Professional Documents
Culture Documents
Wound Healing Fitzpatrick's Dermatology 9th Edition, 2-Volume Set - 220212 - 121805
Wound Healing Fitzpatrick's Dermatology 9th Edition, 2-Volume Set - 220212 - 121805
Uploaded by
Brigitta ClaraCopyright:
Available Formats
You might also like
- Gastrointestinal Physiology LANGEDocument281 pagesGastrointestinal Physiology LANGEUlquiorra Schiffer100% (4)
- Treatment Strategy For Nonunions and MalunionsDocument25 pagesTreatment Strategy For Nonunions and MalunionsAnisa AnisatusholihahNo ratings yet
- The Physiology of Guitar Playing - IznaolaDocument37 pagesThe Physiology of Guitar Playing - Iznaolajduque825504380% (5)
- Medpox RecallsDocument8 pagesMedpox RecallsmedpoxNo ratings yet
- Ergonomics in Dentistry: By, DR - Rakesh R Nair P.G Student Cons & Endo KVG Dental CollegeDocument94 pagesErgonomics in Dentistry: By, DR - Rakesh R Nair P.G Student Cons & Endo KVG Dental Collegenur awanisNo ratings yet
- Wound Bed PreparationDocument24 pagesWound Bed PreparationnudiaNo ratings yet
- Angiogenesis With Wound HealingDocument36 pagesAngiogenesis With Wound HealingHemant Gupta100% (1)
- Manajemen LukaDocument50 pagesManajemen LukaindraNo ratings yet
- Chronic Wound ManagementDocument31 pagesChronic Wound Managementadrianus andriNo ratings yet
- Basinga Idys C ZPDocument26 pagesBasinga Idys C ZPruiduartNo ratings yet
- Webinar Perawatan Luka Dan Tata Laksana Pemeriksaan InfeksiDocument41 pagesWebinar Perawatan Luka Dan Tata Laksana Pemeriksaan Infeksiqoote3No ratings yet
- Annals of SurgeryDocument12 pagesAnnals of SurgeryNada GhammemNo ratings yet
- Brand Guidelines - GOJEKDocument39 pagesBrand Guidelines - GOJEKGM ProNo ratings yet
- Soft - Tissue 4.1.0.0.REL CAPCPDocument21 pagesSoft - Tissue 4.1.0.0.REL CAPCPaNo ratings yet
- (Upgraded) Damage Control Orthopaedics DR Bambang SpOTDocument37 pages(Upgraded) Damage Control Orthopaedics DR Bambang SpOTroroNo ratings yet
- 02 TissueDocument26 pages02 Tissuecow dasNo ratings yet
- Intraoperative Posterior Polar Cortical Disc.Document5 pagesIntraoperative Posterior Polar Cortical Disc.Danty IndriastutyNo ratings yet
- 3-3 No Antibiotic in Hand InfectionDocument26 pages3-3 No Antibiotic in Hand InfectionProfesseur Christian DumontierNo ratings yet
- Pediatric Neuroanesthesia.3Document4 pagesPediatric Neuroanesthesia.3Mae Importers IncNo ratings yet
- Silver Sulfadiazine For Treatment of Burns and Wounds PDFDocument7 pagesSilver Sulfadiazine For Treatment of Burns and Wounds PDFprakas.rao39695No ratings yet
- Facial LacerationsDocument50 pagesFacial LacerationssevattapillaiNo ratings yet
- Evaluacion Inicial Del Paciente QuemadoDocument12 pagesEvaluacion Inicial Del Paciente QuemadoRyan BNo ratings yet
- AWMA 2011 Standards For Wound Management v2Document36 pagesAWMA 2011 Standards For Wound Management v2Agung Ginanjar100% (1)
- Flaps Cadaver Dissection RMESDocument124 pagesFlaps Cadaver Dissection RMESTeo ChreliasNo ratings yet
- Anatomy & Function of The SkinDocument9 pagesAnatomy & Function of The Skinعبدالعزيز احمد علي عتشNo ratings yet
- Shanz - Ent 1.06 Facial Nerve and Traumatic Facial ParalysisDocument3 pagesShanz - Ent 1.06 Facial Nerve and Traumatic Facial ParalysisPetrina XuNo ratings yet
- Arcuate-Lines - Hernia MagazineDocument24 pagesArcuate-Lines - Hernia MagazineSAURIN CHAUDHARYNo ratings yet
- Gen Surgery EssaysDocument161 pagesGen Surgery EssaysВлади ПетковNo ratings yet
- Mindray iMEC12 SpecsDocument6 pagesMindray iMEC12 SpecsJose Ivan Carvajal CortizosNo ratings yet
- Modul Otologi Gangguan Nervus FasialisDocument65 pagesModul Otologi Gangguan Nervus FasialisHERIZALNo ratings yet
- Controlling Nasal Tip Projection and Rotation With.16Document10 pagesControlling Nasal Tip Projection and Rotation With.16AdRiaNa JuLIetH LoZaDa PaTiÑoNo ratings yet
- Splinting Techniques: by Madhumitha M, Aruna G, Abi P, Sakthivelayudham G, Sujidha R, Srivignesh MDocument99 pagesSplinting Techniques: by Madhumitha M, Aruna G, Abi P, Sakthivelayudham G, Sujidha R, Srivignesh MSakthivelayudhamganesanNo ratings yet
- A Review of Wound Dressing PracticesDocument13 pagesA Review of Wound Dressing PracticesAnonymous 1nMTZWmzNo ratings yet
- Brar, Nicol, Boguniewicz - 2019 - Strategies For Successful Management of Severe Atopic DermatitisDocument16 pagesBrar, Nicol, Boguniewicz - 2019 - Strategies For Successful Management of Severe Atopic DermatitisFranciscoNo ratings yet
- Dengue Insight DR Amit Johari Edited 2020Document82 pagesDengue Insight DR Amit Johari Edited 2020Vedehi BansalNo ratings yet
- Anatomy of The EarDocument63 pagesAnatomy of The EargabrielNo ratings yet
- Fracture and Dislocation-Rahardyan Magetsari (2016) PDFDocument105 pagesFracture and Dislocation-Rahardyan Magetsari (2016) PDFRobertOktaChandraNo ratings yet
- TIME METHOD For WOUND ASSESSMENT (OSCE)Document1 pageTIME METHOD For WOUND ASSESSMENT (OSCE)S. CapanateraisoNo ratings yet
- 3.wound ClassificationDocument7 pages3.wound ClassificationFabi Samad0% (1)
- Pressure Ulcer Prevention & Management: Wocare ClinicDocument20 pagesPressure Ulcer Prevention & Management: Wocare ClinicShoahir RustanNo ratings yet
- 3 Soft Tissue Injury HabtamuDocument80 pages3 Soft Tissue Injury HabtamuWasihunNo ratings yet
- Rekapitulasi Bimbingan DisertasiDocument52 pagesRekapitulasi Bimbingan DisertasiAnnisa NovitaNo ratings yet
- Surgery FinalDocument70 pagesSurgery FinalIris BakerNo ratings yet
- Instruction Manual ECP-TIDocument35 pagesInstruction Manual ECP-TIBryanJermyHendrik100% (1)
- EYE Histology: Dr. OkoloDocument60 pagesEYE Histology: Dr. OkoloAbiola NerdNo ratings yet
- Surgical Access IncisionsDocument7 pagesSurgical Access IncisionsFiliberto RiosNo ratings yet
- 3 - Right Heart AssessmentDocument47 pages3 - Right Heart Assessmentpatricia wageyNo ratings yet
- Review Hemostatic DressingsDocument21 pagesReview Hemostatic DressingsJean Cotte100% (1)
- FinalDocument39 pagesFinalAmeerNo ratings yet
- Parkland Trauma Soft TissueDocument14 pagesParkland Trauma Soft TissueJulieNo ratings yet
- EktremitasDocument40 pagesEktremitasBram wijayaNo ratings yet
- BeauiPHIcation Global ApproachDocument31 pagesBeauiPHIcation Global ApproachKentVilandkaNo ratings yet
- A AaaaaaaDocument6 pagesA AaaaaaaAnonymous d9Bzr1No ratings yet
- Abstracts From The Global Embolization Sympo 2021 Journal of Vascular and inDocument21 pagesAbstracts From The Global Embolization Sympo 2021 Journal of Vascular and infreedy freedyNo ratings yet
- Modern Wound Care - Lohmann & RauscherDocument18 pagesModern Wound Care - Lohmann & Rauschersins1984No ratings yet
- Macrophage ICDocument10 pagesMacrophage ICchristian lunaNo ratings yet
- Class Ii Lower Premolar Mod Amalgam Preparation & RestorationDocument4 pagesClass Ii Lower Premolar Mod Amalgam Preparation & RestorationKizzy SarriaNo ratings yet
- Imaging in Oral Cancers: Ead and Eck YmposiumDocument14 pagesImaging in Oral Cancers: Ead and Eck YmposiumHayyu F RachmadhanNo ratings yet
- 1987 Haapasalo, M., & Ørstavik, D. (1987) - in Vitro Infection and of Dentinal Tubules. Journal of Dental ResearchDocument5 pages1987 Haapasalo, M., & Ørstavik, D. (1987) - in Vitro Infection and of Dentinal Tubules. Journal of Dental ResearchAlexandra Illescas GómezNo ratings yet
- Unit IV A. Physical AssessmentDocument129 pagesUnit IV A. Physical AssessmentGadez JeanpelNo ratings yet
- Management of Dengue FeverDocument31 pagesManagement of Dengue FeverDaniel RajNo ratings yet
- Auric Recon Slides 070516Document92 pagesAuric Recon Slides 070516Yudhistira AdeNo ratings yet
- Bovine Surger y of The Skin: Matt D. MiesnerDocument10 pagesBovine Surger y of The Skin: Matt D. MiesnerGuadalupe Cristina Chuchón CáceresNo ratings yet
- Active Isolated Stretching The Mattes Method 151 184Document38 pagesActive Isolated Stretching The Mattes Method 151 184Nazareth Varas AlonsoNo ratings yet
- Neurological Disorders MCQSDocument78 pagesNeurological Disorders MCQSninestar102100% (3)
- Staging of Bladder Cancer: ReviewDocument23 pagesStaging of Bladder Cancer: ReviewIsabel Gago CastilloNo ratings yet
- Medical Examiner InvestigationDocument11 pagesMedical Examiner InvestigationColleen WelcherNo ratings yet
- CBSE Class 9 Science NCERT Exemplar Solutions Chapter - 6 TissueDocument6 pagesCBSE Class 9 Science NCERT Exemplar Solutions Chapter - 6 TissueNaliniKumaresanNo ratings yet
- Module 2 The Human Reproductive Anatomy and PhysiologyDocument27 pagesModule 2 The Human Reproductive Anatomy and PhysiologyJhunna Talangan100% (1)
- WebpdfDocument233 pagesWebpdfapuntesjmznNo ratings yet
- District: Rajkot Name of Institute: P.D.U. Medical CollegeDocument9 pagesDistrict: Rajkot Name of Institute: P.D.U. Medical CollegeManas K. TrivediNo ratings yet
- Connective Tissue ImagesDocument54 pagesConnective Tissue ImagesSaaraAlleyahAlAnaziNo ratings yet
- Solution Manual For Human Anatomy Laboratory Manual With Cat Dissections 7 e 7th EditionDocument36 pagesSolution Manual For Human Anatomy Laboratory Manual With Cat Dissections 7 e 7th Editionfingrigoasperxwq6100% (35)
- Latihan F4 KSSM 3Document7 pagesLatihan F4 KSSM 3Hamirah Abd HamidNo ratings yet
- 1971 Albus - A Theory of Cerebellar FunctionDocument37 pages1971 Albus - A Theory of Cerebellar FunctionmarkmcwilliamsNo ratings yet
- IGCSE-Revision-Booklet-Part-1-2018-2019 - (New-Spec)Document69 pagesIGCSE-Revision-Booklet-Part-1-2018-2019 - (New-Spec)MaryamNo ratings yet
- Topic 5 - The Uptake and Transport of Water and MineralsDocument32 pagesTopic 5 - The Uptake and Transport of Water and MineralsAshley BedassieNo ratings yet
- 3rd Week of DevelopmentDocument20 pages3rd Week of DevelopmentSidra AslamNo ratings yet
- Plant and Animal Cell WebquestDocument3 pagesPlant and Animal Cell Webquestapi-3133243170% (3)
- GYN - Development of Sexual Organ and SexualityDocument38 pagesGYN - Development of Sexual Organ and SexualityEsha KuttiNo ratings yet
- Bachelors of Physiotherapy Syllabus-1Document98 pagesBachelors of Physiotherapy Syllabus-1golagani praveenkumarNo ratings yet
- Children: The Respiratory Management of The Extreme Preterm in The Delivery RoomDocument21 pagesChildren: The Respiratory Management of The Extreme Preterm in The Delivery RoomRhea Kathleen MejiaNo ratings yet
- Biology Form 3 Reproduction in Plants and Animals - Knec Study Materials, RevisDocument25 pagesBiology Form 3 Reproduction in Plants and Animals - Knec Study Materials, Reviskiraguripeter1994No ratings yet
- Rapid Pathology Pathology Textbook For Medical StudentsDocument89 pagesRapid Pathology Pathology Textbook For Medical Studentsyennqing100% (1)
- Anatomy Compilation of Past PapersDocument162 pagesAnatomy Compilation of Past Papers2803214No ratings yet
- Year 7 Cells and Reproduction - Mark SchemeDocument4 pagesYear 7 Cells and Reproduction - Mark SchemeAnonymous tc7XPINo ratings yet
- TL Gonzalez Sala ValeriaDocument26 pagesTL Gonzalez Sala ValeriagloriaNo ratings yet
- Notes of Human Physiology Class 11Document9 pagesNotes of Human Physiology Class 11ADWAITH LALU100% (1)
- The Study of Biology As The Science of LifeDocument33 pagesThe Study of Biology As The Science of LifeClyde PreciadoNo ratings yet
- Accounting Information Systems Understanding Business Processes 5th Edition Parkes Solutions ManualDocument26 pagesAccounting Information Systems Understanding Business Processes 5th Edition Parkes Solutions ManualKimberlyMendezyptr100% (50)
Wound Healing Fitzpatrick's Dermatology 9th Edition, 2-Volume Set - 220212 - 121805
Wound Healing Fitzpatrick's Dermatology 9th Edition, 2-Volume Set - 220212 - 121805
Uploaded by
Brigitta ClaraOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Wound Healing Fitzpatrick's Dermatology 9th Edition, 2-Volume Set - 220212 - 121805
Wound Healing Fitzpatrick's Dermatology 9th Edition, 2-Volume Set - 220212 - 121805
Uploaded by
Brigitta ClaraCopyright:
Available Formats
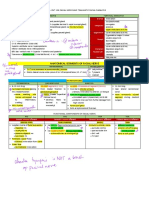
22 Chapter 149 :: Wound Healing
:: Afsaneh Alavi & Robert S. Kirsner
AT-A-GLANCE DIFFERENT TYPES OF
■ While acute and chronic wounds are different, all
WOUND HEALING
chronic wounds start as an acute wound. Primary healing, also called healing by primary or first
■ In acute wounds, there is an orderly progression intention, is the closure of the wound soon after wound
from injury to coagulation, inflammation, cell and creation, as seen in surgical wounds and clean lacera-
Part 22
matrix proliferation, cell migration, and tissue tions. Wound closure is aided by approximation of the
remodeling. wound edges using sutures, glues, tapes, or mechani-
■ In the initial phases, a wide range of growth cal devices, and in side-to-side closure and with grafts
factors, including platelet-derived growth and flaps.
::
factor and transforming growth factor-β1, Delayed primary healing is the slightly delayed closure
Vascular Diseases
play an important role. In the proliferation/ of a wound, typically by a few days. As an example, a
migration and modeling phases, tissue matrix contaminated wound may first be treated with anti-
metalloproteinases (MMPs), integrins, basic microbials to assure eradication of bacteria that might
fibroblast growth factor, and epidermal growth delay healing.
factor are critical. MMP-1, MMP-9, and MMP-10 In healing by secondary intention, the open wound
are essential for remodeling. heals through a process that includes granulation
■ For acute wounds, moist wounds heal faster, and a
tissue formation and epithelialization. Commonly
variety of wound dressings are available, including
employed after an excessive loss of soft tissue, such as
hydrogels, polyurethane films, hydrocolloids,
major trauma or severe burns, the large defect requires
foams, alginates, superabsorbent dressings, and
ingrowth of granulation tissue and extracellular matrix
collagen-based products.
(ECM) formation. Myofibroblasts plays a major role in
this type of healing,1 appearing 3 days after the injury
■ In chronic wounds, the linear progression
and reaching a maximum level 10 to 21 days postin-
between the sequential phases of acute wound
jury. Secondary intention healing may result in wound
healing is lost. Chronic wounds are often the
contracture and can cause functional restriction.
result of ischemia, pressure, and infection;
Tertiary intention occurs when a wound originally
healing, in part, is dependent on addressing
closed by primary intention dehisces and then heals
these factors.
by secondary intention.
■ Healing after skin grafting is also different, The time to complete healing depends on many
as it depends on revascularization, either factors such as the depth of the wound, location of
neovascularization or inosculation. the wound (eg, facial wounds heal faster than acral
wounds), vascular supply, presence of infection, and
wound shape (smaller diameter wounds heal faster
than larger diameter wounds of the same size/area.)3
Wound healing involves a complex but overlapping
sequential series of events aimed at barrier restoration,
from hemostasis to inflammation, proliferation, and
remodeling. Many mediators, such as platelets, neutro- MECHANISMS OF
phils, macrophages, cytokines, growth factors, matrix
metalloproteinases, and their inhibitors regulate these WOUND HEALING
events.1 Some wounds fail to move through these
stages in an orderly and timely fashion and become PHASES OF WOUND HEALING
chronic wounds. All these components play a role in
healing, and alteration in one or more of these com- Tissue injury triggers a cascade of sequential, overlap-
ponents may impair healing and/or lead to abnormal ping events that have been categorized into several
scar formation, such as a hypertrophic scar or keloid.2 phases, including: (a) coagulation, (b) the inflamma-
Wounds can be categorized by the depth of the wound, tory phase, (c) the proliferative (and migratory) phase,
which helps predict the amount of scarring that will and (d) the remodeling phase. Figure 149-2 illustrates
occur. Greater scarring occurs in full-thickness versus these phases in diagrammatic form, and Fig. 149-3
partial or spilt-thickness wounds. Figure 149-1 out- shows specific events that take place during the vari-
lines these differences. ous phases. The cell types primarily involved in wound
Kang_CH149_p2700-2718.indd 2700 04/12/18 9:34 am
Split- and full-thickness wound areas
healing are platelets, neutrophils, and macrophages,
fibroblasts, endothelial cells, and epithelial cells. More
22
recently, increasing importance is accumulating for the
Full-thickness Split-thickness
wound wound role, either directly or indirectly, of lymphocytes.4,5
COAGULATION
Immediately after injury, disruption of blood vessels
Epidermis
leads to local release of blood cells and bloodborne
elements, resulting in clot formation and activation
of the intrinsic and extrinsic coagulation cascade.3
While the blood clot within the vessel lumen provides
Dermis hemostasis, the clot within the injury site acts as a
provisional matrix for cell migration, leads to further
Chapter 149 :: Wound Healing
formation of ECM,6 and provides a reservoir for cyto-
kines and growth factors.7,8 Platelets degranulate and
release α granules which secret growth factors includ-
ing platelet-derived growth factors, insulin-like growth
Subcutaneous
tissue factors, epidermal growth factors, transforming growth
factor-β, and platelet factor 4. Platelets also release a
number of chemotactic factors that attract other plate-
lets, leukocytes, and fibroblasts to the site of injury.8,9
Figure 149-1 Diagrammatic representation of the skin, The clot also contains fibrin, fibronectin, vitronectin, von
with 2 inverted triangles representing either a split-
Willebrand factor, and thrombospondin, which provide
thickness or full-thickness wound. Extending the injury
below the reservoir of keratinocytes present in skin a matrix for cell migration. Vasoactive amines released
appendages (full-thickness wound) removes the capa- from platelets, such as serotonin, facilitate cell migration
bility of the keratinocytes to populate the defect from by increased microvascular permeability. Hageman fac-
within the wound bed, which means healing has to tor XII is a specific enzyme released following platelet
occur from the wound edges and more scarring takes aggregation to initiate the intrinsic coagulation cascade.
place. Prothrombin transforms into thrombin, converting sol-
uble fibrinogen to insoluble fibrin. Additionally, injured
The different phases of wound healing
Phases of healing Main cell types involved
Coagulation Platelets
phase
Inflammatory Platelets
phase Macrophages
Neutrophils
Macrophages
Migratory/proliferative Fibroblasts
phase Epithelial cells
Endothelial cells
Remodeling Fibroblasts
phase Myofibroblasts
Injury Hours Days Weeks
2701
Figure 149-2 Schematic, different of the different phases of wound healing.
Kang_CH149_p2700-2718.indd 2701 04/12/18 9:34 am
22 The phases of wound healing and key cells and events involved
Time Phases Main cell types Specific events
Coagulation
Platelet aggregation and release of
Fibrin plug formation,
Platelets fibrinogen fragments and other
release of growth factors,
pro-inflammatory mediators
cytokines, hypoxia
Hours
Inflammatory Selectins slow down blood cells + binding
Neutrophils
Cell recruitment and to integrins diapedesis
Monocytes
chemotaxis, wound Hemidesomosome break-down
Macrophages
debridement keritinocyte migration
Days
Part 22
Migratory/proliferative
Keratinocytes Cross-talk between MMPs, integrins,
Epidermal resurfacing, Fibroblasts cells, cytokines cell migration,
fibroplasia, angiogenesis, Endothelial cells ECM production
ECM deposition, contraction
::
Vascular Diseases
Remodeling Phenotypic switch to
Scar formation and revision, Myofibroblasts myofibroblasts from
Weeks ECM degredation, further fibroblasts
to contraction and tensile strength
months
Figure 149-3 The phases of wound healing, and key cells and events involved. (Reprinted from Falanga V. Wound healing
and its impairment in the diabetic foot. The Lancet. 2005;366:1736-1743; with permission. Copyright © Elsevier.)
tissue releases a tissue factor that activates the extrinsic of these same chemoattractants are also responsible
coagulation pathway.9 for recruitment of neutrophils.13,14 Other more specific
chemoattractants further recruit monocytes, includ-
INFLAMMATION ing collagen fragments, fibronectin, elastin, and trans-
forming growth factor (TGF)-β1. Monocytes undergo a
Inflammation begins with activation of classic and phenotypic change to tissue macrophages critical for
alternative complement cascades and subsequent the progression of healing.15,16 Macrophages release che-
neutrophil infiltration to the wound site within 24 motactic factors to attract fibroblasts to the wound area.
to 48 hours of injury. White cells have multiple func- Importantly, they display impressive plasticity, and at
tions, including phagocytosis of necrotic material and least 2 subsets of macrophages exist and have distinct
bacteria, as well as the production of certain critical phenotypes in various stages of healing (see below).
cytokines.10,11 Leukocytes adhere to the adjacent blood They also produce a variety of growth factors, such
vessels (margination) and actively move through as platelet-derived growth factor (PDGF), fibroblast
the vessel wall via diapedesis. Leukocytes release growth factors (FGFs), and vascular endothelial growth
enzymes and oxygen-derived free radicals. After the factors (VEGFs), as well as TGF-β and TGF-α. Altera-
first few days, the constituency of white cells changes tions in tissue macrophages or circulating monocytes
as neutrophils are replaced by macrophages.12 lead to poor intrinsic debridement, delay proliferation
Macrophages, often considered the most important of fibroblasts, and allow for inadequate angiogenesis
regulatory cells in the wound healing inflammatory and overall poor healing.17
process, typically appear in the wound site 72 hours Macrophages are divided into M1 (or classically
after the injury. Macrophages, key regulator cells for activated) and M2 (or alternatively activated) mac-
repair, are the main phagocytic cells and release pro- rophages. M1 phenotype macrophages are activated
teolytic enzymes such as a variety of collagenases. by interferon-γ and tumor necrosis factor (TNF)-α
Macrophages also produce growth factors responsible following wound formation. They release interleu-
for the smooth muscle proliferation and endothelial kin (IL)-12 and promote a proinflammatory T-helper
cell and fibroblast proliferation, all of which contribute (Th)-1 immune response early on. Subsequently, M2
to ECM production. This hypoxic environment is asso- macrophages, activated by IL-4 and IL-13, work to
ciated with high levels of proteases and low pH, both downregulate inflammation by releasing antiinflam-
of which contribute to activation of growth factors.11 matory cytokines such as IL-10. These M2 macro-
2702 Monocytes are attracted to the injury site by kallikrein, phages present later in healing during granulation
fibrinopeptides, and fibrin-degradation products; some tissue formation.17-19
Kang_CH149_p2700-2718.indd 2702 04/12/18 9:34 am
ABNORMAL INFLAMMATORY PHASE proliferate and produce a matrix consisting of fibronec-
tin and hyaluronan initially, and collagen and proteo-
22
Immediately after injury, local vasodilation, extrava- glycans later. These components are essential for new
sation of blood and fluid, and lymphatic drainage ECM formation and tissue repair. ECM serves both as
blockage (in some cases) can lead to cardinal symp- turgor of soft tissue and as a scaffold and regulator of
toms of inflammation such as heat, redness, pain, cell adhesion and growth. It is made of an interstitial
and swelling. The acute inflammatory response may matrix of adhesive proteins embedded in proteogly-
last 2 weeks; however, prolongation of inflammation can and glycosaminoglycan gel as well as the fibrinous
(chronic inflammation) may delay healing.20 structural proteins collagen and elastin.23
With chronic inflammation, the wound often con- Fibroblasts make collagen, the most abundant
tains necrotic tissue and pathogenic organisms. In protein in the body, and noncollagenous proteins.
this case, granulocytes disappear and mononuclear During the proliferative phase, collagen synthesis
cells, particularly monocytes, lymphocytes, and mac- is induced by PDGF, basic FGF (bFGF), TGF-β, IL-1,
rophages, become the predominant cells at the site of and TNF. There are 18 different types of collagen.
Chapter 149 :: Wound Healing
inflammation. Fibrillar collagens, such as I, III, and V, form the con-
From the clinical standpoint, certain wounds, such nective tissue in the healing wound, and nonfibril-
as pyoderma gangrenosum, have excessive inflamma- lar forms, such as collagen IV, form the basement
tion and treatment, with corticosteroids for example, membrane.
leads to downregulation of inflammation and healing. Collagen gene expression is regulated by multiple
Fine-tuning the inflammatory response may represent factors such as TGF-β and FGF. TGF-β stimulates pro-
a therapeutic target for other wounds as well.21 duction of collagen I and collagen III. The overexpres-
sion of matrix metalloproteinases (MMPs) and/or
impaired counteraction of tissue inhibitor of metal-
PROLIFERATION loproteinases (TIMPs) contributes to delayed healing
and fibrosis. Interaction between these cytokines is
The proliferative phase, characterized by fibroblast extremely important. The fibroblasts in patients with
migration, deposition of ECM, and formation of gran- longstanding diabetic foot ulcers show a decreased
ulation tissue, normally starts at about day 3 after response to TGF-β1 and decreased expression of TGF-β
wounding and lasts for 2 to 4 weeks. Figure 149-4 receptors. Although overexpression may be problem-
illustrates events that occur in the proliferative/migra- atic, tissue matrix MMPs and other enzymes, such
tory and remodeling phases. An important event in as plasminogen activator inhibitor, are critical to the
this phase is reepithelialization. This critical event also movement of cells through provisional structural
involves migration of keratinocytes and the interde- matrix components.
pendence between keratinocyte movement over the Adhesive proteins, including fibronectin (FN), lam-
provisional fibrin matrix, recruitment of fibroblasts inin, thrombospondin, and integrins, help guide cel-
and endothelial cells, and ECM formation.22 lular migration.24 FN is a large heterodimer linked to
Growth factors, such as PDGF and TGF-β, attract cell surfaces, basal membranes, and the ECM. FN can
fibroblasts to the wound. Fibroblasts subsequently attach to ECM components such as collagen, fibrin,
Keratinocyte proliferative burst
Epidermal migration
Fibrin plug Hair follicle keratinocyte
contribution after injury
Hemidesmosome
disassembly/keratinocyte migration
Angiogenesis Cell migration and recruitment
ECM deposition stimulated by
growth factors, cytokines
Figure 149-4 Schematic, using a modified photomicrograph section, of the events taking place shortly after injury, includ- 2703
ing formation of a fibrin plug, epidermal migration, and extracellular matrix deposition.
Kang_CH149_p2700-2718.indd 2703 04/12/18 9:35 am
22 and proteoglycan, or to integrins and directly mediate
the cell migration. FN also activates intracellular sig-
to a protein backbone that modulate cell growth
and differentiation. Additionally, glycosaminoglycans
naling pathways to increase the sensitivity of certain without a protein core (hyaluronan) are also important
cells, such as endothelial cells, to growth factors.25 components of the ECM.
Integrins are important in cell–cell and cell–matrix Histopathology of a granulating wound bed shows
adhesion, serving to regulate interaction between proliferation of fibroblasts and capillaries in a loose
ECM and the cytoskeleton. The integrins, consisting ECM. Neovascularization, or formation of new blood
of at least 24 αβ heterodimers (18 α and 8 β subunits), vessels, is characteristic of this stage. Several factors
are transmembrane cell surface receptors that bind the induce angiogenesis as a part of granulation tissue
ECM to cytoskeletal structures.25 The integrin profile is development; new capillaries sprout, invading the
very dynamic during the repair process. For example, fibrin and FN-rich clot. The density of blood ves-
dermal fibroblasts undergo a switch from α2 to α3 and sels is reduced over time with scar formation and as
α5 integrin subunits. As another example, endothelial the wound moves toward the remodeling phase.26
cells cannot respond to angiogenic stimuli without Fibroblast replication and longevity are enhanced in
the expression of αvβ5 integrin. Certain polypeptide
Part 22
hypoxia, and low oxygen tension stimulates clonal
growth factors are essential to angiogenesis, including expansion of dermal fibroblasts seeded as single cells.27
bFGF and VEGF.25,26 Table 149-1 highlights the main Moreover, the synthesis of a number of growth factors
cytokines and growth factors shown to play a role in is enhanced in hypoxic cells.
::
the repair process. After a provisional matrix has formed, keratino-
Vascular Diseases
Another constituent of ECM are noncollagenous cytes migrate to epithelize the wound. MMP function
proteins such as proteoglycans, which are glycosami- is critical for allowing keratinocytes at the edge of the
noglycans (dermatan sulfate, heparin sulfate) linked wound to detach from their hemidesmosomal and
TABLE 149-1
The Major Growth Factors Involved in Wound Healing and Their Functions39
GROWTH FACTOR MAJOR SOURCES FUNCTION
Epidermal growth factor (EGF) Platelets, macrophages, fibroblasts Epithelialization
Fibroblast proliferation
Keratinocyte proliferation
Angiogenesis
Transforming growth factor Keratinocytes, macrophages, fibroblasts, Keratinocyte migration
(TGF)-α lymphocytes
TGF-β Macrophages, fibroblasts, keratinocytes, Inflammation, angiogenesis, reepithelialization, connective tissue
platelets regeneration, remodeling
TGF-β1, TGF-β2: promote fibrosis and scar formation
TGF-β3: antiscar properties
Activins Fibroblasts, keratinocytes Epithelialization
Fibroblast growth factor (FGF) Keratinocytes, fibroblasts, smooth muscle FGF-2: granulation tissue formation, reepithelialization, tissue
cells, chondrocytes, endothelial cells, remodeling, fibroblast migration, collagen formation
mast cells FGF-7, FGF-10: increase transcription factors, detoxification of
reactive oxygen species
FGF-7: neovascularization
Platelet-derived growth factor Platelets, macrophages, vascular Fibroblast proliferation
endothelium, fibroblasts Angiogenesis
Matrix formation
Vascular endothelial growth Keratinocytes, endothelial cells, Angiogenesis
factor (A-E) fibroblasts, smooth muscle cells,
platelets, neutrophils, macrophages
Granulocyte-macrophage Macrophages Keratinocyte proliferation
colony-stimulating factor Fibroblasts Epithelialization
Endothelial cells Cell migration
Natural killer cells Chemotaxis
Mast cells Angiogenesis
Interleukin (IL)-1 Monocytes Keratinocyte proliferation
Macrophages Fibroblast proliferation
Keratinocytes Angiogenesis
Neutrophil chemotaxis
IL-6 Neutrophils Keratinocytes proliferation
2704 Monocytes Neutrophil chemotaxis
Kang_CH149_p2700-2718.indd 2704 04/12/18 9:35 am
desmosomal attachments and migrate across the pro-
visional matrix. Other proteins play important roles,
breakdown of collagen as the ECM evolves. Start-
ing early in the healing process, wound remodeling
22
including plasminogen activator inhibitor, a serine may continue for months. The interaction of ECM
protein inhibitor that functions as the main inhibitor of and fibroblasts causes wound contraction and is
tissue plasminogen activator, and urokinase plasmino- influenced by multiple cytokines, including TGF-β,
gen activator.28 PDGF and bFGF.
Upregulation of tissue plasminogen activator and The remodeling of the ECM, as well as the move-
urokinase plasminogen activator are important for ment of cells, is highly dependent on MMPs and serine
keratinocyte migration, which may depend on cross- proteases.33 An important component of this depen-
talk and interactions between α3β1, keratinocytes, and dence on MMPs is MMP-driven degradation of ECM
collagen. These events lead to the induction of MMP-1 and the resulting exposure of selective bioactive ECM
(collagenase-1 or interstitial collagenase), which is segments that influence cell behavior, including migra-
important for keratinocyte migration and epitheliali- tion and proliferation.6,33
zation.6 MMP-9 plays a fundamental role in “cutting” Metalloproteinases produced by fibroblasts, neu-
Chapter 149 :: Wound Healing
Type IV and Type VII collagen, which are essential trophils, keratinocytes, and macrophages, include
components of the basement membrane and anchor- interstitial collagenase (degrades collagen Types I,
ing fibrils, and promotes inflammation and neutro- II, and III), gelatinases (degrades denatured collagen
phil migration. For keratinocyte migration to occur, and FN) and stromelysins (degrades proteoglycans,
a necessity exists to break down these complex struc- laminin, FN, and amorphous collagen). MMP-10
tures anchoring the basal keratinocytes to the basement (stromelysin) breaks down other noncollagenous
membrane and neighboring keratinocytes. This pro- ECM components and facilitates migration.6,11,34 Other
cess is as complex as the structure itself, and involves mediators, such as thymosin-β, upregulate MMPs
interactions between MMPs, integrins, growth factors, during wound repair.35 The activity of MMPs are
and structural proteins. In the normal resting state, tightly regulated because they may degrade essential
laminin-332 is bound to α6β4-integrin, the latter linking collagens and impair healing. They are activated by
the intracellular keratin filaments of keratinocytes to certain proteins (plasmin) and inhibited by specific
the basement membrane. As a result of the interaction tissue inhibitors of metalloproteinases. Table 149-2
of integrins (including their phosphorylation status) summarizes certain MMPs and their prominent effect
with the ECM and their receptor clustering on the sur- in wound healing.
face of keratinocytes, important morphologic changes, During the remodeling process, a phenotypic switch
such as lamellipodia formation, occur for keratinocyte occurs in certain cell subpopulations from fibroblasts
locomotion.29-31 Migration of keratinocytes is essential to myofibroblasts.36 Although the early process of heal-
for resurfacing of the wound.26,32 ing relies largely on matrix accumulation, which, in
Keratinocytes begin to migrate from the wound turn, facilitates cell migration, later healing requires a
edge and from skin appendages within the first dampening of ECM formation to a level that at least
24 hours. The hair bulge, the germinative portion approximates the preinjury state. However, the remod-
of the hair, is an important reservoir for keratino- eling phase is more than a breakdown of excess mac-
cytes in partial thickness wounds. A series of events romolecules formed during the proliferative phase of
in migration involves elongation of keratinocytes, wound healing. During this phase, cells within the
development of pseudopod-like projection of lamel- wound are returned to a stable phenotype, ECM mate-
lipodia, loss of cell-to-cell adhesion, retraction of rial is altered (ie, collagen Type III to collagen Type I),
intracellular tonofilaments, and formation of actin and granulation tissue disappears.11,26 Granulation tis-
filaments at the edge of the cytoplasm, all of which sue evolves to a scar composed of less-active fibro-
occur while the proliferative ability of keratinocytes blasts, dense collagen, and fragments of elastic tissue
is inhibited. along with the rest of ECM. Scar matures and the ten-
To facilitate migration, there is a marked increase in sile strength increases to a maximum of 80% strength
mitotic activity within the basal epithelial cells of the of noninjured skin. In full-thickness wounds, contrac-
wound edge from 12 hours, extending lamellipodia tion is responsible for 40% of the decrease in wound
along the wound edges. Subsequently keratinocytes size.
lose their attachment to the underlying dermis to
migrate in a leapfrog fashion. Eventually a new base-
ment membrane forms and further growth and dif-
ferentiation of epithelial cells establishes the stratified FETAL HEALING
epithelium. The process of epithelialization is facili-
tated in a moist environment, serving as the biologic During early embryogenesis, wounded fetal tissue
basis for modern occlusive dressings. heals without fibrosis. Regeneration, as opposed
to repair, occurs. Later in embryogenesis (last tri-
mester) and after childbirth, repair (as opposed to
REMODELING regeneration) occurs, with resulting fibrosis. Among
factors that affect scarring, fibromodulin is a small
The final phase, remodeling, is typically the lon- glycoprotein that mediates scarless healing in fetal 2705
gest phase, involving the continuous synthesis and skin.37
Kang_CH149_p2700-2718.indd 2705 04/12/18 9:35 am
22 TABLE 149-2
Matrix Metalloproteinases Proteinases with Well-Established,
Functional Effects on Wound Healing
CORRESPONDING
EFFECT COMMON NAMES MMP DESIGNATION SOME SPECIFIC EFFECTS
Keratinocyte prolifera- Collagenase 1 MMP-1 Increased migration
tion and migration Gelatinase A MMP-2
Stromelysin 2 MMP-10
Matrilysin-1 MMP-7
Epilysin MMP-28
Endothelial cell (EC) Collagenase 3 MMP-13 Increases EC migration
migration Gelatinase A MMP-2 Needed for angiogenesis
MT1-MMP MMP-14 Needed for angiogenesis
Part 22
Cell migration Stromelysin 1 MMP-3 Required for excisional
Stromelysin 2 MMP-10 wounds
Matrilysin-2 MMP-26
::
Inflammation Collagenase 2 MMP-8 Antiinflammatory
Vascular Diseases
Gelatinase A MMP-2 Antiinflammatory
Gelatinase B MMP-9 Promotes inflammation
Matrilysin-1 MMP-7
Neutrophil migration Gelatinase B MMP-9
MT6-MMP MMP-25 Increases neutrophil
migration
Apoptosis Collagenase 2 MMP-8 Prevents apoptosis
MT1-MMP MMP-14 Antiapoptotic
MT2-MMP MMP-15
MT6-MMP MMP-25
MMP, matrix metalloprotease; MT, membrane type.
EGF is secreted in a paracrine fashion by platelets,
GROWTH FACTORS AND macrophages and fibroblasts and acts on keratino-
CYTOKINES cytes. Faulty location of the EGF receptor may be prob-
lematic in some nonhealing wounds. An in vitro study
demonstrated the presence of EGFR in the cytoplasm,
Wound healing is regulated by multiple growth fac- rather than the extracellular membrane, of cells in
tors and cytokines released at the wound site. Growth non,healing wounds, suggesting receptor downregu-
factors are biologically active polypeptides that can lation within chronic wounds.42-44 TGF-α is another
alter the growth, differentiation and metabolism of a member of the EGF family that is secreted by kerati-
target cell. They are important elements in the healing nocytes, macrophages, fibroblasts, and lymphocytes,
of wounds. Table 149-1 lists the major growth factors and works in an autocrine fashion.45,46 TGF-α induces
and cytokines involved in healing and their respective expression of keratin 6 and keratin 16 (present in pro-
roles.38-40 Although potentially important in healing liferating keratinocytes) and increases keratinocyte
from a therapeutic standpoint, only PDGF-BB, bFGF, migration.47
and granulocyte-macrophage colony-stimulating fac-
tor (GM-CSF) are used clinically in the management of
wounds, and only PDGF is approved for wound heal-
ing by the U.S. Food and Drug Administration (FDA). TRANSFORMING GROWTH
FACTOR-β FAMILY
EPIDERMAL GROWTH TGF-β family members include TGF-β1 to TGF-β3,
FACTOR FAMILY bone morphogenic proteins, and activins. TGF-β1,
TGF-β2, and TGF-β3 promote the migration of fibro-
Epidermal growth factor (EGF) family members bind blasts and endothelial cells and deposition of extra-
to a tyrosine kinase transmembrane protein or EGF cellular matrices by fibroblasts during granulation
receptor.41 EGFR normally localizes throughout the tissue formation. TGF-β1 predominates in wound
epidermis with its membranous presence being more healing.48 Interestingly, TGF-β1 and TGF-β2 promote
prominent in the basal layer. EGFR plays an important fibrosis and scar formation, whereas TGF-β3 has antifi-
2706 role in reepithelialization by increasing keratinocyte brotic properties.49 TGF-β, produced by macrophages,
proliferation and cell migration.42,43 fibroblasts, keratinocytes, and platelets, is important
Kang_CH149_p2700-2718.indd 2706 04/12/18 9:35 am
in the wound healing processes of inflammation,
angiogenesis, reepithelialization, and connective tis-
factors such as TGF-β.62 PDGF plays an important role
in blood vessel maturation and works synergistically
22
sue regeneration.48,50 TGF-β1 facilitates recruitment of with hypoxia to stimulate VEGF formation in vitro.
inflammatory cells, and promotes macrophage medi- However, PDGF angiogenic activity is less than FGF
ated debridement and granulation tissue formation. and VEGF.63 While not directly affecting keratinocyte
During reepithelialization, TGF-β1 shifts keratinocyte migration, PDGF plays role in reepithelialization by
integrin expression toward a more migratory sub- in vitro production of insulin-like growth factor-1 and
type.51 In the remodeling phase, TGF-β1 plays a major thrombospondin-1. PDGF also enhances the prolifera-
role in collagen production and inhibits collagen tion of fibroblasts and, in turn, the production of ECM.
breakdown by inhibiting MMP-1, MMP-3, and MMP- Recombinant human PDGF-BB (becaplermin) is the
9, and promoting TIMP-1.52,53 only FDA-approved drug for nonhealing neuropathic
TGF-β1 plays an important role in the formation diabetic foot ulcers.64,65
of hypertrophic scars and keloids by overexpression
of connective tissue growth factor.54 In fetal wounds,
VASCULAR ENDOTHELIAL GROWTH
Chapter 149 :: Wound Healing
deceases in TGF-β1 transcription help explain the scar-
less healing that is seen.55 FACTOR FAMILY
Activins are members of the TGF-β family produced
by fibroblasts and keratinocytes and play role in reepi- Members of the VEGF family include VEGF-A to
thelization. Activin inhibits keratinocyte proliferation VEGF-E and placental growth factor.66 VEGF-A, which
and induces terminal differentiation of keratinocytes. is secreted by keratinocytes, endothelial cells, fibro-
bone morphogenic proteins are another member of blast smooth muscle cells, platelets, neutrophils, and
the family involved in keratinocyte differentiation. macrophages, binds to a tyrosine kinase surface recep-
Overexpression of bone morphogenic protein-6 is tor that is located on the endothelial surface of blood
associated with delayed healing.39,56 vessels, early in wound healing angiogenesis.67 Plate-
lets release VEGF-A upon injury. Macrophages release
VEGF-A directly but also release TNF-α, which induces
FIBROBLAST GROWTH VEGF-A expression on keratinocytes and fibroblasts.
Hypoxia is a major stimulus for release of VEGF-A,
FACTOR FAMILY and the VEGF-A gradient parallels the hypoxia gradi-
The 3 main members of the FGF family involved in ent. VEGF-A is also involved mainly in the inflamma-
wound healing are FGF-2, FGF-7, and FGF-10. FGFs tory stage of wound healing. Placental growth factor is
are produced by keratinocytes, fibroblasts, smooth expressed by keratinocytes and endothelial cells as a
muscle cells, chondrocytes, endothelial cells, and mast proangiogenic molecule. Placental growth factor stim-
cells.57 FGF receptors 1 to 4 are tyrosine kinase trans- ulates cultured fibroblast migration and stimulates
membrane proteins that work like EGFR.45 granulation tissue formation.68
bFGF or FGF-2 plays a role in granulation tissue for-
mation, reepithelialization, and tissue remodeling.58
FGF-2 regulates the synthesis of ECM components,
GRANULOCYTE-MONOCYTE
and facilitates keratinocyte and fibroblast migra- COLONY-STIMULATING FACTOR
tion and collagenase formation. bFGF is decreased in
chronic wounds.59 GM-CSF has particular importance in the inflamma-
FGF-7 or keratinocyte growth factor-1 and FGF 10 tory stage of wound healing by increasing keratino-
or keratinocyte growth factor-2. FGF-7 and FGF-10 are cyte proliferation and enhancing reepithelialization.
secreted in a paracrine fashion, found only on kerati- GM-CSF promotes proliferation and differentiation
nocytes, and have a role in reepithelialization. FGF-7 of neutrophils and hence increases host defenses.69
and FGF-10 increase transcription factors involved GM-CSF indirectly upregulates IL-6. In 2 studies on
in detoxification of reactive oxygen species. FGF-7 is diabetic foot ulcers, in total 67 patients with infected
a strong mitogen of vascular endothelial cells and is diabetic foot ulcers were treated either with placebo
important during neovascularization.60 or topical GM-CSF. Although GM-CSF improved
neutrophil function and increased absolute neutro-
phil numbers, the addition of topical GM-CSF to
PLATELET-DERIVED GROWTH standard care had no additional beneficial clinical
effect.69
FACTOR FAMILY
PDGFs, produced by platelets, macrophages, vascu-
lar endothelium, fibroblasts, and keratinocytes, bind
PROINFLAMMATORY CYTOKINES
to 2 different transmembrane tyrosine kinase recep- Proinflammatory cytokines, including IL-1, IL-6, and
tors (α and β).61 Upon injury PDGF is released from TNF-α, are upregulated in the inflammatory phase of
degranulating platelets. PDGF, chemotactic for mono- wound healing. IL-1 is produced by monocytes, macro-
cytes, macrophages, and neutrophils, is a mitogen for phages, monocytes, and keratinocytes, with both para-
fibroblasts and smooth muscle cells in vitro. PDGF crine and autocrine functions. IL-1 induces expression 2707
also stimulates macrophages to produce growth of keratin 6 and keratin 16 in migrating keratinocytes,
Kang_CH149_p2700-2718.indd 2707 04/12/18 9:35 am
22 and activates fibroblasts to secrete FGF-7.70 IL-6 is
produced by neutrophils and monocytes with mito- TABLE 149-3
genic and proliferative effect on keratinocytes and Debridement Techniques
chemoattractive effects on neutrophils. TNF-α and
IL-1β are increased in chronic wounds. The effect of DEBRIDEMENT
TECHNIQUES ADVANTAGES DISADVANTAGES
exogenous TNF is dependent on the concentration
and duration of exposure.70,71 TNF-α at low levels Surgical, sharp (with High speed Painful procedure,
promotes healing by stimulating inflammation and scissors and/or Selectivity expensive
increasing macrophage-produced growth factors, scalpel) Needs skilled
whereas at higher levels TNF-α impairs wound heal- professionals
Contraindicated in
ing by suppressing production of ECM and TIMP and
ischemic tissue and
increasing MMPs. Chronic inflammation stimulates
bleeding disorders
production of TNF-α and IL-1β that synergistically
Enzymatic Low pain Medium cost and low
increases production of MMPs and suppress produc-
(collagenase) selectivity
Part 22
tion of TIMPs.72
Some patients are
allergic to the
CHEMOKINES enzyme preparation
::
Biologic (larval High speed and High cost
Chemokines are a family of small cytokines or signal- therapy) high selectivity Contraindicated in
Vascular Diseases
ing proteins that attract neutrophils to the site. Macro- Medium pain bleeding diathesis
phage chemoattractant protein-1 (or CCL2) is induced and deep, tunneling
by keratinocytes and is chemoattractant for monocyte/ wounds
macrophages, T cells, and mast cells.73 Mechanical (wet Medium speed Painful
Interferon-inducible protein 10 (or CXCL10) is to dry dressings, Nonselective
another cytokine that negatively impacts wound heal- hydrotherapy,
ing. Interferon-inducible protein 10 inhibits migration ultrasonography)
of fibroblasts. IL-8 increases keratinocyte migration and Autolytic Low pain Low speed
proliferation, and is a chemoattractant of neutrophils.74 (endogenous Low selectivity
enzymes with Relatively high cost
moisture-retentive Contraindicated in
CLINICAL ISSUES IN
dressings) infected wounds
Risk of exposed bone/
WOUND HEALING
tendon and friable
skin
WOUND BED PREPARATION
of microorganisms that protect themselves through
Although the majority of wounds heal in a timely community living, in part by a surrounding glycocalyx
manner, a proportion of wounds stall and do not fol- (Fig. 149-5). Disruption of biofilms with debridement,
low the stages of healing. A nonhealing wound needs with or without antimicrobial agents, helps alleviate
wound bed preparation to promote healing. The con- persistent inflammation.77
cept of wound bed preparation has been summarized The term antimicrobial includes disinfectants, anti-
using the pneumonic TIME: Tissue debridement, septics, and antibiotics. Antiseptics are broad spectrum
Infection/inflammation, Moisture balance, Epithelia with less risk of bacterial resistance. The difference
edge tissue.21,32,75 between antibiotics and antiseptics is that antiseptics
Tissue debridement plays a key role in tissue prep- are nonspecific, while antibiotics work specifically on
aration by removing nonviable tissue and patho- bacteria functions or processes such as disputing cell
genic bacteria. Multiple techniques to debride exist, wall function but also can allow bacteria opportunity
including surgical, enzymatic, biologic, mechanical, to mutate and develop resistance. As a result, topical
and autolytic techniques. Newer tools, such as low- antibiotics are not recommended for chronic wounds
frequency ultrasound and hydrosurgery devices, have because of the risk of antibiotic resistance. A variety of
been developed.76 Table 149-3 lists techniques used for modern antiseptic-impregnated dressings have been
tissue debridement. used to reduce microorganism numbers in the dress-
Treating infection and inflammation implies assess- ings and, in theory, on the wound surface. Their effect
ment of the need for topical antiseptic and/or systemic on biofilm organisms is less-well defined. Table 149-4
antibiotic use to control infection and subsequent lists these antiseptics.
inflammation. Although inflammation is a physiologic Moisture imbalance involves the assessment and
process in wound healing, inappropriate inflamma- management of wound exudate. While acute wound
tion can cause delayed healing. Infection may be clas- fluid promotes cell growth and is rich in cytokines
sically seen as a host response, as in cellulitis. Bacteria and growth factors, chronic wound fluid inhibits cell
2708 may also delay healing through formation of biofilm, growth and contains high levels of proteases and
seen in 60% of chronic wounds. Biofilms are colonies proinflammatory cytokines. Thus, acute wounds
Kang_CH149_p2700-2718.indd 2708 04/12/18 9:35 am
Biofilm formation In Vivo 22
(Porcine)
SEM
Wound bed Staphylococcus aureus
72 hours
Chapter 149 :: Wound Healing
Figure 149-5 Biofilm formation. Colonies of microorganisms with a surrounding glycocalyx. SEM, scanning electron micrograph.
benefit from contact with wound fluid, whereas can tolerate the often subtle (but important) trauma
chronic wounds do not. Moisture can hinder wound that comes from removal of adhesive dressings such as
healing in other ways as well: extra moisture can dam- films. Thin contact layers, consisting of different poly-
age periwound skin, and lack of moisture can hinder meric materials, some with perforations, allow wound
keratinocyte migration. fluid to escape and are useful in preventing tissue
The major dressing types (Table 149-5) include injury upon dressing changes.
hydrogels, transparent polyurethane films, hydrocol- Edge assessment involves the assessment of non-
loids, gelling fibers, alginates, foams, superabsorbents, advancing wound edges and proper use of therapies
and collagen products. In determining the most appro- to advance the wound edge.21 Keratinocytes from the
priate dressing for a particular wound, one must con- edge of chronic wounds often abnormally express
sider the need for absorption of exudate (foams and c-myc and treatments, such as debridement, which
alginates), the need for additional moisture (hydro- remove or reverse this cellular biomarker, can promote
gels), and whether the wound and its epithelial edges keratinocyte migration.78-80
TABLE 149-4
Common Antiseptics Used in Wound Healing109,110,125,126
ANTISEPTICS MAIN ADVANTAGES MAIN DISADVANTAGES
Iodine Based:
Povidine-iodine 10% ■ Broad spectrum ■ Toxic to granulation tissue in high concentration
■ Cadexomer iodine ■ Good penetration to biofilm ■ Risk of thyroid dysfunction
■ Inadine ■ Proinflammatory ■ Risk of contact dermatitis
Chlorhexidine Based:
■ PHMB (polyhexamethylene ■ Broad spectrum ■ May damage cartilage/ear toxicity
biguanide)—foam, gauze ■ 0.02% concentration use for
wound irrigation
Silver-Based:
■ Microcrystalline silver Antiinflammatory, antibacterial, Silver toxicity, argyria with silver sulfasalazine; silver sulfadiazine +
■ Silver sulfadiazine cream antifungal, antiviral silver nitrate sticks may produce pseudoeschar/delay healing
■ Silver nitrate sticks
Honey-Based:
■ Honey alginate Antiinflammatory, best for hard Risk of botulism; may promote bacterial growth
■ Honey gel adherent eschar
2709
Kang_CH149_p2700-2718.indd 2709 04/12/18 9:35 am
22 TABLE 149-5
Main Categories of Dressings109,110,125,126
DRESSING CATEGORY INGREDIENTS FUNCTION COMMENTS
Hydrogels ■ Polymers with high water content ■ Provide moisture ■ Needs secondary dressings
■ Nonpainful ■ Contraindicated in infected wounds
■ Needs frequent dressing change
Films ■ Semipermeable adhesive sheets of elastic ■ Transparent ■ Adherent (trauma when removed)
polyurethane ■ Nonabsorbent
■ Impermeable to water and bacteria
Hydrocolloids ■ Hydrophilic colloid particles bound to ■ Long wear time ■ Nonabsorptive
polyurethane film ■ Autolytic debridement ■ Trauma with removal
■ Some composed of gelatin, pectin, and ■ Allergy to adhesives
carboxy methylcellulose ■ Smell
Part 22
Calcium alginates ■ Sheets (wick laterally) ■ Hemostatic ■ Need secondary dressing
■ Ropes (wick upward) ■ Absorptive
■ From seaweed-kelp ■ Autolytic debridement
::
Gelling fibers ■ Sheets or ribbons ■ Absorptive ■ Needs secondary dressing
■ Autolytic debridement
Vascular Diseases
Foams ■ Polyurethane foam fluid exchange with ■ Absorbent ■ Bulky and may macerate surround-
partial fluid retention if variable pore size ing skin
Superabsorbent ■ Fiber technology/conducts moisture ■ Absorbent ■ Bulky
dressings ■ Diaper technology
Collagen-based ■ Bovine-derived collagen dressings ■ Promote healing ■ Cost
dressings ■ Reduce matrix
metalloproteinases
example “prewounding” of the donor site skin prior
SKIN GRAFTS to grafting enhances the graft’s ability to stimulate
healing.83,84 Ki67 antibody and β1-integrin expression
Skin grafts are categorized by the amount of tissue after grafting has been noted, as has production of
being grafting. For example, split-thickness grafts stimulatory growth factors and cytokines, implying
include a portion of dermis and full-thickness grafts that healing stimuli were provided by the grafts.85
contain the entire dermis. The likelihood of the survival
and whether wound contracture is reduced depends on
the amount of dermis in the graft. Split-thickness skin
grafts can survive in areas with less vascularity but also
SKIN SUBSTITUTES
are less likely to prevent wound contracture, whereas
full-thickness skin grafts require better vascularity for Skin substitutes are divided into 2 main groups of cel-
survival and but can better prevent contracture. lular and acellular matrix products (Table 149-6).86
While skin grafting is centuries old, modern grafting is
thought to have begun with the first skin autotransplant
done in 1869 by Reverdin and then in 1929 by Brown and
CELLULAR PRODUCTS
colleagues who introduced the technique of the split- The cellular skin substitute products with best avail-
thickness skin graft.81 The healing of a skin graft, how- able evidence are the bilayered living cellular construct
ever, is different from the description provided earlier of (BLCC), Apligraf (Organogenesis, Canton, MA) and
the events after acute injury. One distinguishing feature cellular dermal matrix, Dermagraft (Organogenesis,
of skin graft “take” or healing is the dependence of the Canton, MA). BLCC is a tissue-engineered cellular
graft on the recipient wound bed for revascularization, matrix composed of bovine Type I collage with neo-
which requires several unique physiologic events. natal foreskin fibroblasts for dermal component and
Much of the remainder of skin graft healing involves human neonatal keratinocytes for epidermis.87 BLCC
events in common with the normal wound healing has FDA approval for venous leg ulcers (VLUs) greater
process. Infiltration by fibroblasts in the graft occurs than 4 weeks’ duration and for full-thickness diabetic
3 to 5 days after grafting, followed by a progressive foot ulcers present for longer than 3 weeks. The evi-
increase in both graft and recipient fibroblasts within dence supports the safety and efficacy of up to 5 appli-
the graft.82,83 Although graft “take” allows for donor cations of BLCC. An example of its efficacy is 47% of
tissue to replace missing tissue in the recipient wound, chronic, hard-to-heal VLUs present longer than 1 year
2710 skin grafts may also stimulate wound healing of the treated with BLCC healed after 24 weeks compared to
recipient site, and this ability can be augmented. For 19% in the group with compression alone.88
Kang_CH149_p2700-2718.indd 2710 04/12/18 9:35 am
TABLE 149-6
22
Cellular and Acellular Matrices86
NAMES ADVANTAGE FDA APPROVAL
Cellular Matrices:
Bilayered living cellular construct (Apligraf, Dermal part: Bovine Type I collagen with Noninfected partial- and full-thickness venous
Organogenesis, Canton, MA) human neonatal foreskin fibroblasts leg ulcers, >1 month duration
Epidermal part: keratinocytes Full-thickness diabetic foot ulcers, >3 weeks’
duration
Cellular dermal matrix (Dermagraft, Human neonatal foreskin fibroblasts cultured Full-thickness diabetic foot ulcers >6 weeks’
Organogenesis, Canton, MA) onto a bioresorbable glycolic acid scaffold duration that do not involve tendon, muscle,
(polyglactin 910) joint capsule, or bones
Dehydrated human amnion/chorion DHACM is composed of a single layer of DHACM is composed of a single layer of
Chapter 149 :: Wound Healing
membrane (DHACM) (Epifix, MiMedx Group epithelial cells, a basement membrane, and epithelial cells, a basement membrane, and
Inc., Marietta, GA) an avascular connective tissue matrix an avascular connective tissue matrix
Cryopreserved placental membrane (Grafix, Human viable wound matrix provides the Human viable wound matrix provides the
Osiris Therapeutics, Inc., Columbia, MD) wound with mesenchymal stem cells, wound with mesenchymal stem cells,
neonatal fibroblasts, epithelial cells, growth neonatal fibroblasts, epithelial cells, growth
factors, and angiogenic factors factors, and angiogenic factors
Acellular Matrices:
Dermal regeneration matrix (Integra Dermal Composed of a crosslinked bovine tendon FDA-approved device (510[k] for diabetic foot
Regeneration Template, Integra, Life Sciences, collagen and glycosaminoglycan der- ulcers)
Plainsboro, NJ) mal equivalent, and a semipermeable
polysiloxane (silicone) epidermal equivalent
Porcine small intestinal submucosa (Cook Derived from small intestinal submucosa of FDA-approved 510(k)-cleared medical device
Biotech, West Lafayette, Indiana) porcine; 3-dimensional extracellular matrix
that acts as a scaffold to allow for cellular
migration, formation of granulation tissue,
and vascularization of the wound
Cadaveric allograft (AlloDerm Regenerative Cadaveric human skin that has been processed Regulated by the FDA as human tissue for
Tissue Matrix [RTM], LifeCell, , Branchburg, NJ) to remove the epidermis and cells that lead transplantation
to tissue rejection and graft failure
Poly-N-acetyl glucosamine–derived membrane Composed of poly-N-acetyl glucosamine short- FDA approved—510(k)
(Talymed, Marine Polymer Technologies Inc., ened fibers that are derived from microalgae
Danvers, MA)
Cellular dermal matrix is composed of human neo- regeneration matrix, porcine small intestinal sub-
natal foreskin fibroblasts cultured onto a bioabsorbable mucosa, cadaveric allograft, and poly-N-acetyl
glycolic acid scaffold. The fibroblasts secrete collagen, glucosamine.86
matrix proteins, growth factors, and cytokines. It has INTEGRA Dermal Regeneration Template (Integra
FDA approval for diabetic foot ulcers of longer than LifeSciences Corp.) is a bilayered acellular matrix com-
6 weeks’ duration. posed of crosslinked bovine tendon collagen, a glycos-
Human placental products also are used to speed aminoglycan dermal equivalent, and a semipermeable
healing of chronic wounds. The 2 supported by evi- polysiloxane epidermal equivalent. It is approved for
dence (albeit less robust) include dehydrated human burns and diabetic foot ulcers. In a recent study on
amnion/chorion membrane (Epifix, MiMedx, Marietta, diabetic foot ulcer patients, 51% of patients on Dermal
GA) and cryopreserved placental membrane (Grafix, Regeneration Template achieved complete healing,
Osiris Therapeutics Inc.). Epifix is composed of a sin- compared to 32% of controls.93,94 Porcine small intes-
gle layer of epithelial cells, a basement membrane, and tine submucosa (Oasis, Smith, & Nephew) is a scaffold
a connective tissue matrix. Grafix is composed of pla- for cellular migration, granulation tissue formation
cental membrane, a source of mesenchymal stem cells, and neovascularization. The evidence supports the
neonatal fibroblasts, epithelial cells, growth factors, successful use of small intestine submucosa in patients
and angiogenic cells.89-92 with diabetic foot ulcers and VLUs.95 Cadaveric
allograft is made of cadaveric human skin. It is indi-
ACELLULAR PRODUCTS cated for tissue repair in abdominal wall and breast
reconstruction.96 Poly-N-acetyl glucosamine (Talymed)
Acellular products function as a scaffold for cel- is derived from microalgae and has FDA approval for a
lular migration, proliferation, and matrix forma- variety of wounds. Poly-N-acetyl glucosamine has also
2711
tion. Examples of acellular products include dermal antibacterial properties.97
Kang_CH149_p2700-2718.indd 2711 04/12/18 9:35 am
22 STEM CELL THERAPY
mechanisms or inability to heal readily. Clinically, the
best example of this is the intense fibrosis surround-
ing venous ulcers, as seen in lipodermatosclerosis.107,108
The use of stem cells in the management of wounds Lipodermatosclerosis is a risk factor for ulceration, and
aims to replace the wound resident cells with new venous ulcers surrounded by lipodermatosclerosis are
cells with the potential to respond to wound heal- more difficult to heal.109,110
ing process signals. Numerous animal studies and a Evidence suggests an alteration of the cellular
small number of pilot studies in human have shown makeup of wounds that do not heal. Fibroblasts
that bone marrow mesenchymal cells can promote derived from venous ulcers are unresponsive to cer-
wound healing.98,99 In 2003, freshly applied autologous tain selected cytokines and growth factors.111 For exam-
bone marrow aspirate and cultured bone marrow cells ple, venous ulcer fibroblasts are unresponsive to the
helped 3 wounds heal.100,101 In animal models, the use action of TGF-β1 and PDGF.111,112 The lack of response
of stem cells is associated with healing and increase in to stimuli such as TGF-β1 may be because of decreased
tensile strength. In addition to bone marrow–derived expression of Type II TGF-β receptors. This receptor
Part 22
cells, other sources of stem cells, such as fat and hair abnormality also leads to decreased phosphorylation
follicles, may be beneficial.98 of key TGF-β signaling proteins, including Smad2,
However, most studies of adult stem cell therapy Smad3, and mitogen-activated protein kinases.113 Cells
for human wounds have used cultured bone marrow– in diabetic ulcers are altered, such that chronic wounds
::
derived mesenchymal stem cells.102 The improvement of are said to be “stuck” in a certain phases of the repair
Vascular Diseases
wounds with adult stem cells may be a result of either process.114 An association has been reported between
integration of the stem cells or their paracrine effects.103 some of these cellular alterations and the inability to
Topically applied autologous mesenchymal stem cells heal.115,116
accelerate the healing of human and murine wounds.104
The first randomized, controlled trial reported the use
of bone marrow mesenchymal stem cell application via
IM and subcutaneous injection to chronic nonhealing AGE-RELATED CHANGES IN
wounds with success compared to standard care.105
WOUND HEALING
The population is aging, and older adults are more
prone to develop all type of wounds, including VLUs,
CHRONIC WOUNDS AND arterial ulcers, and pressure ulcers. For both acute
IMPAIRED HEALING and chronic wounds, aging is associated with delayed
healing. The healing response by ECM changes
throughout life.117 Overexpression of MMPs has been
Acute wounds, such as those created by surgery or
shown in elderly skin.117 The vasoregulation in aged
by trauma, have a predictable time-frame for healing
skin includes fewer progenitor cells, impaired per-
and generally heal quite readily when not interrupted.
fusion and changes in temperature regulation. Age-
Impaired healing in chronic wounds may be a conse-
associated aberrations in macrophage function delay
quence of many factors.
vascularization, collagen formation, and remodeling.
Some chronic wounds are the result of ischemia,
Mitochondrial dysfunction and lower levels of anti-
pressure, and infection or a combination, thereof.26
oxidants also are associated with aging. Comorbidities
There is still considerable controversy whether hyper-
and polypharmacy may also factor into delayed heal-
glycemia itself plays a pathophysiologic role in the
ing in the elderly population.118-120
development of ulcers in patients with diabetes mel-
litus, although neutrophil function is impaired in this
setting, and the propensity to infection is enhanced in
the diabetic state.26 Importantly, the notion of “small
vessel disease” in diabetes mellitus has not been
BASIC STANDARDS OF
shown to be an obstructive phenomenon. Revascular- WOUND CARE
ization of the diabetic foot is now viewed as standard
care in the presence of large vessel disease and good Reversing or treating the underlying cause of impaired
run-off circulation. healing is the focus of wound care treatment. Treat-
Perhaps the best example of truly impaired healing, ment relies in part on wound etiology. A thorough
not related to undue pressure and poor arterial sup- history and examination, along with adjunctive diag-
ply, is venous ulceration. The underlying abnormality nostic tests, such as wound biopsy, vascular studies,
in the development of venous ulcers is the presence of imaging, tissue culture, and laboratory analysis may
sustained ambulatory venous pressure, also known help with diagnosis.121,122 The most common lower
as venous hypertension, which refers to the inability extremity ulcers are venous, diabetic, and arterial
of venous pressure in the leg and feet to decrease in ulcers. Chronic wounds are common. VLUs have a 2%
response to exercise.106 It should also be recognized prevalence in developed countries, and diabetic foot
2712 that the tissue surrounding chronic wounds is not nor- ulcers occur in 1 in 4 patients with diabetes mellitus
mal and has been altered by the primary pathogenic over their lifetime.17,123,124
Kang_CH149_p2700-2718.indd 2712 04/12/18 9:35 am
Using VLUs as an example, the fundamental of
treatment is compression therapy with adjunctive
in terms of improving the fundamentals of care in
limited-resource countries, as well as research gaps in
22
medical and surgical therapies.109,110,125,126 With regard smart biologic dressings, bioengineered skin, and stem
to medical therapy, pentoxifylline has been tested in cell therapy. We need continued and increased under-
several large randomized trials for its ability to acceler- standing of the science involved. It is also possible
ate the healing of venous ulcers. The results have var- that lessons learned from failure to heal, as in chronic
ied, and it may be that a high dose of pentoxifylline, wounds, will provide valuable lessons for the general
800 mg 3 times a day, is more effective than 400 mg principles of surgical and acute wound healing.
3 times a day.127 Whether the use of pentoxifylline
should be considered standard therapy for venous
ulcers is unclear at the moment. The anabolic steroid
stanozolol has been effective in diminishing the indu- REFERENCES
ration of lipodermatosclerosis, and in the acute and
painful phase of lipodermatosclerosis, when compres- 1. Enoch S, Leaper DJ. Basic science of wound healing.
Surgery (Oxford). 2008;26:31-37.
Chapter 149 :: Wound Healing
sion bandages and stockings are too painful to use.128
Danazol may be a useful substitute for stanozolol if 2. Li J, Chen J, Kirsner R. Pathophysiology of acute
wound healing. Clin Dermatol. 2007;25:9-18.
it is not available. Recent studies show an effect of
3. Kirsner RS, Eaglstein WH. The wound healing process.
statins in the healing of VLUs (and possibly diabetic Dermatol Clin. 1993;11:629-640.
foot ulcers).129,130 The only known medical approach 4. Nosbaum A, Prevel N, Truong HA, et al. Cutting edge:
for decreasing recurrence of venous ulcers seems to be regulatory T cells facilitate cutaneous wound healing.
graded elastic stockings, with a pressure at the ankle J Immunol. 2016;196(5):2010-2014.
in the range of 40 mm Hg along. Surgical therapy is an 5. Vatankhah N, Jahangiri Y, Landry GJ, et al. Predictive
adjunct, if indicated. Stockings should be considered a value of neutrophil-to-lymphocyte ratio in diabetic
lifelong therapy to help prevent ulcer recurrence and wound healing. J Vasc Surg. 2017;65(2):478-483.
the other manifestations of venous disease. 6. Xue M, Le NT, Jackson CJ. Targeting matrix metal-
loproteases to improve cutaneous wound healing.
Expert Opin Ther Targets. 2006;10:143-155.
7. Werner S, Grose R. Regulation of wound healing by
PREDICTING WOUND growth factors and cytokines. Physiol Rev. 2003;83:
835-870.
CLOSURE 8. Patel S, Maheshwari A, Chandra A. Biomarkers for
wound healing and their evaluation. J Wound Care.
Several recent studies now allow the prediction of 2016;25:46-55.
9. Golebiewska EM, Poole AW. Platelet secretion: From
whether a wound will heal in a timely fashion from
haemostasis to wound healing and beyond. Blood
simple observation in the first 3 to 4 weeks of therapy. Rev. 2015;29:153-162.
The methods used to predict wound closure range 10. Leaper D. Perfusion, oxygenation and warming. Int
from simple measurements of wound size (width and Wound J. 2007;4(suppl 3):4-8.
length) and change in wound area, to computerized 11. Ramasastry SS. Acute wounds. Clin Plast Surg. 2005;
planimetric analysis and assessment of migration of 32:195-208.
the wound edge.131 In a study of 56,488 wounds, it was 12. Rothwell SW, Sawyer E, Dorsey J, et al. Wound heal-
shown that a percent change of approximately 30% at ing and the immune response in swine treated
4 weeks could predict wound closure with a sensitivity with a hemostatic bandage composed of salmon
of 0.67, a specificity of 0.69, and had a positive and neg- thrombin and fibrinogen. J Mater Sci Mater Med.
2009;20:2155-2166.
ative predictive value of 0.80 and 0.52, respectively.132
13. Frechette JP, Martineau I, Gagnon G. Platelet-rich
In practical terms, the appearance of the wound plasmas: growth factor content and roles in wound
edge is important. Steep edges imply no progress healing. J Dent Res. 2005;84:434-439.
of the wound, while the edges of healing wounds 14. Martin P, Leibovich SJ. Inflammatory cells during
become less steep and begin to migrate toward the wound repair: the good, the bad and the ugly. Trends
center. The implications of the ability to predict Cell Biol. 2005;15:599-607.
closure are very important. By 4 weeks, the clinician 15. Baum CL, Arpey CJ. Normal cutaneous wound heal-
should be able to determine whether the current ing: clinical correlation with cellular and molecular
therapy should be continued or whether a change events. Dermatol Surg. 2005;31:674-686; discussion
is required, including a complete reassessment of the 686.
16. Pull SL, Doherty JM, Mills JC, et al. Activated mac-
clinical situation. The prognostic value of the healing
rophages are an adaptive element of the colonic
rate by 4 weeks of therapy has been confirmed.132,133 epithelial progenitor niche necessary for regen-
erative responses to injury. Proc Natl Acad Sci U S A.
2005;102:99-104.
CONCLUSIONS 17. Snyder RJ, Lantis J, Kirsner RS, et al. Macrophages: a
review of their role in wound healing and their thera-
Wound healing is a complex process of overlapping peutic use. Wound Repair Regen. 2016;24:613-629.
phases of inflammation, proliferation and remodel- 18. Pradhan L, Cai X, Wu S, et al. Gene expression of
ing. The burden of wounds on millions of people is pro-inflammatory cytokines and neuropeptides in 2713
globally underappreciated. There are still challenges, diabetic wound healing. J Surg Res. 2011;167:336-342.
Kang_CH149_p2700-2718.indd 2713 04/12/18 9:35 am
You might also like
- Gastrointestinal Physiology LANGEDocument281 pagesGastrointestinal Physiology LANGEUlquiorra Schiffer100% (4)
- Treatment Strategy For Nonunions and MalunionsDocument25 pagesTreatment Strategy For Nonunions and MalunionsAnisa AnisatusholihahNo ratings yet
- The Physiology of Guitar Playing - IznaolaDocument37 pagesThe Physiology of Guitar Playing - Iznaolajduque825504380% (5)
- Medpox RecallsDocument8 pagesMedpox RecallsmedpoxNo ratings yet
- Ergonomics in Dentistry: By, DR - Rakesh R Nair P.G Student Cons & Endo KVG Dental CollegeDocument94 pagesErgonomics in Dentistry: By, DR - Rakesh R Nair P.G Student Cons & Endo KVG Dental Collegenur awanisNo ratings yet
- Wound Bed PreparationDocument24 pagesWound Bed PreparationnudiaNo ratings yet
- Angiogenesis With Wound HealingDocument36 pagesAngiogenesis With Wound HealingHemant Gupta100% (1)
- Manajemen LukaDocument50 pagesManajemen LukaindraNo ratings yet
- Chronic Wound ManagementDocument31 pagesChronic Wound Managementadrianus andriNo ratings yet
- Basinga Idys C ZPDocument26 pagesBasinga Idys C ZPruiduartNo ratings yet
- Webinar Perawatan Luka Dan Tata Laksana Pemeriksaan InfeksiDocument41 pagesWebinar Perawatan Luka Dan Tata Laksana Pemeriksaan Infeksiqoote3No ratings yet
- Annals of SurgeryDocument12 pagesAnnals of SurgeryNada GhammemNo ratings yet
- Brand Guidelines - GOJEKDocument39 pagesBrand Guidelines - GOJEKGM ProNo ratings yet
- Soft - Tissue 4.1.0.0.REL CAPCPDocument21 pagesSoft - Tissue 4.1.0.0.REL CAPCPaNo ratings yet
- (Upgraded) Damage Control Orthopaedics DR Bambang SpOTDocument37 pages(Upgraded) Damage Control Orthopaedics DR Bambang SpOTroroNo ratings yet
- 02 TissueDocument26 pages02 Tissuecow dasNo ratings yet
- Intraoperative Posterior Polar Cortical Disc.Document5 pagesIntraoperative Posterior Polar Cortical Disc.Danty IndriastutyNo ratings yet
- 3-3 No Antibiotic in Hand InfectionDocument26 pages3-3 No Antibiotic in Hand InfectionProfesseur Christian DumontierNo ratings yet
- Pediatric Neuroanesthesia.3Document4 pagesPediatric Neuroanesthesia.3Mae Importers IncNo ratings yet
- Silver Sulfadiazine For Treatment of Burns and Wounds PDFDocument7 pagesSilver Sulfadiazine For Treatment of Burns and Wounds PDFprakas.rao39695No ratings yet
- Facial LacerationsDocument50 pagesFacial LacerationssevattapillaiNo ratings yet
- Evaluacion Inicial Del Paciente QuemadoDocument12 pagesEvaluacion Inicial Del Paciente QuemadoRyan BNo ratings yet
- AWMA 2011 Standards For Wound Management v2Document36 pagesAWMA 2011 Standards For Wound Management v2Agung Ginanjar100% (1)
- Flaps Cadaver Dissection RMESDocument124 pagesFlaps Cadaver Dissection RMESTeo ChreliasNo ratings yet
- Anatomy & Function of The SkinDocument9 pagesAnatomy & Function of The Skinعبدالعزيز احمد علي عتشNo ratings yet
- Shanz - Ent 1.06 Facial Nerve and Traumatic Facial ParalysisDocument3 pagesShanz - Ent 1.06 Facial Nerve and Traumatic Facial ParalysisPetrina XuNo ratings yet
- Arcuate-Lines - Hernia MagazineDocument24 pagesArcuate-Lines - Hernia MagazineSAURIN CHAUDHARYNo ratings yet
- Gen Surgery EssaysDocument161 pagesGen Surgery EssaysВлади ПетковNo ratings yet
- Mindray iMEC12 SpecsDocument6 pagesMindray iMEC12 SpecsJose Ivan Carvajal CortizosNo ratings yet
- Modul Otologi Gangguan Nervus FasialisDocument65 pagesModul Otologi Gangguan Nervus FasialisHERIZALNo ratings yet
- Controlling Nasal Tip Projection and Rotation With.16Document10 pagesControlling Nasal Tip Projection and Rotation With.16AdRiaNa JuLIetH LoZaDa PaTiÑoNo ratings yet
- Splinting Techniques: by Madhumitha M, Aruna G, Abi P, Sakthivelayudham G, Sujidha R, Srivignesh MDocument99 pagesSplinting Techniques: by Madhumitha M, Aruna G, Abi P, Sakthivelayudham G, Sujidha R, Srivignesh MSakthivelayudhamganesanNo ratings yet
- A Review of Wound Dressing PracticesDocument13 pagesA Review of Wound Dressing PracticesAnonymous 1nMTZWmzNo ratings yet
- Brar, Nicol, Boguniewicz - 2019 - Strategies For Successful Management of Severe Atopic DermatitisDocument16 pagesBrar, Nicol, Boguniewicz - 2019 - Strategies For Successful Management of Severe Atopic DermatitisFranciscoNo ratings yet
- Dengue Insight DR Amit Johari Edited 2020Document82 pagesDengue Insight DR Amit Johari Edited 2020Vedehi BansalNo ratings yet
- Anatomy of The EarDocument63 pagesAnatomy of The EargabrielNo ratings yet
- Fracture and Dislocation-Rahardyan Magetsari (2016) PDFDocument105 pagesFracture and Dislocation-Rahardyan Magetsari (2016) PDFRobertOktaChandraNo ratings yet
- TIME METHOD For WOUND ASSESSMENT (OSCE)Document1 pageTIME METHOD For WOUND ASSESSMENT (OSCE)S. CapanateraisoNo ratings yet
- 3.wound ClassificationDocument7 pages3.wound ClassificationFabi Samad0% (1)
- Pressure Ulcer Prevention & Management: Wocare ClinicDocument20 pagesPressure Ulcer Prevention & Management: Wocare ClinicShoahir RustanNo ratings yet
- 3 Soft Tissue Injury HabtamuDocument80 pages3 Soft Tissue Injury HabtamuWasihunNo ratings yet
- Rekapitulasi Bimbingan DisertasiDocument52 pagesRekapitulasi Bimbingan DisertasiAnnisa NovitaNo ratings yet
- Surgery FinalDocument70 pagesSurgery FinalIris BakerNo ratings yet
- Instruction Manual ECP-TIDocument35 pagesInstruction Manual ECP-TIBryanJermyHendrik100% (1)
- EYE Histology: Dr. OkoloDocument60 pagesEYE Histology: Dr. OkoloAbiola NerdNo ratings yet
- Surgical Access IncisionsDocument7 pagesSurgical Access IncisionsFiliberto RiosNo ratings yet
- 3 - Right Heart AssessmentDocument47 pages3 - Right Heart Assessmentpatricia wageyNo ratings yet
- Review Hemostatic DressingsDocument21 pagesReview Hemostatic DressingsJean Cotte100% (1)
- FinalDocument39 pagesFinalAmeerNo ratings yet
- Parkland Trauma Soft TissueDocument14 pagesParkland Trauma Soft TissueJulieNo ratings yet
- EktremitasDocument40 pagesEktremitasBram wijayaNo ratings yet
- BeauiPHIcation Global ApproachDocument31 pagesBeauiPHIcation Global ApproachKentVilandkaNo ratings yet
- A AaaaaaaDocument6 pagesA AaaaaaaAnonymous d9Bzr1No ratings yet
- Abstracts From The Global Embolization Sympo 2021 Journal of Vascular and inDocument21 pagesAbstracts From The Global Embolization Sympo 2021 Journal of Vascular and infreedy freedyNo ratings yet
- Modern Wound Care - Lohmann & RauscherDocument18 pagesModern Wound Care - Lohmann & Rauschersins1984No ratings yet
- Macrophage ICDocument10 pagesMacrophage ICchristian lunaNo ratings yet
- Class Ii Lower Premolar Mod Amalgam Preparation & RestorationDocument4 pagesClass Ii Lower Premolar Mod Amalgam Preparation & RestorationKizzy SarriaNo ratings yet
- Imaging in Oral Cancers: Ead and Eck YmposiumDocument14 pagesImaging in Oral Cancers: Ead and Eck YmposiumHayyu F RachmadhanNo ratings yet
- 1987 Haapasalo, M., & Ørstavik, D. (1987) - in Vitro Infection and of Dentinal Tubules. Journal of Dental ResearchDocument5 pages1987 Haapasalo, M., & Ørstavik, D. (1987) - in Vitro Infection and of Dentinal Tubules. Journal of Dental ResearchAlexandra Illescas GómezNo ratings yet
- Unit IV A. Physical AssessmentDocument129 pagesUnit IV A. Physical AssessmentGadez JeanpelNo ratings yet
- Management of Dengue FeverDocument31 pagesManagement of Dengue FeverDaniel RajNo ratings yet
- Auric Recon Slides 070516Document92 pagesAuric Recon Slides 070516Yudhistira AdeNo ratings yet
- Bovine Surger y of The Skin: Matt D. MiesnerDocument10 pagesBovine Surger y of The Skin: Matt D. MiesnerGuadalupe Cristina Chuchón CáceresNo ratings yet
- Active Isolated Stretching The Mattes Method 151 184Document38 pagesActive Isolated Stretching The Mattes Method 151 184Nazareth Varas AlonsoNo ratings yet
- Neurological Disorders MCQSDocument78 pagesNeurological Disorders MCQSninestar102100% (3)
- Staging of Bladder Cancer: ReviewDocument23 pagesStaging of Bladder Cancer: ReviewIsabel Gago CastilloNo ratings yet
- Medical Examiner InvestigationDocument11 pagesMedical Examiner InvestigationColleen WelcherNo ratings yet
- CBSE Class 9 Science NCERT Exemplar Solutions Chapter - 6 TissueDocument6 pagesCBSE Class 9 Science NCERT Exemplar Solutions Chapter - 6 TissueNaliniKumaresanNo ratings yet
- Module 2 The Human Reproductive Anatomy and PhysiologyDocument27 pagesModule 2 The Human Reproductive Anatomy and PhysiologyJhunna Talangan100% (1)
- WebpdfDocument233 pagesWebpdfapuntesjmznNo ratings yet
- District: Rajkot Name of Institute: P.D.U. Medical CollegeDocument9 pagesDistrict: Rajkot Name of Institute: P.D.U. Medical CollegeManas K. TrivediNo ratings yet
- Connective Tissue ImagesDocument54 pagesConnective Tissue ImagesSaaraAlleyahAlAnaziNo ratings yet
- Solution Manual For Human Anatomy Laboratory Manual With Cat Dissections 7 e 7th EditionDocument36 pagesSolution Manual For Human Anatomy Laboratory Manual With Cat Dissections 7 e 7th Editionfingrigoasperxwq6100% (35)
- Latihan F4 KSSM 3Document7 pagesLatihan F4 KSSM 3Hamirah Abd HamidNo ratings yet
- 1971 Albus - A Theory of Cerebellar FunctionDocument37 pages1971 Albus - A Theory of Cerebellar FunctionmarkmcwilliamsNo ratings yet
- IGCSE-Revision-Booklet-Part-1-2018-2019 - (New-Spec)Document69 pagesIGCSE-Revision-Booklet-Part-1-2018-2019 - (New-Spec)MaryamNo ratings yet
- Topic 5 - The Uptake and Transport of Water and MineralsDocument32 pagesTopic 5 - The Uptake and Transport of Water and MineralsAshley BedassieNo ratings yet
- 3rd Week of DevelopmentDocument20 pages3rd Week of DevelopmentSidra AslamNo ratings yet
- Plant and Animal Cell WebquestDocument3 pagesPlant and Animal Cell Webquestapi-3133243170% (3)
- GYN - Development of Sexual Organ and SexualityDocument38 pagesGYN - Development of Sexual Organ and SexualityEsha KuttiNo ratings yet
- Bachelors of Physiotherapy Syllabus-1Document98 pagesBachelors of Physiotherapy Syllabus-1golagani praveenkumarNo ratings yet
- Children: The Respiratory Management of The Extreme Preterm in The Delivery RoomDocument21 pagesChildren: The Respiratory Management of The Extreme Preterm in The Delivery RoomRhea Kathleen MejiaNo ratings yet
- Biology Form 3 Reproduction in Plants and Animals - Knec Study Materials, RevisDocument25 pagesBiology Form 3 Reproduction in Plants and Animals - Knec Study Materials, Reviskiraguripeter1994No ratings yet
- Rapid Pathology Pathology Textbook For Medical StudentsDocument89 pagesRapid Pathology Pathology Textbook For Medical Studentsyennqing100% (1)
- Anatomy Compilation of Past PapersDocument162 pagesAnatomy Compilation of Past Papers2803214No ratings yet
- Year 7 Cells and Reproduction - Mark SchemeDocument4 pagesYear 7 Cells and Reproduction - Mark SchemeAnonymous tc7XPINo ratings yet
- TL Gonzalez Sala ValeriaDocument26 pagesTL Gonzalez Sala ValeriagloriaNo ratings yet
- Notes of Human Physiology Class 11Document9 pagesNotes of Human Physiology Class 11ADWAITH LALU100% (1)
- The Study of Biology As The Science of LifeDocument33 pagesThe Study of Biology As The Science of LifeClyde PreciadoNo ratings yet
- Accounting Information Systems Understanding Business Processes 5th Edition Parkes Solutions ManualDocument26 pagesAccounting Information Systems Understanding Business Processes 5th Edition Parkes Solutions ManualKimberlyMendezyptr100% (50)