Professional Documents
Culture Documents
새로운 혈액분석 장비 Abbott Alinityhq의 확장 적혈구 지표의 참고범위 설정
새로운 혈액분석 장비 Abbott Alinityhq의 확장 적혈구 지표의 참고범위 설정
Uploaded by
Paul Avelino CallupeOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
새로운 혈액분석 장비 Abbott Alinityhq의 확장 적혈구 지표의 참고범위 설정
새로운 혈액분석 장비 Abbott Alinityhq의 확장 적혈구 지표의 참고범위 설정
Uploaded by
Paul Avelino CallupeCopyright:
Available Formats
CROSSMARK_logo_3_Test 1/1
Letter to the Editor
Lab Med Online
Vol. 11, No. 2: 149-151, April 2021 진단혈액학
https://doi.org/10.47429/lmo.2021.11.2.149
https://crossmark-cdn.crossref.org/widget/v2.0/logos/CROSSMARK_Color_square.svg 2017-03-16
새로운 혈액분석 장비 Abbott Alinityhq의 확장 적혈구
지표의 참고범위 설정
Reference Values for Extended Red Blood Cell Parameters on the New Abbott Alinityhq
Hematology Analyzer
우광숙·정인화·안규대·한진영
Kwang-Sook Woo, M.D., In-Hwa Jeong, M.D., Gyu-Dae An, M.D., Jin-Yeong Han, M.D.
동아대학교병원 진단검사의학과
Departments of Laboratory Medicine, Dong-A University College of Medicine, Busan, Korea
Dear Editor: differences in technology and lack of standardization, there is a
Alinityhq (Abbott Diagnostics, Santa Clara, CA, USA) is a fully difference between the values of these parameters measured us-
optical hematology analyzer that provides a complete blood ing different instruments [5-8]. These differences imply that in-
count (CBC) with a 6-part white blood cell differential count, strument-specific reference ranges are necessary for clinical diag-
which includes the count of immature granulocytes (IGs). In addi- nosis. Therefore, this study aimed to establish reference ranges for
tion, red blood cells (RBCs) and platelets can also be analyzed us- extended RBC parameters measured with the new Abbott hema-
ing the optical technology. With advances in optical technology tology analyzer in Korean population.
and single cell analysis based on light scattered by isovolumetri- This study enrolled 770 healthy individuals (413 men and 357
cally sphered RBCs, extended RBC parameters have become women) from Dong-A University Hospital. Peripheral blood sam-
available. Advanced technology enables the measurement of the ples were obtained during periodic health checks. All samples
cellular hemoglobin (Hb) concentration in individual erythro- were analyzed using the new Abbott hematology analyzer. Blood
cytes as well as measurement of the volume of erythrocytes. was drawn into evacuated tubes containing K2-EDTA as antico-
These parameters provide clinical utility for the screening and di- agulant and the tubes were kept at ambient temperature for no
agnosis of various anemic and certain other conditions and moni- longer than 6 hours after blood collection. The data obtained
toring of treatment response [1-4]. For interpretation of the results, were analyzed to identify the underlying normal distribution in
reliable reference ranges are needed. However, most published men and women separately and the reference ranges were calcu-
data include only Western population; thus, there is a lack of de- lated as mean ± 2 standard deviations (SD). If no statistical differ-
finitive data on Asian or Korean population. Additionally, due to ence was detected between the data obtained for men and
women, then data of both the sexes were analyzed together. In
Corresponding author: Jin-Yeong Han, M.D., Ph.D.
https://orcid.org/0000-0003-0280-2739
cases of non-Gaussian distribution, non-parametric methods
Department of Laboratory Medicine, Dong-A University College of Medicine, were used for analysis. For comparing results between gender
26 Daesingongwon-ro, Seo-gu, Busan 49201, Korea
Tel: +82-51-240-5323, Fax: +82-51-255-9366, E-mail: jyhan@dau.ac.kr and age groups, standard statistical methods were used in the
MedCalc Statistical Software version 14.8.1 (MedCalc Software
Received: April 22, 2020
Revision received: June 10, 2020 bvba, Ostend, Belgium). The results of the reference ranges for
Accepted: June 16, 2020 extended RBC parameters are shown in Table 1. The data distri-
This article is available from https://www.labmedonline.org butions were considered to be Gaussian or non-Gaussian (non-
2021, Laboratory Medicine Online parametric) depending on the parameters. Gaussian distributions
This is an Open Access article distributed under the terms of the Creative Commons
Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/4.0/) were observed for hypochromic RBC and macrocytic RBC, while
which permits unrestricted non-commercial use, distribution, and reproduction in any
medium, provided the original work is properly cited. the remaining six parameters, including reticulocyte mean cor-
eISSN 2093-6338 www.labmedonline.org 149
우광숙 외: Reference Values for Extended RBC Parameters
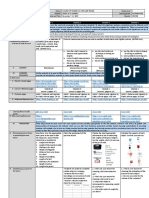
Table 1. Ranges of reference values of extended RBC parameters reticulocyte parameters; however, in our study, we observed dif-
Parameter (unit) Gender Mean ± 2SD 95th percentile ferences in all parameters except for HDW and MCVr. Moreover,
Microcytic RBC (%) Male 0.24-2.06 in our study, the values of microcytic RBC, macrocytic RBC, hy-
Female 0.23-7.14 pochromic RBC, and hyperchromic RBC were higher, and those
Macrocytic RBC (%) Male 0.09 ± 5.48
Female 0.73 ± 4.63
of HDW, MCVr, and MCHr were lower than the values reported in
Hypochromic RBC (%) Male 0.25-2.48 previous studies [11, 12]. Therefore, necessity for instrument- and
Female 0.27-13.26 population-specific reference ranges was confirmed.
Hyperchromic RBC (%) Male 0.06-0.56
However, the selection of healthy individuals as a reference
Female 0.04-0.30
HDW (%) Both 4.29-6.29 group may be difficult when dealing with parameters that can be
MCVr (fL) Both 82.39-101.61 abnormal even in apparently healthy subjects. In order to circum-
MCHr (pg) Male 26.52-32.44
vent these difficulties, we included subjects who were referred to
Female 23.86-31.88
MCHCr (g/dL) Male 30.17-32.98 a health care center for periodic health checks and in whom the
Female 29.87 ± 32.65 incidence of disease is much lower than in patients. We also in-
Abbreviations: RBC, red blood cell; SD, standard deviation; HDW, hemoglobin con- cluded a relatively wide range of age groups. However, we are not
centration distribution width; MCVr, mean cellular volume of reticulocytes; MCHr,
mean cellular hemoglobin content of reticulocytes; MCHCr, mean cellular hemo- sure whether patients were completely excluded from the dataset
globin concentration of reticulocytes. because we had not reviewed the medical records of all subjects.
Both laboratory scientists and clinicians need to be up-to-date
puscular volume (MCVr), reticulocyte mean corpuscular hemo- with new parameters and methods in hematology. Oftentimes,
globin (MCHr), microcytic RBC, hyperchromic RBC, hemoglobin the laboratory scientists introduce new parameters and their clini-
distribution width (HDW), and reticulocyte mean corpuscular he- cal utility to the clinicians. In summary, we established reference
moglobin concentration (MCHCr), exhibited non-Gaussian distri- ranges for extended RBC parameters measured with the new Ab-
bution. HDW and MCVr were identical for both the sexes. The bott hematology analyzer in healthy Korean population. Our
values of the other parameters (microcytic RBC, hyperchromic findings showed that there were statistically significant differ-
RBC, MCHr, and MCHCr) were higher in men than in women, ex- ences in reference values according to sex as well as ethnicity.
cept for hypochromic RBC and macrocytic RBC. Further studies specially focused on clinical usefulness of RBCs
Automated blood cell counters are becoming more sophisti- and RBC parameters in neonates, infants, and children are neces-
cated and the range of reportable parameters is ever increasing. sary.
Establishing reference ranges is the first step toward good labora-
tory practice and is essential for correct interpretation of labora- Conflicts of Interest
tory results, which helps ensure that reliable results are reported
to the clinician for decision-making. Procedures of how to estab- None declared.
lish reference intervals are described in international guidelines
and recommendations [9, 10]. In the literature, only few authors Acknowledgements
have reported reference ranges for extended RBC and reticulo-
cyte parameters, which are mainly based on data obtained from This work was supported by the National Research Foundation of
Western population [11, 12]. Previously, studies on the clinical use- Korea (NRF) grant funded by the Korea government (MSIP) (2018-
fulness of extended RBC and reticulocyte parameters measured R1A1A3A04078765).
using another hematology analyzer have been published; how-
ever, most of them have also evaluated on Western population [1- REFERENCES
8]. There are also controversies over the reference ranges. Hoff-
mann et al. [11] described that there were no differences between 1. Gilsanz F, Ricard MP, Millan I. Diagnosis of hereditary spherocytosis
women and men regarding the values of all extended RBC and with dual-angle differential light scattering. Am J Clin Pathol 1993;110:
150 www.labmedonline.org https://doi.org/10.47429/lmo.2021.11.2.149
우광숙 외: Reference Values for Extended RBC Parameters
119-22. pendent patients with end-stage renal disease on continuous erythro-
2. Ricard MP and Gilsanz F. Assessment of the severity of hereditary poietin receptor activator versus epoetin beta therapy. Acta Haematol
spherocytosis using routine haematological data obtained with dual 2010;124:27-33.
angle laser scattering cytometry. Clin Lab Haematol 1996;18:75-8. 8. Miwa N, Akiba T, Kimata N, Hamaguchi Y, Arakawa Y, Tamura T, et
3. Urrechaga E. Discriminant value of % microcytic/% hypochromic ra- al. Usefulness of measuring reticulocyte hemoglobin equivalent in the
tio in the differential diagnosis of microcytic anemia. Clin Chem Lab management of haemodialysis patients with iron deficiency. Int J Lab
Med 2008;46:1752-8. Hematol 2010;32:248-55.
4. Urrechaga E. Red blood cell microcytosis and hypochromia in the 9. Clinical and Laboratory Standards Institute. Defining, establishing,
differential diagnosis of iron deficiency and β-thalassaemia trait. Int J and verifying reference intervals in the clinical laboratory; Approved
Lab Hematol 2009;31:528-34. guideline-Third edition. CLSI guideline C28-A3. Wayne, PA: Clinical
5. Rehu M, Ahonen S, Punnonen K. The diagnostic accuracy of the per- and Laboratory Standards Institute, 2010.
centage of hypochromic red blood cells (%HYPOm) and cellular he- 10. Ichihara K and Boyd JC. An appraisal of statistical procedures used in
moglobin in reticulocytes (CHr) in differentiating iron deficiency ane- derivation of reference intervals. Clin Chem Lab Med 2010;48:1537-51.
mia and anemia of chronic diseases. Clin Chim Acta 2011;412:1809-13. 11. Hoffmann JJ, van den Broek NM, Curvers J. Reference intervals of ex-
6. Buttarello M, Temporin V, Ceravolo R, Farina G, Bulian P. The new re- tended erythrocyte and reticulocyte parameters. Clin Chem Lab Med
ticulocyte parameter (RET-Y) of the Sysmex XE 2100: its use in the di- 2012;50:941-8.
agnosis and monitoring of posttreatment sideropenic anemia. Am J 12. Teixeira C, Barbot J, Freitas MI. Reference values for reticulocyte pa-
Clin Pathol 2004;121:489-95. rameters and hypochromic RBC in healthy children. Int J Lab Hematol
7. Jonckheere S, Dierick J, Vanhouteghem H, Devleeschouwer M, Stove 2015;37:626-30.
V. Erythrocyte indices in the assessment of iron status in dialysis-de-
https://doi.org/10.47429/lmo.2021.11.2.149 www.labmedonline.org 151
You might also like
- Administrative Order No. 2010 0021 Sustainable Sanitation As A National PolicyDocument12 pagesAdministrative Order No. 2010 0021 Sustainable Sanitation As A National PolicyLaissa Arryanne SimNo ratings yet
- Global Centrifugal Pumps Market - 2022-32 - FMIDocument11 pagesGlobal Centrifugal Pumps Market - 2022-32 - FMITanaka ChiguvareNo ratings yet
- Carl Jung and The Visions of ZosimosDocument3 pagesCarl Jung and The Visions of ZosimosWolfMensch1216No ratings yet
- Research About Makahiya As Antibacterial AgentsDocument62 pagesResearch About Makahiya As Antibacterial AgentsSo What100% (1)
- Organizational Change A Review of Theory and Research in The 1990s Armenakis 1999Document24 pagesOrganizational Change A Review of Theory and Research in The 1990s Armenakis 1999Paul Avelino CallupeNo ratings yet
- Derived Hematology Reference Intervals For Healthy Males in Eastern IndiaDocument7 pagesDerived Hematology Reference Intervals For Healthy Males in Eastern IndiaSudhir BabuNo ratings yet
- cyto.b.21105Document6 pagescyto.b.21105angelicaalor2No ratings yet
- (Rev3)1-11 Determination of Complete Blood Count Reference Values of Mindray Bc-760 HematoloDocument11 pages(Rev3)1-11 Determination of Complete Blood Count Reference Values of Mindray Bc-760 HematolofirmianisaNo ratings yet
- Peripheral Blood Smear Pathologist ToolDocument3 pagesPeripheral Blood Smear Pathologist ToolSimon HafeniNo ratings yet
- Ok 3Document11 pagesOk 3cydolusNo ratings yet
- Impact Analysis of The Complete Blood Count Parameter Using Naive BayesDocument6 pagesImpact Analysis of The Complete Blood Count Parameter Using Naive BayesBrightworld ProjectsNo ratings yet
- Sindrom NefrotikDocument7 pagesSindrom NefrotikDania SaraswatiNo ratings yet
- Evaluation and Comparison of The New Mindray BC-6200 Hematology Analyzer With ADVIA 2120iDocument8 pagesEvaluation and Comparison of The New Mindray BC-6200 Hematology Analyzer With ADVIA 2120iGABRIELA HERRERANo ratings yet
- Evaluation of The Performance of The Sysmex XT-200Document11 pagesEvaluation of The Performance of The Sysmex XT-200Игорь БеняNo ratings yet
- Blood Group Testing: Hong-Yang Li and Kai GuoDocument11 pagesBlood Group Testing: Hong-Yang Li and Kai Guodkp rbmNo ratings yet
- Journal Reading Hematologi 4Document8 pagesJournal Reading Hematologi 4xastratariganNo ratings yet
- Comparison of Point-of-Care Measurement of Electrolyte Concentrations On Calculations of The Anion Gap and The Strong Ion DifferenceDocument8 pagesComparison of Point-of-Care Measurement of Electrolyte Concentrations On Calculations of The Anion Gap and The Strong Ion DifferenceMuhammad DaffaNo ratings yet
- Furosemide Stress Test As A Predictive Marker of Acute Kidney Injury Progression or Renal Replacement TherapyDocument13 pagesFurosemide Stress Test As A Predictive Marker of Acute Kidney Injury Progression or Renal Replacement Therapyjose luis iribarrenNo ratings yet
- Evaluation of The Abbott CELL-DYN 4000 HematologyDocument10 pagesEvaluation of The Abbott CELL-DYN 4000 Hematologypasamuco473No ratings yet
- Comparing The Efficacy and Safety of Apheresis and Whole Blood-Derived Platelet Transfusions - A Systematic ReviewDocument12 pagesComparing The Efficacy and Safety of Apheresis and Whole Blood-Derived Platelet Transfusions - A Systematic ReviewPritha BhuwapaksophonNo ratings yet
- Effective and Practical Complete Blood Count DeltaDocument7 pagesEffective and Practical Complete Blood Count Deltarince noveliaNo ratings yet
- HarrisADVIA2120methods LabHema2005 11 47-61 PDFDocument16 pagesHarrisADVIA2120methods LabHema2005 11 47-61 PDFedu_14cNo ratings yet
- Advia 2Document7 pagesAdvia 2Asmaa Nasr-El-DineNo ratings yet
- Evaluation of The Performance of Sysmex XN-3100 Automated Hematology Analyzer Regarding The Sysmex XE-2100 and Microscopic ExaminationDocument9 pagesEvaluation of The Performance of Sysmex XN-3100 Automated Hematology Analyzer Regarding The Sysmex XE-2100 and Microscopic ExaminationbalkisNo ratings yet
- (14374331 - Clinical Chemistry and Laboratory Medicine (CCLM) ) Analytical Evaluation of Four Faecal Immunochemistry Tests For HaemoglobinDocument6 pages(14374331 - Clinical Chemistry and Laboratory Medicine (CCLM) ) Analytical Evaluation of Four Faecal Immunochemistry Tests For HaemoglobinguschinNo ratings yet
- Spurious counts and spurious results on haematology analysers a review. Part I plateletsDocument17 pagesSpurious counts and spurious results on haematology analysers a review. Part I plateletsMezouar AbdennacerNo ratings yet
- An Artificial Intelligence-Assisted Diagnostic PlaDocument11 pagesAn Artificial Intelligence-Assisted Diagnostic Plahanrong912No ratings yet
- Cytometry Part B Clinical - 2020 - Illingworth - International Guidelines For The Flow Cytometric Evaluation of PeripheralDocument28 pagesCytometry Part B Clinical - 2020 - Illingworth - International Guidelines For The Flow Cytometric Evaluation of PeripheralUcha PrasetyoNo ratings yet
- Brereton Et Al-2016-International Journal of Laboratory HematologyDocument11 pagesBrereton Et Al-2016-International Journal of Laboratory HematologycindyNo ratings yet
- Gray-Matter Volume Estimate Score - A Novel Semi-Automatic Method Measuring Early Ischemic Change On CTDocument7 pagesGray-Matter Volume Estimate Score - A Novel Semi-Automatic Method Measuring Early Ischemic Change On CTkartini ciatawiNo ratings yet
- 173 FullDocument13 pages173 FullYaser MNo ratings yet
- Ok 2Document7 pagesOk 2cydolusNo ratings yet
- BMC - GcaDocument7 pagesBMC - GcaMuhammad Imran MirzaNo ratings yet
- Can Wearable DevicesDocument15 pagesCan Wearable DevicesJosé A. AristizabalNo ratings yet
- 1 s2.0 S0255085720315590 MainDocument4 pages1 s2.0 S0255085720315590 MainMahmoud FathyNo ratings yet
- Jalm 0366Document12 pagesJalm 0366Erick MartinezNo ratings yet
- KJR 20 880 PDFDocument14 pagesKJR 20 880 PDFNam LeNo ratings yet
- European Journal of Biomedical AND Pharmaceutical SciencesDocument5 pagesEuropean Journal of Biomedical AND Pharmaceutical SciencesGaurav AggarwalNo ratings yet
- Performance of CellaVision DM96 in Leukocyte ClassificationDocument5 pagesPerformance of CellaVision DM96 in Leukocyte ClassificationarielNo ratings yet
- HarrisADVIA2120methods LabHema2005 11 47-61 PDFDocument16 pagesHarrisADVIA2120methods LabHema2005 11 47-61 PDFSilvânia RochaNo ratings yet
- Reference Intervals For Serum Creatinine in Nepal.Document5 pagesReference Intervals For Serum Creatinine in Nepal.editorjmstNo ratings yet
- lvad112Document9 pageslvad112bruceayim30No ratings yet
- Systematic Review and Meta Analysis of Validated PDocument8 pagesSystematic Review and Meta Analysis of Validated Pevelynmoreirappgcmh.ufpaNo ratings yet
- Botero Et Al. - 2017 - Diagnostic Testing Approaches For Activated Protein C Resistance and Factor V LeidenA Comparison of InstitutionalDocument7 pagesBotero Et Al. - 2017 - Diagnostic Testing Approaches For Activated Protein C Resistance and Factor V LeidenA Comparison of InstitutionalnadaNo ratings yet
- 2017 Clin Lab Sci Doing and Zhang A Methodical Approach To Interpreting The RBC Parameters of The CBCDocument13 pages2017 Clin Lab Sci Doing and Zhang A Methodical Approach To Interpreting The RBC Parameters of The CBCJonathan MilhomensNo ratings yet
- Ok 1Document6 pagesOk 1cydolusNo ratings yet
- Study 3Document8 pagesStudy 3Suyash BagdeNo ratings yet
- Academic Emergency Medicine - 2011 - RossDocument9 pagesAcademic Emergency Medicine - 2011 - RossgomcoiteNo ratings yet
- Laboratory Hematology CriteriaDocument7 pagesLaboratory Hematology CriteriaRosNo ratings yet
- PRO 1 - MethodologyDocument9 pagesPRO 1 - MethodologyImran KhatriNo ratings yet
- Doppler-Based Renal Resistive Index For Prediction of Acute Kidney Injury in Critically Ill Patients - A Systematic Review and Meta-AnalysisDocument14 pagesDoppler-Based Renal Resistive Index For Prediction of Acute Kidney Injury in Critically Ill Patients - A Systematic Review and Meta-AnalysisMiftah Furqon AuliaNo ratings yet
- 01 02 03Document8 pages01 02 03alingh98No ratings yet
- CSF ParkinsonDocument4 pagesCSF ParkinsonYunita Christiani BiyangNo ratings yet
- Jurnal AlinDocument8 pagesJurnal Alinherlina armarianiNo ratings yet
- Guidance For Storing Blood Samples in Laboratories Performingcomplete Blood Count With DifferentialDocument6 pagesGuidance For Storing Blood Samples in Laboratories Performingcomplete Blood Count With Differentialimran ahmed siddiquiNo ratings yet
- 1 s2.0 S0169260718312252 MainDocument7 pages1 s2.0 S0169260718312252 MainWilder Gonzalez DiazNo ratings yet
- Research Article: Robust Method For Semantic Segmentation of Whole-Slide Blood Cell Microscopic ImagesDocument14 pagesResearch Article: Robust Method For Semantic Segmentation of Whole-Slide Blood Cell Microscopic ImagesSatish Kumar SattiNo ratings yet
- Verification of A Novel Point-Of-Care HbA1c DeviceDocument9 pagesVerification of A Novel Point-Of-Care HbA1c DeviceОксана КожокаруNo ratings yet
- 382-Article Text-1808-1-10-20210816Document8 pages382-Article Text-1808-1-10-20210816Dr. Asaad Mohammed Ahmed BabkerNo ratings yet
- Beckman Coulter, Sysmex, 2019Document10 pagesBeckman Coulter, Sysmex, 2019balkisNo ratings yet
- Cam4 10 5062Document16 pagesCam4 10 5062Sebastian ChavesNo ratings yet
- The Application of New Complex Indicators in The Detection of UrineDocument8 pagesThe Application of New Complex Indicators in The Detection of UrinePepin SalasNo ratings yet
- Blood Typing Using Chromatographic Separation On Antibody Treated PaperDocument7 pagesBlood Typing Using Chromatographic Separation On Antibody Treated PaperErika SantiagoNo ratings yet
- Evaluation of Automated Platelet Aggregation TestDocument7 pagesEvaluation of Automated Platelet Aggregation TestRafat ElshemiNo ratings yet
- Hematopathology: Advances in UnderstandingFrom EverandHematopathology: Advances in UnderstandingRenu SaxenaNo ratings yet
- Systematic Errors in Analytical Measurement ResultsDocument8 pagesSystematic Errors in Analytical Measurement ResultsPaul Avelino CallupeNo ratings yet
- Concepto de InertidumbreDocument6 pagesConcepto de InertidumbrePaul Avelino CallupeNo ratings yet
- Qualitative Research Methods in Health TechnologyDocument295 pagesQualitative Research Methods in Health TechnologyPaul Avelino CallupeNo ratings yet
- Gunn NeurodegenerationDocument9 pagesGunn NeurodegenerationPaul Avelino Callupe100% (1)
- Vaccines Variants PDFDocument5 pagesVaccines Variants PDFPaul Avelino CallupeNo ratings yet
- Brochure DM96Document12 pagesBrochure DM96Paul Avelino CallupeNo ratings yet
- Metabolites: Changes of Hematological and Hemorheological Parameters in Rabbits With HypercholesterolemiaDocument12 pagesMetabolites: Changes of Hematological and Hemorheological Parameters in Rabbits With HypercholesterolemiaPaul Avelino CallupeNo ratings yet
- Verification and Standardization of Blood Cell Counters For Routine Clinical Laboratory TestsDocument15 pagesVerification and Standardization of Blood Cell Counters For Routine Clinical Laboratory TestsPaul Avelino CallupeNo ratings yet
- HARLECO® Dyes & Stains: Microscopy Products To Support Your SuccessDocument8 pagesHARLECO® Dyes & Stains: Microscopy Products To Support Your SuccessPaul Avelino CallupeNo ratings yet
- Hematology Residency Training Program HandbookDocument319 pagesHematology Residency Training Program HandbookPaul Avelino CallupeNo ratings yet
- Continued Success in Providing Timely Palliative Radiation Therapy at The Rapid Response Radiotherapy Program: A Review of 2008-2012Document6 pagesContinued Success in Providing Timely Palliative Radiation Therapy at The Rapid Response Radiotherapy Program: A Review of 2008-2012Paul Avelino CallupeNo ratings yet
- 5-Westgard Quality Control 4 SlidesDocument9 pages5-Westgard Quality Control 4 SlidesPaul Avelino CallupeNo ratings yet
- Motallebi - 2019 - Full-Scale Testing of Stiffened Extended Shear Tab Connections Under Combined Axial and Shear ForcesDocument37 pagesMotallebi - 2019 - Full-Scale Testing of Stiffened Extended Shear Tab Connections Under Combined Axial and Shear ForcesaykutNo ratings yet
- Math7 Q2W2Document6 pagesMath7 Q2W2Meryl Fe P. GumeraNo ratings yet
- 24 PCM EncodingDocument4 pages24 PCM EncodingAli Mohammed Quasim MofasselNo ratings yet
- Construction Project Management 101 - ChecklistDocument5 pagesConstruction Project Management 101 - ChecklistUsman ShahidNo ratings yet
- Section 9 Solutions: Statistics 104 Spring 2020Document6 pagesSection 9 Solutions: Statistics 104 Spring 2020joshua arnettNo ratings yet
- Approved-Laboratories For COVID-19 TestDocument21 pagesApproved-Laboratories For COVID-19 TestAhmed ZaheerNo ratings yet
- Olympus 35 LCDocument25 pagesOlympus 35 LCHuy Nguyễn HữuNo ratings yet
- PNP and DSWD PartnershipDocument29 pagesPNP and DSWD Partnershiproneldayo62100% (1)
- Mom Chapter 5 (Torsion) - 20191108082142Document69 pagesMom Chapter 5 (Torsion) - 20191108082142PHILIP LIONEL PETERNo ratings yet
- Che313 Che333 Note BDocument78 pagesChe313 Che333 Note BIteoluwakiishi AberuagbaNo ratings yet
- Petron Risk ManagementDocument29 pagesPetron Risk ManagementfritzgeraldbulanNo ratings yet
- Environmental Science - Pollutants and Water PollutionDocument9 pagesEnvironmental Science - Pollutants and Water Pollutionaazadi47.mbp50No ratings yet
- 13 Energetics II PDFDocument11 pages13 Energetics II PDFSamson AmosNo ratings yet
- ISWM Practice ProblemsDocument4 pagesISWM Practice ProblemsApoorv DixitNo ratings yet
- Commercial Cooking NC Iii Rostering Staff: Company Agreements andDocument14 pagesCommercial Cooking NC Iii Rostering Staff: Company Agreements andCaracciolo CulinaryNo ratings yet
- IntesisHome FJ-RC-WIFI-1 Compatibility ListDocument15 pagesIntesisHome FJ-RC-WIFI-1 Compatibility ListFabian VázquezNo ratings yet
- TECHNICAL CATALOGUE - VSF - IEC - ATEX - EN - Rev1 - 2017 PDFDocument172 pagesTECHNICAL CATALOGUE - VSF - IEC - ATEX - EN - Rev1 - 2017 PDFLASCARZAMFIRESCUNo ratings yet
- Compensation Workbench: Presented by Ted Geary Natrona TechnologiesDocument28 pagesCompensation Workbench: Presented by Ted Geary Natrona TechnologieslistoNo ratings yet
- El Support Lesson Cause and Effect StructureDocument16 pagesEl Support Lesson Cause and Effect Structureapi-335012938100% (1)
- Zero Energy BuildingDocument7 pagesZero Energy BuildingIJRASETPublicationsNo ratings yet
- Fermentation: Bio Lab ManualDocument11 pagesFermentation: Bio Lab Manualthegp12No ratings yet
- The Artificial Ear Dilemma: The Challenges of Modern Handset TestingDocument13 pagesThe Artificial Ear Dilemma: The Challenges of Modern Handset TestingjulianpalacinoNo ratings yet
- 01-Modeling, Simulation, and Design of Hybrid EV Battery Charger For Optimum Grid Utilization, PSIMDocument108 pages01-Modeling, Simulation, and Design of Hybrid EV Battery Charger For Optimum Grid Utilization, PSIMViet Anh DoNo ratings yet
- BDA 100 - 01 Bridge Sample PlansDocument28 pagesBDA 100 - 01 Bridge Sample PlansCho Awa YanickNo ratings yet
- DLP in Math Grade 1 Week 2Document8 pagesDLP in Math Grade 1 Week 2Novelyn Lazo DucoNo ratings yet
- Gri Adis 2022Document79 pagesGri Adis 2022amellgothiqueNo ratings yet