Professional Documents
Culture Documents
TOPIC1Chronic Forms of Coronary Heart Disease
TOPIC1Chronic Forms of Coronary Heart Disease
Uploaded by
Adi Pomeranz0 ratings0% found this document useful (0 votes)
8 views3 pages1. A 47-year-old man complains of chest pain during exertion and was diagnosed with chronic stable angina based on his symptoms and a normal ECG. A survey plan is proposed including exercise treadmill testing and potential imaging to further evaluate his coronary arteries and determine if revascularization is needed.
2. A 55-year-old woman complains of chest pain during exertion and was diagnosed with aortic stenosis based on her history of heart attack, enlarged heart on exam, murmur and ECG showing hypertrophy. Her treatment plan involves using echocardiography to further evaluate the severity of her aortic stenosis.
Original Description:
TOPIC1Chronic Forms of Coronary Heart Disease
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Document1. A 47-year-old man complains of chest pain during exertion and was diagnosed with chronic stable angina based on his symptoms and a normal ECG. A survey plan is proposed including exercise treadmill testing and potential imaging to further evaluate his coronary arteries and determine if revascularization is needed.
2. A 55-year-old woman complains of chest pain during exertion and was diagnosed with aortic stenosis based on her history of heart attack, enlarged heart on exam, murmur and ECG showing hypertrophy. Her treatment plan involves using echocardiography to further evaluate the severity of her aortic stenosis.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
0 ratings0% found this document useful (0 votes)
8 views3 pagesTOPIC1Chronic Forms of Coronary Heart Disease
TOPIC1Chronic Forms of Coronary Heart Disease
Uploaded by
Adi Pomeranz1. A 47-year-old man complains of chest pain during exertion and was diagnosed with chronic stable angina based on his symptoms and a normal ECG. A survey plan is proposed including exercise treadmill testing and potential imaging to further evaluate his coronary arteries and determine if revascularization is needed.
2. A 55-year-old woman complains of chest pain during exertion and was diagnosed with aortic stenosis based on her history of heart attack, enlarged heart on exam, murmur and ECG showing hypertrophy. Her treatment plan involves using echocardiography to further evaluate the severity of her aortic stenosis.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
You are on page 1of 3
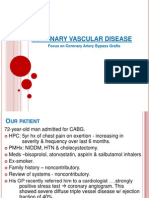
TOPIC1
Chronic forms of coronary heart disease (CHD)
1. A 47-year-old man complains of compressive pain behind the sternum during
accelerated walking, climbing 3 floor. He has been sick for 6 months.
Clinician-observed: Height - 172 cm, weight - 98 kg.
Lungs: vesicular breathing.
The borders of the heart are not shifted, the tones are muffled, the rhythm is correct,
heart rate = PS = 72 bpms., BP = 135/80 mm Hg.
The liver is not palpable, no swelling of the legs.
ECG is without changes. In the blood:
Red blood cells - 4.5*10¹², white blood cells - 7.0*10⁹, ESR - 5 mm / h.
Formulate a clinical diagnosis.
IHD: First established angina pectoris- Class I experience angina with strenuous or protracted
physical activity
Make a survey plan with rationale.
In chronic stable angina, typical history and presence of risk factors are the most important
information for diagnosis. The physical examination is usually not helpful but may provide
evidence of left ventricular systolic or diastolic dysfunction (S3 or S4, respectively). During an
attack of angina, patients tend to be still and may appear pale. The ECG is normal in more than
half of patients with coronary atherosclerosis, but there may be evidence of prior myocardial
infarction or ischemia (e.g., ST depression).
The three most important determinants of prognosis in patients with chronic stable angina are
age, number of diseased coronary arteries, and left ventricular function.
An exercise treadmill test can diagnose CAD by the development of ECG changes with
exercise. In addition, symptoms during exercise, blood pressure response, and duration of
exercise are all important in determining the post-test probability of CAD and whether the
patient needs further evaluation.
The treadmill test can be enhanced by assessing left ventricular wall motion (with
echocardiography) or myocardial perfusion (with nuclear imaging). Pharmacologic stress testing
can be used in patients who are unable to exercise.
The recent advent of 64-slice computed tomography (CT) scanners has enabled noninvasive
coronary angiography. Patients are given an intravenous bolus of contrast dye, and then the
coronary arteries are imaged. The usefulness of this test remains to be determined, but there are
promising data, especially in excluding CAD in low-risk patients.
CT angiography has several limitations, including significant radiation exposure, exposure to
contrast dye, the need to be in sinus rhythm, and an ability to tolerate relative bradycardia.
Direct coronary angiography remains the gold standard for diagnosing CAD.
This test, which involves direct injection of contrast dye into the coronary arteries, delineates the
location and severity of obstructive coronary disease. As such, angiography is a necessary
prerequisite for coronary revascularization through either percutaneous intervention or coronary
artery bypass surgery.
Left ventriculography, generally performed immediately before or after coronary angiography,
provides important information regarding intracardiac pressures and left ventricular function.
Clinically assessing the functional importance of intermediate lesions (lesions that appear to
obstruct 40% to 60% of the coronary lumen) may be difficult using coronary angiography alone.
This limitation can be partially overcome by using intracoronary ultrasound or by measuring
coronary flow velocity or intracoronary pressure changes during maximal hyperemia.
Define treatment tactics.
Nonpharmacologic Interventions Controlling risk factors for atherosclerosis is crucial. In
particular, patients should be advised on the need to lower the intake of cholesterol and saturated
fat in their diets, the importance of weight loss if obese, and the need to avoid tobacco. A regular
exercise program should be prescribed for all patients in whom it is feasible. An exercise stress
test can be used to determine safe levels of activity. Transmyocardial revascularization, enhanced
external counterpulsation, spinal cord stimulation, and sympathectomy are occasionally used in
patients who have refractory angina despite optimal medical treatment. Pharmacologic
Interventions Pharmacologic therapy for angina was traditionally directed at relieving symptoms.
More recently, medications have been classifi ed based on their effect on survival .
Medications that improve survival and decrease cardiovascular events in patients with CAD
include aspirin, hydroxymethyl glutaryl–coenzyme A (HMG-CoA) reductase inhibitors
(“statins”), and angiotensin-converting enzyme inhibitors.
In patients with prior myocardial infarction or left ventricular dysfunction, β-blockers also
reduce mortality. Medications that treat symptoms without improving survival include nitrates
and calcium channel blockers. The use of calcium channel blockers, with the exception of
amlodipine and felodipine, should be avoided in patients with left ventricular dysfunction.
Low-density lipoprotein (LDL) cholesterol levels should be aggressively lowered, even in
patients with ostensibly normal LDL levels, through the use of diet and statins. Recent guidelines
suggest that LDL cholesterol should be less than 70 mg/dL in patients with CAD. Blood pressure
should be closely monitored, with optimum levels below 140/90 mm Hg.
In diabetic patients, optimum levels are even lower, with the goal of diastolic blood pressures at
80 mm Hg or less. Patients must be strongly encouraged to quit smoking and offered
pharmacologic aids (e.g., nicotine patches, bupropion, varenicline) or support group help as
needed. Antioxidant vitamins have not been shown to be beneficial.
2. A 55-year-old woman complains of burning pain behind the sternum, which appears
while walking up to 200 meters, climbing 1 floor; interruptions in the work of the
heart. Considers herself sick since 2017, when she suffered from AMI. The same year
coronary angiography was performed (stenosis 85% in the right coronary artery was
revealed) and PCA stenting was performed.
No menstruation for 5 years.
Constantly takes beta-blockers, aspirin, when she is in pain - nitroglycerin.
Clinicianobserved: Lungs: vesicular breathing. The borders of the heart are extended
to the left +1 cm, tones are muffled, single extrasystoles, heart rate = 86 bpms, PS =
82 per minute, blood pressure = 155/85 mm Hg. The legs are pasty. Blood: White
blood cells - 5.6*10⁹, ESR - 12 mm / h. ECG - ventricular extrasystoles, left
ventricular hypertrophy.
Specify the most likely diagnosis.
AORTIC STENOSIS
What is your treatment tactic?
Although careful physical examination and electrocardiography can detect left
ventricular hypertrophy in moderate or severe obstruction, precise quantifi cation of
aortic stenosis requires echocardiography for anatomic assessment and evaluation of
left ventricular wall thickness, chamber size, and contractile performance.
Simultaneous Doppler studies should be performed to measure left ventricular outfl
ow velocity, mean transvalvular pressure gradient, and valve area. Invasive
assessment in the cardiac catheterization laboratory may be recommended in
symptomatic patients when noninvasive tests are inconclusive or there is discrepancy
between clinical and echocardiographic fi ndings.
You might also like
- AAFP Family Med Board QuestionsDocument96 pagesAAFP Family Med Board QuestionsKamil Hanna100% (2)
- AAFP Board Review ClinchersDocument53 pagesAAFP Board Review ClinchersJessica E Isom100% (2)
- Mksap 17 MCQ FullDocument282 pagesMksap 17 MCQ Fullfermann100% (1)
- Cardiac Function TestDocument8 pagesCardiac Function Testramanrajesh83100% (2)
- Review On Natural Language ProcessingDocument4 pagesReview On Natural Language ProcessingzemikeNo ratings yet
- Geron CardioDocument45 pagesGeron CardioApril AlomiaNo ratings yet
- 9 CsaDocument34 pages9 Csaمحمد بن الصادقNo ratings yet
- تقرير ضغط الدمDocument10 pagesتقرير ضغط الدمlyh355754No ratings yet
- Heart Transplant ContentDocument17 pagesHeart Transplant ContentrajNo ratings yet
- EpidemiologyDocument5 pagesEpidemiologyMylene MendozaNo ratings yet
- Question 1 of 10: AAFP Board Review Clinchers Cardio Quiz 1Document53 pagesQuestion 1 of 10: AAFP Board Review Clinchers Cardio Quiz 1angel_sagun_1No ratings yet
- Hemant Mahanand (201941103034) Case StudyDocument50 pagesHemant Mahanand (201941103034) Case StudyHemiNo ratings yet
- Yash 18ll8a CopyxxDocument13 pagesYash 18ll8a CopyxxPatel YashNo ratings yet
- Diagnostic Evaluation of The HeartDocument25 pagesDiagnostic Evaluation of The HeartClaire GidoNo ratings yet
- Abdominal Aortic AneurysmDocument10 pagesAbdominal Aortic AneurysmPrince K. TaileyNo ratings yet
- Question 1 of 10: AAFP Board Review Clinchers Cardio Quiz 1Document60 pagesQuestion 1 of 10: AAFP Board Review Clinchers Cardio Quiz 1pramesh1No ratings yet
- Acute Coronary SyndromeDocument46 pagesAcute Coronary SyndromeEmma Andaya100% (1)
- Prof - Dr.Medhat Ashmawy Professor of Cardiology, Tanta UniversityDocument104 pagesProf - Dr.Medhat Ashmawy Professor of Cardiology, Tanta UniversityIvana LmsNo ratings yet
- PracticeExam1 & 2Document160 pagesPracticeExam1 & 2Arash SamieiNo ratings yet
- Stress Test: BY: Jobelyn Delena Tunay, RNDocument92 pagesStress Test: BY: Jobelyn Delena Tunay, RNJobelyn TunayNo ratings yet
- Clinical Pearls CardiologyDocument6 pagesClinical Pearls CardiologyMaritza24No ratings yet
- Unit 4 Coronary Artery Disease and Ischaemic Heart Disease: StructureDocument37 pagesUnit 4 Coronary Artery Disease and Ischaemic Heart Disease: StructurebtaleraNo ratings yet
- Complete Heart BlockDocument13 pagesComplete Heart BlockSubhranil MaityNo ratings yet
- Clin Cardiology CasesDocument34 pagesClin Cardiology CasesSunny Singh0% (1)
- Coronary Artery Disease and StableDocument13 pagesCoronary Artery Disease and StableMuhammad GassanNo ratings yet
- CapricornDocument6 pagesCapricornMarkanthony256No ratings yet
- Practice Exam 1Document103 pagesPractice Exam 1aayceeNo ratings yet
- Diagnosis and Management in Peripheral Artery Disease EditedDocument5 pagesDiagnosis and Management in Peripheral Artery Disease Editedwahyu suparnoNo ratings yet
- Cardiac - Potpourri Rev 2015Document80 pagesCardiac - Potpourri Rev 2015Sanaz NikiNo ratings yet
- 475 FullDocument9 pages475 Fullvonnyandira28No ratings yet
- Cardiac Stress TestDocument5 pagesCardiac Stress TestKristianCapili100% (1)
- KillipsDocument12 pagesKillipsNhorlyn Adante SoltesNo ratings yet
- Hypertension in Geriatric PopulationDocument52 pagesHypertension in Geriatric PopulationDiana TiganucNo ratings yet
- Summary 2013 Esc GuidelinesDocument8 pagesSummary 2013 Esc GuidelinesNick StamatiadisNo ratings yet
- Media 115008 en PDFDocument12 pagesMedia 115008 en PDFsukandeNo ratings yet
- Coronary Vascular Disease: Focus On Coronary Artery Bypass GraftsDocument15 pagesCoronary Vascular Disease: Focus On Coronary Artery Bypass Graftstrion_hNo ratings yet
- Increased Arterial Blood PressureDocument25 pagesIncreased Arterial Blood PressureAjmalNo ratings yet
- Conrad Fischer MCQsDocument328 pagesConrad Fischer MCQsPopescu Tina100% (1)
- Acute Coronary Syndrome PDFDocument12 pagesAcute Coronary Syndrome PDFElsy MayjoNo ratings yet
- Clinical Exposure Vi Assignment: Faculty of Medicine Universitas Pelita HarapanDocument16 pagesClinical Exposure Vi Assignment: Faculty of Medicine Universitas Pelita HarapanSteven MatualiNo ratings yet
- Coronary Artery DiseaseDocument38 pagesCoronary Artery Diseaseshaitabligan100% (3)
- ACC Cardiovascular Board Review MCQ 2017Document64 pagesACC Cardiovascular Board Review MCQ 2017Adeel Lakhiar100% (1)
- Cerebrovascular AccidentDocument26 pagesCerebrovascular AccidentMustafa Aadan100% (1)
- Arterial Septal Defect (Asd)Document38 pagesArterial Septal Defect (Asd)Rhahima SyafrilNo ratings yet
- The Cardiovascular System ReviewDocument18 pagesThe Cardiovascular System ReviewDanisha Reeves100% (1)
- Final Hemodynamic MonitoringDocument6 pagesFinal Hemodynamic MonitoringchandhomepcNo ratings yet
- Coronary Artery Bypass Grafting: Coronary Bypass Surgery Is An Open-Heart Surgery, You MightDocument17 pagesCoronary Artery Bypass Grafting: Coronary Bypass Surgery Is An Open-Heart Surgery, You MightNuzhat FatimaNo ratings yet
- Symptoms, Diagnosis, TreatmentDocument17 pagesSymptoms, Diagnosis, TreatmentatanNo ratings yet
- Defibrillators in Nonischemic Cardiomyopathy Treatment EvaluationDocument7 pagesDefibrillators in Nonischemic Cardiomyopathy Treatment EvaluationYanahi Oropeza HidalgoNo ratings yet
- Hypertension: Hypertension Is One of The Most Common Worldwide Diseases Afflicting Humans. BecauseDocument8 pagesHypertension: Hypertension Is One of The Most Common Worldwide Diseases Afflicting Humans. BecauseKramojNo ratings yet
- The Effect of Cilostazol On Right Heart FunctionDocument43 pagesThe Effect of Cilostazol On Right Heart FunctionGunawan YogaNo ratings yet
- Hypertension Syakib Bakri - BPJS 2015 FINALDocument116 pagesHypertension Syakib Bakri - BPJS 2015 FINALPeriyent Liveryent VozzervodNo ratings yet
- Untitled DocumentDocument6 pagesUntitled DocumentCharlyn JenselNo ratings yet
- Cardiac Dysrhythmia Case StudyDocument6 pagesCardiac Dysrhythmia Case StudyCharlyn JenselNo ratings yet
- Flashcards - QuizletDocument7 pagesFlashcards - QuizletNEsreNo ratings yet
- Hemodynamics Basic Concepts 1204053445109897 4Document115 pagesHemodynamics Basic Concepts 1204053445109897 4valeriesolidum100% (1)
- Internal Medicine Lecture 4 Chronic Forms of Ischemic Heart DiseaseDocument59 pagesInternal Medicine Lecture 4 Chronic Forms of Ischemic Heart DiseaseAdi PomeranzNo ratings yet
- 11 Localization of Functions in Cortex-QDocument6 pages11 Localization of Functions in Cortex-QAdi PomeranzNo ratings yet
- 19 - 22 Inflammatory Diseases of Nervous SystemDocument37 pages19 - 22 Inflammatory Diseases of Nervous SystemAdi PomeranzNo ratings yet
- 16 Vascular Diseases of Nervous System-QDocument24 pages16 Vascular Diseases of Nervous System-QAdi PomeranzNo ratings yet
- 3-4 Extrapyramydal System-QDocument6 pages3-4 Extrapyramydal System-QAdi Pomeranz100% (1)
- Unit 2 PythonDocument37 pagesUnit 2 PythonANSH SINGHNo ratings yet
- You Exec - Cost Optimization FreeDocument7 pagesYou Exec - Cost Optimization FreeAta JaafatNo ratings yet
- Sensor Presion Barometrica NRG - BP60 - Tech - Product - Sheet - 2022 - V3 - WEBDocument2 pagesSensor Presion Barometrica NRG - BP60 - Tech - Product - Sheet - 2022 - V3 - WEBDOUSAN ALEUNo ratings yet
- 65458d2eb36b4ac4e91ab6f2 ZizodiwuDocument2 pages65458d2eb36b4ac4e91ab6f2 Zizodiwushahid94lhrNo ratings yet
- Raine 2002 PDFDocument32 pagesRaine 2002 PDFdiyei_patoNo ratings yet
- Here Is The MoonDocument2 pagesHere Is The MoonDeepakNo ratings yet
- 20 Must-Know Rocks Licks: Shuffle Lick 5Document3 pages20 Must-Know Rocks Licks: Shuffle Lick 5julyfriska100% (1)
- Verba Latina (Verbs)Document21 pagesVerba Latina (Verbs)Gladius GrandeNo ratings yet
- Radomiro Mechanical - Presenation SR800P9 150323Document44 pagesRadomiro Mechanical - Presenation SR800P9 150323Juan PerezNo ratings yet
- Georges A. Barrois, Jesus Christ and The Temple: Cărți Pentru TraducereDocument2 pagesGeorges A. Barrois, Jesus Christ and The Temple: Cărți Pentru TraducereAlin GogaNo ratings yet
- The Happy PrinceDocument3 pagesThe Happy PrinceLaurence UyNo ratings yet
- E4-E5 - Text - Chapter 3. OUTSOURCING - CONTRACT MANAGEMENTDocument12 pagesE4-E5 - Text - Chapter 3. OUTSOURCING - CONTRACT MANAGEMENTAGM S&M-CMNo ratings yet
- Price and Output Determination Under Monopolistic OnDocument13 pagesPrice and Output Determination Under Monopolistic OnShoaib Ahmed KhosoNo ratings yet
- Meeting 7 Unsupervised LearnignDocument95 pagesMeeting 7 Unsupervised LearnignAntonio VictoryNo ratings yet
- Unit1 FinalDocument132 pagesUnit1 FinalPiyush ChaturvediNo ratings yet
- Michael Stephen ResumeDocument2 pagesMichael Stephen ResumeMichael MololuwaNo ratings yet
- SL S185X501-25-03 (V00) INTEGRA ELTs Approvals - 0Document6 pagesSL S185X501-25-03 (V00) INTEGRA ELTs Approvals - 0ravi k singhNo ratings yet
- ExamplesDocument1 pageExamplesSwordhamza KyatNo ratings yet
- Ignou Assignment Wala Ehi 1 Solved Assignment 2018-19Document7 pagesIgnou Assignment Wala Ehi 1 Solved Assignment 2018-19NEW THINK CLASSES100% (1)
- Notes On Ropes & Wires SOT I 2012 Unit 4Document21 pagesNotes On Ropes & Wires SOT I 2012 Unit 4James MonishNo ratings yet
- Section 1 QNSDocument32 pagesSection 1 QNSKay HanNo ratings yet
- Jurisprudence Research Paper TopicsDocument5 pagesJurisprudence Research Paper TopicsAmandeep MalikNo ratings yet
- Reading 15 Analysis of Dividends and Share Repurchases - AnswersDocument31 pagesReading 15 Analysis of Dividends and Share Repurchases - AnswersNeerajNo ratings yet
- Cyber WorldDocument7 pagesCyber WorldPranya BatraNo ratings yet
- Characteristics of LDCsDocument22 pagesCharacteristics of LDCstinsaeres100% (2)
- Ford MotorsDocument4 pagesFord Motorssalman sheikhNo ratings yet
- Laptop Repair Course OutlineDocument1 pageLaptop Repair Course Outlineredant21ltd100% (1)
- 4-SSS SAS ASA and AAS Congruence PDFDocument4 pages4-SSS SAS ASA and AAS Congruence PDFAivie Jannelle Columna BejoNo ratings yet
- Literature Review of Home Automation Using BluetoothDocument8 pagesLiterature Review of Home Automation Using BluetoothaflsodoamNo ratings yet