Professional Documents
Culture Documents
The Following Resources Related To This Article Are Available Online at
The Following Resources Related To This Article Are Available Online at
Uploaded by
Verghese George MCopyright:
Available Formats
You might also like
- 500 Feedback Questions Bank PDFDocument40 pages500 Feedback Questions Bank PDFmariyam hasnainNo ratings yet
- National Board Questions Pediatric DentistryDocument50 pagesNational Board Questions Pediatric DentistryVerghese George MNo ratings yet
- Adhesive Restoration of Endodontically Treated TeethFrom EverandAdhesive Restoration of Endodontically Treated TeethRating: 3 out of 5 stars3/5 (2)
- Adc MCQ Sep 2006 Paper1Document28 pagesAdc MCQ Sep 2006 Paper1api-2629165189% (19)
- 1 - Ahmed Sle MCQ EndoDocument29 pages1 - Ahmed Sle MCQ EndoShabana Serju82% (17)
- Prometric Questions 20014Document100 pagesPrometric Questions 20014aliakdr3414100% (1)
- Interdisciplinary Approach in Periodontal TherapyDocument100 pagesInterdisciplinary Approach in Periodontal Therapypoojawadkar92% (13)
- Mineral Trioxide Aggregate Pulpotomies: A Case Series Outcomes AssessmentDocument9 pagesMineral Trioxide Aggregate Pulpotomies: A Case Series Outcomes AssessmentWidya JuliantiNo ratings yet
- The Purpose of Calcium Hydroxide in Root Canal TreatmentDocument4 pagesThe Purpose of Calcium Hydroxide in Root Canal TreatmentIJRASETPublicationsNo ratings yet
- Calcium HydroxideDocument12 pagesCalcium HydroxideKarina KariadiNo ratings yet
- Materials 13 02670 v2Document42 pagesMaterials 13 02670 v2Jose Manuel Quintero RomeroNo ratings yet
- Comparative Study of Efficacy of Formocresol and Calcium Hydroxide Pulpotomy in Primary MolarsDocument15 pagesComparative Study of Efficacy of Formocresol and Calcium Hydroxide Pulpotomy in Primary MolarsPipin HeryantoNo ratings yet
- P Esker Soy 2020Document9 pagesP Esker Soy 2020Gawi ChangNo ratings yet
- Apexification With Calcium Hydroxide and Mineral Trioxide AggregateDocument5 pagesApexification With Calcium Hydroxide and Mineral Trioxide AggregateTalitha NabilaNo ratings yet
- Liners & Bases in DentistryDocument12 pagesLiners & Bases in Dentistryjawaad293No ratings yet
- Artigo 11 Jeeruphan, 2012Document7 pagesArtigo 11 Jeeruphan, 2012damacenobpmNo ratings yet
- Journal of Oral Biology and Craniofacial ResearchDocument9 pagesJournal of Oral Biology and Craniofacial ResearchCyber MagicNo ratings yet
- Apexogenesis of A Symptomatic MolarDocument5 pagesApexogenesis of A Symptomatic MolarFoysal SirazeeNo ratings yet
- El MeligyDocument7 pagesEl Meligysystematic reviewNo ratings yet
- Management of Open ApexDocument7 pagesManagement of Open ApexMineet KaulNo ratings yet
- Calcium Hydroxide-Induced Resorption of Deciduous Teeth - A Possible ExplanationDocument5 pagesCalcium Hydroxide-Induced Resorption of Deciduous Teeth - A Possible ExplanationAhmad AssariNo ratings yet
- Content ServerDocument6 pagesContent Serveranon_688123777No ratings yet
- The Effect of Long-Term Dressing With CalciumDocument6 pagesThe Effect of Long-Term Dressing With CalciumArturo Trejo VeraNo ratings yet
- Intracanal Medicament and ResilonDocument5 pagesIntracanal Medicament and ResilonLuLu NikhlaturNo ratings yet
- Apexification With Mineral Trioxide Aggregate: An Overview of The Material and TechniqueDocument5 pagesApexification With Mineral Trioxide Aggregate: An Overview of The Material and Techniquedrvivek reddyNo ratings yet
- Int Endodontic J - 2016 - Galler - European Society of Endodontology Position Statement Revitalization ProceduresDocument7 pagesInt Endodontic J - 2016 - Galler - European Society of Endodontology Position Statement Revitalization ProceduresShivangiJainNo ratings yet
- ReviewsDocument6 pagesReviewsDenisa BlažekNo ratings yet
- Cytotoxicity and Bioactivity of Dental Pulp-Capping (Pedano) (2020)Document16 pagesCytotoxicity and Bioactivity of Dental Pulp-Capping (Pedano) (2020)juan salazarNo ratings yet
- Remineralization of TeethDocument37 pagesRemineralization of TeethPrajakta ChavanNo ratings yet
- Calcium Hydroxide - A Great Calcific WallDocument5 pagesCalcium Hydroxide - A Great Calcific WallAki AvlonNo ratings yet
- Australian Dental Journal: Liners and Bases in General DentistryDocument13 pagesAustralian Dental Journal: Liners and Bases in General DentistryAngela Gissela Moncada BoulanggerNo ratings yet
- Jurnal 2 IKGADocument13 pagesJurnal 2 IKGAekaapriany45No ratings yet
- Case Study Vital Pulp Therapy 5Document1 pageCase Study Vital Pulp Therapy 5chen danielNo ratings yet
- Ridge Preservation Using Composite AlloplasticDocument8 pagesRidge Preservation Using Composite Alloplasticarun perioNo ratings yet
- Carrier-Based Root Canal Filling Materials A Literature ReviewDocument7 pagesCarrier-Based Root Canal Filling Materials A Literature ReviewMegha GhoshNo ratings yet
- Calcium Sulfate in Implantology Biphasic Calcium SDocument24 pagesCalcium Sulfate in Implantology Biphasic Calcium Smarco.cedilloNo ratings yet
- Condezo 2020Document9 pagesCondezo 2020Rafael Zetehaku AraujoNo ratings yet
- Endodontics and Pulp Biology: The Impact Clinically: Rci Icw IclcDocument4 pagesEndodontics and Pulp Biology: The Impact Clinically: Rci Icw IclcdrashotiNo ratings yet
- Traditional and Contemporary Techniques For Optimizing Root Canal IrrigationDocument9 pagesTraditional and Contemporary Techniques For Optimizing Root Canal IrrigationrintanfsNo ratings yet
- Jur Endo 11Document8 pagesJur Endo 11Fadli FadelNo ratings yet
- 12 Shikha Dorgra DentalDocument4 pages12 Shikha Dorgra DentalHarish ChowdaryNo ratings yet
- IEJ - Revitalization in EndodonticsDocument7 pagesIEJ - Revitalization in Endodonticssoho1303No ratings yet
- Iej 10 2009Document100 pagesIej 10 2009Israel CurveloNo ratings yet
- Removal Efficacy of Propoliscalcium Hydroxide MediDocument6 pagesRemoval Efficacy of Propoliscalcium Hydroxide Medifelipe martinezNo ratings yet
- KokichDocument2 pagesKokichFederico LisiNo ratings yet
- Vital Pulp Therapy For The Mature Tooth Can It WorkDocument8 pagesVital Pulp Therapy For The Mature Tooth Can It WorkRamona MateiNo ratings yet
- Apexification Using Different Approaches - Case Series Report With A Brief Literature ReviewDocument12 pagesApexification Using Different Approaches - Case Series Report With A Brief Literature ReviewIJAR JOURNALNo ratings yet
- Cytotoxicity and Genotoxicity of Newly Developed Calcium Phosphate-Based Root Canal SealersDocument14 pagesCytotoxicity and Genotoxicity of Newly Developed Calcium Phosphate-Based Root Canal SealersNunoGonçalvesNo ratings yet
- What Leave Behind in Canals Endodontic Treatment: Issues and ConcernsDocument7 pagesWhat Leave Behind in Canals Endodontic Treatment: Issues and ConcernsSitiKhadijahNo ratings yet
- In Vitro Cytotoxicity of Calcium Silicate-Contain - Endodontic Sealers - Joe 20015Document7 pagesIn Vitro Cytotoxicity of Calcium Silicate-Contain - Endodontic Sealers - Joe 20015Andrea UrgilesNo ratings yet
- Endodontology 1: RootsDocument44 pagesEndodontology 1: RootsCarlos San Martin100% (1)
- Chou2018-The Effect of Plasma Treatment On The Osseointegration of Rough Titanium Implant A Histo-Morphometric Study in RabbitsDocument7 pagesChou2018-The Effect of Plasma Treatment On The Osseointegration of Rough Titanium Implant A Histo-Morphometric Study in RabbitsYohann GNo ratings yet
- Overview of Bleaching TechniquesDocument7 pagesOverview of Bleaching TechniquesAnonymous WtgTCQJdNNo ratings yet
- Posterior Composite Restoration UpdateDocument10 pagesPosterior Composite Restoration UpdateBianca IovoaiaNo ratings yet
- Scopeofendo RegendoDocument2 pagesScopeofendo Regendosalman azizNo ratings yet
- Avulsions and Intrusions: The Controversial Displacement InjuriesDocument7 pagesAvulsions and Intrusions: The Controversial Displacement InjuriessaeedrahmaniNo ratings yet
- Int J of Pediatric Dent 2Document107 pagesInt J of Pediatric Dent 2Diana DrutaNo ratings yet
- WhiteandElezar CaOHweakeningdentinDocument3 pagesWhiteandElezar CaOHweakeningdentinJigar M. UpadhyayNo ratings yet
- Galler Et Al-2016-International Endodontic JournalDocument7 pagesGaller Et Al-2016-International Endodontic JournalMaja Maja BułkaNo ratings yet
- 10 4 2013Document49 pages10 4 2013Anonymous 2h5lIeNo ratings yet
- Bioactive Glass Nanoparticles (NovaMin®) For Applications in DentistryDocument6 pagesBioactive Glass Nanoparticles (NovaMin®) For Applications in DentistryIOSRjournalNo ratings yet
- Direct Pulp CapDocument3 pagesDirect Pulp CapMelliya heptaniaNo ratings yet
- JCM 10 01600 v2Document17 pagesJCM 10 01600 v2ShivangiJainNo ratings yet
- 2 PBDocument6 pages2 PBMenna SalemNo ratings yet
- Response of Human Dental Pulp Capped With Biodentine and Mta Nowicka 1Document5 pagesResponse of Human Dental Pulp Capped With Biodentine and Mta Nowicka 1Adriiana Jaimes JaimesNo ratings yet
- An Evaluation of Ethical Aspects Concerning Endodontic Instrument FractureDocument4 pagesAn Evaluation of Ethical Aspects Concerning Endodontic Instrument FractureVerghese George MNo ratings yet
- The Role of Nurses in The Resuscitation of In-Hospital Cardiac ArrestsDocument5 pagesThe Role of Nurses in The Resuscitation of In-Hospital Cardiac ArrestsVerghese George MNo ratings yet
- 2006-2007 Dental Decks PDFDocument625 pages2006-2007 Dental Decks PDFVerghese George MNo ratings yet
- LightspeedDocument8 pagesLightspeedVerghese George MNo ratings yet
- Pharmacology For Dentistry PDFDocument501 pagesPharmacology For Dentistry PDFOfier SikiNo ratings yet
- Straight Line AccessDocument9 pagesStraight Line AccessVerghese George MNo ratings yet
- Cracked Tooth Syndrome-Decoding The EnigmaDocument3 pagesCracked Tooth Syndrome-Decoding The EnigmaVerghese George MNo ratings yet
- KrasnerandRankowJOE2004 PDFDocument12 pagesKrasnerandRankowJOE2004 PDFVerghese George MNo ratings yet
- Splinting MaterialsDocument1 pageSplinting MaterialsVerghese George MNo ratings yet
- 10 Besar 1 TH 2017Document356 pages10 Besar 1 TH 2017dartosNo ratings yet
- Vital Pulp Therapy 1Document6 pagesVital Pulp Therapy 1Mostafa Afifi Ali100% (1)
- Newapproachestopain Management: Orrett E. OgleDocument10 pagesNewapproachestopain Management: Orrett E. OgleNajeeb UllahNo ratings yet
- Pulpal DiagnosisDocument14 pagesPulpal DiagnosisSimina LungociNo ratings yet
- SRMJResDentSci73158-2129782 003529Document4 pagesSRMJResDentSci73158-2129782 003529MarsyaNo ratings yet
- Essentials of Endodontics 2Nd Edition Vimal K Sikri Online Ebook Texxtbook Full Chapter PDFDocument69 pagesEssentials of Endodontics 2Nd Edition Vimal K Sikri Online Ebook Texxtbook Full Chapter PDFjames.mozak676100% (11)
- Pulp Therapy For Primary TeethDocument14 pagesPulp Therapy For Primary TeethMahmoudFayedNo ratings yet
- Past Papers 1 200Document55 pagesPast Papers 1 200AmarAldujaili100% (1)
- Endodontics Key Points by DaneshDocument16 pagesEndodontics Key Points by DaneshNoor HaiderNo ratings yet
- Interstitial Fluid Pressure Normal Inflamed PulpDocument9 pagesInterstitial Fluid Pressure Normal Inflamed PulpAbeerNo ratings yet
- Endodontic Mcqs - DocShare - Tips 2Document1 pageEndodontic Mcqs - DocShare - Tips 2Stela NichevaNo ratings yet
- SOCA Blok 12Document21 pagesSOCA Blok 12safiraNo ratings yet
- Dental Caries - Its Sequelae and Treatment Among Patients in A Tertiary Hospital in North-Western Nigeria-A Retrospective StudyDocument7 pagesDental Caries - Its Sequelae and Treatment Among Patients in A Tertiary Hospital in North-Western Nigeria-A Retrospective Studyabdurrazaq taiwoNo ratings yet
- Common Causes of Dental Pain in Children (Differential Diagnosis)Document21 pagesCommon Causes of Dental Pain in Children (Differential Diagnosis)jamie chewNo ratings yet
- Clinical and Radiographic Evaluation of Pulpal and Periradicular TissueDocument6 pagesClinical and Radiographic Evaluation of Pulpal and Periradicular TissueMónïcå Lÿdïå RómåúlïèNo ratings yet
- Endodontics Key Points by DaneshDocument6 pagesEndodontics Key Points by DaneshDanesh KumarNo ratings yet
- Osteomyelitis: Deo Jake Lacpacan Jhunevyl MallorcaDocument36 pagesOsteomyelitis: Deo Jake Lacpacan Jhunevyl MallorcaDeo Jake Lacpacan100% (1)
- DR - Ritty Arouje Recent Question Paper FileDocument118 pagesDR - Ritty Arouje Recent Question Paper Filemuneer024No ratings yet
- 322 RDS Pre-Clinical EndodonticsDocument6 pages322 RDS Pre-Clinical EndodonticsHadil AltilbaniNo ratings yet
- Atypical Developmental Defects of Enamel in Primary Incisors Versus Preeruptive Intracoronal Resorption (PEIR) : Case ReportsDocument4 pagesAtypical Developmental Defects of Enamel in Primary Incisors Versus Preeruptive Intracoronal Resorption (PEIR) : Case ReportsElizabeth CortésNo ratings yet
- m10 - Segubiense - Pulpal & Periapical InfectionDocument24 pagesm10 - Segubiense - Pulpal & Periapical InfectionKENT DANIEL SEGUBIENSENo ratings yet
- Advanced Endodontics - Informa Healthcare 1 Edition (January 13, 2006) PDFDocument375 pagesAdvanced Endodontics - Informa Healthcare 1 Edition (January 13, 2006) PDFAndra AnduNo ratings yet
- Endodontic Therapy For Primary and Young Permanent Teeth Pediatric EndodonticsDocument31 pagesEndodontic Therapy For Primary and Young Permanent Teeth Pediatric EndodonticsAthenaeum Scientific PublishersNo ratings yet
- Krok 2 Stomatology: Test Items For Licensing ExaminationDocument28 pagesKrok 2 Stomatology: Test Items For Licensing ExaminationjimmyNo ratings yet
- ICD 10 Kedokteran GigiDocument3 pagesICD 10 Kedokteran GigiAnggit PurwatiNo ratings yet
The Following Resources Related To This Article Are Available Online at
The Following Resources Related To This Article Are Available Online at
Uploaded by
Verghese George MOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
The Following Resources Related To This Article Are Available Online at
The Following Resources Related To This Article Are Available Online at
Uploaded by
Verghese George MCopyright:
Available Formats
Mineral trioxide aggregate pulpotomies: A case series outcomes assessment David E. Witherspoon, Joel C. Small and Gary Z.
Harris J Am Dent Assoc 2006;137;610-618 The following resources related to this article are available online at jada.ada.org ( this information is current as of June 12, 2011):
Updated information and services including high-resolution figures, can be found in the online version of this article at:
http://jada.ada.org/content/137/5/610
Downloaded from jada.ada.org on June 12, 2011
This article cites 78 articles, 7 of which can be accessed free: http://jada.ada.org/content/137/5/610/#BIBL This article appears in the following subject collections: Restoratives http://jada.ada.org/cgi/collection/restoratives Information about obtaining reprints of this article or about permission to reproduce this article in whole or in part can be found at:
http://www.ada.org/prof/resources/pubs/jada/permissions.asp
2011 American Dental Association. The sponsor and its products are not endorsed by the ADA.
C L I N I C A L
P R A C T I C E
Mineral trioxide aggregate pulpotomies
A case series outcomes assessment
David E. Witherspoon, BDSc, MS; Joel C. Small, DDS; Gary Z. Harris, DDS
raumatic injuries and dental caries are the greatest challenges to the integrity of the developing tooth. Both can cause the dental pulp to undergo irreversible damage, causing necrosis of the pulpal tissues, which can result in the arrest of normal root development. Abnormal root development will have an impact on the long-term prognosis for tooth retention.1-4 The primary goal of treatment, therefore, should be to maintain pulp vitality so that normal root development can occur. By maintaining pulp vitality, apexogenesis can occur.5-8 This is the preferred treatment because it promotes healing by regeneration rather than repair. Pulpotomy involves the surgical removal of a portion of an affected vital coronal pulp tissue, while the clinician leaves the radicular tissue in situ to allow for normal root development.
ABSTRACT
A Background. The greatest threats to developing teeth are dental1 RT I treatment is caries and traumatic injury. A primary goal of all restorativeC L E to maintain pulp vitality so that normal root development or apexogenesis can occur. If pulpal exposure occurs, then a pulpotomy procedure aims to preserve pulp vitality to allow for normal root development. Historically, calcium hydroxide has been the material of choice for pulpotomy procedures. Recently, an alternative material called mineral trioxide aggregate (MTA) has demonstrated the ability to induce hard-tissue formation in pulpal tissue. The authors describe the clinical and radiographic outcome of a series of cases involving the use of MTA in pulpotomy procedures. Methods. Twenty-three cases in 18 patients were treated with MTA pulpotomy procedures in an endodontic private practice. All of the patients had been referred to the practice for diagnosis and treatment of a symptomatic tooth. All of the authors provided treatment. Pulpal exposures were either due to caries or complicated enamel dentin fractures. Results. Nineteen teeth in 14 patients were available for recall. The mean time of recall was 19.7 months. Of the 19 cases, 15 involved healed teeth, and three involved teeth that were healing. One of 19 cases involved a tooth with persistent disease. Conclusions. MTA may be useful as a substitute for calcium hydroxide in pulpotomy procedures. Further research, however, is required to clarify this conclusion. Clinical Implications. MTA conceivably could replace calcium hydroxide as the material of choice for pulpotomy procedures, if future research continues to show promising results. Key Words. Pulpotomy; mineral trioxide aggregate; apexogenesis. JADA 2006;137:610-8.
Dr. Witherspoon is in private practice limited to endodontics, Plano, Texas. Address reprint requests to Dr. Witherspoon at North Texas Endodontic Associates, 5800 Coit Road, Suite 200, Plano, Texas 75023, e-mail dewspoon@ntendo.com. Dr. Small is in private practice limited to endodontics, Plano, Texas. Dr. Harris is in private practice limited to endodontics, Sherman, Texas.
Downloaded from jada.ada.org on June 12, 2011
PULPOTOMIES: A REVIEW THE LITERATURE
Several materials have been advocated to induce normal root development.9-11 To date, the material of choice has been calcium hydroxide.12-18 In the past decade, an alternative material called mineral trioxide aggregate (MTA) became available for use in pulpal procedures. Clinicians should evaluate
610 JADA, Vol. 137
http://jada.ada.org May 2006 Copyright 2005 American Dental Association. All rights reserved.
C L I N I C A L
P R A C T I C E
several elements when choosing a material to be used in vital pulp treatment. These elements include the ability of the material to kill bacteria, induce mineralization and establish a bacteriatight seal. Calcium hydroxide. Calcium hydroxide is a white, crystalline, slightly soluble basic salt that dissociates into calcium ions and hydroxyl ions in solution and exhibits a high alkalinity (pH 11). It is used in both setting and nonsetting forms in dentistry. Codman was the first to use calcium hydroxide in pulpal treatment.19 Dentists also use calcium hydroxide because of its antimicrobial properties20,21 and its ability to induce hard-tissue formation.22 Mineralization. Researchers have shown that calcium hydroxide forms a dentin bridge when placed in contact with pulpal tissues. Calcium hydroxide must be in contact with the tissue for mineralization to occur.23 Initially, a necrotic zone is formed adjacent to the material, and, depending on the pH of the calcium hydroxide material, a dentin bridge is formed directly against the necrotic zone or the necrotic zone is resorbed and replaced by a dentin bridge.24-28 The barrier is not always complete.16 The calcium ions in the calcium hydroxide do not become incorporated in the hard tissue that forms.29,30 Calcium hydroxide is an initiator rather than a substrate for repair.31 Several theories exist as to how calcium hydroxide induces hard-tissue formation. These include the high alkalinity (a pH of 11), which produces a favorable environment for the activation of alkaline phosphatase, an enzyme involved in mineralization. The calcium ions reduce the permeability of new capillaries formed in repairing tissue, decreasing the amount of intercellular fluid and increasing the concentration of calcium ions derived from the blood supply at the mineralization front. This may have two effects on the mineralization process; it may provide a source of calcium ions for mineralization, and it may stimulate the activity of calcium-dependent pyrophosphatase, which reduces the level of mineralization inhibitory pyrophosphate ions within the tissues.31-33 Antimicrobial effect. The antimicrobial effect of pulpotomy materials relates to the ability of the material to kill existing bacteria and prevent the future leakage of bacteria from the oral environment into the pulp. The antimicrobial properties of calcium hydroxide are derived from several fac-
tors. The high pH produces an environment that is not conducive to bacteria growth. There are three mechanisms by which calcium hydroxide induces bacterial lysis: dthe hydroxyl ions destroy phospholipids so the cellular membrane is destroyed; dthe high alkalinity breaks down ionic bonds so that bacterial proteins are denatured; dthe hydroxyl ions react with bacterial DNA, inhibiting replication.33 Calcium hydroxide treatment also has been shown to decrease the effect of bacterialassociated lipopolysaccharide (LPS).21 It can hydrolyze the lipid moiety of bacterial LPS and is able to eliminate the ability of LPS to stimulate tumor-necrosis factor-alpha production in peripheral blood monocytes.34 These actions decrease the ability of bacteria to cause tissue destruction. The ability to prevent penetration of bacteria into the pulp affects pulp survival significantly.35,36 Initially, the two paste calcium hydroxide systems were believed to have the ability to resist bacterial penetration; however, their ability to continue to do so has been called into question.35,37,38 The adhesive bond of calcium hydroxide liners to dentin is weak, and adhesive resin materials do not bond to the surface of the material.35 The incidence of bacterial leakage when calcium hydroxide is used in pulpal procedures has been reported as 47.0 percent.39 This was significantly greater than the leakage associated with bonded resin restorations. The severity of pulpal inflammation was shown to increase with the presence of bacteria. Outcomes. Several studies have assessed the outcomes of calcium hydroxide in vital pulpal treatment. Generally, as the length of the followup period increased, the success rate decreased. At the five- and 10-year follow-ups, pulp capping of cariously exposed teeth resulted in a failure rate of 44.5 percent and 79.7 percent, respectively.40 In teeth with carious exposures treated with calcium hydroxide pulpotomies, healing teeth ranged from approximately 50 to 92 percent.41-43 A study examining 41 teeth with carious pulpal exposures (with or without periradicular changes seen on radiographic examination) treated with pulpotomy and calcium hydroxide reported a healing rate of 87 to 79 percent.41 The healing rate in teeth with pre-existing pain, however, was approximately 50 percent. The follow-up period varied from six to eight months. In a similar
May 2006 611
Downloaded from jada.ada.org on June 12, 2011
JADA, Vol. 137 http://jada.ada.org Copyright 2005 American Dental Association. All rights reserved.
C L I N I C A L
P R A C T I C E
study, investigators found that 26 permanent vital molars with asymptomatic carious pulp exposures and periradicular involvement were treated with calcium hydroxide pulpotomies.42 The patients ranged in age from 10 to 24 years, and 24 teeth (92 percent) achieved healing status. The observation period after pulpotomy treatment was 16 to 72 months; however, investigators followed only 12 teeth beyond 24 months. The mean followup period was not reported in the study. In another study, 37 posterior teeth with deep carious lesions that were exposed during caries removal were treated with calcium hydroxide pulpotomies.43 The patients ranged in age from 6 to 15 years. Six teeth had widened periodontal ligament spaces periradicularly and a history of temporary pain. None of the other teeth had signs and symptoms of pulpal or periradicular inflammation or infection. The healing rate was 89 percent, and the follow-up period ranged from 24 to 140 months, with a mean of 56 months. The healing rates in teeth with traumatic exposures that were treated with calcium hydroxide ranged from 72 to 96 percent.44-48 Fuks and colleagues49 reported the long-term success of partial pulpotomies in complicated crown fractures in permanent incisors that were followed for 7.5 to 11 years at 87.5 percent. MTA. MTA is composed of tricalcium silicate, tricalcium aluminate, tricalcium oxide and silicate oxide. Hydration of the powder results in a colloidal gel composed of calcium oxide crystals in an amorphous structure: 33 percent calcium, 49 percent phosphate, 6 percent silica, 3 percent chloride and 2 percent carbon. This gel solidifies into a hard structure in less than three hours.50 It has a compressive strength equal to zinc oxideeugenol with polymer reinforcement (Caulk IRM Intermediate Restorative Material, Dentsply, York, Pa.) and all-purpose lining and cement (SuperEBA, Harry J. Bosworth, Skokie, Ill.) but less than that of amalgam. It is available commercially as ProRoot MTA (Dentsply Tulsa Dental, Tulsa, Okla.) and has been advocated for use in vital pulp therapy.51-55 Mineralization. MTA has demonstrated the ability to induce hard-tissue formation in pulpal tissues,51,53,56-59 and it promotes rapid cell growth in vitro.60 Compared with calcium hydroxide, MTA has demonstrated a greater ability to maintain the integrity of pulp tissue.51,61 Histologic evaluation of pulpal tissue in animals and humans demonstrated that MTA produces a
612 JADA, Vol. 137
thicker dentinal bridge, less inflammation, less hyperemia and less pulpal necrosis compared with calcium hydroxide.51,58 MTA also appears to induce the formation of a dentin bridge at a faster rate than does calcium hydroxide. The process by which MTA acts to induce dentin bridge formation, however, is not known. Holland and colleagues62 theorized that the tricalcium oxide in MTA reacts with tissue fluids to form calcium hydroxide, resulting in hard-tissue formation in a manner similar to that of calcium hydroxide. Antibacterial effect. According to Torabinejad and colleagues,63 MTA has an antibacterial effect on some facultative bacteria but no effect on strict anaerobic bacteria. This limited antibacterial effect is less than that demonstrated by calcium hydroxide pastes. The ability of MTA to resist the penetration of microorganisms appears to be high. In leakage studies, MTA frequently performs better than amalgam, IRM or SuperEBA.64-68 Compared with ideally placed resin-based composite, MTA leakage patterns are similar.69,70 Furthermore, the presence of blood has little impact on the degree of leakage.67,71 Outcomes. To date, the clinical assessment of MTA has been restricted to case reports. In one, researchers performed partial pulpotomies in two cases of dens evaginatus.72 After six months, researchers removed the teeth as part of planned orthodontic treatment. Histologic examination of these teeth showed an apparent continuous dentin bridge formation in both teeth, and the pulps were free of inflammation. In this article, we describe the clinical and radiographic outcome of a series of cases using MTA in pulpotomy procedures.
MATERIALS AND METHODS
Downloaded from jada.ada.org on June 12, 2011
We treated 23 teeth (cases 1-23) in 18 patients between 1999 and 2003 in an endodontic private practice (Tables 1 and 2, page 614). The patients had no contraindication to dental treatment. We took all of the radiographs using a digital radiographic system according to the manufacturers recommendations, and we conducted pulpal vitality tests to establish a pulpal diagnosis. The treatment followed the standard pulpotomy procedure of removing the pulp to the stump level using a coarse high-speed diamond bur with copious irrigation. We used rubber dam isolation in all cases. In each case, we achieved hemostasis by irrigating pulp tissue with 2 milliliters of 6
http://jada.ada.org May 2006 Copyright 2005 American Dental Association. All rights reserved.
C L I N I C A L
P R A C T I C E
TABLE 1
Individual patient data.
CASE NO. PATIENT NO. 1 1 2 3 4 5 6 7 8 8 9 10 11 12 13 13 13 14 15 16 16 17 18 PATIENT AGE (YEARS) 10 10 14 7.5 16 13 11 12 8 8 11 8 9 8 7 8 8 15 8 9 9 9.5 8.5 TOOTH NO. 19 30 31 14 8 15 13 18 8 9 18 14 9 8 3 19 30 31 30 8 9 14 30 OUTCOME DIAGNOSIS RECALL (MONTHS)
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23
Healing Healing Healed Patient not available for recall Healed Healed Healed Healed Healed Healed Persistent disease Patient not available for recall Healed Patient not available for recall Healed Healed Healed Healed Healed Healed Healed Patient not available for recall Healing
IP/C* IP/C IP/C IP/C IP/T/CEDF IP/C IP/C IP/C IP/T/CEDF IP/T/CEDF IP/C IP/C IP/T/CEDF IP/T/CEDF IP/C IP/C IP/C IP/C IP/C IP/T/CEDF IP/T/CEDF IP/C IP/C
19 19 13 Patient not available for recall 12 12 29 11
Downloaded from jada.ada.org on June 12, 2011
15 15 13 Patient not available for recall 25 Patient not available for recall 33 18 17 6 32 13 13 Patient not available for recall 53
* IP/C: Irreversible pulpitis with caries exposure. IP/T/CEDF: Irreversible pulpitis with a complicated enamel dentin fracture due to a traumatic injury.
percent sodium hypochlorite73 for approximately one minute. We avoided applying pressure to the pulp stumps, as it could crush the delicate tissue, the cotton from the cotton pellets used could get in the tissue and a dentin chip could be forced into the pulp tissue, all of which could have a negative effect on healing. We placed an approximately 2-millimeter-thick layer of MTA (mixed according to the manufacturers recommendations) over the exposed pulpal tissue. We took a final radiograph after we removed the rubber dam. Finally, we referred the patients back to
their restorative dentists. Recall intervals were approximately three months, and we followed all of the cases for as long as possible. Recall appointments included subjective history assessment, thermal pulpal testing, percussion assessment and a radiographic evaluation. We categorized cases as healed, healing or persistent disease (Box). Statistical analysis. We used the KaplanMeier method to assess the probability of tooth survival (that is, whether the tooth required any further treatment) and tooth healing.
May 2006 613
JADA, Vol. 137 http://jada.ada.org Copyright 2005 American Dental Association. All rights reserved.
C L I N I C A L
P R A C T I C E
TABLE 2
BOX
Summary data.
CATEGORY Age (Years) Range Mean Mode Median Recall Total no. (%) Mean (Months) Mode (Months) Median (Months) Range (Months) 19 (83) 19.7 13 17 6 to 53 7 to 16 9.9 8 9 DATA
Case categories.
HEALED
dNo history of pain, discomfort or altered sensation dThermal test results for the treated tooth similar
to those for contralateral control teeth with developmental age
dRadiographic appearance of the tooth consistent
HEALING
dNo history of pain, discomfort or altered sensation dNo response of the treated tooth to thermal
testing or electric pulp testing with developmental age
dRadiographic appearance of the tooth consistent
PERSISTENT DISEASE
dA history of pain, discomfort or altered sensation dNo response of the treated tooth to thermal
testing or electric pulp testing with developmental age
Downloaded from jada.ada.org on June 12, 2011
dRadiographic appearance of the tooth inconsistent
Outcome (No. of Teeth [%]) Healed Healing Persistent disease Diagnosis (No. of Teeth) Irreversible pulpitis due to caries Irreversible pulpitis with a complicated enamel dentin fracture due to a traumatic injury Tooth Type (No. of Teeth) Maxillary molar Mandibular molar Maxillary premolar Mandibular premolar Maxillary incisor Mandibular incisor 5 10 1 0 7 0 16 7 15 (79) 3 (16) 1 (5)
healed (Figures 1 and 2), and three involved teeth that were healing (Figures 3 and 4). One of the 19 cases involved a tooth with persistent disease. The probability of tooth survival at 12 months was 1.0 at a 95 percent confidence interval; the probability decreased to 0.95 at the termination point of the evaluation (Figure 5, page 616). The probability of a tooth being completely healed at 20 months was 0.55 at a 95 percent confidence interval (Figure 6, page 616).
DISCUSSION
RESULTS
Nineteen cases in 14 patients were available for recall (Table 1). The mean time of recall was 19.7 months (Table 2). The age range of patients was from 7 to 16 years, with a mean age of 9.9 years. Thirteen of the 19 cases (68.4 percent) available for recall had a diagnosis of irreversible pulpitis with a caries exposure (Table 1). Of these 13 cases, 70 percent healed, 23 percent were in the healing category, and 7 percent had persistent disease. Molars were the most frequently treated tooth type. Of the 19 cases, 15 involved teeth that
614 JADA, Vol. 137
The primary objective of vital pulp therapy in teeth with incomplete root formation is to promote normal development of the root complex. There are several long-term advantages of this treatment over apexification treatment. The tooth structure that is formed is of great quantity, and its composition appears to have greater structural integrity.3 The result is that the fully developed tooth is more resistant to vertical root fractures.4 The ideal material for vital pulp treatment should resist bacterial leakage and stimulate the remaining pulp tissue to return to a healthy state promoting the formation of dentin. Calcium hydroxide has been the material of choice for such treatments.74 The dentin formed in response to calcium hydroxides stimulation of pulpal tissue typically ranges from a porous dentin-type material to a dentin structure that approaches that of normal dentin.57 The type of dentin structure formed depends on a number of variables and is not predictable.39 These variables
http://jada.ada.org May 2006 Copyright 2005 American Dental Association. All rights reserved.
C L I N I C A L
P R A C T I C E
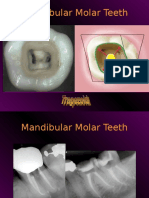
Figure 1. Preoperative radiograph of case no.16.
Figure 2. Postoperative radiograph of case no.16 at 18-month recall (healed).
Downloaded from jada.ada.org on June 12, 2011
Figure 3. Preoperative radiograph of case no. 2.
Figure 4. Postoperative radiograph of case no. 2 at 19-month recall (healing).
include the type of calcium hydroxide material used (powder mixed with water or a commercially available preparation),26,75,76 the degree of contact between the material and the pulp,77 and the ability to control pulpal bleeding.78 Calcium hydroxide also has been shown to have little resistance to bacterial leakage over the medium term in a study.79 In in vitro leakage studies, MTA has resisted leakage, predictably and repeatedly.80,81 In a short-term animal assessment study, MTA consistently induced the formation of dentin at a greater rate with greater structural integrity and more complete dentin bridging than did calcium hydroxide.61 Histologically, in other animal studies, MTA was considerably better at stimu-
lating reparative dentin formation and maintaining the integrity of the pulp.57,59 In a shortterm human study using adult third molars, MTA consistently demonstrated less inflammation, hyperemia and necrosis, as well as a thicker dentinal bridge with more frequent odontoblastic layer formation, than that seen with calcium hydroxide.58 In an outcome assessment of calcium hydroxide in vital pulp treatment, success rates ranged from 50 to 96 percent.41,44,49,82,83 These studies typically focused on asymptomatic teeth with deep carious lesions that resulted in a pulpal exposure or on noncarious teeth with complex enamel fractures, dentin fractures or both. Thus, the pulp had no pre-existing disease process. A 93.5 percent sucMay 2006 615
JADA, Vol. 137 http://jada.ada.org Copyright 2005 American Dental Association. All rights reserved.
C L I N I C A L
P R A C T I C E
1.0 PROBABILITY OF COMPLETE HEALING 0 10 20 30 40 50 PROBABILITY OF TOOTH SURVIVAL
1.0
0.8
0.8
0.6
0.6
0.4
0.4
0.2
0.2
0.0
0.0 0 10 20 30 40 50
TIME (IN MONTHS)
TIME (IN MONTHS)
Figure 5. Kaplan-Meier method plot of probability of tooth survival.
Figure 6. Kaplan-Meier method plot of probability of complete healing.
Downloaded from jada.ada.org on June 12, 2011
cess rate was achieved using a calcium hydroxide partial pulpotomy technique in young posterior teeth with deep carious lesions and exposed pulps.43 All of the teeth had no history of signs or symptoms and responded within normal limits to pulp testing at the time of treatment. In another investigation, calcium hydroxide pulpotomies were used to treat successfully 24 of 26 (92 percent) permanent vital molars with carious pulp exposures and periradicular involvement in patients 10 to 24 years of age.42 In that study, all of the teeth initially were asymptomatic and responded within normal limits to pulp tests. Six to nine months after treatment, investigators removed the coronal restoration and assessed the sensitivity of the radicular pulp. In such studies, the preoperative pulpal diagnosis would have been either normal or reversible pulpitis.42,43 A significant difference in our investigation was the painful condition of a large percentage of the teeth before treatment. Approximately 70 percent of the cases on which we reported in this series involved teeth with caries exposure and a preoperative diagnosis of irreversible pulpitis. For this group, we achieved a 100 percent success rate in terms of the primary goal of normal root development in treating such a tooth. The success rate in terms of maintaining the vitality of the tooth as assessed by a response to thermal or electrical stimulus with the original coronal restoration intact in this group was 75 percent. Only one tooth (5 percent) has required additional endodontic treatment to date. This tooth had not received an appropriate coronal restoration, and recurrent caries was evident.
616 JADA, Vol. 137
CONCLUSION
MTA may be useful as a substitute for calcium hydroxide in pulpotomy procedures. Further research, however, is needed to clarify this conclusion. s
The authors would like to thank Dr. Martha Nunn for her statistical analysis, Dr. John D. Regan for his critical review and the staff members of North Texas Endodontic Associates for their tireless efforts in recalling patients. 1. Robertson A, Andreasen FM, Andreasen JO, Noren JG. Long-term prognosis of crown-fractured permanent incisors: the effect of stage of root development and associated luxation injury. Int J Paediatr Dent 2000;10(3):191-9. 2. Rabie G, Trope M, Tronstad L. Strengthening of immature teeth during long-term endodontic therapy. Endod Dent Traumatol 1986;2(1):43-7. 3. Katebzadeh N, Dalton BC, Trope M. Strengthening immature teeth during and after apexification. J Endod 1998;24:256-9. 4. Cvek M. Prognosis of luxated non-vital maxillary incisors treated with calcium hydroxide and filled with gutta-percha: a retrospective clinical study. Endod Dent Traumatol 1992;8(2):45-55. 5. Love RM. Effects of dental trauma on the pulp. Pract Periodontics Aesthet Dent 1997;9:427-36; quiz 38. 6. Shabahang S, Torabinejad M. Treatment of teeth with open apices using mineral trioxide aggregate. Pract Periodontics Aesthet Dent 2000;12:315-20; quiz 22. 7. Webber RT. Apexogenesis versus apexification. Dent Clin North Am 1984;28:669-97. 8. Massler M. Preventive endodontics: vital pulp therapy. Dent Clin North Am 1967;11:663-73. 9. Horsted-Bindslev P, Vilkinis V, Sidlauskas A. Direct capping of human pulps with a dentin bonding system or with calcium hydroxide cement. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2003;96:591-600. 10. Trope M, McDougal R, Levin L, May KN Jr, Swift EJ Jr. Capping the inflamed pulp under different clinical conditions. J Esthet Restor Dent 2002;14:349-57. 11. Kiba H, Hayakawa T, Nakanuma K, Yamazaki M, Yamamoto H. Pulpal reactions to two experimental bonding systems for pulp capping procedures. J Oral Sci 2000;42(2):69-74. 12. Ulmansky M, Sela J, Langer M, Yaari A. Response of pulpotomy wounds in normal human teeth to successively applied Ledermix and Calxyl. Arch Oral Biol 1971;16:1393-8. 13. Schroder U, Granath LE. Scanning electron microscopy of hard tissue barrier following experimental pulpotomy of intact human teeth and capping with calcium hydroxide. Odontol Revy 1972;23:211-20. 14. Schroder U. Evaluation of healing following experimental pulpotomy of intact human teeth and capping with calcium hydroxide.
http://jada.ada.org May 2006 Copyright 2005 American Dental Association. All rights reserved.
C L I N I C A L
P R A C T I C E
Odontol Revy 1972;23:329-40. 15. Holland R, de Souza V, de Mello W, Nery MJ, Bernabe PF, Otoboni Filho JA. Healing process after pulpotomy and covering with calcium hydroxide, Dycal or MPC: histological study in dog teeth. Rev Fac Odontol Aracatuba 1978;7(2):185-91. 16. Holland R, de Souza V, de Mello W, Nery MJ, Bernabe PF, Otoboni Filho JA. Permeability of the hard tissue bridge formed after pulpotomy with calcium hydroxide: a histologic study. JADA 1979;99:472-5. 17. Stanley HR. Criteria for standardizing and increasing credibility of direct pulp capping studies. Am J Dent 1998;11(special number): S17-34. 18. Haskell EW, Stanley HR, Chellemi J, Stringfellow H. Direct pulp capping treatment: a long-term follow-up. JADA 1978;97:607-12. 19. Codman WW. Ossification of the pulp of a tooth. Newsletter 1851;IV:90. 20. King JB Jr., Crawford JJ, Lindahl RL. Indirect pulp capping: a bacteriologic study of deep carious dentine in human teeth. Oral Surg Oral Med Oral Pathol 1965;20:663-9. 21. Safavi KE, Nichols FC. Effect of calcium hydroxide on bacterial lipopolysaccharide. J Endod 1993;19(2):76-8. 22. Mitchell DF, Shankwalker GB. Osteogenic potential of calcium hydroxide and other materials in soft tissue and bone wounds. J Dent Res 1958;37:1157-63. 23. Rasmussen P, Mjor IA. Calcium hydroxide as an ectopic bone inductor in rats. Scand J Dent Res 1971;79(1):24-30. 24. Stanley HR, Lundy T. Dycal therapy for pulp exposures. Oral Surg Oral Med Oral Pathol 1972;34:818-27. 25. Tronstad L. Reaction of the exposed pulp to Dycal treatment. Oral Surg Oral Med Oral Pathol 1974;38:945-53. 26. Heys DR, Cox CF, Heys RJ, Avery JK. Histological considerations of direct pulp capping agents. J Dent Res 1981;60:1371-9. 27. Pitt Ford TR. Pulpal response to a calcium hydroxide material for capping exposures. Oral Surg Oral Med Oral Pathol 1985;59(2):194-7. 28. Tagger M, Tagger E. Pulp capping in monkeys with Reolit and Life, two calcium hydroxide bases with different pH. J Endod 1985;11:394-400. 29. Sciaky I, Pisanti S. Localization of calcium placed over amputated pulps in dogs teeth. J Dent Res 1960;39:1128-32. 30. Pisanti S, Sciaky I. Origin of calcium in the repair wall after pulp exposure in the dog. J Dent Res 1964;43:641-4. 31. Foreman PC, Barnes IE. Review of calcium hydroxide. Int Endod J 1990;23:283-97. 32. Heithersay GS. Calcium hydroxide in the treatment of pulpless teeth with associated pathology. J Br Endod Soc 1975;8(2):74-93. 33. Siqueira JF Jr, Lopes HP. Mechanisms of antimicrobial activity of calcium hydroxide: a critical review. Int Endod J 1999;32:361-9. 34. Barthel CR, Levin LG, Reisner HM, Trope M. TNF-alpha release in monocytes after exposure to calcium hydroxide treated Escherichia coli LPS. Int Endod J 1997;30(3):155-9. 35. Cox CF, Bogen G, Kopel HM, Ruby JD. Repair of pulpal injury by dental materials. In: Hargreaves KM, Goodis HE, Seltzer S, eds. Seltzer and Benders dental pulp. Chicago: Quintessence; 2002:325-44. 36. Stanley H. Calcium hydroxide and vital pulp therapy. In: Hargreaves KM, Goodis HE, Seltzer S, eds. Seltzer and Benders dental pulp. Chicago: Quintessence; 2002:309-24. 37. Murray PE, Lumley PJ, Smith AJ, Ross HF. The influence of sample dimensions on hydroxyl ion release from calcium hydroxide products. Endod Dent Traumatol 2000;16:251-7. 38. Cox CF, Bergenholtz G, Heys DR, Syed SA, Fitzgerald M, Heys RJ. Pulp capping of dental pulp mechanically exposed to oral microflora: a 1-2 year observation of wound healing in the monkey. J Oral Pathol 1985;14(2):156-68. 39. Murray PE, Hafez AA, Smith AJ, Cox CF. Hierarchy of pulp capping and repair activities responsible for dentin bridge formation. Am J Dent 2002;15:236-43. 40. Barthel CR, Rosenkranz B, Leuenberg A, Roulet JF. Pulp capping of carious exposures: treatment outcome after 5 and 10 yearsa retrospective study. J Endod 2000;26:525-8. 41. Teixeira LS, Demarco FF, Coppola MC, Bonow ML. Clinical and radiographic evaluation of pulpotomies performed under intrapulpal injection of anaesthetic solution. Int Endod J 2001;34:440-6. 42. Caliskan MK. Pulpotomy of carious vital teeth with periapical involvement. Int Endod J 1995;28:172-6. 43. Mejare I, Cvek M. Partial pulpotomy in young permanent teeth with deep carious lesions. Endod Dent Traumatol 1993;9:238-42. 44. Cvek M. A clinical report on partial pulpotomy and capping with calcium hydroxide in permanent incisors with complicated crown fracture. J Endod 1978;4:232-7. 45. Ravn JJ. Follow-up study of permanent incisors with complicated
crown fractures after acute trauma. Scand J Dent Res 1982;90:363-72. 46. Cox CF, Bergenholtz G, Fitzgerald M, et al. Capping of the dental pulp mechanically exposed to the oral microflora: a 5 week observation of wound healing in the monkey. J Oral Pathol 1982;11:327-39. 47. Fuks AB, Cosack A, Klein H, Eidelman E. Partial pulpotomy as a treatment alternative for exposed pulps in crown-fractured permanent incisors. Endod Dent Traumatol 1987;3(3):100-2. 48. Gelbier MJ, Winter GB. Traumatised incisors treated by vital pulpotomy: a retrospective study (published correction appears in Br Dent J 1988;164[11]:361). Br Dent J 1988;164(10):319-23. 49. Fuks AB, Gavra S, Chosack A. Long-term followup of traumatized incisors treated by partial pulpotomy. Pediatr Dent 1993;15:334-6. 50. Torabinejad M, Hong CU, McDonald F, Pitt Ford TR. Physical and chemical properties of a new root-end filling material. J Endod 1995;21:349-53. 51. Ford TR, Torabinejad M, Abedi HR, Bakland LK, Kariyawasam SP. Using mineral trioxide aggregate as a pulp-capping material. JADA 1996;127:1491-4. 52. Torabinejad M, Chivian N. Clinical applications of mineral trioxide aggregate. J Endod 1999;25(3):197-205. 53. Andelin WE, Shabahang S, Wright K, Torabinejad M. Identification of hard tissue after experimental pulp capping using dentin sialoprotein (DSP) as a marker. J Endod 2003;29:646-50. 54. Bakland LK. Management of traumatically injured pulps in immature teeth using MTA. J Calif Dent Assoc 2000;28:855-8. 55. Schmitt D, Lee J, Bogen G. Multifaceted use of ProRoot MTA root canal repair material. Pediatr Dent 2001;23:326-30. 56. Holland R, de Souza V, Murata SS, et al. Healing process of dog dental pulp after pulpotomy and pulp covering with mineral trioxide aggregate or Portland cement. Braz Dent J 2001;12(2):109-13. 57. Dominguez MS, Witherspoon DE, Gutmann JL, Opperman LA. Histological and scanning electron microscopy assessment of various vital pulp-therapy materials. J Endod 2003;29:324-33. 58. Aeinehchi M, Eslami B, Ghanbariha M, Saffar AS. Mineral trioxide aggregate (MTA) and calcium hydroxide as pulp-capping agents in human teeth: a preliminary report. Int Endod J 2003;36:225-31. 59. Tziafas D, Pantelidou O, Alvanou A, Belibasakis G, Papadimitriou S. The dentinogenic effect of mineral trioxide aggregate (MTA) in short-term capping experiments. Int Endod J 2002;35:245-54. 60. Mitchell PJ, Pitt Ford TR, Torabinejad M, McDonald F. Osteoblast biocompatibility of mineral trioxide aggregate. Biomaterials 1999;20(2):167-73. 61. Faraco IM Jr, Holland R. Response of the pulp of dogs to capping with mineral trioxide aggregate or a calcium hydroxide cement. Dent Traumatol 2001;17(4):163-6. 62. Holland R, de Souza V, Nery MJ, Otoboni Filho JA, Bernabe PF, Dezan Junior E. Reaction of rat connective tissue to implanted dentin tubes filled with mineral trioxide aggregate or calcium hydroxide. J Endod 1999;25(3):161-6. 63. Torabinejad M, Hong CU, Pitt Ford TR, Kettering JD. Antibacterial effects of some root end filling materials. J Endod 1995;21:403-6. 64. Torabinejad M, Rastegar AF, Kettering JD, Pitt Ford TR. Bacterial leakage of mineral trioxide aggregate as a root-end filling material. J Endod 1995;21:109-12. 65. Fischer EJ, Arens DE, Miller CH. Bacterial leakage of mineral trioxide aggregate as compared with zinc-free amalgam, intermediate restorative material, and Super-EBA as a root-end filling material. J Endod 1998;24:176-9. 66. Lee SJ, Monsef M, Torabinejad M. Sealing ability of a mineral trioxide aggregate for repair of lateral root perforations. J Endod 1993;19:541-4. 67. Martell B, Chandler NP. Electrical and dye leakage comparison of three root-end restorative materials. Quintessence Int 2002;33(1):30-4. 68. Tang HM, Torabinejad M, Kettering JD. Leakage evaluation of root end filling materials using endotoxin. J Endod 2002;28:5-7. 69. Adamo HL, Buruiana R, Schertzer L, Boylan RJ. A comparison of MTA, Super-EBA, composite and amalgam as root-end filling materials using a bacterial microleakage model. Int Endod J 1999;32:197-203. 70. Fogel HM, Peikoff MD. Microleakage of root-end filling materials (published correction appears in J Endod 2001;27:634). J Endod 2001;27:456-8. 71. Torabinejad M, Higa RK, McKendry DJ, Pitt Ford TR. Dye leakage of four root end filling materials: effects of blood contamination. J Endod 1994;20:159-63. 72. Koh ET, Ford TR, Kariyawasam SP, Chen NN, Torabinejad M. Prophylactic treatment of dens evaginatus using mineral trioxide aggregate. J Endod 2001;27:540-2. 73. Hafez AA, Cox CF, Tarim B, Otsuki M, Akimoto N. An in vivo evaluation of hemorrhage control using sodium hypochlorite and direct capping with a one- or two-component adhesive system in exposed non-
Downloaded from jada.ada.org on June 12, 2011
JADA, Vol. 137 http://jada.ada.org Copyright 2005 American Dental Association. All rights reserved.
May 2006
617
C L I N I C A L
P R A C T I C E
human primate pulps. Quintessence Int 2002;33:261-72. 74. Cohen S, Burns RC, eds. Pathways of the pulp. 7th ed. St. Louis: Mosby; 1998:808-11. 75. Heys DR, Heys RJ, Cox CF, Avery JK. The response of four calcium hydroxides on monkey pulps. J Oral Pathol 1980;9:372-9. 76. Mjor IA. Pulp-dentin biology in restorative dentistry. Chicago: Quintenssence; 2002. 77. Hirschfeld Z, Bab I, Tamari I, Sela J. Primary mineralization of dentin in rats after pulp capping with calcium-hydroxide. J Oral Pathol 1982;11:426-33. 78. Matsuo T, Nakanishi T, Shimizu H, Ebisu S. A clinical study of direct pulp capping applied to carious-exposed pulps. J Endod 1996;22:551-6.
79. Murray PE, Hafez AA, Smith AJ, Cox CF. Identification of hierarchical factors to guide clinical decision making for successful long-term pulp capping. Quintessence Int 2003;34(1):61-70. 80. Wu MK, Kontakiotis EG, Wesselink PR. Long-term seal provided by some root-end filling materials. J Endod 1998;24:557-60. 81. Roy CO, Jeansonne BG, Gerrets TF. Effect of an acid environment on leakage of root-end filling materials. J Endod 2001;27(1):7-8. 82. Blanco L, Cohen S. Treatment of crown fractures with exposed pulps. J Calif Dent Assoc 2002;30:419-25. 83. Mass E, Zilberman U. Clinical and radiographic evaluation of partial pulpotomy in carious exposure of permanent molars. Pediatr Dent 1993;15:257-9.
Downloaded from jada.ada.org on June 12, 2011
618
JADA, Vol. 137
http://jada.ada.org May 2006 Copyright 2005 American Dental Association. All rights reserved.
You might also like
- 500 Feedback Questions Bank PDFDocument40 pages500 Feedback Questions Bank PDFmariyam hasnainNo ratings yet
- National Board Questions Pediatric DentistryDocument50 pagesNational Board Questions Pediatric DentistryVerghese George MNo ratings yet
- Adhesive Restoration of Endodontically Treated TeethFrom EverandAdhesive Restoration of Endodontically Treated TeethRating: 3 out of 5 stars3/5 (2)
- Adc MCQ Sep 2006 Paper1Document28 pagesAdc MCQ Sep 2006 Paper1api-2629165189% (19)
- 1 - Ahmed Sle MCQ EndoDocument29 pages1 - Ahmed Sle MCQ EndoShabana Serju82% (17)
- Prometric Questions 20014Document100 pagesPrometric Questions 20014aliakdr3414100% (1)
- Interdisciplinary Approach in Periodontal TherapyDocument100 pagesInterdisciplinary Approach in Periodontal Therapypoojawadkar92% (13)
- Mineral Trioxide Aggregate Pulpotomies: A Case Series Outcomes AssessmentDocument9 pagesMineral Trioxide Aggregate Pulpotomies: A Case Series Outcomes AssessmentWidya JuliantiNo ratings yet
- The Purpose of Calcium Hydroxide in Root Canal TreatmentDocument4 pagesThe Purpose of Calcium Hydroxide in Root Canal TreatmentIJRASETPublicationsNo ratings yet
- Calcium HydroxideDocument12 pagesCalcium HydroxideKarina KariadiNo ratings yet
- Materials 13 02670 v2Document42 pagesMaterials 13 02670 v2Jose Manuel Quintero RomeroNo ratings yet
- Comparative Study of Efficacy of Formocresol and Calcium Hydroxide Pulpotomy in Primary MolarsDocument15 pagesComparative Study of Efficacy of Formocresol and Calcium Hydroxide Pulpotomy in Primary MolarsPipin HeryantoNo ratings yet
- P Esker Soy 2020Document9 pagesP Esker Soy 2020Gawi ChangNo ratings yet
- Apexification With Calcium Hydroxide and Mineral Trioxide AggregateDocument5 pagesApexification With Calcium Hydroxide and Mineral Trioxide AggregateTalitha NabilaNo ratings yet
- Liners & Bases in DentistryDocument12 pagesLiners & Bases in Dentistryjawaad293No ratings yet
- Artigo 11 Jeeruphan, 2012Document7 pagesArtigo 11 Jeeruphan, 2012damacenobpmNo ratings yet
- Journal of Oral Biology and Craniofacial ResearchDocument9 pagesJournal of Oral Biology and Craniofacial ResearchCyber MagicNo ratings yet
- Apexogenesis of A Symptomatic MolarDocument5 pagesApexogenesis of A Symptomatic MolarFoysal SirazeeNo ratings yet
- El MeligyDocument7 pagesEl Meligysystematic reviewNo ratings yet
- Management of Open ApexDocument7 pagesManagement of Open ApexMineet KaulNo ratings yet
- Calcium Hydroxide-Induced Resorption of Deciduous Teeth - A Possible ExplanationDocument5 pagesCalcium Hydroxide-Induced Resorption of Deciduous Teeth - A Possible ExplanationAhmad AssariNo ratings yet
- Content ServerDocument6 pagesContent Serveranon_688123777No ratings yet
- The Effect of Long-Term Dressing With CalciumDocument6 pagesThe Effect of Long-Term Dressing With CalciumArturo Trejo VeraNo ratings yet
- Intracanal Medicament and ResilonDocument5 pagesIntracanal Medicament and ResilonLuLu NikhlaturNo ratings yet
- Apexification With Mineral Trioxide Aggregate: An Overview of The Material and TechniqueDocument5 pagesApexification With Mineral Trioxide Aggregate: An Overview of The Material and Techniquedrvivek reddyNo ratings yet
- Int Endodontic J - 2016 - Galler - European Society of Endodontology Position Statement Revitalization ProceduresDocument7 pagesInt Endodontic J - 2016 - Galler - European Society of Endodontology Position Statement Revitalization ProceduresShivangiJainNo ratings yet
- ReviewsDocument6 pagesReviewsDenisa BlažekNo ratings yet
- Cytotoxicity and Bioactivity of Dental Pulp-Capping (Pedano) (2020)Document16 pagesCytotoxicity and Bioactivity of Dental Pulp-Capping (Pedano) (2020)juan salazarNo ratings yet
- Remineralization of TeethDocument37 pagesRemineralization of TeethPrajakta ChavanNo ratings yet
- Calcium Hydroxide - A Great Calcific WallDocument5 pagesCalcium Hydroxide - A Great Calcific WallAki AvlonNo ratings yet
- Australian Dental Journal: Liners and Bases in General DentistryDocument13 pagesAustralian Dental Journal: Liners and Bases in General DentistryAngela Gissela Moncada BoulanggerNo ratings yet
- Jurnal 2 IKGADocument13 pagesJurnal 2 IKGAekaapriany45No ratings yet
- Case Study Vital Pulp Therapy 5Document1 pageCase Study Vital Pulp Therapy 5chen danielNo ratings yet
- Ridge Preservation Using Composite AlloplasticDocument8 pagesRidge Preservation Using Composite Alloplasticarun perioNo ratings yet
- Carrier-Based Root Canal Filling Materials A Literature ReviewDocument7 pagesCarrier-Based Root Canal Filling Materials A Literature ReviewMegha GhoshNo ratings yet
- Calcium Sulfate in Implantology Biphasic Calcium SDocument24 pagesCalcium Sulfate in Implantology Biphasic Calcium Smarco.cedilloNo ratings yet
- Condezo 2020Document9 pagesCondezo 2020Rafael Zetehaku AraujoNo ratings yet
- Endodontics and Pulp Biology: The Impact Clinically: Rci Icw IclcDocument4 pagesEndodontics and Pulp Biology: The Impact Clinically: Rci Icw IclcdrashotiNo ratings yet
- Traditional and Contemporary Techniques For Optimizing Root Canal IrrigationDocument9 pagesTraditional and Contemporary Techniques For Optimizing Root Canal IrrigationrintanfsNo ratings yet
- Jur Endo 11Document8 pagesJur Endo 11Fadli FadelNo ratings yet
- 12 Shikha Dorgra DentalDocument4 pages12 Shikha Dorgra DentalHarish ChowdaryNo ratings yet
- IEJ - Revitalization in EndodonticsDocument7 pagesIEJ - Revitalization in Endodonticssoho1303No ratings yet
- Iej 10 2009Document100 pagesIej 10 2009Israel CurveloNo ratings yet
- Removal Efficacy of Propoliscalcium Hydroxide MediDocument6 pagesRemoval Efficacy of Propoliscalcium Hydroxide Medifelipe martinezNo ratings yet
- KokichDocument2 pagesKokichFederico LisiNo ratings yet
- Vital Pulp Therapy For The Mature Tooth Can It WorkDocument8 pagesVital Pulp Therapy For The Mature Tooth Can It WorkRamona MateiNo ratings yet
- Apexification Using Different Approaches - Case Series Report With A Brief Literature ReviewDocument12 pagesApexification Using Different Approaches - Case Series Report With A Brief Literature ReviewIJAR JOURNALNo ratings yet
- Cytotoxicity and Genotoxicity of Newly Developed Calcium Phosphate-Based Root Canal SealersDocument14 pagesCytotoxicity and Genotoxicity of Newly Developed Calcium Phosphate-Based Root Canal SealersNunoGonçalvesNo ratings yet
- What Leave Behind in Canals Endodontic Treatment: Issues and ConcernsDocument7 pagesWhat Leave Behind in Canals Endodontic Treatment: Issues and ConcernsSitiKhadijahNo ratings yet
- In Vitro Cytotoxicity of Calcium Silicate-Contain - Endodontic Sealers - Joe 20015Document7 pagesIn Vitro Cytotoxicity of Calcium Silicate-Contain - Endodontic Sealers - Joe 20015Andrea UrgilesNo ratings yet
- Endodontology 1: RootsDocument44 pagesEndodontology 1: RootsCarlos San Martin100% (1)
- Chou2018-The Effect of Plasma Treatment On The Osseointegration of Rough Titanium Implant A Histo-Morphometric Study in RabbitsDocument7 pagesChou2018-The Effect of Plasma Treatment On The Osseointegration of Rough Titanium Implant A Histo-Morphometric Study in RabbitsYohann GNo ratings yet
- Overview of Bleaching TechniquesDocument7 pagesOverview of Bleaching TechniquesAnonymous WtgTCQJdNNo ratings yet
- Posterior Composite Restoration UpdateDocument10 pagesPosterior Composite Restoration UpdateBianca IovoaiaNo ratings yet
- Scopeofendo RegendoDocument2 pagesScopeofendo Regendosalman azizNo ratings yet
- Avulsions and Intrusions: The Controversial Displacement InjuriesDocument7 pagesAvulsions and Intrusions: The Controversial Displacement InjuriessaeedrahmaniNo ratings yet
- Int J of Pediatric Dent 2Document107 pagesInt J of Pediatric Dent 2Diana DrutaNo ratings yet
- WhiteandElezar CaOHweakeningdentinDocument3 pagesWhiteandElezar CaOHweakeningdentinJigar M. UpadhyayNo ratings yet
- Galler Et Al-2016-International Endodontic JournalDocument7 pagesGaller Et Al-2016-International Endodontic JournalMaja Maja BułkaNo ratings yet
- 10 4 2013Document49 pages10 4 2013Anonymous 2h5lIeNo ratings yet
- Bioactive Glass Nanoparticles (NovaMin®) For Applications in DentistryDocument6 pagesBioactive Glass Nanoparticles (NovaMin®) For Applications in DentistryIOSRjournalNo ratings yet
- Direct Pulp CapDocument3 pagesDirect Pulp CapMelliya heptaniaNo ratings yet
- JCM 10 01600 v2Document17 pagesJCM 10 01600 v2ShivangiJainNo ratings yet
- 2 PBDocument6 pages2 PBMenna SalemNo ratings yet
- Response of Human Dental Pulp Capped With Biodentine and Mta Nowicka 1Document5 pagesResponse of Human Dental Pulp Capped With Biodentine and Mta Nowicka 1Adriiana Jaimes JaimesNo ratings yet
- An Evaluation of Ethical Aspects Concerning Endodontic Instrument FractureDocument4 pagesAn Evaluation of Ethical Aspects Concerning Endodontic Instrument FractureVerghese George MNo ratings yet
- The Role of Nurses in The Resuscitation of In-Hospital Cardiac ArrestsDocument5 pagesThe Role of Nurses in The Resuscitation of In-Hospital Cardiac ArrestsVerghese George MNo ratings yet
- 2006-2007 Dental Decks PDFDocument625 pages2006-2007 Dental Decks PDFVerghese George MNo ratings yet
- LightspeedDocument8 pagesLightspeedVerghese George MNo ratings yet
- Pharmacology For Dentistry PDFDocument501 pagesPharmacology For Dentistry PDFOfier SikiNo ratings yet
- Straight Line AccessDocument9 pagesStraight Line AccessVerghese George MNo ratings yet
- Cracked Tooth Syndrome-Decoding The EnigmaDocument3 pagesCracked Tooth Syndrome-Decoding The EnigmaVerghese George MNo ratings yet
- KrasnerandRankowJOE2004 PDFDocument12 pagesKrasnerandRankowJOE2004 PDFVerghese George MNo ratings yet
- Splinting MaterialsDocument1 pageSplinting MaterialsVerghese George MNo ratings yet
- 10 Besar 1 TH 2017Document356 pages10 Besar 1 TH 2017dartosNo ratings yet
- Vital Pulp Therapy 1Document6 pagesVital Pulp Therapy 1Mostafa Afifi Ali100% (1)
- Newapproachestopain Management: Orrett E. OgleDocument10 pagesNewapproachestopain Management: Orrett E. OgleNajeeb UllahNo ratings yet
- Pulpal DiagnosisDocument14 pagesPulpal DiagnosisSimina LungociNo ratings yet
- SRMJResDentSci73158-2129782 003529Document4 pagesSRMJResDentSci73158-2129782 003529MarsyaNo ratings yet
- Essentials of Endodontics 2Nd Edition Vimal K Sikri Online Ebook Texxtbook Full Chapter PDFDocument69 pagesEssentials of Endodontics 2Nd Edition Vimal K Sikri Online Ebook Texxtbook Full Chapter PDFjames.mozak676100% (11)
- Pulp Therapy For Primary TeethDocument14 pagesPulp Therapy For Primary TeethMahmoudFayedNo ratings yet
- Past Papers 1 200Document55 pagesPast Papers 1 200AmarAldujaili100% (1)
- Endodontics Key Points by DaneshDocument16 pagesEndodontics Key Points by DaneshNoor HaiderNo ratings yet
- Interstitial Fluid Pressure Normal Inflamed PulpDocument9 pagesInterstitial Fluid Pressure Normal Inflamed PulpAbeerNo ratings yet
- Endodontic Mcqs - DocShare - Tips 2Document1 pageEndodontic Mcqs - DocShare - Tips 2Stela NichevaNo ratings yet
- SOCA Blok 12Document21 pagesSOCA Blok 12safiraNo ratings yet
- Dental Caries - Its Sequelae and Treatment Among Patients in A Tertiary Hospital in North-Western Nigeria-A Retrospective StudyDocument7 pagesDental Caries - Its Sequelae and Treatment Among Patients in A Tertiary Hospital in North-Western Nigeria-A Retrospective Studyabdurrazaq taiwoNo ratings yet
- Common Causes of Dental Pain in Children (Differential Diagnosis)Document21 pagesCommon Causes of Dental Pain in Children (Differential Diagnosis)jamie chewNo ratings yet
- Clinical and Radiographic Evaluation of Pulpal and Periradicular TissueDocument6 pagesClinical and Radiographic Evaluation of Pulpal and Periradicular TissueMónïcå Lÿdïå RómåúlïèNo ratings yet
- Endodontics Key Points by DaneshDocument6 pagesEndodontics Key Points by DaneshDanesh KumarNo ratings yet
- Osteomyelitis: Deo Jake Lacpacan Jhunevyl MallorcaDocument36 pagesOsteomyelitis: Deo Jake Lacpacan Jhunevyl MallorcaDeo Jake Lacpacan100% (1)
- DR - Ritty Arouje Recent Question Paper FileDocument118 pagesDR - Ritty Arouje Recent Question Paper Filemuneer024No ratings yet
- 322 RDS Pre-Clinical EndodonticsDocument6 pages322 RDS Pre-Clinical EndodonticsHadil AltilbaniNo ratings yet
- Atypical Developmental Defects of Enamel in Primary Incisors Versus Preeruptive Intracoronal Resorption (PEIR) : Case ReportsDocument4 pagesAtypical Developmental Defects of Enamel in Primary Incisors Versus Preeruptive Intracoronal Resorption (PEIR) : Case ReportsElizabeth CortésNo ratings yet
- m10 - Segubiense - Pulpal & Periapical InfectionDocument24 pagesm10 - Segubiense - Pulpal & Periapical InfectionKENT DANIEL SEGUBIENSENo ratings yet
- Advanced Endodontics - Informa Healthcare 1 Edition (January 13, 2006) PDFDocument375 pagesAdvanced Endodontics - Informa Healthcare 1 Edition (January 13, 2006) PDFAndra AnduNo ratings yet
- Endodontic Therapy For Primary and Young Permanent Teeth Pediatric EndodonticsDocument31 pagesEndodontic Therapy For Primary and Young Permanent Teeth Pediatric EndodonticsAthenaeum Scientific PublishersNo ratings yet
- Krok 2 Stomatology: Test Items For Licensing ExaminationDocument28 pagesKrok 2 Stomatology: Test Items For Licensing ExaminationjimmyNo ratings yet
- ICD 10 Kedokteran GigiDocument3 pagesICD 10 Kedokteran GigiAnggit PurwatiNo ratings yet