Professional Documents
Culture Documents
Transient Inhibition of NF-enhances Hematopoietic Stem Cells
Transient Inhibition of NF-enhances Hematopoietic Stem Cells
Uploaded by
eriwinOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Transient Inhibition of NF-enhances Hematopoietic Stem Cells
Transient Inhibition of NF-enhances Hematopoietic Stem Cells
Uploaded by
eriwinCopyright:
Available Formats
ARTICLE Hematopoiesis
Transient inhibition of NF-κB signaling
Ferrata Storti
Foundation enhances ex vivo propagation of human
hematopoietic stem cells
Mehrnaz Safaee Talkhoncheh, Agatheeswaran Subramaniam,
Mattias Magnusson, Praveen Kumar, Jonas Larsson and Aurélie Baudet
Division of Molecular Medicine and Gene Therapy, Lund Stem Cell Center, Lund
University, Sweden
Haematologica 2018
Volume 103(9):1444-1450
ABSTRACT
D
espite extensive studies, defining culture conditions in which
hematopoietic stem cells can be expanded ex vivo has been chal-
lenging. Here we show that chemical inhibition of the NF-κB sig-
naling pathway leads to a significant improvement of hematopoietic
stem cell function from ex vivo cultured human umbilical cord blood
derived CD34+ cells. We found a distinct peak of activation of the NF-κB
pathway shortly after cells were put in culture, and consequently inhibi-
tion of the pathway was both necessary and sufficient during the first 24
hours of culture where it reduced the levels of several pro-inflammatory
cytokines. Taken together, NF-κB pathway inhibition facilitates propaga-
tion of hematopoietic stem cells in culture and may complement other
strategies for hematopoietic stem cell expansion by relieving stress sig-
nals that are induced as an immediate response to culture initiation.
Introduction
Correspondence: Umbilical cord blood (CB) has emerged as a promising source of hematopoietic
jonas.larsson@med.lu.se stem and progenitor cells (HSPCs) for transplantation. Unfortunately, the use of CB
grafts is mainly restricted to pediatric transplantation as the number of HSPCs per
unit is usually too low to allow the infusion of the minimal cell dose required for
successful transplantation in adults.1-3 Potentially, the ex vivo expansion of CB-
Received: January 12, 2018.
derived HSPCs prior to transplantation could extend the use of CB transplantation
Accepted: May 17, 2018. to adult patients.4 Successful HSPC expansion would further facilitate the develop-
Pre-published: June 7, 2018. ment of more advanced cell therapies for hematologic diseases, including gene ther-
apy applications.5
Hematopoietic stem cell self-renewal is regulated by a combination of positive-
doi:10.3324/haematol.2018.188466 negative feedback signaling.6 An incomplete understanding of this complex regula-
tory mechanism and how it would fit in a culture system has limited successful HSC
Check the online version for the most updated ex vivo expansion. Despite the well-studied role of positive signals such as growth
information on this article, online supplements, factors on HSC self-renewal, several studies highlighted the importance of inhibito-
and information on authorship & disclosures: ry signals in restricting HSC self-renewal and function ex vivo. It has been suggested
www.haematologica.org/content/103/9/xxx that, when under culture, HSCs undergo an immediate and transient “culture shock”
that compromises their maintenance and function. This is due to upregulation of
negative regulators of HSC expansion such as tumor necrosis factor (TNF signaling)
©2018 Ferrata Storti Foundation and members of the aryl hydrocarbon receptor (AhR) signaling pathway.7,8
Material published in Haematologica is covered by copyright. Furthermore, the secretion of inhibitory signaling factors, mainly from more differ-
All rights are reserved to the Ferrata Storti Foundation. Use of entiated cells, constitutes a major restriction to all HSC culture systems.8 To further
published material is allowed under the following terms and
conditions:
explore this notion, our laboratory has performed high-throughput forward RNAi
https://creativecommons.org/licenses/by-nc/4.0/legalcode. screens and identified negative regulators of ex vivo expansion of human HSPCs,
Copies of published material are allowed for personal or inter- including the cohesin family of genes, and p38 (MAPK14).9,10 Through these studies,
nal use. Sharing published material for non-commercial pur- we also identified shRNAs which display a remarkable ability to expand phenotyp-
poses is subject to the following conditions:
ically-defined HSPCs in culture but whose gene target has not been validated. We
https://creativecommons.org/licenses/by-nc/4.0/legalcode,
sect. 3. Reproducing and sharing published material for com- reasoned that, although it would be very difficult to identify the gene targets
mercial purposes is not allowed without permission in writing responsible for the phenotype, the molecular characterization of cells targeted by
from the publisher. such off-target shRNAs could provide general clues about the context under which
HSPCs can be propagated ex vivo. Here, we report that the expression signature of
cells showing enhanced expansion from one specific off-target shRNA (sh758)
1444 haematologica | 2018; 103(9)
NF-κB inhibition promotes human HSCs in culture
involved the downmodulation of genes involved in NF-κB Statistical analysis
signaling pathway. We found that pharmacological inhibi- Statistical significance was calculated using a two-tailed
tion of the NF-κB signaling leads to a significant improve- Student t-test with GraphPad Prism software unless otherwise
ment in HSC function from ex vivo cultured CB-derived stated. Statistical significance in the figures are indicated: *P<0.05,
CD34+ cells, as assessed by transplantation to NSG mice. **P<0.01, ***P<0.001, ****P<0.0001. Error bars indicate Standard
The effect of NF-κB pathway inhibition was most critical Error of the Mean (SEM) unless otherwise stated and n represents
early during the culture where it reduced the levels of sev- the number of independent experiments.
eral pro-inflammatory cytokines induced as an immediate Methods describing microarray analysis, CFC assays, western
response to culture initiation. blot and cell cycle analysis can be found in the Online
Supplementary Appendix.
Methods
Results
shRNA experiments
The RNAi screening strategy has been thoroughly described The NF-κB pathway modulates ex vivo cultured human
previously.9,10 The target sequence for the candidate shRNA sh758 HSPCs
is GATATGCAAGTCTGTGAATTT. CD34+ cells were trans- From RNAi-based screens conducted in our laboratory
duced with a pLKO1-GFP lentiviral vector harboring either sh758 aimed at identifying novel modifiers of HSPC expan-
or control (scrambled) shRNA and subsequently cultured for sev- sion,10,11 we have identified several off-target hits: shRNAs
eral weeks according to previously described protocol.9,10 that display profound effects on HSPC expansion but do
not affect the expression of their predicted target. One
Cord blood CD34+ isolation and culture such shRNA, TRC00000758 (sh758), predicted to specifi-
Umbilical CB samples were collected from full-term deliveries cally knock-down (CLK1), induced an especially strong
at maternity wards of Lund, Malmö and Helsingborg Hospitals. proliferative advantage of CB CD34+ cells, as the trans-
CB unit collection, mononuclear cell isolation, and CD34+ cell duced, GFP+ population eventually dominated the culture
enrichment and culture were carried out as previously described.10 (Figure 1A). Moreover, when cultured for seven days,
IKKβ inhibitors, PF184 and TPCA1 (Tocris Bioscience), kept in CD34+CD38-CD90+CD45RA- cells expressing sh758 main-
DMSO, were added at a final concentration of 400nM. Control tained a substantially higher percentage of immature
wells were supplemented with DMSO at a matching concentra- CD34hiCD90+ cells, which is known to contain the
tion. Cultures were kept at 37°C and 5% CO2 and the medium engraftable HSCs (Figure 1B). Given the dramatic increase
(including inhibitors) was refreshed after four days. of CD34hiCD90+ cells induced by sh758, we reasoned that
the molecular signature of cells expressing sh758 could
Flow cytometry and cell sorting provide valuable clues about the genes and pathways that
For cell surface marker staining, cells were collected, washed modulate HSC expansion ex vivo. We performed global
once with PBS supplemented with 2% FCS (FACS buffer). Cells transcriptional profiling of CD34hiCD90+ cells expressing
were incubated with anti CD34 (#343516581), CD90 either sh758 or a control shRNA (shCTL) after seven days
(#3281145E10) and EPCR (#351906) (BioLegend) antibodies for 30 of culture. The gene expression profiles revealed a down-
minutes (min) at 4°C, and washed once with cold FACS buffer. modulation of cellular stress-related genes and pathways,
For cell sorting, CD34+ cells were quickly thawed and stained for such as MAPK14 and genes involved in NF-κB signaling, in
CD34, CD38 (#345806), CD45RA (#560362) (BD Bioscience) and sh758 transduced cells (Figure 1C). Of note, the expression
CD90 following the same procedure as above. When specified, levels of CLK1, as well as other predicted targets of sh758
cells were stained with the Annexin V Apoptosis Detection Kit, (based on sequence homology), were not repressed by the
according to the manufacturer’s protocol (BD Bioscience). All data shRNA. We have previously reported on the role of
were collected on FACS Canto II or LSRII analyzer (Becton MAPK14 (p38) in HSPC expansion10 and therefore decided
Dickinson), and analyzed with FlowJo software. Cells were sort- to further investigate the role of NF-κB signaling in this
ed on a FACS Aria II or III (Becton Dickinson). context. We first addressed whether the NF-κB pathway is
activated upon ex vivo culture of CB CD34+ cells and found
Human engraftment assay that the key regulator of NF-κB signaling, IkBa,12 was read-
All experiments with mice were reviewed and conducted under ily detected and also showed an increased expression dur-
approved protocol from the Lund/Malmö Local Ethical ing culture (Figure 1D). We further measured the phospho-
Committee. NOD.Cg-PrkdcscidIl2rgtm1Wjl/SzJ mice (NSG; Jackson rylated form of the IκBa protein (p-IκBa), as an indicator
Laboratory) were sublethally irradiated (300 cGy) before trans- of NF-κB activity, at different time points during culture of
plantation. Fresh cells or the cultured equivalent of 30,000 input CB CD34+ cells. We observed that the p-IκBa signal was
CD34+ cells were injected intravenously into 10-12-week old NSG detected throughout the culture and with particularly high
mice. Human cell contribution in peripheral blood (PB) and bone levels during the first 24 hours (Figure 1D). Collectively,
marrow (BM) of NSG was assessed 16 weeks post transplanta- this suggests that the NF-κB pathway is activated in cul-
tion. tured HSPCs and may negatively influence their expan-
sion.
Cytokine secretion and Bioplex assay
Supernatants were collected from duplicate samples after six NF-κB pathway inhibition mediated by targeting IKKβ
hours treatment of CB CD34+ cells with TPCA1 or STF. The increases expansion of CD34+CD90+ cells ex vivo
secreted cytokines in the supernatants were measured by using To further explore the role of NF-κB signaling in cul-
human 27-plex panel (M500KCAF0Y, Bio-Rad) in the Bio-Rad tured HSPCs, we next blocked the pathway pharmacolog-
Luminex instrument. Samples were prepared and analyzed as per ically. As the down-regulated genes detected in the gene
the manufacturer’s protocol. expression profiling (Figure 1C) are acting through canon-
haematologica | 2018; 103(9) 1445
M.S. Talkhoncheh et al.
A B
Figure 1. The sh758-depen-
dent ex vivo expansion
effect is associated with a
downmodulation of the NF-
κB pathway. (A) Growth of
C D
GFP+ cells was assessed by
FACS and normalized to day
2-transduction efficiency. (B)
The percentage of CD34+90+
cells in the GFP+ fraction was
quantified by FACS seven
days after transduction of
CD34+CD38-CD90+CD45RA-
cells (n=2). (C) Gene expres-
sion data mining showed
modulation of members of
NF-κB signaling in sh758
expressing CD34+CD90+
cells. (D) The expression of
total and phosphorylated
ΙκΒa was quantified by west-
ern blot in CD34+ cells at
indicated culture time
points. Actin expression is
shown as loading control.
ical NF-κB signaling, we decided to target IKKβ which is a erated a higher proportion of primitive colonies with a
central molecule in integrating upstream signals in the mixed phenotype (Figure 3A), indicating improved func-
canonical pathway.13 Thus, we treated CD34+ cells with tional integrity of the cultured progenitor cells. Next, to
two specific inhibitors of the IKKβ subunit: PF184 and test the in vivo regenerative capacity of HSCs cultured with
TPCA1.14,15 IκBa is the canonical target of IKKβ and both IKKβ inhibitors, we performed transplantation experi-
inhibitors induced a strong reduction of the phosphorylat- ments. Fresh CB CD34+ (30,000) cells or 7-day cultured
ed-to-total IκBa ratio after four hours treatment (Figure equivalents of 30,000 CB CD34+ were transplanted into
2A). After seven days of culture, we observed a marked sub-lethally irradiated NOD.Cg-PrkdcscidIl2rgtm1Wjl/SzJ
increase in both the frequency and number of (NSG) mice (Figure 3B). Cells treated with PF184 and
CD34+CD90+ cells (Figure 2B). TPCA1 yielded 53% and 64% human engraftment,
However, the total cell number remained unaffected respectively, while control cells generated lower (38%)
(Figure 2C), suggesting that the increase in CD34+CD90+ human engraftment in bone marrow 16 weeks post trans-
cells number is not due to a generally higher proliferation plantation (Figure 3C). The engrafted cells contributed to
rate of cells treated with NF-κB inhibitors. Since NF-κB both myeloid and lymphoid lineages (Figure 3D and E).
has well described effects on apoptosis16 and prolifera- Finally, the frequency of the HSC enriched CD34+CD38-
tion,17 we assayed cell cycle and apoptosis parameters in population among the engrafted human cells was similar
CD34+ cells treated with PF184 and TPCA1 in an attempt to that of control cells (Online Supplementary Figure S1),
to understand the basis for the increased numbers of demonstrating an overall higher long-term engraftment of
CD34+CD90+ cells. However, we could not detect any sig- also the most immature cells from cultures with PF184 and
nificant difference in cell cycle status (Figure 2D) or apop- TPCA1. Although IKKβ inhibitor treated cells showed
totic cell levels (Figure 2E) of CD34+90+ cells. slightly lower long-term engraftment compared to non-
cultured cells, our data demonstrate a strong benefit of
NF-κB pathway inhibition enhances the ex vivo NF-κB inhibition in preserving functional HSPCs during ex
propagation of transplantable HSCs vivo expansion cultures.
To assess in more detail the functional consequences of
growing HSPCs in the presence of NF-κB inhibition, we NF-κB inhibition is most beneficial during an early
cultured CD34+ cells for seven days with or without IKKβ time window where it down-regulates several
inhibitors, and then assayed the cells for colony forming pro-inflammatory cytokines
ability in methylcellulose medium. Cells cultured in the We had previously observed a peak in p-IκBa levels dur-
presence of inhibitors produced a significantly higher ing the first 24 hours of culture (Figure 1D), and therefore
number of colonies compared to the control, and also gen- next assessed if there is a critical time window for addi-
1446 haematologica | 2018; 103(9)
NF-κB inhibition promotes human HSCs in culture
A B
C D E
Figure 2. Targeting of the NF-κB regulator IKKβ increases the number of human hematopoietic stem and progenitor cells (HSPCs) in vitro without affecting cell
proliferation and survival. (A) The protein level of total and phosphorylated IκBa were quantified in CD34+ cells after 4-hour treatment with STF/PF/TP in culture.
Actin expression is shown as loading control (n=2). (B) FACS plots and graph show cell surface expression of CD34 and CD90 and number of CD34+CD90+ cells
respectively at day 7 (n=4). (C) Graph displays total live (7AAD-) cell number at day 7 (n=4). (D) Cell cycle distribution, and (E) apoptosis (7AAD-/ AnnexinV+) of
CD34+CD90+ cells were assessed by FACS at days 4 and 7, respectively (n=3). p-IκBa: phosphorylated IκBa; t-IκBa: total IκBa; PF: PF184; TP: TPCA1.
tion of IKKβ inhibitors. We found that delaying IKKβ inhi- role in other processes such as cell growth, survival and
bition for 24 hours abolished the beneficial effects and development.13 To further identify which NF-κB associat-
resulted in lower numbers of CD34+CD90+ cells after five ed functions were targeted in our cultured HSPCs, we sub-
days compared to cultures where the inhibitor was added jected bulk CD34+ and sorted CD34+CD90+ cells to global
directly. Similarly, treating cells for only the first 24 hours gene expression profiling using microarrays (Figure 4D
with IKKβ inhibitor resulted in similarly elevated numbers and E, Online Supplementary Table S1 and Online
of CD34+CD90+ cells compared to 5-day treatment (Figure Supplementary Figure S3). We used 6-hour culture time for
4A). Collectively, these findings suggest that NF-κB activa- the transcriptome analysis as this time point showed a
tion is most detrimental during the first 24 hours of culture clear increase in NF-κB activity (Figure 1D). Although rel-
and define a time window when NF-κB inhibition is both atively few transcriptional changes were detected within
necessary and sufficient to execute protective effects on the more heterogeneous bulk of CD34+ cells (Online
HSPCs. Supplementary Figure S3), 51 annotated genes were modu-
In order to further characterize the potential of NF-κB lated in the CD34+CD90+ population upon exposure to the
inhibition in improving expansion protocols, we com- IKKβ inhibitor (Figure 4D and E, and Online Supplementary
pared TPCA1 to two other known expansion molecules Table S1). Out of these, all coding genes (23 genes) were
for human HSCs: SR1 and UM171.18,19 We evaluated the down-regulated and mainly related to inflammatory
output of CD34+90+ cells as well as CD34+CD90+EPCR+ processes (15 genes), for example, IL1a, TNF-a, GM-CSF
cells, as EPCR expression recently has been associated (CSF2), MCP-1 (CCL2), TCA3 (CCL1), and MIP-1β
with the regenerative activity of ex vivo cultured HSPCs in (CCL4) (Online Supplementary Table S1). Using Bioplex
the context of UM171 mediated expansion.20 All three bead arrays, we confirmed the reduction of several pro-
compounds showed a clear increase in both CD34+CD90+ inflammatory factors, including TNF-a, IL-6, IP-10
and CD34+CD90+EPCR+ cell numbers compared to control (CXCL10) and IL-8 in supernatants collected from cultures
cultures (Figure 4B and C, and Online Supplementary Figure of CB CD34+ cell after a 6-hour exposure to the IKKβ
S2). However, TPCA1 treatment resulted in larger num- inhibitor (Figure 4F and G). Taken together, these findings
bers of these cell populations compared to SR1, while indicate that the beneficial effect of IKKβ inhibitors on cul-
UM171 showed a significant increase compared to both tured human HSPCs is associated with the downregula-
TPCA1 and SR1 (Figure 4B and C). Interestingly, the com- tion of NF-κB-dependent pro-inflammatory molecules.
bination of the IKKβ inhibitor with either SR1 and UM171
led to a marked increase in CD34+90+ and
CD34+CD90+EPCR+ cell numbers, compared to each com- Discussion
pound alone (Figure 4B and C), indicating that targeting
NF-κB signaling may enhance HSPC expansion protocols In this study, we demonstrate that the NF-κB signaling
driven by other compounds. has a negative impact on ex vivo cultured human CB
NF-κB proteins are considered key players in inflamma- HSPCs, and that pharmacological inhibition of the path-
tion and immunity. However, they also play an important way improves their propagation and regenerative poten-
haematologica | 2018; 103(9) 1447
M.S. Talkhoncheh et al.
A B Figure 3. Targeting of the NF-
κB regulator IKKβ improves
the in vitro and in vivo func-
tion of cultured cord blood
(CB)-derived hematopoietic
stem and progenitor cells
(HSPCs). (A) Colonies per 300
CD34+ input cells were
scored after 14 days (n=3).
(B) Schematic representation
of in vivo transplantation
experiment. (C) Human
engraftment was assessed by
quantifying the percentage of
human CD45+ cells in the
bone marrow (BM) of NSG
recipients four months post
transplantation (data from 2
independent experiments).
C D
(D) Lineage distribution was
quantified by FACS analysis of
human B cells (CD19), T cells
(CD3), and myeloid
(CD33/CD15) in CD45+ cells
of the BM of recipients. (E)
Representative FACS plots for
gating strategy of lineage
reconstitution. PF: PF184; TP:
TPCA1.
tial after culture. Our findings further showed that this is molecular signature associated with sh758, an shRNA that
associated with inhibition of pro-inflammatory signals in dramatically expands phenotypically defined HSPCs.
CD34+CD90+ cells during the early phases of the culture. However, even if chemical inhibition of IKKβ, the inte-
NF-κB signaling can be activated in both immune and grating kinase of NF-κB signaling, did lead to a robust and
non-immune tissues by various extracellular signals, such consistent increase in CD34+CD90+ cells, it could not
as reactive oxygen species,21 pro-inflammatory cytokines reproduce the full extent of the sh758 phenotype.
such as interleukin-1,22 and members of the TNF super- Specifically, the effect of IKKβ inhibition was limited to a
family.23 Cellular responses largely depend on the cell short time window during the first 24 hours of culture.
type, include positive or negative modulation of prolifera- This suggests that the profound and persistent expansion
tion and apoptosis,16 differentiation,24 development,13,25 and of CD34+CD90+ cells induced by sh758 is only partly
are mediated by secretion of a large variety of signals21 mediated by reduced activity of the NF-κB pathway, and
and direct expression control of cell cycle/apoptosis medi- that other genes and pathways must be involved as well.
ators.16 In hematopoiesis, knockout mouse models of dif- One strong candidate is MAPK14 (p38), which was also
ferent NF-κB subunits have revealed defects in HSPCs down-regulated in sh758-transduced cells. We have previ-
function, as well as impaired immune response, lym- ously shown that p38 inhibition enhances the stem cell
phopoiesis, granulocytosis, and splenomegaly.26,27 In output from cultured HSPCs.
human settings, overexpression of p65 or a constitutively Despite the well described function of NF-κB in regulat-
active form of IKKβ did not influence growth and differ- ing proliferation and apoptosis,29 we did not observe any
entiation of CB-derived CD34+ cells.28 However, the actu- significant changes in cell cycle, or apoptotic status of
al role of NF-κB signaling and the consequences of inhibit- CD34+CD90+ cells upon NF-κB pathway inhibition.
ing the pathway in normal HSPCs had not previously Additionally, NF-κB signaling has been linked to ROS pro-
been addressed. duction,21 which must be tightly regulated to maintain
We initially identified the NF-κB pathway as part of a HSPC function.30 However, intracellular ROS levels were
1448 haematologica | 2018; 103(9)
NF-κB inhibition promotes human HSCs in culture
A B C
D E
F G
Figure 4. The benefit of NF-κB pathway inhibition is limited to a short time window, and results in downregulation of inflammatory signaling. (A) Number of
CD34+CD90+ cells was assessed after five days by FACS, when TP/STF was added directly or 24 hours after culture start or removed after 24 hours (n=3). (B) Graph
shows number of CD34+CD90+ cells after treatment with STF, TP, SR1, UM171 and combination of TP with either SR1 or UM171 at day 6 (representative data from
2 experiments). (C) Graph shows number of CD34+CD90+EPCR+ cells after treatment with STF, TP, SR1, UM171 and combination of TP with either SR1 or UM171 at
day 6 (representative data from 2 experiments). (D and E) CD34+ cells were treated with or without TP for six hours and subjected to transcriptome analysis by
microarrays after sorting for CD34+90+ population. Volcano plot and GO classification of 2-fold modulated (down-regulated) genes are shown for each condition. See
also Online Supplementary Figure S3 and Online Supplementary Table S1. (F) The log ratio (TP/STF) of factors present in supernatant after six hours of culture of
CB-derived CD34+ cells is shown (n=3). (G) Each graph displays individual data point for significantly modulated cytokines (IL6, TNFa, IL8, and IP10), extracted from
the experiments presented in (F). The stars in (F) indicate that those factors were not detectable. PF: PF184; TP: TPCA1.
not significantly altered during the early phase of the cul- to negatively influence self-renewal and lineage commit-
ture (data not shown), when the effects of NF-κB pathway ment of HSCs.32,33 Therefore, considering the lack of effect
inhibition were seen to enhance HSPC activity. This sug- on cell proliferation, the increased HSC output after NF-κB
gests that the preserved stem cell output of cultured pathway inhibition may rather be associated with pre-
HSPCs upon NF-κB pathway inhibition is not related to served stem cell integrity by restricting differentiation. It is
ROS modulation. likely that the most immature HSPC are particularly sen-
Based on the IκBa phosphorylation pattern, we showed sitive to the early culture shock as they showed the most
that there is a critical 6-24-hour time frame necessary and profound transcriptional changes upon NF-κB pathway
sufficient for NF-κB pathway inhibition to benefit the inhibition.
propagation of the CD34+CD90+ population. In agreement It could be argued that pro-inflammatory stress could be
with this, previous studies also reported on an immediate relieved by simply exchanging the media similar to the
variation in gene expression profile of inhibitory HSPC fed-batch system.8 However, during the critical first 24
regulators as the cultured cells experience an initial culture hours, the cell density is very low and a media exchange
shock.7,8 In fact, we showed downregulation of several system is not likely to have an impact during this short
pro-inflammatory genes such as MCP-1 (CCL2), TCA3 time frame. It is possible that restricting inhibitory signals
(CCL1), IL1a, TNF-a and MIP-1β (CCL4) upon NF-κB in expansion cultures have a bi-phasic pattern; one pulse
inhibition, which are known to inhibit HSPC function.31 that is induced immediately upon culture initiation and
Although these pro-inflammatory cytokines are essential one that accumulates over time and that is dependent on
for a proper defense mechanism,24 they have been shown cell density and media changes. The latter can be relieved
haematologica | 2018; 103(9) 1449
M.S. Talkhoncheh et al.
by fed-batch systems, but the acute effect may rather be ment at the Division of Molecular Medicine and Gene Therapy,
intrinsically triggered and require pharmacological target- The Lund Stem Cell Center FACS and Vector cores, as well as
ing, in this case NF-κB pathway inhibition, to be reduced. the Animal facility at the Biomedical Center. This work was
Our finding that targeting NF-κB signaling further funded by grants from the Swedish Research Council, the
enhances HSPC expansion driven by other compounds Swedish Cancer Foundation, the Swedish Pediatric Cancer
suggests that this should be further exploited in strategies Foundation and the European Research Council (ERC) under the
aimed at HSC expansion for clinical benefit. European Union’s Horizon 2020 research and innovation pro-
gram (grant agreement n. 648894) to JL. The work was further
Acknowledgments supported by the HematoLinné and StemTherapy programs at
The authors are thankful to the technical staff and manage- Lund University.
RNAi screens in primary human hematopoi- phocytes. J Biol Chem. 1992;267(22):15836-
References etic stem/progenitor cells. Blood. 15841.
1. Brunstein CG, Gutman JA, Weisdorf DJ, et 2009;113(16): 3690-3695. 23. Baud V, Karin M. Signal transduction by
al. Allogeneic hematopoietic cell transplan- 12. Hayden MS, Ghosh S. Shared principles in tumor necrosis factor and its relatives.
tation for hematologic malignancy: relative NF-kappaB signaling. Cell. 2008;132(3):344- Trends Cell Biol. 2001;11(9):372-377.
risks and benefits of double umbilical cord 362. 24. Espin-Palazon R, Stachura DL, Campbell
blood. Blood. 2010;116(22):4693-4699. 13. Oeckinghaus A, Hayden MS, Ghosh S. CA, et al. Proinflammatory signaling regu-
2. Wagner JE, Gluckman E. Umbilical cord Crosstalk in NF-kappaB signaling pathways. lates hematopoietic stem cell emergence.
blood transplantation: the first 20 years. Nat Immunol. 2011;12(8):695-708. Cell. 2014;159(5):1070-1085.
Semin Hematol. 2010;47(1):3-12. 14. Mora E, Guglielmotti A, Biondi G, Sassone- 25. Oeckinghaus A, Ghosh S. The NF-kappaB
3. Ballen KK, Gluckman E, Broxmeyer HE. Corsi P. Bindarit: an anti-inflammatory small family of transcription factors and its regula-
Umbilical cord blood transplantation: the molecule that modulates the NFkappaB tion. Cold Spring Harb Perspect Biol.
first 25 years and beyond. Blood. pathway. Cell Cycle. 2012;11(1):159-169. 2009;1(4):a000034.
2013;122(4):491-498. 15. Podolin PL, Callahan JF, Bolognese BJ, et al. 26. Stein SJ, Baldwin AS. Deletion of the NF-
4. Broxmeyer HE. Enhancing the efficacy of Attenuation of murine collagen-induced kappaB subunit p65/RelA in the hematopoi-
engraftment of cord blood for hematopoiet- arthritis by a novel, potent, selective small etic compartment leads to defects in
ic cell transplantation. Transfus Apher Sci. molecule inhibitor of IkappaB Kinase 2, hematopoietic stem cell function. Blood.
2016;54(3):364-372. TPCA-1 (2-[(aminocarbonyl)amino]-5-(4- 2013;121(25):5015-5024.
5. Farahbakhshian E, Verstegen MM, Visser TP, fluorophenyl)-3-thiophenecarboxamide), 27. Nakata S, Matsumura I, Tanaka H, et al. NF-
et al. Angiopoietin-like protein 3 promotes occurs via reduction of proinflammatory kappaB family proteins participate in multi-
preservation of stemness during ex vivo cytokines and antigen-induced T cell ple steps of hematopoiesis through elimina-
expansion of murine hematopoietic stem Proliferation. J Pharmacol Exp Ther. tion of reactive oxygen species. J Biol Chem.
cells. PLoS One. 2014;9(8):e105642. 2005;312(1):373-381. 2004;279(53):55578-55586.
6. Kirouac DC, Ito C, Csaszar E, et al. 16. Barkett M, Gilmore TD. Control of apopto- 28. Schepers H, Eggen BJ, Schuringa JJ, Vellenga
Dynamic interaction networks in a hierar- sis by Rel/NF-kappaB transcription factors. E. Constitutive activation of NF-kappa B is
chically organized tissue. Mol Syst Biol. Oncogene. 1999;18(49):6910-6924. not sufficient to disturb normal steady-state
2010;6:417. 17. Naugler WE, Karin M. NF-kappaB and can- hematopoiesis. Haematologica. 2006;91(12):
7. Magnusson M, Sierra MI, Sasidharan R, et cer-identifying targets and mechanisms. 1710-1711.
al. Expansion on stromal cells preserves the Curr Opin Genet Dev. 2008;18(1):19-26. 29. Radhakrishnan SK, Kamalakaran S. Pro-
undifferentiated state of human hematopoi- 18. Boitano AE, Wang J, Romeo R, et al. Aryl apoptotic role of NF-kappaB: implications
etic stem cells despite compromised recon- hydrocarbon receptor antagonists promote for cancer therapy. Biochim Biophys Acta.
stitution ability. PLoS One. 2013;8(1): the expansion of human hematopoietic 2006;1766(1):53-62.
e53912. stem cells. Science. 2010;329(5997):1345- 30. Ito K, Hirao A, Arai F, et al. Regulation of
8. Csaszar E, Kirouac DC, Yu M, et al. Rapid 1348. oxidative stress by ATM is required for self-
expansion of human hematopoietic stem 19. Fares I, Chagraoui J, Gareau Y, et al. Cord renewal of haematopoietic stem cells.
cells by automated control of inhibitory blood expansion. Pyrimidoindole deriva- Nature. 2004;431(7011):997-1002.
feedback signaling. Cell Stem Cell. 2012;10 tives are agonists of human hematopoietic 31. Baldridge MT, King KY, Goodell MA.
(2):218-229. stem cell self-renewal. Science. Inflammatory signals regulate hematopoiet-
9. Galeev R, Baudet A, Kumar P, et al. 2014;345(6203):1509-1512. ic stem cells. Trends Immunol. 2011;32(2):
Genome-wide RNAi Screen Identifies 20. Fares I, Chagraoui J, Lehnertz B, et al. EPCR 57-65.
Cohesin Genes as Modifiers of Renewal and expression marks UM171-expanded 32. Dybedal I, Bryder D, Fossum A, Rusten LS,
Differentiation in Human HSCs. Cell Rep. CD34(+) cord blood stem cells. Blood. Jacobsen SE. Tumor necrosis factor (TNF)-
2016;14(12):2988-3000. 2017;129(25):3344-3351. mediated activation of the p55 TNF receptor
10. Baudet A, Karlsson C, Safaee Talkhoncheh 21. Morgan MJ, Liu ZG. Crosstalk of reactive negatively regulates maintenance of cycling
M, et al. RNAi screen identifies MAPK14 as oxygen species and NF-kappaB signaling. reconstituting human hematopoietic stem
a druggable suppressor of human Cell Res. 2011;21(1):103-115. cells. Blood. 2001;98(6):1782-1791.
hematopoietic stem cell expansion. Blood. 22. Stylianou E, O'Neill LA, Rawlinson L, et al. 33. Pietras EM. Inflammation: a key regulator of
2012;119(26):6255-6258. Interleukin 1 induces NF-kappa B through hematopoietic stem cell fate in health and
11. Ali N, Karlsson C, Aspling M, et al. Forward its type I but not its type II receptor in lym- disease. Blood. 2017;130(15):1693-1698.
1450 haematologica | 2018; 103(9)
You might also like
- Robert Plutchik (Auth.), Manfred Clynes, Jaak Panksepp (Eds.) - Emotions and Psychopathology-Springer US (1988)Document336 pagesRobert Plutchik (Auth.), Manfred Clynes, Jaak Panksepp (Eds.) - Emotions and Psychopathology-Springer US (1988)Lalón Gitud De Onda100% (1)
- Dulce BattleDocument98 pagesDulce BattleMarc St-Germain100% (3)
- 6 Enzymes and Cellular Regulation-SDocument5 pages6 Enzymes and Cellular Regulation-Sapi-502781581No ratings yet
- Animal Habitat Diorama Project InstructionsDocument7 pagesAnimal Habitat Diorama Project Instructionsapi-293342816No ratings yet
- Cells 12 00321Document30 pagesCells 12 00321uttamNo ratings yet
- GeneDocument10 pagesGeneLýDiệuNo ratings yet
- JHep 2010Document10 pagesJHep 2010wangyu81No ratings yet
- Hematopoietic Stem and ProgenitorCellsDocument10 pagesHematopoietic Stem and ProgenitorCellsRuxandra MesarosNo ratings yet
- POT0024 - 1117B - StemCell Insider Issue 8 (Expansion)Document2 pagesPOT0024 - 1117B - StemCell Insider Issue 8 (Expansion)Francisco MoralesNo ratings yet
- 42 Uniform Scale Independent Gene Transfer To Striated Muscle After Transvenular Extravasation of VectorDocument2 pages42 Uniform Scale Independent Gene Transfer To Striated Muscle After Transvenular Extravasation of VectorMuinimula aluminiuM (MuminiminimuM)No ratings yet
- Neural Differentiation of Human Pluripotent Stem CellsDocument12 pagesNeural Differentiation of Human Pluripotent Stem Cellsilmiah neurologiNo ratings yet
- Silibinin Inhibits Proliferation and Migration of Human Hepatic Stellate LX-2 CellsDocument3 pagesSilibinin Inhibits Proliferation and Migration of Human Hepatic Stellate LX-2 CellsSILVIA BAQUEIRONo ratings yet
- (Review) (Biological Chemistry) Bernd Giebel Et Michael Punzel 2008Document12 pages(Review) (Biological Chemistry) Bernd Giebel Et Michael Punzel 2008Priscilla FreschuNo ratings yet
- Wharton's JellyDocument13 pagesWharton's JellyZ MNo ratings yet
- Ijsc 13 001 2Document12 pagesIjsc 13 001 2dimiz77No ratings yet
- SCT3 6 0864Document13 pagesSCT3 6 0864Z MNo ratings yet
- Zeng 2013Document7 pagesZeng 2013angela_karenina_1No ratings yet
- Cancer 1Document8 pagesCancer 1JoseRodrigoSuarezCamposNo ratings yet
- LCH TargetDocument5 pagesLCH TargetSeham GoharNo ratings yet
- Mehta 2011Document10 pagesMehta 2011Giulia AndreeaNo ratings yet
- NIH Public AccessDocument18 pagesNIH Public AccessSofia BottiNo ratings yet
- The Physical Microenvironment of Hematopoietic Stem Cells and Its Emerging Roles in Engineering ApplicationsDocument13 pagesThe Physical Microenvironment of Hematopoietic Stem Cells and Its Emerging Roles in Engineering ApplicationsDemie PearlNo ratings yet
- Gene TherapyDocument6 pagesGene TherapyHafizah RamliNo ratings yet
- Hematopoietic Stem Cells: Gordon KellerDocument7 pagesHematopoietic Stem Cells: Gordon KellerPisi MicaNo ratings yet
- BBA - Molecular Cell ResearchDocument11 pagesBBA - Molecular Cell ResearchPUSKESMAS KECAMATAN KEPULAUAN SERIBU UTARANo ratings yet
- BPM EN Produccion de FibroblastosDocument14 pagesBPM EN Produccion de FibroblastosAndrea Garcia CaycedoNo ratings yet
- Artigo Biotecnologia Tecido AdiposoDocument15 pagesArtigo Biotecnologia Tecido AdiposoLuiz Gabriel Ferreira da SilvaNo ratings yet
- Changes in The Cell Surface Markers During NormalDocument10 pagesChanges in The Cell Surface Markers During NormalMaw BerryNo ratings yet
- Dimensions of Neutrophil Life and Fate 2020Document7 pagesDimensions of Neutrophil Life and Fate 2020brunareis1999No ratings yet
- Advances in Pluripotent Stem Cells: History, Mechanisms, Technologies, and ApplicationsDocument30 pagesAdvances in Pluripotent Stem Cells: History, Mechanisms, Technologies, and ApplicationsnembutalNo ratings yet
- Cells 12 02765 v2Document22 pagesCells 12 02765 v2Naga MuthuNo ratings yet
- Cell Regeneration 2012Document10 pagesCell Regeneration 2012ИгорьNo ratings yet
- Science Ade6967Document9 pagesScience Ade69670728lrhNo ratings yet
- Base Editing of Hematopoietic Stem Cells Rescues Sickle Cell Disease in MiceDocument42 pagesBase Editing of Hematopoietic Stem Cells Rescues Sickle Cell Disease in MiceOsvaldo VillarNo ratings yet
- Chapter 3Document39 pagesChapter 3hedieh abedNo ratings yet
- Jurnal Metastasis Paru 2Document25 pagesJurnal Metastasis Paru 2widiastrikNo ratings yet
- IJKD - News Letter1 20 26Document8 pagesIJKD - News Letter1 20 26Kapil SejpalNo ratings yet
- Pnas 1911951117Document11 pagesPnas 1911951117Lucero RamirezNo ratings yet
- Increased Mab Production in Amplified CHO Cell Lines Is Associated With Increased Interaction of CREB1 With Transgene PromoterDocument9 pagesIncreased Mab Production in Amplified CHO Cell Lines Is Associated With Increased Interaction of CREB1 With Transgene PromoterSusan SharfsteinNo ratings yet
- S74 Poster Abstracts: Table 1Document1 pageS74 Poster Abstracts: Table 1HanaNo ratings yet
- 2023 Article 529Document22 pages2023 Article 529amirNo ratings yet
- Cell Reprogramming: Expectations and Challenges For Chemistry in Stem Cell Biology and Regenerative MedicineDocument8 pagesCell Reprogramming: Expectations and Challenges For Chemistry in Stem Cell Biology and Regenerative MedicinenembutalNo ratings yet
- Fimmu 13 814030Document15 pagesFimmu 13 814030yunitaknNo ratings yet
- Gene TherapyDocument10 pagesGene TherapyIsabella MejiaNo ratings yet
- Hepatitis B Research PapersDocument4 pagesHepatitis B Research Papersafnhgewvmftbsm100% (1)
- ACTN4-자궁경부암 관계 입증 논문-3Document12 pagesACTN4-자궁경부암 관계 입증 논문-3김승훈(이과대학 화학)No ratings yet
- NatureDocument32 pagesNaturezhouqunli514No ratings yet
- CA A Cancer J Clinicians - March April 1988 - Virji - Tumor Markers in Cancer Diagnosis and PrognosisDocument23 pagesCA A Cancer J Clinicians - March April 1988 - Virji - Tumor Markers in Cancer Diagnosis and PrognosisIssahaku AbdallahNo ratings yet
- The Concept of Radiation-Enhanced Stem Cell Differentiation: Research ArticleDocument8 pagesThe Concept of Radiation-Enhanced Stem Cell Differentiation: Research ArticledwinugrohojuandaNo ratings yet
- A Recombinant Human Anti-Platelet SCFV Antibody Produced in Pichia Pastoris For Atheroma TargetingDocument18 pagesA Recombinant Human Anti-Platelet SCFV Antibody Produced in Pichia Pastoris For Atheroma TargetingSyahputraWibowoNo ratings yet
- Yu Et Al-2018-Journal of Cellular and Molecular MedicineDocument9 pagesYu Et Al-2018-Journal of Cellular and Molecular MedicineHanzZzAravlaNo ratings yet
- Nihms 1807736Document15 pagesNihms 1807736sirfengchenNo ratings yet
- Identification of Cancer-Related Mutations in Human Pluripotent Stem Cells Using RNA-seq AnalysisDocument16 pagesIdentification of Cancer-Related Mutations in Human Pluripotent Stem Cells Using RNA-seq AnalysisgangligonNo ratings yet
- 2020 The Application of Cell Surface Markers To Demarcate Distinct Human Pluripotent States (Experimental Cell Research)Document9 pages2020 The Application of Cell Surface Markers To Demarcate Distinct Human Pluripotent States (Experimental Cell Research)Thakoon TtsNo ratings yet
- Embedding The Future of Regenerative Medicine Into The Open Epigenomic Landscape of Pluripotent Human Embryonic Stem CellsDocument29 pagesEmbedding The Future of Regenerative Medicine Into The Open Epigenomic Landscape of Pluripotent Human Embryonic Stem CellsMili GiménezNo ratings yet
- Clonally Resolved Single Cell Multi Omics Identifies Routes of 2023 Cell STDocument25 pagesClonally Resolved Single Cell Multi Omics Identifies Routes of 2023 Cell STdimiz77No ratings yet
- Recombinant Human G-CSF Production As A Protein Based Drug Candidate For Hematology and OncologyDocument9 pagesRecombinant Human G-CSF Production As A Protein Based Drug Candidate For Hematology and OncologyZminasariNo ratings yet
- HomingDocument14 pagesHomingMaría P SNo ratings yet
- Poster Presentations Experimental Hematology 44 (2016) S56-S110Document1 pagePoster Presentations Experimental Hematology 44 (2016) S56-S110aymenNo ratings yet
- Stem Cell: The Spleen Contributes Stem Cells To Peripheral Blood Stem Cell TransplantsDocument4 pagesStem Cell: The Spleen Contributes Stem Cells To Peripheral Blood Stem Cell TransplantsAnuj MittalNo ratings yet
- Multi Lineage Progenitor Cells Ped 1660 06Document2 pagesMulti Lineage Progenitor Cells Ped 1660 06608943No ratings yet
- IUBMB Life - 2020 - Pozzi - Cancer Stem Cell Enrichment Is Associated With Enhancement of Nicotinamide N MethyltransferaseDocument11 pagesIUBMB Life - 2020 - Pozzi - Cancer Stem Cell Enrichment Is Associated With Enhancement of Nicotinamide N MethyltransferasePatricia SolarNo ratings yet
- Eshtiaghi 2019Document6 pagesEshtiaghi 2019dimiz77No ratings yet
- Diagnosis of Blood and Bone Marrow DisordersFrom EverandDiagnosis of Blood and Bone Marrow DisordersSa A. WangNo ratings yet
- Thesis Statement For HoneybeesDocument5 pagesThesis Statement For Honeybeesgjgcnp6z100% (2)
- Navarro College Medical Laboratory Technology Degree PlanDocument1 pageNavarro College Medical Laboratory Technology Degree PlanNavarro CollegeNo ratings yet
- Glycolysis Krebscycle Practice Questions SCDocument2 pagesGlycolysis Krebscycle Practice Questions SCapi-323720899No ratings yet
- Probni Test 1. Godina - Ina KlipaDocument4 pagesProbni Test 1. Godina - Ina KlipaMickoNo ratings yet
- Myo 5 ADocument26 pagesMyo 5 Aapi-221640706No ratings yet
- Chromatography REVISED2016Document10 pagesChromatography REVISED2016Abby LumanglasNo ratings yet
- Checklist - Bathing An Adult ClientDocument1 pageChecklist - Bathing An Adult ClientDonaJeanNo ratings yet
- Summary of Pub Med Articles Protandim PDFDocument2 pagesSummary of Pub Med Articles Protandim PDFLeslee MasonNo ratings yet
- Experiment 3 An O-Toluidine Method For Blood Glucose DeterminationDocument9 pagesExperiment 3 An O-Toluidine Method For Blood Glucose DeterminationAlmas MalikNo ratings yet
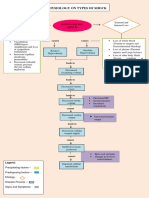
- Pathophysiology On Types of ShockDocument4 pagesPathophysiology On Types of ShockJessa Mae Alforque AsentistaNo ratings yet
- Anatomy and Physiology CNS Brain and Spinal Cord Chart Completed AP BiologyDocument12 pagesAnatomy and Physiology CNS Brain and Spinal Cord Chart Completed AP BiologyTiffany GallinaNo ratings yet
- Introduction To MorphologyDocument17 pagesIntroduction To MorphologydibabasarNo ratings yet
- Ankylosing SpondylitisDocument19 pagesAnkylosing SpondylitisZulhida YuniNo ratings yet
- Attention and Concentration in SportsDocument30 pagesAttention and Concentration in SportsArundhathy GopakumarNo ratings yet
- Radtke-Schuller2016 Article BrainAtlasOfTheMongolianGerbilDocument272 pagesRadtke-Schuller2016 Article BrainAtlasOfTheMongolianGerbilCharlotte NordenNo ratings yet
- P (3) Centrifuge Uses and MaitenanceDocument17 pagesP (3) Centrifuge Uses and MaitenanceSaadNo ratings yet
- Diffenrece Between Filipino TraditionalDocument19 pagesDiffenrece Between Filipino TraditionalJansen ValdezNo ratings yet
- New Case Study Booklet-1Document13 pagesNew Case Study Booklet-1Dr Sumant SharmaNo ratings yet
- Hipotiroidisme Pasca Radioterapi Untuk Karsinoma NasofaringDocument28 pagesHipotiroidisme Pasca Radioterapi Untuk Karsinoma NasofaringDeandles WattimuryNo ratings yet
- PhyloCode v5 BetaDocument69 pagesPhyloCode v5 Betagobxs4b1iNo ratings yet
- Life Sciences Part 2 CSIR JRF NET GATE DBT PDFDocument167 pagesLife Sciences Part 2 CSIR JRF NET GATE DBT PDFsaranya100% (2)
- FCI Previous Question PapersDocument5 pagesFCI Previous Question PapersRohit BeriNo ratings yet
- Rheedea19 73-74Document2 pagesRheedea19 73-74manudevkmadhavanNo ratings yet
- Core Program Spring 2022 23 Course Details Jan09Document54 pagesCore Program Spring 2022 23 Course Details Jan09movefe8960No ratings yet
- Hia HraDocument30 pagesHia Hrashintia febrianiNo ratings yet
- Diamond 1997Document457 pagesDiamond 1997Learning Club100% (3)