Professional Documents
Culture Documents
Etanercept in Alzheimer Disease: A Randomized, Placebo-Controlled, Double-Blind, Phase 2 Trial
Etanercept in Alzheimer Disease: A Randomized, Placebo-Controlled, Double-Blind, Phase 2 Trial
Uploaded by
Giuseppe AcanforaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Etanercept in Alzheimer Disease: A Randomized, Placebo-Controlled, Double-Blind, Phase 2 Trial
Etanercept in Alzheimer Disease: A Randomized, Placebo-Controlled, Double-Blind, Phase 2 Trial
Uploaded by
Giuseppe AcanforaCopyright:
Available Formats
Etanercept in Alzheimer disease
A randomized, placebo-controlled, double-blind, phase 2 trial
Joseph Butchart, MRCP ABSTRACT
Laura Brook, BSc Objectives: To determine whether the tumor necrosis factor a inhibitor etanercept is well tolerated
Vivienne Hopkins, RMN and obtain preliminary data on its safety in Alzheimer disease dementia.
Jessica Teeling, PhD
Methods: In a double-blind study, patients with mild to moderate Alzheimer disease dementia
Ursula Püntener, PhD
were randomized (1:1) to subcutaneous etanercept (50 mg) once weekly or identical placebo over
David Culliford, MSc
a 24-week period. Tolerability and safety of this medication was recorded including secondary
Richard Sharples, MD
outcomes of cognition, global function, behavior, and systemic cytokine levels at baseline, 12
Saif Sharif, MRCPsych
weeks, 24 weeks, and following a 4-week washout period. This trial is registered with EudraCT
Brady McFarlane,
(2009-013400-31) and ClinicalTrials.gov (NCT01068353).
MRCPsych
Rachel Raybould, PhD Results: Forty-one participants (mean age 72.4 years; 61% men) were randomized to etanercept
Rhodri Thomas, BSc (n 5 20) or placebo (n 5 21). Etanercept was well tolerated; 90% of participants (18/20) com-
Peter Passmore, FRCP pleted the study compared with 71% (15/21) in the placebo group. Although infections were
V. Hugh Perry, DPhil more common in the etanercept group, there were no serious adverse events or new safety
Clive Holmes, FRCPsych concerns. While there were some interesting trends that favored etanercept, there were no sta-
tistically significant changes in cognition, behavior, or global function.
Conclusions: This study showed that subcutaneous etanercept (50 mg/wk) was well tolerated in
Correspondence to this small group of patients with Alzheimer disease dementia, but a larger more heterogeneous
Prof. Holmes:
c.holmes@soton.ac.uk group needs to be tested before recommending its use for broader groups of patients.
Classification of evidence: This study shows Class I evidence that weekly subcutaneous etaner-
cept is well tolerated in Alzheimer disease dementia. Neurology® 2015;84:2161–2168
GLOSSARY
AD 5 Alzheimer disease; ADAS-cog 5 Alzheimer’s Disease Assessment Scale–cognitive; BADLS 5 Bristol Activities of Daily
Living Scale; CGI-I 5 Clinical Global Impression–Improvement; CI 5 confidence interval; CRP 5 C-reactive protein; IL 5
interleukin; IQR 5 interquartile range; ITT-LOCF 5 intention to treat–last observation carried forward; NPI 5 Neuropsychi-
atric Inventory; RPCT 5 randomized placebo-controlled trial; sMMSE 5 standardized Mini-Mental State Examination; TNF-
a 5 tumor necrosis factor a.
Acute and chronic systemic inflammation is characterized by the production of proinflammatory
cytokines including tumor necrosis factor a (TNF-a) from immune cells. TNF-a has a role in
systemic immune-to-brain communication by activating the central immune response.1 In
humans, low levels of chronic systemic inflammation are associated with evidence of microglial
activation.2 In animals, experimentally induced acute systemic inflammation results in an exag-
gerated central immune response leading to exacerbated neurodegeneration.3 In participants
with Alzheimer disease (AD) dementia, we have shown that modestly increased serum TNF-a
levels are associated with an increased rate of cognitive decline4 and an exaggeration of neuro-
psychiatric symptoms.5
Peer-reviewed published data on the use of the TNF-a inhibitor etanercept in AD dementia
is limited to small open-label studies6–8 purporting to deliver etanercept centrally9 through a
perispinal administration route. However, we have hypothesized that peripheral administration
Supplemental data
at Neurology.org
From the Faculty of Medicine, Clinical Experimental Sciences (J.B., L.B., D.C., C.H.), and Faculty of Natural and Environmental Science, Centre
for Biological Sciences (J.T., U.P., V.H.P.), University of Southampton; Memory Assessment and Research Centre (J.B., L.B., V.H., R.S., S.S.,
C.H.), Moorgreen Hospital, Southern Health Foundation Trust, Southampton; Becton Health Centre (B.M.), Southern Health Foundation Trust,
New Milton; Centre for Public Health (P.P.), Queens University Belfast; MRC Centre for Neuropsychiatric Genetics and Genomics (R.R., R.T.),
Institute of Psychological Medicine and Clinical Neurosciences, Cardiff University, UK.
Go to Neurology.org for full disclosures. Funding information and disclosures deemed relevant by the authors, if any, are provided at the end of the article.
© 2015 American Academy of Neurology 2161
ª 2015 American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
of a TNF-a inhibitor with high affinity and psychometric measures of subcutaneous eta-
specificity could, if well tolerated and safe, nercept in a mild to moderate AD population.
have long-term beneficial cognitive and behav-
ioral efficacy in an AD dementia population METHODS Standard protocol approvals, registrations,
and participant consents. The protocol and consent forms were
through inhibition of peripheral signaling to approved by a multicenter research ethics committee (Southamp-
the brain.10 Peripheral administration of TNF- ton and South West Hampshire REC [A], reference number
a inhibitors is licensed for a wide range of 10/H0502). All participants provided informed consent before
rheumatologic and skin conditions in the screening procedures. The study was registered with EudraCT
(2009-013400-31) and ClinicalTrials.gov (NCT01068353).
elderly but there are no randomized placebo-
controlled trials (RPCTs) of these drugs in AD Study design and participants. Safety and Tolerability of Eta-
nercept in Alzheimer’s Disease was an investigator-initiated, 24-
dementia that give comparative data regarding week, single-center, phase 2, double-blind RPCT to assess the
tolerability, safety, or its effects (beneficial or tolerability and safety of weekly 50 mg subcutaneous etanercept
otherwise) on measures of clinical outcome. in participants with AD dementia including cognitive, behavioral,
and functional outcomes.
We report the findings of a double-blind,
The study was performed in accordance with the Declaration of
phase 2 RPCT examining the tolerability, Helsinki and the principles of Good Clinical Practice. An indepen-
safety, and clinical effects on secondary clinical dent data and safety monitoring board monitored adverse events.
Figure 1 Trial profile
ITT-LOCF 5 intention to treat–last observation carried forward.
2162 Neurology 84 May 26, 2015
ª 2015 American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
At screening, eligible participants had to be aged 55 years or team health professionals who were blinded to treatment
older, be diagnosed with probable AD defined by the National allocation.
Institute of Neurological and Communicative Disorders and
Stroke–Alzheimer’s Disease and Related Disorders Association Procedures. Following consent, patients underwent a screening
period including initial tuberculosis and infectious disease screen
criteria11 (diagnostic accuracy approximately 75%12,13), have a
modified Hachinski Ischemic Scale score14 of less than 5 points, (i.e., a chest radiograph, tuberculin skin, and an interferon
have a standardized Mini-Mental State Examination (sMMSE)15 gamma release test). Participants fulfilling the inclusion and
exclusion criteria received etanercept 50 mg or placebo subcuta-
score above 10 and below 27 points, have an informant spending
at least 24 hours per week with the participant, and be capable of neously once per week for 24 weeks. This was followed by a 4-
giving informed consent. Patients receiving a cholinesterase week washout period in which no injections were given but in
which blinding was maintained. Clinic visits took place at
inhibitor, memantine, or antidepressant medication were
required to have been on medication for a minimum period of screening, baseline, week 12, week 24, and 4 weeks after the
90 days before baseline. Patients with prior exposure to amyloid last study drug injection (week 28). Patients who withdrew
vaccines, monoclonal antibodies, or IV immunoglobulins for the from the study before scheduled clinic visits were seen within
1 week of withdrawal for an early termination visit. During
treatment of AD were excluded. Patients with rheumatoid arthri-
tis, psoriasis, psoriatic arthritis, or ankylosing spondylitis, or those these visits, adverse event monitoring and psychometric
taking anti–TNF-a agents, immunosuppressive drugs, and/or evaluation took place. Adverse events were recorded as
definitely related, probably related, possibly related, unlikely to
oral prednisone .10 mg/d within the past 90 days were excluded.
Participants with known contraindications (active infections) or be related, or unrelated to the blinded study intervention.
cautions (previous significant exposure to tuberculosis, herpes Patients experiencing a serious adverse event or recurrent
infections were withdrawn from the study. Psychometric
zoster, hepatitis B, heart failure [New York Heart Association
grades 3 and 4], demyelination disorders, and active malignancy measures included the sMMSE,15 Alzheimer’s Disease
within past 5 years) to the use of etanercept were excluded. Assessment Scale–cognitive section (ADAS-cog),16 Bristol
Activities of Daily Living Scale (BADLS),17 Clinical Global
Randomization and masking. ACE Pharmaceuticals BV Impression–Improvement (CGI-I) scale,18 Cornell Scale for
(Zeewolde, the Netherlands) manufactured the placebo and pack- Depression in Dementia (Cornell),19 and the Neuropsychiatric
aged both the study medication and placebo to ensure blinding. Inventory (NPI).20
They used a computer to generate a simple random allocation At screening, blood samples were taken for routine clinical
sequence (1:1), stratified in blocks of 4, to ensure 20 patients laboratory assessments with additional measures of immunoglo-
in the treatment group (subcutaneous etanercept 50 mg) and bulins, anti-nuclear antibody, anti-cardiolipin, and a midstream
20 patients in the placebo group (water for injection). The inves- urine test for infection. Blood for DNA (principally for APOE
tigators had no knowledge of the allocation sequence, which re- e4 analysis) was taken at baseline. APOE genotypes were deter-
mained concealed throughout the study. ACE Pharmaceuticals mined by TaqMan genotyping of single nucleotide polymor-
loaded etanercept or placebo vials into serially numbered contain- phism (SNP) rs7412 and KASP genotyping of SNP rs429358.
ers according to the allocation sequence. The loaded containers, Blood for routine laboratory assessments and serum inflammatory
and the interventions inside them, were identical in appearance markers were taken at baseline, week 12, week 24, and week 28
and consistency to ensure concealment of the allocation sequence between 9 AM and 12 noon. Serum samples for inflammatory
from the investigators. After successful screening, participants markers were immediately placed on ice and stored within 2
were assigned the container with the next available serial number hours at 280°C. Samples were analyzed blind to the treatment
in strict chronological order. Study drug was administered by allocation using a V-PLEX assay (Meso Scale Discovery [MSD]).
weekly subcutaneous injection at home or in the clinic by study A protocol provided by MSD for custom assays was used with no
major modifications. Five serum inflammatory markers were
measured: TNF-a, interleukin (IL)-6, IL-10, IL-12p70, and C-
reactive protein (CRP).
Table 1 Characteristics of patients entering the randomization phase
Outcomes. The primary outcomes of the study were tolerability
Etanercept 50 mg Placebo Mean difference (95% CI) or Χ2, and safety. Tolerability was measured by compliance (number of
Characteristic (n 5 20) (n 5 21) p value injections given/number of planned injections) over the 24-week
Mean age, y (SE) 72.0 (2.1) 72.9 (2.2) 0.9 (25.3 to 7.1), p 5 0.8 trial period. Associated safety was measured by the number of
serious adverse events and adverse events during the study
Men, n (%) 15 (75) 10 (48) Χ2 3.2, p 5 0.07
treatment period coded using the Medical Dictionary for
White, non-Hispanic, % 1 (5) 0 (0) Χ2 1.1, p 5 0.3 Regulatory Activities (version 15.0) preferred term (http://www.
Disease duration, y (SE) 5.1 (0.8) 4.1 (0.4) 21.0 (22.8 to 0.8), p 5 0.2 meddra.org). A symptom checklist was used at each visit to probe
for adverse events.
e4 carriers, n (%) 9 (45) 11 (52) Χ2 0.2, p 5 0.6
Secondary outcomes were differences in the change from
sMMSE pts (SE) 20.0 (1.4) 20.3 (1.2) 0.3 (23.3 to 4.0), p 5 0.9 baseline of the psychometric measures (sMMSE, ADAS-cog,
ADAS-cog pts (SE) 25.8 (2.9) 25.7 (2.5) 20.1 (27.8 to 7.7), p 5 1.0 BADLS, CGI-I, Cornell, and NPI) at 12 weeks and 24 weeks
between intervention groups for observed cases and intention
BADLS pts (SE) 16.5 (3.0) 14.0 (1.7) 22.5 (29.3 to 4.3), p 5 0.5
to treat–last observation carried forward (ITT-LOCF). In addi-
NPI pts (SE) 16.4 (2.5) 12.0 (2.7) 24.4 (211.8 to 3.0), p 5 0.2 tion, emergent adverse events and psychometric changes follow-
Cornell pts (SE) 6.4 (0.8) 5.6 (1.0) 20.8 (23.4 to 1.9), p 5 0.6 ing a 4-week washout phase were measured.
Abbreviations: ADAS-cog 5 Alzheimer’s Disease Assessment Scale–cognitive; BADLS 5 Statistical analysis. This study was powered to assess tolerabil-
Bristol Activities of Daily Living Scale; CI 5 confidence interval; Cornell 5 Cornell Scale ity (dropout rates) of weekly etanercept 50-mg subcutaneous
for Depression in Dementia; NPI 5 Neuropsychiatric Inventory; pts 5 points; SE 5 standard injections and to identify adverse events associated with poor
error; sMMSE 5 standardized Mini-Mental State Examination. tolerability in an AD dementia population. The study also
Neurology 84 May 26, 2015 2163
ª 2015 American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
plots. Changes in psychometric measures and serum
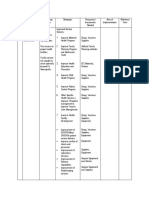
Table 2 Incidence of adverse events by system organ class category
inflammatory protein levels between the 2 intervention groups
were measured by unpaired t test and linear regression for
Adverse events,
no. of events parametric variables or Mann–Whitney U test for
(no. of participants) nonparametric variables. Clinical psychometric outcomes were
adjusted for baseline age, sex, and baseline psychometric score,
Etanercept Placebo
Disorder (n 5 20) (n 5 21)
and were conducted at p , 0.0017 significance to allow for 30
multiple comparisons.
All disorders 42 events 55
events
Blood and lymphatic system (normocytic anemia, benign 0 (0) 3 (3) RESULTS Participant disposition. Participant disposi-
monoclonal hypergammaglobulinemia)
tion is detailed in figure 1. Between January 2011
Cardiac (abnormal heart sounds, angina pectoris, irregular heart 2 (2) 2 (2) and February 2013, a total of 67 patients were screened
rate, atrial fibrillation)
at the Memory Assessment and Research Centre,
Eye (eye pain) 0 (0) 2 (2)
Southampton, UK, of whom 41 entered the study
Ear and labyrinth (wax impaction, deafness) 0 (0) 2 (1) and were assigned to either etanercept or placebo. Rea-
Gastrointestinal (nausea and vomiting, hematochezia, epigastric 5 (5) 7 (5) sons for screen failure included prior exposure to tuber-
discomfort, diarrhea, constipation, colonic polyp)
culosis or latent tuberculosis (46% [12/26]),
General fatigue 1 (1) 1 (1)
monoclonal gammopathy of unknown significance
Injection-site reaction 4 (2) 1 (1) (12% [3/26]), MMSE screen failure (8% [2/26]),
Infections (gastroenteritis, respiratory tract, urinary tract, 11 (9) 7 (6) abnormal chest radiology (8% [2/26]), skin cancer
pharyngitis, cellulitis)
(8% [2/26]), consent withdrawn before baseline (8%
Injury (falls) 2 (2) 4 (4)
[2/26]), abdominal aortic aneurysm requiring surgery
Investigations (DNA antibody positive, increase serum CRP, 6 (6) 5 (5) (4% [1/26]), clinically significant anemia (4% [1/26]),
creatinine, transaminase, colonoscopy)
and lack of adequate informant time (4% [1/26]).
Metabolic (hyperkalemia, dehydration) 2 (1) 1 (1)
Randomization phase. The mean age of the patients
Musculoskeletal (sciatica, osteoarthritis, joint stiffness, back 1 (1) 5 (3)
pain, thoracic vertebral fracture, muscle weakness) entering the study was 72.4 (SD 9.7) years, and the
Neoplasms 0 (0) 0 (0) majority (61%) were men. Randomization of patients
Nervous system (parosmia, headache, parkinsonism, balance 2 (2) 2 (2)
at baseline led to 2 treatment groups that were similar
disorder) in demographic details, APOE e4 carrier status, and
Psychiatric (poor sleep, confusional state, behavioral symptoms, 3 (3) 6 (5) psychometric test scores (p values in all cases .0.1
mood alteration, hallucinations, delusions)
except sex, p 5 0.07) (table 1). There was no signif-
Renal and urinary (urinary frequency, urinary incontinence) 1 (1) 1 (1) icant difference between treatment groups in the fre-
Respiratory (yawning) 1 (1) 0 (1) quency of participants taking a cholinesterase
Skin (varicose eczema, hyperhidrosis, seborrheic dermatitis, 1 (1) 4 (3) inhibitor (16/20 [80%] etanercept vs 18/21 [86%]
seborrheic keratitis, eczema)
placebo; Χ2 0.2, p 5 0.6), memantine (3/20 [15%]
Vascular (hypertension, lymphedema) 0 (0) 2 (2) etanercept vs 3/21 [14%] placebo; Χ2 0.004, p 5
Abbreviation: CRP 5 C-reactive protein. 0.9), or antidepressant medication (7/20 [35%] eta-
Adverse events include definitely, probably, possibly, unlikely, and not thought to be related nercept vs 8/21 [38%] placebo; Χ2 0.01, p 5 0.8).
to the study intervention. Participants could report multiple events in any category. Adverse
drug reactions are coded by the MedDRA preferred term (Medical Dictionary for Regulatory Tolerability and safety. Compliance to medication was
Activities, MedDRA 15.0). high over the 6-month trial period: overall median
100% (interquartile range [IQR] 87.5%–100%).
aimed to inform a potential phase 3 study of the variance and There was no significant difference in the median
mean differences in clinical outcome measures. To measure compliance frequency between treatment groups
dropout such that a 95% confidence interval (CI) about the (etanercept 100% [IQR 95.8%–100%] vs placebo
estimated rate had a margin of error of 615%, normal 94% [IQR 62.5%–100%]; MWU p 5 0.2). Eight
approximation about a proportion showed that 36 to 41
participants (20%) (2 on etanercept and 6 on
participants would be required for a dropout rate
commensurate with previous AD studies of between 29% and
placebo) failed to complete the study following
41%.21,22 This sample size also fell between 24 and 50 randomization. Of the 8 noncompleters, 4
recommended as necessary to estimate SDs for a future phase 3 participants (all taking placebo) failed to complete the
study.23–25 Efficacy analyses were performed on observed cases, study to 12 weeks, of whom one declined an early
defined as all patients who received at least one dose of study termination visit, and 4 participants (2 taking placebo
medication, and who provided data at baseline, week 12, and and 2 taking etanercept) failed to complete the study to
week 24, and on ITT-LOCF cases, defined as all patients who
24 weeks. Of the 2 noncompleters in the etanercept
received at least one dose of study medication, and had at least
one postrandomization assessment. Study demographic group, one participant contracted a chest infection
characteristics, efficacy measure outcomes, and serum and was withdrawn because of safety concerns and
inflammatory proteins were assessed for normality using Q-Q one participant withdrew consent because of drug
2164 Neurology 84 May 26, 2015
ª 2015 American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
delivery logistic problems. Of the 6 noncompleters in Secondary clinical outcomes. Changes in psychometric
the placebo group, 5 participants were withdrawn scores for observed cases and ITT-LOCF at 12 and
because of safety concerns (one participant contracted 24 weeks after randomization are shown in table 3
a urinary tract infection, one developed a monoclonal and figure 2. One participant randomized to placebo
gammopathy of unknown significance, one experienced withdrew from the study at 4 weeks and declined an
blood in stools, one experienced worsening of behavioral early termination assessment of clinical outcomes.
symptoms, and one participant required an elective hip Increases in psychometric scores from baseline
replacement). One participant withdrew consent indicate a worsening in outcomes except for the
because of family commitments. sMMSE for which an increase indicates an
The overall study completion was 81% (33/41). improvement. None of the clinical outcomes were
There was no statistical difference in the completion statistically significant between treatment groups
rates between those allocated to etanercept and those following Bonferroni correction.
allocated to placebo (90% [18/20] from the etaner- Washout phase. No serious adverse events occurred
cept group were completers vs 71% [15/21] from during the 4-week washout phase of the study. Six
the placebo group; Fisher exact test, p 5 0.2). participants experienced a total of 7 adverse events:
A total of 97 adverse events occurred during the 3 adverse events (fall, upper respiratory tract
24-week randomization phase of the study with one infection, gastric irritation) in 3 participants taking
serious adverse event (one participant in the placebo etanercept previously and 4 adverse events
arm was admitted to hospital with a urinary tract (disturbed sleep, fall, constipation and fall) in 3
infection). Adverse events grouped by system are participants taking placebo previously.
summarized in table 2. There were 42 (43%) adverse Allowing for Bonferroni correction, there were no
events in 20 participants in the etanercept group and significant differences in the change of psychometric
55 (57%) in 21 participants in the placebo group. scores for the sMMSE, ADAS-cog, BADLS, NPI, Cor-
Infections, injection site reactions, and investigational nell, or CGI-I during the 4-week washout phase of the
abnormalities were present in a greater number of study between those participants previously taking eta-
participants in the etanercept arm compared with nercept compared with those previously taking pla-
the placebo arm but no statistical differences were cebo: sMMSE: etanercept 20.3 vs placebo 20.1
found between groups (Χ2, all p . 0.1). points (mean difference 20.2 points [95% CI 1.7 to
Table 3 Changes in psychometric scores 12 weeks and 24 weeks for observed and ITT-LOCF after randomization compared with baseline
Week 12 Week 24
Etanercept Placebo Mean difference Etanercept Placebo Mean difference
(n 5 20) (SE) (n 5 17) (SE) correcteda (95% CI) p Value (n 5 18) (SE) (n 5 15) (SE) correcteda (95% CI) p Value
Observed
cases
sMMSE 20.6 (0.5) 20.5 (0.7) 0.004 (21.9 to 1.9) 1.0 20.1 (0.5) 21.9 (1.2) 22.5 (25.2 to 0.2) 0.07
ADAS-cog 1.3 (1.4) 1.4 (1.5) 0.2 (24.3 to 4.6) 0.9 3.2 (1.8) 5.6 (2.0) 1.2 (25.1 to 7.5) 0.7
BADLS 21.1 (2.1) 1.2 (0.9) 0.6 (24.6 to 5.8) 0.8 0.8 (1.2) 6.0 (2.1) 5.6 (0.4 to 10.9) 0.04
NPI 22.0 (2.7) 3.8 (1.6) 4.4 (23.0 to 11.7) 0.2 20.3 (3.3) 10.2 (3.6) 13.2 (2.4 to 24.0) 0.02
Cornell 20.2 (0.9) 0.1 (1.0) 0.1 (22.8 to 3.0) 0.9 0.4 (1.0) 1.9 (1.5) 1.6 (22.3 to 5.5) 0.4
CGI-I 0.4 (0.2) 0.5 (0.2) 0.2 (20.5 to 0.8) 0.6 0.6 (0.2) 0.9 (0.3) 0.3 (20.6 to 1.1) 0.3
ITT-LOCF
sMMSE 20.6 (0.5) 20.5 (0.7) 0.05 (21.7 to 1.9) 0.9 20.2 (0.5) 21.4 (1.0) 21.4 (23.8 to 1.0) 0.2
ADAS-cog 1.3 (1.4) 1.9 (1.4) 0.6 (23.6 to 4.8) 0.8 2.9 (1.7) 5.1 (1.6) 1.6 (23.5 to 6.6) 0.5
BADLS 21.1 (2.1) 1.4 (0.9) 0.5 (24.2 to 5.2) 0.8 0.5 (1.2) 4.9 (1.7) 3.7 (20.9 to 9.3) 0.1
NPI 22.0 (2.7) 3.7 (1.5) 4.2 (22.6 to 11.1) 0.2 0.8 (3.1) 6.9 (3.2) 6.5 (23.4 to 16.5) 0.2
Cornell 20.2 (0.9) 0.4 (0.8) 0.2 (22.4 to 2.9) 0.9 0.5 (0.9) 1.9 (1.2) 0.8 (22.4 to 3.9) 0.6
CGI-I 0.4 (0.2) 0.5 (0.2) 0.1 (20.5 to 0.7) 0.7 0.7 (0.2) 0.7 (0.3) 0.1 (20.8 to 0.6) 0.8
Abbreviations: ADAS-cog 5 Alzheimer’s Disease Assessment Scale–cognitive; BADLS 5 Bristol Activities of Daily Living Scale; CGI-I 5 Clinical Global
Impression–Improvement; CI 5 confidence interval; Cornell 5 Cornell Scale for Depression in Dementia; ITT-LOCF 5 intention to treat–last observation
carried forward; NPI 5 Neuropsychiatric Inventory; SE 5 standard error; sMMSE 5 standardized Mini-Mental State Examination.
All p values are 2-sided.
a
Corrected for baseline age, sex, and psychometric score.
Neurology 84 May 26, 2015 2165
ª 2015 American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
Figure 2 Mean change in outcome scores (observed cases weeks 12 and 24) and ITT-LOCF (week 24) from baseline
ADAS-cog 5 Alzheimer’s Disease Assessment Scale–cognitive; BADLS 5 Bristol Activities of Daily Living Scale; CGI-I 5 Clinical Global Impression–Improve-
ment; Cornell 5 Cornell Scale for Depression in Dementia; ITT-LOCF 5 intention to treat–last observation carried forward; MMSE 5 standardized Mini-
Mental State Examination; NPI 5 Neuropsychiatric Inventory.
22.0]), p 5 0.9; ADAS-cog: etanercept 1.3 vs placebo other participants completing the study (18
24.2 points (mean difference 5.5 points [95% CI randomized to etanercept and 14 to placebo) are
9.0–2.0]), p 5 0.003; BADLS: etanercept 2.4 vs pla- shown at baseline (week 0), week 12, week 24, and
cebo 21.7 points (mean difference 4.1 points [95% after the 4-week washout phase (week 28) in table e-1
CI 7.0 to 21.4]), p 5 0.004; NPI: etanercept 22.4 vs on the Neurology® Web site at Neurology.org. At
placebo 23.5 points (mean difference 1.1 points [95% baseline, there were no statistical differences in
CI 7.7 to 25.6]), p 5 0.7; Cornell: etanercept 20.8 vs serum TNF-a or IL-12 between the treatment and
placebo 22.1 points (mean difference 1.2 points [95% placebo groups. Following randomization, serum
CI 3.1 to 20.6]), p 5 0.6; CGI-I: etanercept 0 vs TNF-a was higher in the treatment compared with
placebo 0 points (mean difference 0 points [95% CI the placebo group at weeks 12 and 24 and was still
0.7 to 20.8]), p 5 1.0. significantly increased, although diminished, at week
Serum inflammatory markers. Serum was not available 28. Serum IL-12 was also higher in the treatment
in one (placebo randomized) participant. Serum levels compared with the placebo group at week 12 but
for TNF-a, IL-6, IL-10, IL-12p70, and CRP for all not significantly different from placebo at week 24
2166 Neurology 84 May 26, 2015
ª 2015 American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
or week 28. At baseline, serum IL-10 was statistically The current study should not be seen to support
lower in the treatment compared with the placebo the use of unlicensed subcutaneous etanercept for
group. Following randomization, serum IL-10 was the treatment of AD dementia. Etanercept has recog-
no longer significantly different from placebo at nized potentially serious adverse effects in the popula-
week 12 or 24, but following withdrawal was lower tion,27 and independent validation is needed in a
in the treatment arm at week 28. There were no larger more heterogeneous AD dementia population
significant differences between the serum to fully assess the long-term safety and clinical effects
inflammatory markers IL-6 or CRP between the of this approach.
treatment and placebo groups at baseline or weeks
12, 24, and 28. AUTHOR CONTRIBUTIONS
J.B. made a substantial contribution to the design of the work, the
acquisition and interpretation of the data, drafting the work, and re-
DISCUSSION Of the 67 patients screened for this viewing it for important intellectual content. L.B. made a substantial
study, 26 failed to meet the inclusion or exclusion cri- contribution to the design of the work, the acquisition of the data,
teria. The 2-year recruitment period was the result of and reviewing it for important intellectual content. V.H., J.T.,
U.P., R.S., S.S., R.R., R.T. made a substantial contribution to the
screening failures, the majority of which (n 5 12 acquisition of the data and reviewing it for important intellectual con-
[46%]) were attributable to prior exposure to tent. P.P., V.H.P., D.C., B.M. made a substantial contribution to the
tuberculosis, of high frequency in the United interpretation of the data and reviewing it for important intellectual
content. C.H. made a substantial contribution to the conception of
Kingdom aged population,26 and to drug delivery
the study, the design of the work, the acquisition and interpretation
delay following Pfizer’s acquisition of Wyeth. of the data, drafting the work, and reviewing it for important intellec-
Compliance was high over the 24-week trial period tual content. All authors had full access to all of the data in the study
with no significant differences between treatment and C.H. had final responsibility for the decision to submit for
publication.
groups. Ninety percent of patients (18/20)
completed the etanercept arm of the study. There ACKNOWLEDGMENT
were no serious adverse events in the etanercept The authors thank study personnel at the Memory Assessment and
arm. Adverse events, including infection rates and Research Centre who were involved in administration, drug delivery, ven-
esection, and sample preparation including Lyn Davies, Suzanne Dodge,
injection-site reactions, were in keeping with the Isobel Lewsey, Margaret Nicholls, Ceri Rayner, Rebecca Sussams, and
known, and potentially serious, side effects of Annette Stevens. The authors also thank NIHR DenDRoN for support
etanercept,27 but no new safety concerns were and all patients and carers who took part in this study.
found regarding the use of etanercept in patients
STUDY FUNDING
with AD dementia.
This study was funded as an independent investigator-initiated grant
Whereas the psychometric changes in the placebo awarded by Pfizer Pharmaceuticals to Prof. Clive Holmes.
arm are in keeping with observed changes reported
elsewhere in similar populations,28,29 the change in DISCLOSURE
ADAS-cog was double than anticipated.4 While every J. Butchart, L. Brook, V. Hopkins, J. Teeling, U. Püntener, D. Culliford,
R. Sharples, S. Sharif, B. McFarlane, R. Raybould, R. Thomas, P. Pass-
attempt was made to improve internal validity by
more, and V. Perry report no disclosures relevant to the manuscript.
ensuring raters received the same psychometric rating C. Holmes reports receiving an independent investigator-initiated grant
training and, wherever possible, not change between from Pfizer to fund this study. Go to Neurology.org for full disclosures.
visits, small numbers in the study cannot rule out the
random allocation of a more rapidly declining group Received November 28, 2014. Accepted in final form February 15, 2015.
to the placebo arm and differences between groups
REFERENCES
should be viewed with caution. There was no statis- 1. Perry VH, Cunningham C, Holmes C. Systemic infec-
tical difference between the cognitive, functional, and tions and inflammation affect chronic neurodegeneration.
behavioral assessments in the etanercept compared Nat Rev Immunol 2007;7:161–167.
with the placebo group (or worsening following with- 2. Drake C, Boutin H, Jones MS, et al. Brain inflammation
drawal) after Bonferroni correction. Serum TNF-a is induced by co-morbidities and risk factors for stroke.
Brain Behav Immun 2011;25:1113–1122.
showed a marked increase in the etanercept-treated
3. Cunningham C, Wilcockson DC, Campion S, Lunnon K,
group compared with the placebo group, reflecting Perry VH. Central and systemic endotoxin challenges
the increased half-life of the inert dimeric fusion pro- exacerbate the local inflammatory response and increase
tein after binding of TNF-a.30,31 neuronal death during chronic neurodegeneration.
The use of subcutaneous etanercept in this study is J Neurosci 2005;25:9275–9284.
based on the hypothesis of modifying long-term, low- 4. Holmes C, Cunningham C, Zotova E, et al. Systemic
inflammation and disease progression in Alzheimer disease.
grade peripheral systemic inflammation,1,4,10,32 a
Neurology 2009;73:768–774.
different concept than the hypothesized rapid modi-
5. Holmes C, Cunningham C, Zotova E, Culliford D,
fication of central TNF-a through a periventricular Perry VH. Proinflammatory cytokines, sickness behav-
approach,7 which has not been participant to an ior, and Alzheimer disease. Neurology 2011;77:
RPCT and remains highly controversial.33 212–218.
Neurology 84 May 26, 2015 2167
ª 2015 American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
6. Tobinick E, Gross H, Weinberger A, Cohen H. TNF- 20. Cummings JL. The neuropsychiatric inventory: assessing
alpha modulation for treatment of Alzheimer’s disease: a psychopathology in dementia patients. Neurology 1997;
6-month pilot study. MedGenMed 2006;8:25. 48(5 suppl 6):S10–S16.
7. Tobinick EL, Gross H. Rapid cognitive improvement in 21. Birks J. Cholinesterase inhibitors for Alzheimer’s disease.
Alzheimer’s disease following perispinal etanercept admin- Cochrane Database Syst Rev 2006;(1):CD005593.
istration. J Neuroinflammation 2008;5:2. 22. Tabet N, Feldman H. Indomethacin for the treatment of
8. Tobinick EL, Gross H. Rapid improvement in verbal Alzheimer’s disease patients. Cochrane Database Syst Rev
fluency and aphasia following perispinal etanercept in 2002;(2):CD003673.
Alzheimer’s disease. BMC Neurol 2008;8:27. 23. Browne RH. On the use of a pilot sample for sample size
9. Tobinick EL, Chen K, Chen X. Rapid intracerebroven- determination. Stat Med 1995;14:1933–1940.
tricular delivery of Cu-DOTA-etanercept after peripheral 24. Sim J, Lewis M. The size of a pilot study for a clinical trial
administration demonstrated by PET imaging. BMC Res should be calculated in relation to considerations of preci-
Notes 2009;2:28. sion and efficiency. J Clin Epidemiol 2012;65:301–308.
10. Perry VH, Holmes C. Microglial priming in neurodegen- 25. Julious SA. Sample size of 12 per group rule of thumb for
erative disease. Nat Rev Neurol 2014;10:217–224. a pilot study. Pharm Stat 2005;4:287–291.
11. McKhann G, Drachman D, Folstein M, Katzman R, Price D, 26. British Thoracic Society Standards of Care Committee.
Stadlan EM. Clinical diagnosis of Alzheimer’s disease: report BTS recommendations for assessing risk and for managing
of the NINCDS-ADRDA Work Group under the auspices of Mycobacterium tuberculosis infection and disease in pa-
Department of Health and Human Services Task Force on tients due to start anti-TNF-alpha treatment. Thorax
Alzheimer’s Disease. Neurology 1984;34:939–944. 2005;60:800–805.
12. Lim A, Tsuang D, Kukull W, et al. Clinico-neuropatho- 27. Summary of product characteristics (ENBREL). Available at:
logical correlation of Alzheimer’s disease in a community- http://www.medicines.org.uk/emc/medicine/3343/SPC/
based series. J Am Geriatr Soc 1999;47:564–569. Enbrel1251mg1powder1and1solvent1for1solution
13. Holmes C, Cairns N, Lantos P, Mann A. Validity of cur- 1for1injection/. Accessed January 29, 2015.
rent clinical criteria for Alzheimer’s disease, vascular 28. McGuinness B, O’Hare J, Craig D, Bullock R, Malouf R,
dementia and dementia with Lewy bodies. Br J Psychiatry Passmore P. Statins for the treatment of dementia. Co-
1999;174:45–50. chrane Database Syst Rev 2010;(8):CD007514.
14. Hachinski VC, Iliff LD, Zilhka E, et al. Cerebral blood 29. Howard R, Phillips P, Johnson T, et al. Determining
flow in dementia. Arch Neurol 1975;32:632–637. the minimum clinically important differences for out-
15. Molloy DW, Standish TI. A guide to the standardized comes in the DOMINO trial. Int J Geriatr Psychiatry
Mini-Mental State Examination. Int Psychogeriatr 1997; 2011;26:812–817.
9(suppl 1):87–94; discussion 143–150. 30. Schulz M, Dotzlaw H, Neeck G. Ankylosing spondylitis
16. Rosen WG, Mohs RC, Davis KL. A new rating scale for and rheumatoid arthritis: serum levels of TNF-alpha and
Alzheimer’s disease. Am J Psychiatry 1984;141:1356–1364. its soluble receptors during the course of therapy with
17. Bucks RS, Ashworth DL, Wilcock GK, Siegfried K. etanercept and infliximab. Biomed Res Int 2014;2014:
Assessment of activities of daily living in dementia: devel- 675108.
opment of the Bristol Activities of Daily Living Scale. Age 31. Madhusudan S, Muthuramalingam SR, Braybrooke JP,
Ageing 1996;25:113–120. et al. Study of etanercept, a tumor necrosis factor-alpha
18. Guy W. Clinical Global Impressions (CGI) Scale. In: inhibitor, in recurrent ovarian cancer. J Clin Oncol 2005;
Rush J; American Psychiatric Association. Task Force for 23:5950–5959.
the Handbook of Psychiatric Measures. Handbook of Psy- 32. Holmes C, Butchart J. Systemic inflammation and
chiatric Measures. Washington, DC: American Psychiatric Alzheimer’s disease. Biochem Soc Trans 2011;39:898–901.
Association; 2000. 33. Novella S. Enbrel for Stroke and Alzheimer’s: Science
19. Alexopoulos GS, Abrams RC, Young RC, Shamoian CA. Based Medicine. 2014. Available at: http://www.
Cornell Scale for Depression in Dementia. Biol Psychiatry sciencebasedmedicine.org/enbrel-for-stroke-and-
1988;23:271–284. alzheimers/. Accessed January 29, 2015.
Subspecialty Alerts by E-mail!
Customize your online journal experience by signing up for e-mail alerts related to your subspecialty or
area of interest. Access this free service by visiting Neurology.org/site/subscriptions/etoc.xhtml or click
on the “E-mail Alerts” link on the home page. An extensive list of subspecialties, methods, and study
design choices will be available for you to choose from—allowing you priority alerts to cutting-edge
research in your field!
2168 Neurology 84 May 26, 2015
ª 2015 American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
You might also like
- Geriatric Anxiety Scale v2.0 FINALDocument2 pagesGeriatric Anxiety Scale v2.0 FINALpujipurwaningsih67% (3)
- Return To School FormDocument2 pagesReturn To School FormAmy LawsonNo ratings yet
- Exchange Transfusion SheetDocument2 pagesExchange Transfusion SheetWilda Awlia100% (1)
- Prospective Long-Term Study of Vagus Nerve Stimulation The Treatment of Refractory SeizuresDocument6 pagesProspective Long-Term Study of Vagus Nerve Stimulation The Treatment of Refractory SeizuresZeptalanNo ratings yet
- A 7 Minute Neurocognitive Screening Battery Highly Sensitive To Alzheimer's DiseaseDocument7 pagesA 7 Minute Neurocognitive Screening Battery Highly Sensitive To Alzheimer's DiseaseRealidades InfinitasNo ratings yet
- Advocating For Demonstration of Disease Modification - Have We Been Approaching Clinical Trials in Early Alzheimer Disease Incorrectly?Document2 pagesAdvocating For Demonstration of Disease Modification - Have We Been Approaching Clinical Trials in Early Alzheimer Disease Incorrectly?Lorrane NevesNo ratings yet
- Research Article: Neuroprotective Effects of Cistanches Herba Therapy On Patients With Moderate Alzheimer's DiseaseDocument13 pagesResearch Article: Neuroprotective Effects of Cistanches Herba Therapy On Patients With Moderate Alzheimer's DiseaseVeronica Yosita AnandaNo ratings yet
- Ref 12Document12 pagesRef 12Tiago BaraNo ratings yet
- Rogers 1993Document4 pagesRogers 1993Nadia SaiNo ratings yet
- Fisher 2010Document10 pagesFisher 2010Estereotaxia BrasilNo ratings yet
- ACD856, A Novel Positive Allosteric Modulator of TRK Receptors, Single Ascending Doses in Healthy Subjects: Safety and PharmacokineticsDocument11 pagesACD856, A Novel Positive Allosteric Modulator of TRK Receptors, Single Ascending Doses in Healthy Subjects: Safety and PharmacokineticsMichael UNo ratings yet
- Upper Airway Stimulation For Obstructive Sleep Apnea: Durability of The Treatment Effect at 18 MonthsDocument9 pagesUpper Airway Stimulation For Obstructive Sleep Apnea: Durability of The Treatment Effect at 18 MonthsHamzeh AlsalhiNo ratings yet
- Long-Term Efficacy and Safety of Thalamic Stimulation For Drug Resistant Partial EpilepsyDocument9 pagesLong-Term Efficacy and Safety of Thalamic Stimulation For Drug Resistant Partial Epilepsyana maria gonzalez uribeNo ratings yet
- Pilot Study of An Intracranial ElectroencephalographyDocument6 pagesPilot Study of An Intracranial Electroencephalographymisacho82No ratings yet
- Epi 12739Document8 pagesEpi 12739Juan Diego De La Cruz MiñanoNo ratings yet
- NLR Bells PalsyDocument4 pagesNLR Bells PalsyIskandar HasanNo ratings yet
- JurnalDocument8 pagesJurnalTher RayNo ratings yet
- Friedreich's AtaxiaDocument20 pagesFriedreich's AtaxiaSherief AKNo ratings yet
- 157 - Clinical Trials Adverse Events ChaDocument6 pages157 - Clinical Trials Adverse Events ChaWoo Rin ParkNo ratings yet
- Rhonda Byrne - El SecretoDocument8 pagesRhonda Byrne - El SecretoAlzeniraNo ratings yet
- Long Term Outcomes of Status Epilepticus: A Critical AssessmentDocument15 pagesLong Term Outcomes of Status Epilepticus: A Critical AssessmentnafamaulidinaNo ratings yet
- 1 s2.0 S0890856714004079 MainDocument10 pages1 s2.0 S0890856714004079 MainPar DoNo ratings yet
- 0202011002Document6 pages0202011002Gita DewiNo ratings yet
- Loratadine Versus Cetirizine Assessment of Somnolence and Motivation During The Workday PDFDocument10 pagesLoratadine Versus Cetirizine Assessment of Somnolence and Motivation During The Workday PDFJericho ImmanuelaNo ratings yet
- Donepezil in Vascular Dementia: A Randomized, Placebo-Controlled StudyDocument9 pagesDonepezil in Vascular Dementia: A Randomized, Placebo-Controlled StudyDian ArdiansyahNo ratings yet
- Epilepsy Duration and Seizure Outcome in Epilepsy Surgery: A Systematic Review and Meta-AnalysisDocument9 pagesEpilepsy Duration and Seizure Outcome in Epilepsy Surgery: A Systematic Review and Meta-Analysisbaba ababNo ratings yet
- Jurnal Anes 3Document10 pagesJurnal Anes 3Ari SamadNo ratings yet
- Comparative Cognitive Effects of Levetiracetam and Topiramate in Intractable EpilepsyDocument6 pagesComparative Cognitive Effects of Levetiracetam and Topiramate in Intractable EpilepsyDHIVYANo ratings yet
- Appi Neuropsych 18010005Document6 pagesAppi Neuropsych 18010005sarahNo ratings yet
- HshsjneDocument5 pagesHshsjneyunia habsariNo ratings yet
- CGJ01Document8 pagesCGJ01Dewi NofiantiNo ratings yet
- Effectiveness of Treatment For Sudden Sensorineural Hearing LossDocument4 pagesEffectiveness of Treatment For Sudden Sensorineural Hearing Lossronaldyohanesf87No ratings yet
- Hemifacial Spasm in Singapore: Clinical Characteristics and Patients' PerceptionsDocument5 pagesHemifacial Spasm in Singapore: Clinical Characteristics and Patients' PerceptionsBinita SinhaNo ratings yet
- Calin 2004 PDFDocument8 pagesCalin 2004 PDFRafaela Queiroz MascarenhasNo ratings yet
- Score Predictivo NMDA 2018Document10 pagesScore Predictivo NMDA 2018Pablo Sebastián SaezNo ratings yet
- Chemotherapy Related Cog. Dysf.Document9 pagesChemotherapy Related Cog. Dysf.Manuel Guerrero GómezNo ratings yet
- Joi 140178Document11 pagesJoi 140178holisNo ratings yet
- Nejmoa 2212948Document13 pagesNejmoa 2212948Giovanny A. RivasNo ratings yet
- Hongliang Mao Short and Long Term Response of VagusDocument16 pagesHongliang Mao Short and Long Term Response of VagusArbey Aponte PuertoNo ratings yet
- DR Makam Sri Harsha ThesisDocument33 pagesDR Makam Sri Harsha ThesissumitNo ratings yet
- Liu Et Al. (2019)Document6 pagesLiu Et Al. (2019)viniciuskiss99No ratings yet
- Impacto Do TMExpiratorio Na ELA - Clinical Trial Randomizado 2019Document7 pagesImpacto Do TMExpiratorio Na ELA - Clinical Trial Randomizado 2019dehalitedNo ratings yet
- IVIgG AmiloidDocument4 pagesIVIgG AmiloidyinvilllNo ratings yet
- Jurnal NeuroDocument12 pagesJurnal NeuroFelicia SinjayaNo ratings yet
- Behavioral Effects of Rufinamide in LGSDocument6 pagesBehavioral Effects of Rufinamide in LGSkmarmol77No ratings yet
- 2022 LEQ - CLARITY AD StudyDocument13 pages2022 LEQ - CLARITY AD Study歐陽陞No ratings yet
- CTS PDFDocument6 pagesCTS PDFBiola DwikoNo ratings yet
- Clinical Characteristics and PDocument10 pagesClinical Characteristics and Pmiss betawiNo ratings yet
- Wang 2004Document13 pagesWang 2004Ricardo Jose De LeonNo ratings yet
- Proceedings of The 2014 Spring Meeting of The Society of British 2014Document40 pagesProceedings of The 2014 Spring Meeting of The Society of British 2014rabiatul adawiyahNo ratings yet
- Copia de 09enero Sedacion Prot Vs No ProtDocument22 pagesCopia de 09enero Sedacion Prot Vs No ProtMartin LafuenteNo ratings yet
- NIH Public AccessDocument3 pagesNIH Public AccessCamilo MoraNo ratings yet
- Vagus Nerve Stimulation in The Treatment of Drug Resistant Epilepsy in 29 Children 2016 European Journal of Paediatric NeurologyDocument6 pagesVagus Nerve Stimulation in The Treatment of Drug Resistant Epilepsy in 29 Children 2016 European Journal of Paediatric NeurologyZeptalanNo ratings yet
- A Meta-Analysis On Progressive Atrophy in Intractable Temporal Lobe EpilepsyDocument12 pagesA Meta-Analysis On Progressive Atrophy in Intractable Temporal Lobe EpilepsyBeny RiliantoNo ratings yet
- Remission in Schizophrenia: One-Year Italian Prospective Study of Risperidone Long-Acting Injectable (RLAI) in Patients With Schizophrenia or Schizoaffective DisorderDocument11 pagesRemission in Schizophrenia: One-Year Italian Prospective Study of Risperidone Long-Acting Injectable (RLAI) in Patients With Schizophrenia or Schizoaffective Disorderdr.cintaNo ratings yet
- Long-Term Effects of The Concomitant Use of Memantine With Cholinesterase Inhibition in Alzheimer DiseaseDocument10 pagesLong-Term Effects of The Concomitant Use of Memantine With Cholinesterase Inhibition in Alzheimer DiseaseDewi SariNo ratings yet
- Aigner Et Al. - 2017 - Repurposing of The Anti-Asthmatic Drug Montelukast For The Treatment of Alzheimer's DiseaseDocument2 pagesAigner Et Al. - 2017 - Repurposing of The Anti-Asthmatic Drug Montelukast For The Treatment of Alzheimer's DiseaseSubashNo ratings yet
- Advantage of Modified MRI Protocol For HDocument148 pagesAdvantage of Modified MRI Protocol For HasasakopNo ratings yet
- Jurnal Etdq7 ValidatingDocument12 pagesJurnal Etdq7 Validatingdr. EndahNo ratings yet
- Research Paper: NeuropsychiatryDocument11 pagesResearch Paper: NeuropsychiatryveerrajuNo ratings yet
- Status Epilepticus in Adults: A Study From Nigeria: SciencedirectDocument6 pagesStatus Epilepticus in Adults: A Study From Nigeria: SciencedirectLuther ThengNo ratings yet
- Yoa70030 1115 1122Document8 pagesYoa70030 1115 1122Dewi NofiantiNo ratings yet
- Neuropathology Simplified: A Guide for Clinicians and NeuroscientistsFrom EverandNeuropathology Simplified: A Guide for Clinicians and NeuroscientistsNo ratings yet
- Scarlet Fever (Scarlatina) : Bacterial Infection Etiology Oral Manifestations Prevention and ControlDocument16 pagesScarlet Fever (Scarlatina) : Bacterial Infection Etiology Oral Manifestations Prevention and ControlFatima CarlosNo ratings yet
- Severe Injured Patient Multiple Fracture Patient Principle of Treatment & Maintenance of PatientDocument14 pagesSevere Injured Patient Multiple Fracture Patient Principle of Treatment & Maintenance of PatientAilar NasirzadehNo ratings yet
- Compounding Pharmacist Resume ExampleDocument1 pageCompounding Pharmacist Resume Exampleakanksha pisalNo ratings yet
- Doh Health Programs (Child Program)Document64 pagesDoh Health Programs (Child Program)Wilma Nierva BeraldeNo ratings yet
- CLOZAPINEDocument14 pagesCLOZAPINEsumaryatiNo ratings yet
- Jurnal Hubungan Faktor Sosial Ekonomi Ibu HamilDocument10 pagesJurnal Hubungan Faktor Sosial Ekonomi Ibu HamilNarulitha ririnNo ratings yet
- RBM 2530 - Tutorial 2 - Neuropathology-2011Document6 pagesRBM 2530 - Tutorial 2 - Neuropathology-2011Lina TanNo ratings yet
- Bronchopneumonia in ChildrenDocument3 pagesBronchopneumonia in ChildrenputraNo ratings yet
- Perfection Biology MCQDocument25 pagesPerfection Biology MCQAnupriya TiwariNo ratings yet
- Working Your Way Through Adas t2d Treatment AlgorithmDocument61 pagesWorking Your Way Through Adas t2d Treatment AlgorithmNgọc BíchNo ratings yet
- Asthma Drugs PDFDocument2 pagesAsthma Drugs PDFRahmat PasaribuNo ratings yet
- Expert Pediatrician Exposes Vaccine MythsDocument12 pagesExpert Pediatrician Exposes Vaccine Mythsmonika_boskovic_1No ratings yet
- Emergency NurseDocument16 pagesEmergency NurseMalathi VarnaNo ratings yet
- Intracavernosal Injection InformationDocument4 pagesIntracavernosal Injection InformationJason ArbogastNo ratings yet
- Zen ShiatsuDocument90 pagesZen ShiatsuLuz Violeta Platino100% (1)
- Forensic Med. CertificateDocument9 pagesForensic Med. Certificatedeeksha100% (2)
- Endocrine Davidson Shortlisted (Hira - Fj'23)Document45 pagesEndocrine Davidson Shortlisted (Hira - Fj'23)saifsaffa2No ratings yet
- National Consortium For Ph.D. in Nursing by Indian Nursing CouncilDocument3 pagesNational Consortium For Ph.D. in Nursing by Indian Nursing CouncilRio RioNo ratings yet
- ElectrocardiogramDocument17 pagesElectrocardiogramvinnu kalyanNo ratings yet
- Diagnosis of Brown Sequard SyndromeDocument3 pagesDiagnosis of Brown Sequard SyndromeOktavianus PrayitnoNo ratings yet
- AOP Form 3Document4 pagesAOP Form 3Ferzada SajiranNo ratings yet
- Common Drugs in Pet PracticeDocument2 pagesCommon Drugs in Pet Practiceshahbaz zafarNo ratings yet
- Multiple PregnancyDocument18 pagesMultiple PregnancyNishaThakuri100% (5)
- Icu Equipments BY: Presented Bhupender Kumar MehtoDocument35 pagesIcu Equipments BY: Presented Bhupender Kumar Mehtobhupendermehto012No ratings yet
- Crockett 2014Document14 pagesCrockett 2014JulioRoblesZanelliNo ratings yet
- DME in Saudi Arabia - Myth or FactDocument25 pagesDME in Saudi Arabia - Myth or FactHassan Al-DhibiNo ratings yet
- Msap Safety IDocument5 pagesMsap Safety IJoseph AldrinNo ratings yet