Professional Documents
Culture Documents
Schizophrenia NCP and Drugstudy
Schizophrenia NCP and Drugstudy
Uploaded by
Elle Monge100%(3)100% found this document useful (3 votes)
7K views11 pagesThe nursing care plan addresses a client experiencing schizophrenia manifested by sensory distortions (hallucinations) and disturbed thought processes (delusions). Short term goals are for the client to discuss hallucinations with the nurse, demonstrate coping techniques, and recognize delusions occur during anxiety. Interventions include observing for signs of hallucinations, avoiding touching unexpectedly, showing acceptance, engaging in distracting activities, and decreasing stimuli. The long term goal is for the client to define and test reality without hallucinations.
Original Description:
Original Title
SCHIZOPHRENIA NCP AND DRUGSTUDY
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThe nursing care plan addresses a client experiencing schizophrenia manifested by sensory distortions (hallucinations) and disturbed thought processes (delusions). Short term goals are for the client to discuss hallucinations with the nurse, demonstrate coping techniques, and recognize delusions occur during anxiety. Interventions include observing for signs of hallucinations, avoiding touching unexpectedly, showing acceptance, engaging in distracting activities, and decreasing stimuli. The long term goal is for the client to define and test reality without hallucinations.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
100%(3)100% found this document useful (3 votes)
7K views11 pagesSchizophrenia NCP and Drugstudy
Schizophrenia NCP and Drugstudy
Uploaded by
Elle MongeThe nursing care plan addresses a client experiencing schizophrenia manifested by sensory distortions (hallucinations) and disturbed thought processes (delusions). Short term goals are for the client to discuss hallucinations with the nurse, demonstrate coping techniques, and recognize delusions occur during anxiety. Interventions include observing for signs of hallucinations, avoiding touching unexpectedly, showing acceptance, engaging in distracting activities, and decreasing stimuli. The long term goal is for the client to define and test reality without hallucinations.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
You are on page 1of 11
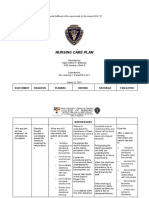
NURSING CARE PLAN
Assessment Diagnosis Planning Interventions Rationale Evaluation
Subjective: Disturbed sensory Short-term Goal: Observed client Early interventionAfter a week of
“Naririnig ko perception secondary Within a week of for signs of may nursing interventions,
prevent
silang pinag to schizophrenia as nursing interventions hallucinations aggressive the client was able to
uusapan ako! Sabi manifested by sensory client will be able to: (listening pose, responses discuss content of
to
nila wala daw distortions discuss content of laughing or talking command hallucinations with
akong kwenta!” (hallucinations) hallucinations with to self, stopping in hallucinations. nurse or therapist and
“Naaamoy nyo ba nurse or therapist mid-sentence). demonstrated
‘yon? Takpan nyo demonstrate Avoided touching techniques that help
ilong nyo dali! techniques that the client before Client may distract him or her
May lason yung help distract him warning him that perceive touch as from the voices.
hangin!” or her from the you are about to threatening and
Objective: voices. do so. respond in an
Noted to be aggressive
mumbling to Long-term Goal Showed an manner.
himself and often Client will be able to attitude of This is important
pausing as if he define and test reality, acceptance that in order to prevent
were listening to eliminating the encouraged the possible injury to
someone. occurrence of client to share the the client or others
Suspicious hallucinations. content of his from command
behavior hallucination. hallucinations.
Did not reinforce Words like “they”
the hallucination. validate that the
Used words such voices are real.
as “the voices”
instead of “they”
when referring to
the hallucination.
Tried to connect If client can learn
the times of the to interrupt
hallucinations to escalating anxiety,
times of increased hallucinations may
anxiety. Helped be prevented.
the client to
understand this
Involvement in
connection.
interpersonal
Distracted the activities and
client away from explanation of the
the hallucination actual situation
by engaging client will help bring the
in reality-based client back to
activities such as reality; acceptable
card playing, activities can
writing, drawing, decrease the
doing simple arts possibility of
and crafts or acting on
listening to music. hallucinations and
help distract from
voices.
Decrease the
potential for
Decreased anxiety that might
environmental trigger
stimuli when hallucinations.
possible (low Helps calm client.
noise, minimal The client can
activity). sometimes learn to
Stayed with client push voices aside
when starting to when given
hallucinate, and repeated
directed him to tell instructions.
the “voices they especially within
hear” to go away. the framework of
Repeat often in a a trusting
matter-of-fact relationship.
manner.
Assessment Diagnosis Planning Interventions Rationale Evaluation
Subjective: Disturbed thought Short-term Goal: Conveyed It is important to Within 2 weeks of
Pt verbalized processes secondary Within 2 weeks of acceptance of communicate to nursing interventions
delusions of to schizophrenia as nursing interventions client’s need for the client that you the client was able to
reference and manifested by client will be able to the false belief, do not accept the recognize and
persecution such as delusions. recognize and while letting him delusion as reality. verbalize that false
sound of blasts and verbalize that false or her know that ideas occur at times of
a relative inflicting ideas occur at times of you do not share Arguing with the increased anxiety
him of some increased anxiety. the belief. client or denying
mantras Long-term Goal Did not argue or the belief serves
Objective: By time of discharge denied the belief. no useful purpose,
Suspicious from treatment, Used reasonable because delusional
behavior client’s speech will doubt as a ideas are not
Restless reflect reality-based therapeutic eliminated by this
Irritable thinking. technique: “I approach, and the
During understand that development of a
conversation, there you believe this is trusting
were blank true, but I relationship may
intervals and personally find it be impeded.
tangentiality in his hard to accept.” If the client can
train of thoughts, learn to interrupt
with changes in escalating anxiety,
pitch. Helped client try delusional
Generalizations to connect the thinking may be
based on in- false beliefs to prevented.
appropriate or times of increased
limited anxiety. Discussed
information techniques that
was not able to could be used to
understand and use control anxiety
the concepts (e.g., deep-
easily. breathing
exercises, other
relaxation
exercises, thought Discussions that
stopping focus on the false
techniques). ideas are
Reinforced and purposeless and
focused on reality. useless, and may
Discourage long even aggravate the
ruminations about psychosis.
the irrational
thinking. Talk
about real events
and real people Verbalization of
Assisted and feelings in a
supported client in nonthreatening
his attempt to environment may
verbalize feelings help client come to
of anxiety, fear, or terms with long-
insecurity. unresolved issues.
Assessment Diagnosis Planning Interventions Rationale Evaluation
Patient had an Risk for other- Short-term Goal: Maintained low Anxiety level rises Within 2 weeks of
incident of a violent directed violence Within 2 weeks of level of stimuli in in a stimulating nursing intervention
attack on his mother related to nursing intervention client’s environment. A client was able to
just before the arrival suspiciousness and client will be able to: environment (low suspicious, recognize signs of
in the health care perception of the recognize signs of lighting, few agitated client may increasing anxiety and
center. environment as increasing anxiety people, simple perceive agitation and report to
threatening secondary and agitation and decor, low noise individuals as staff for assistance
to schizophrenia report to staff for level). threatening. with intervention and
assistance with Observed client’s So as to avoid did not harm self or
intervention. behavior creating others.
not harm self or frequently (every suspiciousness in
others. 15 minutes). Did the individual.
Long-term Goal: this while carrying Close observation
Client will not out routine is necessary so
harm self or activities that intervention
others. can occur if
required to ensure
client’s (and
others’) safety.
So that in his or
her agitated,
Removed all
dangerous objects confused state
from client’s client may not
environment use them to harm
self or others.
Physical exercise
Tried to redirect is a safe and
the violent effective way of
behavior with relieving pent-up
physical outlets tension.
for the client’s
anxiety (e.g.,
punching bag). Anxiety is
Maintained and contagious and
conveyed a calm can be
attitude toward transmitted from
client. staff to client.
This shows the
client evidence
Had sufficient of control over
staff available to the situation and
indicate a show of provides some
strength to client if physical security
it becomes for staff.
necessary.
The avenue of
the “least
Dependent: restrictive
Administered alternative” must
tranquilizing be selected when
medications as planning
ordered by interventions for
physician. a psychiatric
Monitored client.
medication for its
effectiveness and
for any adverse
side effects.
Drug Study
Drugs Classification Mechanism of Indications Caution and Side and Adverse Nursing
Action Contraindications Effects Considerations
Generic PHARMACO Antagonizes PO: Management Cautions: Disorders Frequent: Monitor B/P, serum
Name: THERAPEU alpha1- of manifestations in which CNS Drowsiness, glucose, lipids, LFT.
olanzapine TIC: Second- adrenergic, of schizophrenia. depression is agitation, insomnia, Assess for tremors,
Brand generation Dopamine, Treatment of acute prominent; cardiac headache, changes in gait,
Name: (atypical) histamine, mania associated disease, hemodynamic nervousness, abnormal muscular
Zyprexa antipsychotic. muscarinic, with bipolar instability, prior MI, hostility, dizziness, movements, behavior.
CLINICAL: serotonin disorder as ischemic heart rhinitis. Occasional: Supervise suicidal-risk
Antipsychotic. receptors. monotherapy or in disease; Anxiety, pt closely during early
Produces combination with hyperlipidemia, pts at constipation, therapy (as depression
anticholinergic, lithium or risk for aspiration nonaggressive lessens, energy level
histaminic, CNS valproate. pneumonia, decreased atypical behavior, improves, increasing
depressant IM: ZyPREXA. GI motility, urinary dry mouth, weight suicide potential).
effects. Controls acute retention, BPH, gain, orthostatic Assess for therapeutic
Therapeutic agitation in narrow-angle hypotension, fever, response (interest in
Effect: schizophrenia and glaucoma, diabetes, arthralgia, surroundings,
Diminishes bipolar mania. elderly, pts at risk for restlessness, cough, improvement in self-
psychotic Relprevv: Long- suicide, Parkinson’s pharyngitis, visual care, increased ability
symptoms. acting disease, severe changes (dim to concentrate, relaxed
antipsychotic for renal/hepatic vision). facial expression).
IM impairment, Adverse Reactions: Assist with ambulation
injection for predisposition to Rare reactions if dizziness occurs.
treatment of seizures. include seizures, Assess sleep pattern.
schizophrenia. Contraindications: neuroleptic Notify physician if
Hypersensitivity to malignant syndrome, extrapyramidal
olanzapine a potentially symptoms (EPS)
fatal syndrome occur.
characterized by Patient/family
hyperpyrexia, teaching
muscle rigidity, Avoid dehydration,
irregular pulse or particularly during
B/P, tachycardia, exercise, exposure
diaphoresis, cardiac to extreme heat,
arrhythmias. concurrent use of
Extrapyramidal medication causing
symptoms dry mouth, other
(EPS), dysphagia drying effects.
may occur. Overdose Sugarless gum, sips
(300 mg) produces of water may
drowsiness, slurred relieve dry mouth.
speech. Report suspected
pregnancy.
Take medication as
prescribed; do not
stop taking or
increase dosage.
Slowly go from
lying to standing.
Avoid alcohol.
Avoid tasks that
require alertness,
motor skills until
response to drug is
established.
Monitor diet,
exercise program to
prevent weight
gain.
Generic PHARMACO Directly increases Monotherapy/ Cautions: Children Frequent: Nausea, Monitor CBC, LFT,
Name: THERAPEU concentration of adjunctive therapy younger than 2 yrs. drowsiness. serum ammonia.
Divalproex TIC: Histone inhibitory of complex partial Pts at risk for Occasional: Antimanic: Question
sodium or deacetylase neurotransmitter seizures, simple hepatotoxicity. Asthenia, abdominal for suicidal ideation.
valproic inhibitor. gammaaminobuty and complex History of hepatic pain, dyspepsia, rash Assess for therapeutic
acid CLINICAL: ric absence seizures. impairment, bleeding Adverse Effects: response (Interest in
Brand Anticonvulsant acid (GABA). Adjunctive therapy abnormalities, pts at Hepatotoxicity may surroundings,
Name: , antimanic, Therapeutic of multiple seizures high risk for suicide, occur, particularly in increased ability to
Depakote antimigraine. Effect: Decreases including elderly pts. first 6 mos of concentrate, relaxed
seizure activity, absence seizures. Contraindications: therapy. May be facial expression).
stabilizes mood, Hypersensitivity to preceded by loss of Patient/ family
prevents migraine valproic acid. Active seizure control, teaching
headache. hepatic disease, urea malaise, weakness, Do not abruptly
cycle disorders, lethargy, anorexia, discontinue
known mitochondrial vomiting rather than medication after
disorders; migraine abnormal LFT long-term use (may
prevention in pregnant results. Blood precipitate
women. dyscrasias may seizures).
occur. Strict maintenance
of drug therapy is
essential for seizure
control.
Avoid tasks that
require alertness,
motor skills until
response to drug is
established.
Drowsiness usually
disappears during
continued therapy.
Avoid alcohol.
Report liver
problems such as
nausea, vomiting,
lethargy, altered
mental status,
weakness, loss of
appetite, abdominal
pain, yellowing of
skin, unusual
bruising/bleeding.
Report if seizure
control worsens,
suicidal ideation
(depression,
unusual changes in
behavior, suicidal
thoughts) occurs.
Generic Central Phenothiazine Management of Cautions: CNS: Drowsiness, Assessment & Drug
Name: Nervous similar to manifestations of Previously detected insomnia, dizziness, Effects
Trifluopera System Agent; chlorpromazine. psychotic breast cancer; agitation, Monitor HR and
zine Psychotherape Produces less disorders; "possibly compromised extrapyramidal BP. Hypotension is
Brand utic; sedative, effective" control respiratory function; effects, neuroleptic a common adverse
Name: Antipsychotic cardiovascular, of excessive seizure disorders. malignant syndrome. effect.
Espazine Phenothiazine and anxiety and tension Special Senses: Hypotension and
anticholinergic associated with Contraindications: Nasal congestion, extrapyramidal
effects and more neuroses or somatic Hypersensitivity to dry mouth, blurred effects (especially
prominent conditions. phenothiazines; vision, pigmentary akathisia and
antiemetic and comatose states; CNS retinopathy. dystonia) are most
extrapyramidal depression; blood Hematologic: likely to occur in
effects than other dyscrasias; children Agranulocytosis. patients receiving
phenothiazines. <6 y; bone marrow Skin: high doses or
Antipsychotic depression; Photosensitivity, parenteral
effects thought preexisting liver skin rash, sweating. administration and
related to disease; pregnancy GI: Constipation. in older adults.
blockade of (category C), CV: Tachycardia, Withhold drug and
postsynaptic lactation. hypotension. notify physician if
dopamine Respiratory: patient has
receptors in the Depressed cough dysphagia, neck
brain. reflex. Endocrine: muscle spasm, or if
Therapeutic Gynecomastia, tongue protrusion
Effect: Indicated galactorrhea. occurs.
by increase in Monitor I&O ratio
mental and and bowel
physical activity. elimination pattern.
Strong Check for
antipsychotic abdominal
drug with more distention and pain.
prolonged Encourage adequate
pharmacologic fluid intake as
effects than that prophylaxis for
of constipation and
chlorpromazine. xerostomia. The
depressed patient
may not seek help
for either symptom
or for urinary
retention.
Be aware that since
trifluoperazine
potentiates
analgesics, its use
may reduce amount
of narcotic required
in painful long-term
illness such as
cancer.
Agitation,
jitteriness, and
sometimes
insomnia may
simulate original
neurotic or
psychotic
symptoms. These
adverse effects may
disappear
spontaneously.
Expect maximum
therapeutic
response within 2–3
wk after initiation
of therapy.
Patient & Family
Education
Take drug as
prescribed; do not
alter dosing
regimen or stop
medication without
consulting
physician.
Consult physician
about use of any
OTC drugs during
therapy.
Do not take alcohol
and other
depressants during
therapy.
Avoid potentially
hazardous activities
such as driving or
operating
machinery, until
response to drug is
known. Drowsiness
and dizziness may
be prominent during
this time.
Cover as much skin
surface as possible
with clothing when
you must be in
direct sunlight. Use
a SPF >12
sunscreen on
exposed skin.
Urine may be
discolored or
reddish brown and
this is harmless.
Do not breast feed
while taking this
drug.
You might also like
- Schizophrenia NCPDocument4 pagesSchizophrenia NCPGladys Barcelona91% (56)
- Nursing Care Plan - SchizophreniaDocument3 pagesNursing Care Plan - SchizophreniaJasmin Jacob76% (46)
- Breast Cancer Radiation TherapyDocument439 pagesBreast Cancer Radiation TherapyJuan RivasNo ratings yet
- 4 NCP SchizophreniaDocument9 pages4 NCP SchizophreniaHazel Banday100% (5)
- NCPDocument1 pageNCPNneka Andrea Datiles0% (2)
- NCP Disturbed Thought Process Related To SchizophreniaDocument6 pagesNCP Disturbed Thought Process Related To Schizophrenianaishel0% (1)
- A NCP SchizoDocument5 pagesA NCP SchizoJoseph Wilson Macasa50% (4)
- FDAR For Urinary Tract InfectionDocument2 pagesFDAR For Urinary Tract InfectionElle Monge100% (1)
- NCP For Risk For Self-Directed ViolenceDocument4 pagesNCP For Risk For Self-Directed ViolenceGhale Annetoinette Reyes100% (1)
- Jean Pearl R. Caoili Bsn3 NCB Diagnosis: Paranoid Schizophrenia Psychiatric Nursing Care Plan Assessment Explanation of The Problem Goals/ Objectives Interventions Rationale EvaluationDocument9 pagesJean Pearl R. Caoili Bsn3 NCB Diagnosis: Paranoid Schizophrenia Psychiatric Nursing Care Plan Assessment Explanation of The Problem Goals/ Objectives Interventions Rationale Evaluationpj casteNo ratings yet
- Severe Anxiety As Evidenced by Repetitive ActionDocument1 pageSevere Anxiety As Evidenced by Repetitive ActionRomzy Basañes100% (3)
- Schizophrenia NCPDocument2 pagesSchizophrenia NCPNicole cuencos100% (3)
- Crisis Intervention: Psychiatric Nursing Nursing Care PlanDocument13 pagesCrisis Intervention: Psychiatric Nursing Nursing Care PlanKatherine 'Chingboo' Leonico Laud100% (4)
- Nursing Care PlanDocument2 pagesNursing Care PlanJewelyn Bronda100% (2)
- NCP Disturbed Thought ProcessDocument2 pagesNCP Disturbed Thought ProcessCesara Lacorte80% (5)
- Schizophrenia Care Plan RNDocument8 pagesSchizophrenia Care Plan RNlisa75% (4)
- Nursing Care Plans SchizDocument27 pagesNursing Care Plans SchizClariza Castro76% (17)
- Bipolar NCPDocument2 pagesBipolar NCPweehdinga89% (9)
- Nursing Care Plan For DepressionDocument7 pagesNursing Care Plan For DepressionCatherineNo ratings yet
- GINA Assessment of Asthma ControlDocument12 pagesGINA Assessment of Asthma ControlaranspeterNo ratings yet
- NCP PsychosisDocument3 pagesNCP PsychosisKristian Karl Bautista Kiw-is100% (1)
- NCP and Fdar: Data Goals/ Expected Outcomes Action/ Nursing Interventions Rationale Response & EvaluationDocument3 pagesNCP and Fdar: Data Goals/ Expected Outcomes Action/ Nursing Interventions Rationale Response & EvaluationKristian Karl Bautista Kiw-isNo ratings yet
- NCP SchizophreniaDocument2 pagesNCP Schizophreniajoshua canja100% (5)
- OCD NCPDocument2 pagesOCD NCPkharla suriaga100% (2)
- NCP PsychosisDocument3 pagesNCP Psychosisinagasi100% (7)
- NCP PsychDocument8 pagesNCP Psychjmanipon_1100% (1)
- Paranoid Schizophrenia NCPDocument8 pagesParanoid Schizophrenia NCPCherubim Lei DC Flores75% (4)
- Disturbed Thought Processes DescribeDocument2 pagesDisturbed Thought Processes DescribePRINCESS LARA CASILAONo ratings yet
- Care Plan For SchizophreniaDocument6 pagesCare Plan For SchizophreniaAllea Likestolaugh Brown100% (2)
- Disturbed Thought ProcessDocument4 pagesDisturbed Thought ProcessJessieRamosAnicetoNo ratings yet
- Nursing Care Plan - SchizophreniaDocument2 pagesNursing Care Plan - SchizophreniaJasmin Jacob80% (5)
- Nursing Care Plan BipolarDocument1 pageNursing Care Plan BipolarRobert de Guzman Jr.100% (1)
- NCP (Psychiatric)Document6 pagesNCP (Psychiatric)Erl Joy Montaño Cañete100% (1)
- NCP - Major Depressive DisorderDocument7 pagesNCP - Major Depressive DisorderJaylord Verazon100% (1)
- Bipolar NCPDocument4 pagesBipolar NCPcandy19agustin100% (2)
- Bipolar NCPDocument2 pagesBipolar NCPGenevieve VLs100% (1)
- NCPDocument3 pagesNCPCharles Mallari Valdez100% (1)
- Xi. Nursing Care PlansDocument4 pagesXi. Nursing Care PlansNic Ji100% (1)
- NCP Violence - OtherDocument2 pagesNCP Violence - OtherRosean Venus SilangNo ratings yet
- (26 29) Process Recording FormatDocument4 pages(26 29) Process Recording Formatpoleene de leonNo ratings yet
- Nursing Care Plan For A Patient With SchizophreniaDocument9 pagesNursing Care Plan For A Patient With Schizophreniaاسيرالاحزان100% (1)
- NCP For Bipolar DisorderDocument1 pageNCP For Bipolar DisorderJohn Carlo Santos100% (7)
- NCP For Bipolar Risk For Injury Related To Extreme Hyperactivity As Evidenced by Excessive and Constant Motor ActivityDocument3 pagesNCP For Bipolar Risk For Injury Related To Extreme Hyperactivity As Evidenced by Excessive and Constant Motor Activitydana75% (4)
- NCP For SchizoDocument5 pagesNCP For SchizoRichelene Mae Canja100% (2)
- Process RecordingDocument4 pagesProcess RecordingSheena MosesNo ratings yet
- Name of Drug Generic Name: Chlorpromazine BrandDocument1 pageName of Drug Generic Name: Chlorpromazine BrandkarenmichellelecarozNo ratings yet
- NCP Depressive DisorderDocument3 pagesNCP Depressive Disorderluthercarl cachoNo ratings yet
- Defensive Coping Related To Perceived Lack of Self-Efficacy As Evidenced by Denial of Obvious ProblemsDocument2 pagesDefensive Coping Related To Perceived Lack of Self-Efficacy As Evidenced by Denial of Obvious ProblemsJeyser T. GamutiaNo ratings yet
- NCP PsychDocument2 pagesNCP PsychJray Inocencio50% (4)
- Nursing CARE PLAN PsychDocument7 pagesNursing CARE PLAN Psychtiptopyo100% (1)
- N C PDocument3 pagesN C PTrixia Diaz100% (1)
- NCP FinalDocument22 pagesNCP FinalAlmira Ahamad100% (1)
- NCP SchizophreniaDocument2 pagesNCP Schizophreniabryan matiasNo ratings yet
- X. Nursing Care Plan: Assessment Nursing Diagnosis Planning Intervention Rationale Evaluation Goal MetDocument10 pagesX. Nursing Care Plan: Assessment Nursing Diagnosis Planning Intervention Rationale Evaluation Goal MetAnonymous TpI3Lk50No ratings yet
- Discussion: Answer The Following QuestionsDocument11 pagesDiscussion: Answer The Following QuestionsAndrew Del RosarioNo ratings yet
- Nursing Care Plan: in Partial Fulfillment of The Requirements For The Subject NCM 117Document6 pagesNursing Care Plan: in Partial Fulfillment of The Requirements For The Subject NCM 117Ingrid Valerie BalendezNo ratings yet
- Assessment Nursing Diagnosis Planning Nursing Interventions Rationale Evaluation Short-Term Goals: Short-Term GoalsDocument3 pagesAssessment Nursing Diagnosis Planning Nursing Interventions Rationale Evaluation Short-Term Goals: Short-Term GoalsDashiKONICNo ratings yet
- Schizophrenia NCPDocument6 pagesSchizophrenia NCPMark EvangelioNo ratings yet
- Psych NCP SchizopreniaDocument5 pagesPsych NCP SchizopreniaPatricia Lae Retonda DeLazoNo ratings yet
- Nursing Care Plan Cues Nursing Diagnosis Objectives Interventions Rationale EvaluationDocument2 pagesNursing Care Plan Cues Nursing Diagnosis Objectives Interventions Rationale EvaluationLi Luren Raphaelle TanNo ratings yet
- Hallucinations NCP PDFDocument3 pagesHallucinations NCP PDFANGELA ERES BALINGBING100% (2)
- Assessment Diagnosis Planning Interventions Rationale Evaluation Subjectives: Short-Term GoalDocument5 pagesAssessment Diagnosis Planning Interventions Rationale Evaluation Subjectives: Short-Term Goalmark OrpillaNo ratings yet
- Cues Nursing Diagnosis Outcome Nursingintervention Rationale Evaluation Discharge PlanningDocument5 pagesCues Nursing Diagnosis Outcome Nursingintervention Rationale Evaluation Discharge PlanningBSN 3B-Bulatao,Goergie Ann L. CPUSNNo ratings yet
- Obstacles To Medical CareDocument9 pagesObstacles To Medical CareElle MongeNo ratings yet
- Cholecystitis Case StudyDocument7 pagesCholecystitis Case StudyElle MongeNo ratings yet
- Words On Bathroom Walls ReviewDocument3 pagesWords On Bathroom Walls ReviewElle MongeNo ratings yet
- Sametclassificationarticle PDFDocument12 pagesSametclassificationarticle PDFAmada GonzálezNo ratings yet
- Summary Mindfulnes SetDocument1 pageSummary Mindfulnes Setjōōstech SLNo ratings yet
- Common Surgeries: The Appendectomy Surgery Instrument Set IncludesDocument3 pagesCommon Surgeries: The Appendectomy Surgery Instrument Set IncludesRica Marie Garcera SubongNo ratings yet
- Person Centered TherapyDocument4 pagesPerson Centered Therapysusanwhitten100% (2)
- MycosesDocument28 pagesMycosesAiman TymerNo ratings yet
- Sample Review Questions in Medical and Surgical Nursing and Sample Board Exam QuestionsDocument22 pagesSample Review Questions in Medical and Surgical Nursing and Sample Board Exam Questionstinea nigraNo ratings yet
- A Case Study On The Ayurvedic Management of Cerebral PalsyDocument10 pagesA Case Study On The Ayurvedic Management of Cerebral PalsyHiramandalam PatanjaliNo ratings yet
- PSYCHOTHERAPY ObjectivesDocument3 pagesPSYCHOTHERAPY Objectivesdrc.psyNo ratings yet
- Effect of Divorce On WomenDocument1 pageEffect of Divorce On WomenAmarendra GandhiNo ratings yet
- Inner Demon Destroyer MakeshiftDocument18 pagesInner Demon Destroyer MakeshiftMike H100% (1)
- IDweek Poster No397 Final CorrectedDocument1 pageIDweek Poster No397 Final CorrectedanaluvcNo ratings yet
- HHKHJKDocument1 pageHHKHJKputri windianiNo ratings yet
- Clinical Drug Research As Per GCP Guidelines Dr. Shivani SharmaDocument32 pagesClinical Drug Research As Per GCP Guidelines Dr. Shivani SharmaShivani SharmaNo ratings yet
- Aapi Guide To Nutrition Health and Diabetes PDFDocument188 pagesAapi Guide To Nutrition Health and Diabetes PDFaquamaverickNo ratings yet
- Lecithin - A Useful Byproduct of Edible Oil ExtractionDocument11 pagesLecithin - A Useful Byproduct of Edible Oil Extractionadda100% (1)
- Vitamin A DeficiencyDocument16 pagesVitamin A DeficiencyNikhil ShresthaNo ratings yet
- Hemophilia FinalDocument4 pagesHemophilia FinalDom Mar Manuel SuicoNo ratings yet
- Actionplan - SAHANPUR BijnorDocument43 pagesActionplan - SAHANPUR BijnorLimra TravelsNo ratings yet
- Zolpidem TartrateDocument2 pagesZolpidem Tartrateapi-3797941No ratings yet
- Discipline & Ideas in Applied Social Sciences Social SciencesDocument4 pagesDiscipline & Ideas in Applied Social Sciences Social Sciencesholly nightshadeNo ratings yet
- Waht-Cri-005 V2Document17 pagesWaht-Cri-005 V2Innas DoankNo ratings yet
- @@assessment of Medical Documentation As Per Joint Commission InternationDocument6 pages@@assessment of Medical Documentation As Per Joint Commission InternationNahari ArifinNo ratings yet
- Vogt Koyanagi Harada SyndromeDocument9 pagesVogt Koyanagi Harada SyndromeBianca PavelNo ratings yet
- 02 Tips For Teaching Nursing DiagnosisDocument20 pages02 Tips For Teaching Nursing DiagnosisMr. BamsNo ratings yet
- Mental Health Case StudyDocument14 pagesMental Health Case Studyapi-546467833No ratings yet
- Nadine Ayouch 201702815 Assignment 2Document2 pagesNadine Ayouch 201702815 Assignment 2Nadine AyouchNo ratings yet
- By Dinesh GannerllaDocument74 pagesBy Dinesh GannerllagannerllaNo ratings yet
- 74 - Quality and Safety in RadiotherapyDocument632 pages74 - Quality and Safety in RadiotherapyMelati A. PratiwiNo ratings yet