Professional Documents
Culture Documents
Health History Questionnaire: Yes Self Family What Treatment Received and Date(s)
Health History Questionnaire: Yes Self Family What Treatment Received and Date(s)
Uploaded by
Vignesh VijayOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Health History Questionnaire: Yes Self Family What Treatment Received and Date(s)
Health History Questionnaire: Yes Self Family What Treatment Received and Date(s)
Uploaded by
Vignesh VijayCopyright:
Available Formats
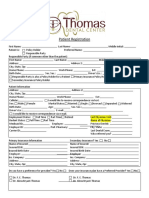
HEALTH HISTORY QUESTIONNAIRE
Client Name (First, MI, Last) Client No. Age
Has the client or family member had any of the following health problems? What was the family relationship?
Yes self Family What Treatment Received and Date(s)
Anemia
Arthritis
Asthma
Bleeding Disorder
Blood Pressure (high or low)
Bone/Joint Problems
Cancer
Cirrhosis/Liver Disease
Diabetes
Epilepsy/Seizures
Eye Disease/Blindness
Fibromyalgia/Muscle Pain
Glaucoma
Headaches
Head Injury/Brain Tumor
Hearing Problems/Deafness
Heart Disease
Hepatitis/Jaundice
Kidney Disease
Lung Disease
Menstrual Pain
Oral Health/Dental
Stomach/Bowel Problems
Stroke
Thyroid
Tuberculosis
AIDS/HIV
Sexual Transmitted Disease
Learning Problems
Speech Problems
Anxiety
Bipolar Disorder
Depression
Eating Disorder
Hyperactivity/ADD
Schizophrenia
Sexual Problems
Sleep Disorder
Suicide Attempts/Thoughts
Chronic Bronchitis
Sickle Cell Anemia
Substance Use Disorder
Other:
Has client had medical hospitalizations/surgical procedures in the last 3 years?
No Yes If yes, complete information below.
SOQIC-C 1/27/11 v2.0 Page 1 of 3
Client Name (First, MI, Last) Client No. Age
Hospital City Date Reason
None Allergies/Drug Sensitivities
Food (specify):
Medicine (specify):
Other (specify):
Not Pertinent Pregnancy History
Currently pregnant? If yes, expected delivery date. Receiving pre-natal healthcare? If yes, indicate provider.
No Yes No Yes
Are you currently breast
No Yes
feeding?
Last Menstrual Period Date Any significant pregnancy history? If yes, explain.
No Yes
Last Physical Examination
By Whom Date Phone No. (if known)
Has client had any of the following symptoms in the past 30 days? Please check.
Ankle Swelling Coughing Lightheadedness Penile Discharge Urination Difficulty
Bed-wetting Cramps Memory Problems Pulse Irregularity Vaginal Discharge
Blood in Stool Diarrhea Mole/Wart Changes Seizures Vision Changes
Breathing Difficulty Dizziness Muscle Weakness Shakiness Vomiting
Chest Pain Falling Nervousness Sleep Problems Other:
Confusion Gait Unsteadiness Nosebleeds Sweats (night)
Consciousness Hair Change Numbness Tingling in Arms & Other:
Loss Legs
Constipation Hearing Loss Panic Attacks Tremor
Not Applicable Immunizations/Test
Immunizations - Has client had or been immunized or tested for the following diseases? Please check.
Hepatitis B TB Flu Hepatitis A
Tetanus Other:
Immunizations Within the Past Year
Height/Weight
Height If reporting for a child, has height changed in the past year?
No Yes If yes, by how much (+ or -)?
Weight Has client’s weight changed in the past year?
No Yes If yes, by how much (+ or -)?
Nutritional Screening (please check if within the last 30 days)
No Problem Eating More Less Fluids More Less Appetite
Not Eating Takes Liquids Only Increased Decreased
SOQIC-C 1/27/11 v2.0 Page 2 of 3
Client Name (First, MI, Last) Client No. Age
Nausea Vomiting Trouble Chewing or Swallowing
How many meals do you eat per day?
Where do you eat your meals? Home Friend/Family Shelter/Drop-in Center Church Other:
Special Diet Other
Comments:
Pain Screening
Does pain currently interfere with your activities? If yes, how much does it interfere with these activities (please check)
No Yes Not at Mildly Moderately Severely Extremely
All
Please indicate the source of the pain.
Substance Use History/Current Use (please check appropriate columns)
No Past Current No Past Current No Past Current
Substance Substance Substance
Use Use Use Use Use Use Use Use Use
Alcohol/Beer/Wine Sleep Medication Cocaine/Crack
Marijuana Tranquilizers Heroin
Hashish Hallucinogens Pain Medication
Stimulants Inhalants Other:
Caffeine use? If yes, form (coffee, tea, pop, etc.) How much per day (cups, bottles)?
No Yes
Tobacco use? If yes, form (cigarettes, cigars, smokeless, etc.) How many per day (packs, etc.)?
No Yes
Print Name of Person Completing this Questionnaire Signature of Person Completing this Questionnaire Date
SOQIC-C 1/27/11 v2.0 Page 3 of 3
You might also like
- Medical History FormDocument1 pageMedical History Formapi-5429941880% (1)
- Health Declaration FormDocument3 pagesHealth Declaration FormMaja Aira BumatayNo ratings yet
- Comprehensive Geriatric Assessment Proforma Apr-15Document11 pagesComprehensive Geriatric Assessment Proforma Apr-15Udin Nicotinic100% (2)
- Patient Assessment Form For AdultsDocument2 pagesPatient Assessment Form For AdultsAriane CauanNo ratings yet
- New Patient Health History Form: (Please Explain Below)Document2 pagesNew Patient Health History Form: (Please Explain Below)KevinNo ratings yet
- LLC Health FormDocument2 pagesLLC Health Formcesar maguigadNo ratings yet
- Adult Medical History Form: Please Complete All Pages NameDocument5 pagesAdult Medical History Form: Please Complete All Pages NameCaroline IberfuentesNo ratings yet
- Case History: Health ReportDocument2 pagesCase History: Health Reporteric wruckNo ratings yet
- As Per Merchant Shipping (Medical Examination) Rules, 2010 & Ism/Stcwcode /9 and MLC Convention 2006 (A Rhha 2Document4 pagesAs Per Merchant Shipping (Medical Examination) Rules, 2010 & Ism/Stcwcode /9 and MLC Convention 2006 (A Rhha 2avishkar guptaNo ratings yet
- Medical Health Record 2 LONGDocument2 pagesMedical Health Record 2 LONGipanagclaire8No ratings yet
- Medical History QuestionnaireDocument1 pageMedical History QuestionnaireHare MasterYodaNo ratings yet
- Client Intake Form 03Document2 pagesClient Intake Form 03KerriNo ratings yet
- Patient Evaluation Form - Cerebral Palsy: Click or Use The TAB Key To Move Between FieldsDocument7 pagesPatient Evaluation Form - Cerebral Palsy: Click or Use The TAB Key To Move Between FieldsSyed Ali ShahNo ratings yet
- Medical History FormatDocument5 pagesMedical History Formatkrzia TehNo ratings yet
- Heathrow Medicals Cabin Crew Medical and ConsentDocument3 pagesHeathrow Medicals Cabin Crew Medical and ConsentSplash1No ratings yet
- Medical History FormDocument2 pagesMedical History FormUtkarsh LakraNo ratings yet
- Physician S Report FormDocument4 pagesPhysician S Report FormpaolaNo ratings yet
- Patient Registration FormDocument5 pagesPatient Registration FormCari WithrowNo ratings yet
- Health History QuestionDocument9 pagesHealth History QuestionSunil Murkikar (GM - PMI Quality Operations)No ratings yet
- Student Health Services Form 2020Document2 pagesStudent Health Services Form 2020Asiaui HendersonNo ratings yet
- Physician's Report Form: Part A (Completed by The Applicant) 1. 2. 3Document4 pagesPhysician's Report Form: Part A (Completed by The Applicant) 1. 2. 3Arturo MBNo ratings yet
- University of South Florida College of Nursing: Msi & Msii Patient Assessment Tool 1 Patient InformationDocument19 pagesUniversity of South Florida College of Nursing: Msi & Msii Patient Assessment Tool 1 Patient Informationapi-418237167No ratings yet
- ms1 PatDocument14 pagesms1 Patapi-364212510No ratings yet
- Adult Med HXDocument2 pagesAdult Med HXapi-3868874No ratings yet
- Drexel Medicine New Patient Questionnaire 20160504Document7 pagesDrexel Medicine New Patient Questionnaire 20160504Sameer shetyeNo ratings yet
- Student Medical RecordDocument3 pagesStudent Medical Recordhamsa RasbiehNo ratings yet
- Medical Conditions Declaration Form1Document1 pageMedical Conditions Declaration Form1Khôi Mạc NguyênNo ratings yet
- Family First Chiropractic Client Intake 03172Document6 pagesFamily First Chiropractic Client Intake 03172Trina AsterinoNo ratings yet
- Physical Exam Format WordDocument3 pagesPhysical Exam Format WordEsshairah PelingonNo ratings yet
- East Valley Internal Medicine SNF Progress Note: Patient Name: Dob: DoaDocument4 pagesEast Valley Internal Medicine SNF Progress Note: Patient Name: Dob: Doabakfam1No ratings yet
- University of South Florida College of Nursing: Msi & Msii Patient Assessment Tool 1 Patient InformationDocument17 pagesUniversity of South Florida College of Nursing: Msi & Msii Patient Assessment Tool 1 Patient Informationapi-355083078No ratings yet
- Medical History FormDocument2 pagesMedical History Formapi-279870303No ratings yet
- Health Declaration FormDocument4 pagesHealth Declaration Formbrgyanos03No ratings yet
- Health Declaration Form 1Document2 pagesHealth Declaration Form 1asansur esNo ratings yet
- Med Q English PDFDocument2 pagesMed Q English PDFxryanxNo ratings yet
- Msii Pat 1-1Document22 pagesMsii Pat 1-1api-404285262No ratings yet
- University of South Florida College of Nursing: Msi & Msii Patient Assessment Tool 1 Patient InformationDocument21 pagesUniversity of South Florida College of Nursing: Msi & Msii Patient Assessment Tool 1 Patient Informationapi-385494784No ratings yet
- Last Name First Name Middle Name: Medical HistoryDocument2 pagesLast Name First Name Middle Name: Medical HistorySatish R ChilkuryNo ratings yet
- Pat ms1 3 08Document14 pagesPat ms1 3 08api-371817203No ratings yet
- CWH OB-GYN History 011222Document2 pagesCWH OB-GYN History 011222alikhanomer5No ratings yet
- Pat Fundies 2016Document18 pagesPat Fundies 2016api-371817203No ratings yet
- Pat Semester 1Document16 pagesPat Semester 1api-404285262No ratings yet
- Health History FormDocument4 pagesHealth History FormAsem Al-domainiNo ratings yet
- Patient Health Assessment PDFDocument8 pagesPatient Health Assessment PDFVictor BarbosaNo ratings yet
- Ms Pat 2Document19 pagesMs Pat 2api-379546477No ratings yet
- Personal Health History: Complete Incomplete Don't Know Females Only LMP (Last Menstrual Period)Document3 pagesPersonal Health History: Complete Incomplete Don't Know Females Only LMP (Last Menstrual Period)ERICKA GRACE DA SILVANo ratings yet
- Secrets Body Transformation Lesson 4 MenDocument58 pagesSecrets Body Transformation Lesson 4 MennazlaabadrNo ratings yet
- Chemical Dependency EvaluationDocument1 pageChemical Dependency EvaluationBekki JonesNo ratings yet
- GeorgeDocument2 pagesGeorgeSteve MaguireNo ratings yet
- ALFIAN INNAS Form English Alfian 201902002Document4 pagesALFIAN INNAS Form English Alfian 201902002Eca SaputriNo ratings yet
- Tinnitus QuestionnaireDocument8 pagesTinnitus QuestionnaireEmmanuelOliveiraNo ratings yet
- Up Form No2Document2 pagesUp Form No2Mitch Elle InfanteNo ratings yet
- New Patient Application UpdatedDocument5 pagesNew Patient Application UpdatedAbdu AryaNo ratings yet
- PT Medi History FormDocument4 pagesPT Medi History Formmirha fatima100% (1)
- PT Medi History Form M2Document4 pagesPT Medi History Form M2Muhammad SyaifudinNo ratings yet
- Patient History Form: 1 Physician InitialsDocument4 pagesPatient History Form: 1 Physician InitialsHenok TamiruNo ratings yet
- Child Adol Traditional Biopsychosocial TemplateDocument11 pagesChild Adol Traditional Biopsychosocial Templateyeney armenteros100% (1)
- Patient History Edited 2019Document3 pagesPatient History Edited 2019api-468186696No ratings yet
- Southside Dental Practice: Medical History FormDocument2 pagesSouthside Dental Practice: Medical History FormSanjay DaveNo ratings yet
- Joint Hypermobility Syndrome (Ehlers Danlos Syndrome)From EverandJoint Hypermobility Syndrome (Ehlers Danlos Syndrome)Rating: 1 out of 5 stars1/5 (1)
- Resume 07 10 2023 12 06 48 AmDocument2 pagesResume 07 10 2023 12 06 48 AmVignesh VijayNo ratings yet
- Invoice # 7Document1 pageInvoice # 7Vignesh VijayNo ratings yet
- An Analysis of Job Satisfaction in CE Infosystems PVT LTD: Sonia Lohia and Priyanka BediDocument6 pagesAn Analysis of Job Satisfaction in CE Infosystems PVT LTD: Sonia Lohia and Priyanka BediVignesh VijayNo ratings yet
- Project Job SatisfactionDocument46 pagesProject Job SatisfactionVignesh VijayNo ratings yet
- Friends Service Center BillDocument1 pageFriends Service Center BillVignesh VijayNo ratings yet
- Review of LiteratureDocument19 pagesReview of LiteratureVignesh VijayNo ratings yet
- The Role of Planning and Forcasting in Business OrganizationDocument72 pagesThe Role of Planning and Forcasting in Business OrganizationVignesh VijayNo ratings yet
- MY ResumeDocument1 pageMY ResumeVignesh VijayNo ratings yet
- A Study of Role in Forecasting and Planning in Business OrganisationDocument63 pagesA Study of Role in Forecasting and Planning in Business OrganisationVignesh VijayNo ratings yet
- Company Profle Digital SeoDocument2 pagesCompany Profle Digital SeoVignesh VijayNo ratings yet
- A Study On Agricultural Awareness Among The Rural Area Youngsters in MaharastraDocument14 pagesA Study On Agricultural Awareness Among The Rural Area Youngsters in MaharastraVignesh VijayNo ratings yet
- WEAN To Sale - Final Low Res PDFDocument284 pagesWEAN To Sale - Final Low Res PDFOjobo ClementNo ratings yet
- Michelson Contrast Sensitivity PDFDocument5 pagesMichelson Contrast Sensitivity PDFPradit SaraonNo ratings yet
- nhiệt độ nhân viên, công nhânDocument1 pagenhiệt độ nhân viên, công nhânMon Trang NguyễnNo ratings yet
- Asset Life Assessment (PRS022a)Document2 pagesAsset Life Assessment (PRS022a)bilalNo ratings yet
- SDL 2 Wound and Wound HealingDocument4 pagesSDL 2 Wound and Wound HealingDn Ezrinah Dn EshamNo ratings yet
- Transcultural Nursing - Sas 6Document3 pagesTranscultural Nursing - Sas 6Allyza Jane SartigaNo ratings yet
- Safer at Home Order Final 7.29.20 PDFDocument11 pagesSafer at Home Order Final 7.29.20 PDFMary HodginNo ratings yet
- Updated Open Elective For Final 7th Semester (Syllabus)Document83 pagesUpdated Open Elective For Final 7th Semester (Syllabus)Vikash KumarNo ratings yet
- Gendering LanguageDocument53 pagesGendering LanguagePRINCESS KAYE ANGEL MAMALONo ratings yet
- Assessment of KidneysDocument1 pageAssessment of KidneysWendy EscalanteNo ratings yet
- Basic Medical Instrumentation System:-: Amitshanu - inDocument5 pagesBasic Medical Instrumentation System:-: Amitshanu - inÃmît ShâñúNo ratings yet
- Guidelines For The Treatment of Venous UlcersDocument14 pagesGuidelines For The Treatment of Venous UlcerssorinmoroNo ratings yet
- Clinic Laboratories With Price List ConsDocument10 pagesClinic Laboratories With Price List ConsZyla PaulineNo ratings yet
- PhysioEx Exercise 11 Activity 4 - MD3N3Document4 pagesPhysioEx Exercise 11 Activity 4 - MD3N3Dorlisca Montes GarcesNo ratings yet
- To Study The Efficacy of Nirgundipatra Swaras Taila Karnapurana in The Management of Pootikarna With Special Reference To Chronic Suppurative Otitis MediaDocument6 pagesTo Study The Efficacy of Nirgundipatra Swaras Taila Karnapurana in The Management of Pootikarna With Special Reference To Chronic Suppurative Otitis MediaEditor IJTSRDNo ratings yet
- PhiliasDocument24 pagesPhiliasShén MauvéNo ratings yet
- Users of The Convention CenterDocument19 pagesUsers of The Convention CenterGilchrist NoconNo ratings yet
- Cosmetics 10 00071 v2Document31 pagesCosmetics 10 00071 v2nguyen.hongle3103No ratings yet
- 14 Leadership Qualities Which Are Checked in Issb PDFDocument1 page14 Leadership Qualities Which Are Checked in Issb PDFAbdul Qadeer50% (2)
- Legal and Ethical Issues in NursingDocument18 pagesLegal and Ethical Issues in Nursingavinash dhameriya100% (2)
- Rigel 333 Instruction ManualDocument37 pagesRigel 333 Instruction ManualTerraTerro Welleh WellehNo ratings yet
- Nursing (Tutor) - DR - AdvertisementDocument4 pagesNursing (Tutor) - DR - AdvertisementDharti RajNo ratings yet
- MyBenefits - Program Brochure (FY21-22)Document27 pagesMyBenefits - Program Brochure (FY21-22)Manan ChaniyaraNo ratings yet
- Safety Data Sheet: (SDS) No. Bm-Msds 011ADocument5 pagesSafety Data Sheet: (SDS) No. Bm-Msds 011AChou JoeNo ratings yet
- Fundamentals of A Workplace First-Aid Program: Best Practices GuideDocument28 pagesFundamentals of A Workplace First-Aid Program: Best Practices Guidefsixteen5070No ratings yet
- A Review Article of Oral Health and Diabetes Mellitus: Ankita AgarwalDocument2 pagesA Review Article of Oral Health and Diabetes Mellitus: Ankita Agarwalankita agarwalNo ratings yet
- J Clinic Periodontology - 2021 - Martin - Effect of Orthodontic Therapy in Periodontitis and Non Periodontitis Patients ADocument30 pagesJ Clinic Periodontology - 2021 - Martin - Effect of Orthodontic Therapy in Periodontitis and Non Periodontitis Patients Apaulina becerraNo ratings yet
- Church, Dawson - The Heart of HealingDocument316 pagesChurch, Dawson - The Heart of HealingRenato CamarãoNo ratings yet
- I Dont Want To Join BNI - BNI Education SlotDocument10 pagesI Dont Want To Join BNI - BNI Education SlotKanadNo ratings yet
- GVPT 200 Syllabus - Fall 2021 (v2)Document14 pagesGVPT 200 Syllabus - Fall 2021 (v2)mimiNo ratings yet