Professional Documents
Culture Documents
007 - Cardiovascular Physiology) MASTER ECG
007 - Cardiovascular Physiology) MASTER ECG
Uploaded by
SWATHIKA LCopyright:
Available Formats
You might also like
- EKG Cheat SheetDocument9 pagesEKG Cheat SheetAlert Twitter100% (5)
- The 12-Lead Electrocardiogram for Nurses and Allied ProfessionalsFrom EverandThe 12-Lead Electrocardiogram for Nurses and Allied ProfessionalsNo ratings yet
- EKG Pocket GuideDocument2 pagesEKG Pocket GuideFabian Ramirez HincapiéNo ratings yet
- A Review On Coronary Artery Disease, Its Risk Factors, and TherapeuticsDocument12 pagesA Review On Coronary Artery Disease, Its Risk Factors, and TherapeuticsshishichanNo ratings yet
- IM Platinum 3rd-EdDocument357 pagesIM Platinum 3rd-EdJust Some Files100% (2)
- Cardiac ArrhythmiasDocument4 pagesCardiac Arrhythmiassmurf096No ratings yet
- EKG WorkbookDocument22 pagesEKG WorkbookZiac Lortab100% (1)
- Revised PPClues - 3-3-08Document16 pagesRevised PPClues - 3-3-08jeffjohnson909100% (2)
- DYSRHYTHMIAS (A.k.a. Arrhythmias) Disorders in TheDocument3 pagesDYSRHYTHMIAS (A.k.a. Arrhythmias) Disorders in TheDarell M. Book100% (1)
- Clinical Medicine Cheat Sheet Ebook PDFDocument18 pagesClinical Medicine Cheat Sheet Ebook PDFMoka100% (1)
- Backup of Goljan TransciptsDocument178 pagesBackup of Goljan TransciptsSarah RyanNo ratings yet
- Antibiotics Study Guide For NursesDocument3 pagesAntibiotics Study Guide For NursesLauren Trotman100% (7)
- 500 Single Best Answers in MedicineDocument443 pages500 Single Best Answers in Medicineasma .sassi100% (3)
- Protocolo FATE (Eco TT)Document4 pagesProtocolo FATE (Eco TT)darlingcarvajalduqueNo ratings yet
- ERC ALS Lecture 1 IntroductionDocument10 pagesERC ALS Lecture 1 IntroductioniamyourgasmanNo ratings yet
- Modul EKGDocument101 pagesModul EKGAjeng Dwik01No ratings yet
- Advanced Ekg Interpretation: Micelle J. Haydel, M.D. LSU New Orleans Emergency MedicineDocument88 pagesAdvanced Ekg Interpretation: Micelle J. Haydel, M.D. LSU New Orleans Emergency MedicineRoroNo ratings yet
- Pain 2. Pallor Poikylothermia Parasthesia Pulselessness Factor V Leiden (Activated Protein C Resistance)Document3 pagesPain 2. Pallor Poikylothermia Parasthesia Pulselessness Factor V Leiden (Activated Protein C Resistance)Ryan TurnerNo ratings yet
- EKG+Mastery +ischemia PDFDocument6 pagesEKG+Mastery +ischemia PDFCatur Ari Intan PuspitasariNo ratings yet
- Disorders Due To Hormone Deficiency (Hyposecretion) : List of Hormonal DisordersDocument2 pagesDisorders Due To Hormone Deficiency (Hyposecretion) : List of Hormonal Disordersritik shuklaNo ratings yet
- Arrhythmias: Sing Khien Tiong Gpst1Document34 pagesArrhythmias: Sing Khien Tiong Gpst1preethi preethaNo ratings yet
- Shock Cheat SheetDocument2 pagesShock Cheat SheetCindia LaiNo ratings yet
- Final PhysioDocument1,111 pagesFinal PhysioSana Savana Aman R100% (1)
- Classification of MurmursDocument2 pagesClassification of MurmursNazneen SiddiquiNo ratings yet
- 2 - Respiratory SystemDocument9 pages2 - Respiratory SystemHannah Grace CorveraNo ratings yet
- Cardiovascular I: CAD: Coronary Artery Disease (Most Common in US) Risk FactorsDocument4 pagesCardiovascular I: CAD: Coronary Artery Disease (Most Common in US) Risk FactorsJessica100% (1)
- Respiratory PathophysDocument1 pageRespiratory PathophysTori IkeharaNo ratings yet
- ECG Master Class-1Document132 pagesECG Master Class-1Shohag ID Center100% (1)
- Dysrhytmia NotesDocument11 pagesDysrhytmia NoteshannahhwolfNo ratings yet
- Ecg Interpretation New TemplateDocument88 pagesEcg Interpretation New TemplateJonathan NgNo ratings yet
- Heart Sounds: Mitral Regurgitation Congestive Heart FailureDocument6 pagesHeart Sounds: Mitral Regurgitation Congestive Heart FailurecindyNo ratings yet
- Approach To ArrhythmiasDocument1 pageApproach To ArrhythmiasADITYA SARANGINo ratings yet
- STEMI Mimics A Mnemonic.Document13 pagesSTEMI Mimics A Mnemonic.Simon Mark Daley100% (1)
- Cardiac PathophysiologyDocument36 pagesCardiac Pathophysiologykim suhoNo ratings yet
- Internal Medicine Table SummaryDocument31 pagesInternal Medicine Table SummaryShazaan Nadeem100% (1)
- Acid BaseDocument89 pagesAcid BaseEdouinaNo ratings yet
- Rhythm Strip ReviewDocument8 pagesRhythm Strip ReviewDouglas Greg Cook100% (2)
- ECG Interpretation in One PageDocument2 pagesECG Interpretation in One PageRyan AycockNo ratings yet
- Ecg Reading NotesDocument17 pagesEcg Reading NotesMarian FloresNo ratings yet
- Cardiology MnemonicsDocument12 pagesCardiology MnemonicsEliza SparkNo ratings yet
- Chart - WBC DisordersDocument1 pageChart - WBC DisordersSamuel RothschildNo ratings yet
- Alkalosis Acidosis ChartDocument1 pageAlkalosis Acidosis ChartrobingailNo ratings yet
- Respiratory System-Review PathoDocument100 pagesRespiratory System-Review PathoSadiePartington-Riopelle100% (1)
- Cardiac Murmurs - 1p Cheat Sheet PDFDocument1 pageCardiac Murmurs - 1p Cheat Sheet PDFPkernNo ratings yet
- Rhythm Interpretation and Its ManagementDocument6 pagesRhythm Interpretation and Its Managementjh_ajjNo ratings yet
- 3rd Lecture On Arrythmias by Dr. RoomiDocument16 pages3rd Lecture On Arrythmias by Dr. RoomiMudassar Roomi100% (2)
- DR K Chan - Ecg For SVT Made EasyDocument66 pagesDR K Chan - Ecg For SVT Made Easyapi-346486620No ratings yet
- Cardiac Physiology NotesDocument11 pagesCardiac Physiology Notespunter11100% (1)
- Abx FinalDocument3 pagesAbx Finalyanks1120No ratings yet
- Cardiac NotesDocument25 pagesCardiac Noteslovelyc95No ratings yet
- May/No P: Inverted/B/ A Qrs P (Befor e QRS) - 0.12Document3 pagesMay/No P: Inverted/B/ A Qrs P (Befor e QRS) - 0.12is_aradanas0% (1)
- ELECTROCARDIOGRAM by Aldrin Jayson AlmadenDocument23 pagesELECTROCARDIOGRAM by Aldrin Jayson AlmadenItsMe AJNo ratings yet
- 3rd Lecture On Cardiac Physiology by Dr. RoomiDocument11 pages3rd Lecture On Cardiac Physiology by Dr. RoomiMudassar Roomi100% (2)
- Ecg Taking and Interpretation.... PowerpointDocument37 pagesEcg Taking and Interpretation.... PowerpointJara Maris Moreno BudionganNo ratings yet
- My Cheat SheetDocument3 pagesMy Cheat SheetTenzin KyizomNo ratings yet
- Cardiac Rhythms and DysrhythmiasDocument14 pagesCardiac Rhythms and DysrhythmiasShawn Gaurav Jha100% (1)
- ECG InterpretationDocument40 pagesECG InterpretationMuhammad BadrushshalihNo ratings yet
- Properties of Cardiac Muscle and Conducting SystemsDocument38 pagesProperties of Cardiac Muscle and Conducting Systemsnirilib100% (4)
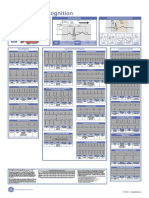
- Poster1 Arrhythmia Recognition e PDFDocument1 pagePoster1 Arrhythmia Recognition e PDFMiko RamosoNo ratings yet
- THE Electrocardiogram (ECG)Document13 pagesTHE Electrocardiogram (ECG)Bander Binjabaan Al-QahtaniNo ratings yet
- Umyu Ecg WorkshopDocument55 pagesUmyu Ecg WorkshopzainabhassansadaNo ratings yet
- ECG in 100 StepsDocument38 pagesECG in 100 StepsAlok MishraNo ratings yet
- Clinical Demonstration: Topic: Electrocardiogram (ECG)Document24 pagesClinical Demonstration: Topic: Electrocardiogram (ECG)soniya josephNo ratings yet
- Care Hospital Bhubaneswar - Doctors, Appointment, Charges, Other DetailsDocument7 pagesCare Hospital Bhubaneswar - Doctors, Appointment, Charges, Other DetailsSubhasish GiriNo ratings yet
- Relationship of Frontal QRS-T Angle With Syntax Score in Non-St Elevated Myocardial Infarction Patients in H. Adam Malik General Hospital MedanDocument8 pagesRelationship of Frontal QRS-T Angle With Syntax Score in Non-St Elevated Myocardial Infarction Patients in H. Adam Malik General Hospital MedanInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Biology Ecg Question 7Document2 pagesBiology Ecg Question 7Jumana SmairatNo ratings yet
- Trends in Prevalence and Control of Hypertension According To The 2017 American College of Cardiology/American Heart Association (ACC/AHA) GuidelineDocument11 pagesTrends in Prevalence and Control of Hypertension According To The 2017 American College of Cardiology/American Heart Association (ACC/AHA) GuidelineDiana Alvarez SedanoNo ratings yet
- Non-Invasive Cardiovascular ImagingDocument760 pagesNon-Invasive Cardiovascular ImagingOrlin ZlatarskiNo ratings yet
- Acls MegacodeDocument8 pagesAcls Megacodes33d_destinyNo ratings yet
- Textbook of Physiotherapy For Cardio-Respiratory Cardiac Surgery and Thoracic Surgery ConditionsDocument9 pagesTextbook of Physiotherapy For Cardio-Respiratory Cardiac Surgery and Thoracic Surgery ConditionsSuman DeyNo ratings yet
- Ekg Normal PapdiDocument51 pagesEkg Normal PapdifennyaliskaNo ratings yet
- Treatment MGRDocument12 pagesTreatment MGRMod AntbugNo ratings yet
- Kursus Ekg DR Ismi-1Document78 pagesKursus Ekg DR Ismi-1Sekar Ayu WulandariNo ratings yet
- 1500 Ebook Clinical Medicine Up PDFDocument215 pages1500 Ebook Clinical Medicine Up PDFAhmad Arif100% (1)
- Ebook Case Studies in Clinical Cardiac Electrophysiology PDF Full Chapter PDFDocument67 pagesEbook Case Studies in Clinical Cardiac Electrophysiology PDF Full Chapter PDFserafina.rios491100% (39)
- Preoperative Preparation and Postoperative CareDocument103 pagesPreoperative Preparation and Postoperative Carechowhan04No ratings yet
- Esc Guidelines For The Management of Heart Failure (Autosaved)Document80 pagesEsc Guidelines For The Management of Heart Failure (Autosaved)Ahmad AlKhataybehNo ratings yet
- Mohamed Abdel Shafy Mohammady Tabl - 7 - Safety of Ticagrelor Post Fibrinolysis in STEMI PatientsDocument60 pagesMohamed Abdel Shafy Mohammady Tabl - 7 - Safety of Ticagrelor Post Fibrinolysis in STEMI PatientsJovita SardanisNo ratings yet
- CME Cyanotic Heart DiseaseDocument38 pagesCME Cyanotic Heart DiseaseTan Zhi HongNo ratings yet
- Risk Factor For Atrial FibrilationDocument19 pagesRisk Factor For Atrial FibrilationDanny Soegianto IINo ratings yet
- AcceptedDocument28 pagesAcceptedChistian LassoNo ratings yet
- Pharmacology Review Questions For QuizDocument14 pagesPharmacology Review Questions For QuizusedforfunplocNo ratings yet
- Rheumatic Heart Disease Short Case PresentationDocument1 pageRheumatic Heart Disease Short Case PresentationPrerna SehgalNo ratings yet
- Topnotch ECG Interpretation For MoonlightersDocument25 pagesTopnotch ECG Interpretation For Moonlightersmefav7778520100% (1)
- Brunilda Alushi@Document3 pagesBrunilda Alushi@brunilda.alushiNo ratings yet
- Rundown Iaca 7Document2 pagesRundown Iaca 7Muh Anugerah YusroNo ratings yet
- A. Abnormal Blood Pressure Changes On ExerciseDocument1 pageA. Abnormal Blood Pressure Changes On ExerciseosamahihiNo ratings yet
007 - Cardiovascular Physiology) MASTER ECG
007 - Cardiovascular Physiology) MASTER ECG
Uploaded by
SWATHIKA LOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
007 - Cardiovascular Physiology) MASTER ECG
007 - Cardiovascular Physiology) MASTER ECG
Uploaded by
SWATHIKA LCopyright:
Available Formats
Last edited: 9/7/2021
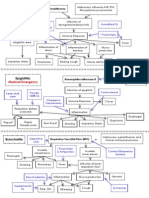
5. MASTER EKG INTERPRETATION
Master EKG Interpretation: A systematic approach for 12 Lead EKG Medical Editor: Maxine Abigale R. Bunao
OUTLINE
I) INTRODUCTION
II) ST SEGMENT AND ABNORMALITIES
III) T WAVE AND ABNORMALITIES
IV) QRS COMPLEX AND ABNORMALITIES
V) QT INTERVAL AND ABNORMALITIES
VI) P WAVE / PR INTERVAL AND ABNORMALITIES
VII) CARDIAC AXIS AND ABNORMALITIES
VIII) APPENDIX
IX) REVIEW QUESTIONS
X) REFRENCES
I) INTRODUCTION
(A) BASICS OF EKG
Table 1. Waveforms and interpretations.
WAVEFORM INTERPRETATION
P wave Positive Atrial depolarization
deflection (From the SA node spreads
throughout the atria)
PR Isoelectric line AV node depolarization
Segment
Period where all the electrical
activity from SA node converge
and come to the AV node, which
holds on to it and manifests as an
isoelectric line.
PR Interval - Time from when SA node fires > Figure 1. Parts of the heart the leads interpret.
AV node depolarization > getting
ready to send action potentials
down to ventricles
QRS Q – negative Ventricular depolarization
complex R – positive
S - negative
ST Isoelectric line Ventricular depolarization
Segment But no net electrical activity in
any direction, ventricles are just
holding on to it
T wave Positive Ventricular repolarization
deflection
QT Interval - Time period right before the Q
wave starts (ventricular
depolarization) up until the end of
T wave (ventricular
repolarization)
Lead Placements
o To pick up the electrical activity of the heart and put it
on an EKG graph Figure 2. Demonstration of large and small boxes'
measurements.
o Put different types of leads to determine the electrical
activity of the heart in different planes 1 Large box (thick outline)
o Width: 5 mm
Table 2. Parts of the heart the leads interpret. More important one which tells about the time or
Parts of the heart Limb Leads Chest Leads how long is it taking for this electrical activity to
move
RV aVR V1-V3
5 mm = 0.20 seconds
Basal septum V2-V3 o Height: 5 mm
Anterior wall of the - Determines the amplitude or voltage
V2-V4
heart 5 mm = 0.5 mv
High lateral wall of Lead I, avL 1 large box = 55 = 25 small boxes
V5-V6
the LV o 1 small box
Inferior wall of the Lead II, III, Width: 1 mm = 0.04 seconds
-
heart avF Height: 1 mm = 0.1 mv
• Important for measuring ST segment elevation
Master EKG Interpretation CARDIOVASCULAR PHYSIOLOGY : Note #5. 1 of 8
(A) RATE & RHYTHM (iv) QRS
o Width: Narrow or Wide?
Table 3. Bipolar limb leads and their placements. o <0.12 seconds or 3 small boxes = Narrow
Standard Bipolar Limb Leads (Vertical plane) o >0.12 seconds or 3 small boxes = Wide
Lead I (→) Lead II (↘) Lead III (↙)
(L) arm (+) (L) foot (+) (L) leg (+) (v) Sinus P-waves present?
(R) arm (-) (R) arm (-) (L) arm (-)
o Position:
Table 4. Augmented Unipolar Limb Leads and their
Upright P-wave in Lead II?
placements.
Augmented Unipolar Limb Leads (Vertical plane)
Inverted P-wave in Lead aVR?
Every P followed by QRS?
aVR aVL aVF
(R) arm (+) (L) arm (+) (L) foot (+) (vi) P-R Interval
o Time:
Table 5. Precordial chest leads and their placements. <0.2 seconds = Normal
Precordial Chest Leads (Horizontal plane) >0.2 seconds = Prolonged
V1 V2 V3 V4 V5 V6 Constant
4th ICS 4th ICS between 5th ICS 5th ICS 5th ICS Variable
(R) PSB (L) PSB V2 & V4 on (L) MCL (L) AAL (L) MAL
Progressively Longer
the (L)
Differential Diagnosis of Tachycardia
Table 6. Differential diagnosis of tachycardia.
EKG Strip
Pattern Differential Diagnosis
Sinus Tachycardia
Upright P waves in Lead III
Inverted P-wave in Lead aVR
Narrow + Regular Every P followed by QRS
2:1 Atrial Flutter
Supraventricular tachycardia
Atrial fibrillation (most common)
Narrow + Irregular Variable A-flutter
Multifocal atrial tachycardia
Figure 3. 12 Lead EKG strip. Ventricular tachycardia, until
(i) Rhythm strip (bottom) proven otherwise
Supraventricular tachycardia with
o Focuses on one of the 12 leads and continues for 10
Wide + Regular Bundle branch block
seconds in duration
o Usually used is Lead II Sinus tachycardia with Bundle
branch block
(ii) Rate Antidromic WPW
o Time: Polymorphic Supraventricular
Too Fast >100 = Tachycardia tachycardia
Too Slow <60 = Bradycardia Wide + Irregular Atrial fibrillation with WPW
Normal 60-100 = Normal Atrial fibrillation with Bundle
o To determine: branch block
Usually included in the print-out of the 12 Lead
EKG Differential Diagnosis of Bradycardia
• Usually, accurate Sinus bradycardia
• If there’s peaked T-wave, that can track off the A-V Blocks
T wave and the QRS complex Junctional rhythm
Box method Ventricular rhythm
• Measure the distance between 2 R waves
• Using big box = 300 / Count the boxes in
between them
• Using small box = 1500 / Count the boxes in
between them
R-Waves x 6
• Look at the rhythm strip
• Count how many R waves x 6
• Ex above: 9 R waves x 6 = 56 bpm
(iii) Rhythm
o Regularity: Regular or Irregular?
May use a card to mark 2 intervals. Compare the
width with the other R-R intervals.
o R-R interval constant? It’s regular.
o R-R interval NOT constant? It’s irregular.
2 of 8 CARDIOVASCULAR PHYSIOLOGY: Note #5. Master EKG Interpretation
II) ST SEGMENT AND ABNORMALITIES (3) J-Wave
What you need to determine in 12 lead EKG is what’s
going to kill the patient the quickest, so must look out for:
o arrhythmias
o ischemia or infarction
ST segments
(1) ST Elevation
Figure 6. J-waves.
Also called Osborne waves in a setting of hypothermia or
hypercalcemia
(i) CRITERIA
Figure 4. ST Elevation. o No S wave (doesn’t go down to the isoelectric point)
(i) CRITERIA: but produces like a downslope of the R wave
o Quick little positive deflection / wave before T wave
o Elevation in ANY lead J wave
o height of amplitude to be considered as elevated ST
segment: (ii) Differential Diagnosis
measure the mm above the isoelectric line J o Benign early repolarization
point J wave differentiates it from ST Segment
• 1 mm in any 2 contiguous leads except V2-V3 elevation, myocardial infarction
true ST segment elevation o Hypothermia
• 2 mm in V2-V3 true ST segment elevation o Hypercalcemia
o Brugada syndrome
(ii) Differential Diagnosis:
ST segment elevations
o STEMI Right bundle branch blocks
o Benign early repolarization Sometimes a visible J wave
o Pericarditis
o Vasospasm (Prinzmetal Angina) III) T WAVE AND ABNORMALITIES
o Pulmonary embolism
o LV Aneurysm Can also be a sign of impending ischemia or infarction
o LV Hypertrophy (1) T-wave inversion
o LBBB
Use Sgarbossa’s criteria
(2) ST Depression
Figure 7. T-wave inversion.
Normal: V1-V2, Lead III
(i) CRITERIA:
Figure 5. Morphology of ST Depression.
o ≥ 1 mm depression, below the isoelectric line or point
(i) CRITERIA: o T wave inversion in aVL only, suspicion of impending
inferior MI
o measure the mm from the J point until below the
isoelectric line (ii) Differential Diagnosis:
≥ 0.5 mm in any 2 contiguous leads true ST
o LVH Strain
depression
o Increased ICP (cerebral T waves)
o Horizontal ST depression: most concerning for
o Pulmonary embolism
ischemia
Seen in S1Q3T3 pattern
Do not send them home
o BBB
o Upsloping ST depression:
o Ischemia (Wellens B Criteria)
use De Winter T waves criteria in V1-V3 w/
T-wave inversions at Lead V2-V3
peaked T waves most concerning for LAD
occlusion
(ii) Differential Diagnosis:
o NSTEMI
o Posterior MI
ST depression
Upright T waves
Dominant R waves V1-V3
o LBBB
o LVH with Strain
o Reciprocal changes
o Digoxin toxicity
U or sagging type of down sloping ST depression
Master EKG Interpretation CARDIOVASCULAR PHYSIOLOGY : Note #5. 3 of 8
(2) Hyperacute T-Wave (5) Peaked T-Waves
Figure 11. Peaked T-wave.
Figure 8. Hyperacute T-wave.
(i) CRITERIA:
o Tall, narrow based, relatively symmetrically peaked
(i) CRITERIA: o >10 mm height
o tall & broad base (ii) Differential Diagnosis:
o asymmetrical peak
can fit the size of QRS inside of it o Hyperkalemia (first thing to think of)
o Hypermagnesemia
(ii) Differential Diagnosis: o Ischemia
o De Winters T wave
o Vasospasm
V1-V3 & Upsloping ST depression proximal
o Early STEMI especially if there’s a flat line going into
LAD occlusion
the peak
Upright peaked T waves
(3) Biphasic T-Wave
IV) QRS COMPLEX AND ABNORMALITIES
(1) Wide QRS
Figure 12. Wide QRS.
Figure 9. Biphasic T-wave. (i) CRITERIA:
o >0.12 seconds or 3 small boxes
CRITERIA o Indeterminate point: 0.10-0.12 seconds
o Upward wave immediately succeeded with downward
wave (ii) Differential Diagnosis:
o Alarming in V2-V3: o Bundle branch block
Fulfills Wellens A criteria Proximal LAD o Hyperkalemia
occlusion o Ventricular tachycardia
Differential Diagnosis: o Antidromic WPW Syndrome
o Hyperkalemia o Paced rhythm (with pacemaker)
o Drugs: TCA overdose
(4) Flat T-Wave
Figure 10. Flat T-wave.
(i) CRITERIA
o Differentiate from ST segment depression which is ≥ Figure 13. LBBB vs RBBB.
0.5-1 mm in any 2 contiguous leads below the
isoelectric line Left BBB
o Should be between -1 mm of depression up to 1 mm (iii) CRITERIA:
of elevation
V1-V2: Deep S wave, may sometimes form a bifid
(ii) Differential Diagnosis: pattern
o Ischemia V5-V6: positive deflection with a little dip on the
o Hypokalemia QRS, looks like letter “M”
(iv) Right BBB
o CRITERIA:
V1-V2: characteristics R-S-R’ (r prime) pattern
V5-V6: slurring of S wave
4 of 8 CARDIOVASCULAR PHYSIOLOGY: Note #5. Master EKG Interpretation
(2) Q-Wave (4) Poor R-Wave Progression
Figure 16. Poor R-wave Progression.
Normal: R wave exponentially increases from V1-V6
Figure 14. Q-wave. (i) Pathologic:
Can be a part of normal QRS complex o R wave doesn't progressively increase from V1-V6
o S wave is still a bit big in V5-V6
(i) PATHOLOGICAL CRITERIA:
o Never seen in V1-V3 (ii) Differential Diagnosis:
o >0.04 seconds or 1 small box o Anterior MI
o >2 mm deep from isoelectric line or point o RVH with Strain
o Measurement:
isoelectric line or point down to the bottom of Q
wave 25% of QRS complex (5) Dominant R-Wave Progression
(ii) Differential Diagnosis:
o Old or New Myocardial infarction
o Pulmonary embolism
o LBBB
o LVH
(3) Low Voltage QRS Figure 17. Dominant R-wave.
Normal: Smaller R waves and bigger S waves in V1-V3
(i) Pathologic:
o R wave > S waves in V1-V3 which means greater
impulse towards the right
o ST depression
o Upright T waves
Figure 15. Low voltage QRS.
(ii) Differential Diagnosis:
Something is blocking the impulse going to the electrodes o Posterior MI (first to think about)
o Fluid, fat, air o RBBB
o Heart is unable to generate / conduct enough action o RVH
potential (6) LVH & RVH
o Heart is floppy / weak
o Deposits within the heart
(i) CRITERIA:
o Summation of voltage of leads:
I + II + III = <15 mm OR
V1 + V2 + V3 = <30 mm
Figure 18. LVH vs RVH.
(ii) Differential Diagnosis: CRITERIA:
o Pericardial effusion (highest concern) LVH RVH
big concern w/ increased HR + Shortness of
V1-V2 - take the
breath V1-V2 - take the height (mm) in
height (mm) in S
o Obesity R wave
wave
o COPD
V5-V6 - take the
o Heart Failure V5-V6 - take the height (mm) in
height (mm) in R
o Infiltrative disease (rare): S wave
wave
Amyloidosis
Sarcoidosis Add both S wave and R wave
>10 mm
>35 mm Associated findings: RAD
Differential RVH due to:
Diagnosis: o Pulmonic stenosis
o Hypertension o Pulmonary hypertension
o Aortic stenosis due to COPD/ Interstitial
lung diseases
Master EKG Interpretation CARDIOVASCULAR PHYSIOLOGY : Note #5. 5 of 8
V) QT INTERVAL AND ABNORMALITIES VI) P WAVE / PR INTERVAL AND ABNORMALITIES
(1) Prolonged QT Interval (1) Right Atrial Enlargement (RAE)
Figure 19. Prolonged QT-interval.
(i) CRITERIA:
o Recall: Measured from point before Q wave until after
T- wave
o Female: Long >460 ms
o Male: >450 ms
o Requires QT-C for accurate measuring
Use Bazett’s formula to see if truly prolonged
o QT-interval should be aboult half of preceding R-R
interval Figure 21. RAE.
o Prolonged QT ↑ risk of Torsades de pointes which
can present as polymorphic ventricular tachycardia
(i) CRITERIA
o Lead II, III and aVF: >2.5 mm P-wave:
(ii) Differential Diagnosis: o Lead V1: Biphasic P-wave (+) deflection > (-)
o Antiarrhythmics deflection
o Antibiotics
o Antipsychotics (ii) Diagnosis:
o Antidepressants 2D ECHO
o Antiemetics o to see for atrial enlargement
o Ischemia
o Hypokalemia (iii) Differential Diagnosis:
o Hypomagnesemia Tricuspid valve stenosis
o Hypocalcemia o Pulmonary Hypertension
(2) Short QT Interval o Pulmonic Valve Stenosis
(2) Left Atrial Enlargement (LAE)
Figure 20. Short QT-interval.
Not as significant
(i) CRITERIA:
o Short <350 ms
(ii) Differential Diagnosis:
o Hyperkalemia
Figure 22. LAE.
o Hypermagnesemia
o Digoxin toxicity (i) CRITERIA:
o Lead II:
bifid camel's hump / P-wave > 0.04 second (1
small box)
o Lead V1:
Use to enhance diagnostic ability
Biphasic P-wave (-) deflection > (+) deflection
Explanation: Since impulse is pulled towards the
LA, it moves away from the positive electrode at
V1 (right inferior) so (-) deflection > (+)
deflection
(ii) Differential Diagnosis:
o Mitral valve stenosis
o Aortic valve stenosis
o Systemic HTN causes things to back up into the
pulmonary circulation ↑ blood volume and pressure
in the left atrium (LA)
6 of 8 CARDIOVASCULAR PHYSIOLOGY: Note #5. Master EKG Interpretation
(3) Short PR-Interval (2) Left Axis Deviation (LAD)
(i) Lead reading for R wave:
o Lead I R wave positive deflection Left thumb UP
o Lead aVF S wave negative deflection CHECK
Figure 23. Short PR-interval. Lead II
o Lead II negative deflection LAD
(i) CRITERIA:
bigger impulse directed to the left side of the heart
o <0.12 seconds (<3 small boxes) (ventricle)
ventricular depolarization moves primarily in the
(ii) Differential Diagnosis: left axis
o WPW Syndrome bigger S wave negative deflection
o Premature atrial contractions (PAC) in ectopic area
somewhere that fires quicker + closer to the AV node (ii) Causes:
= shortening of PR-interval o Obesity
(4) Prolonged PR-Interval Due to elevation of the diaphragmatic level
o LBBB: electrical activity has to come from the right
side to the left side
o LVH: thicker more electrical activity pushed to this
side
Figure 24. Prolonged PR-interval. o Inferior Myocardial infarction
o Hyperkalemia
(i) CRITERIA:
(3) Right Axis Deviation (RAD)
o >0.20s (>1 big box or >5 small boxes)
(i) Lead reading:
(ii) Differential Diagnosis:
o Lead II S wave negative deflection Left thumbs
o 1st Degree Heart block: same prolonged PR interval
DOWN
throughout the rhythm strip
o Lead aVF R wave positive deflection Right
o 2nd Degree Mobitz Type 1: prolongation
thumb UP RAD
progressively gets longer and longer throughout the
Since ventricular depolarization is more deviated
rhythm strip
to the right and approaches the location of the (+)
o 3rd Degree Heart block: variable prolongation
electrode bigger positive deflection
throughout the rhythm strip
(ii) Causes:
VII) CARDIAC AXIS AND ABNORMALITIES
o Extremely thin people
o RBBB
Causes the left side of the heart to bring electrical
activity to the right side
o RVH
Thick Right ventricle ↑ electrical activity
o Anterior MI
o Ventricular tachycardia
↑ electrical activity originating from the left side of
the heart which gets pushed to the right side of
the heart
Figure 25. Cardiac axis and abnormalities. (4) Extreme Right Axis Deviation (ERAD)
(1) Normal Axis (i) Lead reading:
(i) Based on 2 leads: o Lead II S wave negative deflection Left thumbs
DOWN
o Lead I Left thumb
o aVF S wave negative deflection Left thumbs
o Lead aVF Right thumb
DOWN
(ii) R wave deflection:
(ii) Causes:
o Setting 1:
o Extreme RVH: RV pulls ↑ electrical activity to it
Lead I positive deflection Left thumb UP
o Ventricular tachycardia:
Lead aVF positive deflection Right thumb UP
Electrical focus developing within the left side ↑
Both thumbs up = normal axis
electrical activity towards the right side
o Setting 2:
o Extremely thin individuals
Lead I positive deflection Left thumb UP
Lead aVF positive deflection BUT S wave is
bigger, predominant Right thumb DOWN
Lead II: always look at this IF Lead I up, Lead aVF
down
• You base LAD diagnosis on the presence of R
wave in Lead II
• Lead II positive deflection Normal Axis
• Lead II negative deflection LAD
Master EKG Interpretation CARDIOVASCULAR PHYSIOLOGY : Note #5. 7 of 8
VIII) APPENDIX
Table 7. Abbreviations.
AAL Anterior axillary line
BBB Bundle branch block
LA Left atrium
LAD Left axis deviation
LAE Left atrial enlargement
MAL Mid-axillary line
MCL Midclavicular line
PSB Parasternal border
RAD Right axis deviation
RAE Right atrial enlargement
RV Right ventricle
RVH Right ventricular hypertrophy
IX) REVIEW QUESTIONS X) REFRENCES
● Le T, Bhushan V, Sochat M, Chavda Y, Zureick A. First Aid for
1) After checking the EKG strip, you find out the USMLE Step 1 2018. New York, NY: McGraw-Hill Medical; 2017
aberrancies in Leads I and aVF. Lead I has a positive ● Mancini MC. Heart Anatomy. In: Berger S Heart Anatomy. New
deflection for its R-wave but aVF reveals negative York, NY: WebMD.https://emedicine.medscape.com/article/905502-
overview.
deflection for its S-wave. What is your next step of ● Hill M. Cardiovascular System - Heart Histology.
action? https://embryology.med.unsw.edu.au/embryology/index.php/Cardiov
a) Diagnose the patient with Left axis deviation ascular_System_-_Heart_Histology. Rosen IM and Manaker S.
Oxygen delivery and consumption. In: Post TW, ed. UpToDate .
b) Check first Lead II. Diagnose with Left axis deviation ● Waltham, MA:
if found to have a negative deflection for S wave in UpToDate.https://www.uptodate.com/contents/oxygen-delivery-and-
Lead II. consumption#H4.
● McCorry LK. Physiology of the Autonomic Nervous System. Am
c) Check first Lead II. Diagnose with Left axis deviation
J Pharm Educ .2007; 71(4): p.78. doi: 10.5688/aj710478.
if found to have a positive deflection for S wave in ● Standring S. Gray's Anatomy: The Anatomical Basis of Clinical
Lead II. Practice. Elsevier Health Sciences; 2016
d) This is still considered a normal axis. ● Leslie P. Gartner, James L. Hiatt. Color Textbook of Histology.
New York (NY): Grune & Stratton Inc.; 2006
2) As the clinical intern on duty, you were tasked to ● U. S. National Institutes of Health, National Cancer Institute. NIH
SEER Training Modules - Classification & Structure of Blood
read the EKG strip of the patient. You noticed the Vessels.
width of the QRS interval was beyond 3 small boxes, https://training.seer.cancer.gov/anatomy/cardiovascular/blood/classi
or >0.12 seconds. What differentials should you fication.html.
● Ostenfeld E, Flachskampf FA. Assessment of right ventricular
consider?
volumes and ejection fraction by echocardiography: from geometric
a) Bundle branch block approximations to realistic shapes. Echo research and practice
b) Hypokalemia .2015; 2(1): p.R1-R11. doi: 10.1530/ERP-14-0077.
c) TCA overdose ● Maceira AM, Prasad SK, Khan M, Pennell DJ. Reference right
ventricular systolic and diastolic function normalized to age, gender
d) Ventricular fibrillation and body surface area from steady-state free precession
e) A & C cardiovascular magnetic resonance.. Eur Heart J .2006; 27(23):
f) B & D p.2879-88. doi: 10.1093/eurheartj/ehl336. Klabunde RE.
Hemorrhagic Shock.
3) When considering STEMI, what should you find in http://www.cvphysiology.com/Blood%20Pressure/BP031.
the EKG strip? ● Drucker WR, Chadwick CD, Gann DS. Transcapillary refill in
hemorrhage and shock.. Arch Surg .1981; 116(10): p.1344-53.
a) ST segment Elevation of 1 mm above the isoelectric pmid: 7283706.
line to the J point, in any 2 contiguous leads except ● Kaur P, Basu S, Kaur G, Kaur R. Transfusion protocol in
V2-V3 trauma. J Emerg Trauma Shock .2011; 4(1): p.103. doi:
10.4103/0974-2700.76844.
b) ST segment Elevation of 2 mm above the isoelectric ● Campbell RL, Li JTC, Nicklas RA, Sadosty AT. Emergency
line to the J point, in any 2 contiguous leads except department diagnosis and treatment of anaphylaxis: a practice
V2-V3 parameter. Ann Allergy Asthma Immunol .2014; 113(6): p.599-608.
doi: 10.1016/j.anai.2014.10.007
c) ST segment Elevation of 2 mm above the isoelectric ● Consortium for Spinal Cord Medicine. Early acute management
line to the J point, in any 2 contiguous leads except in adults with spinal cord injury: A clinical practice guideline for
V1-V2 health-care professionals.. J Spinal Cord Med .2008; 31(4): p.403-
79. pmid: 18959359.
d) None of the above. ● Marieb EN, Hoehn K. Anatomy & Physiology. Hoboken, NJ:
4) To differentiate RVH from LVH, Pearson; 2020. Boron WF, Boulpaep EL. Medical Physiology.;
2017. "
a) You must add the heights (mm) of S wave in leads
V1-V2 with the heights (mm) of R wave in leads V5-
V6, which must exceed >35 mm
b) You must add the heights (mm) of R wave in leads
V1-V2 with the heights (mm) of S wave in leads V5-
V6, which must exceed >10 mm
c) Both
CHECK YOUR ANSWERS
8 of 8 CARDIOVASCULAR PHYSIOLOGY: Note #5. Master EKG Interpretation
You might also like
- EKG Cheat SheetDocument9 pagesEKG Cheat SheetAlert Twitter100% (5)
- The 12-Lead Electrocardiogram for Nurses and Allied ProfessionalsFrom EverandThe 12-Lead Electrocardiogram for Nurses and Allied ProfessionalsNo ratings yet
- EKG Pocket GuideDocument2 pagesEKG Pocket GuideFabian Ramirez HincapiéNo ratings yet
- A Review On Coronary Artery Disease, Its Risk Factors, and TherapeuticsDocument12 pagesA Review On Coronary Artery Disease, Its Risk Factors, and TherapeuticsshishichanNo ratings yet
- IM Platinum 3rd-EdDocument357 pagesIM Platinum 3rd-EdJust Some Files100% (2)
- Cardiac ArrhythmiasDocument4 pagesCardiac Arrhythmiassmurf096No ratings yet
- EKG WorkbookDocument22 pagesEKG WorkbookZiac Lortab100% (1)
- Revised PPClues - 3-3-08Document16 pagesRevised PPClues - 3-3-08jeffjohnson909100% (2)
- DYSRHYTHMIAS (A.k.a. Arrhythmias) Disorders in TheDocument3 pagesDYSRHYTHMIAS (A.k.a. Arrhythmias) Disorders in TheDarell M. Book100% (1)
- Clinical Medicine Cheat Sheet Ebook PDFDocument18 pagesClinical Medicine Cheat Sheet Ebook PDFMoka100% (1)
- Backup of Goljan TransciptsDocument178 pagesBackup of Goljan TransciptsSarah RyanNo ratings yet
- Antibiotics Study Guide For NursesDocument3 pagesAntibiotics Study Guide For NursesLauren Trotman100% (7)
- 500 Single Best Answers in MedicineDocument443 pages500 Single Best Answers in Medicineasma .sassi100% (3)
- Protocolo FATE (Eco TT)Document4 pagesProtocolo FATE (Eco TT)darlingcarvajalduqueNo ratings yet
- ERC ALS Lecture 1 IntroductionDocument10 pagesERC ALS Lecture 1 IntroductioniamyourgasmanNo ratings yet
- Modul EKGDocument101 pagesModul EKGAjeng Dwik01No ratings yet
- Advanced Ekg Interpretation: Micelle J. Haydel, M.D. LSU New Orleans Emergency MedicineDocument88 pagesAdvanced Ekg Interpretation: Micelle J. Haydel, M.D. LSU New Orleans Emergency MedicineRoroNo ratings yet
- Pain 2. Pallor Poikylothermia Parasthesia Pulselessness Factor V Leiden (Activated Protein C Resistance)Document3 pagesPain 2. Pallor Poikylothermia Parasthesia Pulselessness Factor V Leiden (Activated Protein C Resistance)Ryan TurnerNo ratings yet
- EKG+Mastery +ischemia PDFDocument6 pagesEKG+Mastery +ischemia PDFCatur Ari Intan PuspitasariNo ratings yet
- Disorders Due To Hormone Deficiency (Hyposecretion) : List of Hormonal DisordersDocument2 pagesDisorders Due To Hormone Deficiency (Hyposecretion) : List of Hormonal Disordersritik shuklaNo ratings yet
- Arrhythmias: Sing Khien Tiong Gpst1Document34 pagesArrhythmias: Sing Khien Tiong Gpst1preethi preethaNo ratings yet
- Shock Cheat SheetDocument2 pagesShock Cheat SheetCindia LaiNo ratings yet
- Final PhysioDocument1,111 pagesFinal PhysioSana Savana Aman R100% (1)
- Classification of MurmursDocument2 pagesClassification of MurmursNazneen SiddiquiNo ratings yet
- 2 - Respiratory SystemDocument9 pages2 - Respiratory SystemHannah Grace CorveraNo ratings yet
- Cardiovascular I: CAD: Coronary Artery Disease (Most Common in US) Risk FactorsDocument4 pagesCardiovascular I: CAD: Coronary Artery Disease (Most Common in US) Risk FactorsJessica100% (1)
- Respiratory PathophysDocument1 pageRespiratory PathophysTori IkeharaNo ratings yet
- ECG Master Class-1Document132 pagesECG Master Class-1Shohag ID Center100% (1)
- Dysrhytmia NotesDocument11 pagesDysrhytmia NoteshannahhwolfNo ratings yet
- Ecg Interpretation New TemplateDocument88 pagesEcg Interpretation New TemplateJonathan NgNo ratings yet
- Heart Sounds: Mitral Regurgitation Congestive Heart FailureDocument6 pagesHeart Sounds: Mitral Regurgitation Congestive Heart FailurecindyNo ratings yet
- Approach To ArrhythmiasDocument1 pageApproach To ArrhythmiasADITYA SARANGINo ratings yet
- STEMI Mimics A Mnemonic.Document13 pagesSTEMI Mimics A Mnemonic.Simon Mark Daley100% (1)
- Cardiac PathophysiologyDocument36 pagesCardiac Pathophysiologykim suhoNo ratings yet
- Internal Medicine Table SummaryDocument31 pagesInternal Medicine Table SummaryShazaan Nadeem100% (1)
- Acid BaseDocument89 pagesAcid BaseEdouinaNo ratings yet
- Rhythm Strip ReviewDocument8 pagesRhythm Strip ReviewDouglas Greg Cook100% (2)
- ECG Interpretation in One PageDocument2 pagesECG Interpretation in One PageRyan AycockNo ratings yet
- Ecg Reading NotesDocument17 pagesEcg Reading NotesMarian FloresNo ratings yet
- Cardiology MnemonicsDocument12 pagesCardiology MnemonicsEliza SparkNo ratings yet
- Chart - WBC DisordersDocument1 pageChart - WBC DisordersSamuel RothschildNo ratings yet
- Alkalosis Acidosis ChartDocument1 pageAlkalosis Acidosis ChartrobingailNo ratings yet
- Respiratory System-Review PathoDocument100 pagesRespiratory System-Review PathoSadiePartington-Riopelle100% (1)
- Cardiac Murmurs - 1p Cheat Sheet PDFDocument1 pageCardiac Murmurs - 1p Cheat Sheet PDFPkernNo ratings yet
- Rhythm Interpretation and Its ManagementDocument6 pagesRhythm Interpretation and Its Managementjh_ajjNo ratings yet
- 3rd Lecture On Arrythmias by Dr. RoomiDocument16 pages3rd Lecture On Arrythmias by Dr. RoomiMudassar Roomi100% (2)
- DR K Chan - Ecg For SVT Made EasyDocument66 pagesDR K Chan - Ecg For SVT Made Easyapi-346486620No ratings yet
- Cardiac Physiology NotesDocument11 pagesCardiac Physiology Notespunter11100% (1)
- Abx FinalDocument3 pagesAbx Finalyanks1120No ratings yet
- Cardiac NotesDocument25 pagesCardiac Noteslovelyc95No ratings yet
- May/No P: Inverted/B/ A Qrs P (Befor e QRS) - 0.12Document3 pagesMay/No P: Inverted/B/ A Qrs P (Befor e QRS) - 0.12is_aradanas0% (1)
- ELECTROCARDIOGRAM by Aldrin Jayson AlmadenDocument23 pagesELECTROCARDIOGRAM by Aldrin Jayson AlmadenItsMe AJNo ratings yet
- 3rd Lecture On Cardiac Physiology by Dr. RoomiDocument11 pages3rd Lecture On Cardiac Physiology by Dr. RoomiMudassar Roomi100% (2)
- Ecg Taking and Interpretation.... PowerpointDocument37 pagesEcg Taking and Interpretation.... PowerpointJara Maris Moreno BudionganNo ratings yet
- My Cheat SheetDocument3 pagesMy Cheat SheetTenzin KyizomNo ratings yet
- Cardiac Rhythms and DysrhythmiasDocument14 pagesCardiac Rhythms and DysrhythmiasShawn Gaurav Jha100% (1)
- ECG InterpretationDocument40 pagesECG InterpretationMuhammad BadrushshalihNo ratings yet
- Properties of Cardiac Muscle and Conducting SystemsDocument38 pagesProperties of Cardiac Muscle and Conducting Systemsnirilib100% (4)
- Poster1 Arrhythmia Recognition e PDFDocument1 pagePoster1 Arrhythmia Recognition e PDFMiko RamosoNo ratings yet
- THE Electrocardiogram (ECG)Document13 pagesTHE Electrocardiogram (ECG)Bander Binjabaan Al-QahtaniNo ratings yet
- Umyu Ecg WorkshopDocument55 pagesUmyu Ecg WorkshopzainabhassansadaNo ratings yet
- ECG in 100 StepsDocument38 pagesECG in 100 StepsAlok MishraNo ratings yet
- Clinical Demonstration: Topic: Electrocardiogram (ECG)Document24 pagesClinical Demonstration: Topic: Electrocardiogram (ECG)soniya josephNo ratings yet
- Care Hospital Bhubaneswar - Doctors, Appointment, Charges, Other DetailsDocument7 pagesCare Hospital Bhubaneswar - Doctors, Appointment, Charges, Other DetailsSubhasish GiriNo ratings yet
- Relationship of Frontal QRS-T Angle With Syntax Score in Non-St Elevated Myocardial Infarction Patients in H. Adam Malik General Hospital MedanDocument8 pagesRelationship of Frontal QRS-T Angle With Syntax Score in Non-St Elevated Myocardial Infarction Patients in H. Adam Malik General Hospital MedanInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Biology Ecg Question 7Document2 pagesBiology Ecg Question 7Jumana SmairatNo ratings yet
- Trends in Prevalence and Control of Hypertension According To The 2017 American College of Cardiology/American Heart Association (ACC/AHA) GuidelineDocument11 pagesTrends in Prevalence and Control of Hypertension According To The 2017 American College of Cardiology/American Heart Association (ACC/AHA) GuidelineDiana Alvarez SedanoNo ratings yet
- Non-Invasive Cardiovascular ImagingDocument760 pagesNon-Invasive Cardiovascular ImagingOrlin ZlatarskiNo ratings yet
- Acls MegacodeDocument8 pagesAcls Megacodes33d_destinyNo ratings yet
- Textbook of Physiotherapy For Cardio-Respiratory Cardiac Surgery and Thoracic Surgery ConditionsDocument9 pagesTextbook of Physiotherapy For Cardio-Respiratory Cardiac Surgery and Thoracic Surgery ConditionsSuman DeyNo ratings yet
- Ekg Normal PapdiDocument51 pagesEkg Normal PapdifennyaliskaNo ratings yet
- Treatment MGRDocument12 pagesTreatment MGRMod AntbugNo ratings yet
- Kursus Ekg DR Ismi-1Document78 pagesKursus Ekg DR Ismi-1Sekar Ayu WulandariNo ratings yet
- 1500 Ebook Clinical Medicine Up PDFDocument215 pages1500 Ebook Clinical Medicine Up PDFAhmad Arif100% (1)
- Ebook Case Studies in Clinical Cardiac Electrophysiology PDF Full Chapter PDFDocument67 pagesEbook Case Studies in Clinical Cardiac Electrophysiology PDF Full Chapter PDFserafina.rios491100% (39)
- Preoperative Preparation and Postoperative CareDocument103 pagesPreoperative Preparation and Postoperative Carechowhan04No ratings yet
- Esc Guidelines For The Management of Heart Failure (Autosaved)Document80 pagesEsc Guidelines For The Management of Heart Failure (Autosaved)Ahmad AlKhataybehNo ratings yet
- Mohamed Abdel Shafy Mohammady Tabl - 7 - Safety of Ticagrelor Post Fibrinolysis in STEMI PatientsDocument60 pagesMohamed Abdel Shafy Mohammady Tabl - 7 - Safety of Ticagrelor Post Fibrinolysis in STEMI PatientsJovita SardanisNo ratings yet
- CME Cyanotic Heart DiseaseDocument38 pagesCME Cyanotic Heart DiseaseTan Zhi HongNo ratings yet
- Risk Factor For Atrial FibrilationDocument19 pagesRisk Factor For Atrial FibrilationDanny Soegianto IINo ratings yet
- AcceptedDocument28 pagesAcceptedChistian LassoNo ratings yet
- Pharmacology Review Questions For QuizDocument14 pagesPharmacology Review Questions For QuizusedforfunplocNo ratings yet
- Rheumatic Heart Disease Short Case PresentationDocument1 pageRheumatic Heart Disease Short Case PresentationPrerna SehgalNo ratings yet
- Topnotch ECG Interpretation For MoonlightersDocument25 pagesTopnotch ECG Interpretation For Moonlightersmefav7778520100% (1)
- Brunilda Alushi@Document3 pagesBrunilda Alushi@brunilda.alushiNo ratings yet
- Rundown Iaca 7Document2 pagesRundown Iaca 7Muh Anugerah YusroNo ratings yet
- A. Abnormal Blood Pressure Changes On ExerciseDocument1 pageA. Abnormal Blood Pressure Changes On ExerciseosamahihiNo ratings yet