Professional Documents
Culture Documents
369 Full
369 Full
Uploaded by
putramahardanaCopyright:
Available Formats
You might also like
- ACSM Guidelines DownloadDocument11 pagesACSM Guidelines DownloadGOLDEN FIZZIK GYM14% (14)
- Obstetricia y Ginecología Beckman 8a EdicionDocument477 pagesObstetricia y Ginecología Beckman 8a EdicionAlejandro Mora100% (3)
- Research ProposalDocument19 pagesResearch ProposalNordean Afd KNo ratings yet
- Strength Training in Children and Adolescents: Raising The Bar For Young Athletes?Document4 pagesStrength Training in Children and Adolescents: Raising The Bar For Young Athletes?LEE JunhyukNo ratings yet
- Sports Med CareersDocument4 pagesSports Med Careersgrimuri31No ratings yet
- May JYI 2Document5 pagesMay JYI 2sooriroyNo ratings yet
- Youth Resistance Training Position StateDocument22 pagesYouth Resistance Training Position StateLeonidas FagundesNo ratings yet
- Viewcontent CgiDocument13 pagesViewcontent CgimariaNo ratings yet
- ACSM Exercise Science Career PathsDocument5 pagesACSM Exercise Science Career PathsHugo MaisNo ratings yet
- Review of Literature: Presented By: Mrunmayi Gadre 1 MPT Department of Pediatric PhysiotherapyDocument41 pagesReview of Literature: Presented By: Mrunmayi Gadre 1 MPT Department of Pediatric PhysiotherapyANKITA SHETTYNo ratings yet
- Position - Stand - Youth - Resistance - Training - 2009 PDFDocument20 pagesPosition - Stand - Youth - Resistance - Training - 2009 PDFDân NguyễnNo ratings yet
- Strength Training: The Physician and SportsmedicineDocument10 pagesStrength Training: The Physician and SportsmedicineAdrian RuizNo ratings yet
- ACSMs Exercise Testing Prescription PDFDocument6 pagesACSMs Exercise Testing Prescription PDFHARIZNo ratings yet
- ACSMs Exercise Testing Prescription PDFDocument6 pagesACSMs Exercise Testing Prescription PDFHARIZNo ratings yet
- Versic 2021Document16 pagesVersic 2021Willian da costaNo ratings yet
- Faigenbaum y Myer - 2009 - Pediatric Resistance Training Benefits, ConcernsDocument9 pagesFaigenbaum y Myer - 2009 - Pediatric Resistance Training Benefits, ConcernsAna IriarteNo ratings yet
- Importance of Health Science Education For.4Document6 pagesImportance of Health Science Education For.4Giovanni PontelliNo ratings yet
- AJGP 0102 2020 Focus Desbrow Sports Nutrition Amateur Athletes WEBDocument6 pagesAJGP 0102 2020 Focus Desbrow Sports Nutrition Amateur Athletes WEBIgor PavlovicNo ratings yet
- 06 Chapter - 1Document24 pages06 Chapter - 1Jyothish KBNo ratings yet
- Research Article Prevention of Physical Risk and Rehabilitation of Muscle Injury in Sanda CompetitionDocument9 pagesResearch Article Prevention of Physical Risk and Rehabilitation of Muscle Injury in Sanda Competition壮No ratings yet
- Sports Medicine .....Document9 pagesSports Medicine .....ScribdTranslationsNo ratings yet
- Ra 3Document10 pagesRa 3Heli MalivadNo ratings yet
- Sports MedicineDocument25 pagesSports MedicinedhanushrcksNo ratings yet
- Efects of Inspiratory Muscle Training in Older AdultsDocument10 pagesEfects of Inspiratory Muscle Training in Older AdultsMaría Camila Zuluaga AriasNo ratings yet
- 2019 Article AbstractsFromThe5thInternation PDFDocument41 pages2019 Article AbstractsFromThe5thInternation PDFStephano NgangiNo ratings yet
- Ijspt 06 241 PDFDocument13 pagesIjspt 06 241 PDFNovy DitaNo ratings yet
- Citius Altius Fortius Beneficial Effects of Resistance Training For Young AthletesDocument9 pagesCitius Altius Fortius Beneficial Effects of Resistance Training For Young Athletesfrancosala2012No ratings yet
- Effects of Different Exercise Interventions On Risk of Falls A Systematic ReviewDocument10 pagesEffects of Different Exercise Interventions On Risk of Falls A Systematic ReviewLeonardoValenzuelaNo ratings yet
- Haff 2010Document13 pagesHaff 2010DJNo ratings yet
- Effect of Supervised, Periodized Exercise Training vs. Self-Directed Training On Lean Body Mass and Other Fitness Variables in Health Club MembersDocument12 pagesEffect of Supervised, Periodized Exercise Training vs. Self-Directed Training On Lean Body Mass and Other Fitness Variables in Health Club MembersCeleste AyalaNo ratings yet
- Dose in Exercise Based Dysphagia Therapies: A Scoping ReviewDocument32 pagesDose in Exercise Based Dysphagia Therapies: A Scoping ReviewValentina SalasNo ratings yet
- Nutrition and Physical Activity InterventionsDocument28 pagesNutrition and Physical Activity Interventionsoknutricion1No ratings yet
- Peterson Et Al, 2004Document6 pagesPeterson Et Al, 2004Bernardo Ravanello da CostaNo ratings yet
- 01 SynopsisDocument24 pages01 SynopsisBilisuma MuletaNo ratings yet
- Strength Training Frequency and Athletic PerformanceDocument13 pagesStrength Training Frequency and Athletic Performance超卓No ratings yet
- 10.1519 1533-4287 (2003) 017 0734 Iotpoi 2.0Document5 pages10.1519 1533-4287 (2003) 017 0734 Iotpoi 2.0Stefan KovačevićNo ratings yet
- 216 FullDocument5 pages216 Fullalinaisabelaanghel5306No ratings yet
- American Medical Society For Sports MedicineDocument13 pagesAmerican Medical Society For Sports MedicineAlvaroNo ratings yet
- The Physiological and Physical Benefits of Two Types of Concurrent Training: A Randomized Controlled TrialDocument10 pagesThe Physiological and Physical Benefits of Two Types of Concurrent Training: A Randomized Controlled TrialChloe BujuoirNo ratings yet
- Physiotherapy in Sports 2013Document8 pagesPhysiotherapy in Sports 2013Diany CéspedesNo ratings yet
- Journal of Exercise Science & Fitness: Shi Zhou, Kade Davison, Fei Qin, Kuei-Fu Lin, Bik-Chu Chow, Jie-Xiu ZhaoDocument10 pagesJournal of Exercise Science & Fitness: Shi Zhou, Kade Davison, Fei Qin, Kuei-Fu Lin, Bik-Chu Chow, Jie-Xiu Zhaoapi-583367679No ratings yet
- The Overtraining Syndrome NeuroDocument11 pagesThe Overtraining Syndrome NeurodserraNo ratings yet
- Practical ExamDocument8 pagesPractical ExamRexNo ratings yet
- 08 Iajps08102017 PDFDocument5 pages08 Iajps08102017 PDFBaru Chandrasekhar RaoNo ratings yet
- Ackermann Et Al 2022 - Assessing Performing Artists in Medical and Health Practice - The Dancers, Instrumentalists, Vocalists, and Actors Screening ProtocolDocument3 pagesAckermann Et Al 2022 - Assessing Performing Artists in Medical and Health Practice - The Dancers, Instrumentalists, Vocalists, and Actors Screening ProtocolCarlos TinocoNo ratings yet
- Ajay VermaDocument18 pagesAjay VermabugsbusgNo ratings yet
- Knowledge Attitude and Practices KAP TowDocument9 pagesKnowledge Attitude and Practices KAP TowJaheda AktherNo ratings yet
- PP Assignment 2 by Anas Bin Mujeeb SAP# 21625 (MSPT-SPT)Document4 pagesPP Assignment 2 by Anas Bin Mujeeb SAP# 21625 (MSPT-SPT)Anas MujeebNo ratings yet
- NR527 Module 3 (Health Promotion)Document5 pagesNR527 Module 3 (Health Promotion)96rubadiri96No ratings yet
- The Systemic Effects of Blood Flow Restriction Training A Systematic ReviewDocument13 pagesThe Systemic Effects of Blood Flow Restriction Training A Systematic ReviewFederico BristotNo ratings yet
- Musculoskeletal Physiotherapists' Use of Psychological Interventions: A Systematic Review of Therapists' Perceptions and PracticeDocument8 pagesMusculoskeletal Physiotherapists' Use of Psychological Interventions: A Systematic Review of Therapists' Perceptions and PracticeTom StevensNo ratings yet
- Intconference PatialaDocument15 pagesIntconference PatialaPrakash S MNo ratings yet
- Applsci 11 08397Document10 pagesApplsci 11 08397Jyothish KBNo ratings yet
- High Intensity Small Muscle Mass Training in Patients With CHFDocument7 pagesHigh Intensity Small Muscle Mass Training in Patients With CHFbcvaughn019No ratings yet
- Essay - Role of PT in SportsDocument2 pagesEssay - Role of PT in SportsAlexander ScottNo ratings yet
- PIIS1440244018312702Document25 pagesPIIS1440244018312702Jesus Maturana YañezNo ratings yet
- SMB Youth Strength TrainingDocument2 pagesSMB Youth Strength Traininghadyahmed0318No ratings yet
- DaliwalDocument8 pagesDaliwalV.T. SrinivasanNo ratings yet
- 2022 Contribución de Los Fisioterapeutas Deportivos Al Equipo de Medicina Deportiva y Del Ejercicio.Document2 pages2022 Contribución de Los Fisioterapeutas Deportivos Al Equipo de Medicina Deportiva y Del Ejercicio.contact.movementsiteNo ratings yet
- Study of Physical Fitness Index Using Modified Harvard Step Test in Relation With Body Mass Index in Physiotherapy StudentsDocument4 pagesStudy of Physical Fitness Index Using Modified Harvard Step Test in Relation With Body Mass Index in Physiotherapy StudentsUswatun HasanahNo ratings yet
- 3Document4 pages3Rafiq ShahNo ratings yet
- Doctor List: Employee Name Employee Code Head QTR Division GatleDocument53 pagesDoctor List: Employee Name Employee Code Head QTR Division GatleNext Vision HomeNo ratings yet
- Training Manual On How To Teach Medical EthicsDocument33 pagesTraining Manual On How To Teach Medical EthicsghaiathmeNo ratings yet
- Developmental Pediatric ReviewDocument16 pagesDevelopmental Pediatric ReviewGhada HusseinNo ratings yet
- CombinedMerit2nd RjmornkDocument73 pagesCombinedMerit2nd RjmornkBhumi GargNo ratings yet
- JSS Medical College Mysore: Admissions 2023, Courses Offerd, Fees Structure, Cutoff, CounsellingDocument27 pagesJSS Medical College Mysore: Admissions 2023, Courses Offerd, Fees Structure, Cutoff, CounsellingJustGetAdmissionNo ratings yet
- The Role of Assessment in Competency-Based Medical EducationDocument8 pagesThe Role of Assessment in Competency-Based Medical EducationMaria PalaciosNo ratings yet
- (AIQ AND DNB) Seat Matrix Stray Vacancy Round MDDocument261 pages(AIQ AND DNB) Seat Matrix Stray Vacancy Round MDSathish KumarNo ratings yet
- Advt 2023 For WebsiteDocument5 pagesAdvt 2023 For WebsiteSumit SinghNo ratings yet
- Web Options - YSRUHSDocument2 pagesWeb Options - YSRUHSshivesh.agrawalNo ratings yet
- Educational Leadership Portfolio Template: Match To Standard-Setting Example(s)Document2 pagesEducational Leadership Portfolio Template: Match To Standard-Setting Example(s)Lileng LeeNo ratings yet
- Department of OphthalmologyDocument1 pageDepartment of Ophthalmologybibiah705No ratings yet
- Clear Vacancy Round 2 Mbbs - Bds Ug Counselling 2022Document232 pagesClear Vacancy Round 2 Mbbs - Bds Ug Counselling 2022punithNo ratings yet
- Stephanie H. Pincus, M.D., M.B.A.Document25 pagesStephanie H. Pincus, M.D., M.B.A.allcooNo ratings yet
- Abim Cbe The BasicsDocument53 pagesAbim Cbe The Basicsperie_mdNo ratings yet
- UG MBBS 2021-22college Wise P2Document75 pagesUG MBBS 2021-22college Wise P2sony sonyNo ratings yet
- Unfilled Programs by State: Reproduction Is Prohibited Without The Written Consent of The NRMP ®Document1 pageUnfilled Programs by State: Reproduction Is Prohibited Without The Written Consent of The NRMP ®Kuljeet VirkNo ratings yet
- Aipmt Round 3Document335 pagesAipmt Round 3AnweshaBoseNo ratings yet
- AIIMS Jodhpur Is The Best Medical College To Lead The Way To Success With MBBS in 2023-24.Document23 pagesAIIMS Jodhpur Is The Best Medical College To Lead The Way To Success With MBBS in 2023-24.Edufever OfficialNo ratings yet
- KONSULTA 073123 v1Document124 pagesKONSULTA 073123 v1Substationsix MalaboncpsNo ratings yet
- Medical Education in India and The Medical Council of India (MCI)Document22 pagesMedical Education in India and The Medical Council of India (MCI)Sabyasachi Sircar33% (3)
- Rajiv Gandhi University of Health SciencesDocument148 pagesRajiv Gandhi University of Health Sciencesriya yadavNo ratings yet
- A J InstituteDocument9 pagesA J InstitutealnavaraNo ratings yet
- Antiragging Committee - Jan-20Document1 pageAntiragging Committee - Jan-20TRH RECRUITMENTNo ratings yet
- BME 2015 v2 PDFDocument60 pagesBME 2015 v2 PDFTito PajueloNo ratings yet
- RMC Meu Annual Report 2019 20Document14 pagesRMC Meu Annual Report 2019 20abcqwe123No ratings yet
- List of Agencies With Recognition Status and ApplyingDocument6 pagesList of Agencies With Recognition Status and ApplyingMwanja MosesNo ratings yet
- Usmle Score CorrelationDocument4 pagesUsmle Score CorrelationIffat KabirNo ratings yet
- Simulation-Based Medical Education: Time For A Pedagogical ShiftDocument5 pagesSimulation-Based Medical Education: Time For A Pedagogical ShiftAshish kumarNo ratings yet
369 Full
369 Full
Uploaded by
putramahardanaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
369 Full
369 Full
Uploaded by
putramahardanaCopyright:
Available Formats
Consensus statement
Br J Sports Med: first published as 10.1136/bjsports-2021-104819 on 10 January 2022. Downloaded from http://bjsm.bmj.com/ on March 19, 2022 by guest. Protected by copyright.
Exercise medicine and physical activity promotion:
core curricula for US medical schools, residencies and
sports medicine fellowships: developed by the
American Medical Society for Sports Medicine and
endorsed by the Canadian Academy of Sport and
Exercise Medicine
Irfan Asif ,1 Jane S Thornton ,2 Stephen Carek,3 Christopher Miles,4
Melissa Nayak,5 Melissa Novak,6 Mark Stovak,7 Jason L Zaremski,8
Jonathan Drezner 9
For numbered affiliations see ABSTRACT interventions for the treatment and prevention of
end of article. Regular physical activity provides a variety of health non-communicable diseases is physical activity and
benefits and is proven to treat and prevent several exercise. Despite the proven benefits of regular phys-
Correspondence to
non-communicable diseases. Specifically, physical ical activity on cardiometabolic parameters, mental
Dr Irfan Asif, Department
of Family and Community activity enhances muscular and osseous strength, health and cognition, many medical professionals
Medicine, The University of improves cardiorespiratory fitness, and reduces the feel ill equipped to counsel patients on appropriate
Alabama at Birmingham, risk of hypertension, coronary heart disease, stroke, lifestyle behaviours centred on physical activity.2 This
Birmingham, Alabama, USA; type 2 diabetes, mental health disorders, cognitive is partly due to training deficiencies during medical
imasif@uabmc.edu
decline and several cancers. Despite these well-known education.3–6 For instance, the average that American
Accepted 15 December 2021 benefits, physical activity promotion in clinical practice medical schools require is only 8 hours of curriculum
Published Online First is underused due to insufficient training during medical on physical activity over the 4 years of training.7
10 January 2022 education. Medical trainees in the USA receive relatively Similarly, the average offered by primary care resi-
few hours of instruction in sports and exercise medicine dency programmes was only 3 hours per year of
(SEM). One reason for this shortage of instruction is didactic training on physical activity, nutrition and
a lack of curricular resources at each level of medical obesity, while a survey of American sports medicine
education. To address this need, the American Medical fellowship directors found that 63% of fellows were
Society for Sports Medicine (AMSSM) assembled a not taught how to write an exercise prescription.2 8
group of SEM experts to develop curricular guidance for Without fundamental knowledge in exercise medi-
exercise medicine and physical activity promotion at the cine and proper training on how to promote phys-
medical school, residency and sports medicine fellowship ical activity in clinical practice, use of this low-cost,
levels of training. After an evidence review of existing evidence-based intervention for the prevention and
curricular examples, we performed a modified Delphi treatment of chronic diseases will remain limited.
process to create curricula for medical students, residents Additionally, because physical inactivity and several
and sports medicine fellows. Three training level-specific associated non- communicable diseases dispropor-
curricula emerged, each containing Domains, General tionately affect marginalised communities including
Learning Areas, and Specific Learning Areas; options for under-represented minorities and persons of colour,
additional training and suggestions for assessment and there is an urgent need for broader education and
evaluation were also provided. Review and comment on implementation of physical activity promotion to
the initial curricula were conducted by three groups: a foster equitable healthcare delivery.9–11
second set of experts in exercise medicine and physical To address this training deficiency in medical
activity promotion, sports medicine fellowship directors
education, the American Medical Society for Sports
representing a variety of fellowship settings and the
Medicine (AMSSM) assembled a group of experts
AMSSM Board of Directors. The final curricula for each
in sports and exercise medicine (SEM) education to
training level were prepared based on input from the
design a series of curricula in exercise medicine and
review groups. We believe enhanced medical education
physical activity promotion (EM-PAP) to be imple-
will enable clinicians to better integrate exercise
mented at the medical school, residency and sports
medicine and physical activity promotion in their clinical
medicine fellowship levels. The curricula have
© Author(s) (or their practice and result in healthier, more physically active
employer(s)) 2022. No a particular focus on the promotion of physical
patients.
commercial re-use. See rights activity in clinical practice and include components
and permissions. Published related to medical knowledge and experiential
by BMJ.
training. By developing this resource, we hope
To cite: Asif I, Thornton JS, INTRODUCTION to enable medical schools and specialty training
Carek S, et al. Br J Sports Med Up to 80% of diseases in the USA. are due to programmes to deliver high- quality education in
2022;56:369–375. lifestyle behaviours.1 One of the most effective the field of EM-PAP.
Asif I, et al. Br J Sports Med 2022;56:369–375. doi:10.1136/bjsports-2021-104819 369
Consensus statement
Br J Sports Med: first published as 10.1136/bjsports-2021-104819 on 10 January 2022. Downloaded from http://bjsm.bmj.com/ on March 19, 2022 by guest. Protected by copyright.
IMPLEMENTATION by a second group of 10 experts in EM-PAP, a group of five
We believe EM-PAP curricula should be a core component of sports medicine fellowship directors with proficiency in medical
basic medical education, residency and sports medicine fellow- education and representing a variety of fellowship settings, two
ship training. However, we also recognise the ability to initially experts in the field of diversity, equity and inclusion, and the
satisfy all elements within each curriculum is aspirational, espe- AMSSM Board of Directors, was conducted. The suggested
cially as programmes develop new educational resources. In changes were used to strengthen the language within the docu-
particular, the comprehensive nature of the outlined curriculum ment, while not fundamentally altering the Delphi process for
for sports (and exercise) medicine fellowship training may be the curriculum.
difficult to complete within a 1-year time frame, and we antic-
ipate that further experience will be gained through clinical
practice and continued medical education. EM-PAP education RESULTS
is recognised as a critical gap for learners and the adoption of Tables 1–3 depict curricula for medical students, residents
any curricular elements will likely yield an improvement in the and sports medicine fellows, respectively. Considerations for
knowledge and ability of trainees to apply EM-PAP within their optional training as well as suggestions for assessment and eval-
clinical practice. While the ability to differentiate between basic uation are also provided.
and advanced curricular elements would be ideal, programmes
should consider implementation based on resource availability
Optional content for student training enhancement in EM-PAP
within their institution. Additionally, the numbers of procedures
For students who desire more education in EM-PAP
and experiences that are presented in this document are based
► Participate in a scholarly project.
on consensus opinion since objective data to create established
► Create quality improvement (QI) Initiative.
benchmarks do not yet exist. These curricula are presented in
► Participate in (or organise) journal clubs related to exercise
their entirety to encourage and assist medical schools, residen-
medicine and physical activity.
cies, and sports medicine fellowships to place a greater focus on
► Present and discuss the benefits of exercise with a commu-
EM-PAP education.
nity group facing barriers to physical activity.
► Serve as a longitudinal health coach, with a focus on exer-
cise and physical activity, for a core panel of patients with
METHODS
chronic disease and track their disease outcomes.
The EM-PAP group included nine experts in SEM who have clin-
► Serve longitudinally as an exercise/physical activity mentor
ical and educational (eg, presentation, publication or implemen-
for patients with (or at- risk for) adult and/or paediatric
tation experience) experience in physical activity promotion. For
obesity.
each of the three curricula (medical school, residency and sports
► Create patient education handouts or infographics.
medicine fellowship), a modified Delphi process was followed.
► Create exam/test questions.
After a review of curricula examples in EM-PAP, two members
of the group (IA and JD) created a draft curriculum for each
training level, with resulting questions created for each of the Assessment and evaluation of medical school student
three curricula.12 13 These questions were presented to the larger performance in EM-PAP
group via an anonymous survey using Survey Monkey. The ques- Examples of student assessment
tionnaires were distributed via a link embedded within an email. ► Using a standardised checklist, (eg, Observed Structured
Members of the group were given approximately 2 weeks to Clinical Examination (OSCE)) observe a student counselling
complete the questionnaires; a reminder email was sent 1 week a patient on exercise/physical activity.
prior to the due date. Questionnaires were closed after reaching ► Using a standardised checklist, (eg, OSCE) review a written
a 100% response rate from all nine members. exercise prescription from a patient encounter.
Each questionnaire posed a series of questions around ► Administer a short answer or essay exam to assess student
topic areas with members agreeing or disagreeing on a topic’s learning of EM-PAP curriculum content.
inclusion in the curricula. Members were given the option of ► Review a written description of what the student would do
commenting on the topics and making suggestions for improve- in response to a presented case to assess student learning of
ment. Each response to a question involved a 5-point Likert EM-PAP curriculum content.
scale as to whether the topic should be included in the curricula: ► Allow the trainee to evaluate the EM-PAP programme with
1=strongly disagree to 5=strongly agree. An element was an opportunity to incorporate the trainee’s suggestions for
included if 80% of participants agreed or strongly agreed it programme improvement.
should be part of the curricula. Results of the survey, commen-
tary and additional suggestions were collated and circulated to Optional content for resident training enhancement in EM-
the group with the option of further open comment. It was not PAP
possible for the collator to identify who had provided particular For residents who desire more education in EM-PAP
comments. Where appropriate, follow-up or revised questions ► Participate in a scholarly project related to EM-PAP or life-
on the topic areas were posed in the next iteration of the ques- style medicine.
tionnaire through the Delphi process. ► Create a QI Initiative related to EM-PAP or lifestyle medicine.
To ensure a sequence of foundational elements, the curric- ► Participate in or organise journal clubs related to EM-PAP.
ulum for medical education was developed first, followed by the ► Present and discuss the benefits of exercise and physical
residency programme and then the sports medicine fellowship activity with a community group.
curriculum. The curricula are hierarchical; the top level contains ► Serve as a longitudinal health coach, with a focus on exer-
the ‘Domains’, the second level contains ‘General Learning cise and physical activity, for a core panel of patients with
Areas’ (GLA) and each GLA is divided into ‘Specific Learning chronic disease while tracking their physical activity and
Areas’. Before finalising the curricula, open review and comment disease outcomes.
370 Asif I, et al. Br J Sports Med 2022;56:369–375. doi:10.1136/bjsports-2021-104819
Consensus statement
Br J Sports Med: first published as 10.1136/bjsports-2021-104819 on 10 January 2022. Downloaded from http://bjsm.bmj.com/ on March 19, 2022 by guest. Protected by copyright.
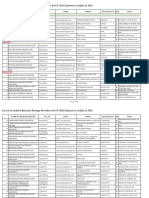
Table 1 Medical school education curriculum
Domain General learning areas Specific learning areas
1. Foundations of Exercise Medicine 1.1 Understand the basics of exercise in 1.1.1 Describe the role of exercise medicine and physical activity in disease prevention/
and Physical Activity Promotion health and medicine. treatment.
1.1.2 Review standard recommendations for exercise, physical activity, step counts, and
sedentary behaviour in the general population, including children, teenagers, and adults.17 18
1.1.3 Outline the FITT (frequency, intensity, time, and type) or FITT-volume, progression
framework.
1.2 Understand the basics of exercise 1.2.1 Review general principles of writing an exercise prescription.
prescription. 1.2.2 Write a general exercise prescription.
1.2.3 Outline safety considerations/contraindications.
1.3 Understand the basics of behavioural 1.3.1 Define models of behaviour change.
change. 1.3.2 Review the practical aspects of motivational interviewing and brief intervention that
can be used in the clinical setting.
2. Exercise Prescriptions in Medical 2.1 Learn modifications and 2.1.1 Cardiovascular: coronary artery disease, heart failure, and obesity.
Conditions and Special Populations recommendations for exercise in various 2.1.2: Pulmonary: COPD, asthma, and cystic fibrosis.
common conditions (may be incorporated 2.1.3 Gastrointestinal: post-abdominal surgery.
into case-based discussions). 2.1.4 Renal: hypertension.
2.1.5 Neurosciences: depression.
2.1.6 Musculoskeletal: knee osteoarthritis, low back pain, physical disability.
2.1.7 Endocrine: type II diabetes.
2.1.8 Reproductive: pregnancy.
2.1.9 Haematology-oncology: cancer, sickle cell trait/disease.
3. Exercise Medicine and Physical 3.1 Experience writing exercise prescriptions 3.1.1 Assess physical activity levels during ambulatory patient encounters.
Activity Promotion in Clinical during patient encounters. 3.1.2 Write exercise prescriptions as part of ambulatory clinical rotations.
Practice
3.2 Promote individual and community 3.2.1 Learn general barriers (including social and economic) to physical activity that are
engagement. specific to an individual.
3.2.2 Learn general barriers (including the built environment, traffic, pollution, and climate)
to physical activity that are specific to a community.
3.2.3 Identify community resources available for patients to engage in physical activity.
3.2.4 Learn that bias (implicit or explicit) can affect one’s ability to counsel patients.
Practical elements
► Assess physical activity levels and write exercise prescriptions for five patients as part of an ambulatory clinical rotation (eg, Family Medicine Clerkship/rotation*).
► Assess physical activity levels and write exercise prescriptions for 10 patients as part of an ambulatory acting internship/subinternship.†
► Locate at least three different types of accessible resources (eg, community partners, online videos) that can be used to assist physical activity promotion for patients or a
community.
► Identify at least one funding source to assist patients in need of financial assistance to conduct a physical activity programme.
► Participate in a local fitness event (charity run/walk, group fitness class, etc).
*The introductory rotation in family medicine and preventative care.
†An ambulatory acting internship/subinternship is an advanced level of clinical training beyond the basic clerkship which provides an opportunity for greater autonomy and care
for patients in a way that approximates early postgraduate (internship) training.
► Serve longitudinally as an exercise/physical activity mentor Optional content for fellow training enhancement in EM-PAP
for patients with or at risk for paediatric obesity. For fellows who desire more education in EM-PAP
► Create patient education handouts or other enduring mate- ► Participate in a scholarly project related to EM-PAP.
rials as resources. ► Create a QI Initiative related to EM-PAP.
► Create exam/test questions related to EM-PAP. ► Participate in journal clubs related to EM-PAP.
► Present and discuss the benefits of exercise and physical
Assessment and evaluation of resident performance in EM- activity with a community group.
PAP ► Serve as a longitudinal health coach, with a focus on exer-
Examples of resident assessment cise and physical activity, for a core panel of patients with
► Using a standardised checklist (eg, OSCE), evaluate a resi- chronic disease while tracking their physical activity and
dent counselling a patient on exercise medicine and physical disease outcomes.
activity. ► Serve longitudinally as an exercise/physical activity mentor
► Using a standardised checklist (eg, OSCE), evaluate a written for patients with or at risk for paediatric obesity.
exercise prescription from a patient encounter. ► Create patient education handouts or other enduring mate-
► Administer a short-answer or essay exam to assess resident rials in EM-PAP as resources.
learning of EM-PAP curriculum content. ► Create exam/test questions related to EM-PAP.
► Evaluate a written description of what the resident would do
in response to a patient case to assess learning of EM-PAP Assessment and evaluation of fellow performance in EM-PAP
curriculum content. Examples of fellow assessment
► Allow the trainee to evaluate the EM-PAP programme with ► Using a standardised checklist (eg, OSCE), evaluate a fellow
an opportunity to incorporate the trainee’s suggestions for counselling a patient on exercise medicine and physical
programme improvement. activity.
Asif I, et al. Br J Sports Med 2022;56:369–375. doi:10.1136/bjsports-2021-104819 371
Consensus statement
Br J Sports Med: first published as 10.1136/bjsports-2021-104819 on 10 January 2022. Downloaded from http://bjsm.bmj.com/ on March 19, 2022 by guest. Protected by copyright.
Table 2 Residency education curriculum
Domain General learning areas Specific learning areas
1. Healthy Bbehaviours 1.1 Identify the role of physical activity, 1.1.1 Examine how physical activity—as part of a broader curriculum focused on healthy
nutrition, mental health, sleep, and reduction behaviours—can be used to prevent/treat common diseases encountered within a residency,
of substance use in health promotion and across disciplines/specialties.
disease prevention. 1.1.2 Demonstrate motivational interviewing techniques that could be used to promote
healthy behaviours.
1.1.3 Demonstrate ways to work with patients who disagree or cannot complete
recommendations.
Practical elements
Use motivational interviewing techniques to promote healthy behaviours with 10 patients
2.Exercise Medicine and Physical 2.1 Practice physical activity promotion 2.1.1 If needed, review the Medical School Curriculum in Exercise Medicine and Physical
Activity Promotion in Clinical and exercise counselling during patient Activity Promotion, including disease-specific exercise recommendations and motivational
Practice encounters. interviewing best practices in the clinical setting.
2.1.2 Implement routine assessment of physical activity levels of patients during ambulatory
clinical patient encounters.
2.1.3 Implement routinely writing exercise prescriptions during ambulatory clinical patient
encounters.
2.1.4 Classify the billing and coding mechanisms for physical activity promotion and exercise
counselling.
2.2 Promote individual and community 2.2.1 Interpret general barriers (including social and economic) to physical activity that are
engagement. specific to an individual.
2.2.2 Describe general barriers (including the built environment, traffic, pollution, and climate)
to physical activity that are specific to a community.
2.2.3 Organise community resources available for patients to engage in physical activity.
2.2.4 Examine the bias (implicit or explicit) that can affect one’s ability to counsel patients.
Practical elements
► As part of a longitudinal experience in residency, write 30 exercise prescriptions (adults and/or children), including both aerobic exercise, resistance training, balance and
flexibility, with disease-specific recommendations when indicated.
► Over the course of residency education, record and then view five clinical encounters of physical activity promotion in 1-to-1 and/or group sessions and examine opportunities
for improving content delivery and patient comprehension.
► Examine physical activity log for 30 patients (approximately 10 per year).
► Perform 10 chart audits with a medical coding specialist of patients receiving exercise counselling.
► As part of a quality improvement initiative, examine the effect of physical activity on one prioritised quality measure (eg, blood pressure, blood sugar, body mass index,
depression) within the home institution.
► Locate at least five different types of accessible resources (eg, community partners, online videos) that can be used to assist physical activity promotion for patients or a
community.
► Identify at least one funding source to assist patients in need of financial assistance to undertake a physical activity programme.
► Serve as a medical volunteer for a community event focused on physical activity (eg, 5 k run).
3.Self-care with physical activity 3.1 Understand that self-care can enhance 3.1.1 Demonstrate how to develop a personal wellness plan
well-being, minimise burnout, and improve
effectiveness of patient counselling
Practical elements
► Create a personal wellness plan with Specific, Measurable, Attainable, Relevant and Time-Based goals that are adopted for at least 1 month, with reviews and modifications
every 7 days as needed
► Participate in local fitness event (eg, charity run/walk, group fitness class).
► Using a standardised checklist (eg, OSCE), evaluate a written for SEM specialty training.12 13 Our group, appointed by the
exercise prescription from a patient encounter. AMSSM, sought to take this work further by proposing curricula
► Administer a short- answer or essay exam to assess fellow across the US medical education spectrum (medical student, resi-
learning of EM-PAP curriculum content. dent and fellow), while also providing practical elements to help
► Evaluate a written description of what the fellows would do solidify medical knowledge into clinical practice. Additionally,
in response to a patient case to assess learning of EM-PAP since the length of training programmes vary across the world,
curriculum content. it was important to develop curricula that could be used within
► Allow the trainee to evaluate the EM-PAP programme with similar medical education systems. These proposed curricula
an opportunity to incorporate the trainee’s suggestions for provide a standard set of objectives to improve trainee educa-
programme improvement. tion, but also offer flexibility in how they may be incorporated
within a given institution or training programme.
DISCUSSION To promote use in clinical practice, the proposed curricula
Regular exercise and physical activity are proven to enhance include a combination of theory and practical experiences to
health, well-being and address a number of chronic diseases faced solidify understanding. The medical school curriculum offers
by patients today. However, there is a gap between these known content to be incorporated longitudinally using exercise prescrip-
benefits and the implementation of exercise and physical activity tions for commonly encountered medical conditions, and to facil-
promotion in clinical practice, due in part to deficiencies in itate discussion of how disease can be modified by exercise and
training and education. The International Syllabus in Sport and physical activity. Importantly, if the proposed curricula are incor-
Exercise Medicine Group developed an international syllabus porated, every physician completing medical school will have
372 Asif I, et al. Br J Sports Med 2022;56:369–375. doi:10.1136/bjsports-2021-104819
Consensus statement
Br J Sports Med: first published as 10.1136/bjsports-2021-104819 on 10 January 2022. Downloaded from http://bjsm.bmj.com/ on March 19, 2022 by guest. Protected by copyright.
Table 3 Fellowship education curriculum
Domain General learning areas Specific learning areas
1.Exercise Physiology 1.1 Understand the body’s normal 1.1.1 Examine the effects of exercise on the body, with special emphasis on the musculoskeletal, cardiovascular,
and abnormal responses to exercise respiratory, neuromuscular, and endocrine systems, as well as brain/mental health
and recovery
2.Exercise Nutrition 2.1 Describe how energy is derived 2.1.1 Explain the biological pathways involved in exercise metabolism
and used to fuel various types of 2.1.2 Explain energy absorption and release from macronutrient sources (carbohydrates, fats, proteins)
exercise and physical activity 2.1.3 Explain the effects of low energy availability on the ability to exercise
2.2. Understand sources of nutrition 2.2.1 Outline recommendations for the dietary intake of carbohydrates, fats, proteins, micronutrients and vitamins
in the general and athletic populations
2.2.2 Define resting metabolic rate to estimate caloric use at rest, and active metabolic rate to estimate energy
needs during exercise at different intensities
2.2.3 Differentiate the rationale for and the risks associated with nutritional supplements and ergogenic aids
2.2.4 Cite common equations and tools used to determine energy needs in adults and children18
2.2.5 Compare the elements and methods of a body composition analysis and how those values assist in
developing a nutrition plan
2.2.6 Examine how social, economic, and cultural factors can impact nutrition and dietary choices of athletes and
physically active patients
Practical elements
► Counsel 10 patients on hydration and fuelling plans for physical activity or exercise
► Design or participate in the design of nutrition plans (including daily metabolic/caloric needs, as well as social, economic or other cultural influences on dietary choices) for 10
individuals with chronic disease participating in physical activity.
► Design or participate in the design of nutrition plans (including daily metabolic/caloric needs) for 10 competitive athletes.
► Design or participate in the design of nutrition plans for 5 teams of differing energy demands.
► Examine a food recall diary for 10 physically active individuals (or patients).
► Perform resting metabolic rate assessments for 10 patients and determine the ratio of macronutrient energy utilisation at rest.
► Complete a body composition analysis on 10 physically active individuals (or patients).
► Counsel at least five athletes demonstrating low energy availability or poor nutritional intake.
3.Exercise Training 3.1 Describe training principles and 3.1.1 Distinguish the following types of exercise, their physiological effects, methods of fitness assessment and
types of exercise. ways to optimise their health benefits
► Aerobic
► Anaerobic
► Strength and Power
► Flexibility
► Balance/Proprioception
► Mind-body
3.2 Define how exercise capacity can 3.2.1 Demonstrate how to monitor exercise capacity via internal (eg, heart rate, blood lactate, oxygen
be used to monitor physical fitness. consumption, and ratings of perceived exertion (RPE)) and external (power output, speed, acceleration, time–
motion analysis, global positioning system (GPS) parameters, and accelerometer)training load measurements
3.2.2 Describe the signs and symptoms of overtraining and outline prevention and treatment strategies
Practical elements
► Participate in the design of 25 exercise training programmes for competitive athletes or physically active individuals (or patients).
4.Exercise and 4.1 Define barriers to exercise and 4.1.1 Describe the foundations of behaviour change (eg, Transtheoretical model of change)
Behaviour Change physical activity. 4.1.2 Analyse how social, economic, and other factors can create barriers to exercise and physical activity
4.2.3 Outline general barriers (including social and economic) to physical activity that are specific to an individual
4.2.4 Identify general barriers (including the built environment, traffic, pollution, and climate) to physical activity
that are specific to a community
4.2 Describe how to motivate or work 4.2.1. Develop cognitive and behavioural strategies for increasing physical activity behaviour (eg, enhancing self-
with patients to begin or maintain an efficacy, goal setting)
exercise programme. 4.2.2 Outline collaborative strategies and approaches to increase exercise adoption and adherence (eg,
motivational interviewing)
4.2.3 Produce ways to work with patients who disagree or cannot complete recommendations
Practical elements
► Utilise behavioural change and/or motivational interviewing techniques to increase physical activity behaviour during 25 patient encounters.
5.Exercise Prescription 5.1 Define when and how to screen 5.1.1 Identify the populations for which a screening health assessment is recommended prior to beginning a new
prior to the initiation of a physical exercise programme
activity or exercise programme. 5.1.2 Demonstrate the major components of a screening evaluation with special emphasis on the general medical,
cardiovascular, musculoskeletal, and neurologic elements
5.1.3 Define ancillary testing and prevention in patients at higher risk for adverse events with exercise (eg,
cardiovascular disease, diabetes)
5.1.4 Understand contraindications to beginning an exercise programme
Continued
Asif I, et al. Br J Sports Med 2022;56:369–375. doi:10.1136/bjsports-2021-104819 373
Consensus statement
Br J Sports Med: first published as 10.1136/bjsports-2021-104819 on 10 January 2022. Downloaded from http://bjsm.bmj.com/ on March 19, 2022 by guest. Protected by copyright.
Table 3 Continued
Domain General learning areas Specific learning areas
5.2 Define how to write exercise 5.2.1 Describe the Frequency, Intensity, Time, Type, Volume, and Progression model for writing an exercise
prescriptions for healthy individuals prescription
and those with chronic disease. 5.2.2 Write an exercise prescription for healthy/low-risk patients
5.2.3 Appreciate modifications of an exercise prescription for commonly encountered medical (eg, coronary artery
disease, obesity, asthma, diabetes, pregnancy) and musculoskeletal (eg, osteoarthritis) conditions
5.2.4 Write exercise prescription modifications for special circumstances (eg, advanced age, children, physical
disability, learning disability, beginners, post-surgery)18
5.2.5 Explain the effect of commonly used medications in children (eg, stimulants) and adults that might influence
exercise capacity (eg, beta blockers, diuretics) or create risk with exercise (eg, insulin, fluoroquinolones, QT
prolonging medications, impaired thermoregulation with anti-cholinergic medication)18
Practical elements
► Examine a physical activity log for 25 patients
► Write a physical activity prescription for 25 patients, including individuals with chronic disease or mobility impairment
6.Exercise Testing 6.1 Use exercise testing for screening, 6.1.1 Demonstrate the appropriate use and indications for the following tests for screening, diagnosis, or
diagnosis or development of exercise development of an exercise programme
programming ► In-office assessment of physical fitness
► Exercise treadmill testing
► -Cardiopulmonary exercise testing
► Pulmonary function testing
Practical elements
► Perform and interpret 50 exercise treadmill tests19 20
► Perform and interpret 50 cardiopulmonary exercise tests
► Perform and interpret 10 active metabolic assessments and use the information to design exercise programmes and target intensity training zones
► Perform and interpret 10 pulmonary function tests
7.Exercise in Clinical 7.1 Define sustainable clinical 7.1.1 Enact models for physical activity assessment, counselling, and referral to community programmes
Practice practice models to promote exercise 7.1.2 Investigate options for billing and coding in a sports and exercise medicine physician’s practice that will help
and physical activity in the sports sustain clinical practice models that support EM-PAP
medicine physician’s office 7.1.3 Determine the multi-disciplinary partners who can facilitate exercise promotion inside and outside of the
clinical practice setting
7.1.4 Define EM-PAP resources for children/youth, particularly in under-resourced settings
7.1.5 Describe how physical activity for youth requires counselling for the entire family
7.1.6 Examine the bias (implicit or explicit) that can affect one’s ability to counsel patients
Practical elements
► Find at least one community partnership that may assist patients who wish to begin an exercise programme
► Conduct 10 billing/coding audits for notes you completed where a patient was counselled on exercise or nutrition
► Assess physical activity levels of 25 patients in the office
8.Exercise and 8.1 Learn how exercise and physical 8.1.1 Assess how physical activity can modify both individual and population health
Population Health activity can help prevent or treat 8.1.2 Explain the health benefits of meeting physical activity guidelines and the health risks of not achieving
chronic disease minimum physical activity levels
8.1.3 Describe how social determinants and community infrastructure can affect physical activity in different
populations
8.1.4 Determine effective physical activity interventions that can improve population health
8.2 Understand strategies for 8.2.1 Organise local community resources that are available to promote exercise and physical activity
community engagement 8.2.2 Examine social and economic barriers to exercise for individuals and communities
Practical elements
► For a defined population of patients within a clinic/hospital-based setting, determine whether physical activity improved a chronic disease marker (eg, hypertension,
hyperlipidaemia, diabetes, obesity) over a 3- month period
► Design an exercise programme for individuals (>10 people) from an underserved community, disadvantaged background, or disabled group
► Locate at least five different types of accessible resources (eg, community partners, online videos) that can be used to assist physical activity promotion for patients or a
community
► Identify at least one funding source to assist patients in need of financial assistance to conduct a physical activity programme
► Identify barriers, including social and economic, to exercise for individuals within your community or society as a whole and consider how advocacy can be part of the solution
the skills necessary to prescribe physical activity for commonly Ultimately, physicians who have the ability to properly promote
encountered medical conditions. Within residency, the promo- exercise and physical activity as a form of medicine in their clin-
tion of physical activity and exercise may be incorporated into ical practices can have a dramatic impact on health outcomes
an existing curriculum, or as a part of a broader lifestyle medi- for their patients at a reduced cost to the healthcare system.14–16
cine curriculum that includes training in how to promote phys- While the curricula offer guidance on physical activity promo-
ical activity, healthy nutrition, and proper sleep hygiene. Finally, tion at various levels of medical education, there are some limita-
the curriculum for EM-PAP within sports medicine fellowship tions worth noting. For instance, institutions and programmes
training includes a more focused, in-depth experience. Expe- may differ in the timing, approach, and evaluation of how
riences and clinical encounter benchmarks may vary based on trainees are educated. These differences may alter how the prin-
institutional and programmatic resources and infrastructure; ciples of the proposed curricula are implemented. Neverthe-
however, the curriculum offers a framework for incorporating less, the curricula capitalise on foundational elements and core
experiences to better prepare the trainee for clinical practice. disease processes that are taught at each level of training. Thus,
374 Asif I, et al. Br J Sports Med 2022;56:369–375. doi:10.1136/bjsports-2021-104819
Consensus statement
Br J Sports Med: first published as 10.1136/bjsports-2021-104819 on 10 January 2022. Downloaded from http://bjsm.bmj.com/ on March 19, 2022 by guest. Protected by copyright.
our hope is that these components can be taught with minimal Aaron Monseau, Paul Gubanich, Jennifer R. Maynard, David Ross, Andrew Gregory,
additional resource utilisation. With regard to residency educa- NiCole Ruth Keith, Nailah Coleman, Cindy Lin, Cynthia R. LaBella, Liz Joy, Keri Denay,
Mats Börjesson, Brandee L. Waite, Lailah Issac, Martin Schwellnus, Robert E. Sallis,
tion, benchmarks for the number of clinical encounters will likely Stephanie A. Kliethermes and Nicola Sewry.
vary because there are significant differences between specialties.
Contributors IA and JD conceived the idea and drafted the initial manuscript. All
Implementation and necessary modifications may occur at the
of the authors contributed to data collection and review of the final manuscript.
discretion of the programme to best fit their training paradigm.
Competing interests Oosterhealth Charitable Foundation (Boston, MA) has
Finally, these curricula have a particular focus on clinical expe-
provided financial support for this work.
rience and training. They are meant to complement, rather than
Patient consent for publication Not applicable.
replace, existing content on the overall benefits of exercise and
physical activity. Provenance and peer review Not commissioned; externally peer reviewed.
Future directions include the development of specific educa- ORCID iDs
tional content within the proposed curricula and standardised Irfan Asif http://orcid.org/0000-0003-0655-6264
assessments that could drive curriculum change at all levels. This Jane S Thornton http://orcid.org/0000-0002-3519-7101
may include online modules that could be adopted by training Jonathan Drezner http://orcid.org/0000-0003-3519-9120
programmes worldwide. Similar educational material has been
created through international collaboration (eg, Sports Cardi- REFERENCES
ology ECG Interpretation Training Modules) and has formed 1 World Health Organization. Preventing chronic diseases: a vital investment. WHO
global report, 2005. Available: https://www.who.int/chp/chronic_disease_report/full_
the basis for elevating the knowledgebase in general medical and
report.pdf [Accessed Mar 2021].
SEM trainees. When developing the suggested resources for use 2 Asif IM, Drezner JA. Sports and exercise medicine education in the USA: call to action.
in medical curricula, the end users of the resources (eg, medical Br J Sports Med 2020;54:195–6.
students/trainees and patients) should be included, especially 3 Dacey ML, Kennedy MA, Polak R, et al. Physical activity counseling in medical school
those from under-represented groups who are at highest risk education: a systematic review. Med Educ Online 2014;19:24325.
4 Wattanapisit A, Petchuay P, Wattanapisit S, et al. Developing a training programme in
of lifestyle diseases, and less likely to meet PA guidelines. This physical activity counselling for undergraduate medical curricula: a nationwide Delphi
will ensure the resources are relevant to the end users, and thus study. BMJ Open 2019;9:e030425.
improve the likelihood of uptake and impact of the resources. 5 Strong A, Stoutenberg M, Hobson-Powell A, et al. An evaluation of physical activity
training in Australian medical school curricula. J Sci Med Sport 2017;20:534–8.
6 Weiler R, Chew S, Coombs N, et al. Physical activity education in the undergraduate
CONCLUSION curricula of all UK medical schools: are tomorrow’s doctors equipped to follow clinical
The adoption of lifelong exercise and physical activity habits guidelines? Br J Sports Med 2012;46:1024–6.
can dramatically improve the health of patients and popula- 7 Stoutenberg M, Stasi S, Stamatakis E, et al. Physical activity training in US medical
tions. Physicians must be appropriately trained to be effective schools: preparing future physicians to engage in primary prevention. Phys Sportsmed
at counselling patients and promoting physical activity. The 2015;43:388–94.
8 Antognoli EL, Seeholzer EL, Gullett H, et al. Primary care resident training for obesity,
proposed curricula are the first published guidelines to offer nutrition, and physical activity counseling: a mixed-methods study. Health Promot
programmatic elements for longitudinal training in EM-PAP for Pract 2017;18:672–80.
medical students, residents and sports medicine fellows at US 9 Fulton JE. Physical inactivity is more common among racial and ethnic minorities
medical institutions. We believe access and implementation of in most states, 2020. Conversations in equity. Available: https://blogs.cdc.gov/
healthequity/2020/04/01/physical-inactivity/ [Accessed Mar 2021].
these curricula will facilitate training of physicians competent
10 Wilson-Frederick SM, Thorpe RJ, Bell CN, et al. Examination of race disparities in
in promoting exercise and physical activity within their clinical physical inactivity among adults of similar social context. Ethn Dis 2014;24:363–9.
practices for the betterment of the health and well-being of their 11 World Health Organization. Physical activity promotion in socially disadvantaged
patients. groups: principles for action, 2013. Available: https://wwwwhoint/chp/chronic_
disease_report/full_reportpdf [Accessed Mar 2021].
12 Humphries D, Jaques R, Dijkstra HP, et al. A Delphi developed syllabus for the medical
Author affiliations
1 specialty of sport and exercise medicine. Br J Sports Med 2018;52:490–2.
Department of Family and Community Medicine, The University of Alabama at
Birmingham, Birmingham, Alabama, USA 13 Humphries D, Jaques R, Dijkstra HP, et al. Delphi developed syllabus for the medical
2
Public Health and Family Medicine, University of Western Ontario Schulich School of specialty of sport and exercise medicine: Part 2. Br J Sports Med 2021;55:81–3.
Medicine and Dentistry, London, Ontario, Canada 14 Sutherland R, Reeves P, Campbell E, et al. Cost effectiveness of a multi-component
3
University of South Carolina School of Medicine Greenville Campus, Greenville, school-based physical activity intervention targeting adolescents: the ’Physical Activity
South Carolina, USA 4 Everyone’ cluster randomized trial. Int J Behav Nutr Phys Act 2016;13:94.
4
Family Medicine and Sports Medicine, Wake Forest University, Winston-Salem, North 15 Dallmeyer S, Wicker P, Breuer C. The relationship between physical activity and out-of-
Carolina, USA pocket health care costs of the elderly in Europe. Eur J Public Health 2020;30:628–32.
5
Orthopaedics, Henry Ford Health System, Sterling Heights, Michigan, USA 16 Carlson SA, Fulton JE, Pratt M, et al. Inadequate physical activity and health care
6
Family Medicine, Howard Hughes Medical Institute-Oregon Health and Science expenditures in the United States. Prog Cardiovasc Dis 2015;57:315–23.
University School of Medicine, Portland, Oregon, USA 17 Saint-Maurice PF, Troiano RP, Bassett DR, et al. Association of daily step count and
7
Department of Family and Community Medicine, University of Nevada Reno School step intensity with mortality among US adults. JAMA 2020;323:1151–60.
of Medicine, Reno, Nevada, USA 18 Lobelo F, Muth ND, Hanson S, et al. Physical activity assessment and counseling in
8
Department of Orthopaedics and Rehabilitation, University of Florida, Gainesville, pediatric clinical settings. Pediatrics 2020;145. doi:10.1542/peds.2019-3992. [Epub
Florida, USA ahead of print: 24 02 2020].
9
Center for Sports Cardiology, University of Washington, Seattle, Washington, USA 19 Asif IM, Drezner JA. Recommendations for sports cardiology training for the sports
medicine physician. In: Wilson MG, Drezner JA, Sharma S, eds. IOC manual of sports
cardiology. Oxford, UK: Wiley Blackwell, 2017: 493–502.
Twitter Jane S Thornton @janesthornton and Jonathan Drezner @DreznerJon 20 Rodgers GP, Ayanian JZ, Balady G, et al. American College of Cardiology/American
Acknowledgements The authors would like to acknowledge the many experts in heart association clinical competence statement on stress testing. Circulation
the field who generously reviewed this manuscript and offered valuable feedback: 2000;102:1726–38.
Asif I, et al. Br J Sports Med 2022;56:369–375. doi:10.1136/bjsports-2021-104819 375
You might also like
- ACSM Guidelines DownloadDocument11 pagesACSM Guidelines DownloadGOLDEN FIZZIK GYM14% (14)
- Obstetricia y Ginecología Beckman 8a EdicionDocument477 pagesObstetricia y Ginecología Beckman 8a EdicionAlejandro Mora100% (3)
- Research ProposalDocument19 pagesResearch ProposalNordean Afd KNo ratings yet
- Strength Training in Children and Adolescents: Raising The Bar For Young Athletes?Document4 pagesStrength Training in Children and Adolescents: Raising The Bar For Young Athletes?LEE JunhyukNo ratings yet
- Sports Med CareersDocument4 pagesSports Med Careersgrimuri31No ratings yet
- May JYI 2Document5 pagesMay JYI 2sooriroyNo ratings yet
- Youth Resistance Training Position StateDocument22 pagesYouth Resistance Training Position StateLeonidas FagundesNo ratings yet
- Viewcontent CgiDocument13 pagesViewcontent CgimariaNo ratings yet
- ACSM Exercise Science Career PathsDocument5 pagesACSM Exercise Science Career PathsHugo MaisNo ratings yet
- Review of Literature: Presented By: Mrunmayi Gadre 1 MPT Department of Pediatric PhysiotherapyDocument41 pagesReview of Literature: Presented By: Mrunmayi Gadre 1 MPT Department of Pediatric PhysiotherapyANKITA SHETTYNo ratings yet
- Position - Stand - Youth - Resistance - Training - 2009 PDFDocument20 pagesPosition - Stand - Youth - Resistance - Training - 2009 PDFDân NguyễnNo ratings yet
- Strength Training: The Physician and SportsmedicineDocument10 pagesStrength Training: The Physician and SportsmedicineAdrian RuizNo ratings yet
- ACSMs Exercise Testing Prescription PDFDocument6 pagesACSMs Exercise Testing Prescription PDFHARIZNo ratings yet
- ACSMs Exercise Testing Prescription PDFDocument6 pagesACSMs Exercise Testing Prescription PDFHARIZNo ratings yet
- Versic 2021Document16 pagesVersic 2021Willian da costaNo ratings yet
- Faigenbaum y Myer - 2009 - Pediatric Resistance Training Benefits, ConcernsDocument9 pagesFaigenbaum y Myer - 2009 - Pediatric Resistance Training Benefits, ConcernsAna IriarteNo ratings yet
- Importance of Health Science Education For.4Document6 pagesImportance of Health Science Education For.4Giovanni PontelliNo ratings yet
- AJGP 0102 2020 Focus Desbrow Sports Nutrition Amateur Athletes WEBDocument6 pagesAJGP 0102 2020 Focus Desbrow Sports Nutrition Amateur Athletes WEBIgor PavlovicNo ratings yet
- 06 Chapter - 1Document24 pages06 Chapter - 1Jyothish KBNo ratings yet
- Research Article Prevention of Physical Risk and Rehabilitation of Muscle Injury in Sanda CompetitionDocument9 pagesResearch Article Prevention of Physical Risk and Rehabilitation of Muscle Injury in Sanda Competition壮No ratings yet
- Sports Medicine .....Document9 pagesSports Medicine .....ScribdTranslationsNo ratings yet
- Ra 3Document10 pagesRa 3Heli MalivadNo ratings yet
- Sports MedicineDocument25 pagesSports MedicinedhanushrcksNo ratings yet
- Efects of Inspiratory Muscle Training in Older AdultsDocument10 pagesEfects of Inspiratory Muscle Training in Older AdultsMaría Camila Zuluaga AriasNo ratings yet
- 2019 Article AbstractsFromThe5thInternation PDFDocument41 pages2019 Article AbstractsFromThe5thInternation PDFStephano NgangiNo ratings yet
- Ijspt 06 241 PDFDocument13 pagesIjspt 06 241 PDFNovy DitaNo ratings yet
- Citius Altius Fortius Beneficial Effects of Resistance Training For Young AthletesDocument9 pagesCitius Altius Fortius Beneficial Effects of Resistance Training For Young Athletesfrancosala2012No ratings yet
- Effects of Different Exercise Interventions On Risk of Falls A Systematic ReviewDocument10 pagesEffects of Different Exercise Interventions On Risk of Falls A Systematic ReviewLeonardoValenzuelaNo ratings yet
- Haff 2010Document13 pagesHaff 2010DJNo ratings yet
- Effect of Supervised, Periodized Exercise Training vs. Self-Directed Training On Lean Body Mass and Other Fitness Variables in Health Club MembersDocument12 pagesEffect of Supervised, Periodized Exercise Training vs. Self-Directed Training On Lean Body Mass and Other Fitness Variables in Health Club MembersCeleste AyalaNo ratings yet
- Dose in Exercise Based Dysphagia Therapies: A Scoping ReviewDocument32 pagesDose in Exercise Based Dysphagia Therapies: A Scoping ReviewValentina SalasNo ratings yet
- Nutrition and Physical Activity InterventionsDocument28 pagesNutrition and Physical Activity Interventionsoknutricion1No ratings yet
- Peterson Et Al, 2004Document6 pagesPeterson Et Al, 2004Bernardo Ravanello da CostaNo ratings yet
- 01 SynopsisDocument24 pages01 SynopsisBilisuma MuletaNo ratings yet
- Strength Training Frequency and Athletic PerformanceDocument13 pagesStrength Training Frequency and Athletic Performance超卓No ratings yet
- 10.1519 1533-4287 (2003) 017 0734 Iotpoi 2.0Document5 pages10.1519 1533-4287 (2003) 017 0734 Iotpoi 2.0Stefan KovačevićNo ratings yet
- 216 FullDocument5 pages216 Fullalinaisabelaanghel5306No ratings yet
- American Medical Society For Sports MedicineDocument13 pagesAmerican Medical Society For Sports MedicineAlvaroNo ratings yet
- The Physiological and Physical Benefits of Two Types of Concurrent Training: A Randomized Controlled TrialDocument10 pagesThe Physiological and Physical Benefits of Two Types of Concurrent Training: A Randomized Controlled TrialChloe BujuoirNo ratings yet
- Physiotherapy in Sports 2013Document8 pagesPhysiotherapy in Sports 2013Diany CéspedesNo ratings yet
- Journal of Exercise Science & Fitness: Shi Zhou, Kade Davison, Fei Qin, Kuei-Fu Lin, Bik-Chu Chow, Jie-Xiu ZhaoDocument10 pagesJournal of Exercise Science & Fitness: Shi Zhou, Kade Davison, Fei Qin, Kuei-Fu Lin, Bik-Chu Chow, Jie-Xiu Zhaoapi-583367679No ratings yet
- The Overtraining Syndrome NeuroDocument11 pagesThe Overtraining Syndrome NeurodserraNo ratings yet
- Practical ExamDocument8 pagesPractical ExamRexNo ratings yet
- 08 Iajps08102017 PDFDocument5 pages08 Iajps08102017 PDFBaru Chandrasekhar RaoNo ratings yet
- Ackermann Et Al 2022 - Assessing Performing Artists in Medical and Health Practice - The Dancers, Instrumentalists, Vocalists, and Actors Screening ProtocolDocument3 pagesAckermann Et Al 2022 - Assessing Performing Artists in Medical and Health Practice - The Dancers, Instrumentalists, Vocalists, and Actors Screening ProtocolCarlos TinocoNo ratings yet
- Ajay VermaDocument18 pagesAjay VermabugsbusgNo ratings yet
- Knowledge Attitude and Practices KAP TowDocument9 pagesKnowledge Attitude and Practices KAP TowJaheda AktherNo ratings yet
- PP Assignment 2 by Anas Bin Mujeeb SAP# 21625 (MSPT-SPT)Document4 pagesPP Assignment 2 by Anas Bin Mujeeb SAP# 21625 (MSPT-SPT)Anas MujeebNo ratings yet
- NR527 Module 3 (Health Promotion)Document5 pagesNR527 Module 3 (Health Promotion)96rubadiri96No ratings yet
- The Systemic Effects of Blood Flow Restriction Training A Systematic ReviewDocument13 pagesThe Systemic Effects of Blood Flow Restriction Training A Systematic ReviewFederico BristotNo ratings yet
- Musculoskeletal Physiotherapists' Use of Psychological Interventions: A Systematic Review of Therapists' Perceptions and PracticeDocument8 pagesMusculoskeletal Physiotherapists' Use of Psychological Interventions: A Systematic Review of Therapists' Perceptions and PracticeTom StevensNo ratings yet
- Intconference PatialaDocument15 pagesIntconference PatialaPrakash S MNo ratings yet
- Applsci 11 08397Document10 pagesApplsci 11 08397Jyothish KBNo ratings yet
- High Intensity Small Muscle Mass Training in Patients With CHFDocument7 pagesHigh Intensity Small Muscle Mass Training in Patients With CHFbcvaughn019No ratings yet
- Essay - Role of PT in SportsDocument2 pagesEssay - Role of PT in SportsAlexander ScottNo ratings yet
- PIIS1440244018312702Document25 pagesPIIS1440244018312702Jesus Maturana YañezNo ratings yet
- SMB Youth Strength TrainingDocument2 pagesSMB Youth Strength Traininghadyahmed0318No ratings yet
- DaliwalDocument8 pagesDaliwalV.T. SrinivasanNo ratings yet
- 2022 Contribución de Los Fisioterapeutas Deportivos Al Equipo de Medicina Deportiva y Del Ejercicio.Document2 pages2022 Contribución de Los Fisioterapeutas Deportivos Al Equipo de Medicina Deportiva y Del Ejercicio.contact.movementsiteNo ratings yet
- Study of Physical Fitness Index Using Modified Harvard Step Test in Relation With Body Mass Index in Physiotherapy StudentsDocument4 pagesStudy of Physical Fitness Index Using Modified Harvard Step Test in Relation With Body Mass Index in Physiotherapy StudentsUswatun HasanahNo ratings yet
- 3Document4 pages3Rafiq ShahNo ratings yet
- Doctor List: Employee Name Employee Code Head QTR Division GatleDocument53 pagesDoctor List: Employee Name Employee Code Head QTR Division GatleNext Vision HomeNo ratings yet
- Training Manual On How To Teach Medical EthicsDocument33 pagesTraining Manual On How To Teach Medical EthicsghaiathmeNo ratings yet
- Developmental Pediatric ReviewDocument16 pagesDevelopmental Pediatric ReviewGhada HusseinNo ratings yet
- CombinedMerit2nd RjmornkDocument73 pagesCombinedMerit2nd RjmornkBhumi GargNo ratings yet
- JSS Medical College Mysore: Admissions 2023, Courses Offerd, Fees Structure, Cutoff, CounsellingDocument27 pagesJSS Medical College Mysore: Admissions 2023, Courses Offerd, Fees Structure, Cutoff, CounsellingJustGetAdmissionNo ratings yet
- The Role of Assessment in Competency-Based Medical EducationDocument8 pagesThe Role of Assessment in Competency-Based Medical EducationMaria PalaciosNo ratings yet
- (AIQ AND DNB) Seat Matrix Stray Vacancy Round MDDocument261 pages(AIQ AND DNB) Seat Matrix Stray Vacancy Round MDSathish KumarNo ratings yet
- Advt 2023 For WebsiteDocument5 pagesAdvt 2023 For WebsiteSumit SinghNo ratings yet
- Web Options - YSRUHSDocument2 pagesWeb Options - YSRUHSshivesh.agrawalNo ratings yet
- Educational Leadership Portfolio Template: Match To Standard-Setting Example(s)Document2 pagesEducational Leadership Portfolio Template: Match To Standard-Setting Example(s)Lileng LeeNo ratings yet
- Department of OphthalmologyDocument1 pageDepartment of Ophthalmologybibiah705No ratings yet
- Clear Vacancy Round 2 Mbbs - Bds Ug Counselling 2022Document232 pagesClear Vacancy Round 2 Mbbs - Bds Ug Counselling 2022punithNo ratings yet
- Stephanie H. Pincus, M.D., M.B.A.Document25 pagesStephanie H. Pincus, M.D., M.B.A.allcooNo ratings yet
- Abim Cbe The BasicsDocument53 pagesAbim Cbe The Basicsperie_mdNo ratings yet
- UG MBBS 2021-22college Wise P2Document75 pagesUG MBBS 2021-22college Wise P2sony sonyNo ratings yet
- Unfilled Programs by State: Reproduction Is Prohibited Without The Written Consent of The NRMP ®Document1 pageUnfilled Programs by State: Reproduction Is Prohibited Without The Written Consent of The NRMP ®Kuljeet VirkNo ratings yet
- Aipmt Round 3Document335 pagesAipmt Round 3AnweshaBoseNo ratings yet
- AIIMS Jodhpur Is The Best Medical College To Lead The Way To Success With MBBS in 2023-24.Document23 pagesAIIMS Jodhpur Is The Best Medical College To Lead The Way To Success With MBBS in 2023-24.Edufever OfficialNo ratings yet
- KONSULTA 073123 v1Document124 pagesKONSULTA 073123 v1Substationsix MalaboncpsNo ratings yet
- Medical Education in India and The Medical Council of India (MCI)Document22 pagesMedical Education in India and The Medical Council of India (MCI)Sabyasachi Sircar33% (3)
- Rajiv Gandhi University of Health SciencesDocument148 pagesRajiv Gandhi University of Health Sciencesriya yadavNo ratings yet
- A J InstituteDocument9 pagesA J InstitutealnavaraNo ratings yet
- Antiragging Committee - Jan-20Document1 pageAntiragging Committee - Jan-20TRH RECRUITMENTNo ratings yet
- BME 2015 v2 PDFDocument60 pagesBME 2015 v2 PDFTito PajueloNo ratings yet
- RMC Meu Annual Report 2019 20Document14 pagesRMC Meu Annual Report 2019 20abcqwe123No ratings yet
- List of Agencies With Recognition Status and ApplyingDocument6 pagesList of Agencies With Recognition Status and ApplyingMwanja MosesNo ratings yet
- Usmle Score CorrelationDocument4 pagesUsmle Score CorrelationIffat KabirNo ratings yet
- Simulation-Based Medical Education: Time For A Pedagogical ShiftDocument5 pagesSimulation-Based Medical Education: Time For A Pedagogical ShiftAshish kumarNo ratings yet