Specification Sheet 39328000Document2 pagesGROHE Specification Sheet 39328000Bharat GouripurNo ratings yet
- MT Handbook GrainDocument250 pagesMT Handbook GrainBharat GouripurNo ratings yet
- Enrolment Numbers 2018-19 BatchDocument2 pagesEnrolment Numbers 2018-19 BatchBharat GouripurNo ratings yet
- Practice F.stone-Walls FinalDocument5 pagesPractice F.stone-Walls FinalBharat GouripurNo ratings yet
- RESUME and Work Experience 080723Document9 pagesRESUME and Work Experience 080723Bharat GouripurNo ratings yet
- Eoi Extension NoticeDocument1 pageEoi Extension NoticeBharat GouripurNo ratings yet
- Course PendingDocument1 pageCourse PendingBharat GouripurNo ratings yet
- Eoi Notice Dated 27.07.2023Document6 pagesEoi Notice Dated 27.07.2023Bharat GouripurNo ratings yet
- 11 - Chapter 2Document37 pages11 - Chapter 2Bharat GouripurNo ratings yet
- New Doc 2020-04-12 14.01.13Document1 pageNew Doc 2020-04-12 14.01.13Bharat GouripurNo ratings yet
- Avalanche 2020Document1 pageAvalanche 2020Bharat GouripurNo ratings yet
- Parent LetterDocument38 pagesParent LetterBharat GouripurNo ratings yet
- Class Section WiseDocument1 pageClass Section WiseBharat GouripurNo ratings yet
- Lec 1Document14 pagesLec 1Bharat GouripurNo ratings yet
- Class - Section - Wise - ATSEC ADocument1 pageClass - Section - Wise - ATSEC ABharat GouripurNo ratings yet
- CIE - MIS Architecture Architecture Semester6 SECBDocument2 pagesCIE - MIS Architecture Architecture Semester6 SECBBharat GouripurNo ratings yet
- CIE - MIS Architecture Architecture Semester2 SECBDocument1 pageCIE - MIS Architecture Architecture Semester2 SECBBharat GouripurNo ratings yet
- School RequirementsDocument3 pagesSchool RequirementsBharat GouripurNo ratings yet
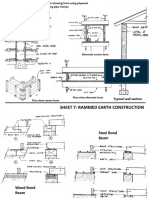
- Sheet 7Document3 pagesSheet 7Bharat GouripurNo ratings yet
- CIE - MIS Architecture Architecture Semester6 SECADocument2 pagesCIE - MIS Architecture Architecture Semester6 SECABharat GouripurNo ratings yet
- Quiz GuideDocument18 pagesQuiz GuideBharat GouripurNo ratings yet
- CIE - MIS Architecture Architecture Semester6 SECBDocument2 pagesCIE - MIS Architecture Architecture Semester6 SECBBharat GouripurNo ratings yet
- BrochureDocument44 pagesBrochureBharat GouripurNo ratings yet
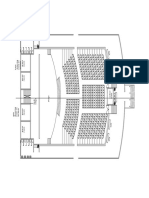
- Auditorium PlanDocument1 pageAuditorium PlanBharat GouripurNo ratings yet
- LibraryDocument5 pagesLibraryBharat GouripurNo ratings yet
- Lec 2Document17 pagesLec 2Bharat GouripurNo ratings yet
- Sheet 8Document8 pagesSheet 8Bharat GouripurNo ratings yet
- Sheet 6Document4 pagesSheet 6Bharat GouripurNo ratings yet
- SITXFSA001 Student Assessment TasksDocument24 pagesSITXFSA001 Student Assessment TasksMukta AktherNo ratings yet
- Dermatology QuestionsDocument3 pagesDermatology QuestionsMuziki Wa KiafrikaNo ratings yet
- Diseases of The NoseDocument3 pagesDiseases of The NoseVannero SembranoNo ratings yet
- Wastewater Characteristics and Effluent Quality ParametersDocument5 pagesWastewater Characteristics and Effluent Quality ParametersVincent SitholeNo ratings yet
- Trinity United Church of Christ BulletinDocument28 pagesTrinity United Church of Christ BulletinWorlee GloverNo ratings yet
- Science Olympiad InvasivesDocument2 pagesScience Olympiad InvasivesYue ZhangNo ratings yet
- Valproic Acid Drug Study PDFDocument4 pagesValproic Acid Drug Study PDFLiza Marie IgnacioNo ratings yet
- Covid Self Declaration Form Visitor PDFDocument3 pagesCovid Self Declaration Form Visitor PDFTipu BabuNo ratings yet
- Chang Et - Al PDFDocument10 pagesChang Et - Al PDFAggy AlbotraNo ratings yet
- 02/27/09 - The Stanford Daily (PDF)Document8 pages02/27/09 - The Stanford Daily (PDF)The Stanford DailyNo ratings yet
- Solid Dosage Forms in Unani System of Medicine AnDocument7 pagesSolid Dosage Forms in Unani System of Medicine AnSiddharth JainNo ratings yet
- mg359 All PDFDocument24 pagesmg359 All PDFsyedsrahmanNo ratings yet
- Men's Treatment GriffinDocument68 pagesMen's Treatment GriffintadcpNo ratings yet
- Mina Drug StudyDocument7 pagesMina Drug StudyChi Chaw Giselle HilarioNo ratings yet
- Family 2Document13 pagesFamily 2Saloni SharmaNo ratings yet
- Latihan Soal Literasi Bahasa Inggris 1Document9 pagesLatihan Soal Literasi Bahasa Inggris 1Daffa AryaputraNo ratings yet
- L A Level Biology MS Jan 06Document180 pagesL A Level Biology MS Jan 06zetsubou-chanNo ratings yet
- Gmail Maxicare EReady Advance PDFDocument7 pagesGmail Maxicare EReady Advance PDFShirelyNo ratings yet
- Family Nursing Care PlanDocument7 pagesFamily Nursing Care PlanMarilou Jumalon MontefalconNo ratings yet
- Adolescent HealthDocument47 pagesAdolescent HealthsushmaNo ratings yet
- Volume 42, Issue 34 - August 26, 2011Document56 pagesVolume 42, Issue 34 - August 26, 2011BladeNo ratings yet
- Actualizacion de La PreeclampsiaDocument8 pagesActualizacion de La PreeclampsiaPierina VeramatosNo ratings yet
- DHS CFS 600 Certificate of Child Examination Form IL444-4737Document2 pagesDHS CFS 600 Certificate of Child Examination Form IL444-4737ArtueroNo ratings yet
- RADIOLOGY 1.6 Introduction To MammographyDocument9 pagesRADIOLOGY 1.6 Introduction To MammographyZazaNo ratings yet
- Science As Proof of The Bible.Document3 pagesScience As Proof of The Bible.AndrewNo ratings yet
- Lorma Colleges College of Physical and Respiratory TherapyDocument33 pagesLorma Colleges College of Physical and Respiratory TherapyAnab Mohamed Elhassan Abbas AlnowNo ratings yet
- Best Practice Workbook - Bipolar Disorder-Yong Xiang YiDocument45 pagesBest Practice Workbook - Bipolar Disorder-Yong Xiang YiJuraidahMohdNooh100% (1)
- Communicable Disease ControlDocument52 pagesCommunicable Disease ControlNidonama E. KabmatNo ratings yet
Time Kinetics of Viral Clearance and Resolution of Symptoms in Novel Coronavirus Infection
Time Kinetics of Viral Clearance and Resolution of Symptoms in Novel Coronavirus Infection
Uploaded by
Bharat GouripurOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Time Kinetics of Viral Clearance and Resolution of Symptoms in Novel Coronavirus Infection
Time Kinetics of Viral Clearance and Resolution of Symptoms in Novel Coronavirus Infection
Uploaded by
Bharat GouripurCopyright:
Available Formats
Page 1 of 12
Time Kinetics of Viral Clearance and Resolution of Symptoms in Novel
Coronavirus Infection
De Chang1,4* MD&PhD, Guoxin Mo1* MD, Xin Yuan2* MD, Yi Tao1 MD, Xiaohua Peng5
MD, Fusheng Wang2✉️ MD, Lixin Xie1✉️ MD, Lokesh Sharma5# PhD, Charles S. Dela
Cruz5# MD&PhD, Enqiang Qin#2✉️ MD
1. College of Pulmonary and Critical Care Medicine, Chinese PLA General Hospital,
Beijing 100083, China
2. College of Infectious Disease, Chinese PLA General Hospital, Beijing 100083, China
3. Department of Critical Care Medicine, 5th center of Chinese PLA General Hospital,
Beijing 100039, China
4. 3rd Medical Center, Chinese PLA General Hospital, Beijing 100083, China
5. Section of Pulmonary and Critical Care and Sleep Medicine, Department of Medicine,
Yale University School of Medicine, New Haven, CT 06520, USA
* First authors contributed equally: De Chang, Guoxin Mo and Xin Yuan
# Senior authors contributed equally: Lokesh Sharma, Charles S. Dela Cruz and
Enqiang Qin
✉️ Corresponding authors: Fusheng Wang(fswang302@163.com, Lixin Xie
(2464277169@qq.com), Enqiang Qin(qeq2004@sina.com)
Total word count: 998 words.
AJRCCM Articles in Press. Published March 23, 2020 as 10.1164/rccm.202003-0524LE
Copyright © 2020 by the American Thoracic Society
Page 2 of 12
This article has an online data supplement, which is accessible from this issue's table of
content online at www.atsjournals.org.
This article is open access and distributed under the terms of the Creative Commons
Attribution Non-Commercial No Derivatives License 4.0
(http://creativecommons.org/licenses/by-nc-nd/4.0/). For commercial usage and reprints
please contact Diane Gern (dgern@thoracic.org).
AJRCCM Articles in Press. Published March 23, 2020 as 10.1164/rccm.202003-0524LE
Copyright © 2020 by the American Thoracic Society
Page 3 of 12
Introduction
SARS-CoV-2 (previously 2019-nCoV) has infected >167,000 patients and killed >6600
people(1). It has been reported that a patient in Germany had high viral titers after the
resolution of fever and infected two of the close contacts after the resolution of
symptoms(2). In the wake of these cases, it is still unclear how long the patient was
virus positive after the resolution of the symptoms. In this study, we aimed to determine
the time kinetics of viral clearance in reference to the resolution of symptoms in 16
patients treated in Beijing, China, and show that half of the patients with COVID-19
were viral positive even after resolution of their symptoms.
Cases
We studied all 16 confirmed COVID-19 patients released from the Treatment Center of
PLA General Hospital in Beijing, China, between Jan 28th - Feb 9th, 2020. All patients had
throat swabs collected on alternative days and analyzed. Patients were discharged after
their recovery and confirmation of “viral negative” status by at least two consecutive real-
time PCR(3). There was only one case of a false negative result in our study where patient
No.6 was detected negative followed by a positive detection and then two consecutive
negative tests were obtained. Travel and possible exposure history were obtained from
the patient and noted on their records. Epidemiologically, ten patients visited Wuhan after
the outbreak, and three had exposure to a known infected patient, two came in contact
with people from Wuhan while 1 had no known exposure. The basic clinical
characteristics are given in Table1. The median age was 35.5 years (range 3-68 years),
with 11/16 males. The major symptoms in these patients were fever (14/16), cough
AJRCCM Articles in Press. Published March 23, 2020 as 10.1164/rccm.202003-0524LE
Copyright © 2020 by the American Thoracic Society
Page 4 of 12
(11/16), pharyngalgia (5/16) and dyspnea (2/16). The day of onset and resolution of these
symptoms were noted.
Ground glass opacities (GGO) were observed by CT chest in both sides of the lungs in
six patients, only in the right lung in one patient. Levels of CRP and procalcitonin between
the first sample obtained at the time of hospitalization and the last sample obtained before
discharge were comparable (Table 1).
All the patients received various medical care to treat the COVID-19. Fifteen patients were
treated with alpha-interferon, along with other antiviral drugs including oseltamivir (1/16),
lopinavir/ritonavir (11/16), acyclovir (1/16), moxifloxacin (5/16), methylprednisolone
(2/16), gamma globulin (2/16), vancomycin (1/16) and meropenem (1/16) either alone or
in combination. Only one patient required respiratory support involving mechanical
ventilation.
Time kinetics of symptom onset, duration of symptoms and viral clearance is described
in Table 1. The viral detection test was performed upon clinical presentation and repeated
every other day until the patient tested negative. The negative test was confirmed again
the next day. Upon confirmation of the negative test, the patient was asked to quarantine
at home for the next two weeks with a follow-up visit to the hospital after one week to
confirm the viral negative status. The incubation periods were estimated based on the
history of the patient’s travel or potential exposure. Our data show an incubation period
of 5 days (IQR 1-6 days) among the patients (except for patient 12 who had no specific
exposure). The mean duration of symptoms was estimated to be 8 days (IQR 6.25-11.5).
Most importantly, half (8/16) of the patient remained viral positive (a surrogate marker of
AJRCCM Articles in Press. Published March 23, 2020 as 10.1164/rccm.202003-0524LE
Copyright © 2020 by the American Thoracic Society
Page 5 of 12
shedding) even after the resolution of symptoms (Median 2.5 days, range 1 to 8 days).
Some of our patients had other comorbidities, which included diabetes (2/16) and
tuberculosis (1/16), both of which did not affect the time course of the disease. Similarly,
the clinical course for the 3-year-old male did not significantly differ from the rest of the
patients.
Discussion
The current COVID-19 pandemic is the third and the most lethal outbreak of coronavirus
in the 21st century(4), where the number of infections and mortality has surpassed both
MERS and SARS infections within a short period(1, 5). Although the infection appears to
be milder with the most lethality in the older male population with pre-existing
morbidities(3, 6), it is contagious. The ability to spread may arise from the ability of the
virus to transmit from subclinical patients. Cases have been reported where a patient
could infect their close contacts even after “apparent recovery” from the infection(2). This
warrants us to investigate the “shedding window” after the clinical recovery of the patient.
In this study, we report that half of the patients continued to be viral positive even after
the resolution of symptoms up to eight days (Figure 1). The viral clearance kinetics were
similar in another study by Young et al (12 days), where all the patients survived the
infection(7). In contrast virus persisted for 20 days in other study, which had a significant
high mortality of >40%(8). This information can provide useful tool for clinicians and
policymakers to ensure that recovered patients do not spread the virus. It is important to
note that all our patients were milder infections that recovered from the disease. However,
it is currently unclear if there is a delayed viral clearance in the more vulnerable population
such as those older or have immune deficiencies or are on immunosuppressive therapies.
AJRCCM Articles in Press. Published March 23, 2020 as 10.1164/rccm.202003-0524LE
Copyright © 2020 by the American Thoracic Society
Page 6 of 12
The current data are derived from mostly young and male subjects, which is consistent
with our previous report in Beijing(9). Similar to previous study, here, we also demonstrate
another child (3-year-old male) with COVID-19 indicating the ability of this virus to infect
young children as described recently(10).
Our study is limited by the number of patients as there have been limited cases outside
the epicenter of the coronavirus outbreak that has been successfully treated so far to be
released from the hospital. Our study provides initial insights into the viral clearance
kinetics and the ability of the virus to persist even after the resolution of the for as long as
8 days, which may pose a significant challenge in controlling the spread of the disease.
However, further studies are needed to investigate if the real-time PCR-detected virus is
capable of transmission at the later stage of the disease.
Acknowledgments:
None of the co-authors report any conflict of interest. This study was supported by
funding from China 13th Five-year National Key Grant (LXX; No.2018ZX09201013),
China Scholarship Council (DC; No.201809112037), Beijing Nova Program (DC; No.
Z171100001117012), Beijing Nova Program Interdisciplinary Cooperation Project (DC;
No. Z191100001119021).
AJRCCM Articles in Press. Published March 23, 2020 as 10.1164/rccm.202003-0524LE
Copyright © 2020 by the American Thoracic Society
Page 7 of 12
Reference:
(1) World Health Organization. Coronavirus disease 2019 (COVID-19) Situation Report
– 56. 2020;2020.
(2) Rothe C, Schunk M, Sothmann P, Bretzel G, Froeschl G, Wallrauch C, Zimmer T,
Thiel V, Janke C, Guggemos W. Transmission of 2019-nCoV infection from an
asymptomatic contact in Germany. N Engl J Med 2020.
(3) Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, Ren R, Leung KSM, Lau EHY, Wong
JY, Xing X, Xiang N, Wu Y, Li C, Chen Q, Li D, Liu T, Zhao J, Li M, Tu W, Chen C, Jin
L, Yang R, Wang Q, Zhou S, Wang R, Liu H, Luo Y, Liu Y, Shao G, Li H, Tao Z, Yang
Y, Deng Z, Liu B, Ma Z, Zhang Y, Shi G, Lam TTY, Wu JTK, Gao GF, Cowling BJ, Yang
B, Leung GM, Feng Z. Early Transmission Dynamics in Wuhan, China, of Novel
Coronavirus-Infected Pneumonia. N Engl J Med 2020.
(4) Carlos WG, Dela Cruz CS, Cao B, Pasnick S, Jamil S. Novel Wuhan (2019-nCoV)
Coronavirus. American journal of respiratory and critical care medicine 2020;201:P7-P8.
(5) Su S, Wong G, Shi W, Liu J, Lai AC, Zhou J, Liu W, Bi Y, Gao GF. Epidemiology,
genetic recombination, and pathogenesis of coronaviruses. Trends Microbiol
2016;24:490-502.
(6) Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X. Clinical
features of patients infected with 2019 novel coronavirus in Wuhan, China. The Lancet
2020.
AJRCCM Articles in Press. Published March 23, 2020 as 10.1164/rccm.202003-0524LE
Copyright © 2020 by the American Thoracic Society
Page 8 of 12
(7) Young BE, Ong SWX, Kalimuddin S, Low JG, Tan SY, Loh J, Ng O, Marimuthu K,
Ang LW, Mak TM. Epidemiologic features and clinical course of patients infected with
SARS-CoV-2 in Singapore. JAMA 2020.
(8) Zhou Fei YT. Clinical course and risk factors for mortality of adult inpatients with
COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 2020.
(9) Chang D, Lin M, Wei L, Xie L, Zhu G, Cruz CSD, Sharma L. Epidemiologic and
Clinical Characteristics of Novel Coronavirus Infections Involving 13 Patients Outside
Wuhan, China. JAMA 2020.
(10) Wei M, Yuan J, Liu Y, Fu T, Yu X, Zhang Z. Novel Coronavirus Infection in
Hospitalized Infants Under 1 Year of Age in China. 2020.
AJRCCM Articles in Press. Published March 23, 2020 as 10.1164/rccm.202003-0524LE
Copyright © 2020 by the American Thoracic Society
Page 9 of 12
Figure Legends:
Fig. 1. Time kinetics of viral presence in relationship with resolution of symptoms. Day 0
is the first day of symptoms while the blue dots indicate the resolution of symptoms.
First orange box represents the day of first positive viral detection and the last orange
box indicates the day of first negative viral qPCR. F and L indicates the first and the last
time-point laboratory blood tests were conducted during the hospitalization.
AJRCCM Articles in Press. Published March 23, 2020 as 10.1164/rccm.202003-0524LE
Copyright © 2020 by the American Thoracic Society
Page 10 of 12
Table 1: Clinical Presentation and Two-time Pertinent Laboratory Findings of Patient
Population With SARS-CoV-2
Overall (n=16) Median (IQR)
Age (years) 35.5(24-43)
Days from onset of symptoms to hospital admission 3.5(3-4)
Days from onset of symptoms to positive viral test 3(2-4)
Days from onset of symptoms to virus negative 10.5(6-12)
Days from onset of symptoms to resolution of
symptoms 8(6.25-11.5)
Days of hospitalization 6.5(5.25-11)
Days from virus positive to virus negative 5.5(4-8)
Days between virus negative to resolution of
symptoms (In 8 patients who continue to be viral
positive after resolution of symptoms) 2.5(1.25,4.5) (n=8))
incubation period 5(1,6)
Fever N, (%) 14 (87.5%)
Febrile Days 6.5(5-8)
Cough N, (%) 11 (68.75%)
Productive Cough N, (%) 3 (18.75%)
Pharyngalgia N, (%) 5 (31.25%)
Dyspnea N, (%) 2 (12.5%)
Diarrhea N, (%) 1 (6.25%)
Weakness N, (%) 5 (31.25%)
Dizzy N, (%) 2 (12.5%)
Overall (n=16) Mean (SD)
During admission Before discharge
WBCs, ×109/L 5.484 (2.44) 6.331 (1.564)
Neutrophils, % 58.22 (16.30) 60.17 (14.45)
Absolute neutrophils, ×109/L 3.35 (2.60) 3.879 (1.62)
Lymphocytes, % 32.47 (15.19) 29.61 (13.68)
Absolute lymphocytes, ×109/L 1.633 (0.88) 1.807 (0.91)
Monocytes, % 7.689 (2.01) 7.359 (1.93)
Absolute monocytes, ×109/L 0.4053 (0.14) 0.4513 (0.10)
Eosinophils, % 1.347 (1.15) 2.499 (2.35)
Absolute eosinophils, ×109/L 0.08067 (0.09) 0.1693 (0.22)
Basophils, % 0.28 (0.22) 0.3853 (0.17)
Absolute basophils, ×109/L 0.01533 (0.01) 0.024 (0.01)
RBC 10^12/L 4.498 (0.94) 4.718 (0.64)
Hemoglobin, g/L 130.4 (28.9) 136.5 (18.75)
Platelets, ×109/L 162.6 (59.44) 233.5 (97.75)
AJRCCM Articles in Press. Published March 23, 2020 as 10.1164/rccm.202003-0524LE
Copyright © 2020 by the American Thoracic Society
Page 11 of 12
CRP, mg/L 24.81 (41.18) 11.52 (22.67)
PCT, ng/mL 0.6821 (2.45) 0.1325 (0.36)
Fe, μmol/L 16.24 (6.96) 15.71 (7.29)
IL-6, pg/mL 18.14 (18.83) 11.66 (17.69)
Serum Ferritin, ng/mL 341.4 (227.2) 402.4 (405.20)
Table 1: Clinical presentation and two-time pertinent laboratory findings of patient
population with COVID-19.
AJRCCM Articles in Press. Published March 23, 2020 as 10.1164/rccm.202003-0524LE
Copyright © 2020 by the American Thoracic Society
Page 12 of 12
Time kinetics of viral presence in relationship with resolution of symptoms. Day 0 is the first day of
symptoms while the blue dots indicate the resolution of symptoms. First orange box represents the day of
first positive viral detection and the last orange box indicates the day of first negative viral qPCR. F and L
indicates the first and the last time-point laboratory blood tests were conducted during the hospitalization.
2362x1429mm (72 x 72 DPI)
AJRCCM Articles in Press. Published March 23, 2020 as 10.1164/rccm.202003-0524LE
Copyright © 2020 by the American Thoracic Society
You might also like
- Why You Need To Quit Drinking Soda PersuasiveDocument3 pagesWhy You Need To Quit Drinking Soda PersuasiveEdcel Abustan100% (1)
- Smoking Stinks Lesson PlanDocument3 pagesSmoking Stinks Lesson PlanNatalia Soledad RojasNo ratings yet
- PIIS0140673620306334Document2 pagesPIIS0140673620306334Dina sofianaNo ratings yet
- Preliminary Study To Identify Severe From Moderate Cases of COVID-19 Using Combined Hematology ParametersDocument15 pagesPreliminary Study To Identify Severe From Moderate Cases of COVID-19 Using Combined Hematology Parameterstrisna amijayaNo ratings yet
- Piis0923753420363833 PDFDocument26 pagesPiis0923753420363833 PDFSyed HossainNo ratings yet
- COVID-19: Towards Controlling of A Pandemic: CommentDocument4 pagesCOVID-19: Towards Controlling of A Pandemic: CommentEugenNo ratings yet
- 10.5811@westjem.2020.6.47919 (2) 81105Document7 pages10.5811@westjem.2020.6.47919 (2) 81105Giovan GaulNo ratings yet
- Journal Pre-Proof: Journal of Clinical VirologyDocument18 pagesJournal Pre-Proof: Journal of Clinical VirologyOkki Wahyu AtikasariNo ratings yet
- Association of Procalcitonin Levels With The Progression and Prognosis of Hospitalized Patients With COVID-19Document9 pagesAssociation of Procalcitonin Levels With The Progression and Prognosis of Hospitalized Patients With COVID-19Dian Putri NingsihNo ratings yet
- Reduction and Functional Exhaustion of T Cells inDocument14 pagesReduction and Functional Exhaustion of T Cells inChavdarNo ratings yet
- Clinical Characteristics of Children With Coronavirus Disease 2019 in Hubei, ChinaDocument6 pagesClinical Characteristics of Children With Coronavirus Disease 2019 in Hubei, ChinaBobanBisercicNo ratings yet
- Rccm.202002 0445oc Clinics ChineseDocument53 pagesRccm.202002 0445oc Clinics ChineseAlex Escobar GavilánNo ratings yet
- A Novel Severity Score To Predict Inpatient Mortality in COVID 19 PatientsDocument8 pagesA Novel Severity Score To Predict Inpatient Mortality in COVID 19 PatientsanscstNo ratings yet
- 1 s2.0 S0272638620306120 ManinDocument10 pages1 s2.0 S0272638620306120 ManinrezaNo ratings yet
- Sars-Cov-2 Viral Load in Clinical Samples of Critically Ill PatientsDocument15 pagesSars-Cov-2 Viral Load in Clinical Samples of Critically Ill Patientsrahma_husna_1No ratings yet
- UK Estimates of The Severity of COVID-19 DiseaseDocument32 pagesUK Estimates of The Severity of COVID-19 DiseaseRogueNo ratings yet
- 4) Komorbid Dan Usia (Rebecca) 10.1002@art.41456Document25 pages4) Komorbid Dan Usia (Rebecca) 10.1002@art.41456Mastifa HanasitaNo ratings yet
- Clinical Characteristics of Imported Cases of COVID-19 in Jiangsu Province A Multicenter Descriptive StudyDocument23 pagesClinical Characteristics of Imported Cases of COVID-19 in Jiangsu Province A Multicenter Descriptive StudyAna Maria Romero IbagonNo ratings yet
- Journal Pre-Proof: International Journal of Infectious DiseasesDocument18 pagesJournal Pre-Proof: International Journal of Infectious DiseasesKenya EspinozaNo ratings yet
- Coagulation Disorder PDFDocument4 pagesCoagulation Disorder PDFBrownell TraciNo ratings yet
- 1 LRDocument12 pages1 LRaoonNo ratings yet
- A Case Series Describing The Epidemiology and Clinical Characteristics of COVID-19 Infection in Jilin ProvinceDocument4 pagesA Case Series Describing The Epidemiology and Clinical Characteristics of COVID-19 Infection in Jilin Provinceabeer alrofaeyNo ratings yet
- Asymptomatic and Human To Human Transmission of SARS COV 2Document3 pagesAsymptomatic and Human To Human Transmission of SARS COV 2belinda thaniaNo ratings yet
- Covid-19 in Critically Ill Patients in The Seattle Region - Case SeriesDocument18 pagesCovid-19 in Critically Ill Patients in The Seattle Region - Case SeriesZelgi PutraNo ratings yet
- Journal Pre-Proof: Journal of Cardiothoracic and Vascular AnesthesiaDocument21 pagesJournal Pre-Proof: Journal of Cardiothoracic and Vascular AnesthesiaJuan Esteban Paez MolinaNo ratings yet
- Covid Er ArticleDocument6 pagesCovid Er ArticleReeb BukhariNo ratings yet
- Pathological Evidence of Pulmonary Thrombotic Phenomena in Severe COVID 19Document5 pagesPathological Evidence of Pulmonary Thrombotic Phenomena in Severe COVID 19Victor AugustoNo ratings yet
- Coagulation Disorders in Coronavirus Infected PatientsDocument6 pagesCoagulation Disorders in Coronavirus Infected PatientsQuang TrầnNo ratings yet
- Journal Pre-Proof: International Journal of Infectious DiseasesDocument14 pagesJournal Pre-Proof: International Journal of Infectious DiseasesKenya EspinozaNo ratings yet
- Clinical Characteristics and Durations of Hospitalized Patients With COVID-19 in BeijingDocument18 pagesClinical Characteristics and Durations of Hospitalized Patients With COVID-19 in BeijingTOMMYNo ratings yet
- An Epidemiological Study of Laboratory Confirmed COVID-19 Cases Admitted in Dhaka Medical College HospitalDocument7 pagesAn Epidemiological Study of Laboratory Confirmed COVID-19 Cases Admitted in Dhaka Medical College HospitalPranto BaraiNo ratings yet
- Seminario CovidDocument17 pagesSeminario CovidGonzalo Ccahuana YanqueNo ratings yet
- Multisystem Inflammatory Syndrome in Children and Adolescents With COVID-19Document3 pagesMultisystem Inflammatory Syndrome in Children and Adolescents With COVID-19Maria BriceñoNo ratings yet
- Jurnal Chen Et AlDocument31 pagesJurnal Chen Et AlUtami MNo ratings yet
- Fimmu 11 00827Document7 pagesFimmu 11 00827yangxiao9511No ratings yet
- Epidemiological and Clinical Characteristics of 671 COVID-19 Patients in Henan Province, ChinaDocument11 pagesEpidemiological and Clinical Characteristics of 671 COVID-19 Patients in Henan Province, ChinaOrlando JúniorNo ratings yet
- Title Authors:: Snarain@northwell - EduDocument17 pagesTitle Authors:: Snarain@northwell - EduPaola A. Zeña HuancasNo ratings yet
- Clinical Immunology: Koichi Yuki, Miho Fujiogi, Sophia Koutsogiannaki TDocument7 pagesClinical Immunology: Koichi Yuki, Miho Fujiogi, Sophia Koutsogiannaki TishmahNo ratings yet
- Coccidioidomycosis in Patients With HIV-1 Infection in The Era of Potent Antiretroviral TherapyDocument7 pagesCoccidioidomycosis in Patients With HIV-1 Infection in The Era of Potent Antiretroviral Therapydata32No ratings yet
- Ciaa242 2 PDFDocument8 pagesCiaa242 2 PDFHesbon MomanyiNo ratings yet
- Estudo DiabetesDocument9 pagesEstudo DiabetesFulano de TalNo ratings yet
- Analysis Clinical Features of COVID-19 Infection IDocument6 pagesAnalysis Clinical Features of COVID-19 Infection Imohamed atefNo ratings yet
- Ciaa 414Document7 pagesCiaa 414Kev Jose Ruiz RojasNo ratings yet
- Us Chest CT Findings in Coronavirus Disease PDFDocument7 pagesUs Chest CT Findings in Coronavirus Disease PDFRomit JainNo ratings yet
- Clinical Features of Patients Infected With 2019 Novel Coronavirus in Wuhan China Chaolin Huang 2 Full Chapter PDFDocument34 pagesClinical Features of Patients Infected With 2019 Novel Coronavirus in Wuhan China Chaolin Huang 2 Full Chapter PDFhassidcaraza100% (8)
- Dong J - Prediction For Progression Risk in Patients With COVID - 19 Pneumonia The CALL ScoreDocument7 pagesDong J - Prediction For Progression Risk in Patients With COVID - 19 Pneumonia The CALL ScoreMercedes Ah CardenasNo ratings yet
- Aksungar 2007Document10 pagesAksungar 2007twarrenNo ratings yet
- PIIS0140673622003270Document7 pagesPIIS0140673622003270chaivat kNo ratings yet
- Clinical Features of Patients Infected With 2019 Novel Coronavirus in Wuhan China Chaolin Huang Full Chapter PDFDocument34 pagesClinical Features of Patients Infected With 2019 Novel Coronavirus in Wuhan China Chaolin Huang Full Chapter PDFhassidcaraza100% (8)
- Pages From WhuDocument2 pagesPages From Whurahat879No ratings yet
- Coronavirus Disease 2019 (COVID-19) A Perspective From ChinaDocument29 pagesCoronavirus Disease 2019 (COVID-19) A Perspective From ChinabackupNo ratings yet
- CCDCW220132Document7 pagesCCDCW220132Lin ZhouNo ratings yet
- Preprint corticoidesNeuminiaCOVIDDocument16 pagesPreprint corticoidesNeuminiaCOVIDJorgelina BernetNo ratings yet
- Journal Pre-Proof: Clinical ImmunologyDocument23 pagesJournal Pre-Proof: Clinical ImmunologypqrsehunNo ratings yet
- Clinical Characteristics of Covid-19 in China: CorrespondenceDocument3 pagesClinical Characteristics of Covid-19 in China: CorrespondenceSofia VidalNo ratings yet
- New Insights of Emerging Sars-Cov-2: Epidemiology, Etiology, Clinical Features, Clinical Treatment, and PreventionDocument22 pagesNew Insights of Emerging Sars-Cov-2: Epidemiology, Etiology, Clinical Features, Clinical Treatment, and PreventionWendi IochNo ratings yet
- Liu2020 Article ClinicalAndBiochemicalIndexesFDocument11 pagesLiu2020 Article ClinicalAndBiochemicalIndexesFGabriel Ibarra TrujilloNo ratings yet
- Gender Differences in Patients With COVID-19: Focus On Severity and MortalityDocument18 pagesGender Differences in Patients With COVID-19: Focus On Severity and MortalityYogi drNo ratings yet
- Analysis of Mortality in Covid 19 Patients - A Study in A District Covid Hospital in Andhra Pradesh During The First WaveDocument6 pagesAnalysis of Mortality in Covid 19 Patients - A Study in A District Covid Hospital in Andhra Pradesh During The First WaveIJAR JOURNALNo ratings yet
- Dengue How ClassifyDocument5 pagesDengue How ClassifyErlin IrawatiNo ratings yet
- COVID-19 Mortality Review in Malaysia & Updates on Clinical Management of COVID-19From EverandCOVID-19 Mortality Review in Malaysia & Updates on Clinical Management of COVID-19No ratings yet
- Facing COVID-19 with the benefits of medical cannabisFrom EverandFacing COVID-19 with the benefits of medical cannabisNo ratings yet
- Aluminium Glass Shutter Profile 2Document2 pagesAluminium Glass Shutter Profile 2Bharat GouripurNo ratings yet
- 1Document40 pages1Bharat GouripurNo ratings yet
- GROHE Specification Sheet 39328000Document2 pagesGROHE Specification Sheet 39328000Bharat GouripurNo ratings yet
- MT Handbook GrainDocument250 pagesMT Handbook GrainBharat GouripurNo ratings yet
- Enrolment Numbers 2018-19 BatchDocument2 pagesEnrolment Numbers 2018-19 BatchBharat GouripurNo ratings yet
- Practice F.stone-Walls FinalDocument5 pagesPractice F.stone-Walls FinalBharat GouripurNo ratings yet
- RESUME and Work Experience 080723Document9 pagesRESUME and Work Experience 080723Bharat GouripurNo ratings yet
- Eoi Extension NoticeDocument1 pageEoi Extension NoticeBharat GouripurNo ratings yet
- Course PendingDocument1 pageCourse PendingBharat GouripurNo ratings yet
- Eoi Notice Dated 27.07.2023Document6 pagesEoi Notice Dated 27.07.2023Bharat GouripurNo ratings yet
- 11 - Chapter 2Document37 pages11 - Chapter 2Bharat GouripurNo ratings yet
- New Doc 2020-04-12 14.01.13Document1 pageNew Doc 2020-04-12 14.01.13Bharat GouripurNo ratings yet
- Avalanche 2020Document1 pageAvalanche 2020Bharat GouripurNo ratings yet
- Parent LetterDocument38 pagesParent LetterBharat GouripurNo ratings yet
- Class Section WiseDocument1 pageClass Section WiseBharat GouripurNo ratings yet
- Lec 1Document14 pagesLec 1Bharat GouripurNo ratings yet
- Class - Section - Wise - ATSEC ADocument1 pageClass - Section - Wise - ATSEC ABharat GouripurNo ratings yet
- CIE - MIS Architecture Architecture Semester6 SECBDocument2 pagesCIE - MIS Architecture Architecture Semester6 SECBBharat GouripurNo ratings yet
- CIE - MIS Architecture Architecture Semester2 SECBDocument1 pageCIE - MIS Architecture Architecture Semester2 SECBBharat GouripurNo ratings yet
- School RequirementsDocument3 pagesSchool RequirementsBharat GouripurNo ratings yet
- Sheet 7Document3 pagesSheet 7Bharat GouripurNo ratings yet
- CIE - MIS Architecture Architecture Semester6 SECADocument2 pagesCIE - MIS Architecture Architecture Semester6 SECABharat GouripurNo ratings yet
- Quiz GuideDocument18 pagesQuiz GuideBharat GouripurNo ratings yet
- CIE - MIS Architecture Architecture Semester6 SECBDocument2 pagesCIE - MIS Architecture Architecture Semester6 SECBBharat GouripurNo ratings yet
- BrochureDocument44 pagesBrochureBharat GouripurNo ratings yet
- Auditorium PlanDocument1 pageAuditorium PlanBharat GouripurNo ratings yet
- LibraryDocument5 pagesLibraryBharat GouripurNo ratings yet
- Lec 2Document17 pagesLec 2Bharat GouripurNo ratings yet
- Sheet 8Document8 pagesSheet 8Bharat GouripurNo ratings yet
- Sheet 6Document4 pagesSheet 6Bharat GouripurNo ratings yet
- SITXFSA001 Student Assessment TasksDocument24 pagesSITXFSA001 Student Assessment TasksMukta AktherNo ratings yet
- Dermatology QuestionsDocument3 pagesDermatology QuestionsMuziki Wa KiafrikaNo ratings yet
- Diseases of The NoseDocument3 pagesDiseases of The NoseVannero SembranoNo ratings yet
- Wastewater Characteristics and Effluent Quality ParametersDocument5 pagesWastewater Characteristics and Effluent Quality ParametersVincent SitholeNo ratings yet
- Trinity United Church of Christ BulletinDocument28 pagesTrinity United Church of Christ BulletinWorlee GloverNo ratings yet
- Science Olympiad InvasivesDocument2 pagesScience Olympiad InvasivesYue ZhangNo ratings yet
- Valproic Acid Drug Study PDFDocument4 pagesValproic Acid Drug Study PDFLiza Marie IgnacioNo ratings yet
- Covid Self Declaration Form Visitor PDFDocument3 pagesCovid Self Declaration Form Visitor PDFTipu BabuNo ratings yet
- Chang Et - Al PDFDocument10 pagesChang Et - Al PDFAggy AlbotraNo ratings yet
- 02/27/09 - The Stanford Daily (PDF)Document8 pages02/27/09 - The Stanford Daily (PDF)The Stanford DailyNo ratings yet
- Solid Dosage Forms in Unani System of Medicine AnDocument7 pagesSolid Dosage Forms in Unani System of Medicine AnSiddharth JainNo ratings yet
- mg359 All PDFDocument24 pagesmg359 All PDFsyedsrahmanNo ratings yet
- Men's Treatment GriffinDocument68 pagesMen's Treatment GriffintadcpNo ratings yet
- Mina Drug StudyDocument7 pagesMina Drug StudyChi Chaw Giselle HilarioNo ratings yet
- Family 2Document13 pagesFamily 2Saloni SharmaNo ratings yet
- Latihan Soal Literasi Bahasa Inggris 1Document9 pagesLatihan Soal Literasi Bahasa Inggris 1Daffa AryaputraNo ratings yet
- L A Level Biology MS Jan 06Document180 pagesL A Level Biology MS Jan 06zetsubou-chanNo ratings yet
- Gmail Maxicare EReady Advance PDFDocument7 pagesGmail Maxicare EReady Advance PDFShirelyNo ratings yet
- Family Nursing Care PlanDocument7 pagesFamily Nursing Care PlanMarilou Jumalon MontefalconNo ratings yet
- Adolescent HealthDocument47 pagesAdolescent HealthsushmaNo ratings yet
- Volume 42, Issue 34 - August 26, 2011Document56 pagesVolume 42, Issue 34 - August 26, 2011BladeNo ratings yet
- Actualizacion de La PreeclampsiaDocument8 pagesActualizacion de La PreeclampsiaPierina VeramatosNo ratings yet
- DHS CFS 600 Certificate of Child Examination Form IL444-4737Document2 pagesDHS CFS 600 Certificate of Child Examination Form IL444-4737ArtueroNo ratings yet
- RADIOLOGY 1.6 Introduction To MammographyDocument9 pagesRADIOLOGY 1.6 Introduction To MammographyZazaNo ratings yet
- Science As Proof of The Bible.Document3 pagesScience As Proof of The Bible.AndrewNo ratings yet
- Lorma Colleges College of Physical and Respiratory TherapyDocument33 pagesLorma Colleges College of Physical and Respiratory TherapyAnab Mohamed Elhassan Abbas AlnowNo ratings yet
- Best Practice Workbook - Bipolar Disorder-Yong Xiang YiDocument45 pagesBest Practice Workbook - Bipolar Disorder-Yong Xiang YiJuraidahMohdNooh100% (1)
- Communicable Disease ControlDocument52 pagesCommunicable Disease ControlNidonama E. KabmatNo ratings yet