Professional Documents
Culture Documents
Abortion Background: Classification
Abortion Background: Classification
Uploaded by
Cristyl Shine BariaoCopyright:
Available Formats
You might also like
- Chapter 21: Nursing Care of A Family Experiencing A Sudden Pregnancy ComplicationDocument9 pagesChapter 21: Nursing Care of A Family Experiencing A Sudden Pregnancy ComplicationAlyssaGrandeMontimor100% (1)
- BIOLOGY INVESTIGATORY PROJECT Zaid PDFDocument16 pagesBIOLOGY INVESTIGATORY PROJECT Zaid PDFMohammed Zaid82% (11)
- High Risk PregnancyDocument10 pagesHigh Risk PregnancyRoy Mujeres CabueñasNo ratings yet
- AbortionDocument121 pagesAbortionSindhu JojoNo ratings yet
- MootDocument21 pagesMootAnandhu Satheesh100% (1)
- ABORTIONDocument23 pagesABORTIONCristyl Shine BariaoNo ratings yet
- NCM 109 (PRELIMS) - Lesson 3Document17 pagesNCM 109 (PRELIMS) - Lesson 3nianNo ratings yet
- High Risk Ob Notes 1Document20 pagesHigh Risk Ob Notes 1pinpindalgoNo ratings yet
- A Woman Who Develops A Complication of PregnancyDocument24 pagesA Woman Who Develops A Complication of PregnancyLady Jane CaguladaNo ratings yet
- Types of AbortionDocument2 pagesTypes of AbortionMaako MonteverdeNo ratings yet
- A 3.1 Sudden Pregnancy Complications PDFDocument47 pagesA 3.1 Sudden Pregnancy Complications PDFCamille Joy BaliliNo ratings yet
- Abortion HandoutDocument3 pagesAbortion HandoutShena Mie Adis ValleceraNo ratings yet
- Notes On The Complications During The Labor and Delivery ProcessDocument7 pagesNotes On The Complications During The Labor and Delivery ProcessjyzzadNo ratings yet
- MCN NotesDocument20 pagesMCN NotesLiamLexus JavierNo ratings yet
- Cmca2 (Prelim) 2Document16 pagesCmca2 (Prelim) 2NOEL YRIGONNo ratings yet
- Clinical Manifestations Therapeutic Management: Lozano, Michael Anfernee BSN2A2-3Document3 pagesClinical Manifestations Therapeutic Management: Lozano, Michael Anfernee BSN2A2-3Hazel LorenzoNo ratings yet
- Early Pregnancy BleedingDocument23 pagesEarly Pregnancy Bleedingdafac7777No ratings yet
- High Risk PregnancyDocument104 pagesHigh Risk PregnancyNovelyn PuaNo ratings yet
- Lesson 3Document38 pagesLesson 3Kyla GambanNo ratings yet
- Maternal Child Nursing ModuleDocument7 pagesMaternal Child Nursing ModuleWizzardNo ratings yet
- High-Risks-Of-Pregnancies - JillDocument13 pagesHigh-Risks-Of-Pregnancies - JillMaureline DominarNo ratings yet
- Vaginal Bleeding in PregnancyDocument4 pagesVaginal Bleeding in PregnancyAra BaltarNo ratings yet
- AbortionDocument36 pagesAbortionAnjali Rahul AjmeriNo ratings yet
- COMPLETE DISCUSSION NCM 109 LEC-WEEK 3 CARE GiVEN TO A MOTHER WITH SUDDEN COMPLICATIONS OF PREGNANCY WITH Recorded DiscussionDocument79 pagesCOMPLETE DISCUSSION NCM 109 LEC-WEEK 3 CARE GiVEN TO A MOTHER WITH SUDDEN COMPLICATIONS OF PREGNANCY WITH Recorded DiscussionMa. Isabel A. EnriquezNo ratings yet
- Bleeding in Early PregnancyDocument28 pagesBleeding in Early Pregnancyinciy093No ratings yet
- High-Risk Labor & Delivery Client & Her FamilyDocument68 pagesHigh-Risk Labor & Delivery Client & Her FamilyJAMES ROD MARINDUQUENo ratings yet
- Maternal LEC - Week 3 - TransesDocument21 pagesMaternal LEC - Week 3 - TransesEcka- EckaNo ratings yet
- Maternal Reviewer NervanzDocument20 pagesMaternal Reviewer NervanzRovic GasmenNo ratings yet
- Vaginal Bleeding in Early PregnancyDocument8 pagesVaginal Bleeding in Early PregnancyBal Ri Mekoleu100% (1)
- NCM 109 Abnormal Ob High Risk PregnancyDocument13 pagesNCM 109 Abnormal Ob High Risk PregnancyMatth N. ErejerNo ratings yet
- Amplify The Learning (Ob) Week #2: Vidon, Aubrey Rose A. April 18, 2020 BSN 2Y2-2Document2 pagesAmplify The Learning (Ob) Week #2: Vidon, Aubrey Rose A. April 18, 2020 BSN 2Y2-2AriaNo ratings yet
- Spontaneous Abortion (Miscarriage) Definition:: SyndromeDocument9 pagesSpontaneous Abortion (Miscarriage) Definition:: SyndromeSridevi DevarajNo ratings yet
- Module 9 Student Activity SheetDocument6 pagesModule 9 Student Activity SheetJenny Agustin FabrosNo ratings yet
- Najax 123Document4 pagesNajax 123Najax Faarax MahamudNo ratings yet
- Pregnancy Complication: Department of Gynaecology and ObstetricsDocument59 pagesPregnancy Complication: Department of Gynaecology and ObstetricssanjivdasNo ratings yet
- Abnormal Uterine ActionDocument14 pagesAbnormal Uterine ActionSwara RamtekeNo ratings yet
- AbortionDocument62 pagesAbortionRaj KumarNo ratings yet
- Presentation 1Document53 pagesPresentation 1Nor Ubudiah SetiNo ratings yet
- Urdaneta City University College of Health Sciences Bachelor of Science in Nursing ProgramDocument4 pagesUrdaneta City University College of Health Sciences Bachelor of Science in Nursing ProgramMary Ruth CruzNo ratings yet
- ABORTIONDocument10 pagesABORTIONSivi Joseph100% (1)
- Abortion ..Document53 pagesAbortion ..Karan SinghNo ratings yet
- AbortionDocument28 pagesAbortionlordgoncarNo ratings yet
- Feb 19. CA 2 - 1681737641118Document9 pagesFeb 19. CA 2 - 1681737641118HANNAH BANGKILINGNo ratings yet
- Emmergency Obstretics 2Document22 pagesEmmergency Obstretics 2gracebally06No ratings yet
- Level 1 Nursing in LpuDocument8 pagesLevel 1 Nursing in LpuBritney TamuraNo ratings yet
- Abortion (BEST)Document40 pagesAbortion (BEST)lemesamamo2023No ratings yet
- AbortionDocument42 pagesAbortionKondapavuluru Jyothi50% (2)
- AbortionDocument35 pagesAbortionHoney May Rollan VicenteNo ratings yet
- Nle - High-Risk PregnancyDocument113 pagesNle - High-Risk Pregnancytachycardia01No ratings yet
- Those Related To The Pregnant State: AbortionDocument43 pagesThose Related To The Pregnant State: AbortionJohannah DaroNo ratings yet
- AbortionDocument19 pagesAbortionAhmed SabryNo ratings yet
- Premature Cervical DilationDocument22 pagesPremature Cervical DilationJanelle Lois EscolanoNo ratings yet
- Ectopic Preg Unit-2Document24 pagesEctopic Preg Unit-2moh1209No ratings yet
- NCM 102 OB Abnormal 2Document113 pagesNCM 102 OB Abnormal 2Maria Garcia Pimentel Vanguardia IINo ratings yet
- Abortion II ND Yr MSC NursingDocument121 pagesAbortion II ND Yr MSC Nursingesthereugenia100% (2)
- Show Note - MCH High RiskDocument145 pagesShow Note - MCH High RiskHoneylouAzOpondaNo ratings yet
- Normal Labor 2013 Nursing GabstDocument125 pagesNormal Labor 2013 Nursing GabstYibelu BazezewNo ratings yet
- Week 3 Care of The Woman Experiencing A Sudden Pregnancy ComplicationsDocument68 pagesWeek 3 Care of The Woman Experiencing A Sudden Pregnancy ComplicationsWendell Mark B FernandezNo ratings yet
- Bleeding in Early PregnancyDocument20 pagesBleeding in Early Pregnancynanapet80No ratings yet
- Abortion: DEFINITION-Abortion Is The Separation Partial orDocument77 pagesAbortion: DEFINITION-Abortion Is The Separation Partial orPadmaNo ratings yet
- It's Not Just a Heavy Period; The Miscarriage HandbookFrom EverandIt's Not Just a Heavy Period; The Miscarriage HandbookRating: 2 out of 5 stars2/5 (1)
- Getting Pregnant Faster: Step-By-Step Guide To Achieving PregnancyFrom EverandGetting Pregnant Faster: Step-By-Step Guide To Achieving PregnancyNo ratings yet
- I&IDocument7 pagesI&ICristyl Shine BariaoNo ratings yet
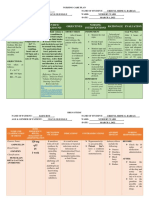
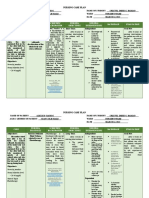
- Cues Nursing Diagnosis Scientific Background Nursing Objectives Nursing Interventions Rationale EvaluationDocument1 pageCues Nursing Diagnosis Scientific Background Nursing Objectives Nursing Interventions Rationale EvaluationCristyl Shine BariaoNo ratings yet
- Questionniare (REVISED)Document2 pagesQuestionniare (REVISED)Cristyl Shine BariaoNo ratings yet
- 2 Drug Study (Mvh-ns3 Bariao, Cristyl Shine G.)Document2 pages2 Drug Study (Mvh-ns3 Bariao, Cristyl Shine G.)Cristyl Shine BariaoNo ratings yet
- ABORTIONDocument23 pagesABORTIONCristyl Shine BariaoNo ratings yet
- BROCHURE (CHN-Different Family Planning)Document2 pagesBROCHURE (CHN-Different Family Planning)Cristyl Shine BariaoNo ratings yet
- NCP and Drug Study (Isph-Gs Nursery)Document4 pagesNCP and Drug Study (Isph-Gs Nursery)Cristyl Shine BariaoNo ratings yet
- Assessment (Self Defense)Document3 pagesAssessment (Self Defense)Cristyl Shine BariaoNo ratings yet
- 4 Drug Study (Opd)Document4 pages4 Drug Study (Opd)Cristyl Shine BariaoNo ratings yet
- 2 NCP & 3 Drug StudyDocument6 pages2 NCP & 3 Drug StudyCristyl Shine BariaoNo ratings yet
- 2 NCPDocument3 pages2 NCPCristyl Shine BariaoNo ratings yet
- Module 1 Lesson 1-4Document4 pagesModule 1 Lesson 1-4Kristine JeanNo ratings yet
- Pr22 25 LetterDocument2 pagesPr22 25 LetterWBIR Channel 10No ratings yet
- MarchDocument122 pagesMarchZozo Mostafa100% (3)
- Strategies To Improve Maternal Health in The Next Decade: Annette BongiovanniDocument24 pagesStrategies To Improve Maternal Health in The Next Decade: Annette BongiovanniSyeda Fizzah Z. GardeziNo ratings yet
- PCW Letter To DOJ-CCC Re Abortion 2014Document2 pagesPCW Letter To DOJ-CCC Re Abortion 2014HumanRights_PhNo ratings yet
- The Responsible Parenthood and Reproductive Health Act of 2012Document1 pageThe Responsible Parenthood and Reproductive Health Act of 2012Divina Gracia Fabicon AranaNo ratings yet
- Where Have All The Criminals GoneDocument2 pagesWhere Have All The Criminals GoneRaul Augustus D. FACONNo ratings yet
- Induced AbortionDocument17 pagesInduced AbortionMwenemutapa FernandoNo ratings yet
- Planned Parenthood Mar Monte and StemExpress InvoiceDocument4 pagesPlanned Parenthood Mar Monte and StemExpress InvoiceMary Margaret Olohan100% (1)
- National SM Protocol Final Draft - 21-9-16 (Repaired)Document172 pagesNational SM Protocol Final Draft - 21-9-16 (Repaired)Theophilus BaidooNo ratings yet
- Val02 Act 3 Chapter 3 - SalongaDocument3 pagesVal02 Act 3 Chapter 3 - SalongaMARY JOY SALONGANo ratings yet
- Ethics of Abortion PDFDocument2 pagesEthics of Abortion PDFLisaNo ratings yet
- Ethical Issues at The Beginning of LifeDocument37 pagesEthical Issues at The Beginning of LifeGeorgiana ButurăNo ratings yet
- By: Christine G. Dela CruzDocument34 pagesBy: Christine G. Dela CruzMuhammad AbeeshNo ratings yet
- New Microsoft Word DocumentDocument14 pagesNew Microsoft Word DocumentKaizer Aldrych Taroma EspelitaNo ratings yet
- Soma Marik - The Love of Worker Bees in Context - Revised - KollontaiDocument23 pagesSoma Marik - The Love of Worker Bees in Context - Revised - KollontaiMaíra Mee Daher Dutra da SilvaNo ratings yet
- Abortion in The PhilippinesDocument2 pagesAbortion in The PhilippinesRosario Antoniete R. Cabilin100% (1)
- Abortion-21 10 2018Document52 pagesAbortion-21 10 2018Mahmoud HalalshehNo ratings yet
- Resource Unit SampleDocument16 pagesResource Unit SampleShania CabucosNo ratings yet
- Rumus DemografiDocument23 pagesRumus Demografidannyindrajaya_bpNo ratings yet
- Risky Sexual Behavior and The Prevalecy of Teenage Pregenancy in Luzira Parish, Kampala DistrictDocument64 pagesRisky Sexual Behavior and The Prevalecy of Teenage Pregenancy in Luzira Parish, Kampala DistrictBold Ronald OjanNo ratings yet
- Does Morality Depend On ReligionDocument14 pagesDoes Morality Depend On ReligionOcirej OrtsacNo ratings yet
- Charlie Baum Final WgsDocument6 pagesCharlie Baum Final Wgsapi-544195874No ratings yet
- Implementing Rules and Regulations of 10354Document35 pagesImplementing Rules and Regulations of 10354ChewieNo ratings yet
- MTP Act 1971Document16 pagesMTP Act 1971akash tiwariNo ratings yet
- Post Abortion CareDocument35 pagesPost Abortion CareNatukunda DianahNo ratings yet
- Christian Pro-Life Resources For The PhilippinesDocument4 pagesChristian Pro-Life Resources For The PhilippinesCBCP for LifeNo ratings yet
- "Teenage Pregnancy, A Gloom in Our Society" by Jyra Libertine SabueloDocument17 pages"Teenage Pregnancy, A Gloom in Our Society" by Jyra Libertine SabueloJhessa Samantha DulayNo ratings yet
Abortion Background: Classification
Abortion Background: Classification
Uploaded by
Cristyl Shine BariaoOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Abortion Background: Classification
Abortion Background: Classification
Uploaded by
Cristyl Shine BariaoCopyright:
Available Formats
ABORTION
BACKGROUND
Abortion is a medical term for termination of a pregnancy before a fetus is viable
(means able to survive outside the uterus) and weight less than 500 grams (0.5 kg). A viable
fetus is when it reach beyond 20 weeks to 24 weeks of gestation and weight at least 500
grams or more than 500 grams. A fetus born before this age is considered miscarriage, or
premature, or immature birth (Cootauco & Althaus, 2007).
CLASSIFICATION
1. SPONTANEOUS ABORTION
- It is also called miscarriage, it occurs naturally without any medical or
mechanical, or surgical intervention. It arises in 15% - 30% of all
pregnancies that caused by natural causes. It is classified into two:
Early Miscarriage – occurs before 16 weeks of pregnancy.
Late Miscarriage – occurs between 16 to 24 weeks of pregnancy.
5 TYPES OF SPONTANEOUS ABORTION:
a. Threatened
- defined as a vaginal bleeding before 20 weeks of gestation but the
cervix is closed and the products of conception are still intact.
- A situation in which a viable pregnancy is in jeopardy and the
prognosis is uncertain because it may or may not result in an abortion.
Signs & Symptoms:
scant bleeding, usually bright red (1st sign)
mild uterine cramping felt at the back and lower
abdomen
(-) cervical dilatation-closed cervix
no passage of tissue
soft, no tender, enlarged uterus
Nursing Management:
Instruct the patient to avoid strenuous activity or limit to
no strenuous activity because bleeding usually stops 24
to 48 hours after the woman reduces her activity.
For 1-2 days, Initiate complete bed rest without
bathroom privileges.
Coitus should be avoided for up to 2 weeks after the
bleeding has stopped to avoid further bleeding and
infection (semen contains prostaglandins).
Keep all the perineal pads and blood clots.
Provide psychological support
There may be feelings of shock, anger and
frustration, guilt, and grief.
Allow the woman and her family to express their
emotions.
BARIAO, CRISTYL SHINE G. – BSN 2D
To reduce feelings of guilt, inform the woman
about the causes of miscarriage.
Explain that this happened on its own accord
and that there is nothing to be held responsible
for.
Medical Management:
Progestational agents to relax uterine vasculature
b. Inevitable/Imminent
- Threatened abortion becomes imminent when cervical dilatation and
uterine contractions occur, it means that the pregnancy termination is
already in progress and cannot be stopped or loss of pregnancy can no
longer be prevented.
Signs & Symptoms:
vaginal bleeding
(+) uterine contractions
(+) cervical dilatation and rupture of membranes
(-) FHT
2 Kinds of Inevitable/Imminent
i. Complete
- The complete expulsion of uterine contents occurs when the
pre-born child and the placenta have been expelled from the
uterus; the entire products of conception (fetus, membranes,
and placenta) are expelled spontaneously without any
assistance (medical, surgical or chemical means).
Signs & Symptoms:
Self-limiting vaginal bleeding – slows down and
stops after a few days.
Cervical dilatation and cramping.
The products of conception are
passed/completely expelled.
ii. Incomplete
- The products of conception are not completely expelled.
Some fragments are retained in the uterus usually the fetus is
expelled but the membrane or placenta is retained in the uterus
that can cause infection.
Signs & Symptoms:
(+) uterine contractions
(+) cervical dilatation
Profuse vaginal bleeding because of retained
product that interfere with uterine contraction.
Incomplete products of conception.
Nursing Management:
BARIAO, CRISTYL SHINE G. – BSN 2D
Psychological support
Medical/Surgical Management:
Administering oxytocin to encourage expulsion
of retained fragments and blood loss.
Performing D and C (Dilatation and Curettage)
– most commonly done for incomplete abortion
to remove remaining tissue in the uterus.
c. Early Pregnancy Failure (Missed)
- A dead embryo or fetus is not expelled from the uterus for 4 weeks or
more; a fetus dies in utero but is not expelled; this is usually
discovered during a prenatal exam, when the fundal height is measured
and no increase in size can be demonstrated, or when previously heard
fetal heart sounds are no longer audible.
Signs &Symptoms:
(-) fetal movement
(-) FHT
regression of uterus and mammary glands with or
without bleeding
coagulation defects
(-) HCG titer
Nursing Management:
Psychological support
Medical/Surgical Management:
Sonogram/Ultrasound
Labor induction and performing D and E (Dilatation
and Evacuation) to make sure that all the products of
conception would be removed from the uterus.
If the pregnancy is over 14 weeks, labor can be induced
with prostaglandin or misoprositol (Cytotec) to dilate
the cervix, followed by oxytocin or mifepristone.
d. Septic/Infected
- Infection can occur after a spontaneous miscarriage, but it is more
common in women who attempted to self-abort or were illegally
aborted using a nonsterile instrument such as a knitting needle.
Because the uterus is a warm, moist, dark cavity, infectious organisms
grow quickly once introduced, especially if products of conception
such as necrotic membranes are still present.
- An abortion that has been complicated by infection during the
procedure. If not treated, it can result in Toxic Shock Syndrome,
Septicemia, kidney failure, or fetal death.
Signs & Symptoms:
Vaginal discharge has a foul odor.
Fever of 38°C or higher
pelvic cause pain (cramp abdominal pain)
When the uterus is palpated, it feels tender.
BARIAO, CRISTYL SHINE G. – BSN 2D
Nursing Management:
Intravenous infusion to restore fluid volume and
provide a route for high-dose antibiotics
Hourly insertion of an indwelling Foley catheter to
monitor urine output to assess renal function
Medical/Surgical Management:
Subcutaneous administration of tetanus toxoid or
intramuscular administration of tetanus immunoglobulin
for prevention of tetanus.
Antibiotics Broad-spectrum antibiotic therapy, the
combination of PenG, gentamicin, and clindamycin.
D and C to remove all necrotic tissue in the uterus.
e. Recurrent Pregnancy Loss (Habitual)
- 3 abortions in a row before the 20th week at the same gestational age
were labeled "habitual aborters"; may be caused by long-term factors
such as infection, maternal hormonal problems, defective spermatozoa,
and so on.
- occurs in approximately 1% of women who wish to become pregnant.
Causes:
Spermatozoa or ova that are defective
Endocrine factors such as low levels of protein-bound
iodine and poor thyroid function
Uterine deviations such as septate or bicornuate uterus,
as well as an incompetent cervix
Chorioamnionitis or uterine infection
Autoimmune conditions such as lupus anticoagulant and
antiphospholipid antibodies.
CAUSES/RISK FACTORS
Fetal Factors:
Most frequent cause is abnormal fetus due to either teratogenic factor or
chromosomal aberration. About 50% - 80% of fetuses aborted early have a
structural abnormalities.
Poor Implantation/ Abnormalities in implantation, 50% of zygotes are unlikely
to be implanted. Inadequate implantation results in poor placental circulation
and insufficient fetal nutrition. Poor implantation can be caused by insufficient
endometrial formation or an inappropriate implantation site.
Placental Factors:
Premature separation of placenta
Abnormal placental implantation
Immunologic:
An immune response that result of rejection of embryo or Rh incompatibility.
Malnutrition
Low progesterone level:
BARIAO, CRISTYL SHINE G. – BSN 2D
It is when corpus luteum which helps in maintaining pregnancy fails to
produce enough progesterone to maintain the decidua basalis (part of the
endometrium in which the blastocyst is attached on.)
Infection or other diseases/trauma:
Rubella, syphilis, poliomyelitis, CMV (Cytomegalovirus), toxoplasmosis, and
TORCH Syndrome are infections that easily cross the placenta, potentially
resulting in fetal death.
Miscarriage is also more common if you have a UTI.
Infection causes the fetus to stop growing and the placenta to produce less
estrogen and progesterone that can lead to endometrial sloughing.
Prostaglandins are released during the sloughing process, which causes uterine
contraction and cervical dilatation, as well as the expulsion of pregnancy
products.
Abnormality in reproductive organs – incompetent cervix
Emotional shock:
The release of maternal epinephrine in response to severe stress or fright may
be sufficient to cause extensive vasoconstriction, leading to necrosis of the
decidua basalis; poor fetal blood supply—fetal death.
Drug intake
Paternal factors:
The genetic factor carried by sperm may be deficient in a crucial factor
required for normal embryonic development.
2. ELECTIVE/INDUCED ABORTION
- Pregnancy termination by artificial (surgical, mechanical, or medical)
methods; procedure performed to intentionally end (induce) the pregnancy
before the age of viability.
2 TYPES OF ELECTIVE/INDUCED ABORTION:
a. Therapeutic/Medical
- refers to the termination of a pregnancy as considered necessary by a
physician. It is carried out in hospitals/clinics for medical or legal
reasons. Abortion-on-demand refers to a pregnant woman's right to
have an abortion performed at her request (if the woman does not want
to continue her pregnancy).
b. Criminal
- Intentional termination of pregnancy under any condition prohibited
by law; may result in infection and uterine damage if performed by an
untrained person. A pregnancy termination performed outside of
appropriate medical facilities.
PURPOSES OF ELECTIVE ABORTION:
When woman's life is in endangers, such as pregnancy in a
dangerous situation a woman suffering from chronic heart
disease.
This entails a fetus discovered via amniocentesis having a
chromosomal error.
BARIAO, CRISTYL SHINE G. – BSN 2D
Undesirable because it is the result of rape or incest.
A woman who chooses not to have a child at this time in her
life due to factors such as being too young, not wanting to be a
single parent, not wanting any more children, financial
difficulties, or failed contraception.
DIAGNOSTIC TEST
PREGNANCY TEST
If vaginal bleeding occurs, this is done first to confirm the pregnancy. If the
test results are negative, the woman will be subjected to additional diagnostic tests to
confirm the nature and cause of the vaginal bleeding. If it is positive, abortion will be
considered, and it will be classified based on the signs and symptoms.
ULTRASOUND
The safest and most reliable pregnancy test. It can confirm whether or not the
pregnancy is positive, as well as whether or not the products of conception are still
intact.
MEDICAL AND SURGICAL TREATMENTS
MEDICAL TREATMENTS
PROGESTERONE ANTAGONIST/MORNING-AFTER PILL
Mifepristone can be used to medically induce an abortion during the
first 7 weeks of pregnancy (up to 49 days after conception).
Progesterone is a hormone that maintains the basal decidua, which
nourishes the next developing embryo. Two days later, the woman
returned to the nurse to take misoprostol.
PROSTAGLANDIN INFUSION
Misoprostol or Cytotec induce labor causing uterine contractions and
cervical dilation leading to the expulsion of conceptus. Approximately
12 days after taking misoprostol, the woman returns to her caregiver to
see if the abortion was successful.
SALINE INDUCTION
If the pregnancy is 16 to 24 weeks they give 200 ml of hypertonic
saline infused into amniotic fluid. The fetus dies in about an hour.
Uterine contractions occur within 12-36 hours. Then, oxytocin is given
to help labor and is now rarely used due to life-threatening
complications such as hypernatremia.
SURGICAL TREATMENTS
MENTSRUAL EXTRACTION (ME)
They create a vacuum that sucks the contents of the uterus from the
cervix. Procedurally, ME is a type of vacuum aspiration and is a
common procedure for abortion in countries where abortion is legal.
However, it can be used both for early abortions and as a way to go
through the entire menstrual period at once.
VACUUM EXTRACTION
It performed 5-7 weeks after LMP. The cervix is dilated, a suction
catheter is inserted, and the suction catheter is used to remove the
contents of the uterus. The procedure is rapid, about 5 minutes, with
BARIAO, CRISTYL SHINE G. – BSN 2D
minimal blood loss then after administration of oxytocin the mother is
discharged 4 hours later without complications.
VACUUM ASPIRATION
This procedure is a common method used during early pregnancy. It
uses a thin tube (cannula) with tubes attached to the bottle and pump to
create a gentle vacuum. Insert the cannula into the uterus, switch on the
pump and carefully remove the tissue from the uterus.
DILATATION AND CURATTAGE
It is done if gestational age is less than 13 weeks. The cervix is dilated
and the product is gently scraped off on the base of uterus and can be
done using a traditional dilator or a laminaria tent dilator — cervical
pad made of compressed seaweed that swells and dilates the cervix.
DILATATION AND EVACUATION
It is done between 12 – 16 weeks. The cervix is dilated and product
removed by the use of vacuum aspiration and also surgical tools too
like forceps.
HYSTEROTOMY
It is done when the gestational age exceeds to 16-18 weeks. It is the
removal of fetus similar to a caesarian section when prostaglandin and
other management failed or if sterilization/ tubal ligation is desired.
POSSIBLE COMPLICATIONS OF ABORTION:
o Hemorrhage
o Infection
o Isoimmunization
o Cervical Injury
o Infertility
o Depression
NURSING MANAGEMENT/INTERVENTIONS
Encourage family members to be there for the patient before, during, and after the
abortion.
Ensure that the patient is physically and psychologically prepared for the procedure
before performing an induced therapeutic abortion.
Keep an eye on the patient for signs of complications and initiate appropriate
treatment:
Monitor vital signs
Check for vaginal bleeding.
Place the woman flat on her side on her left lateral side of the bed to maintain
optimal placental and renal function and to avoid supine hypotension/supine
vena cava syndrome.
Begin IV fluid administration, such as lactated Ringer's, to replace
intravascular fluid volume.
Administer oxygen as needed-at 2-4 LPM, provide adequate maternal
oxygenation despite decreased circulating blood volume.
Take antibiotics as directed.
Use an external monitor to track uterine contractions and FHR to see if labor is
present.
BARIAO, CRISTYL SHINE G. – BSN 2D
Weigh perineal pads and save any clots or tissues passed in order to determine
maternal blood loss.
Monitor Intake and Output to assess renal function.
Nutritional Diet
Provide emotional support
NURSING DIAGNOSIS
Risk for fluid volume deficit r/t maternal bleeding
Anticipatory grieving r/t loss of pregnancy, cause of abortion, future childbearing
Risk for infection r/t dilated cervix and open uterine vessels
Acute pain r/t uterine cramping and possible procedures
Knowledge deficit r/t signs and symptoms of possible complications
HEALTH TEACHINGS
Health Education about Family Planning Methods
Sexual Health Education Programs to Young Adults.
Antenatal Counselling
REFERENCES:
Sebastian, S, (2015). “Abortion.ppt for 2nd msc.” Retrieved from
https://www.slideshare.net/sindhujojo/abortionppt-for-2nd-msc
Belleza, M, (2017). “Abortion.” Retrieved from https://nurseslabs.com/abortion/
Pillitteri, Adele, (2019). MATERNAL AND CHILD HEALTH NURSING, 8TH ED.
WOLTERS KLUWER, LIPPINCOTT WILLIAMS & WILKINS, SINGAPORE.
Pillitteri, Adele, (2010). MATERNAL AND CHILD HEALTH NURSING, 6TH ED.
WOLTERS KLUWER, LIPPINCOTT WILLIAMS & WILKINS, SINGAPORE.
BARIAO, CRISTYL SHINE G. – BSN 2D
You might also like
- Chapter 21: Nursing Care of A Family Experiencing A Sudden Pregnancy ComplicationDocument9 pagesChapter 21: Nursing Care of A Family Experiencing A Sudden Pregnancy ComplicationAlyssaGrandeMontimor100% (1)
- BIOLOGY INVESTIGATORY PROJECT Zaid PDFDocument16 pagesBIOLOGY INVESTIGATORY PROJECT Zaid PDFMohammed Zaid82% (11)
- High Risk PregnancyDocument10 pagesHigh Risk PregnancyRoy Mujeres CabueñasNo ratings yet
- AbortionDocument121 pagesAbortionSindhu JojoNo ratings yet
- MootDocument21 pagesMootAnandhu Satheesh100% (1)
- ABORTIONDocument23 pagesABORTIONCristyl Shine BariaoNo ratings yet
- NCM 109 (PRELIMS) - Lesson 3Document17 pagesNCM 109 (PRELIMS) - Lesson 3nianNo ratings yet
- High Risk Ob Notes 1Document20 pagesHigh Risk Ob Notes 1pinpindalgoNo ratings yet
- A Woman Who Develops A Complication of PregnancyDocument24 pagesA Woman Who Develops A Complication of PregnancyLady Jane CaguladaNo ratings yet
- Types of AbortionDocument2 pagesTypes of AbortionMaako MonteverdeNo ratings yet
- A 3.1 Sudden Pregnancy Complications PDFDocument47 pagesA 3.1 Sudden Pregnancy Complications PDFCamille Joy BaliliNo ratings yet
- Abortion HandoutDocument3 pagesAbortion HandoutShena Mie Adis ValleceraNo ratings yet
- Notes On The Complications During The Labor and Delivery ProcessDocument7 pagesNotes On The Complications During The Labor and Delivery ProcessjyzzadNo ratings yet
- MCN NotesDocument20 pagesMCN NotesLiamLexus JavierNo ratings yet
- Cmca2 (Prelim) 2Document16 pagesCmca2 (Prelim) 2NOEL YRIGONNo ratings yet
- Clinical Manifestations Therapeutic Management: Lozano, Michael Anfernee BSN2A2-3Document3 pagesClinical Manifestations Therapeutic Management: Lozano, Michael Anfernee BSN2A2-3Hazel LorenzoNo ratings yet
- Early Pregnancy BleedingDocument23 pagesEarly Pregnancy Bleedingdafac7777No ratings yet
- High Risk PregnancyDocument104 pagesHigh Risk PregnancyNovelyn PuaNo ratings yet
- Lesson 3Document38 pagesLesson 3Kyla GambanNo ratings yet
- Maternal Child Nursing ModuleDocument7 pagesMaternal Child Nursing ModuleWizzardNo ratings yet
- High-Risks-Of-Pregnancies - JillDocument13 pagesHigh-Risks-Of-Pregnancies - JillMaureline DominarNo ratings yet
- Vaginal Bleeding in PregnancyDocument4 pagesVaginal Bleeding in PregnancyAra BaltarNo ratings yet
- AbortionDocument36 pagesAbortionAnjali Rahul AjmeriNo ratings yet
- COMPLETE DISCUSSION NCM 109 LEC-WEEK 3 CARE GiVEN TO A MOTHER WITH SUDDEN COMPLICATIONS OF PREGNANCY WITH Recorded DiscussionDocument79 pagesCOMPLETE DISCUSSION NCM 109 LEC-WEEK 3 CARE GiVEN TO A MOTHER WITH SUDDEN COMPLICATIONS OF PREGNANCY WITH Recorded DiscussionMa. Isabel A. EnriquezNo ratings yet
- Bleeding in Early PregnancyDocument28 pagesBleeding in Early Pregnancyinciy093No ratings yet
- High-Risk Labor & Delivery Client & Her FamilyDocument68 pagesHigh-Risk Labor & Delivery Client & Her FamilyJAMES ROD MARINDUQUENo ratings yet
- Maternal LEC - Week 3 - TransesDocument21 pagesMaternal LEC - Week 3 - TransesEcka- EckaNo ratings yet
- Maternal Reviewer NervanzDocument20 pagesMaternal Reviewer NervanzRovic GasmenNo ratings yet
- Vaginal Bleeding in Early PregnancyDocument8 pagesVaginal Bleeding in Early PregnancyBal Ri Mekoleu100% (1)
- NCM 109 Abnormal Ob High Risk PregnancyDocument13 pagesNCM 109 Abnormal Ob High Risk PregnancyMatth N. ErejerNo ratings yet
- Amplify The Learning (Ob) Week #2: Vidon, Aubrey Rose A. April 18, 2020 BSN 2Y2-2Document2 pagesAmplify The Learning (Ob) Week #2: Vidon, Aubrey Rose A. April 18, 2020 BSN 2Y2-2AriaNo ratings yet
- Spontaneous Abortion (Miscarriage) Definition:: SyndromeDocument9 pagesSpontaneous Abortion (Miscarriage) Definition:: SyndromeSridevi DevarajNo ratings yet
- Module 9 Student Activity SheetDocument6 pagesModule 9 Student Activity SheetJenny Agustin FabrosNo ratings yet
- Najax 123Document4 pagesNajax 123Najax Faarax MahamudNo ratings yet
- Pregnancy Complication: Department of Gynaecology and ObstetricsDocument59 pagesPregnancy Complication: Department of Gynaecology and ObstetricssanjivdasNo ratings yet
- Abnormal Uterine ActionDocument14 pagesAbnormal Uterine ActionSwara RamtekeNo ratings yet
- AbortionDocument62 pagesAbortionRaj KumarNo ratings yet
- Presentation 1Document53 pagesPresentation 1Nor Ubudiah SetiNo ratings yet
- Urdaneta City University College of Health Sciences Bachelor of Science in Nursing ProgramDocument4 pagesUrdaneta City University College of Health Sciences Bachelor of Science in Nursing ProgramMary Ruth CruzNo ratings yet
- ABORTIONDocument10 pagesABORTIONSivi Joseph100% (1)
- Abortion ..Document53 pagesAbortion ..Karan SinghNo ratings yet
- AbortionDocument28 pagesAbortionlordgoncarNo ratings yet
- Feb 19. CA 2 - 1681737641118Document9 pagesFeb 19. CA 2 - 1681737641118HANNAH BANGKILINGNo ratings yet
- Emmergency Obstretics 2Document22 pagesEmmergency Obstretics 2gracebally06No ratings yet
- Level 1 Nursing in LpuDocument8 pagesLevel 1 Nursing in LpuBritney TamuraNo ratings yet
- Abortion (BEST)Document40 pagesAbortion (BEST)lemesamamo2023No ratings yet
- AbortionDocument42 pagesAbortionKondapavuluru Jyothi50% (2)
- AbortionDocument35 pagesAbortionHoney May Rollan VicenteNo ratings yet
- Nle - High-Risk PregnancyDocument113 pagesNle - High-Risk Pregnancytachycardia01No ratings yet
- Those Related To The Pregnant State: AbortionDocument43 pagesThose Related To The Pregnant State: AbortionJohannah DaroNo ratings yet
- AbortionDocument19 pagesAbortionAhmed SabryNo ratings yet
- Premature Cervical DilationDocument22 pagesPremature Cervical DilationJanelle Lois EscolanoNo ratings yet
- Ectopic Preg Unit-2Document24 pagesEctopic Preg Unit-2moh1209No ratings yet
- NCM 102 OB Abnormal 2Document113 pagesNCM 102 OB Abnormal 2Maria Garcia Pimentel Vanguardia IINo ratings yet
- Abortion II ND Yr MSC NursingDocument121 pagesAbortion II ND Yr MSC Nursingesthereugenia100% (2)
- Show Note - MCH High RiskDocument145 pagesShow Note - MCH High RiskHoneylouAzOpondaNo ratings yet
- Normal Labor 2013 Nursing GabstDocument125 pagesNormal Labor 2013 Nursing GabstYibelu BazezewNo ratings yet
- Week 3 Care of The Woman Experiencing A Sudden Pregnancy ComplicationsDocument68 pagesWeek 3 Care of The Woman Experiencing A Sudden Pregnancy ComplicationsWendell Mark B FernandezNo ratings yet
- Bleeding in Early PregnancyDocument20 pagesBleeding in Early Pregnancynanapet80No ratings yet
- Abortion: DEFINITION-Abortion Is The Separation Partial orDocument77 pagesAbortion: DEFINITION-Abortion Is The Separation Partial orPadmaNo ratings yet
- It's Not Just a Heavy Period; The Miscarriage HandbookFrom EverandIt's Not Just a Heavy Period; The Miscarriage HandbookRating: 2 out of 5 stars2/5 (1)
- Getting Pregnant Faster: Step-By-Step Guide To Achieving PregnancyFrom EverandGetting Pregnant Faster: Step-By-Step Guide To Achieving PregnancyNo ratings yet
- I&IDocument7 pagesI&ICristyl Shine BariaoNo ratings yet
- Cues Nursing Diagnosis Scientific Background Nursing Objectives Nursing Interventions Rationale EvaluationDocument1 pageCues Nursing Diagnosis Scientific Background Nursing Objectives Nursing Interventions Rationale EvaluationCristyl Shine BariaoNo ratings yet
- Questionniare (REVISED)Document2 pagesQuestionniare (REVISED)Cristyl Shine BariaoNo ratings yet
- 2 Drug Study (Mvh-ns3 Bariao, Cristyl Shine G.)Document2 pages2 Drug Study (Mvh-ns3 Bariao, Cristyl Shine G.)Cristyl Shine BariaoNo ratings yet
- ABORTIONDocument23 pagesABORTIONCristyl Shine BariaoNo ratings yet
- BROCHURE (CHN-Different Family Planning)Document2 pagesBROCHURE (CHN-Different Family Planning)Cristyl Shine BariaoNo ratings yet
- NCP and Drug Study (Isph-Gs Nursery)Document4 pagesNCP and Drug Study (Isph-Gs Nursery)Cristyl Shine BariaoNo ratings yet
- Assessment (Self Defense)Document3 pagesAssessment (Self Defense)Cristyl Shine BariaoNo ratings yet
- 4 Drug Study (Opd)Document4 pages4 Drug Study (Opd)Cristyl Shine BariaoNo ratings yet
- 2 NCP & 3 Drug StudyDocument6 pages2 NCP & 3 Drug StudyCristyl Shine BariaoNo ratings yet
- 2 NCPDocument3 pages2 NCPCristyl Shine BariaoNo ratings yet
- Module 1 Lesson 1-4Document4 pagesModule 1 Lesson 1-4Kristine JeanNo ratings yet
- Pr22 25 LetterDocument2 pagesPr22 25 LetterWBIR Channel 10No ratings yet
- MarchDocument122 pagesMarchZozo Mostafa100% (3)
- Strategies To Improve Maternal Health in The Next Decade: Annette BongiovanniDocument24 pagesStrategies To Improve Maternal Health in The Next Decade: Annette BongiovanniSyeda Fizzah Z. GardeziNo ratings yet
- PCW Letter To DOJ-CCC Re Abortion 2014Document2 pagesPCW Letter To DOJ-CCC Re Abortion 2014HumanRights_PhNo ratings yet
- The Responsible Parenthood and Reproductive Health Act of 2012Document1 pageThe Responsible Parenthood and Reproductive Health Act of 2012Divina Gracia Fabicon AranaNo ratings yet
- Where Have All The Criminals GoneDocument2 pagesWhere Have All The Criminals GoneRaul Augustus D. FACONNo ratings yet
- Induced AbortionDocument17 pagesInduced AbortionMwenemutapa FernandoNo ratings yet
- Planned Parenthood Mar Monte and StemExpress InvoiceDocument4 pagesPlanned Parenthood Mar Monte and StemExpress InvoiceMary Margaret Olohan100% (1)
- National SM Protocol Final Draft - 21-9-16 (Repaired)Document172 pagesNational SM Protocol Final Draft - 21-9-16 (Repaired)Theophilus BaidooNo ratings yet
- Val02 Act 3 Chapter 3 - SalongaDocument3 pagesVal02 Act 3 Chapter 3 - SalongaMARY JOY SALONGANo ratings yet
- Ethics of Abortion PDFDocument2 pagesEthics of Abortion PDFLisaNo ratings yet
- Ethical Issues at The Beginning of LifeDocument37 pagesEthical Issues at The Beginning of LifeGeorgiana ButurăNo ratings yet
- By: Christine G. Dela CruzDocument34 pagesBy: Christine G. Dela CruzMuhammad AbeeshNo ratings yet
- New Microsoft Word DocumentDocument14 pagesNew Microsoft Word DocumentKaizer Aldrych Taroma EspelitaNo ratings yet
- Soma Marik - The Love of Worker Bees in Context - Revised - KollontaiDocument23 pagesSoma Marik - The Love of Worker Bees in Context - Revised - KollontaiMaíra Mee Daher Dutra da SilvaNo ratings yet
- Abortion in The PhilippinesDocument2 pagesAbortion in The PhilippinesRosario Antoniete R. Cabilin100% (1)
- Abortion-21 10 2018Document52 pagesAbortion-21 10 2018Mahmoud HalalshehNo ratings yet
- Resource Unit SampleDocument16 pagesResource Unit SampleShania CabucosNo ratings yet
- Rumus DemografiDocument23 pagesRumus Demografidannyindrajaya_bpNo ratings yet
- Risky Sexual Behavior and The Prevalecy of Teenage Pregenancy in Luzira Parish, Kampala DistrictDocument64 pagesRisky Sexual Behavior and The Prevalecy of Teenage Pregenancy in Luzira Parish, Kampala DistrictBold Ronald OjanNo ratings yet
- Does Morality Depend On ReligionDocument14 pagesDoes Morality Depend On ReligionOcirej OrtsacNo ratings yet
- Charlie Baum Final WgsDocument6 pagesCharlie Baum Final Wgsapi-544195874No ratings yet
- Implementing Rules and Regulations of 10354Document35 pagesImplementing Rules and Regulations of 10354ChewieNo ratings yet
- MTP Act 1971Document16 pagesMTP Act 1971akash tiwariNo ratings yet
- Post Abortion CareDocument35 pagesPost Abortion CareNatukunda DianahNo ratings yet
- Christian Pro-Life Resources For The PhilippinesDocument4 pagesChristian Pro-Life Resources For The PhilippinesCBCP for LifeNo ratings yet
- "Teenage Pregnancy, A Gloom in Our Society" by Jyra Libertine SabueloDocument17 pages"Teenage Pregnancy, A Gloom in Our Society" by Jyra Libertine SabueloJhessa Samantha DulayNo ratings yet