Professional Documents
Culture Documents
PIIS000293781502102X
PIIS000293781502102X
Uploaded by
Yosep SutandarCopyright:
Available Formats
You might also like
- Zootechnic Practice QuestionsDocument21 pagesZootechnic Practice QuestionsLaureece Salm ApduhanNo ratings yet
- MSBTE Diploma Project Report TempletDocument8 pagesMSBTE Diploma Project Report Templet53 Hirole Aadesh100% (5)
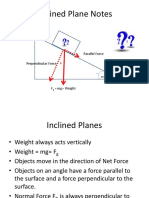
- Inclined Planes and Forces Notes PDFDocument19 pagesInclined Planes and Forces Notes PDFJohnLesterLaurelNo ratings yet
- Lee Et Al-2016-BJOG An International Journal of Obstetrics & GynaecologyDocument8 pagesLee Et Al-2016-BJOG An International Journal of Obstetrics & GynaecologyDhia UlfajriNo ratings yet
- Rotura Prematura de Membranas y ObesidadDocument5 pagesRotura Prematura de Membranas y ObesidadLaura AgudeloNo ratings yet
- Effects of Prepregnancy Dietary Patterns On Infant Birth Weight A Prospective Cohort StudyDocument11 pagesEffects of Prepregnancy Dietary Patterns On Infant Birth Weight A Prospective Cohort StudyLola SantiaNo ratings yet
- Poster Session I: Perinatal Outcome of Women With Epilepsy: Results From A Population-Based Cohort StudyDocument1 pagePoster Session I: Perinatal Outcome of Women With Epilepsy: Results From A Population-Based Cohort StudyasfwegereNo ratings yet
- Risk Factors For Excess Weight Loss and Hypernatremia in Exclusively Breast-Fed InfantsDocument6 pagesRisk Factors For Excess Weight Loss and Hypernatremia in Exclusively Breast-Fed InfantsHariz Ghulam RamadhanNo ratings yet
- Natural History of Fetal Position During Pregnancy.11Document6 pagesNatural History of Fetal Position During Pregnancy.11PutriNo ratings yet
- Ijwh 5 501Document7 pagesIjwh 5 501MarianaafiatiNo ratings yet
- Association Between Maternal Sleep Practices and Late Stillbirth - Findings From A Stillbirth Case-Control StudyDocument9 pagesAssociation Between Maternal Sleep Practices and Late Stillbirth - Findings From A Stillbirth Case-Control StudyWinniaTanelyNo ratings yet
- AmericanDocument1 pageAmericanAdzkia_ZRNo ratings yet
- Geist 2006Document5 pagesGeist 2006Marifer EstradaNo ratings yet
- Hersh 2019Document10 pagesHersh 2019RosiNo ratings yet
- ContentServer AspDocument7 pagesContentServer AspScribdNo ratings yet
- Cervical EncerclageDocument25 pagesCervical EncerclageKartheek VarmaNo ratings yet
- Merced 2019Document14 pagesMerced 2019Vanessa CarinoNo ratings yet
- Poster Session II: ConclusionDocument2 pagesPoster Session II: ConclusionFahmi Nur SuwandiNo ratings yet
- Ectopic Pregnancy: A ReviewDocument13 pagesEctopic Pregnancy: A ReviewDinorah MarcelaNo ratings yet
- Alustokat 2014Document8 pagesAlustokat 2014Syienthia RahmatikaNo ratings yet
- Intrauterine Growth Restriction: Diagnosis and ManagementDocument7 pagesIntrauterine Growth Restriction: Diagnosis and ManagementLarasati Gilang Fuzi AstutiNo ratings yet
- The Preterm Labor Index and Fetal Fibronectin For.24Document6 pagesThe Preterm Labor Index and Fetal Fibronectin For.24bombonlrNo ratings yet
- The Impact of Fetal Growth Restriction On Latency in The Setting of Expectant Management of PreeclampsiaDocument7 pagesThe Impact of Fetal Growth Restriction On Latency in The Setting of Expectant Management of PreeclampsiagusriaNo ratings yet
- Anomalía Uterinas Congénitas y Resultados Adversos en El EmbarazoDocument5 pagesAnomalía Uterinas Congénitas y Resultados Adversos en El EmbarazoAlexiis CabascangoNo ratings yet
- Normograma Perdida de PesoDocument10 pagesNormograma Perdida de PesoUTI NeonatologíaNo ratings yet
- Failed of LaborDocument12 pagesFailed of LaborStéphanieNo ratings yet
- Precision Medicine Personalized, Problematic, And.7Document3 pagesPrecision Medicine Personalized, Problematic, And.7Ben AllenNo ratings yet
- 1 s2.0 S0301211521007569Document1 page1 s2.0 S0301211521007569erikglu2796No ratings yet
- 2017 Julio Comunidad y SaludDocument3 pages2017 Julio Comunidad y SaludremediosisabelNo ratings yet
- Pregnancy Outcome in POCSDocument6 pagesPregnancy Outcome in POCSMeera Al AliNo ratings yet
- Ijnh 09-JS-2023-13 20231118 V2Document9 pagesIjnh 09-JS-2023-13 20231118 V2Apacetech IluvbNo ratings yet
- Effects of Anti M Llerian Hormone and Follicle Sti - 2014 - Taiwanese Journal ofDocument4 pagesEffects of Anti M Llerian Hormone and Follicle Sti - 2014 - Taiwanese Journal ofSami KahtaniNo ratings yet
- Exercise During Pregnancy Protects Against Hypertension and Macrosomia: Randomized Clinical TrialDocument8 pagesExercise During Pregnancy Protects Against Hypertension and Macrosomia: Randomized Clinical TrialDaniela VenegasNo ratings yet
- Iams 2011Document6 pagesIams 20118jxfv2gc5tNo ratings yet
- Research: Outcomes of Elective Induction of Labour Compared With Expectant Management: Population Based StudyDocument13 pagesResearch: Outcomes of Elective Induction of Labour Compared With Expectant Management: Population Based StudyAndinNo ratings yet
- The NeoUpdates - DecDocument7 pagesThe NeoUpdates - DecDr Satish MishraNo ratings yet
- Neurodevelopmental Outcomes of Extremely Preterm InfantsDocument10 pagesNeurodevelopmental Outcomes of Extremely Preterm Infantsmarta.sanz.alvarezNo ratings yet
- Estimated Fetal Weight: Comparison of Clinical Versus Ultrasound EstimateDocument6 pagesEstimated Fetal Weight: Comparison of Clinical Versus Ultrasound EstimateNadia AyuningtiasNo ratings yet
- Maternal Demography and Neonatal Outcomes in Term Pre Labour Rupture of Membranes Versus Spontaneous Labour Preceding Ruptured Membranes in Lagos, Nigeria A Comparative StudyDocument6 pagesMaternal Demography and Neonatal Outcomes in Term Pre Labour Rupture of Membranes Versus Spontaneous Labour Preceding Ruptured Membranes in Lagos, Nigeria A Comparative StudyInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Mihu 2015Document7 pagesMihu 2015Nuryasni NuryasniNo ratings yet
- Anemia MaternityDocument5 pagesAnemia MaternityBonaventura Ahardiansyah BoNo ratings yet
- Association Between Early Amniotomy in Labour Induction and Severe Maternal and Neonatal MorbidityDocument7 pagesAssociation Between Early Amniotomy in Labour Induction and Severe Maternal and Neonatal MorbidityLizbeth RomeroNo ratings yet
- Fetal Movements As A Predictor of HealthDocument8 pagesFetal Movements As A Predictor of HealthWordtreader PtNo ratings yet
- Pregnancy Complications and Outcomes in Women With Epilepsy: Mirzaei Fatemeh, Ebrahimi B. NazaninDocument5 pagesPregnancy Complications and Outcomes in Women With Epilepsy: Mirzaei Fatemeh, Ebrahimi B. NazaninMentari SetiawatiNo ratings yet
- Taiwanese Journal of Obstetrics & Gynecology: Dittakarn Boriboonhirunsarn, Rungnapa WaiyanikornDocument4 pagesTaiwanese Journal of Obstetrics & Gynecology: Dittakarn Boriboonhirunsarn, Rungnapa WaiyanikornirmaNo ratings yet
- Articulo EndometriosisDocument7 pagesArticulo EndometriosisMaIt VeFloNo ratings yet
- Poster Session I: Study DesignDocument1 pagePoster Session I: Study DesignRegina PizanNo ratings yet
- Hipoglicemia 4Document2 pagesHipoglicemia 4juanNo ratings yet
- Jurnal ObsgynDocument11 pagesJurnal ObsgynVivie Tirany SoediroNo ratings yet
- E057981 FullDocument11 pagesE057981 FulledmondNo ratings yet
- Severity of Anemia During Pregnancy and Adverse Maternal and Fetal OutcomesDocument13 pagesSeverity of Anemia During Pregnancy and Adverse Maternal and Fetal OutcomesIlda IldaNo ratings yet
- Exploring The Relationship Between Preterm Placental Calcification and Adverse Maternal and Fetal OutcomeDocument7 pagesExploring The Relationship Between Preterm Placental Calcification and Adverse Maternal and Fetal OutcomeMaulida HalimahNo ratings yet
- Jurnal 2 MisoprostolDocument17 pagesJurnal 2 MisoprostolaldoNo ratings yet
- Duan 2010Document3 pagesDuan 2010ShirleyNo ratings yet
- A Randomized Trial of Synthetic Osmotic Cervical D - 2022 - American Journal ofDocument20 pagesA Randomized Trial of Synthetic Osmotic Cervical D - 2022 - American Journal ofLuis GómezNo ratings yet
- Induction of LaborDocument8 pagesInduction of LaborwiwimbakNo ratings yet
- Predictors of Cephalopelvic Disproportion in Labour A Tertiary Hospital in Bayelsa State, NigeriaDocument7 pagesPredictors of Cephalopelvic Disproportion in Labour A Tertiary Hospital in Bayelsa State, NigeriaAndri Muhrim SiddiqNo ratings yet
- PCOS and IVF Success Rates in Melati Clinic Harapan Kita HospitalDocument1 pagePCOS and IVF Success Rates in Melati Clinic Harapan Kita HospitalCindikia Ayu SNo ratings yet
- To Compare The Safety and Efficacy of Manual Vacuum Aspiration With Misoprostol (ST Mom) 600mg in Incomplete MiscarriageDocument4 pagesTo Compare The Safety and Efficacy of Manual Vacuum Aspiration With Misoprostol (ST Mom) 600mg in Incomplete MiscarriageHassan KhanNo ratings yet
- Original Research: Screening Extremely Obese Pregnant Women For Obstructive Sleep ApneaDocument18 pagesOriginal Research: Screening Extremely Obese Pregnant Women For Obstructive Sleep ApneaappNo ratings yet
- The Interactive Effect of Prepregnancy Overweight/Obesity and Isolated Maternal Hypothyroxinemia On MacrosomiaDocument8 pagesThe Interactive Effect of Prepregnancy Overweight/Obesity and Isolated Maternal Hypothyroxinemia On MacrosomiaAndres GallegosNo ratings yet
- Wu 2020 Oi 200461Document12 pagesWu 2020 Oi 200461Antje IrmellaNo ratings yet
- Diminished Ovarian Reserve and Assisted Reproductive Technologies: Current Research and Clinical ManagementFrom EverandDiminished Ovarian Reserve and Assisted Reproductive Technologies: Current Research and Clinical ManagementOrhan BukulmezNo ratings yet
- Routine Firsttrimester Ultrasound Screening Using A Standardized Anatomical ProtocolDocument15 pagesRoutine Firsttrimester Ultrasound Screening Using A Standardized Anatomical ProtocolYosep SutandarNo ratings yet
- Physiology of Amniotic Fluid Volume RegulationDocument8 pagesPhysiology of Amniotic Fluid Volume RegulationYosep SutandarNo ratings yet
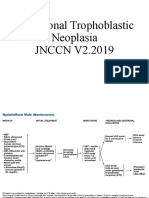
- Gestational Trophoblastic NeoplasiaDocument14 pagesGestational Trophoblastic NeoplasiaYosep SutandarNo ratings yet
- Ferra RettiDocument51 pagesFerra RettiYosep SutandarNo ratings yet
- Mao2014 Article ImagingOfPelvicLymphNodesDocument13 pagesMao2014 Article ImagingOfPelvicLymphNodesYosep SutandarNo ratings yet
- Ovarian Reserve Testing: A User's Guide: Expert ReviewsDocument12 pagesOvarian Reserve Testing: A User's Guide: Expert ReviewsYosep SutandarNo ratings yet
- Changes in The Sexual Function During Pregnancy: Aim. MethodsDocument10 pagesChanges in The Sexual Function During Pregnancy: Aim. MethodsYosep SutandarNo ratings yet
- Acog Committee Opinion: Dysmenorrhea and Endometriosis in The AdolescentDocument10 pagesAcog Committee Opinion: Dysmenorrhea and Endometriosis in The AdolescentYosep SutandarNo ratings yet
- Eng - PDF JsessionidDocument34 pagesEng - PDF JsessionidYosep SutandarNo ratings yet
- Pi Is 0884217517304100Document3 pagesPi Is 0884217517304100Yosep SutandarNo ratings yet
- Enteral NutritionDocument73 pagesEnteral NutritionYosep Sutandar100% (1)
- Practice Bullet In: Emergency ContraceptionDocument11 pagesPractice Bullet In: Emergency ContraceptionYosep SutandarNo ratings yet
- Clue CellsDocument10 pagesClue CellsYosep SutandarNo ratings yet
- 7 Meaning - Sri StutiDocument24 pages7 Meaning - Sri StutiLeela KNo ratings yet
- Overview Six Sigma PhasesDocument3 pagesOverview Six Sigma Phaseshans_106No ratings yet
- Anatomy and Physiology of Salivary GlandsDocument55 pagesAnatomy and Physiology of Salivary GlandsSuprit SnNo ratings yet
- Flangeless Horseshoe Maxillary Complete Denture - A Prosthodontic Solution To Maxillary ToriDocument3 pagesFlangeless Horseshoe Maxillary Complete Denture - A Prosthodontic Solution To Maxillary ToriMohammad Abdulmon’emNo ratings yet
- CONTEMPT OF COURT JurisprudenceDocument10 pagesCONTEMPT OF COURT Jurisprudencenxfkfbvjw7No ratings yet
- 14 Best Hypoallergenic Cat BreedDocument11 pages14 Best Hypoallergenic Cat BreedJunna May AradoNo ratings yet
- INTRAPERSONALCOMMUNICATIONASFOUNDATIONFORPERSONALBRANDING BerylEhondor PDFDocument12 pagesINTRAPERSONALCOMMUNICATIONASFOUNDATIONFORPERSONALBRANDING BerylEhondor PDFDexter JoveloNo ratings yet
- 1st Quarter Exam in Mapeh 10Document4 pages1st Quarter Exam in Mapeh 10Dhan Mark Barlintangco100% (1)
- Loudspeakers Coverage AnglesDocument0 pagesLoudspeakers Coverage AnglesAnthony HubbardNo ratings yet
- Business Ethics and CSR Individual Assignment 1 Concept PaperDocument9 pagesBusiness Ethics and CSR Individual Assignment 1 Concept PaperZeeshan KhanNo ratings yet
- Syllabus: Subject: Software EngineeringDocument4 pagesSyllabus: Subject: Software EngineeringTuyên Kiều VănNo ratings yet
- The ABCs of DR Desmond Ford S Theology W H JohnsDocument16 pagesThe ABCs of DR Desmond Ford S Theology W H JohnsBogdan PlaticaNo ratings yet
- HindustaniMelodic SQPDocument4 pagesHindustaniMelodic SQPAkshit ChauhanNo ratings yet
- Flight1 441 Conquest TutorialDocument10 pagesFlight1 441 Conquest TutorialJosé A. Montiel QuirósNo ratings yet
- International Human Resource ManagementDocument20 pagesInternational Human Resource ManagementAziz UllahNo ratings yet
- Extended Essay IB DiplomaDocument20 pagesExtended Essay IB Diplomasol GonzalezNo ratings yet
- Criminology Comprehensive Examination Set BDocument9 pagesCriminology Comprehensive Examination Set BChristine Anne Ganio ValenciaNo ratings yet
- Crim Justice System PDFDocument3 pagesCrim Justice System PDFKing Monteclaro MonterealNo ratings yet
- Housing First Fact SheetDocument2 pagesHousing First Fact SheetstprepsNo ratings yet
- Arshad CVDocument4 pagesArshad CVAli BaseejiNo ratings yet
- Assignment Brief Unit 47 QCFDocument14 pagesAssignment Brief Unit 47 QCFAlamzeb KhanNo ratings yet
- Republic Vs LedesmaDocument2 pagesRepublic Vs LedesmaestvanguardiaNo ratings yet
- Addition Word ProblemsDocument10 pagesAddition Word ProblemsmarycperezNo ratings yet
- A Freemason's 33rd Degree InitiationDocument12 pagesA Freemason's 33rd Degree InitiationMax SchmidtNo ratings yet
- Ioug Selectjournal 2014q1cDocument8 pagesIoug Selectjournal 2014q1carunjacNo ratings yet
- Topology PaperDocument9 pagesTopology PaperNestor Bong Bordaje NemeñoNo ratings yet
PIIS000293781502102X
PIIS000293781502102X
Uploaded by
Yosep SutandarOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
PIIS000293781502102X
PIIS000293781502102X
Uploaded by
Yosep SutandarCopyright:
Available Formats
ajog.
org Poster Session V
based on the 2003 version of the Birth Certificate, it can be currently in the active management group had a higher rate of fever of the
used by any state. newborn after delivery than those in the conservative (15.2% vs
27.9%, p¼0.03).No difference in maternal and neonatal complica-
tions were documented between the study groups.
CONCLUSION: Women with isolated oligohydramnios had a higher
rate of induction of labor compared with women with normal
amount of amniotic fluid. There was a higher rate of caesarian
sections in the conservative management group compared to the
active management, especially because non-vertex presentation.
Although the active management of isolated oligohydramnios during
the late preterm was associated with a lower rate of cesarean de-
liveries, this is mainly attributed to the higher proportion of mal
presentation in this group that would have been delivered by ce-
sarean anyway. Moreover, induction of labor comes with a price of
increased neonatal fever, suggesting that the beneficial effect of in-
duction of labor in women with isolated oligohydramnios at the late
preterm period should be reconsidered.
750 The effects of maternal obesity on fetal and neonatal
outcomes among those born large for gestational age
Ruofan Yao1, Bo Y. Park2, Aaron B. Caughey3
1
University of Maryland Medical Center, Baltimore, MD, 2Johns Hopkins
University, School of Public Health, Baltimore, MD, 3Oregon Health &
Science University, Portland, OR
OBJECTIVE: It is unclear if the association between maternal obesity
and higher birth weight is physiological or pathological. The purpose
of this study is to determine the differences in fetal and neonatal
outcomes among large for gestational age(LGA) births in obese
women compared to normal weight women.
STUDY DESIGN: This was a retrospective cohort study of all non-
anomalous singleton neonates born in Texas from 2006-2011.
Analysis was limited to births between 34 and 42 weeks gestation
749 How to manage isolated oligohydramnios at late with birth weight above the 90th percentile among this cohort.
preterm? Lessons from a population based study Results were stratified by maternal pre-pregnancy BMI, classified
Offer Erez1, Noa Brzezinski Sinai1, Tal Rafaeli-Yehudai1, according to WHO guideline. Neonatal and fetal outcomes of in-
Majdi Imterat1, Salvatore Andrea Mastrolia2, terest included stillbirth, neonatal death, neonatal intensive care
Maayan Yitshak-Sade1, Moshe Stavsky1 unit(NICU) admission and low 5 minute APGAR scores. These
1
Soroka University Medicial Center, Beer Sheva, Israel, 2Azienda Ospedaliero- outcomes were analyzed for births above the 90th, 95th and 97th
Universitaria Policlinico di Bari, School of Medicine, University of Bari “Aldo percentile. Multivariable logistic regression analysis was performed
Moro”, Bari, Italy to estimate the association between maternal pre-pregnancy obesity
OBJECTIVE: The management of isolated oligohydramnios occurring and fetal/neonatal outcomes compared to normal weight controls
at 34-36.6 weeks of gestation is under debate. The objective of this controlling for potential confounding variables.
study was to determine the maternal and neonatal outcome resulting RESULTS: After exclusion, 236,017 births were analyzed. The preva-
from induction of labor vs. expectant management in women with lence of LGA births among obese women (15.6%) was higher than
isolated oligohydramnios at late preterm. normal weight controls (8.5%, p<0.001). The rates of stillbirth
STUDY DESIGN: This retrospective population based cohort study among normal weight women for birth weight above 90th, 95th and
included 3 groups: 1) Conservative management-women with iso- 97th percentile were 4.8, 8.8 and 14.0 per 1,000 births respectively. In
lated oligohydramnios that delivered spontaneously (n¼146); 2) comparison the rates among obese women were 5.2(OR:1.11
active management-women with isolated oligohydramnios who [.97,1.26]), 10.3(OR:.95[.83,1.09]) and 14.9(OR: .87[.76, .99]). The
underwent induction of labor (n¼ 114); 3) Control group-women rates of neonatal deaths among normal weight women were 3.3, 3.7,
with normal amount of amniotic fluid who delivered at 34-36.6 and 3.6 per 1,000 births respectively. In comparison the rates among
weeks (n¼9,225). obese women were 3.0(OR: .91[.76,1.08]), 2.8(OR: .74[.56, .94]),
RESULTS: The 9,485 women had 11,089 births divided into 146 in the and 2.9(OR: .81[.61,1.07]) respectively. The rates of NICU admis-
conservative management group, 115 in the active management sion and low APGAR score were significantly higher among obese
group, and 10828 in the control group. The rate of inducing labor pregnancies compared to normal weight controls (figure 1).
was higher in the oligohydramnios group compared to the control CONCLUSION: Maternal obesity is not associated with increased risks
group (75%, 32.6% respectively). The rate of caesarian sections was of stillbirth or neonatal death among infants born LGA. Compared
higher in the conservative than the active management groups at 35 to normal weight controls, maternal obesity is associated with a
weeks (57.5% vs. 18.2%, p<0.001) and 36 weeks (52.0% vs. 3.0%, P reduction in stillbirth among neonates with birth weight greater than
<0.001) of gestation. The main indication for caesarean section was 97th percentile, and a reduction in neonatal death among neonates
mal presentation of the fetus (60.6% vs 22.2%, p<0.001). Neonates with birth weight greater than 95th percentile.
Supplement to JANUARY 2016 American Journal of Obstetrics & Gynecology S393
You might also like
- Zootechnic Practice QuestionsDocument21 pagesZootechnic Practice QuestionsLaureece Salm ApduhanNo ratings yet
- MSBTE Diploma Project Report TempletDocument8 pagesMSBTE Diploma Project Report Templet53 Hirole Aadesh100% (5)
- Inclined Planes and Forces Notes PDFDocument19 pagesInclined Planes and Forces Notes PDFJohnLesterLaurelNo ratings yet
- Lee Et Al-2016-BJOG An International Journal of Obstetrics & GynaecologyDocument8 pagesLee Et Al-2016-BJOG An International Journal of Obstetrics & GynaecologyDhia UlfajriNo ratings yet
- Rotura Prematura de Membranas y ObesidadDocument5 pagesRotura Prematura de Membranas y ObesidadLaura AgudeloNo ratings yet
- Effects of Prepregnancy Dietary Patterns On Infant Birth Weight A Prospective Cohort StudyDocument11 pagesEffects of Prepregnancy Dietary Patterns On Infant Birth Weight A Prospective Cohort StudyLola SantiaNo ratings yet
- Poster Session I: Perinatal Outcome of Women With Epilepsy: Results From A Population-Based Cohort StudyDocument1 pagePoster Session I: Perinatal Outcome of Women With Epilepsy: Results From A Population-Based Cohort StudyasfwegereNo ratings yet
- Risk Factors For Excess Weight Loss and Hypernatremia in Exclusively Breast-Fed InfantsDocument6 pagesRisk Factors For Excess Weight Loss and Hypernatremia in Exclusively Breast-Fed InfantsHariz Ghulam RamadhanNo ratings yet
- Natural History of Fetal Position During Pregnancy.11Document6 pagesNatural History of Fetal Position During Pregnancy.11PutriNo ratings yet
- Ijwh 5 501Document7 pagesIjwh 5 501MarianaafiatiNo ratings yet
- Association Between Maternal Sleep Practices and Late Stillbirth - Findings From A Stillbirth Case-Control StudyDocument9 pagesAssociation Between Maternal Sleep Practices and Late Stillbirth - Findings From A Stillbirth Case-Control StudyWinniaTanelyNo ratings yet
- AmericanDocument1 pageAmericanAdzkia_ZRNo ratings yet
- Geist 2006Document5 pagesGeist 2006Marifer EstradaNo ratings yet
- Hersh 2019Document10 pagesHersh 2019RosiNo ratings yet
- ContentServer AspDocument7 pagesContentServer AspScribdNo ratings yet
- Cervical EncerclageDocument25 pagesCervical EncerclageKartheek VarmaNo ratings yet
- Merced 2019Document14 pagesMerced 2019Vanessa CarinoNo ratings yet
- Poster Session II: ConclusionDocument2 pagesPoster Session II: ConclusionFahmi Nur SuwandiNo ratings yet
- Ectopic Pregnancy: A ReviewDocument13 pagesEctopic Pregnancy: A ReviewDinorah MarcelaNo ratings yet
- Alustokat 2014Document8 pagesAlustokat 2014Syienthia RahmatikaNo ratings yet
- Intrauterine Growth Restriction: Diagnosis and ManagementDocument7 pagesIntrauterine Growth Restriction: Diagnosis and ManagementLarasati Gilang Fuzi AstutiNo ratings yet
- The Preterm Labor Index and Fetal Fibronectin For.24Document6 pagesThe Preterm Labor Index and Fetal Fibronectin For.24bombonlrNo ratings yet
- The Impact of Fetal Growth Restriction On Latency in The Setting of Expectant Management of PreeclampsiaDocument7 pagesThe Impact of Fetal Growth Restriction On Latency in The Setting of Expectant Management of PreeclampsiagusriaNo ratings yet
- Anomalía Uterinas Congénitas y Resultados Adversos en El EmbarazoDocument5 pagesAnomalía Uterinas Congénitas y Resultados Adversos en El EmbarazoAlexiis CabascangoNo ratings yet
- Normograma Perdida de PesoDocument10 pagesNormograma Perdida de PesoUTI NeonatologíaNo ratings yet
- Failed of LaborDocument12 pagesFailed of LaborStéphanieNo ratings yet
- Precision Medicine Personalized, Problematic, And.7Document3 pagesPrecision Medicine Personalized, Problematic, And.7Ben AllenNo ratings yet
- 1 s2.0 S0301211521007569Document1 page1 s2.0 S0301211521007569erikglu2796No ratings yet
- 2017 Julio Comunidad y SaludDocument3 pages2017 Julio Comunidad y SaludremediosisabelNo ratings yet
- Pregnancy Outcome in POCSDocument6 pagesPregnancy Outcome in POCSMeera Al AliNo ratings yet
- Ijnh 09-JS-2023-13 20231118 V2Document9 pagesIjnh 09-JS-2023-13 20231118 V2Apacetech IluvbNo ratings yet
- Effects of Anti M Llerian Hormone and Follicle Sti - 2014 - Taiwanese Journal ofDocument4 pagesEffects of Anti M Llerian Hormone and Follicle Sti - 2014 - Taiwanese Journal ofSami KahtaniNo ratings yet
- Exercise During Pregnancy Protects Against Hypertension and Macrosomia: Randomized Clinical TrialDocument8 pagesExercise During Pregnancy Protects Against Hypertension and Macrosomia: Randomized Clinical TrialDaniela VenegasNo ratings yet
- Iams 2011Document6 pagesIams 20118jxfv2gc5tNo ratings yet
- Research: Outcomes of Elective Induction of Labour Compared With Expectant Management: Population Based StudyDocument13 pagesResearch: Outcomes of Elective Induction of Labour Compared With Expectant Management: Population Based StudyAndinNo ratings yet
- The NeoUpdates - DecDocument7 pagesThe NeoUpdates - DecDr Satish MishraNo ratings yet
- Neurodevelopmental Outcomes of Extremely Preterm InfantsDocument10 pagesNeurodevelopmental Outcomes of Extremely Preterm Infantsmarta.sanz.alvarezNo ratings yet
- Estimated Fetal Weight: Comparison of Clinical Versus Ultrasound EstimateDocument6 pagesEstimated Fetal Weight: Comparison of Clinical Versus Ultrasound EstimateNadia AyuningtiasNo ratings yet
- Maternal Demography and Neonatal Outcomes in Term Pre Labour Rupture of Membranes Versus Spontaneous Labour Preceding Ruptured Membranes in Lagos, Nigeria A Comparative StudyDocument6 pagesMaternal Demography and Neonatal Outcomes in Term Pre Labour Rupture of Membranes Versus Spontaneous Labour Preceding Ruptured Membranes in Lagos, Nigeria A Comparative StudyInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Mihu 2015Document7 pagesMihu 2015Nuryasni NuryasniNo ratings yet
- Anemia MaternityDocument5 pagesAnemia MaternityBonaventura Ahardiansyah BoNo ratings yet
- Association Between Early Amniotomy in Labour Induction and Severe Maternal and Neonatal MorbidityDocument7 pagesAssociation Between Early Amniotomy in Labour Induction and Severe Maternal and Neonatal MorbidityLizbeth RomeroNo ratings yet
- Fetal Movements As A Predictor of HealthDocument8 pagesFetal Movements As A Predictor of HealthWordtreader PtNo ratings yet
- Pregnancy Complications and Outcomes in Women With Epilepsy: Mirzaei Fatemeh, Ebrahimi B. NazaninDocument5 pagesPregnancy Complications and Outcomes in Women With Epilepsy: Mirzaei Fatemeh, Ebrahimi B. NazaninMentari SetiawatiNo ratings yet
- Taiwanese Journal of Obstetrics & Gynecology: Dittakarn Boriboonhirunsarn, Rungnapa WaiyanikornDocument4 pagesTaiwanese Journal of Obstetrics & Gynecology: Dittakarn Boriboonhirunsarn, Rungnapa WaiyanikornirmaNo ratings yet
- Articulo EndometriosisDocument7 pagesArticulo EndometriosisMaIt VeFloNo ratings yet
- Poster Session I: Study DesignDocument1 pagePoster Session I: Study DesignRegina PizanNo ratings yet
- Hipoglicemia 4Document2 pagesHipoglicemia 4juanNo ratings yet
- Jurnal ObsgynDocument11 pagesJurnal ObsgynVivie Tirany SoediroNo ratings yet
- E057981 FullDocument11 pagesE057981 FulledmondNo ratings yet
- Severity of Anemia During Pregnancy and Adverse Maternal and Fetal OutcomesDocument13 pagesSeverity of Anemia During Pregnancy and Adverse Maternal and Fetal OutcomesIlda IldaNo ratings yet
- Exploring The Relationship Between Preterm Placental Calcification and Adverse Maternal and Fetal OutcomeDocument7 pagesExploring The Relationship Between Preterm Placental Calcification and Adverse Maternal and Fetal OutcomeMaulida HalimahNo ratings yet
- Jurnal 2 MisoprostolDocument17 pagesJurnal 2 MisoprostolaldoNo ratings yet
- Duan 2010Document3 pagesDuan 2010ShirleyNo ratings yet
- A Randomized Trial of Synthetic Osmotic Cervical D - 2022 - American Journal ofDocument20 pagesA Randomized Trial of Synthetic Osmotic Cervical D - 2022 - American Journal ofLuis GómezNo ratings yet
- Induction of LaborDocument8 pagesInduction of LaborwiwimbakNo ratings yet
- Predictors of Cephalopelvic Disproportion in Labour A Tertiary Hospital in Bayelsa State, NigeriaDocument7 pagesPredictors of Cephalopelvic Disproportion in Labour A Tertiary Hospital in Bayelsa State, NigeriaAndri Muhrim SiddiqNo ratings yet
- PCOS and IVF Success Rates in Melati Clinic Harapan Kita HospitalDocument1 pagePCOS and IVF Success Rates in Melati Clinic Harapan Kita HospitalCindikia Ayu SNo ratings yet
- To Compare The Safety and Efficacy of Manual Vacuum Aspiration With Misoprostol (ST Mom) 600mg in Incomplete MiscarriageDocument4 pagesTo Compare The Safety and Efficacy of Manual Vacuum Aspiration With Misoprostol (ST Mom) 600mg in Incomplete MiscarriageHassan KhanNo ratings yet
- Original Research: Screening Extremely Obese Pregnant Women For Obstructive Sleep ApneaDocument18 pagesOriginal Research: Screening Extremely Obese Pregnant Women For Obstructive Sleep ApneaappNo ratings yet
- The Interactive Effect of Prepregnancy Overweight/Obesity and Isolated Maternal Hypothyroxinemia On MacrosomiaDocument8 pagesThe Interactive Effect of Prepregnancy Overweight/Obesity and Isolated Maternal Hypothyroxinemia On MacrosomiaAndres GallegosNo ratings yet
- Wu 2020 Oi 200461Document12 pagesWu 2020 Oi 200461Antje IrmellaNo ratings yet
- Diminished Ovarian Reserve and Assisted Reproductive Technologies: Current Research and Clinical ManagementFrom EverandDiminished Ovarian Reserve and Assisted Reproductive Technologies: Current Research and Clinical ManagementOrhan BukulmezNo ratings yet
- Routine Firsttrimester Ultrasound Screening Using A Standardized Anatomical ProtocolDocument15 pagesRoutine Firsttrimester Ultrasound Screening Using A Standardized Anatomical ProtocolYosep SutandarNo ratings yet
- Physiology of Amniotic Fluid Volume RegulationDocument8 pagesPhysiology of Amniotic Fluid Volume RegulationYosep SutandarNo ratings yet
- Gestational Trophoblastic NeoplasiaDocument14 pagesGestational Trophoblastic NeoplasiaYosep SutandarNo ratings yet
- Ferra RettiDocument51 pagesFerra RettiYosep SutandarNo ratings yet
- Mao2014 Article ImagingOfPelvicLymphNodesDocument13 pagesMao2014 Article ImagingOfPelvicLymphNodesYosep SutandarNo ratings yet
- Ovarian Reserve Testing: A User's Guide: Expert ReviewsDocument12 pagesOvarian Reserve Testing: A User's Guide: Expert ReviewsYosep SutandarNo ratings yet
- Changes in The Sexual Function During Pregnancy: Aim. MethodsDocument10 pagesChanges in The Sexual Function During Pregnancy: Aim. MethodsYosep SutandarNo ratings yet
- Acog Committee Opinion: Dysmenorrhea and Endometriosis in The AdolescentDocument10 pagesAcog Committee Opinion: Dysmenorrhea and Endometriosis in The AdolescentYosep SutandarNo ratings yet
- Eng - PDF JsessionidDocument34 pagesEng - PDF JsessionidYosep SutandarNo ratings yet
- Pi Is 0884217517304100Document3 pagesPi Is 0884217517304100Yosep SutandarNo ratings yet
- Enteral NutritionDocument73 pagesEnteral NutritionYosep Sutandar100% (1)
- Practice Bullet In: Emergency ContraceptionDocument11 pagesPractice Bullet In: Emergency ContraceptionYosep SutandarNo ratings yet
- Clue CellsDocument10 pagesClue CellsYosep SutandarNo ratings yet
- 7 Meaning - Sri StutiDocument24 pages7 Meaning - Sri StutiLeela KNo ratings yet
- Overview Six Sigma PhasesDocument3 pagesOverview Six Sigma Phaseshans_106No ratings yet
- Anatomy and Physiology of Salivary GlandsDocument55 pagesAnatomy and Physiology of Salivary GlandsSuprit SnNo ratings yet
- Flangeless Horseshoe Maxillary Complete Denture - A Prosthodontic Solution To Maxillary ToriDocument3 pagesFlangeless Horseshoe Maxillary Complete Denture - A Prosthodontic Solution To Maxillary ToriMohammad Abdulmon’emNo ratings yet
- CONTEMPT OF COURT JurisprudenceDocument10 pagesCONTEMPT OF COURT Jurisprudencenxfkfbvjw7No ratings yet
- 14 Best Hypoallergenic Cat BreedDocument11 pages14 Best Hypoallergenic Cat BreedJunna May AradoNo ratings yet
- INTRAPERSONALCOMMUNICATIONASFOUNDATIONFORPERSONALBRANDING BerylEhondor PDFDocument12 pagesINTRAPERSONALCOMMUNICATIONASFOUNDATIONFORPERSONALBRANDING BerylEhondor PDFDexter JoveloNo ratings yet
- 1st Quarter Exam in Mapeh 10Document4 pages1st Quarter Exam in Mapeh 10Dhan Mark Barlintangco100% (1)
- Loudspeakers Coverage AnglesDocument0 pagesLoudspeakers Coverage AnglesAnthony HubbardNo ratings yet
- Business Ethics and CSR Individual Assignment 1 Concept PaperDocument9 pagesBusiness Ethics and CSR Individual Assignment 1 Concept PaperZeeshan KhanNo ratings yet
- Syllabus: Subject: Software EngineeringDocument4 pagesSyllabus: Subject: Software EngineeringTuyên Kiều VănNo ratings yet
- The ABCs of DR Desmond Ford S Theology W H JohnsDocument16 pagesThe ABCs of DR Desmond Ford S Theology W H JohnsBogdan PlaticaNo ratings yet
- HindustaniMelodic SQPDocument4 pagesHindustaniMelodic SQPAkshit ChauhanNo ratings yet
- Flight1 441 Conquest TutorialDocument10 pagesFlight1 441 Conquest TutorialJosé A. Montiel QuirósNo ratings yet
- International Human Resource ManagementDocument20 pagesInternational Human Resource ManagementAziz UllahNo ratings yet
- Extended Essay IB DiplomaDocument20 pagesExtended Essay IB Diplomasol GonzalezNo ratings yet
- Criminology Comprehensive Examination Set BDocument9 pagesCriminology Comprehensive Examination Set BChristine Anne Ganio ValenciaNo ratings yet
- Crim Justice System PDFDocument3 pagesCrim Justice System PDFKing Monteclaro MonterealNo ratings yet
- Housing First Fact SheetDocument2 pagesHousing First Fact SheetstprepsNo ratings yet
- Arshad CVDocument4 pagesArshad CVAli BaseejiNo ratings yet
- Assignment Brief Unit 47 QCFDocument14 pagesAssignment Brief Unit 47 QCFAlamzeb KhanNo ratings yet
- Republic Vs LedesmaDocument2 pagesRepublic Vs LedesmaestvanguardiaNo ratings yet
- Addition Word ProblemsDocument10 pagesAddition Word ProblemsmarycperezNo ratings yet
- A Freemason's 33rd Degree InitiationDocument12 pagesA Freemason's 33rd Degree InitiationMax SchmidtNo ratings yet
- Ioug Selectjournal 2014q1cDocument8 pagesIoug Selectjournal 2014q1carunjacNo ratings yet
- Topology PaperDocument9 pagesTopology PaperNestor Bong Bordaje NemeñoNo ratings yet