Professional Documents
Culture Documents
Maldigestion/malabsorption Syndromes: Fecal Analysis
Maldigestion/malabsorption Syndromes: Fecal Analysis
Uploaded by
Monica Domingo0 ratings0% found this document useful (0 votes)
56 views2 pagesFecal analysis is used to detect gastrointestinal bleeding, liver and biliary disorders, malabsorption syndromes, and infections. It involves macroscopic and microscopic examination of feces as well as chemical analyses. Specific tests are used to detect occult blood, fat malabsorption, inflammation, and pancreatic insufficiency. Accurate specimen collection is important for meaningful analysis and diagnosis.
Original Description:
Reference: AUBf; Strasinger
Original Title
Fecal Analysis
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentFecal analysis is used to detect gastrointestinal bleeding, liver and biliary disorders, malabsorption syndromes, and infections. It involves macroscopic and microscopic examination of feces as well as chemical analyses. Specific tests are used to detect occult blood, fat malabsorption, inflammation, and pancreatic insufficiency. Accurate specimen collection is important for meaningful analysis and diagnosis.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
0 ratings0% found this document useful (0 votes)
56 views2 pagesMaldigestion/malabsorption Syndromes: Fecal Analysis
Maldigestion/malabsorption Syndromes: Fecal Analysis
Uploaded by
Monica DomingoFecal analysis is used to detect gastrointestinal bleeding, liver and biliary disorders, malabsorption syndromes, and infections. It involves macroscopic and microscopic examination of feces as well as chemical analyses. Specific tests are used to detect occult blood, fat malabsorption, inflammation, and pancreatic insufficiency. Accurate specimen collection is important for meaningful analysis and diagnosis.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
You are on page 1of 2
Fecal Analysis Mucus/blood-streaked mucus
o Colitis (Inflammation of the intestinal wall)
Used in the detection of gastrointestinal (GI) bleeding, liver and o Dysentry Malignancy
biliary duct disorders, malabsorption syndromes, and infections. o Constipation
Routine fecal examination: Clay-colored, pale
o Macroscopic o Bile-duct obstruction/obstructive jaundice
o Microscopic Microscopic Examination
o chemical analyses: of Feces
early detection of gastrointestinal (GI) bleeding Fecal leukocytes
liver and biliary duct disorders Determine cause of diarrhea
maldigestion/malabsorption syndromes Neutrophils:
inflammation Bacterial intestinal wall infections or ulcerative colitis, abscesses
causes of diarrhea and steatorrhea. No neutrophils: Toxin-producing bacteria, viruses, and
Fluid regulation in the gastrointestinal parasites
tract. Common Fecal Test for Diarrhea
Qualitative fecal fat:
Detects fat malabsorption disorders by staining
fecal fats with Sudan III or oil red O; increased fecal fat (>60
Specimen Collection droplets/hpf) suggestive of steatorrhea
Collection of a fecal specimen, frequently called a stool Muscle fibers: Look for undigested striated muscle fibers,
specimen, which may
is not an easy task for patients. Detailed instructions and o indicate pancreatic insufficiency seen in cystic fibrosis
appropriate containers should be provided. Methylene Blue Stain Procedure
Patients should be instructed to collect the specimen in a clean for Fecal Leukocytes
container, such as a bedpan or disposable container, and transfer o Place mucus or a drop of liquid stool on a slide.
the specimen to the laboratory container o Add two drops Löffler methylene blue.
usually collected in plastic or glass containers with screw- o Mix with a wooden applicator stick.
capped tops similar to those used for urine specimens. o Allow to stand 2–3 minutes.
For quantitative testing, such as for fecal fats, timed specimens o Examine for neutrophils under high power.
are required(the most representative sample is a 3-day Muscle Fiber Procedure
collection) o Emulsify a small amount of stool in two drops of 10%
Macroscopic Screening eosin in alcohol.
Color o Coverslip and let stand 3 minutes.
Black (tarry) stool: o Examine under high power for 5 minutes.
o Upper GI bleeding o Count the number of undigested fibers.
o iron therapy Chemical Testing of Feces
o Charcoal Occult blood
o Bismuth (antacids) Used for early detection of colorectal cancer; old name, guaiac
Red stool: test
o Lower GI bleeding Occult blood most frequently performed fecal analysis
o Beets and Food coloring Several chemicals used that vary in sensitivity
o Rifampin o Ortho-toluidine: Pseudoperoxidase activity of hemoglobin
Pale Yellow, White, Gray (Hb)
o Bile-duct obstruction reacts with H2O2 to oxidize a colorless reagent to a
o Barium sulfate colored product.
Hb —» H2O2 —> ortho-toluidine —» blue oxidized
Green
indicator
o Biliverdin-oral antibiotics
o Gum guaiac: Least sensitive, most common
o Green Vegetables
Occult Blood Testing Interference
Bulky/Frothy False-Positive
o Bile-duct obstruction o Aspirin and anti-inflammatory medications
o Pancreatic disorders o Horseradish
Ribbon-like o Melons
o Intestinal constriction/ Bowel obstruction
o Menstrual and hemorrhoid contamination
o Raw broccoli, cauliflower, radishes, turnips
o Red meat
False-Negative
o Iron supplements containing vitamin C
o Vitamin C 250 mg/d
Immunological:
Use of an antihemoglobin to react with the patient's hemoglobin
has the advantage of not requiring any special diet before sample
collection.
There is the possibility, however, of hemoglobin degradation
(and nondetection by antibody), if the gastrointestinal bleed is in
the upper intestine
DNA test
detects K-ras mutation, which is associated with colorectal
cancer.
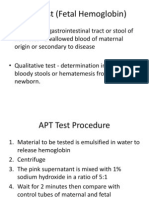
APT Test (Fetal Hemoglobin)
Grossly bloody stools and vomitus are sometimes seen in
neonates as the result of swallowing maternal blood during
delivery.
o Should it be necessary to distinguish between the presence
of fetal blood or maternal blood in an infant’s stool or
vomitus, the APT test may be requested.
The APT test distinguishes not only between fetal hemoglobin
and hemoglobin A but also between maternal hemoglobins AS,
CS, and SS, and fetal hemoglobin. The presence of maternal
thalassemia major would produce erroneous results owing the
high concentration of hemoglobin F. Stool specimens should be
tested when fresh. They may appear bloody bu should not be
black and tarry, because this would indicate already denatured
hemoglobin
APT Test Procedure
o Emulsify specimen in water.
o Centrifuge.
o Divide pink supernatant into two tubes.
o Add 1% sodium hydroxide to one tube.
o Wait 2 minutes.
o Compare color with that in the control tube.
o Prepare controls using cord blood and adult blood.
Trypsin
Emulsified specimen placed on x-ray paper determines ability to
digest gelatin
Inability to digest gelatin indicates lack of trypsin
Clinitest
Addition of Clinitest tablet to emulsified stool detects presence
of reducing substances
Reaction of 0.5 g/dL reducing substances suggests carbohydrate
intolerance
Fecal chymotrypsin
It is more resistant to intestinal degradation and is a more
sensitive indicator of less severe cases of pancreatic
insufficiency.
remains stable in fecal specimens for up to 10 days at room
temperature.
Chymotrypsin is capable of gelatin hydrolysis but is most
frequently measured by spectrophotometric method.
Elastase I
Elastase I is an isoenzyme of the enzyme elastase and is the
enzyme form produced by the pancreas. It is present in high
concentrations in pancreatic secretions and is strongly resistant
to degradation. It accounts for about 6% of all secreted
pancreated enzymes.
Elastase I can be measured by immunoassay using the ELISA kit
You might also like
- UrinalysisDocument16 pagesUrinalysisJestha Parayno De Vera100% (6)
- Stool ExaminationDocument82 pagesStool Examinationambadepravin100% (2)
- Mission Urinalysis Strips InsertDocument1 pageMission Urinalysis Strips Insertquirmche70No ratings yet
- APT Test (Fetal Hemoglobin)Document11 pagesAPT Test (Fetal Hemoglobin)Diovic TanNo ratings yet
- Clerks UA FADocument2 pagesClerks UA FALanceNo ratings yet
- FECALYSISDocument13 pagesFECALYSISXyleene Jency Bien IINo ratings yet
- Stool Exam and Lab HepatitisDocument10 pagesStool Exam and Lab HepatitisGabriella TjondroNo ratings yet
- Routine FecalysisDocument25 pagesRoutine FecalysisE. B. F.No ratings yet
- Parasitology Lab M2 Routine FecalysisDocument4 pagesParasitology Lab M2 Routine Fecalysiseumhir7No ratings yet
- (HANDOUT) Phar 112 Lab - Fecalysis and Fecal Occult Blood TestDocument2 pages(HANDOUT) Phar 112 Lab - Fecalysis and Fecal Occult Blood TestHan SoloNo ratings yet
- GROUP 1 - Sweat and UrineDocument9 pagesGROUP 1 - Sweat and Urinechocoholic potchiNo ratings yet
- Fecal Analisys: Evi Puspita SariDocument17 pagesFecal Analisys: Evi Puspita Sarisepti dwi andiniNo ratings yet
- 4.special Methods and Clinical Identification in Digestive SystemDocument37 pages4.special Methods and Clinical Identification in Digestive SystemToafan MegaNo ratings yet
- StolDocument4 pagesStolRohit kumar SainiNo ratings yet
- StoolDocument28 pagesStoolThampron ThongphanNo ratings yet
- FECAL ANALYSIS Lecture NotesDocument2 pagesFECAL ANALYSIS Lecture NotesanonacadsNo ratings yet
- Gastrointestinal SystemDocument7 pagesGastrointestinal SystemSofia P. PanlilioNo ratings yet
- Clinical MicrosDocument20 pagesClinical MicrosKG CubilNo ratings yet
- Clin Path - UrinalysisDocument6 pagesClin Path - UrinalysisequneNo ratings yet
- Clinical Pathology Final PresentationDocument16 pagesClinical Pathology Final Presentationmomin.laangNo ratings yet
- 2 3 4 General Stool Examination Intestinal Pathogenic Protozoa 2Document24 pages2 3 4 General Stool Examination Intestinal Pathogenic Protozoa 2بلسم محمود شاكرNo ratings yet
- Stool Analysis: What Is The Stool or Feces?Document28 pagesStool Analysis: What Is The Stool or Feces?Annisa SafiraNo ratings yet
- Activity 12 UrineDocument52 pagesActivity 12 UrineNoraine Princess TabangcoraNo ratings yet
- Iii. Medical Management A. Diagnostic and Laboratory ProceduresDocument11 pagesIii. Medical Management A. Diagnostic and Laboratory ProceduresNickaela CalalangNo ratings yet
- Activity 8 - HERCE - BSMT1BDocument3 pagesActivity 8 - HERCE - BSMT1BJolan Fernando HerceNo ratings yet
- Lab Exercise 10 Stool Specimen CollectionDocument12 pagesLab Exercise 10 Stool Specimen CollectionArianne Jans Munar100% (1)
- Fecal AnalysisDocument13 pagesFecal AnalysisYormae QuezonNo ratings yet
- Para Lab Part 1Document2 pagesPara Lab Part 1Vanessa May BlancioNo ratings yet
- Ladja, Irish V. BSN 3-C Laboratory ResultsDocument13 pagesLadja, Irish V. BSN 3-C Laboratory ResultsEzra LambarteNo ratings yet
- FECALYSISDocument14 pagesFECALYSISMarl EstradaNo ratings yet
- MetabolismDocument58 pagesMetabolismZ ZernsNo ratings yet
- AUBF Lec Week#5 Chemical ExaminationDocument48 pagesAUBF Lec Week#5 Chemical ExaminationLexaNatalieConcepcionJuntadoNo ratings yet
- Sild 2021Document20 pagesSild 2021Elham AlwagaaNo ratings yet
- Stool AnalysisDocument8 pagesStool AnalysisAbed AbusalemNo ratings yet
- Labdxtransfinals PDFDocument16 pagesLabdxtransfinals PDFSubhan Souda MangalasseryNo ratings yet
- D. Bile Salts: Hay's TestDocument19 pagesD. Bile Salts: Hay's TestAjay SomeshwarNo ratings yet
- Chemical Urinalysis TransDocument8 pagesChemical Urinalysis TransIan Carlo B GalangNo ratings yet
- Gastrointestinal Bleeding in Infants and Children AAPDocument16 pagesGastrointestinal Bleeding in Infants and Children AAPDina MarselinaNo ratings yet
- Aubf Lec Fecal AnalysisDocument23 pagesAubf Lec Fecal Analysisborn to slay btsNo ratings yet
- Clinical Pathology: Sample Chapter From BSAVA Manual of Canine and Feline 2nd EditionDocument21 pagesClinical Pathology: Sample Chapter From BSAVA Manual of Canine and Feline 2nd EditionAvram Ionut RazvanNo ratings yet
- Urine Dipstick Testing + Common Renal Problem 2012Document52 pagesUrine Dipstick Testing + Common Renal Problem 2012Ainul ArinaNo ratings yet
- Aubf Chemical Examination Credits To The OwnerDocument19 pagesAubf Chemical Examination Credits To The Ownerchippai100% (2)
- Evaluation and Management of Chronic Diarrhea: Joe Harkins, PA-C Gastroenterology Center of Maine EMMC Bangor, MEDocument74 pagesEvaluation and Management of Chronic Diarrhea: Joe Harkins, PA-C Gastroenterology Center of Maine EMMC Bangor, MErehan hayderNo ratings yet
- Urine Physical ExamDocument3 pagesUrine Physical ExamFait HeeNo ratings yet
- Primary Care: Review ArticleDocument9 pagesPrimary Care: Review Articleapi-2284391100% (2)
- UrinalysisDocument35 pagesUrinalysisAbdulelah MurshidNo ratings yet
- Stool AnalysisDocument8 pagesStool AnalysisLuciaGomez100% (1)
- Clinical Microscopy (Fecalysis)Document2 pagesClinical Microscopy (Fecalysis)Sheng Ramos AglugubNo ratings yet
- Clinical Pathology (Urin and Feces) 4semesterDocument6 pagesClinical Pathology (Urin and Feces) 4semesterSiddhi KaulNo ratings yet
- Stool Analysis: Formation of Feces/stoolDocument16 pagesStool Analysis: Formation of Feces/stoolTifanny WijayaNo ratings yet
- Urinalysis and Body Fluids2020Document47 pagesUrinalysis and Body Fluids2020MONFOLA100% (2)
- Metabolic DisturbancesDocument34 pagesMetabolic DisturbancesKyle DapulagNo ratings yet
- Clinical Pathology Fecalysis and UrnalysisDocument16 pagesClinical Pathology Fecalysis and UrnalysisRem Alfelor100% (3)
- اليزيد UrinalysisDocument48 pagesاليزيد UrinalysisRa'aft Al-SamawiNo ratings yet
- UrineDocument52 pagesUrineMohammed Tahoun100% (1)
- Urine Examination & Analysis: Assigned By: DR - Javeria Khan Presented By: DR - Noor-ul-Ain SarwarDocument123 pagesUrine Examination & Analysis: Assigned By: DR - Javeria Khan Presented By: DR - Noor-ul-Ain SarwarErenjaeger TitanNo ratings yet
- Clinical MicrosDocument28 pagesClinical MicrosKristine Jamella Maris NaragNo ratings yet
- Urine AnalysisDocument33 pagesUrine AnalysisajaysomNo ratings yet
- URINALYSIS Power Point PresentationDocument20 pagesURINALYSIS Power Point PresentationOlugbenga A AdetunjiNo ratings yet
- Liver Cirrhosis, A Simple Guide To The Condition, Treatment And Related DiseasesFrom EverandLiver Cirrhosis, A Simple Guide To The Condition, Treatment And Related DiseasesNo ratings yet
- A Simple Guide to Blood in Stools, Related Diseases and Use in Disease DiagnosisFrom EverandA Simple Guide to Blood in Stools, Related Diseases and Use in Disease DiagnosisRating: 3 out of 5 stars3/5 (1)
- Chapter 2 - Safety in The Hematology LaboratatoryDocument10 pagesChapter 2 - Safety in The Hematology LaboratatoryMonica DomingoNo ratings yet
- Chapter 1 - Introduction To HematologyDocument9 pagesChapter 1 - Introduction To HematologyMonica DomingoNo ratings yet
- Chapter 3 - Blood Specimen CollectionDocument12 pagesChapter 3 - Blood Specimen CollectionMonica DomingoNo ratings yet
- Streptococcus Infection, On TheDocument3 pagesStreptococcus Infection, On TheMonica DomingoNo ratings yet
- Chemical Examination of Urine: Summary of Reagent Strip Testing Quality ControlDocument5 pagesChemical Examination of Urine: Summary of Reagent Strip Testing Quality ControlMonica DomingoNo ratings yet
- Introduction To UrinalysisDocument1 pageIntroduction To UrinalysisMonica DomingoNo ratings yet
- Renal Function and Related DiseasesDocument3 pagesRenal Function and Related DiseasesMonica DomingoNo ratings yet
- Red Urine: Basic (Routine) UrinalysisDocument4 pagesRed Urine: Basic (Routine) UrinalysisMonica DomingoNo ratings yet
- Apt 1955Document7 pagesApt 1955yorghiLNo ratings yet
- Vaka TustimeDocument887 pagesVaka TustimeMohamed AbbasNo ratings yet
- Poop Emoji Minitheme by SlidesgoDocument31 pagesPoop Emoji Minitheme by SlidesgoNikoh Anthony EwayanNo ratings yet
- Maldigestion/malabsorption Syndromes: Fecal AnalysisDocument2 pagesMaldigestion/malabsorption Syndromes: Fecal AnalysisMonica DomingoNo ratings yet
- Pre-NEET Pediatrics Taruna MehraDocument181 pagesPre-NEET Pediatrics Taruna MehraNick Amonsull Phanuwat0% (1)
- Lower Gastrointestinal Bleeding in Children - Causes and Diagnostic Approach - UpToDateDocument37 pagesLower Gastrointestinal Bleeding in Children - Causes and Diagnostic Approach - UpToDateRizaru RinarudeNo ratings yet
- Trans Aubf Lec13Document5 pagesTrans Aubf Lec13USLT- Angoluan, Andrei T.No ratings yet