Professional Documents
Culture Documents
Laycock 2001 PERFECTscheme
Laycock 2001 PERFECTscheme
Uploaded by
Ravisha GalaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Laycock 2001 PERFECTscheme
Laycock 2001 PERFECTscheme
Uploaded by
Ravisha GalaCopyright:
Available Formats
Professional articles Key Words 631
Pelvic floor, assessment,
research, validity, reliability.
by J Laycock
Pelvic Floor Muscle D Jerwood
Assessment:
The PERFECT Scheme
Summary
Introduction
Aims of study
The pelvic floor muscles (PFM) consist of
1. To develop a digital technique to assess pelvic floor
approximately 70% slow-twitch (type 1)
muscles (PFM). and 30% fast-twitch (type 2) muscle fibres
2. To validate the technique and test for validity and (Gilpin et al, 1989). Although the PFM are
reliability. thought to work tonically and reflexly
3. To translate the assessment into an exercise-based during routine daily activities, voluntary
regimen. contractions are required for training.
PFM weakness is recognised as one of
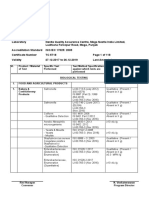
Method and Results PERFECT is an acronym with the problems encountered in patients
P representing power (or pressure, a measure of strength with urinary and faecal incontinence, and
using a manometric perineometer), E = endurance, re-education should address the perceived
R = repetitions, F = fast contractions, and finally ECT = every deficit, be it in the slow- or/and fast-twitch
muscle fibres. There are several ways by
contraction timed. The scheme was developed to simplify
which to assess the PFM, including digital
and clarify PFM assessment. The pressure (referred to palpation (Brink et al, 1989), using a
hereafter as power, although actually a surrogate measure pressure perineometer (Laycock and
of muscular strength) of a contraction was validated by Jerwood, 1994), electromyography (EMG)
examining perineal lift and perineometric pressure during (Haslam, 2002) ultrasound scanning
a maximum voluntary contraction (MVC). Data analysis (Vierhout and Jansen, 1989) and
magnetic resonance imaging (MRI)
demonstrated significant positive correlations between power
(Khullar, 2002). Evaluation of muscle
and both lift (r = 0.864; p = 0.031) and perineometric strength and endurance provides
pressure (r = 0.786; p = 0.001); digitally assessed endurance information on the severity of muscle
correlated with the area under the pressure curve of a weakness and forms the basis of patient-
sophisticated perineometer (r = 0.549; p = 0.001). A study specific exercise programmes.
of inter-examiner reliability demonstrated highly significant Research involving PFM assessment
probably started with the work of Kegel
positive correlations between two examiners for power
(1948), who advocated clinical assessment
(r = 0.947; p < 0.001), endurance (r = 0.946; p < 0.001), of the pubococcygeus as part of a routine
repetitions (r = 0.730; p < 0.005) and number of fast gynaecological examination, using one
contractions (r = 0.909; p < 0.001). Scatter diagrams finger to palpate the pubococcygeus per
confirmed a lack of systematic bias between examiners. vaginam. He maintained that two fingers
Test-retest reliability produced highly significant correlations placed the vaginal tissues under tension
and distorted the anatomic relationships
(p < 0.001) between power (r = 0.929) and endurance values
(Kegel, 1956). However, the premise that
(r = 0.988) recorded on two different occasions, with no stretching the vaginal tissues during ass-
convincing evidence of significant discrepancies between the essment may adversely affect outcomes
pair of assessments. was challenged by Chiarelli (1989) who
maintained that stretching the muscle
Conclusions The PERFECT scheme has demonstrated may produce an enhanced response. In
reliability and validity as an assessment tool. Furthermore, support of this hypothesis, Jahnke et al
it is proposed that this scheme provides guidelines for the (1989) showed that the initial phase of
planning of patient-specific exercise programmes which passive muscle stretching is associated
satisfy the principles of muscle training. with a rise in reflex tone.
The one-finger assessment technique
Physiotherapy December 2001/vol 87/no 12
632
was again described by Hendrickson can easily slip out, a score of 1 is given.
(1981), who defined a mild contraction If the finger can be gripped somewhat
as slight unsustained pressure on the but remains in the same position, a
examiner's finger; a moderate contraction score of 2 is given, and if the finger is
as firm pressure held for one to three forcibly gripped, expelled, or pulled
seconds; and a strong contraction as anteriorly, a score of 3 is given.
forceful pressure on the examiner's finger Test-retest reliability of this scoring
sustained for four seconds or more. system showed a statistically significant
A different method was devised by relationship of observation between ten
Graber et al (1981) based on four com- patients examined and then re-examined
ponents: control, sustained strength, 10 days later.
atrophy and tone. Control is measured Another scoring system, this time linked
using a perineometer and indicates the with incontinence, was described by Brink
patient's ability to contract and relax the et al (1989). This measure uses concepts
PFM to command. Sustained strength is of pressure (rated 1 to 4), time and
an indication of the time (up to 10 displacement. These were evaluated by
seconds) that a strong contraction could the index and middle fingers in the
be held. Atrophy is used to describe the antero-posterior position (index finger
development and wastage of the muscle. resting on the middle finger) introduced
This involved the technique of mapping, 4 cm to 6 cm into the vagina. Test-retest
which necessitated palpating the PFM and for this scoring method was r = 0.65,
charting areas of reduced muscle bulk. p < 0.01, with inter-rater reliability
Tone was determined by the degree of r = 0.91, p < 0.01. A negative correlation
resistance of the muscle against moderate between muscle strength and both urine
pressure from the examining finger. loss and age was demonstrated.
A further report (Worth et al, 1986) The authors of all the aforementioned
described another one-finger digital studies did not attempt to use any
vaginal assessment with four components: standard international muscle-grading
pressure, duration, ribbing and position scheme or to differentiate between
(of the examining finger). slow- and fast-twitch muscle activity.
■ They defined pressure as the strength Furthermore, they did not relate the
of contraction. If no pressure is felt, a assessment findings to an individual
score of 1 is given. If moderate pressure exercise programme. Moreover, co-
is felt, a score of 2 is given, and firm contraction of the abdominal muscles
pressure is recorded as 3. was discouraged and this is now
acknowledged to be inappropriate
■ Duration is based on the length of time (Sapsford et al, 2001).
a contraction can be sustained. If no
contraction is felt or the contraction Aims of Study
lasts no longer than 1 second, a score 1. To develop a digital technique for
of 1 is assigned. A contraction held for quantitative assessment of the
2 to 3 seconds is scored 2, and a score voluntary contractility of the PFM.
of 3 is assigned to a contraction held
for 4 or more seconds. 2. To validate the above technique and
■ An assessment of ribbing refers to the test for observer reliability.
tone and texture of the PFM during
a contraction. If the muscle feels soft 3. To translate the measurements from
and flabby, it is assigned a score of 1; the digital assessment into the
a score of 2 describes a muscle that planning of a patient-specific exercise
feels different from the surrounding programme.
tissues but not ribbed, and a score of
3 is assigned if the muscle feels distinct, Methods and Materials
Laycock, J and PERFECT is an acronym to remind all
like rings of ribbing or ribbed muscle
Jerwood, D (2001).
tissue. health professionals of the need to
‘Pelvic floor muscle
assessment: The ■ Assessment of position refers to the assess the main components of PFM
PERFECT Scheme’, contractility. This assessment scheme was
plane the examining finger is in,
Physiotherapy, 87, 12, developed to provide a simple, reliable
in relation to the vaginal introitus.
631-642. method of PFM evaluation and involves
If no force is exerted and the finger
four components, as shown in table 1.
Physiotherapy December 2001/vol 87/no 12
Professional articles 633
Table 1: The PERFECT assessment scheme stronger can be observed as an in-drawing Authors
of the perineum and anus. J Laycock PhD FCSP
P Power (pressure)
Grade 4 Increased tension and a good is a specialist
E Endurance
contraction are present which are capable continence
R Repetitions
of elevating the posterior vaginal wall physiotherapist in
F Fast private practice who
E Every against resistance (digital pressure
carrried out the
C Contraction
applied to the posterior vaginal wall). research for this
T Timed Grade 5 Strong resistance can be applied article.
to the elevation of the posterior vaginal D Jerwood BSc PhD
Although the study was carried out on wall; the examining finger is squeezed FSS is head of
women by palpating the perivaginal and drawn into the vagina (like a hungry mathematics, School
muscles per vaginam, the PERFECT baby sucking a finger). of Computing and
Mathematics,
assessment can also be used for PFM
University of
assessment per rectum in men and women. Table 2: Proposed modified Oxford grading
scheme Bradford, and was
To ensure reproducibility, the following responsible for the
factors were adopted throughout the Grading Muscle response statistics.
study:
0 Nil
■ The location and action of the pelvic This article was
1 Flicker
floor muscles were described to the received on January
2 Weak 17, 2000, and
subjects in enough detail for adequate
3 Moderate accepted on August
understanding of this muscle group.
4 Good 22, 2001.
■ Whenever possible, subjects were
5 Strong
positioned in supine with their head on
two pillows. The hips were flexed and Address for
abducted, and the knees bent. Correspondence
Consequently, in a specific case, the
■ The PFM were examined using the power could simply be recorded as Jo Laycock,
index finger placed approximately grade 3 for a moderate contraction. The Culgaith Clinic,
Pea Top Grange,
4 cm to 6 cm inside the vagina and However, the registered grade is
Culgaith, Penrith
positioned at 4 o'clock and 8 o'clock permitted to be augmented with a symbol
CA10 1QW.
to monitor muscle activity. Moderate + or –, when the need arises. Thus 3+
pressure was applied over the muscle could be translated as there being more
bulk to assist in the initiation of the than a moderate contraction but less than
appropriate muscle contraction. a good contraction (grade 4). Similarly, a
■ Verbal informed consent was obtained 3-- is recorded when the contraction is less
than a grade 3, but more than a grade 2.
from all subjects.
This augmentation is to allow for an
Power element of doubt to be introduced and
Power is measured on a modified Oxford thereby to soften this (partly subjective)
scale (table 2). The authors acknowledge six-point ordinal scale. There will
that digital palpation during a maximal admittedly be a learning curve involved
voluntary contraction (MVC) evaluates in assessing the strength of a PFM
muscle strength, not power. However, with contraction.
this caveat, the misnomer ‘power’ will be
used throughout the text. Endurance
The following definitions are proposed: Endurance is expressed as the length of
time, up to 10 seconds, that an MVC can
Grade 0 No discernible muscle
be sustained before the strength is
contraction.
reduced by 35% or more. In other
Grade 1 A flicker or pulsation is felt words, the contraction is timed until
under the examiner's finger. the muscle starts to fatigue. A further
possible indication of PFM fatigue may
Grade 2 An increase in tension is
be the simultaneous contraction of hip
detected, without any discernible lift.
adductors and glutei, and the stronger co-
Grade 3 Muscle tension is further contraction of transversus abdominis.
enhanced and characterised by lifting of Breath-holding should be discouraged; if
the muscle belly and also elevation of the detected, the subject should be instructed
posterior vaginal wall. A grade 3 and to contract the pelvic floor on expiration.
Physiotherapy December 2001/vol 87/no 12
634
Example 1: 3/5 = grade 3 held for 5 seconds Validity Study 1
Since an increase in pressure on the
Repetitions
examiner's finger may be misinterpreted
The number of repetitions (up to 10) of
as pressure exerted by an increase in
the specific MVC (eg 3 as in example 1) is
intra-abdominal pressure (rather than by
recorded, allowing four seconds rest
perivaginal muscle contraction), it was
between each contraction (which lasts
necessary to validate the source of activity.
for 5 seconds in example 1). The purpose
It is well documented (Bø et al, 1989) that
of the PERFECT assessment is to
a moderate to strong PFM contraction
determine the number of contractions
also incorporates an element of lift which
necessary to overload the muscle, develop
would not be manifest during an increase
a practicable exercise programme and so
in abdominal pressure alone. Validation
produce a training effect.
of the PFM contraction was therefore
Different ‘rest’ periods have been
ratified by measuring perineal lift.
tested, and in the experience of the
Eight women, mean age 43.9 years
authors, four seconds will allow weak,
(range 21 to 61 years) and mean parity
easily fatigued muscles time to recover
2.5 (range 0 to 5), randomly recruited
without permitting excessive rest periods
from a gynaecology outpatient clinic,
for stronger muscles. It would be im-
agreed to take part in this study. A light-
practical to permit, say, 20 seconds rest
weight vaginal probe with a thin plastic
between each contraction, as this would
rod extension was introduced into the
make the exercise session too long, and
distal 5 cm of the vagina. The rod was
might never overload the PFM in some
placed alongside a ruler and cephalad
cases. Furthermore, in practical terms,
movement of the rod during an MVC was
once a subject can perform 10 repetitions
observed and measured.
of a 10-second maximum contraction, the
rest time is reduced.
Validity Study 2
Limiting both repetitions and en-
A consecutive sample of 233 women
durance to a maximum in this way is
attending a gynaecology outpatient
formally referred to as right-censoring of
clinic were recruited into this study, of
data, and its impact on results will be
whom 147 were diagnosed as having stress
discussed later.
incontinence. Power and endurance were
Example 2: 2/3/6 = grade 2 held for assessed both digitally (as described
3 seconds, and repeated 6 times (with above) and, after a two-minute rest, using
4 seconds rest between each contraction) a sophisticated pressure perineometer
previously tested for reproducibility and
Fast reliability (Laycock and Jerwood, 1994).
After a short rest (at least one minute), This perineometer recorded maximum
the number (up to 10) of one-second pressure and endurance was assessed by
MVCs is assessed. Subjects are instructed calculating the area under the pressure
to ‘contract-relax’ as quickly and strongly cur ve of a maximum 10-second con-
as possible, in their own time, until the traction. The same patient position (see
muscles fatigue. Many patients can above) was used for each method.
perform more than 10 fast contractions,
but for practical reasons, the assessment Inter-examiner Reliability Study
stage should be limited to 10. Subsequent Ten patients were independently assessed
assessment during a treatment prog- by two examiners at the same visit.
ramme may identify a greater number Demographically, all the women were
of fast contractions, and that should be incontinent, mean age 47.6 years (range
the number practised by those patients 26 to 58), and mean parity 2.7 (range 1 to
on a daily basis. 4). Each subject was tested for strength
(scale 0 to 5), endurance (up to 10 sec-
Example 3: 4/6/5//9 = good contraction, onds), number of repetitions (up to 10)
held for 6 seconds, repeated 5 times, and number of fast contractions (up to
followed by 9 fast contractions 10), with at least two minutes rest between
Every Contraction Timed each test and three minutes rest between
This completes the acronym and reminds each examination. The order of exam-
the examiner to time and record the ination between physiotherapists was
above sequence of events. randomised in order to eliminate
Physiotherapy December 2001/vol 87/no 12
Professional articles 635
systematic bias. Inter-examiner reliability a 10-second MVC at regular intervals
over the two assessments was determined during the day, and 10+ fast contractions
using correlation and graphical tech- at other times during the day. Equal
niques. Each examiner recorded the numbers of sessions of slow and fast con-
values of the assessment independently, tractions are encouraged, up to six per
without knowledge of the other's result. day.
Patient 2
Test-retest Reliability
Twenty incontinent women entered this P E R F
study. Assessment was carried out before
2 2 3 – This assessment describes
cystometry and repeated at the first
a patient with a weak
physiotherapy appointment two to (grade 2) contraction,
five weeks later by the same examiner, held for 2 seconds and
evaluating power and endurance. To repeated 3 times
conduct this test responsibly, the results of
the first assessment were not available This patient needs to practise 3 (R) of
until after completion of the second her strongest contractions lasting 2 sec-
examination. Test-retest reliability was onds (E) (with 4 seconds rest between
determined using correlation and graph- each contraction) as many times as
ical techniques for the two results. possible during the day. In view of the
weak state of the PFM, assessing the
Exercise Programme Planning number of fast contractions would be
The third purpose of the study was to confusing, and this should be done at a
formulate a method for translating the later date when endurance has improved
PERFECT assessment into a patient- to 4 seconds. Treatment should progress
specific exercise programme. Not only in the first instance by aiming to hold the
has such a regimen to satisfy general contraction for 3 (then 4) seconds. Once
muscle training principles of overload this is achieved, strength should be
and specificity, but it must also be pract- addressed and the patient encouraged
icable within the context of the individual to contract harder. Once a grade 3 has
patient since, without a high degree of been achieved, endurance is once again
compliance, the therapy is unlikely to be addressed, and the subject encouraged
effective. to increase the length of contraction.
In all cases, regular PFM re-assessment
Patient 1
is required to monitor progress and
P E R F establish a ‘new’ exercise programme.
3 5 4 7 This assessment describes a Results
patient with a moderate
(grade 3) contraction, held Validity Study 1
for 5 seconds and repeated This study measured perineal lift (in
4 times; followed by 7 fast centimetres) during an MVC (P – scale
contractions 0 to 5) and the results are displayed in
table 3. Six of the eight subjects examined
This patient would be instructed during an MVC exhibited cephalad
to practise 4 (R) of her strongest movement of the vaginal probe greater
contractions lasting 5 seconds (E) (with 4
seconds rest between) at each exercise Table 3: Results of study to measure perineal lift
session, and 7 fast (F) strong contractions
Subject Age Parity P Continence status Lift (cm)
at other times. She should aim to increase (years)
the number of repetitions of the long
MVC over subsequent weeks up to 10 1 61 2 2+ Incontinent 0.3
repetitions. After this, over the succeeding 2 51 3 2+ Incontinent 0.4
weeks, she should aim to increase the 3 21 0 3+ Continent 0.5
hold time to 10 seconds. In addition, the 4 36 2 5 Continent 0.7
number of fast contractions should be 5 53 4 2 Incontinent 0.0
progressively increased to the maximum 6 45 2 3+ Incontinent 1.0
number possible (many patients can do 7 51 5 2+ Incontinent 0.1
up to 50 fast contractions). The aim is 8 31 2 4 Incontinent 0.7
to be able to perform 10 repetitions of
Physiotherapy December 2001/vol 87/no 12
636
than 0.1 cm. The subjects who failed to Validity Study 2
demonstrate such a movement (patients 5 The results of the digital and perineo-
and 7, both incontinent) had had metric testing are shown in table 4
delivered per vaginam four and five babies together with a selected number of
respectively, compared with a mean of 1.8 demographic details. It is now relevant
babies for the remaining subjects. Over all to note the large number of subjects
subjects, a degree of negative correlation in each group (86 continent and 147
between perineal lift and parity incontinent), so that statistical compar-
was detected (r = –0.664; p = 0.073) isons between groups are not so sensitive
(Spearman's rho for ordinal data). to choice of test procedure (parametric or
Any correlation coefficient in the range non-parametric).
0.61 to 0.80 can be considered ‘good’, Appealing to the central limit theorem
and with r = –0.664 the coefficient of for induced asymptotic normality, it
variation is 44% (100 ρ2). In other words, becomes reasonable to apply t-tests for
44% of the variation in perineal lift can unrelated samples for all inter-group
be explained by parity alone. It should be comparisons. The incontinent subjects
noted in passing that this evidence has were found to be older on average (by 6.9
been detected in a sample of only eight years), had borne one more child on
patients and therefore fails to reach levels average, and were associated with a higher
at which statistical significance can be BMI (by 2.6 units on average). All these
claimed, although the result may still be differences were found to be statistically
clinically significant. More pertinent is significant with p < 0.00005. It should be
that examination of the data for all eight said that large sample sizes generally
subjects showed a positive value for produce much reduced standard errors
Spearman's coefficient of correlation for the differences in means, and statist-
between P (modified Oxford grading, ical power rises accordingly. In these cases,
scale 0 to 5) and perineal lift (r = 0.864; statistical significance is often easier to
p = 0.031). This coefficient is in excess demonstrate.
of 0.80 and therefore can be considered From a clinical point of view, on av-
‘very good’, however once again this erage, the continent subjects exhibited
result must be viewed in the context of 16% more power (digitally assessed), and
sample size (n = 8). The coefficient of 63% higher maximum pressure, and
variation now rises to almost 75% and generated 60% more area under the
confirms the sympathetic relationship perineometric pressure curve. Each of
between perineal lift and the digital these differences proved statistically
assessment scale discussed earlier. This significant (with p < 0.00005). Only
adds some credence to the hypothesis endurance (also assessed by digital
that digital assessment can be used to palpitation), which registered an average
measure power (P) of a pelvic floor increase of 11% (of continent subjects
muscle contraction. over incontinents) failed to reach levels of
statistical significance (p = 0.103).
Table 4: Results of Validity Study 2. Demographic variables of age,
The relationship between the digital
parity and BMI assessment of pressure (P) and the
maximum perineometric pressure (r =
Variable Continent Incontinent Difference 0.786) implies that 62% of the variation in
(n = 86) (n = 147)
No (SD) No (SD)
perineometric pressure could be
explained by the variation in P. The
Age 38.5 (16.8) 45.4 (11.9) p < 0.00005 relationship between area under the
Parity 1.5 (1.4) 2.5 (1.5) p < 0.00005 pressure curve and endurance (E) was
BMI 23.3 (3.1) 25.9 (4.0) p < 0.00005 less convincing (r = 0.549), whereby only
P 3.6 (1.1) 3.1 (1.2) p < 0.00005 30% of the variation in area could be
Max. press. 52 (24) 32 (21) p < 0.00005 explained by the variation in E.
E 7.0 (2.9) 6.3 (3.3) p = 0.103 Agreement between digital and
Area 346 (198) 216 (156) p < 0.00005 perineometric measurements of pressure
adds further evidence of the validity of
SD = standard deviation this form of assessment for pelvic floor
P = power (scale 0 to 5) digital assessment
Maximum pressure (mm Hg) perineometric assessment
muscles.
E = endurance (seconds) digital assessment
Area (mm Hg.s) measured with perineometer
Physiotherapy December 2001/vol 87/no 12
Professional articles 637
Inter-examiner Reliability Study Table 5: Analysis of results of digital assessment of ten patients
by two examiners (SHD and JL) on the same visit
Reliability between different examin-
ers involved two physiotherapists (JL Patient P E R F
and SHD) each performing complete SHD JL SHD JL SHD JL SHD JL
PERFECT assessments on ten subjects
1 3.0 2.5 7 6 6 5 7 6
on the same visit, and the results are
shown in table 5. Analysis shows highly 2 4.0 4.0 9 10 3 6 8 7
significant positive correlation coefficients 3 5.0 5.0 10 10 8 6 10 10
between the two examiners for P 4 4.5 4.0 10 10 8 7 10 10
(r = 0.947; p < 0.001), E (r = 0.946; 5 2.0 2.0 4 3 3 2 6 5
p < 0.001), R (r = 0.730; p < 0.005) and F 6 2.0 3.0 3 2 4 5 5 6
(r = 0.909; p < 0.001). 7 3.0 3.0 3 3 6 5 5 6
When testing for significance of 8 1.0 1.0 2 2 1 2 3 2
correlation coefficients, the P values 9 1.5 1.0 4 5 3 3 4 5
relate to rejection of a null hypothesis 10 4.0 4.0 3 3 4 5 7 7
claiming that the true correlation is zero Spearman's r = 0.947 r = 0.946 r = 0.730 r = 0.909
which is not a useful concept within correlation
validity studies. Subjects (such as patients Coefficient
3 and 4 in table 5) who are performing at significance p < 0.001 p < 0.001 p < 0.005 p < 0.001
level
the boundary of data censorship (that is,
holding an MVC for at least 10 seconds, 5
and being able to produce at least 10
fast contractions) will enhance any
correlation coefficients. Removing pat- 4
ients 3 and 4 from these correlation
studies will reduce every one of the
Repetitions (SHD)
coefficients given in table 5, the greatest 3
impact being on R, for which the
coefficient falls dramatically from r =
0.730 to r = 0.530. 2
Especially when assessing agreement
between two examiners, it should be
appreciated that a high coefficient of 1
correlation is certainly necessary, but not
(in itself) sufficient. Correlation is a
concept which describes only linearity 0
0 1 2 3 4 5
between variables – not agreement. It is Repetitions (JL)
therefore per fectly feasible for one
Fig 1: Pressure of PFM contractions assessed by JL and SHD with
assessor to display a systematic bias line of equality
(compared with another assessor) with
such consistency, that the results are still 10
highly correlated. For ‘agreement’,
further supportive evidence is required
(Bland and Altman, 1999). This can be 8
provided using a number of techniques,
but perhaps the simplest is the scatter
Repetitions (SHD)
diagram (see figures 1 and 2). The digital 6
assessment of pressure (P) of figure 1
shows six agreements, three over-ass-
essments (by SHD compared to JL) by 4
only a half unit of grading, and only one
(full unit) under-assessment. In nett
terms, the mean difference over ten 2
subjects is 0.05 which, when considered
together with a correlation coefficient of
r = 0.947, suggests a lack of systematic 0
0 2 4 6 8 10
bias and a strong (linear) relationship Repetitions (JL)
between assessors. Fig 2: Numbers of repetitions recorded by JL and SHD with line
Similar plots result from the two of equality
Physiotherapy December 2001/vol 87/no 12
638
assessments of endurance (E) and the two Table 6: Test-retest results of digital assessment
of power (P) and endurance (E)
counts of fast contractions (F) (not
reproduced here), however the weakest Patient Power Endurance
inter-assessor agreement was found with Test 1 Test 2 Test 1 Test 2
repetitions (R) and this is illustrated in
1 3.0 4.0 2 2
figure 2. Now, there is only one (perfect)
2 0.0 0.0 0 0
agreement, with four over-assessments
(totalling 5 units) and three under- 3 3.0 3.0 3 3
assessments (also totalling 5 units); the 4 4.0 3.5 10 10
greatest discrepancies occurr with two 5 3.0 3.5 5 6
subjects who recorded 6 repetitions for 6 3.5 4.0 10 10
JL. The mean nett difference is now zero 7 2.5 2.0 5 6
but (with a correlation coefficient of only 8 2.0 2.0 2 3
0.730), the impression is given of a lack of 9 0.0 0.0 0 0
systematic bias between examiners with 10 3.0 3.5 7 7
less convincing consistency. Notice, 11 2.5 2.5 4 4
however, when recording repetitions the 12 2.5 3.0 2 3
censoring limit of 10 which had been 13 4.0 4.5 8 9
imposed by the physiotherapist was never 14 4.0 4.0 10 10
actually attained for any of these ten 15 4.5 4.0 4 6
subjects, although other imposed maxima 16 2.5 2.5 8 8
were regularly attained by subjects 3 and 4. 17 2.0 2.0 10 10
This could imply that the R component 18 3.0 3.5 10 10
was found to be a particularly fatiguing 19 5.0 5.0 5 5
exercise by those subjects, and its 20 3.5 4.0 10 10
implementation introduced additional Spearman's r = 0.929 r = 0.988
sources of intra-patient variation to be correlation
confounded with inter-assessor variation. Coefficient p < 0.001 p < 0.001
The inter-examiner assessments of significance
number of repetitions (R) apart, taken level
over the remaining three digital scores,
this study demonstrated 46.7% exact minimum unit of graduation (of 0.5).
agreement of the digital scores. However, Regarding endurance, 70% exact
disagreement in all but two cases (both in agreement was demonstrated, with a
the repetition test) did not exceed one variation of only one second in all except
unit of measurement. These encouraging one, which was two seconds. In all cases,
results provide global evidence in support endurance remained the same or
of the inter-examiner reliability of these increased, despite the fact that these
components of the digital assessment of women were not instructed to practise
the PFM. pelvic floor exercises. The complete
absence of patients with shorter
Test-retest Reliability Study endurance periods is surprising, but the
The results of re-testing 20 women two to mean nett shift is only 0.4 seconds per
five weeks after the initial assessment patient and (again) well within the
are shown in table 6. These results show minimum unit of evaluation (of one
that for muscle strength (P), 45% exact second).
agreement was demonstrated. Further- Evaluating Spearman's rank correlation
more, of the 11 measures that differed, coefficients for these test-retest results,
ten of these differed by only 0.5 grade and the coefficient for power (P) is found to
the remainder by one grade. In addition, be 0.929 (p < 0.001) and for endurance
it is shown that 8/11 demonstrated an (E) stands even higher at 0.988. These
increase in strength whereas 3/11 extremely high levels of correlation
demonstrated a decrease. together with mean discrepancies which
Scatter graphs (similar to figures 1 and 2, cannot be reduced by systematic adjust-
but not reproduced here) illustrate a ments provide convincing evidence that,
slight tendency for some patients to for an experienced physiotherapist, the
improve over the period between the digital evaluation of power and
tests. However, the mean nett shift of only endurance of PFM contractions following
+0.125 per patient is well within the a short delay is a reliable technique.
Physiotherapy December 2001/vol 87/no 12
Professional articles 639
Planning Exercise Programmes although a subjective method, has been
The procedure for planning patient- shown to be reliable and reproducible.
specific exercise programmes described The first component P (power/pressure,
earlier follows recognised muscle training but actually evaluating strength) graded
methods and has proved to be successful the pressure exerted on the finger
in clinical practice. However, in the past, from 0 to 5, with intermediate scoring
many women have admitted to neglecting permitted (for example 3+), giving a
to practise their prescribed pelvic floor greater flexibility than the scoring of
exercises and so realistic regimens need 1 to 4 suggested by Brink et al (1989).
to be agreed with each patient. Previously, The Oxford grading system is well under-
the majority of patients have complained stood in physical medicine and the
that pelvic floor exercises were not inter- modifications described herein have
esting, but with the introduction of long, proved to be an effective way of assessing
and fast and short contractions, and the PFM strength. Regarding different muscle
setting of targets, more women are co- components (that is, fast- and slow-twitch
operating in this self-help rehabilitation. fibres), it has been shown that fast
Although data have not been made fibres are recruited only during activities
available here, a number of interesting involving speed and/or power (Edwards,
facts have emerged as a result of this 1978) and if the response to a command
methodology. For example, a woman's to contract the PFM maximally is sluggish,
ability to contract the PFM appears to be then it is probable that only slow-twitch
subject to a learning curve, and many muscle fibres are being used. Jones and
women can begin to produce a stronger Rutherford (1987) reported that in some
and longer contraction before any untrained muscles, the fast-firing muscle
possible physiological change in the fibres are never recruited, and so these
muscle fibres could have taken place. may need targeting in some other way
In addition, some women report an during PFM rehabilitation. It is postulated
improvement in continence symptoms that an MVC will recruit both fast-
without any measurable improvement in and slow-twitch muscle fibres (if the
their PFM contractility. This was discussed contraction is strong and brisk) and so
in a study by Miller et al (1996) who P would represent recruitment of both
described ‘the knack’, a precisely-timed fibre types.
anticipatory pelvic floor contraction It is further hypothesised that the
before and during a cough. Using endurance (E) and repetitions (R) of a
‘the knack’, significant reduction in PFM contraction are measures of slow-
involuntary urine loss during a cough twitch muscle fibre activity. Gosling et al
was demonstrated. (1981) described the PFM slow-twitch
fibres as being responsible for main-
Conclusions and Discussion taining continuous muscle activity over
In physiotherapy practice, palpation of a prolonged periods, with the fast-twitch
muscle can detect changes in resting fibres recruited reflexly during sudden
tone, identify areas of atrophy and increases in intra-abdominal pressure, for
differentiate between the state of example when coughing. A reduction in
contraction and relaxation, and this is slow-twitch activity would therefore
certainly the case with the pelvic floor manifest itself in a short duration
muscles. During a vaginal examination contraction and few repetitions, and PFM
using the distal pad of the index finger to in this category may thus be responsible
palpate the perivaginal muscles, a definite for decreased support of the proximal
bulging and lifting of the muscles are felt urethra and reduced urethral occlusion.
during a contraction, and in both the A reduction in fast-twitch fibre activity
contracted and relaxed state, areas of may result in a slower, weaker reflex
atrophy can be detected. response to increases in intra-abdominal
Furthermore, a moderate to strong pressure. Logically, one should assess both
contraction of the levator ani muscles has the fast- and slow-twitch muscle fibre
both a squeeze and a lift component, and activity before planning an exercise
the proposed digital assessment scoring regimen.
system provides a means of calibrating The third component in the PERFECT
this physical effect. assessment method, the number of
The PERFECT assessment scheme, repetitions a subject could per form
Physiotherapy December 2001/vol 87/no 12
640
before the muscles fatigued, was incorp- using transrectal ultrasound on 17 women
orated into the scheme to provide (15 with stress incontinence and two
information on the number of con- with other bladder problems). They rep-
tractions an individual should per- orted a mean lift of 5.5 mm with a PFM
form at each exercise session to predict contraction which compares well with
‘overload’. Previous studies have sugg- the 5.0 mm lift observed in incontinent
ested a wide range of daily contractions; women in this study (6.0 mm for cont-
Benvenuti et al (1987) proposed 120 daily inent subjects).
PFM contractions whereas Bø et al (1989)
used 8 to 12 daily contractions, and these Validity Study 2
recommendations appeared to be made This study aimed to validate the subjective
at random. The present study proposes digital assessment of P (pressure/power)
patient-specific exercise programmes, as and E (endurance) and to compare
practised in other physiotherapy regimens the sensitivity between digital and
for muscle dysfunction. The number of perineometric techniques in a large
repetitions gives further information on sample of women (n = 233), most of
fatigue; Edwards (1978) states that fatigue whom were incontinent.
is failure to maintain the expected force Accuracy of the digital method was
with continued or repeated contractions. demonstrated by the highly significant
It is postulated that the last component, correlation of P with maximum pressure
F -- number of fast contractions, provides (r = 0.786; p < 0.001), and E with the area
a measure of fast-fibre activity. Millard under the pressure curve (r = 0.549;
(1987) was possibly the first to recognise p < 0.001) as recorded by a perineo-
the importance of practising fast and slow meter. This evidence lends support to the
PFM contractions. validity of the digital method. These
Compared with other studies (Hend- findings are reinforced by the study by
rickson, 1981; Graber et al, 1981; Worth et Brink et al (1989) of 388 older women
al, 1986; Brink et al, 1989), the PERFECT (mean age 67.5), who showed significant
method gives the examiner more flex- positive correlation between digital
ibility and is less ambiguous. pressure scores and electromyography
(EMG) scores (r = 0.60; p < 0.01).
Validity Study 1 Further support for the digital tech-
PFM digital assessment of strength is nique is given in a study (N = 263)
represented by P (power/pressure), comparing digital scores (modified
which is thought to manifest itself Oxford scale) and pressure (using the
with both squeeze pressure and lift. pelvic floor exerciser/perineometer –
Consequently, it was decided to examine PFX), where good agreement between
the ‘lift’ component of an MVC in this the two techniques was demonstrated
study. The sample number is small (n = 8) (Isherwood and Rane, 2000).
and so the results should be interpreted To assess endurance digitally the
with caution, but analysis of the data examiner must be able to detect a
showed a positive and significant reduction in pressure during a 10-second
correlation between perineal lift and MVC, at which point the time (in
digital assessment scores (r = 0.864). This seconds) is recorded. Digital measures
theory would endorse the postural are admittedly less sensitive than
function of the PFM in supporting the perineometric measures, due largely to
proximal urethra, with reduced support, the subjective nature of the test and the
causing bladder neck descent on difficulty in gauging small changes in
coughing, precipitating incontinence. It is pressure. In addition, the area under the
postulated that continuous activity pressure curve is a record of total pressure
(resting tone) of the slow-twitch fibres recorded during the ten-second MVC
should maintain the advantageous (even though it may fluctuate), whereas
position of the bladder neck and E is an estimation of the time an MVC
proximal urethra, with the fast-twitch can be held at the maximum level. This
fibres reflexly recruited to provide a disparity of measurement is reflected in
quick, strong re-enforcement of urethral the reduced (but still highly significant)
lift and squeeze, during, for example, correlation (r = 0.549; p < 0.001). The
coughing. Bladder neck lift was also highly significant differences in both
reported by Vierhout and Jansen (1989) P and E values between continent
Physiotherapy December 2001/vol 87/no 12
Professional articles 641
and incontinent women suggest that personality and lifestyle of individual
these measures are important in the subjects. The number and type of daily
maintenance of continence. repetitions will depend on the initial
assessment, and several sessions per day
Reliability Studies are suggested. This is contrary to general
Inter-examiner reliability was tested on muscle training programmes (2 to 5
ten subjects examined by JL and SHD on sessions per week for athletes) but is
the same visit and showed significantly considered necessary when dealing with a
high coefficients of correlation between flat muscle with a small cross-sectional
the two examiners for all four com- area, as such a muscle is easily fatigued.
ponents of the assessment with the Fitness relates to the amount of work a
greatest discrepancy in assessing the muscle can produce and the time it takes
number of repetitions. This discrepancy to recover (Reilly, 1981) and so careful
may be explained by the different levels of planning to ensure overload, but avoiding
rapport between patient and examiner excess fatigue, is essential. A poor per-
leading to a variable effort on the part of formance due to inadequate rest can be
the patient. Furthermore, there is a demoralising for both an athlete and an
learning curve involved with any new incontinent woman; furthermore,
assessment technique and variability may PFM fatigue may lead to a temporary
be due to differing length of experience aggravation of urinary symptoms.
between the two examiners. Muscle weakness leads to reduction in
mitochondrial oxidative capacity as
Exercise Programme Planning indicated by a decrease in the succinate
The plethora of PFM exercise regimens dehydrogenase (SDH) activity (Eriksson
in the literature indicates a lack of and Haggmark, 1979). Consequently,
standardisation and, when compared with these same authors maintain that it is
general rehabilitation methodology, the necessary to gradually increase the SDH
reports show lack of scientific application. reserves by repeated contractions which
There is a wide range of muscular will deplete levels and stimulate greater
strength and endurance across any female production. This reinforces the theory of
population, and so it is postulated that a overload and supports the need for a
uniform, standard regimen is not programme of regular daily contractions
appropriate. Instead, assessment of the advanced in this study.
fast- and slow-twitch components, leading The proposed PERFECT assessment
to an individual exercise programme, has scheme has the disadvantage of appearing
been proposed, to target specifically the complicated and some therapists may well
weakness of each individual patient. prefer a simpler technique. On the other
Rehabilitation is implemented at the level hand, many patients appreciate the
appropriate to the patient, and rationale behind the assessment
progressed sequentially as power and and individual exercise programme,
endurance increase; progression is guided and respond accordingly. Due to the
by continuous re-assessment. Recently, it subjectivity of the tests, especially
is believed that there is co-contraction of evaluation of strength, standardised
transversus abdominis during a PFM training is required to enable this scheme
contraction (Sapsford et al, 2001) and to be used in any multi-centre studies, to
it is recommended that this is now ensure accurate data collection. However,
incorporated into treatment protocols. individual clinicians should be able to
The recommendations outlined above detect a change in any of the four
have not been tested clinically, and may parameters from the information
need modification to cater for the contained in this report.
References Bø, K, Hagen, R, Jorgensen, J et al (1989).
Benvenuti, F, Caputo, G M, Bandenelli, S et al ‘The effect of two different pelvic floor muscle
(1987). ‘Re-educative treatment of female exercise programs in the treatment of urinary
genuine stress incontinence’, American Journal stress incontinence in women’, Neurourology
of Obstetrics and Gynecology, 154, 1, 58-64. and Urodynamics, 8, 4, 355-356.
Bland, J M and Altman, D G (1999). Brink, C A, Sampselle, C M, Wells, T J et al
‘Measuring agreement in method comparison (1989). ‘A digital test for pelvic muscle
studies’, Statistical Methods in Medical Research, strength in older women with urinary
8, 135-160. incontinence’, Nursing Research, 38, 196-199.
Physiotherapy December 2001/vol 87/no 12
642
Chiarelli, P (1989). ‘Women’s waterworks: Jones, D A and Rutherford, O M (1987).
Curing incontinence’, Century Magazines, New ‘Human muscle strength training: The effects
South Wales. of three different regimes and the nature of
Edwards, R H T (1978). ‘Physiological analysis the resultant changes’, Journal of Physiology,
of skeletal muscle weakness and fatigue’, 391, 1-11.
Clinical Science and Molecular Medicine, 54, Kegel, A H (1948). ‘Progressive resistance
463-470. exercise in the functional restoration of the
Eriksson, E and Haggmark, T (1979). perineal muscles’, American Journal of Obstetrics
‘Comparison of isometric muscle training and and Gynecology, 56, 238.
electrical stimulation supplementing isometric Kegel, A H (1956). ‘Early genital relaxation:
muscle training in the recovery after major New technique of diagnosis and non-surgical
ligament surgery’, American Journal of Sports treatment’, Obstetrics and Gynecology, 8, 545-550.
Medicine, 7, 169-171. Khullar, V (2002). ‘Investigations’ in:
Gilpin, S A, Gosling, J A, Smith, A R B et al Laycock, J and Haslam, J (eds) Therapeutic
(1989). ‘The pathogenesis of genito-urinary Management of Incontinence and Pelvic Pain,
prolapse and stress incontinence of urine: Springer-Verlag, London, in press.
A histological and histochemical study’, British Laycock, J and Jerwood, D (1994).
Journal of Obstetrics and Gynaecology, 96, 31-38. ‘Development of the Bradford perineometer’,
Gosling, J A, Dixon, J S and Humpherson, J R Physiotherapy, 80, 139-142.
(1981). ‘A comparative study of the human Millard, R J (1987). Overcoming Incontinence,
external sphincter and periurethral levator ani Thorsons, Wellingborough, page 21.
muscles’, Journal of Urology, 53, 35-41.
Miller, J, Ashton-Miller, J and DeLancey, J O L
Graber, B, Kline-Graber, G and Golden, C J (1996). ‘The knack: Use of precisely-timed
(1981). ‘A circumvaginal muscle nomogram: pelvic muscle contraction can reduce leakage
A new diagnostic tool for evaluation of sexual in SUI’, Neurourology and Urodynamics, 15, 4,
dysfunction’, Journal of Psychiatry, 42, 157-161. 392-393.
Haslam, J (2002). ‘Biofeedback’ in: Laycock, J Reilly, T (1981). Sports Fitness and Sports
and Haslam, J (eds)Therapeutic Management of Injuries, Faber and Faber, London.
Incontinence and Pelvic Pain, Springer-Verlag,
London, in press. Sapsford, R R, Hodges, P W, Richardson, C A
et al (2001). ‘Co-activation of the abdominal
Hendrickson, L S (1981). ‘The frequency of and pelvic floor muscles during voluntary
stress incontinence in women before and after exercises’, Neurourology and Urodynamics, 20,
the implementation of an exercise program’, 31-42.
Issues in Health Care of Women, 3, 81-92.
Vierhout, M E and Jansen, H (1989). ‘Supine
Isherwood, P J and Rane, A (2000). and sitting transrectal ultrasonographic
‘Comparative assessment of pelvic floor evaluation of the bladder neck during
strength using a perineometer and digital relaxation, straining and squeezing’,
examination’, British Journal of Obstetrics and Neurourology and Urodynamics, 8, 301-302.
Gynaecology, 107, 1007-11.
Worth, A M, Dougherty, M C and McKey, P L
Jahnke, M T, Proske, U and Struppler, A (1986). ‘Development and testing of the
(1989). ‘Measurements of muscle stiffness, the circumvaginal muscles rating scale’, Nursing
electromyogram and activity in single muscle Research, 35, 3, 166-168.
spindles of human muscles following
conditioning by passive stretch or contraction’,
Brain Research, 493, 103-112.
Key Messages
■ Digital assessment of the contractility ■ The PERFECT assessment is easy to
of PFM can be carried out during perform, reliable and reproducible.
vaginal examination.
■ The assessment scheme described
■ Assessment should include evaluation provides information for a patient-
of PFM strength and endurance, and specific exercise programme.
reflex activity (during cough).
Physiotherapy December 2001/vol 87/no 12
You might also like
- Effects of Isometric, Eccentric, or Heavy Slow Resistance Exercises On Pain and Function With PTDocument15 pagesEffects of Isometric, Eccentric, or Heavy Slow Resistance Exercises On Pain and Function With PTTomBramboNo ratings yet
- A Clinical Tool For Office Assessment of Lumbar Spine Stabilization Endurance PDFDocument7 pagesA Clinical Tool For Office Assessment of Lumbar Spine Stabilization Endurance PDFNicolas BavarescoNo ratings yet
- Isoinercial Performance 2018Document12 pagesIsoinercial Performance 2018abcsouzaNo ratings yet
- Evaluating Abdominal Core Muscle Fatigue: Assessment of The Validity and Reliability of The Prone Bridging TestDocument9 pagesEvaluating Abdominal Core Muscle Fatigue: Assessment of The Validity and Reliability of The Prone Bridging TestOMAR ANDRES OSORIO GARCIANo ratings yet
- Attr 39 03 0254Document5 pagesAttr 39 03 0254Bryan HuaritaNo ratings yet
- Hamstring Stretches Frequency Required To Maintain Knee Extension Range of MotionDocument8 pagesHamstring Stretches Frequency Required To Maintain Knee Extension Range of MotionRabiaNo ratings yet
- 3 Chiropractic Subluxation IndicatorsDocument46 pages3 Chiropractic Subluxation IndicatorsMário Ornelas100% (3)
- Tens For DomsDocument5 pagesTens For DomsVanadia NohanNo ratings yet
- Leer Sí o SíDocument9 pagesLeer Sí o SíAngelika Carolina Pineda JuncoNo ratings yet
- 1 s2.0 S1388245704000975 MainDocument12 pages1 s2.0 S1388245704000975 MainpashaNo ratings yet
- Work-Related Thumb Pain in Physiotherapists Is Associated With Thumb Alignment During Performance of PA PressuresDocument5 pagesWork-Related Thumb Pain in Physiotherapists Is Associated With Thumb Alignment During Performance of PA PressuresQuiroprácticaParaTodosNo ratings yet
- Applied Kinesiology Research Articles I Ak Research Compendium DR Scott Cuthbert 10-08-11 LatestDocument218 pagesApplied Kinesiology Research Articles I Ak Research Compendium DR Scott Cuthbert 10-08-11 LatestMOTION ARGENTINANo ratings yet
- Article AR MyotonProDocument10 pagesArticle AR MyotonProzeladazulNo ratings yet
- Serratus Anterior Muscle Strength and Endurance TestsDocument12 pagesSerratus Anterior Muscle Strength and Endurance Testsrudhras22No ratings yet
- Applied Kinesiology and The Cervical SpineDocument5 pagesApplied Kinesiology and The Cervical SpineScott CuthbertNo ratings yet
- Adaptive Responses To Muscle Lengthening and Shortening in HumansDocument8 pagesAdaptive Responses To Muscle Lengthening and Shortening in Humansrafaeldfonseca09No ratings yet
- Lopez 2021Document9 pagesLopez 2021toaldoNo ratings yet
- Andersen2017 (Elastic Shoulder Test)Document8 pagesAndersen2017 (Elastic Shoulder Test)kineluzaNo ratings yet
- Comparison of Cranio-Cervical Flexion Training Versus Cervical Proprioception Training in Pt's With Chronic Neck PainDocument8 pagesComparison of Cranio-Cervical Flexion Training Versus Cervical Proprioception Training in Pt's With Chronic Neck Painbcvaughn019No ratings yet
- Nuevo Método de Imagen para Evaluar La Biomecánica Del SDocument5 pagesNuevo Método de Imagen para Evaluar La Biomecánica Del SLargo FlacoNo ratings yet
- Artigo AssociationbetweenregionaldiVerencesinmuscleactivation1Document8 pagesArtigo AssociationbetweenregionaldiVerencesinmuscleactivation1krissiecbsNo ratings yet
- Inter-Rater and Test-Retest Reliability of Hand Held Dynamometer in Shoulder DysfunctionDocument6 pagesInter-Rater and Test-Retest Reliability of Hand Held Dynamometer in Shoulder DysfunctionNurfitrianti ArfahNo ratings yet
- Mdivion Con Tensiometro 2Document6 pagesMdivion Con Tensiometro 2Carrera De Fisioterapia ManabíNo ratings yet
- Manual Therapy: Hiroshi Takasaki, Takeshi Iizawa, Toby Hall, Takuo Nakamura, Shouta KanekoDocument6 pagesManual Therapy: Hiroshi Takasaki, Takeshi Iizawa, Toby Hall, Takuo Nakamura, Shouta KanekoDiego Cruces OrdoñezNo ratings yet
- Jurnal CCFTDocument8 pagesJurnal CCFTfi.afifah NurNo ratings yet
- NormativeDocument9 pagesNormativeEdher Pliego100% (1)
- Musc UlosDocument8 pagesMusc Ulosangiw fuentesNo ratings yet
- Reliability and Validity Assessment of A Linear Position TransducerDocument9 pagesReliability and Validity Assessment of A Linear Position TransducerAlexandre FerreiraNo ratings yet
- Mini Research-3Document14 pagesMini Research-3Debashis SamantarayNo ratings yet
- The Effects of Proprioceptive or Strength Training On The Neuromuscular Function of The ACL Reconstructed Knee - A Randomized Clinical TrialDocument9 pagesThe Effects of Proprioceptive or Strength Training On The Neuromuscular Function of The ACL Reconstructed Knee - A Randomized Clinical Trialsabilillah putri63No ratings yet
- 23 247Document4 pages23 247Ita MagdalenaNo ratings yet
- WestsideDocument7 pagesWestsideBrandon C WilliamsNo ratings yet
- Proprioception in Musculoskeletal Rehabilitation2Document10 pagesProprioception in Musculoskeletal Rehabilitation2Santiago Cubillos EscobarNo ratings yet
- A Study of Grip Endurance and Strengh in Different Elbow PositionsDocument3 pagesA Study of Grip Endurance and Strengh in Different Elbow Positions伊文超No ratings yet
- Diafragma Ant Posterior ChainDocument7 pagesDiafragma Ant Posterior ChainJulijus MotiejunasNo ratings yet
- The Effects of Kinesio-Taping On Quadriceps Strength During Isokinetic Exercise in Healthy Non Athlete WomenDocument6 pagesThe Effects of Kinesio-Taping On Quadriceps Strength During Isokinetic Exercise in Healthy Non Athlete WomenSurya DiatmikaNo ratings yet
- The Belly-Press Test For The Physical ExaminationDocument5 pagesThe Belly-Press Test For The Physical ExaminationLucyFloresNo ratings yet
- Effect of Task-Oriented Training With and Without Trunk Restraint On Reaching Activity in Adult HemipareticsDocument5 pagesEffect of Task-Oriented Training With and Without Trunk Restraint On Reaching Activity in Adult HemipareticsMunni KNo ratings yet
- WORRELL Et Al., 1994Document6 pagesWORRELL Et Al., 1994Ismenia HelenaNo ratings yet
- Estudio Sobre IsquiosuralesDocument2 pagesEstudio Sobre IsquiosuralesEdu Plaza AlvearNo ratings yet
- Respiratory Physiology & Neurobiology: Short CommunicationDocument4 pagesRespiratory Physiology & Neurobiology: Short CommunicationAnonymous rlZ9gm8HnNo ratings yet
- Effect of Submaximal Contraction Intensity in Contract-Relax Proprioceptive Neuromuscular Facilitation StretchingDocument2 pagesEffect of Submaximal Contraction Intensity in Contract-Relax Proprioceptive Neuromuscular Facilitation StretchingI Made Dhita PriantharaNo ratings yet
- Manual Therapy: Anna Bjerkefors, Maria M. Ekblom, Karin Josefsson, Alf ThorstenssonDocument6 pagesManual Therapy: Anna Bjerkefors, Maria M. Ekblom, Karin Josefsson, Alf ThorstenssonnoxlonNo ratings yet
- Mitchell Et Al. (2009) Reflex Mechanisms Lack of ContributionDocument16 pagesMitchell Et Al. (2009) Reflex Mechanisms Lack of ContributionRafael RodriguesNo ratings yet
- (18997562 - Journal of Human Kinetics) Influence of Exercise Order On Electromyographic Activity During Upper Body Resistance TrainingDocument8 pages(18997562 - Journal of Human Kinetics) Influence of Exercise Order On Electromyographic Activity During Upper Body Resistance TrainingGOVARDHANNo ratings yet
- Quadriceps - Anatomia (US)Document9 pagesQuadriceps - Anatomia (US)LiggieriNo ratings yet
- Accepted ManuscriptDocument17 pagesAccepted ManuscriptFayza RihastaraNo ratings yet
- The Effectiveness of Spinal Manipulation in Increasing Muscle Strength in Healthy Individuals A Systematic Review and Meta-AnalysisDocument11 pagesThe Effectiveness of Spinal Manipulation in Increasing Muscle Strength in Healthy Individuals A Systematic Review and Meta-Analysisdummyy1256No ratings yet
- NG 2007Document8 pagesNG 2007Nacho MicheloniNo ratings yet
- Pulsed Electromagnetic Field in Patients With Shoulder Impingement SyndromeDocument6 pagesPulsed Electromagnetic Field in Patients With Shoulder Impingement SyndromeHanna RikaswaniNo ratings yet
- Maia Et Al. 2014. Effects - of - Different - Rest - Intervals - Between APS Training - JSCRDocument7 pagesMaia Et Al. 2014. Effects - of - Different - Rest - Intervals - Between APS Training - JSCRAbimael Corrêa da SilvaNo ratings yet
- Reliability and Validity of The Modified Sphygmomanometer Test For The Assessment of Strength of Upper Limb Muscles After StrokeDocument9 pagesReliability and Validity of The Modified Sphygmomanometer Test For The Assessment of Strength of Upper Limb Muscles After Strokechocolate cupcakeNo ratings yet
- Ashwort Scale Vs Tone AssessmentDocument4 pagesAshwort Scale Vs Tone Assessmentdezi981No ratings yet
- tjp0584 1019Document10 pagestjp0584 1019SportsciencesNo ratings yet
- Physical Therapy in Sport: Tom K. Tong, Shing Wu, Jinlei NieDocument6 pagesPhysical Therapy in Sport: Tom K. Tong, Shing Wu, Jinlei NieEstebanAspéeNo ratings yet
- Coo Rev Its 2008Document9 pagesCoo Rev Its 2008AdosotoNo ratings yet
- Muscle Contractile Characteristic Relationship To High-IntensityDocument6 pagesMuscle Contractile Characteristic Relationship To High-IntensityCharisNo ratings yet
- Cavallo - CAPESB 2021Document2 pagesCavallo - CAPESB 2021tanvir anwarNo ratings yet
- Townsend 1991Document9 pagesTownsend 1991Jaime SotoNo ratings yet
- Manual of Vibration Exercise and Vibration TherapyFrom EverandManual of Vibration Exercise and Vibration TherapyJörn RittwegerNo ratings yet
- IELTS Listening Test 3: Part 1: Questions 1-10 NUMBER For Each Answer Job InquiryDocument5 pagesIELTS Listening Test 3: Part 1: Questions 1-10 NUMBER For Each Answer Job InquiryAvinash SinghNo ratings yet
- G.R. No. 130547 REYES VS ISTER S OF MERCYDocument8 pagesG.R. No. 130547 REYES VS ISTER S OF MERCYChristine Lory Ruiz AgravanteNo ratings yet
- Complementaria 2. Communication Partner Training in Aphasia An Updated Systematic ReviewDocument58 pagesComplementaria 2. Communication Partner Training in Aphasia An Updated Systematic ReviewCarlonchaCáceresNo ratings yet
- All UL Systems - White Paper - Toshiba White Paper Library (2017 Dec)Document4 pagesAll UL Systems - White Paper - Toshiba White Paper Library (2017 Dec)Арнольд ЧайкоNo ratings yet
- Shs Week 2022 2023Document7 pagesShs Week 2022 2023Kee JeiNo ratings yet
- APS Safety Plan UpdateDocument1 pageAPS Safety Plan UpdateWews WebStaffNo ratings yet
- Research ParticipantsDocument11 pagesResearch ParticipantsJaylineMaeNionesCaminero100% (1)
- Ayush Universities CoursesDocument1 pageAyush Universities CoursesSayem Al MamunNo ratings yet
- Submission Policies For Psychology of Violence Journal APADocument2 pagesSubmission Policies For Psychology of Violence Journal APAJohnNo ratings yet
- Airway Anatomy & Airway Equipment: Presenter - DR Savita SR - DR Faisal Moderator-Dr ShalviDocument48 pagesAirway Anatomy & Airway Equipment: Presenter - DR Savita SR - DR Faisal Moderator-Dr ShalvilakhwinderNo ratings yet
- CH 2Document20 pagesCH 2Vivek SinghNo ratings yet
- Impaired Verbal CommunicationDocument2 pagesImpaired Verbal CommunicationMart AlunanNo ratings yet
- Healthcare Marketing Research Paper TopicsDocument8 pagesHealthcare Marketing Research Paper Topicsthrbvkvkg100% (1)
- Act 3 - GRP 3 - Beed 3BDocument38 pagesAct 3 - GRP 3 - Beed 3BJessabel ColumnaNo ratings yet
- Ectopic PregnancyDocument11 pagesEctopic PregnancyPrincess BalloNo ratings yet
- HSS 3103 Exam Review PDFDocument9 pagesHSS 3103 Exam Review PDFAyman WNo ratings yet
- Resume of S. Sawvik Mittra: Career ObjectivesDocument4 pagesResume of S. Sawvik Mittra: Career ObjectivesSawvik MittraNo ratings yet
- FIQ - Retinal Vein OcclusionDocument31 pagesFIQ - Retinal Vein OcclusionHikban FiqhiNo ratings yet
- HRM Assignment 01-322191-014 PDFDocument6 pagesHRM Assignment 01-322191-014 PDFMuhammad MuzammalNo ratings yet
- Divyamrutayurcare ComDocument2 pagesDivyamrutayurcare ComKothariTech WorkNo ratings yet
- Read The Article About Facial Transplants and Complete The Notes Under The Headings GivenDocument2 pagesRead The Article About Facial Transplants and Complete The Notes Under The Headings GivenAbdulla YaaminNo ratings yet
- SPORTS: An Introduction: Modified Learning Materials/Modules Based On The Deped CurriculumDocument15 pagesSPORTS: An Introduction: Modified Learning Materials/Modules Based On The Deped Curriculumgemma marcitoNo ratings yet
- Flottorp Worksheet 2 Initial Assessment of Determinants ChecklistDocument6 pagesFlottorp Worksheet 2 Initial Assessment of Determinants ChecklistSyafira Ayudarechta Tara WenditaNo ratings yet
- Original Nursing Theories of Florence Nightingale: by Mary B. Knutson, RN, BSN, FCP MSN Student Viterbo UniversityDocument23 pagesOriginal Nursing Theories of Florence Nightingale: by Mary B. Knutson, RN, BSN, FCP MSN Student Viterbo UniversityGlorie Anne AniscoNo ratings yet
- Quality Assurance LaboratoryDocument118 pagesQuality Assurance LaboratoryMahesh KumarNo ratings yet
- AARC Asthma COPD GuidelineDocument5 pagesAARC Asthma COPD GuidelineMarcelo JunWeiNo ratings yet
- Test Bank For Nutrition For Life 3 e Janice J Thompson Melinda ManoreDocument17 pagesTest Bank For Nutrition For Life 3 e Janice J Thompson Melinda Manoreshanesmithbefqiyajrx100% (24)
- Handout On Trauma and ADHDDocument3 pagesHandout On Trauma and ADHDVicki B VeeNo ratings yet
- Mould Pune BrochureDocument11 pagesMould Pune BrochureShiva RamanNo ratings yet
- Iosh Oman Branch Agm 25052022Document94 pagesIosh Oman Branch Agm 25052022Ihab FowzyNo ratings yet