Professional Documents
Culture Documents
Celiac Disease in Children With Moderate-to-Severe Iron-Deficiency Anemia
Celiac Disease in Children With Moderate-to-Severe Iron-Deficiency Anemia
Uploaded by
Anda PostovaruOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Celiac Disease in Children With Moderate-to-Severe Iron-Deficiency Anemia
Celiac Disease in Children With Moderate-to-Severe Iron-Deficiency Anemia
Uploaded by
Anda PostovaruCopyright:
Available Formats
RESEARCH PAPER
Celiac Disease in Children with Moderate-to-Severe Iron-deficiency
Anemia
MANISH NARANG1, RAVIKUMAR NATARAJAN1, DHEERAJ SHAH1, AMARENDER SINGH PURI2, VIKAS MANCHANDA3
AND MRINALINI KOTRU4
From 1Division of Pediatric Gastroenterology, Department of Pediatrics and 4Department of Pathology,University College of
Medical Sciences and GTB Hospital; 2Department of Gastroenterology, GB Pant Institute of Post Graduate Medical Education and
Research;and 3Department of Clinical Microbiology and Infectious Diseases, Chacha Nehru Bal Chikitsalaya; Delhi, India
Correspondence to: Objective: To evaluate the proportion of children with moderate to severe iron-deficiency
Dr Manish Narang, Professor, anemia who have associated celiac disease. Methods: This cross-sectional analytical study
Department of Pediatrics, UCMS and was conducted among children aged 1 to 12 years of age with moderate-to-severe iron
deficiency anemia and control children without anemia.Serum IgA-tissue trans-glutaminase
GTB Hospital, Dilshad Garden,
levels were assessed in both cases and controls. All children with positive celiac serology
Delhi 110095, India. underwent upper gastrointestinal endoscopy and duodenal biopsy; biopsy finding of Marsh
manish_2710@yahoo.com grade 3 was considered positive for celiac disease. Results: There were 152 anemic children
Received: December 28, 2016; and 152 controls with mean (SD) hemoglobinof 7.7 (1.8) and 12.2 (0.74) g/dL, respectively.
Initial review: February 09, 2017; 16 (10.5%) cases and 3 (2%) control patients had positive serology for celiac disease [OR
Accepted: September 22, 2017. (95% CI) 5.33 (1.52-18.67), P=0.007]. Six (3.9%) children with iron-deficiency anemia and
none of the controls had biopsy features diagnostic of celiac disease. Conclusion:In the
Northern Indian tertiary-care hospital outpatient setting, Celiac disease was associated with
4% of children presenting with moderate-to-severe anemia.
Keywords: Biopsy, Diagnosis, Endoscopy, Transglutaminases.
U
nexplained iron-deficiency anemia without in children <5 years of age; <8 g/dL in children of 5 to 12
gastro-intestinal symptoms is a well- years of age [4]. Iron-deficiency was considered as a cause
recognized presentation of celiac disease of anemia if serum ferritin level was <12 ng/mL and/or
(CD) [1]. However, the data regarding the transferrin saturation <16% [5,6]. Healthy siblings of
proportional contribution of CD to unexplained anemia patients visiting the outpatient department were chosen as
in children are scarce, especially from a country like India controls.The controls consisted of children with normal
where nutritional anemias are very common [2]. Children
diagnosed with CD require major dietary modifications Accompanying Editorial: Pages 23-24.
in addition to the treatment of the nutritional anemia [3].
This study was conducted to assess proportionate
hemoglobin level as per the age (hemoglobin>11 g/dL in
contribution of celiac disease as the underlying causative
12-59 month, >11.5 g/dL in 5-11 years of age, >12 g/dL in
factor of the iron deficiency anemia.
12 years of age) and normocytic normochromic cells.
METHODS Exclusion criteria were: severe acute infection
(pneumonia), chronic diseases (cardiac, renal, hepatic,
This cross-sectional study was conducted in the pediatric
autoimmune disease, immunodefi-ciencies),
outpatient department of a tertiary-care center in Delhi
hematological disorders, chronic gastrointes-tinal
over a period of 18 months in 2013-15. Children between
diseases, already diagnosed celiac disease, bleeding,
the ages of 1 and 12 years with visible pallor as detected on
intake of any cytotoxic agents or radiotherapy in the last 6
physical examination were included in the study if they
weeks.
had moderate-to-severe iron-deficiency anemia (IDA).
Moderate anemia was defined as hemoglobin A detailed history with emphasis on current or past
concentration: 7-9.9 g/dL in children <5 years of age and gastrointestinal symptoms was taken from the children or
8-10.9 g/dL in children of 5 to 12 years of age. Severe their parents. Nutritional status was assessed at the time
anemia was defined as hemoglobin concentration: <7 g/dL of entry into the study. All eligible anemic children
INDIAN PEDIATRICS 31 VOLUME 55__JANUARY 15, 2018
Copyright of Indian Pediatrics 2018
For personal use only. Not for bulk copying or unauthorized posting to listserv/websites
NARANG, et al. CELIAC DISEASE IN ANEMIC CHILDREN
underwent hematological work-up that included the modified Marsh grading [7]. Final diagnosis of CD
hemogram, peripheral blood smear, red blood cell was based on serology and endoscopic duodenal biopsy
indices, serum iron levels, total iron binding capacity, (Grade-3). Children diagnosed as CD were adviced strict
transferrin saturation and serum ferritin levels. Stool gluten-free diet and oral iron supple-mentation for
examination was done on two consecutive days for nutritional anemia. Children with IDA were advised oral
identification of parasitic infestations. Children who were iron preprations and dietary supplementation.
recruited as controls had a complete blood count done
A sample size of 138 children with anemia (and 138
prior to enrolment.
non-anemic controls) was calculated to determine the
We measured IgA-anti tissue transglutaminase (IgA- proportion of celiac disease with an estimated proportion
tTG) by ELISA (Aeskulisa) in all included patients. IgA- of 10% [5] with absolute precision of 0.05 and
tTG levels >18 U/mL were as considered positive as per confidence interval of 95%. Assuming 10% loss to follow
information provided by the manufacturer, levels between up, 152 cases and control were recruited. The statistical
12 and 18 U/mL were considered as equivocal, and levels software SPSS 17 for Windows (Illinois, Chicago) was
<12 U/mL were considered as negative. All children who used for statistical analysis. Fischer’s exact test was
screened positive for celiac disease underwent upper applied to compare the proportion IgA-tTG positive
gastrointestinal (UGI) endoscopy. Four biopsy specimens patients among cases and controls. Ethical clearance was
were taken from the second/first portion of the obtained from Institutional ethical committee of
duodenum, out of which at least one sample was taken University College of Medical Sciences. A written
from the duodenal bulb. Histopathological examination informed consent was obtained from parents of children
of duodenal biopsies was performed by a histopathologist eligible for inclusion, and assent was taken from children
blinded to clinical history, and the result was graded using ≥7 years of age.
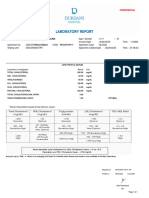
Children with visible pallor Children with normal
screened for low hemoglobin 241 hemoglobin approached 197
Excluded 89
Bleeding history 29
Acute infection 35 Excluded 45
Negative consent 10 Negative consent 32
Thalassemia trait 9 Thalassemia trait 9
Macrocytic anemia 4 Macrocytic anemia 4
Family history of CD 2
Cases (children with moderate Controls (children with normal
to severe IDA) 152 hemoglobin and NCNC RBC) 152
Serum tTG levels 152 Serum tTG levels 152
Positive tTG levels 16 Positive tTG levels 3
Lost to follow-up 1
UGI endoscopy and D2 biopsy 15 UGI endoscopy and D2 biopsy 3
Celiac disease 6 Celiac disease 0
CD: celiac disease; IDA: iron deficiency anemia; NCNC RBC: normocytic normochromic red blood cells; tTG: tissue transglutaminase; UGI: upper
gastro-intestinal; D2: second part of duodenum.
FIG.1 Study flow chart.
INDIAN PEDIATRICS 32 VOLUME 55__JANUARY 15, 2018
Copyright of Indian Pediatrics 2018
For personal use only. Not for bulk copying or unauthorized posting to listserv/websites
NARANG, et al. CELIAC DISEASE IN ANEMIC CHILDREN
TABLE I DEMOGRAPHIC CHARACTERISTICS OF CHILDREN WITH TABLE IICOMPARISON OF ANEMIC PATIENTS WITH OR WITHOUT
AND WITHOUT ANEMIA CELIAC DISEASE
Cases (n=152) Controls (n=152) Celiac disease No celiac disease
(n=6) (n=146)
Gender (M:F) 1.33 1.23
#Age (mo) 41 (32.9) 86.9 (39.0) Wasting 0 16 (11%)
WAZ -1.06 (0.92) -0.93 (0.96) Stunting 0 30 (20.5%)
#HAZ #Hemoglobin (g/dL) 6.4 (1.13) 7.8 (1.80)
-1.41 (0.87) -1.12 (0.95)
WHZ -0.47 (1.36) -0.12 (1.51) *Severe anemia 5 (83.3%) 54 (37%)
MAC (cm) 15.20 (1.63) 16.63 (1.85) Moderate anemia 1 (16.6%) 92 (63%)
*Hemoglobin (g/dL) 7.71 (1.80) 12.2 (0.74) *P=0.02; All value in no (%) except #hemoglobin in mean (SD).
All value in mean (SD); WAZ: weight for age z score; HAZ: height for
age z score; WHZ: weight for height z score; MAC: midarm
circumference. *P=0.001; #P<0.01.
a tertiary-care hospital outpatient setting in Northern India.
Studies in children with iron-deficiency anemia are
RESULTS
limited [1,8,9]. A study by Ertekin, et al. [9] among
The flow of participants in the study is shown in Fig.1. Turkish children had similar results with a mean
We included 152 cases and 152 controls. The non-anemic hemoglobin level significantly lower in IDA patients with
controls were of higher age group as compared to anemic CD than in those without CD [9]. Moreover, those with
cases [mean (SD): 86.9 (39) months vs 41 (32.9) months; severe anemia had higher odds of having CD.
P=0.002] (Table I).
As prevalence of anemia in India children 6 months-
Increased prevalence of IgA-TTG was found among 59 months is 58.4% [2], there is a greater chance of
anemic children, as compared to non-anemic controls (16 missing those children with celiac disease presenting
vs 3; P=0.007). Endoscopy was conducted in 18 children atypically as anemia. Early identification of these
(15 anemic), of which normal villous pattern was seen in subclinical cases in childhood assumes greater
3 controls and 5 with anemia Marsh Grade I and grade importance since these patients are at risk of malignancy
IIIb findings were seen in 6 and 2, respectively of the and mortality in later life and morbidity like the presence
anemic children. Two anemic children had giardiasis. of unsuspected nutritional deficiencies.
After UGI endoscopy and biopsy, six (3.9%) children
The major limitation of this study is that being a
with moderate or severe anemia and none of the control
hospital-based study results obtained in this study might
group were diagnosed as celiac disease (P=0.013).
not be representative of the whole population. The
Among 92 children with moderate anemia, one (1.08%)
sample size was inadequate to find other clinical
patient had celiac disease while among 59 children with
predictors of celiac disease in anemic children. Not doing
severe anemia 5 (8.5%) had celiac disease. There was a
IgA levels to screen for IgA deficiency, non-evaluation of
significant difference between the mean (SD)
occult blood loss in stool, and controls not being age
hemoglobin level between patients with celiac disease
matched are other study limitations. No loss to follow-up
and patients without celiac disease [6.38 (1.13) g/dL vs
and outcome assessment using endoscopy are the
7.77 (1.80) g/dL; P=0.029]. Subgroup analysis between
strengths of the present study.
anemic patients with or without celiac disease is
mentioned in Table II. We conclude that anemic children, especially those
presenting with severe anemia have significantly higher
DISCUSSION
likelihood of having CD. Physicians treating children
This cross-sectional study showed that celiac disease with severe anemia may consider screening them for
accounted for 8.5% and 3.9% of children with severe and celiac disease. We recommend community-based studies
moderate to severe iron deficiency anemia, respectively at to confirm these findings.
WHAT THIS STUDY ADDS?
• Severely anemic patients have higher chances of having associated celiac disease.
INDIAN PEDIATRICS 33 VOLUME 55__JANUARY 15, 2018
Copyright of Indian Pediatrics 2018
For personal use only. Not for bulk copying or unauthorized posting to listserv/websites
NARANG, et al. CELIAC DISEASE IN ANEMIC CHILDREN
Contributors: MN: Study conception and manuscript writing; Health and development; Haemoglobin concentration for
RN: Data collection, analysis and manuscript writing; DS: the Diagnosis of Anaemia and Assessment of Severity.
Study conception, and critical review of manuscript for Geneva, WHO, 2011. (WHO/NMH/NHD/MNM/11.1).
intellectual content; ASP, VM and MK: Study related Available from: http://apps.who.int/iris/bitstream/
procedures (data collection), their interpretation and critical 10665/101179/1/WHO_NMH_NHD_EPG_14.1_eng. pdf.
inputs into manuscript. Accessed December 27, 2016.
Funding: None; Competing interests: None stated. 5. World Health Organization: Serum Ferritin Concentrations
for the Assessment of Iron Status and Iron Deficiency in
REFERENCES Populations. Vitamin and Mineral Nutrition Information
System. Geneva, World Health Organization, 2011.
1. Kavimandan A, Sharma M, Verma AK, Das P, Mishra P, (WHO/NMH/NHD/MNM/11.2). Available from:
Sinha S, et al. Prevalence of celiac disease in nutritional http://www.who.int/vmnis/indicators/serum_ferritin.pdf.
anemia at a tertiary care center. Indian J Gastroenterol. Accessed December 27, 2016.
2013;33:114-8. 6. Bainton DF, Finch CA. The diagnosis of iron deficiency
2. National Family Health Survey-4, 2015-16: India Fact anemia. Am J Med. 1964;37:62-70.
Sheet. Ministry of Health and Family Welfare. Available 7. Marsh MN, Crowe PT. Morphology of the mucosal
from: http://rchiips.org/NFHS/pdf/NFHS4/India.pdf. lesion in gluten sensitivity. Baillieres Clin Gastroenterol.
Accessed April 2, 2017. 1995;9:273-93.
3. Hill ID, Dirks MH, Liptak GS, Colletti RB, Fasano A, 8. Kalayci AG, Kanber Y, Birinci A, Yildiz L, Albayrak D.
Guandalini S, et al. Guideline for the Diagnosis and The prevalence of coeliac disease as detected by screening
Treatment of Celiac Disease in Children: Recommen- in children with iron deficiency anaemia. Acta Paediatr.
dations of the North American Society for Pediatric 2005;94:678-81.
Gastroenterology, Hepatology. J Pediatr Gastroenterol 9. Ertekin V, Tozun MS, Küçük N. The prevalence of celiac
Nutr. 2005;40:1-19. disease in children with iron-deficiency anemia. Turk J
4. World Health Organization: Department of Nutrition for Gastroenterol. 2013;24:334-8.
INDIAN PEDIATRICS 34 VOLUME 55__JANUARY 15, 2018
Copyright of Indian Pediatrics 2018
For personal use only. Not for bulk copying or unauthorized posting to listserv/websites
You might also like
- How To Download Ebook PDF Primary Care of Women 2Nd Edition by Barbara K Hackley Ebook PDF Docx Kindle Full ChapterDocument36 pagesHow To Download Ebook PDF Primary Care of Women 2Nd Edition by Barbara K Hackley Ebook PDF Docx Kindle Full Chaptersteve.books604100% (32)
- Prevalence and Risk Factors of Anemia in Under Five-Year-Old Children in Children's HospitalDocument4 pagesPrevalence and Risk Factors of Anemia in Under Five-Year-Old Children in Children's Hospitalindahsarizahab 28No ratings yet
- Help BasicwoundcareindonesianDocument9 pagesHelp BasicwoundcareindonesianIda Ayu DhitayoniNo ratings yet
- Acquired Platelet Dysfunction With Eosinophilia (APDE)Document4 pagesAcquired Platelet Dysfunction With Eosinophilia (APDE)Rahmat FirdausNo ratings yet
- Ajts 15 160Document6 pagesAjts 15 160Khatidja AllyNo ratings yet
- Manuscript 1Document4 pagesManuscript 1maryNo ratings yet
- Anemia in ChildrenDocument9 pagesAnemia in ChildrenanishaNo ratings yet
- Jurnal AKIDocument7 pagesJurnal AKIAnonymous Vz9teLNo ratings yet
- Celiac Disease With Balanced TranslocationDocument3 pagesCeliac Disease With Balanced TranslocationAdvanced Research PublicationsNo ratings yet
- Toddler's Diarrhea: Is It An Under-Recognized Entity in Developing Countries?Document6 pagesToddler's Diarrhea: Is It An Under-Recognized Entity in Developing Countries?deonardNo ratings yet
- Manuscript 2Document5 pagesManuscript 2maryNo ratings yet
- Kak DyaDocument6 pagesKak DyaNanda AnessaNo ratings yet
- Indeks MentzerDocument5 pagesIndeks MentzerRINNY ARDINA S.ST., M.SiNo ratings yet
- Prevalencia de Anemia en Niños de 6 A 24 Meses de Edad de Tres Centros de Salud de La Ciudad de La PazDocument7 pagesPrevalencia de Anemia en Niños de 6 A 24 Meses de Edad de Tres Centros de Salud de La Ciudad de La PazKarem RamosNo ratings yet
- Iron Def IJPDocument5 pagesIron Def IJPPrahbhjot MalhiNo ratings yet
- Shatha Hussain Ali, Et AlDocument9 pagesShatha Hussain Ali, Et AlJeevaNo ratings yet
- 2006-Intravenous Immunoglobulin in ABO and RH Hemolytic Diseases of NewbornDocument4 pages2006-Intravenous Immunoglobulin in ABO and RH Hemolytic Diseases of Newborn蔡黑面No ratings yet
- 58 123 1 SM PDFDocument5 pages58 123 1 SM PDFNhiyar Indah HasniarNo ratings yet
- 7 Rare Cases in IndiaDocument5 pages7 Rare Cases in IndiaNarendran KumaravelNo ratings yet
- Lower Gastrointestinal Bleeding in Children: Experiences From Referral Center in Southern IranDocument4 pagesLower Gastrointestinal Bleeding in Children: Experiences From Referral Center in Southern IranFernandaNo ratings yet
- Serum Ionic Calcium Levels and Hypocalcemia in DenDocument5 pagesSerum Ionic Calcium Levels and Hypocalcemia in DenJoko Purnomo HNo ratings yet
- Bloody Stool Journal 2Document8 pagesBloody Stool Journal 2dr.herusetiawanNo ratings yet
- Ijpo 5 (1) 6-11Document6 pagesIjpo 5 (1) 6-11Rajesh SahuNo ratings yet
- Serum Zinc Values in Children With Congenital Heart DiseaseDocument6 pagesSerum Zinc Values in Children With Congenital Heart DiseaseTri Novita SariNo ratings yet
- Endocrine Abnormalities in Children With Beta Thalassaemia MajorDocument6 pagesEndocrine Abnormalities in Children With Beta Thalassaemia MajorKrisbiyantoroAriesNo ratings yet
- AnemiaDocument4 pagesAnemiaarlitaNo ratings yet
- Chronic Constipation in A 7-Year-Old Boy: Judy-April Oparaji, MD, RDN, CSP, Theresa Heifert, MDDocument5 pagesChronic Constipation in A 7-Year-Old Boy: Judy-April Oparaji, MD, RDN, CSP, Theresa Heifert, MDbella friscaamaliaNo ratings yet
- Fecal Calprotectin in Celiac Children at Diagnosis and On Gluten-Free Diet - A Pilot StudyDocument2 pagesFecal Calprotectin in Celiac Children at Diagnosis and On Gluten-Free Diet - A Pilot StudyNejc KovačNo ratings yet
- Nutritional Rehabilitation For Children With Congenital Heart Disease With Left To Right ShuntDocument10 pagesNutritional Rehabilitation For Children With Congenital Heart Disease With Left To Right ShuntJiradett Arm KerdsriNo ratings yet
- Nej MoDocument9 pagesNej MoNadia Mrz Mattew MuseNo ratings yet
- Characteristics of Pediatric Patients With Diarrhea in Indonesia: A Laboratory-Based ReportDocument8 pagesCharacteristics of Pediatric Patients With Diarrhea in Indonesia: A Laboratory-Based ReportDrnNo ratings yet
- Clinical, Biochemical, and Histopathology Features of Patients With Glycogenic Hepatopathy 2017Document7 pagesClinical, Biochemical, and Histopathology Features of Patients With Glycogenic Hepatopathy 2017LUIS FRANCISCO GUERRERO MARTÍNEZNo ratings yet
- Iron Deficiency Anemia Among Preschooi Children (2-5) Years in Gaza StripDocument17 pagesIron Deficiency Anemia Among Preschooi Children (2-5) Years in Gaza StripMohammedAAl-HaddadAbo-alaaNo ratings yet
- Iga NephrpathyDocument3 pagesIga NephrpathyKwame AsieduNo ratings yet
- 1 s2.0 S168719792100040X MainDocument4 pages1 s2.0 S168719792100040X MainfelipetheNo ratings yet
- Vitamin D & Osteocalcin Levels in Children With Type 1 DM in Thi - Qar Province South of Iraq 2019Document16 pagesVitamin D & Osteocalcin Levels in Children With Type 1 DM in Thi - Qar Province South of Iraq 2019TJPRC PublicationsNo ratings yet
- Demir 2013Document5 pagesDemir 2013박가영No ratings yet
- FK Concentration in Celiac DiseaseDocument3 pagesFK Concentration in Celiac DiseaseNejc KovačNo ratings yet
- Determinants of Nutritional Anaemia in Children Less Than Five Years AgeDocument6 pagesDeterminants of Nutritional Anaemia in Children Less Than Five Years AgeBaiiqDelaYulianingtyasNo ratings yet
- Anemia Pada Diabetes New OnsetDocument6 pagesAnemia Pada Diabetes New OnsetNurul Kamilah SadliNo ratings yet
- Anemia Pada Diabetes New OnsetDocument6 pagesAnemia Pada Diabetes New OnsetNurul Kamilah SadliNo ratings yet
- Gastroesophageal Reflux Disease (GERD) in ChildrenDocument7 pagesGastroesophageal Reflux Disease (GERD) in ChildrenAndhika DNo ratings yet
- 1833 Manuscript 7430 1 10 20180428Document6 pages1833 Manuscript 7430 1 10 20180428sagarNo ratings yet
- Clinical CourseDocument6 pagesClinical CoursePratistha SatyanegaraNo ratings yet
- Jurnal GEADocument5 pagesJurnal GEARian KurniawanNo ratings yet
- IJP - Volume 5 - Issue 12 - Pages 6189-6194Document6 pagesIJP - Volume 5 - Issue 12 - Pages 6189-6194Yupie Faming JayaNo ratings yet
- Egyptian Pediatric Association Gazette: M.H. Elsamahy, Y.I. Elhenawy, N. AltayebDocument5 pagesEgyptian Pediatric Association Gazette: M.H. Elsamahy, Y.I. Elhenawy, N. Altayebida ayu agung WijayantiNo ratings yet
- Jurnal FixDocument3 pagesJurnal FixasaNo ratings yet
- Jurnal InternationalDocument6 pagesJurnal InternationalLeonal Yudha PermanaNo ratings yet
- Richardson2021 Article L-typeCalciumChannelBlockerUseDocument9 pagesRichardson2021 Article L-typeCalciumChannelBlockerUsetrikusumaNo ratings yet
- Anemia in Pre-School Children-Does Time Change Anything?Document5 pagesAnemia in Pre-School Children-Does Time Change Anything?NZ FreelancersNo ratings yet
- Chronic Kidney Disease in Children and AdolescentsDocument16 pagesChronic Kidney Disease in Children and AdolescentsFernanda SierraNo ratings yet
- Clinical Profile and Outcome in Children of Dengue Hemorrhagic Fever in North IndiaDocument7 pagesClinical Profile and Outcome in Children of Dengue Hemorrhagic Fever in North IndiaAna Rosida SafwanNo ratings yet
- Hyper-Reactive Malarial Splenomegaly: Rare Cause of Pyrexia of Unknown OriginDocument3 pagesHyper-Reactive Malarial Splenomegaly: Rare Cause of Pyrexia of Unknown OriginAshvanee sharmaNo ratings yet
- Jurnal RdsDocument6 pagesJurnal RdsNaman KhalidNo ratings yet
- Autoimmune Hepatitis in Children: Giorgina Mieli-Vergani, MD, PHD, FRCP, FRCPCH, Diego Vergani, MD, PHD, Frcpath, FRCPDocument12 pagesAutoimmune Hepatitis in Children: Giorgina Mieli-Vergani, MD, PHD, FRCP, FRCPCH, Diego Vergani, MD, PHD, Frcpath, FRCPFildzah DheaNo ratings yet
- IJP - Volume 5 - Issue 12 - Pages 6245-6252Document8 pagesIJP - Volume 5 - Issue 12 - Pages 6245-6252Rayhand MubarakhNo ratings yet
- Frequency of Hyponatraemia and Hypokalaemia in Malnourished Children With Acute DiarrhoeaDocument4 pagesFrequency of Hyponatraemia and Hypokalaemia in Malnourished Children With Acute DiarrhoeaRaja Bajak LautNo ratings yet
- A Study On Growth Profiles in Children With Thalassemia Major Between 2-10 Years of Age On Regular Transfusions and Oral Chelation TherapyDocument9 pagesA Study On Growth Profiles in Children With Thalassemia Major Between 2-10 Years of Age On Regular Transfusions and Oral Chelation TherapysagarNo ratings yet
- Naskah JR3Document20 pagesNaskah JR3haekal fauzyNo ratings yet
- Complementary and Alternative Medical Lab Testing Part 5: GastrointestinalFrom EverandComplementary and Alternative Medical Lab Testing Part 5: GastrointestinalNo ratings yet
- OET Practice Reading Test Part A:: The ContinuesDocument8 pagesOET Practice Reading Test Part A:: The ContinuesPrasoon PremrajNo ratings yet
- JatamansiDocument2 pagesJatamansiDinesh Joshi100% (1)
- Ajtj3770052-050224 2662Document1 pageAjtj3770052-050224 2662desilvamnimeshNo ratings yet
- Which Is The Primary Goal of Community Health NursingDocument20 pagesWhich Is The Primary Goal of Community Health NursingKeepItSecretNo ratings yet
- Korelasi Faktor Demografi, Nutrisi Dan Antropometri Terhadap Kejadian Hipertensi Pada Petugas Keamanan Di Universitas Tarumanagara JakartaDocument16 pagesKorelasi Faktor Demografi, Nutrisi Dan Antropometri Terhadap Kejadian Hipertensi Pada Petugas Keamanan Di Universitas Tarumanagara JakartaMery Nurun rNo ratings yet
- Nursing Care Plan FinalDocument9 pagesNursing Care Plan FinalJny SthaNo ratings yet
- BIO02 CO2.3 Sex Linkage and Pedigree AnalysisDocument27 pagesBIO02 CO2.3 Sex Linkage and Pedigree Analysisk marcusNo ratings yet
- Filarial NematodeDocument18 pagesFilarial NematodeHawre NajmaddinNo ratings yet
- Atrial FlutterDocument38 pagesAtrial FlutterLady AngodNo ratings yet
- Conference Paper TitleDocument4 pagesConference Paper Titleshivamsaidane09No ratings yet
- 05 Palmieri-VadalaDocument7 pages05 Palmieri-VadalaSantosNo ratings yet
- College of Nursing: Cebu Normal UniversityDocument3 pagesCollege of Nursing: Cebu Normal UniversityLouie Danielle SegarraNo ratings yet
- Introduction To Evidence-Based Practice: Learning ObjectivesDocument15 pagesIntroduction To Evidence-Based Practice: Learning ObjectivesNicolas VallesNo ratings yet
- Caso 24 2016NEJMcpc1503829Document14 pagesCaso 24 2016NEJMcpc1503829claudia montesNo ratings yet
- PDF Mosquitoes Identification Ecology and Control 3Rd Edition Norbert Becker Ebook Full ChapterDocument40 pagesPDF Mosquitoes Identification Ecology and Control 3Rd Edition Norbert Becker Ebook Full Chapteralbert.doherty404100% (2)
- Blood Glucose MonitoringDocument30 pagesBlood Glucose Monitoringruby cubiona100% (1)
- Why Am I Losing Hair?Document4 pagesWhy Am I Losing Hair?AhsanFayyazNo ratings yet
- Dengue: Denggoy, Dengvaxia, Dengue Ba Sya?Document55 pagesDengue: Denggoy, Dengvaxia, Dengue Ba Sya?KatNo ratings yet
- Case Scenario 2 For StudentsDocument8 pagesCase Scenario 2 For StudentsPrince DetallaNo ratings yet
- Test Bank For Body Structures and Functions 12th Edition ScottDocument9 pagesTest Bank For Body Structures and Functions 12th Edition ScottTonyRamosgbspc100% (32)
- 2 5291964174748882717Document11 pages2 5291964174748882717نشط عقلكNo ratings yet
- Staying Cool in HeatDocument1 pageStaying Cool in HeatJeff Morris100% (1)
- HypocalcemiaDocument6 pagesHypocalcemiaDiana Hazel Delos ReyesNo ratings yet
- Unit 3Document11 pagesUnit 3api-563244553No ratings yet
- LCH 3Document12 pagesLCH 3giant nitaNo ratings yet
- Health 10 LAS Quarter 3Document26 pagesHealth 10 LAS Quarter 3Dennis50% (4)
- Strategies of Reducing Malnutrition by Caregivers Amongst Children 0-5 Years in Opiro CommunityDocument8 pagesStrategies of Reducing Malnutrition by Caregivers Amongst Children 0-5 Years in Opiro CommunityEgbuna ChukwuebukaNo ratings yet
- HOOKWORMSDocument47 pagesHOOKWORMSChipego ChiyaamaNo ratings yet
- Allergic RhinitisDocument27 pagesAllergic Rhinitispaningbatan.kristine.bNo ratings yet