Professional Documents
Culture Documents
Compartments Fluid
Compartments Fluid
Uploaded by
Aurelia AlexandraOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Compartments Fluid
Compartments Fluid
Uploaded by
Aurelia AlexandraCopyright:
Available Formats
FLUID COMPARTMENTS
30. Fluid compartments
Describe the major fluid > Total body water (TBW) varies depending on age, size, gender
compartments of the body in and fat content. It is approximately 60% of body weight (BW) in the
the adult. average adult male (i.e. 42 L) and 50% in the average adult female.
The remainder of the weight is made up of protein, minerals and fat.
The main components of TBW are the extracellular and intracellular
compartments.
> Intracellular fluid (ICF) makes up two-thirds of TBW (i.e. 28 L), and is
contained within the phospholipid bilayer of the cell membrane.
> Extracellular fluid (ECF) makes up one-third of TBW (i.e. 14 L). This is
divided into:
• interstitial fluid (ISF), which makes up 75% of the ECF (i.e. 9.5 L)
and lies between cells, but outside the cell membrane
• plasma, making up 25% of the ECF (i.e. 3.5 L), contained within the
vasculature
• transcellular fluids (TCF) (i.e.1 L), which are secreted fluids that are
separated from the plasma by an epithelial layer (pleural, peritoneal,
gastrointestinal fluids, CSF, intra-ocular fluids, sweat, saliva and bile),
the so-called ‘third space’
> Total blood volume (TBV) consists of plasma and red cell volume, and
is 5–6 L.
Table 30.1 Fluid compartments for a 70 kg male
Compartment % BW % TBW % ECF Volume (L)
TBW ±60 42
ICF 40 67 28
ECF 20 33 14
• ISF 15 10.5 75 9.5
• plasma 5 3.5 25 3.5
• TCF <1 1.0
Compare the adult with the Table 30.2 Comparison of neonatal and adult fluid compartments
neonate fluid compartments.
Compartment Adult Neonate
TBW (% BW) 60 75–85
Fat (% BW) 20–25 5–15
ECF (% BW) 20 30–45
ICF (% BW) 40 <40
Plasma (% BW) 5 5
Note that in premature babies, ECF exceeds ICF.
93
9781785230981_text.indb 93 24/02/16 9:36 pm
01 PHYSIOLOGY
Describe the cell membrane Cell membrane: this is a selectively permeable membrane that separates
and capillary barriers and the the intracellular contents from the extracellular environment. It consists
movement of molecules across of a phospholipid bilayer with hydrophobic heads on either side of the
them. membrane and hydrophilic tails facing inwards. This arrangement allows fat-
soluble molecules to diffuse easily across the membrane, but prevents the
movement of polar molecules (amino acids, nucleic acids, carbohydrates,
proteins and ions), which is enabled by transmembrane protein complexes
such as pores, channels and gates. The movement of substances can be
either ‘passive’ or ‘active’, i.e. with or without the expenditure of energy. The
transport mechanisms involved include:
> Passive osmosis and diffusion across a concentration gradient:
small molecules/ions such as CO2 and O2 can move across the plasma
membrane by diffusion. The concentration gradient also sets up an
osmotic flow for water.
> Transmembrane protein channels and transporters: molecules
such as sugars, amino acids and certain products of metabolism may:
• Passively diffuse through protein channels (such as aquaporins in the
case of water) in facilitated diffusion, or
• Actively be pumped across the membrane by transmembrane
transporters.
> Endocytosis: cell membrane creates a vesicle, capturing the substance
and internalising it, e.g. phagocytosis. This is a form of active transport.
> Exocytosis: the membrane of a vesicle fuses with the plasma
membrane, expelling its contents into the extracellular environment, e.g.
hormones and enzymes.
Capillary wall: consists of a single layer of simple squamous epithelium
and a basement membrane (basal lamina). Capillaries connect arteries and
veins within organ systems across a branched network called the capillary
bed. The more metabolically active an organ is, the larger the capillary bed.
Small molecules (<3 nm) such as water, oxygen and carbon dioxide cross
the capillary wall through the space between cells (paracellular transport),
while larger molecules (>3 nm) such as albumin and other large proteins
pass through transcellular transport carried inside vesicles. There are three
main types of capillaries:
> Continuous: uninterrupted lining with tight junctions and complete basal
lamina. Allow passive diffusion of lipid-soluble molecules and movement
of small molecules such as water and ions through intercellular clefts.
Skeletal muscle and skin have numerous transport vesicles, whereas
CNS (blood–brain barrier) has few, so sealing the paracellular space.
> Fenestrated: endothelial cells have pores or windows (60–80 nm
in diameter) and a complete basal lamina. Allow a limited amount of
proteins to diffuse. They are located in intestines, pancreas, endocrine
glands and renal glomeruli.
> Sinusoidal: large open-pore (30–40 µm in diameter) capillaries, large
gaps between cell junctions and a discontinuous basal lamina. Allow red
and white blood cells (7.5–25 µm diameter) and serum proteins to pass.
Present in bone marrow, lymph nodes, liver, spleen and adrenal glands.
How are the body compartment Dilutional techniques are used to estimate compartment volumes.
volumes estimated? An indicator dye is injected into the compartment to be measured. The dye
should distribute throughout that compartment, but remain contained within
it. The concentration of the dye is measured and the mass administered is
known. Thus, using the formula for volume of distribution (Vd = mass of dye/
concentration), the compartment volume can be estimated.
Some compartments are derived (ICF, ISF and TBV).
94
9781785230981_text.indb 94 24/02/16 9:36 pm
FLUID COMPARTMENTS
Table 30.3 Methods of measurement of fluid compartments
Compartment Characteristic of indicator Indicator
TBW Freely diffusible substance Deuterium oxide
Antipyrine
ECF Substances that do not enter cells Inulin
Thiocyanate
Thiosulphate
ICF TBW – ECF
Plasma Substances confined to plasma Radiolabelled albumin
Evan’s blue dye
Red cell volume Radiolabelled red cells
TBV Plasma volume × 100/(100 – haematocrit)
Interstitial fluid ECF – plasma volume
What factors regulate Water balance governs the ICF, and sodium balance regulates the ECF
body water? compartments. (mnemonic WISE: Water regulates Intracellular; Sodium
regulates Extracellular)
The control of TBW is linked to the secretion of antidiuretic hormone (ADH/
vasopressin) by the posterior pituitary.
ADH is secreted in response to:
> Hyperosmolarity (threshold 1–2%) detected by osmoreceptors in the
hypothalamus, outside the blood–brain barrier. Similarly, osmoreceptors
stimulate thirst
> Volume depletion (ECF) detected by low-pressure baroreceptors in great
veins, atria and pulmonary vessels, and high-pressure baroreceptors in
the carotid sinus and aortic arch (threshold 7% change in volume)
> Angiotensin II (AGII)
> Other: pain, exercise, stress, emotion, nausea and vomiting, standing,
nicotine, morphine, barbiturates, carbamazepine.
ADH secretion is reduced in response to:
> Low osmolarity
> Increased ECF volume
> Alcohol
The renal effects of ADH on water balance include:
> Increased water permeability in cortical collecting tubule (V2 receptors)
> Increased water and urea permeability in medullary collecting tubule
> Increased retention of water
> Reduced urine volume
Other ADH effects include:
> Release of factor 8 by the endothelium (V2)
> Platelet aggregation and degranulation (V1)
> Arteriolar vasoconstriction (V1)
Sodium balance governs the ECF volume (as water passively diffuses across
membranes when sodium is reabsorbed) and is regulated by:
> Dietary sodium intake
> ECF volume (baroreceptors) and ADH secretion
> GFR and tubuloglomerular feedback.
> Renin–angiotensin–aldosterone system:
• Efferent arteriolar vasoconstriction to maintain GFR
• Direct sodium reabsorption
• Secretion of aldosterone from adrenal cortex
• Increased ADH
• Increased thirst (water retention)
• Negative feedback on renin release
95
9781785230981_text.indb 95 24/02/16 9:36 pm
01 PHYSIOLOGY
> Aldosterone and other adrenocortical hormones:
• Reabsorption of NaCl (30–90 minute latent period)
• Excretion of K+
• Secretion of H+
• Accompanied by changes in ADH.
> Rate of tubular secretion of K+ and H+
> Atrial natriuretic peptide (ANP) and other natriuretic hormones:
• Secreted by atrial myocytes in response to atrial stretch due ECF
expansion (from high NaCl intake or IV infusion of saline)
• Actions include natriuresis (by an increase in GFR and tubular
excretion of sodium), reduction in BP (by reduced responsiveness of
vascular smooth muscle to vasoconstrictors) and reduced secretion of
aldosterone, ADH, renin and consequently AGII.
What is the effect of a sudden IV > 5% dextrose is a hypotonic solution and therefore gets distributed
infusion of 5% dextrose? equally throughout all the fluid compartments. It can be thought of as
water because the dextrose gets metabolised leaving behind water,
which diffuses freely.
> Intravascular volume will thus increase only minimally (by approximately
70 mL if 1 L was administered).
> This is less than the 7–10% threshold needed to stimulate the
baroreceptors.
> However, the plasma osmolarity will decrease enough to stimulate
the osmoreceptors (1–2% threshold) and therefore ADH secretion will
decrease, increasing renal water excretion.
What is the effect of an IV infusion This is an isotonic solution and results in ECF expansion, diuresis and
of 1 L 0.9% saline solution? natriuresis as explained below:
> Sodium will diffuse from areas of high concentration to those of lower
concentrations and will be followed by water
> The cell membrane is impermeable to sodium and thus the distribution
of the saline (water) administered will be confined to the ECF with 75%
(750 mL) in the ISF and 25% (250 mL) in the plasma
> The plasma expansion from 3.5 to 3.75 L is enough (7% increase) to be
detected by the baroreceptors and ADH secretion is reduced
> The increased sodium load and ECF expansion will cause an increase in
ANP secretion and natriuresis, and inhibition of the renin–angiotensin–
aldosterone system.
96
9781785230981_text.indb 96 24/02/16 9:36 pm
You might also like
- Preclinical Physiology Review 2023: For USMLE Step 1 and COMLEX-USA Level 1From EverandPreclinical Physiology Review 2023: For USMLE Step 1 and COMLEX-USA Level 1Rating: 1 out of 5 stars1/5 (1)
- ENN PHARMACOLOGY BUNDLE PrintDocument142 pagesENN PHARMACOLOGY BUNDLE Printronique reid88% (8)
- Pharm Phlash Cards Pharmacology Flash Cards 2nd EditionDocument466 pagesPharm Phlash Cards Pharmacology Flash Cards 2nd EditionDerricka Crosby100% (1)
- The Primary FRCA Structured Oral Examination: Study Guide 1Document13 pagesThe Primary FRCA Structured Oral Examination: Study Guide 1Aurelia Alexandra0% (1)
- Lecture & Review Guide in HEMATOLOGY 1 & 2 (COMPLETE)Document58 pagesLecture & Review Guide in HEMATOLOGY 1 & 2 (COMPLETE)Kirt Anonuevo100% (4)
- Cell Physiology Body Fluids Part IIDocument40 pagesCell Physiology Body Fluids Part IIMayne Ramzelle TamanoNo ratings yet
- Fluid PhysiologyDocument4 pagesFluid PhysiologyMd Ahsanuzzaman PinkuNo ratings yet
- Fluids and Electrolytes 2023Document26 pagesFluids and Electrolytes 2023dj77djcqy7No ratings yet
- Body FluidsDocument38 pagesBody FluidsGift AiyegbeniNo ratings yet
- Body Fluid, MML, 2021Document51 pagesBody Fluid, MML, 2021Boon AimanNo ratings yet
- Body Fluids 1 and 2: ObejctivesDocument15 pagesBody Fluids 1 and 2: ObejctivesJoanne Bernadette AguilarNo ratings yet
- L1-Introduction To Human PhysiologyDocument7 pagesL1-Introduction To Human PhysiologyPIH SHTNo ratings yet
- Body Fluids 1Document29 pagesBody Fluids 1Mohammed EzzatNo ratings yet
- Body FluidDocument15 pagesBody Fluidrj100% (1)
- Body FluidDocument22 pagesBody Fluidratishroy56No ratings yet
- Body Fluids Fluid Physiology NotesDocument19 pagesBody Fluids Fluid Physiology NotesBrianNo ratings yet
- Body Fluid CompartmenBDSDocument17 pagesBody Fluid CompartmenBDSHimani JhaNo ratings yet
- Disorders of Water BalanceDocument64 pagesDisorders of Water BalanceRadley Jed C. PelagioNo ratings yet
- PhysiologyDocument72 pagesPhysiologyMurali LeeNo ratings yet
- 3-s2.0-B9780323532655000150 15 - Disorders of Water Balance Joseph G. VerbalisDocument64 pages3-s2.0-B9780323532655000150 15 - Disorders of Water Balance Joseph G. VerbalisDEWINo ratings yet
- (Intravenous Fluids) : Cellular Fluid CompartmentsDocument17 pages(Intravenous Fluids) : Cellular Fluid CompartmentsFatimaNo ratings yet
- Blood & Body Fluid Tortora 15TH EditionDocument20 pagesBlood & Body Fluid Tortora 15TH Edition334scisyb2020rishabhsingalNo ratings yet
- Physiology of Body FluidsDocument23 pagesPhysiology of Body FluidsRamadan Physiology100% (1)
- Body Fluids Membrane PotentialsDocument18 pagesBody Fluids Membrane Potentialsbeneficialboxer9237No ratings yet
- F&E For Elderly - ModuleDocument163 pagesF&E For Elderly - ModuleArihk NiladaNo ratings yet
- NA Control of Cell VolumeDocument28 pagesNA Control of Cell VolumeTom TsouNo ratings yet
- 1 Body FluidsDocument9 pages1 Body FluidsSenthereng MoaisiNo ratings yet
- Ch3 CELLDocument80 pagesCh3 CELLsawalekatumbo1No ratings yet
- Liquidos y Electrolitos 2016Document5 pagesLiquidos y Electrolitos 2016MARIA JOSE MEDINA JAIMES100% (1)
- Surgery Fluids & Electrolytes-1Document9 pagesSurgery Fluids & Electrolytes-1Aimie DagaleaNo ratings yet
- L1-Introduction To Human Physiology-2Document9 pagesL1-Introduction To Human Physiology-2PIH SHTNo ratings yet
- Terapi Cairan: Dr. M Zulkarnain B Mked (An), SpanDocument70 pagesTerapi Cairan: Dr. M Zulkarnain B Mked (An), SpanMerdianing Ika MahendraNo ratings yet
- Body Fluids 2022 StudentDocument36 pagesBody Fluids 2022 Studentshavindrap2000No ratings yet
- How About Organ Level Regulation?Document55 pagesHow About Organ Level Regulation?Raphael SevillaNo ratings yet
- Cell Membrane: Dr. Samia ShahbazDocument26 pagesCell Membrane: Dr. Samia Shahbazreema aslamNo ratings yet
- Kati Sriwiyati, Dr. Bagian Fisiologi FK UnswagatiDocument52 pagesKati Sriwiyati, Dr. Bagian Fisiologi FK UnswagatiMelia100% (1)
- MCQs in Fluid and Electrolyte Balance With AnswersDocument50 pagesMCQs in Fluid and Electrolyte Balance With Answersdrrajendrans80% (5)
- Body Fluid Compartments and Intro To PhysiologyDocument20 pagesBody Fluid Compartments and Intro To PhysiologyDoc HamsNo ratings yet
- Body Fluid: Presented BY DR (MRS) Okorie PDocument56 pagesBody Fluid: Presented BY DR (MRS) Okorie PKELECHI ELEJENo ratings yet
- Cells AnatomyDocument16 pagesCells AnatomyHoneylaine MaravillasNo ratings yet
- PGDBC IDocument47 pagesPGDBC IDr Estari MamidalaNo ratings yet
- 1 Cellular Transport VidDocument57 pages1 Cellular Transport Vidchizy bananaNo ratings yet
- Chapter 3 (Cell Structures)Document56 pagesChapter 3 (Cell Structures)hilmanNo ratings yet
- ScienceDocument32 pagesScienceAwais_123100% (1)
- Fluids and ElectrolytesDocument7 pagesFluids and ElectrolytesKarren FernandezNo ratings yet
- Body Fluids Hbc202-Lecture Notes-1Document9 pagesBody Fluids Hbc202-Lecture Notes-1Shreya AnandNo ratings yet
- Fluids and Electrolyte WorksheetStudentCopySection1Document6 pagesFluids and Electrolyte WorksheetStudentCopySection1XiaoDuckyNo ratings yet
- Body FluidDocument124 pagesBody FluidcussonmarvinNo ratings yet
- Cellular PhysiologyDocument3 pagesCellular PhysiologyMartin AlcantaraNo ratings yet
- Fluid Balance and Electrolyte Distribution in Human Body BCDocument28 pagesFluid Balance and Electrolyte Distribution in Human Body BCMasoume MohammadiNo ratings yet
- Fluid & Electrolyte Imbalances FinalDocument142 pagesFluid & Electrolyte Imbalances FinalPriyanka T100% (3)
- Body Fluids CompartmentDocument9 pagesBody Fluids CompartmentPankaj HatilaNo ratings yet
- Tor ElekDocument9 pagesTor ElekChaori NurfadillahNo ratings yet
- Transport Across Cell MembraneDocument38 pagesTransport Across Cell MembraneViswadeep DasNo ratings yet
- Chapter 3b Worksheet OpenstaxDocument10 pagesChapter 3b Worksheet Openstaxapi-255334265No ratings yet
- Cell Structure & Function-1Document54 pagesCell Structure & Function-1Saad Zafar AwanNo ratings yet
- 2. Introduction to Physiology & Body FluidsDocument25 pages2. Introduction to Physiology & Body Fluidsowotiajoshua7No ratings yet
- Anatomy and Physiology Module 2Document16 pagesAnatomy and Physiology Module 2JayR MendonesNo ratings yet
- Mahan 2Document7 pagesMahan 2KANT JAMES D. MAHANNo ratings yet
- 1-Passive Transport:: Selectively Permeable BarriersDocument19 pages1-Passive Transport:: Selectively Permeable Barriersapi-3706483No ratings yet
- Metabolic Disorders and Critically Ill Patients: From Pathophysiology to TreatmentFrom EverandMetabolic Disorders and Critically Ill Patients: From Pathophysiology to TreatmentCarole IchaiNo ratings yet
- 29 The Impact of Epidural On Bowel FunctionDocument4 pages29 The Impact of Epidural On Bowel FunctionAurelia AlexandraNo ratings yet
- Anti Fribrinolitic DrugsDocument15 pagesAnti Fribrinolitic DrugsAurelia AlexandraNo ratings yet
- Hypotermia and HipertermiaDocument9 pagesHypotermia and HipertermiaAurelia AlexandraNo ratings yet
- Anestezic Intracranial AnevrysmDocument4 pagesAnestezic Intracranial AnevrysmAurelia AlexandraNo ratings yet
- Importance, Scope of AnestheziaDocument4 pagesImportance, Scope of AnestheziaAurelia AlexandraNo ratings yet
- Severe Tracheal StenosisDocument5 pagesSevere Tracheal StenosisAurelia AlexandraNo ratings yet
- Neuromuscular Blockade MonitoringDocument7 pagesNeuromuscular Blockade MonitoringAurelia AlexandraNo ratings yet
- 22 The Application of Farmacodynamics in The Optimization of Antibiotic Therapy PDFDocument2 pages22 The Application of Farmacodynamics in The Optimization of Antibiotic Therapy PDFAurelia AlexandraNo ratings yet
- Hemodinamyc MonitoringDocument2 pagesHemodinamyc MonitoringAurelia AlexandraNo ratings yet
- Pulse OximetryDocument3 pagesPulse OximetryAurelia AlexandraNo ratings yet
- venTILATORIDocument3 pagesvenTILATORIAurelia AlexandraNo ratings yet
- Ultrasound Și DopplerDocument3 pagesUltrasound Și DopplerAurelia AlexandraNo ratings yet
- ADâncimea de Anestezie MOnITORINGDocument3 pagesADâncimea de Anestezie MOnITORINGAurelia AlexandraNo ratings yet
- Poluare Și ScavengingDocument3 pagesPoluare Și ScavengingAurelia AlexandraNo ratings yet
- CT Și RMNDocument3 pagesCT Și RMNAurelia AlexandraNo ratings yet
- Cursuri de Revisitare Și ValveDocument4 pagesCursuri de Revisitare Și ValveAurelia AlexandraNo ratings yet
- Lasers: What Do You Understand by The Term Laser'?Document3 pagesLasers: What Do You Understand by The Term Laser'?Aurelia AlexandraNo ratings yet
- Presiune Arterială WaveformDocument3 pagesPresiune Arterială WaveformAurelia AlexandraNo ratings yet
- Sisteme de BreathingDocument5 pagesSisteme de BreathingAurelia AlexandraNo ratings yet
- Monitori de DiscnecțieDocument2 pagesMonitori de DiscnecțieAurelia AlexandraNo ratings yet
- Featuri de Siguranță A Machinelor AnesteziceDocument3 pagesFeaturi de Siguranță A Machinelor AnesteziceAurelia AlexandraNo ratings yet
- PH MeasurementDocument2 pagesPH MeasurementAurelia AlexandraNo ratings yet
- Temperature MeasurementDocument4 pagesTemperature MeasurementAurelia AlexandraNo ratings yet
- Cardiac Utput MonitoringDocument7 pagesCardiac Utput MonitoringAurelia AlexandraNo ratings yet
- Carbon Dioxide MeasurementDocument2 pagesCarbon Dioxide MeasurementAurelia AlexandraNo ratings yet
- Presiune de Sânge MeasurementDocument3 pagesPresiune de Sânge MeasurementAurelia AlexandraNo ratings yet
- Oxygen MeasurementDocument4 pagesOxygen MeasurementAurelia AlexandraNo ratings yet
- SIGURANȚĂ eLeCTRICĂDocument3 pagesSIGURANȚĂ eLeCTRICĂAurelia AlexandraNo ratings yet
- States of Matter, Heat Capacity and Latent Heat: PhysicsDocument7 pagesStates of Matter, Heat Capacity and Latent Heat: PhysicsAurelia AlexandraNo ratings yet
- Islamic University in Uganda: Name: Abdiqani Omar NoorDocument11 pagesIslamic University in Uganda: Name: Abdiqani Omar NoorUsaid SulaimanNo ratings yet
- American Heart Association's Life's Simple 7: Lifestyle Recommendations, Polygenic Risk, and Lifetime Risk of Coronary Heart DiseaseDocument11 pagesAmerican Heart Association's Life's Simple 7: Lifestyle Recommendations, Polygenic Risk, and Lifetime Risk of Coronary Heart DiseaseJoban PhulkaNo ratings yet
- Part Two: Dr.S.Nishan Silva (MBBS)Document39 pagesPart Two: Dr.S.Nishan Silva (MBBS)SunnyEesuNo ratings yet
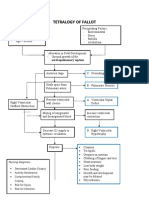
- Concept Map Tetralogy of FallotDocument2 pagesConcept Map Tetralogy of FallotKarl KiwisNo ratings yet
- Np3 Second Simulated Exam Nov 2023Document19 pagesNp3 Second Simulated Exam Nov 2023Shaine Ibarra AlabaNo ratings yet
- Syncope 3Document19 pagesSyncope 3Pratyush PrateekNo ratings yet
- Sas 35Document2 pagesSas 35Sistine Rose LabajoNo ratings yet
- Oparil KombinasiDocument15 pagesOparil KombinasipuspayunitaNo ratings yet
- Foundations of Maternal Newborn and Womens Health Nursing 7Th Edition Murray Test Bank Full Chapter PDFDocument41 pagesFoundations of Maternal Newborn and Womens Health Nursing 7Th Edition Murray Test Bank Full Chapter PDFgabrielthuym96j100% (13)
- Rekap Pasien ICU 2022 02-07Document43 pagesRekap Pasien ICU 2022 02-07anggiaNo ratings yet
- Glycated Hemoglobin: H. B. Chandalia and P. R. KrishnaswamyDocument11 pagesGlycated Hemoglobin: H. B. Chandalia and P. R. Krishnaswamydrafq2000No ratings yet
- Respiratory System - WikipediaDocument1 pageRespiratory System - WikipediaMatias Kristel AnnNo ratings yet
- Alcohol and Heart DiseaseDocument281 pagesAlcohol and Heart DiseaseDaniela Montalvo BarreraNo ratings yet
- What Is CPR?Document7 pagesWhat Is CPR?Harshal AachrekarNo ratings yet
- Sessions 13 Nur 1491Document8 pagesSessions 13 Nur 1491BegNo ratings yet
- Practice Paper Section05Document35 pagesPractice Paper Section05Aby PouloseNo ratings yet
- Diabetes MellitusDocument8 pagesDiabetes MellitusJaja RamosNo ratings yet
- High Ceiling Loop Diuretics Thiazides and Realted DiureticsDocument3 pagesHigh Ceiling Loop Diuretics Thiazides and Realted DiureticsDaphne GoreNo ratings yet
- Anterior Cerebral Artery StrokeDocument9 pagesAnterior Cerebral Artery StrokeAlin CiubotaruNo ratings yet
- Cerebrovascular DiseaseDocument54 pagesCerebrovascular Diseaselisaagustina100% (1)
- Lecture 1 ScalpDocument5 pagesLecture 1 Scalpnatheer ayedNo ratings yet
- Gleeson 2011Document9 pagesGleeson 2011Jerônimo CoelhoNo ratings yet
- Case Presentation On Coronary Artery Disease - 090908Document54 pagesCase Presentation On Coronary Artery Disease - 090908Parth Vasave100% (4)
- DEFIB PPT at PrakaraDocument52 pagesDEFIB PPT at Prakarakvl kandulaNo ratings yet
- TMX428 TMX58 Service Manual EnglishDocument159 pagesTMX428 TMX58 Service Manual Englishedgar corroNo ratings yet
- MR - Nagula Prashanth (Corpahcrya1711230377) Male 26 Years: This Document Holds The Written Radiology Report ForDocument3 pagesMR - Nagula Prashanth (Corpahcrya1711230377) Male 26 Years: This Document Holds The Written Radiology Report Forp13607091No ratings yet
- ACVIM Consensus Guidelines For The Diagnosis and Treatment of Myxomatous Mitral Valve Disease in Dogs.Document14 pagesACVIM Consensus Guidelines For The Diagnosis and Treatment of Myxomatous Mitral Valve Disease in Dogs.Evaldo MamedesNo ratings yet
- The Circulatory System ReviewerDocument4 pagesThe Circulatory System ReviewerKaten KyoukotsuNo ratings yet