Professional Documents
Culture Documents
Bacterial Meningitis and Meningococcal Septicaemia in Under 16s Diagnosis of Bacterial Meningitis and Meningococcal Septicaemia in Secondary Care
Bacterial Meningitis and Meningococcal Septicaemia in Under 16s Diagnosis of Bacterial Meningitis and Meningococcal Septicaemia in Secondary Care
Uploaded by
Natalia E PenagosCopyright:
Available Formats
You might also like
- Pediatric NursingDocument22 pagesPediatric NursingDarren Mae MosadaNo ratings yet
- Admission LetterDocument4 pagesAdmission LetterYasir KNNo ratings yet
- Lesson Plan Lumbar PunctureDocument25 pagesLesson Plan Lumbar PunctureValarmathi50% (4)
- Bacterial Meningitis and Meningococcal Septicaemia: Implementing NICE GuidanceDocument18 pagesBacterial Meningitis and Meningococcal Septicaemia: Implementing NICE GuidanceZarwo Black UstadzNo ratings yet
- Meningitis and Lumbar PunctureDocument38 pagesMeningitis and Lumbar PunctureJeo ThomasNo ratings yet
- Fod en Niños Menores de 3 MesesDocument16 pagesFod en Niños Menores de 3 MesesPaul Gutiérrez MyrickNo ratings yet
- Diagnosis and Treatment of Bacterial Meningitis: Arch. Dis. ChildDocument7 pagesDiagnosis and Treatment of Bacterial Meningitis: Arch. Dis. Childapi-214563632No ratings yet
- Meningitis in Adults: Diagnosis and Management: PembimbingDocument45 pagesMeningitis in Adults: Diagnosis and Management: PembimbingNeny Mathilda UniplaitaNo ratings yet
- Meningitis Workup - Approach Considerations, Blood Studies, Cultures and Bacterial Antigen TestingDocument14 pagesMeningitis Workup - Approach Considerations, Blood Studies, Cultures and Bacterial Antigen TestingdilaNo ratings yet
- Guideline MeningitisDocument1 pageGuideline MeningitisAmbc Smfk-uaj100% (1)
- Infectiousdiseases 130804135335 Phpapp02Document42 pagesInfectiousdiseases 130804135335 Phpapp02OleOhhNo ratings yet
- Investigating Procalcitonin and C-Reactive Protein As Diagnostic Biomarkers in Pediatric Suspected Meningitis: A Forward-Looking Observational AnalysisDocument16 pagesInvestigating Procalcitonin and C-Reactive Protein As Diagnostic Biomarkers in Pediatric Suspected Meningitis: A Forward-Looking Observational AnalysisInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Bacterial Meningitis in Children - DynaMedDocument88 pagesBacterial Meningitis in Children - DynaMedCarlos CalderwoodNo ratings yet
- Reflective Journal ReadingDocument13 pagesReflective Journal Readingعبداللة العمراني الحويطيNo ratings yet
- Bacterial Meningitis in AdultsDocument55 pagesBacterial Meningitis in AdultsfjnaressiNo ratings yet
- The Febrile Infant 29 To 90 Days of Age Management UpToDateDocument74 pagesThe Febrile Infant 29 To 90 Days of Age Management UpToDateSharafuddin SalimiNo ratings yet
- Serum Procalcitonin Levels in Bacterial and Abacterial MeningitisDocument5 pagesSerum Procalcitonin Levels in Bacterial and Abacterial MeningitisSaul Gonzalez HernandezNo ratings yet
- Meningitis PresentationDocument41 pagesMeningitis PresentationO'Mark AndrewsNo ratings yet
- Bacterial Meningitis in Infants Over 3 Months of AgeDocument8 pagesBacterial Meningitis in Infants Over 3 Months of AgedrirrazabalNo ratings yet
- Newborn Sepsis GuidelineDocument2 pagesNewborn Sepsis GuidelineAmelia ArnisNo ratings yet
- Treatment of Children With COVID-19: Position Paper of The Italian Society of Pediatric Infectious DiseaseDocument17 pagesTreatment of Children With COVID-19: Position Paper of The Italian Society of Pediatric Infectious DiseasecurteanancaNo ratings yet
- Covid Ep IiDocument29 pagesCovid Ep IiLuis Armando López SosaNo ratings yet
- Neonatal InfectionsDocument41 pagesNeonatal Infectionsamid sultanNo ratings yet
- Evaluation and Management of Suspected Sepsis and Septic Shock in AdultsDocument48 pagesEvaluation and Management of Suspected Sepsis and Septic Shock in AdultsIsmael IbrahimNo ratings yet
- Neonatal Sepsis: Prof DR Saima BatoolDocument31 pagesNeonatal Sepsis: Prof DR Saima BatoolSAIMA BATOOLNo ratings yet
- TREATMENT Bacterial MeningitisDocument32 pagesTREATMENT Bacterial MeningitisironNo ratings yet
- Research Paper On Bacterial MeningitisDocument8 pagesResearch Paper On Bacterial Meningitisvvgnzdbkf100% (1)
- Case 10 Fever PDFDocument5 pagesCase 10 Fever PDFSue HuangNo ratings yet
- Test ID: PCT Procalcitonin, Serum: Useful ForDocument5 pagesTest ID: PCT Procalcitonin, Serum: Useful ForI Nyoman Gede SemarajanaNo ratings yet
- Research Paper Bacterial MeningitisDocument4 pagesResearch Paper Bacterial Meningitisafeebovus100% (1)
- Bacterial Meningitis ThesisDocument8 pagesBacterial Meningitis ThesisRick Vogel100% (2)
- 35-Article Text-212-1-10-20200524Document4 pages35-Article Text-212-1-10-20200524SONIA AGUILAR RIVERANo ratings yet
- Clin Infect Dis. 2004 Tunkel 1267 84 Idsa MeningitiDocument18 pagesClin Infect Dis. 2004 Tunkel 1267 84 Idsa MeningitiJesus Salvador SerratoNo ratings yet
- Tuberculosis in ChildrenDocument4 pagesTuberculosis in ChildrenMarthin TheservantNo ratings yet
- Bacterial Meningitis in ChildrenDocument10 pagesBacterial Meningitis in ChildrenAnny AryanyNo ratings yet
- Sepsis NeonatalDocument21 pagesSepsis NeonatalRaissa 'Icha' Nurwany RizalNo ratings yet
- Diagnostics: CBC, CRP, UA, PCR, LAT, Blood Cultures CSF: With Opening Pressure, Procalcitonin and SerologyDocument4 pagesDiagnostics: CBC, CRP, UA, PCR, LAT, Blood Cultures CSF: With Opening Pressure, Procalcitonin and SerologyChoi SpeaksNo ratings yet
- Covid 19 Pediatric Multi System Inflammatory SyndromeDocument2 pagesCovid 19 Pediatric Multi System Inflammatory SyndromeministerenqiNo ratings yet
- Guia IDSA-Practice Guidelines For The Management of Bacterial Meningitis-2004Document18 pagesGuia IDSA-Practice Guidelines For The Management of Bacterial Meningitis-2004Brenda Anali Pariona NapaNo ratings yet
- Neonatal SepsisDocument31 pagesNeonatal Sepsisanwar jabariNo ratings yet
- (Methods in Molecular Medicine) Andrew J. Pollard, Martin C.J. Maiden - Meningococcal Disease (2001, Humana Press)Document662 pages(Methods in Molecular Medicine) Andrew J. Pollard, Martin C.J. Maiden - Meningococcal Disease (2001, Humana Press)gnkgbjkgjkNo ratings yet
- PCAP ReportDocument28 pagesPCAP ReportAngeline Zamoras-ToledoNo ratings yet
- Neonatal SepsisDocument5 pagesNeonatal SepsisBhawna PandhuNo ratings yet
- Bacterial MeningitisDocument51 pagesBacterial MeningitiscaseinrenninNo ratings yet
- Bacterial Meningitis in The Neonate - Neurologic Complications - UpToDateDocument9 pagesBacterial Meningitis in The Neonate - Neurologic Complications - UpToDateAngélica PedrazaNo ratings yet
- Meningitis PDFDocument8 pagesMeningitis PDFrizeviNo ratings yet
- Frequency of Thrombocytopenia in Neonatal Sepsis: Dr. Nadia GulDocument9 pagesFrequency of Thrombocytopenia in Neonatal Sepsis: Dr. Nadia GulNaeem NawazNo ratings yet
- Bacterial MeningitisDocument5 pagesBacterial Meningitisjamesignacio787No ratings yet
- ENLS Meningitis and Encephalitis ProtocolDocument20 pagesENLS Meningitis and Encephalitis ProtocolFransiskus MikaelNo ratings yet
- MengititisDocument38 pagesMengititisRas Siko SafoNo ratings yet
- Neonatal Meningitis Due To Clostridium Neonatale: A Case ReportDocument4 pagesNeonatal Meningitis Due To Clostridium Neonatale: A Case ReportCarina ColtuneacNo ratings yet
- MMC 1Document9 pagesMMC 1Maulida 04No ratings yet
- Jurnal AsliDocument8 pagesJurnal AsliDwi PurwantiNo ratings yet
- Sepsis in The Newborn - Latest NewsDocument13 pagesSepsis in The Newborn - Latest NewsBrunaNo ratings yet
- Neonatal SepsisDocument5 pagesNeonatal SepsisLeana SiñelNo ratings yet
- Clinical Features: - Initial Symptoms in Patients With MeningitisDocument12 pagesClinical Features: - Initial Symptoms in Patients With Meningitisyuii_48No ratings yet
- Meningitis in Adults - Diagnosis and Management - Young - 2018 - Internal Medicine Journal - Wiley Online LibraryDocument27 pagesMeningitis in Adults - Diagnosis and Management - Young - 2018 - Internal Medicine Journal - Wiley Online Libraryaslan tonapaNo ratings yet
- Meningitis: By-Dr Nimco A. MDDocument31 pagesMeningitis: By-Dr Nimco A. MDgibreilNo ratings yet
- C V 9 V VV VV V V VVVVVVVV V: "V "V "V "V "VDocument2 pagesC V 9 V VV VV V V VVVVVVVV V: "V "V "V "V "VCharlene Mae CalanoyNo ratings yet
- Paediatrica Indonesiana: Original ArticleDocument5 pagesPaediatrica Indonesiana: Original ArticleSyukron AmrullahNo ratings yet
- Peds InfectiousDocument8 pagesPeds InfectiousMohammad RammalNo ratings yet
- COVID-19 Mortality Review in Malaysia & Updates on Clinical Management of COVID-19From EverandCOVID-19 Mortality Review in Malaysia & Updates on Clinical Management of COVID-19No ratings yet
- Living on the Frontline of COVID-19 in MCO And CMCOFrom EverandLiving on the Frontline of COVID-19 in MCO And CMCONo ratings yet
- Stroke Differential Diagnosis and Mimics: Part 2Document9 pagesStroke Differential Diagnosis and Mimics: Part 2Natalia E PenagosNo ratings yet
- Seizure Pediatric Scenario June 2016Document4 pagesSeizure Pediatric Scenario June 2016Natalia E PenagosNo ratings yet
- Ene 15103Document8 pagesEne 15103Natalia E PenagosNo ratings yet
- Dom 14270Document19 pagesDom 14270Natalia E PenagosNo ratings yet
- Epilepsy Imaging: Approaches and ProtocolsDocument9 pagesEpilepsy Imaging: Approaches and ProtocolsNatalia E PenagosNo ratings yet
- Peeds Infection LecturesDocument190 pagesPeeds Infection LecturesAli Al.JuffairiNo ratings yet
- 282585293Document208 pages282585293hebaNo ratings yet
- Infections FarazDocument10 pagesInfections FarazM R SIFATNo ratings yet
- Lumbar Puncture ResearchDocument6 pagesLumbar Puncture Researchanon_464104226No ratings yet
- CDDocument6 pagesCDMei JoyNo ratings yet
- اسئلة neuroDocument30 pagesاسئلة neuroSoad RedaNo ratings yet
- Brain AbscessDocument2 pagesBrain AbscessIan RomanNo ratings yet
- Stool Analysis and Other Body Fluid AnalysisDocument51 pagesStool Analysis and Other Body Fluid AnalysisPutri Senna Rahayu100% (2)
- 83K English Class Examination Questions of Infectious DiseaseDocument23 pages83K English Class Examination Questions of Infectious Diseasetarun956519No ratings yet
- Intrathecal Hyaluronidase in TB Meningitis: The Unexplored AdjuvantDocument5 pagesIntrathecal Hyaluronidase in TB Meningitis: The Unexplored AdjuvantPriyanka SamalNo ratings yet
- Idr 240162 Management of Acute Bacterial Meningitis in ChildrenDocument13 pagesIdr 240162 Management of Acute Bacterial Meningitis in ChildrenindahrizkygNo ratings yet
- Epidemiology and Management Og Meningococcal MeningitisDocument12 pagesEpidemiology and Management Og Meningococcal MeningitispriyankaNo ratings yet
- Epidemic Cerebrospinal MeningitisDocument76 pagesEpidemic Cerebrospinal MeningitisAngie LawrenceNo ratings yet
- Some Imp Oneliner From VolumesDocument16 pagesSome Imp Oneliner From VolumesTejas KaleNo ratings yet
- Cases Lab 2020Document16 pagesCases Lab 2020Buushi96No ratings yet
- B) Meningococcal MeningitisDocument7 pagesB) Meningococcal MeningitisWe'am QutubNo ratings yet
- MCQ April 2015Document15 pagesMCQ April 2015Sylphana Astharica LawalataNo ratings yet
- Writing Notes: The Ideal Letter Should Have 6 PartsDocument7 pagesWriting Notes: The Ideal Letter Should Have 6 PartsMMW MNo ratings yet
- C CA AS SC CL Liin Niiq QU UE E // C CA AS SE ER RE EP PO OR RT TDocument7 pagesC CA AS SC CL Liin Niiq QU UE E // C CA AS SE ER RE EP PO OR RT TG Virucha Meivila IINo ratings yet
- Meningitis ViralDocument7 pagesMeningitis ViralTia Gustiani Poplei ViolaNo ratings yet
- Communicable Disease ChartDocument5 pagesCommunicable Disease ChartAuspice QatarNo ratings yet
- ENLS Meningitis and Encephalitis ProtocolDocument20 pagesENLS Meningitis and Encephalitis ProtocolFransiskus MikaelNo ratings yet
- Abdullahi V Pfizer Inc PDFDocument44 pagesAbdullahi V Pfizer Inc PDFBevs DomingoNo ratings yet
- Brain InfectionDocument61 pagesBrain Infectionmanisha paikarayNo ratings yet
- Blog Post About National Poultry Day 2023Document63 pagesBlog Post About National Poultry Day 2023ZETTYNo ratings yet
- Date/Time Doctors Order RationaleDocument4 pagesDate/Time Doctors Order RationaleChamCham AquinoNo ratings yet
- HAAD Test 4 QuestionsDocument17 pagesHAAD Test 4 QuestionsPhine PhineNo ratings yet
Bacterial Meningitis and Meningococcal Septicaemia in Under 16s Diagnosis of Bacterial Meningitis and Meningococcal Septicaemia in Secondary Care
Bacterial Meningitis and Meningococcal Septicaemia in Under 16s Diagnosis of Bacterial Meningitis and Meningococcal Septicaemia in Secondary Care
Uploaded by
Natalia E PenagosOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Bacterial Meningitis and Meningococcal Septicaemia in Under 16s Diagnosis of Bacterial Meningitis and Meningococcal Septicaemia in Secondary Care
Bacterial Meningitis and Meningococcal Septicaemia in Under 16s Diagnosis of Bacterial Meningitis and Meningococcal Septicaemia in Secondary Care
Uploaded by
Natalia E PenagosCopyright:
Available Formats
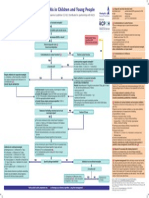
Diagnosis of bacterial meningitis and
meningococcal septicaemia in secondary care
NICE Pathways bring together everything NICE says on a topic in an interactive
flowchart. NICE Pathways are interactive and designed to be used online.
They are updated regularly as new NICE guidance is published. To view the latest
version of this NICE Pathway see:
http://pathways.nice.org.uk/pathways/bacterial-meningitis-and-meningococcal-
septicaemia-in-under-16s
NICE Pathway last updated: 29 November 2021
This document contains a single flowchart and uses numbering to link the boxes to the
associated recommendations.
Bacterial meningitis and meningococcal septicaemia in under 16s Page 1 of 16
© NICE 2022. All rights reserved. Subject to Notice of rights.
Diagnosis of bacterial meningitis and meningococcal septicaemia in secondary NICE Pathways
care
Bacterial meningitis and meningococcal septicaemia in under 16s Page 2 of 16
© NICE 2022. All rights reserved. Subject to Notice of rights.
Diagnosis of bacterial meningitis and meningococcal septicaemia in secondary NICE Pathways
care
1 Child under 16 with suspected bacterial meningitis or meningococcal
septicaemia
No additional information
2 Specific investigations and immediate treatment when petechial rash
is present
Perform a very careful examination for signs of meningitis or septicaemia in children and young
people presenting with petechial rashes (see table 1 symptoms and signs of bacterial meningitis
and meningococcal septicaemia [See page 9]).
When to give intravenous ceftriaxone
Give intravenous ceftriaxone immediately to children and young people with a petechial rash if
any of the following occur at any point during the assessment (these children are at high risk of
having meningococcal disease):
petechiae start to spread
the rash becomes purpuric
there are signs of bacterial meningitis
there are signs of meningococcal septicaemia
the child or young person appears ill to a healthcare professional.
See management in secondary care.
Child with rash and fever
If a child or young person has an unexplained petechial rash and fever (or history of fever) carry
out the following investigations:
full blood count
CRP
coagulation screen
blood culture
whole-blood PCR for N meningitidis
Bacterial meningitis and meningococcal septicaemia in under 16s Page 3 of 16
© NICE 2022. All rights reserved. Subject to Notice of rights.
Diagnosis of bacterial meningitis and meningococcal septicaemia in secondary NICE Pathways
care
blood glucose
blood gas.
Child with rash and fever but no high-risk clinical manifestations
In a child or young person with an unexplained petechial rash and fever (or history of fever) but
none of the high-risk clinical manifestations:
Treat with intravenous ceftriaxone immediately if the CRP and/or WBC count (especially
neutrophil count) is raised, as this indicates an increased risk of having meningococcal
disease.
Be aware that while a normal CRP and normal WBC count mean meningococcal disease is
less likely, they do not rule it out. The CRP may be normal and the WBC normal or low even
in severe meningococcal disease.
Assess clinical progress by monitoring vital signs (respiratory rate, heart rate, blood
pressure, conscious level (Glasgow Coma Scale and/or APVU), temperature), capillary refill
time, and oxygen saturations. Carry out observations at least hourly over the next 4–6
hours.
If doubt remains, treat with antibiotics and admit to hospital.
If the child or young person is assessed as being at low risk of meningococcal disease and is
discharged after initial observation, advise parents or carers to return to hospital if the child or
young person appears ill to them.
Child with non-spreading rash without fever who does not appear ill
Be aware that in children and young people who present with a non-spreading petechial rash
without fever (or history of fever) who do not appear ill to a healthcare professional,
meningococcal disease is unlikely, especially if the rash has been present for more than 24
hours. In such cases consider:
other possible diagnoses
performing a full blood count and coagulation screen.
Quality standards
The following quality statement is relevant to this part of the interactive flowchart.
3. Management of petechial rash
Bacterial meningitis and meningococcal septicaemia in under 16s Page 4 of 16
© NICE 2022. All rights reserved. Subject to Notice of rights.
Diagnosis of bacterial meningitis and meningococcal septicaemia in secondary NICE Pathways
care
3 Blood tests for bacterial meningitis and meningococcal disease
C-reactive protein test and white blood cell count for suspected bacterial meningitis
In children and young people with suspected bacterial meningitis, perform a CRP and WBC
count:
If the CRP and/or white blood cell count is raised and there is a non-specifically abnormal
CSF (for example consistent with viral meningitis), treat as bacterial meningitis.
Be aware that a normal CRP and WBC count does not rule out bacterial meningitis.
Regardless of the CRP and WBC count, if no CSF is available for examination or if the CSF
findings are uninterpretable, manage as if the diagnosis of meningitis is confirmed.
Polymerase chain reaction test for bacterial meningitis and meningococcal disease
Perform whole blood real-time PCR testing (EDTA sample) for N meningitidis to confirm a
diagnosis of meningococcal disease.
The PCR blood sample should be taken as soon as possible because early samples are more
likely to be positive.
Use PCR testing of blood samples from other hospital laboratories if available, to avoid
repeating the test.
Be aware that a negative blood PCR test result for N meningitidis does not rule out
meningococcal disease.
Submit CSF to the laboratory to hold for PCR testing for N meningitidis and S pneumoniae, but
only perform the PCR testing if the CSF culture is negative.
Be aware that CSF samples taken up to 96 hours after admission to hospital may give useful
results.
Quality standards
The following quality statement is relevant to this part of the interactive flowchart.
7. Blood tests
Bacterial meningitis and meningococcal septicaemia in under 16s Page 5 of 16
© NICE 2022. All rights reserved. Subject to Notice of rights.
Diagnosis of bacterial meningitis and meningococcal septicaemia in secondary NICE Pathways
care
4 Cranial CT examination for suspected bacterial meningitis
Use clinical assessment and not cranial CT, to decide whether it is safe to perform a lumbar
puncture. CT is unreliable for identifying raised intracranial pressure.
If a CT scan has been performed, do not perform a lumbar puncture if the CT scan shows
radiological evidence of raised intracranial pressure.
In children and young people with a reduced or fluctuating level of consciousness (Glasgow
Coma Scale score less than 9 or a drop of 3 or more) or with focal neurological signs, perform a
CT scan to detect alternative intracranial pathology.
Do not delay treatment to undertake a CT scan.
Clinically stabilise children and young people before CT scanning.
If performing a CT scan consult an anaesthetist, paediatrician or intensivist.
5 Lumbar puncture and CSF examination for suspected bacterial
meningitis
Perform a lumbar puncture as a primary investigation unless this is contraindicated.
Do not allow lumbar puncture to delay the administration of parenteral antibiotics.
CSF examination should include WBC count and examination, total protein and glucose
concentrations, Gram stain and microbiological culture. A corresponding laboratory-determined
blood glucose concentration should be measured.
In children and young people with suspected meningitis or suspected meningococcal disease,
perform a lumbar puncture unless any of the following contraindications are present:
signs suggesting raised intracranial pressure
shock (see table 2 signs of shock [See page 12])
extensive or spreading purpura
after convulsions until stabilised
coagulation abnormalities
Bacterial meningitis and meningococcal septicaemia in under 16s Page 6 of 16
© NICE 2022. All rights reserved. Subject to Notice of rights.
Diagnosis of bacterial meningitis and meningococcal septicaemia in secondary NICE Pathways
care
local superficial infection at the lumbar puncture site
respiratory insufficiency (lumbar puncture is considered to have a high risk
of precipitating respiratory failure in the presence of respiratory
insufficiency).
In children and young people with suspected bacterial meningitis, if contraindications to lumbar
puncture exist at presentation consider delaying lumbar puncture until there are no longer
contraindications. Delayed lumbar puncture is especially worthwhile if there is diagnostic
uncertainty or unsatisfactory clinical progress.
CSF WBC counts, total protein and glucose concentrations should be made available within 4
hours to support the decision regarding adjunctive steroid therapy.
Start antibiotic treatment for bacterial meningitis if the CSF WBC count is abnormal:
in neonates at least 20 cells/microlitre (be aware that even if fewer than 20 cells/microlitre,
bacterial meningitis should still be considered if other symptoms and signs are present (see
table 1 symptoms and signs of bacterial meningitis and meningococcal septicaemia [See
page 9])
in older children and young people more than 5 cells/microlitre or more than 1 neutrophil/
microlitre, regardless of other CSF variables.
See treatment with antibiotics.
In children and young people with suspected bacterial meningitis, consider alternative
diagnoses if the child or young person is significantly ill and has CSF variables within the
accepted normal ranges.
Consider herpes simplex encephalitis as an alternative diagnosis.
If CSF white cell count is increased and there is a history suggesting a risk of tuberculous
meningitis, evaluate for the diagnosis of tuberculous meningitis in line with the NICE Pathway
on assessing for active tuberculosis.
Perform a repeat lumbar puncture in neonates with:
persistent or re-emergent fever
deterioration in clinical condition
new clinical findings (especially neurological findings) or
persistently abnormal inflammatory markers.
Bacterial meningitis and meningococcal septicaemia in under 16s Page 7 of 16
© NICE 2022. All rights reserved. Subject to Notice of rights.
Diagnosis of bacterial meningitis and meningococcal septicaemia in secondary NICE Pathways
care
Do not perform a repeat lumbar puncture in neonates:
who are receiving the antibiotic treatment appropriate to the causative organism and are
making a good clinical recovery
before stopping antibiotic therapy if they are clinically well.
Quality standards
The following quality statement is relevant to this part of the interactive flowchart.
5. Lumbar puncture for suspected bacterial meningitis
6. CSF microscopy for suspected bacterial meningitis
6 Skin samples
Do not use any of the following techniques when investigating for possible meningococcal
disease: skin scrapings, skin biopsies, petechial or purpuric lesion aspirates (obtained with a
needle and syringe).
7 Management in secondary care
See Bacterial meningitis and meningococcal septicaemia in under 16s / Management of
bacterial meningitis and meningococcal septicaemia in secondary care
8 Non-meningococcal septicaemia
See the NICE Pathway on sepsis.
Bacterial meningitis and meningococcal septicaemia in under 16s Page 8 of 16
© NICE 2022. All rights reserved. Subject to Notice of rights.
Diagnosis of bacterial meningitis and meningococcal septicaemia in secondary NICE Pathways
care
Table 1 Symptoms and signs of bacterial meningitis and meningococcal
septicaemia
Common non-specific symptoms / signs
Meningococcal
Bacterial meningitis
disease
(meningococcal
(meningococcal Meningococcal
Symptom / sign meningitis and
meningitis and/or septicaemia
meningitis caused by
meningococcal
other bacteria)
septicaemia)
Fevera Y Y Y
Vomiting / nausea Y Y Y
Lethargy Y Y Y
Irritable / unsettled Y Y Y
Ill appearance Y Y Y
Refusing food / drink Y Y Y
Headache Y Y Y
Muscle ache / joint
Y Y Y
pain
Respiratory
symptoms / signs or Y Y Y
breathing difficulty
Bacterial meningitis and meningococcal septicaemia in under 16s Page 9 of 16
© NICE 2022. All rights reserved. Subject to Notice of rights.
Diagnosis of bacterial meningitis and meningococcal septicaemia in secondary NICE Pathways
care
Less common non-specific symptoms / signs
Meningococcal
Bacterial meningitis
disease
(meningococcal
(meningococcal Meningococcal
Symptom / sign meningitis and
meningitis and/or septicaemia
meningitis caused by
meningococcal
other bacteria)
septicaemia)
Chills / shivering Y Y Y
Diarrhoea, abdominal
Y Y Not known
pain / distension
Sore throat / coryza
or other ear, nose
Y Y Not known
and throat symptoms
/ signs
More specific symptoms / signs
Meningococcal
Bacterial meningitis
disease
(meningococcal
(meningococcal Meningococcal
Symptom / sign meningitis and
meningitis and/or septicaemia
meningitis caused by
meningococcal
other bacteria)
septicaemia)
Non-blanching rashb Y Y Y
Stiff neck Y Y Not known
Bacterial meningitis and meningococcal septicaemia in under 16s Page 10 of 16
© NICE 2022. All rights reserved. Subject to Notice of rights.
Diagnosis of bacterial meningitis and meningococcal septicaemia in secondary NICE Pathways
care
Altered mental statec Y Y Y
Capillary refill time
Not known Y Y
more than 2 seconds
Unusual skin colour Not known Y Y
Shock Y Y Y
Hypotension Not known Y Y
Leg pain Not known Y Y
Cold hands / feet Not known Y Y
Back rigidity Y Y Not known
Bulging fontanelled Y Y Not known
Photophobia Y Y N
Kernig's sign Y Y N
Brudzinski's sign Y Y N
Unconsciousness Y Y Y
Toxic / moribund
Y Y Y
state
Bacterial meningitis and meningococcal septicaemia in under 16s Page 11 of 16
© NICE 2022. All rights reserved. Subject to Notice of rights.
Diagnosis of bacterial meningitis and meningococcal septicaemia in secondary NICE Pathways
care
Paresis Y Y N
Focal neurological
deficit including
cranial nerve Y Y N
involvement and
abnormal pupils
Seizures Y Y N
Y: symptom or sign present;
N: symptom or sign not present;
Not known: not reported in the evidence.
a
Not always present, especially in neonates;
b
Be aware that a rash may be less visible in darker skin tones – check soles of feet, palms or
hands and conjunctivae;
c
Includes confusion, delirium and drowsiness, and impaired consciousness;
d
Only relevant in children under 2 years.
Table 2 Signs of shock
Signs of shock include:
capillary refill time more than 2 seconds
unusual skin colour
tachycardia and/or hypotension
respiratory symptoms or breathing difficulty
Bacterial meningitis and meningococcal septicaemia in under 16s Page 12 of 16
© NICE 2022. All rights reserved. Subject to Notice of rights.
Diagnosis of bacterial meningitis and meningococcal septicaemia in secondary NICE Pathways
care
leg pain
cold hands/feet
toxic/moribund state
altered mental state/decreased conscious level
poor urine output
Glossary
APVU
Alert, voice, pain, unresponsive.
CRP
C-reactive protein
CSF
Cerebrospinal fluid
CT
Computed tomography
EDTA
ethylenediaminetetraacetic acid
N. meningitidis
Neisseria meningitidis
PCR
polymerase chain reaction
Bacterial meningitis and meningococcal septicaemia in under 16s Page 13 of 16
© NICE 2022. All rights reserved. Subject to Notice of rights.
Diagnosis of bacterial meningitis and meningococcal septicaemia in secondary NICE Pathways
care
_S pneumoniae
Streptococcus pneumoniae
WBC
white blood cell
Sources
Meningitis (bacterial) and meningococcal septicaemia in under 16s: recognition, diagnosis and
management (2010 updated 2015) NICE guideline CG102
Your responsibility
Guidelines
The recommendations in this guideline represent the view of NICE, arrived at after careful
consideration of the evidence available. When exercising their judgement, professionals and
practitioners are expected to take this guideline fully into account, alongside the individual
needs, preferences and values of their patients or the people using their service. It is not
mandatory to apply the recommendations, and the guideline does not override the responsibility
to make decisions appropriate to the circumstances of the individual, in consultation with them
and their families and carers or guardian.
Local commissioners and providers of healthcare have a responsibility to enable the guideline
to be applied when individual professionals and people using services wish to use it. They
should do so in the context of local and national priorities for funding and developing services,
and in light of their duties to have due regard to the need to eliminate unlawful discrimination, to
advance equality of opportunity and to reduce health inequalities. Nothing in this guideline
should be interpreted in a way that would be inconsistent with complying with those duties.
Commissioners and providers have a responsibility to promote an environmentally sustainable
health and care system and should assess and reduce the environmental impact of
implementing NICE recommendations wherever possible.
Bacterial meningitis and meningococcal septicaemia in under 16s Page 14 of 16
© NICE 2022. All rights reserved. Subject to Notice of rights.
Diagnosis of bacterial meningitis and meningococcal septicaemia in secondary NICE Pathways
care
Technology appraisals
The recommendations in this interactive flowchart represent the view of NICE, arrived at after
careful consideration of the evidence available. When exercising their judgement, health
professionals are expected to take these recommendations fully into account, alongside the
individual needs, preferences and values of their patients. The application of the
recommendations in this interactive flowchart is at the discretion of health professionals and
their individual patients and do not override the responsibility of healthcare professionals to
make decisions appropriate to the circumstances of the individual patient, in consultation with
the patient and/or their carer or guardian.
Commissioners and/or providers have a responsibility to provide the funding required to enable
the recommendations to be applied when individual health professionals and their patients wish
to use it, in accordance with the NHS Constitution. They should do so in light of their duties to
have due regard to the need to eliminate unlawful discrimination, to advance equality of
opportunity and to reduce health inequalities.
Commissioners and providers have a responsibility to promote an environmentally sustainable
health and care system and should assess and reduce the environmental impact of
implementing NICE recommendations wherever possible.
Medical technologies guidance, diagnostics guidance and interventional procedures
guidance
The recommendations in this interactive flowchart represent the view of NICE, arrived at after
careful consideration of the evidence available. When exercising their judgement, healthcare
professionals are expected to take these recommendations fully into account. However, the
interactive flowchart does not override the individual responsibility of healthcare professionals to
make decisions appropriate to the circumstances of the individual patient, in consultation with
the patient and/or guardian or carer.
Commissioners and/or providers have a responsibility to implement the recommendations, in
their local context, in light of their duties to have due regard to the need to eliminate unlawful
discrimination, advance equality of opportunity, and foster good relations. Nothing in this
interactive flowchart should be interpreted in a way that would be inconsistent with compliance
with those duties.
Bacterial meningitis and meningococcal septicaemia in under 16s Page 15 of 16
© NICE 2022. All rights reserved. Subject to Notice of rights.
Diagnosis of bacterial meningitis and meningococcal septicaemia in secondary NICE Pathways
care
Commissioners and providers have a responsibility to promote an environmentally sustainable
health and care system and should assess and reduce the environmental impact of
implementing NICE recommendations wherever possible.
Bacterial meningitis and meningococcal septicaemia in under 16s Page 16 of 16
© NICE 2022. All rights reserved. Subject to Notice of rights.
You might also like
- Pediatric NursingDocument22 pagesPediatric NursingDarren Mae MosadaNo ratings yet
- Admission LetterDocument4 pagesAdmission LetterYasir KNNo ratings yet
- Lesson Plan Lumbar PunctureDocument25 pagesLesson Plan Lumbar PunctureValarmathi50% (4)
- Bacterial Meningitis and Meningococcal Septicaemia: Implementing NICE GuidanceDocument18 pagesBacterial Meningitis and Meningococcal Septicaemia: Implementing NICE GuidanceZarwo Black UstadzNo ratings yet
- Meningitis and Lumbar PunctureDocument38 pagesMeningitis and Lumbar PunctureJeo ThomasNo ratings yet
- Fod en Niños Menores de 3 MesesDocument16 pagesFod en Niños Menores de 3 MesesPaul Gutiérrez MyrickNo ratings yet
- Diagnosis and Treatment of Bacterial Meningitis: Arch. Dis. ChildDocument7 pagesDiagnosis and Treatment of Bacterial Meningitis: Arch. Dis. Childapi-214563632No ratings yet
- Meningitis in Adults: Diagnosis and Management: PembimbingDocument45 pagesMeningitis in Adults: Diagnosis and Management: PembimbingNeny Mathilda UniplaitaNo ratings yet
- Meningitis Workup - Approach Considerations, Blood Studies, Cultures and Bacterial Antigen TestingDocument14 pagesMeningitis Workup - Approach Considerations, Blood Studies, Cultures and Bacterial Antigen TestingdilaNo ratings yet
- Guideline MeningitisDocument1 pageGuideline MeningitisAmbc Smfk-uaj100% (1)
- Infectiousdiseases 130804135335 Phpapp02Document42 pagesInfectiousdiseases 130804135335 Phpapp02OleOhhNo ratings yet
- Investigating Procalcitonin and C-Reactive Protein As Diagnostic Biomarkers in Pediatric Suspected Meningitis: A Forward-Looking Observational AnalysisDocument16 pagesInvestigating Procalcitonin and C-Reactive Protein As Diagnostic Biomarkers in Pediatric Suspected Meningitis: A Forward-Looking Observational AnalysisInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Bacterial Meningitis in Children - DynaMedDocument88 pagesBacterial Meningitis in Children - DynaMedCarlos CalderwoodNo ratings yet
- Reflective Journal ReadingDocument13 pagesReflective Journal Readingعبداللة العمراني الحويطيNo ratings yet
- Bacterial Meningitis in AdultsDocument55 pagesBacterial Meningitis in AdultsfjnaressiNo ratings yet
- The Febrile Infant 29 To 90 Days of Age Management UpToDateDocument74 pagesThe Febrile Infant 29 To 90 Days of Age Management UpToDateSharafuddin SalimiNo ratings yet
- Serum Procalcitonin Levels in Bacterial and Abacterial MeningitisDocument5 pagesSerum Procalcitonin Levels in Bacterial and Abacterial MeningitisSaul Gonzalez HernandezNo ratings yet
- Meningitis PresentationDocument41 pagesMeningitis PresentationO'Mark AndrewsNo ratings yet
- Bacterial Meningitis in Infants Over 3 Months of AgeDocument8 pagesBacterial Meningitis in Infants Over 3 Months of AgedrirrazabalNo ratings yet
- Newborn Sepsis GuidelineDocument2 pagesNewborn Sepsis GuidelineAmelia ArnisNo ratings yet
- Treatment of Children With COVID-19: Position Paper of The Italian Society of Pediatric Infectious DiseaseDocument17 pagesTreatment of Children With COVID-19: Position Paper of The Italian Society of Pediatric Infectious DiseasecurteanancaNo ratings yet
- Covid Ep IiDocument29 pagesCovid Ep IiLuis Armando López SosaNo ratings yet
- Neonatal InfectionsDocument41 pagesNeonatal Infectionsamid sultanNo ratings yet
- Evaluation and Management of Suspected Sepsis and Septic Shock in AdultsDocument48 pagesEvaluation and Management of Suspected Sepsis and Septic Shock in AdultsIsmael IbrahimNo ratings yet
- Neonatal Sepsis: Prof DR Saima BatoolDocument31 pagesNeonatal Sepsis: Prof DR Saima BatoolSAIMA BATOOLNo ratings yet
- TREATMENT Bacterial MeningitisDocument32 pagesTREATMENT Bacterial MeningitisironNo ratings yet
- Research Paper On Bacterial MeningitisDocument8 pagesResearch Paper On Bacterial Meningitisvvgnzdbkf100% (1)
- Case 10 Fever PDFDocument5 pagesCase 10 Fever PDFSue HuangNo ratings yet
- Test ID: PCT Procalcitonin, Serum: Useful ForDocument5 pagesTest ID: PCT Procalcitonin, Serum: Useful ForI Nyoman Gede SemarajanaNo ratings yet
- Research Paper Bacterial MeningitisDocument4 pagesResearch Paper Bacterial Meningitisafeebovus100% (1)
- Bacterial Meningitis ThesisDocument8 pagesBacterial Meningitis ThesisRick Vogel100% (2)
- 35-Article Text-212-1-10-20200524Document4 pages35-Article Text-212-1-10-20200524SONIA AGUILAR RIVERANo ratings yet
- Clin Infect Dis. 2004 Tunkel 1267 84 Idsa MeningitiDocument18 pagesClin Infect Dis. 2004 Tunkel 1267 84 Idsa MeningitiJesus Salvador SerratoNo ratings yet
- Tuberculosis in ChildrenDocument4 pagesTuberculosis in ChildrenMarthin TheservantNo ratings yet
- Bacterial Meningitis in ChildrenDocument10 pagesBacterial Meningitis in ChildrenAnny AryanyNo ratings yet
- Sepsis NeonatalDocument21 pagesSepsis NeonatalRaissa 'Icha' Nurwany RizalNo ratings yet
- Diagnostics: CBC, CRP, UA, PCR, LAT, Blood Cultures CSF: With Opening Pressure, Procalcitonin and SerologyDocument4 pagesDiagnostics: CBC, CRP, UA, PCR, LAT, Blood Cultures CSF: With Opening Pressure, Procalcitonin and SerologyChoi SpeaksNo ratings yet
- Covid 19 Pediatric Multi System Inflammatory SyndromeDocument2 pagesCovid 19 Pediatric Multi System Inflammatory SyndromeministerenqiNo ratings yet
- Guia IDSA-Practice Guidelines For The Management of Bacterial Meningitis-2004Document18 pagesGuia IDSA-Practice Guidelines For The Management of Bacterial Meningitis-2004Brenda Anali Pariona NapaNo ratings yet
- Neonatal SepsisDocument31 pagesNeonatal Sepsisanwar jabariNo ratings yet
- (Methods in Molecular Medicine) Andrew J. Pollard, Martin C.J. Maiden - Meningococcal Disease (2001, Humana Press)Document662 pages(Methods in Molecular Medicine) Andrew J. Pollard, Martin C.J. Maiden - Meningococcal Disease (2001, Humana Press)gnkgbjkgjkNo ratings yet
- PCAP ReportDocument28 pagesPCAP ReportAngeline Zamoras-ToledoNo ratings yet
- Neonatal SepsisDocument5 pagesNeonatal SepsisBhawna PandhuNo ratings yet
- Bacterial MeningitisDocument51 pagesBacterial MeningitiscaseinrenninNo ratings yet
- Bacterial Meningitis in The Neonate - Neurologic Complications - UpToDateDocument9 pagesBacterial Meningitis in The Neonate - Neurologic Complications - UpToDateAngélica PedrazaNo ratings yet
- Meningitis PDFDocument8 pagesMeningitis PDFrizeviNo ratings yet
- Frequency of Thrombocytopenia in Neonatal Sepsis: Dr. Nadia GulDocument9 pagesFrequency of Thrombocytopenia in Neonatal Sepsis: Dr. Nadia GulNaeem NawazNo ratings yet
- Bacterial MeningitisDocument5 pagesBacterial Meningitisjamesignacio787No ratings yet
- ENLS Meningitis and Encephalitis ProtocolDocument20 pagesENLS Meningitis and Encephalitis ProtocolFransiskus MikaelNo ratings yet
- MengititisDocument38 pagesMengititisRas Siko SafoNo ratings yet
- Neonatal Meningitis Due To Clostridium Neonatale: A Case ReportDocument4 pagesNeonatal Meningitis Due To Clostridium Neonatale: A Case ReportCarina ColtuneacNo ratings yet
- MMC 1Document9 pagesMMC 1Maulida 04No ratings yet
- Jurnal AsliDocument8 pagesJurnal AsliDwi PurwantiNo ratings yet
- Sepsis in The Newborn - Latest NewsDocument13 pagesSepsis in The Newborn - Latest NewsBrunaNo ratings yet
- Neonatal SepsisDocument5 pagesNeonatal SepsisLeana SiñelNo ratings yet
- Clinical Features: - Initial Symptoms in Patients With MeningitisDocument12 pagesClinical Features: - Initial Symptoms in Patients With Meningitisyuii_48No ratings yet
- Meningitis in Adults - Diagnosis and Management - Young - 2018 - Internal Medicine Journal - Wiley Online LibraryDocument27 pagesMeningitis in Adults - Diagnosis and Management - Young - 2018 - Internal Medicine Journal - Wiley Online Libraryaslan tonapaNo ratings yet
- Meningitis: By-Dr Nimco A. MDDocument31 pagesMeningitis: By-Dr Nimco A. MDgibreilNo ratings yet
- C V 9 V VV VV V V VVVVVVVV V: "V "V "V "V "VDocument2 pagesC V 9 V VV VV V V VVVVVVVV V: "V "V "V "V "VCharlene Mae CalanoyNo ratings yet
- Paediatrica Indonesiana: Original ArticleDocument5 pagesPaediatrica Indonesiana: Original ArticleSyukron AmrullahNo ratings yet
- Peds InfectiousDocument8 pagesPeds InfectiousMohammad RammalNo ratings yet
- COVID-19 Mortality Review in Malaysia & Updates on Clinical Management of COVID-19From EverandCOVID-19 Mortality Review in Malaysia & Updates on Clinical Management of COVID-19No ratings yet
- Living on the Frontline of COVID-19 in MCO And CMCOFrom EverandLiving on the Frontline of COVID-19 in MCO And CMCONo ratings yet
- Stroke Differential Diagnosis and Mimics: Part 2Document9 pagesStroke Differential Diagnosis and Mimics: Part 2Natalia E PenagosNo ratings yet
- Seizure Pediatric Scenario June 2016Document4 pagesSeizure Pediatric Scenario June 2016Natalia E PenagosNo ratings yet
- Ene 15103Document8 pagesEne 15103Natalia E PenagosNo ratings yet
- Dom 14270Document19 pagesDom 14270Natalia E PenagosNo ratings yet
- Epilepsy Imaging: Approaches and ProtocolsDocument9 pagesEpilepsy Imaging: Approaches and ProtocolsNatalia E PenagosNo ratings yet
- Peeds Infection LecturesDocument190 pagesPeeds Infection LecturesAli Al.JuffairiNo ratings yet
- 282585293Document208 pages282585293hebaNo ratings yet
- Infections FarazDocument10 pagesInfections FarazM R SIFATNo ratings yet
- Lumbar Puncture ResearchDocument6 pagesLumbar Puncture Researchanon_464104226No ratings yet
- CDDocument6 pagesCDMei JoyNo ratings yet
- اسئلة neuroDocument30 pagesاسئلة neuroSoad RedaNo ratings yet
- Brain AbscessDocument2 pagesBrain AbscessIan RomanNo ratings yet
- Stool Analysis and Other Body Fluid AnalysisDocument51 pagesStool Analysis and Other Body Fluid AnalysisPutri Senna Rahayu100% (2)
- 83K English Class Examination Questions of Infectious DiseaseDocument23 pages83K English Class Examination Questions of Infectious Diseasetarun956519No ratings yet
- Intrathecal Hyaluronidase in TB Meningitis: The Unexplored AdjuvantDocument5 pagesIntrathecal Hyaluronidase in TB Meningitis: The Unexplored AdjuvantPriyanka SamalNo ratings yet
- Idr 240162 Management of Acute Bacterial Meningitis in ChildrenDocument13 pagesIdr 240162 Management of Acute Bacterial Meningitis in ChildrenindahrizkygNo ratings yet
- Epidemiology and Management Og Meningococcal MeningitisDocument12 pagesEpidemiology and Management Og Meningococcal MeningitispriyankaNo ratings yet
- Epidemic Cerebrospinal MeningitisDocument76 pagesEpidemic Cerebrospinal MeningitisAngie LawrenceNo ratings yet
- Some Imp Oneliner From VolumesDocument16 pagesSome Imp Oneliner From VolumesTejas KaleNo ratings yet
- Cases Lab 2020Document16 pagesCases Lab 2020Buushi96No ratings yet
- B) Meningococcal MeningitisDocument7 pagesB) Meningococcal MeningitisWe'am QutubNo ratings yet
- MCQ April 2015Document15 pagesMCQ April 2015Sylphana Astharica LawalataNo ratings yet
- Writing Notes: The Ideal Letter Should Have 6 PartsDocument7 pagesWriting Notes: The Ideal Letter Should Have 6 PartsMMW MNo ratings yet
- C CA AS SC CL Liin Niiq QU UE E // C CA AS SE ER RE EP PO OR RT TDocument7 pagesC CA AS SC CL Liin Niiq QU UE E // C CA AS SE ER RE EP PO OR RT TG Virucha Meivila IINo ratings yet
- Meningitis ViralDocument7 pagesMeningitis ViralTia Gustiani Poplei ViolaNo ratings yet
- Communicable Disease ChartDocument5 pagesCommunicable Disease ChartAuspice QatarNo ratings yet
- ENLS Meningitis and Encephalitis ProtocolDocument20 pagesENLS Meningitis and Encephalitis ProtocolFransiskus MikaelNo ratings yet
- Abdullahi V Pfizer Inc PDFDocument44 pagesAbdullahi V Pfizer Inc PDFBevs DomingoNo ratings yet
- Brain InfectionDocument61 pagesBrain Infectionmanisha paikarayNo ratings yet
- Blog Post About National Poultry Day 2023Document63 pagesBlog Post About National Poultry Day 2023ZETTYNo ratings yet
- Date/Time Doctors Order RationaleDocument4 pagesDate/Time Doctors Order RationaleChamCham AquinoNo ratings yet
- HAAD Test 4 QuestionsDocument17 pagesHAAD Test 4 QuestionsPhine PhineNo ratings yet