Professional Documents
Culture Documents
Dental Considerations in Pregnancy
Dental Considerations in Pregnancy
Uploaded by
ishas0 ratings0% found this document useful (0 votes)
28 views31 pagesThis document discusses dental considerations during pregnancy. It begins by outlining some of the physiological changes that occur during pregnancy, including changes to the respiratory, cardiovascular, hematological, and hormonal systems. It then discusses specific oral manifestations that may occur, such as gingivitis, granulomas, and erosion. The document concludes by providing dental management guidelines during pregnancy, recommending limiting treatment to prophylaxis and emergencies in the first trimester due to organ development, and allowing for more routine procedures in the second trimester once organogenesis is complete. The overall message is that dental care during pregnancy requires special attention and protocols to care for the health of both the mother and developing fetus.
Original Description:
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThis document discusses dental considerations during pregnancy. It begins by outlining some of the physiological changes that occur during pregnancy, including changes to the respiratory, cardiovascular, hematological, and hormonal systems. It then discusses specific oral manifestations that may occur, such as gingivitis, granulomas, and erosion. The document concludes by providing dental management guidelines during pregnancy, recommending limiting treatment to prophylaxis and emergencies in the first trimester due to organ development, and allowing for more routine procedures in the second trimester once organogenesis is complete. The overall message is that dental care during pregnancy requires special attention and protocols to care for the health of both the mother and developing fetus.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
0 ratings0% found this document useful (0 votes)
28 views31 pagesDental Considerations in Pregnancy
Dental Considerations in Pregnancy
Uploaded by
ishasThis document discusses dental considerations during pregnancy. It begins by outlining some of the physiological changes that occur during pregnancy, including changes to the respiratory, cardiovascular, hematological, and hormonal systems. It then discusses specific oral manifestations that may occur, such as gingivitis, granulomas, and erosion. The document concludes by providing dental management guidelines during pregnancy, recommending limiting treatment to prophylaxis and emergencies in the first trimester due to organ development, and allowing for more routine procedures in the second trimester once organogenesis is complete. The overall message is that dental care during pregnancy requires special attention and protocols to care for the health of both the mother and developing fetus.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
You are on page 1of 31
DENTAL SIGNIFICANCE
IN PREGNANCY
Presented by- ANKITA KUMARI
BDS FINAL YEAR
18008
ABSTRACT
• Pregnancy is a dynamic physiological state which is
evidenced by several transient changes.
• These can develop as various physical signs and
symptoms that can affect the patients health, perceptions
and interactions with others in the environment..
• A gestational woman requires various levels of support
throughout this time, such as medical monitoring or
intervention, preventive care and physical and emotional
assistance.
• The dental management of pregnant patients requires
special attention.
• Dentists may delay certain elective procedures so that
they coincide with the periods of pregnancy which are
devoted to maturation versus organogenesis.
• The dental care professionals need to alter their normal
pharmacological armamentarium to address the patients’
needs versus the fetal demands.
• Applying the basics of preventive dentistry at the
primary level will broaden the scope of the prenatal care.
• Dentists should encourage all the patients of the
childbearing ages to seek oral health counseling and
examinations as soon as they learn that they are pregnant
INTRODUCTION
• The storm of hormones which is induced during
pregnancy causes changes in the mother’s body and the
oral cavity is no exception.
• An increase in the secretion of the female sex hormones,
estrogen by 10 fold and progesterone by 30 fold, is
important for the normal progression of a pregnancy.
• The increased hormonal secretion and the foetal growth
induce several systemic, as well as local physiologic and
physical changes in a pregnant woman.
• The main systemic changes occur in the cardiovascular,
hematologic, respiratory, renal, gastrointestinal,
endocrine, and genitourinary systems and their effects
on oral cavity
PHYSIOLOGY
During pregnancy, women may experience systemic disorders
such as-
Respiratory System Changes
• There is increased respiratory minute volume (upto 40%)
during the first trimester due to progesterone induced
respiratory alkalosis.
• There is decreased respiratory lung movement due to
enlarged uterus during the third trimester.
Both situations may indicate dyspnea (difficulty in
breathing) but are physiologic responses
• Increased estrogen concentration may lead to rhinitis,
sinusitis and other upper respiratory tract infections
Pregnancy and Asthma in Dental Practice
• pregnant people with pre-existing and/or comorbid asthma,
pneumonia, or other respiratory issues may be more prone to
disease exacerbation and respiratory decompensation during
pregnancy
• In mild to moderate cases bronchodilator inhalers such as
salbutamol and terbutaline have been classified as safe during
pregnancy.
• In severe asthma, the use of oral corticosteroids, magnesium sulfate
and beta agonists are recommended.
• Oxygen intake should be closely monitored to prevent maternal
hypoxia and maintain foetal oxygenation
• NSAIDs such as acetaminophen and ibuprofen should be given.
Haematological changes
• During the 2nd trimester, there is an increase in plasma volume
over RBC count which dilutes the blood and reduces Haematocrit
value
• There is marked increase in clotting factors resulting in
hypercoagulability and run the risk of deep vein thrombosis and
pulmonary embolism
• Despite the significant changes that occur to the coagulation
system, standard coagulation tests [prothrombin time (PT),
activated partial thromboplastin time (aPTT)] do not change
during pregnancy or are very slightly decreased because of
compensatory mechanisms.
• Because of great demand for iron by the fetus, the mother
usually develops anemia. It can be rectified by proper prenatal
care and iron replacement.
Cardiovascular changes
• Cardiac output and pulse rate continuously increases and peaks at
3rd trimester (30-50% above normal)
• Systolic and diastolic blood pressure drops by 10-15mmgHg in the
first trimester due to hormonal changes but returns to normal in the
second trimester
• Patient may develop systolic murmur limited to gestational period
• Hormone induced vascular permeability changes may induce
gingivitis and spontaneous gum bleeding during 2nd and 3rd
trimester of pregnancy.
Management include scaling and curettage during 2nd trimester
and oral hygiene instructions
• Around the 3rd trimester, uterine enlargement compresses inferior
vena cava and restricts venous return hence patient may experience
postural hypotension in supine position (Supine Hypotensive
Syndrome)
Management of Supine Hypotensive Syndrome
• C/F-
Caused by excess supination of the dental unit after seating the
patient
The patient exhibits sweating, nausea, fatigue and dyspnoea
Examinations may present hypotension, bradycardia and
syncope
Compression results in lymphatic channel obstruction and pedal
oedema
• Immediate Treatment
Place the patient with head above feet
Elevate right hip with a pillow and shift the uterine weight off the
vena cava to the left side (left lateral displacement)
Roll the patient onto her left side
Hormonal changes
• Pancreatic Insulin changes:
• Human placental lactogen (hPL) conserves blood glucose for
neonates and in some cases cause gestational diabetes Mellitus
(GDM) in the mother
• GDM is associated with significantly increased risks of maternal and
infant morbidity, including preeclampsia, and periodontitis induced
by constant inflammatory response and state of insulin resistance
(caused by hPL) and in uncontrolled cases with existing periodontal
conditions; tooth mobility
• Pregnancy does NOT cause periodontitis but aggravates existing
ones
Adrenal Gland Secretions
• There is increased secretion of Oestrogen,
Progesterone and Cortisol (steroid). Steady
increase of steroids may result in the
formation of pregnancy granuloma in 1st
trimester. Repeated irritation with
circulating steroids lead to proliferation of
the lesion
• The lesion is not associated with
microorganism related infections and
hence should only be excised if it becomes
very large (>2cm) or becomes infected.
• Laser excision is reported to be well
tolerated in pregnancy without any adverse
effects
• Plaque control, scaling, curettage are the
treatment of choice otherwise
• Facial changes as melasma "mask of pregnancy," appearing
as bilateral brown patches in the mid-face begin during the 1st
trimester and are seen in up to 73% of pregnant women
• Parathyroid Hormone increased
• To increase calcium uptake to facilitate for foetal skeletal
development. This results in decreased serum calcium in
mothers
Gastrointestinal Tract Changes
• Acid Reflux
• Progesterone slows down intestinal motility and raises intragastric
pressure. This results in esophageal reflux, nausea, vomiting.
During this time a patient is more prone to have dental erosion if the
oesophageal reflux is uncontrolled with antacids & other PPIs
• During first Trimester, the patient may experience hyperemesis
gravidarum (morning sickness). Such patient should NOT be given
an early morning appointment
• Salivary changes
• Salivary flow decreases during the 1st
and 3rd trimester leading to reduced
buffering abilities and increased
cariogenic activity. Topical fluoride may
be prescribed to control such activities
while also benefitting the foetus from
reduced risks of caries
• Dry mouth results in increased
incidences of oral candidiasis. This
should be managed by cleaning the
infected regions and applying topical
antifungal agents
• Salivary flow increases (ptyalism) during
2nd trimester
Genitourinary System Changes
• Glomerular filtration rate and and plasma flow
increase. This in addition to the uterus restricting the
distention of the urinary bladder results in frequent
micturition. (Bladder Compression)
• In 2nd and 3rd trimesters the patient should be
asked to empty their bladders prior to treatment.
During long dental procedures, office temperature
should be regulated to at or above standard r.t.p.
Otherwise low temperatures can trigger cold
diuresis and trigger micturition reflex in the
patient.
ORAL MANIFESTATIONS IN
PREGNANCY
• Pregnancy gingivitis
• Periodontal disease
• Pregnancy granuloma
• Apthous ulcers (stress, dietary factors, altered immune
response)
• Pallor of oral cavity
• Erosion
Association of periodontitis with preterm birth
DENTAL MANAGEMENT
GUIDELINES DURING PREGNANCY
For the first trimester (1-12 weeks)
• During the first trimester, it is recommended that the patients be
scheduled to assess their current dental health, to inform them
of the changes that they should expect during their pregnancies,
and to discuss on how to avoid maternal dental problems that
may arise from these changes.
• It is not recommended that the procedures may be done at this
time.
• The concern about doing procedures during the first trimester
is twofold. First, the developing child is at a greatest risk which
is posed by teratogens during organogenesis, and second,
during the first trimester, it is known that as many as one in five
pregnancies undergo spontaneous abortions.
The current recommendations are
• To educate the patients about the maternal oral changes which
occur during pregnancy.
• To emphasize strict oral hygiene instructions and thereby,
plaque control.
• To limit the dental treatment to a periodontal prophylaxis and
emergency treatments only.
• To avoid routine radiographs. They should be used selectively
and only whenever they are needed.
For the second trimester (13-24 weeks)
• By the second trimester, the organogenesis is complete, and
the risk to the foetus is low. The mother has also had time to
adjust to her pregnancy, and the foetus has not grown to a
potentially uncomfortable size that would make it difficult for
the mother to remain still for long periods.
The current recommendations are:
• Oral hygiene, instructions and plaque control.
• Scaling, polishing and curettage may be performed if they are
necessary.
• The control of active oral diseases, if any.
• An elective dental care is safe
• Avoid routine radiographs. Use selectively and when they are
needed
For the third trimester (25-40 weeks)
• The foetal growth continues and the focus of the concern now,
is the risk to the upcoming birth process and the safety and
comfort of the pregnant woman (e.g the chair positioning and
the avoidance of drugs that affect the bleeding time).
• It is safe to perform a routine dental treatment in the early part
of the 3rd trimester, but from the middle of the 3rd trimester,
routine dental treatments are avoided.
• The positioning of the pregnant patients is important,
especially during the third trimester.
• As the uterus expands with the growing foetus and the
placenta, it comes to lie directly over the inferior vena cava,
the femoral vessels, and the aorta. If the mother is positioned
supine for the procedures, the weight of the gravid uterus
could apply enough pressure to impede a blood flow through
these major vessels and to cause a condition which is called
supine hypotension.
The current recommendations are:
• Oral hygiene, instructions and plaque control.
• Scaling, polishing and curettage may be performed if they are
necessary.
• Avoid an elective dental care during the 2nd half of the third
trimester.
• Avoid routine radiographs. Use selectively and when they are
needed.
RADIOGRAPHS, PREGNANCY
AND FOETUS
• X-rays are a type of electromagnetic radiation that have the ability
to ionize the material through which it passes. Ionizing living
matter results in a damage to the cells or the DNA.
• Depending on the amount of radiation and the stages of
pregnancy, a damage to the foetal cells may result in miscarriages,
birth defects or mental impairment. However the dental radiation
exposure of the foetus is negligible.
• The embryo and the foetus, being much more radiosensitive than
the adult counterpart, are susceptible to adverse effects which
result from the radiography exposure.
• During the first 2 weeks after the conception, the patient may
have no knowledge of being pregnant, thus making it prudent for
the physician to inquire about the last menstrual period before
obtaining a radiographic image. Because a general questioning
does not give a definitive diagnosis about the pregnancy status, a
lead shielding should be used for all the women who are in their
childbearing years.
• Several precautions can be taken to avoid the foetal exposure
when radiographs need to be taken. Using a lead shield over the
patient’s abdomen, using a properly collimated beam, and using
a high-speed film, can reduce the foetal exposure.
• The teratogenicity of the radiation depends on the foetal age and
the dose of the radiation.
• The greatest risk to the foetus for teratogenicity and death, is
during the first 10 days after the conception. The most critical
period of the foetal development is between 4-18 weeks after
the conception.
• The National Commission for Radiation Protective (NCRP)
recommends that the cumulative foetal exposure to radiation
should not exceed more than 0.20 Gy, which can cause
microcephaly and mental retardation
• CT is quite useful for localizing deep-seated infections and it is the
modality of choice for viewing the lateral pharyngeal infections.
• The skin doses from CT can range from 0.4 to 4.7 rads, with most
of the machines delivering in the 2.5 — rad range.
• These doses to the foetus can be kept to a minimum by carefully
using the shielding devices.
• MRI may be an alternative to CT when the foetal irradiation is
considered.
• MRI has a greater soft tissue sensitivity and contrast as compared
to CT, and thus it may help even more in the difficult cases of
infections.
• MRI uses a magnetic field-assisted nuclear alignment in creating
images and it provides no inonizing radiation.
• However, the risks of the foetal exposure to the strong magnetic
fields are not completely known
TERATOGENESIS
• A teratogen is any agent, that when exposed to the foetus,
causes permanent alterations in the function or form of the
offspring. The organ or structures which are formed during the
time of exposure, are at a risk for damage.
• For practical purposes, a pregnancy can be divided into
three periods:
• Ovum - from fertilization to implantation.
• Embryonic period- from the 2nd through the 8th week.
• Foetal period - after the eighth week until term.
• The embryonic period is the most important for teratogenesis,
because this is the time of organogenesis.
• A teratogenic exposure after the development of the vulnerable
structures usually does not result in alterations. There are a few
exceptions, which include tetracycline, which if taken during the
second half of the pregnancy, causes a yellow-brown
discolouration of the deciduous teeth
Teratogenic drugs
(short limbs)
You might also like
- Psych Consult TemplateDocument4 pagesPsych Consult TemplateJagdishVankarNo ratings yet
- Module 4 PROBLEM ORIENTED MEDICAL RECORDDocument15 pagesModule 4 PROBLEM ORIENTED MEDICAL RECORDdarius bautistaNo ratings yet
- Well Being: Striving For Good Health in Tribal CommunitiesDocument39 pagesWell Being: Striving For Good Health in Tribal CommunitiesRose Weeks100% (1)
- QA For Radiology DepartmentDocument3 pagesQA For Radiology DepartmentRaviraj Pishe100% (1)
- Dental Protocols in PregnancyDocument8 pagesDental Protocols in PregnancyMiki FloreaNo ratings yet
- Jurnal Direct and Indirect Pulp CappingDocument9 pagesJurnal Direct and Indirect Pulp Cappingninis anisaNo ratings yet
- Developmental DisturbanceDocument50 pagesDevelopmental DisturbanceMSH100% (1)
- PROSTHODONTIC MANAGEMENT OF GERIATRIC PATIENTS (Autosaved) (Autosaved)Document35 pagesPROSTHODONTIC MANAGEMENT OF GERIATRIC PATIENTS (Autosaved) (Autosaved)Shilpa SomanNo ratings yet
- Direct Pulp CappingDocument25 pagesDirect Pulp CappingHomura NakamuraNo ratings yet
- Bleeding Disorders: Presented by Janani RGDocument43 pagesBleeding Disorders: Presented by Janani RGJanani GopalakrishnanNo ratings yet
- Abscess and Dental Infections: Nsabimana Usiel Assistant Lecturer School of DentistryDocument24 pagesAbscess and Dental Infections: Nsabimana Usiel Assistant Lecturer School of DentistryNiyonsaba jean claudeNo ratings yet
- Healing of OralwoundsDocument38 pagesHealing of OralwoundsPuspa AdhikariNo ratings yet
- CEMENTUMDocument80 pagesCEMENTUMReshmaa RajendranNo ratings yet
- Ndodontics: Rubber Dam Frames and AccesoriesDocument5 pagesNdodontics: Rubber Dam Frames and AccesoriesFaber SidabutarNo ratings yet
- AIDS and PeriodontiumDocument25 pagesAIDS and PeriodontiumPathivada LumbiniNo ratings yet
- Epidemiologi Dental CariesDocument21 pagesEpidemiologi Dental CariesSampahAjaNo ratings yet
- Dev Dis ToothDocument92 pagesDev Dis ToothVaishnavi ThatiparthiNo ratings yet
- Newmicrosoftpowerpointpresentation2 150920090800 Lva1 App6891Document118 pagesNewmicrosoftpowerpointpresentation2 150920090800 Lva1 App6891priti adsulNo ratings yet
- Host Modulation TherapyDocument65 pagesHost Modulation TherapyKassim OboghenaNo ratings yet
- DR Neeraj Gugnani - Ecc PDFDocument29 pagesDR Neeraj Gugnani - Ecc PDFshailaja chintaNo ratings yet
- Advanced Restorative Dentistry - PPT 3Document39 pagesAdvanced Restorative Dentistry - PPT 3Lim TechchhorngNo ratings yet
- Accuracy of Digital Impressions of Multiple Dental Implants An in Vitro StudyDocument6 pagesAccuracy of Digital Impressions of Multiple Dental Implants An in Vitro StudyFellipeCarvalhoNo ratings yet
- Drug Interaction 2Document65 pagesDrug Interaction 2alhader libraryNo ratings yet
- Role of A Pedodontist in Cleft Lip and Cleft Palate Rehabilitation - An OverviewDocument25 pagesRole of A Pedodontist in Cleft Lip and Cleft Palate Rehabilitation - An OverviewIJAR JOURNALNo ratings yet
- Diet and Dental CariesDocument105 pagesDiet and Dental Cariesdentistpro.org100% (1)
- Root Canal IrrigantsDocument10 pagesRoot Canal IrrigantsAumir BégNo ratings yet
- Root Canal TreatmentDocument21 pagesRoot Canal TreatmentMary Noelyn Degoma100% (3)
- Bite MarksDocument29 pagesBite MarksSinduja GuptaNo ratings yet
- My GingivaDocument88 pagesMy GingivaNishtha BaralNo ratings yet
- SalivaDocument102 pagesSalivacareNo ratings yet
- Denture StomatitisDocument28 pagesDenture StomatitisAmalorNo ratings yet
- 1 Dental Caries PDFDocument38 pages1 Dental Caries PDFmayang putriNo ratings yet
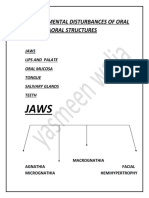
- Developmental Disturbances in Oral CavityDocument14 pagesDevelopmental Disturbances in Oral CavityYashmeen XNo ratings yet
- Oral Leukoplakia Management Using Diode Laser A Case Report (Chaudri DKK, 2019)Document3 pagesOral Leukoplakia Management Using Diode Laser A Case Report (Chaudri DKK, 2019)Rani PutriNo ratings yet
- Management of Geriatric PatientsDocument27 pagesManagement of Geriatric PatientsSuraj ShahNo ratings yet
- Desquamative GingivitisDocument41 pagesDesquamative Gingivitislucents100% (1)
- Unconventional Denture (Autosaved)Document50 pagesUnconventional Denture (Autosaved)Shilpa SomanNo ratings yet
- Orofacial Complications of Non Surgical Cancer TherapyDocument59 pagesOrofacial Complications of Non Surgical Cancer TherapyKassim OboghenaNo ratings yet
- Oral IrrigatorDocument30 pagesOral IrrigatorNorman Tri Kusumo100% (1)
- Oral Pathology Vimal K Sikri Colour Guides, MCQ's Arpit SikriDocument585 pagesOral Pathology Vimal K Sikri Colour Guides, MCQ's Arpit SikriKrish NatbhanjanNo ratings yet
- Dentine HypersensitivityDocument49 pagesDentine Hypersensitivitysamar yousif mohamedNo ratings yet
- Local Drug Delivery in PeriodonticsDocument40 pagesLocal Drug Delivery in PeriodonticsruchaNo ratings yet
- Presentation 16Document149 pagesPresentation 16rasagna reddyNo ratings yet
- Lecture 2 2021Document7 pagesLecture 2 2021Mateusz RadwańskiNo ratings yet
- Dental StonesDocument21 pagesDental StonesramukumarNo ratings yet
- Periodontal Problems in KidsDocument49 pagesPeriodontal Problems in KidsRaksmey PhanNo ratings yet
- Semi-Permanent Restorations of Anterior Teeth PedoDocument27 pagesSemi-Permanent Restorations of Anterior Teeth PedoFourthMolar.com100% (1)
- Dental Implant Awareness Among Patients in Our Institution in Chennai-Cross-Sectional SurveyDocument4 pagesDental Implant Awareness Among Patients in Our Institution in Chennai-Cross-Sectional SurveyInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Pediatric Nutrition and Nutritional Disorders: DR Ibraahim Guled MBCHB, Mmed (Paediatrics)Document74 pagesPediatric Nutrition and Nutritional Disorders: DR Ibraahim Guled MBCHB, Mmed (Paediatrics)Mohamed AliNo ratings yet
- Self Applied Topical Fluorides ClassDocument23 pagesSelf Applied Topical Fluorides ClassultraswamyNo ratings yet
- Introduction Cysts of JawsDocument62 pagesIntroduction Cysts of JawsEnass Alhadi50% (2)
- Oral Mucosa DiagramsDocument8 pagesOral Mucosa DiagramsAyshaNo ratings yet
- Periodontology 1 Compiled PDFDocument598 pagesPeriodontology 1 Compiled PDFCrypto ManiacNo ratings yet
- Extraoral Radiography PDFDocument2 pagesExtraoral Radiography PDFJackNo ratings yet
- Periodontium NotesDocument12 pagesPeriodontium NotesClarisse Mendoza100% (1)
- 1A - Oralist 2 - Summary of Oral PleadingDocument5 pages1A - Oralist 2 - Summary of Oral PleadingKaye LaurenteNo ratings yet
- Tests For Biocompatibility of Dental MaterialsDocument151 pagesTests For Biocompatibility of Dental MaterialsDevanshi SharmaNo ratings yet
- Silver Diamine Fluoride - A Futuristic Remedy For Caries TerminationDocument5 pagesSilver Diamine Fluoride - A Futuristic Remedy For Caries TerminationInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- DiagnosisDocument51 pagesDiagnosisRamya ChowdaryNo ratings yet
- 1 Dental IndicesDocument3 pages1 Dental IndicesAinun Nur Arifah100% (2)
- Advances in Alginate Impression MaterialsDocument27 pagesAdvances in Alginate Impression MaterialsTanu ShreyaNo ratings yet
- Unit 7Document79 pagesUnit 7Elsemieke SiemonsmaNo ratings yet
- Septic ArthritisDocument8 pagesSeptic ArthritisLorebell100% (2)
- Mult AEREL AEACNDocument7 pagesMult AEREL AEACNBart RoofthooftNo ratings yet
- Case Presentation StrokeDocument17 pagesCase Presentation StrokeGURUPRAKASH RNo ratings yet
- Navodaya Application FormatDocument9 pagesNavodaya Application FormatKeshavNo ratings yet
- Uterine Bleeding-A Case StudyDocument4 pagesUterine Bleeding-A Case StudyRoanne Lagua0% (1)
- Intrauterine Growth Restriction IUGRDocument8 pagesIntrauterine Growth Restriction IUGRJyoti Prem UttamNo ratings yet
- Iso 16603 2004 en PDFDocument6 pagesIso 16603 2004 en PDFrenny krisnawatiNo ratings yet
- Bio ProjectDocument25 pagesBio Projectlipi galotNo ratings yet
- PE7 Q3 Mod1 Self Assessment On Physical FitnessDocument22 pagesPE7 Q3 Mod1 Self Assessment On Physical FitnessJOSEFINA MAGADIANo ratings yet
- AcupunctureDocument4 pagesAcupunctureEls TreviñoNo ratings yet
- Sathish MSL 2023-2024Document140 pagesSathish MSL 2023-2024siva chandraNo ratings yet
- Abortion Full EssayDocument6 pagesAbortion Full EssayAlexander AndersonNo ratings yet
- Hematology, Transfusion and Cell Therapy: Review ArticleDocument22 pagesHematology, Transfusion and Cell Therapy: Review ArticleisabelNo ratings yet
- Postmenopause Syndrome in Elderly Woman at Panti Werdha Wisma Mulia, Grogol, West JakartaDocument8 pagesPostmenopause Syndrome in Elderly Woman at Panti Werdha Wisma Mulia, Grogol, West JakartaMonica PramanaNo ratings yet
- Labour and Delivery Nursing CareDocument40 pagesLabour and Delivery Nursing CareNica Baldedara100% (3)
- Mandilectomy PatDocument7 pagesMandilectomy PatMohamed AliNo ratings yet
- Edical Echnologist: Tasks Skills and CompetenciesDocument1 pageEdical Echnologist: Tasks Skills and CompetenciesNinoy C CarranzaNo ratings yet
- Consent - What You Have A Right To Expect: A Guide For ParentsDocument12 pagesConsent - What You Have A Right To Expect: A Guide For Parentshanzierox3825No ratings yet
- Highlights What Is Minimal Residual Disease (MRD) ?Document6 pagesHighlights What Is Minimal Residual Disease (MRD) ?ANo ratings yet
- Correcting Myths and Fallacies About Non Communicable Disease and Practicing Ways To Prevent and Control ItDocument9 pagesCorrecting Myths and Fallacies About Non Communicable Disease and Practicing Ways To Prevent and Control ItJohn Christian RamosNo ratings yet
- Acog Practice Bulletin: Gestational Hypertension and PreeclampsiaDocument25 pagesAcog Practice Bulletin: Gestational Hypertension and Preeclampsiana jaeminNo ratings yet
- List of Eligible Not Eligible Candidates For The Post of Dental Surgeon Under Mobile Dental Clinic Project Under NHMDocument21 pagesList of Eligible Not Eligible Candidates For The Post of Dental Surgeon Under Mobile Dental Clinic Project Under NHMMayank PalNo ratings yet
- PSM Concept BookDocument569 pagesPSM Concept Bookram dheer100% (1)
- Fissured TongueDocument31 pagesFissured Tonguenuratiqah_jasmiadNo ratings yet
- Leskovac Nur 460 PGC Reflection PaperDocument9 pagesLeskovac Nur 460 PGC Reflection Paperapi-527774673No ratings yet
- 19july 2022 WBDDocument4 pages19july 2022 WBDState HQNo ratings yet
- KTI PDF FixDocument89 pagesKTI PDF FixMarisa SinlaeNo ratings yet