Professional Documents
Culture Documents
1.cardiovascular Investigation, ppt1 (1) - Abcdpdf - PDF - To - PPT
1.cardiovascular Investigation, ppt1 (1) - Abcdpdf - PDF - To - PPT
Uploaded by
dawitOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
1.cardiovascular Investigation, ppt1 (1) - Abcdpdf - PDF - To - PPT
1.cardiovascular Investigation, ppt1 (1) - Abcdpdf - PDF - To - PPT
Uploaded by
dawitCopyright:
Available Formats
BASIC CARDIOVASCULAR
INVESTIGATION
Bruke B. (BPharm, MSc clinical pharmacy, PhD in cardio
therapy, clinical pharmacy) WCU, Ethiopia
4/13/2022 Bruke B.(PhD )
22
4/13/2022 Bruke B.(PhD )
33
4/13/2022 Bruke B.(PhD )
THE HISTORY
isthe cornerstone of a cardiovascular workup
The elements of a comprehensive history
the chief complaint,
present problems,
past medical history,
review of systems,
and social history
Chief complaint : is a short brief statement as to
the reason why the patient seeks medical care (get
to the point)
44
4/13/2022 Bruke B.(PhD )
HPI: The duration, any prior Hx of the same
problem, the severity of the problem, and
whether there are any limitations on the
patient’s daily activities
Character, any types of motion or other things
that / the discomfort, any association with
additional Sy/Sx, and whether the
discomfort is increasing in frequency or
duration 55
4/13/2022 Bruke B.(PhD )
Chest pain : is one of the most important symptoms
you will assess as a practitioner
“Do you have any pain or discomfort in your chest?”
“Is the pain related to exertion?”
“What kinds of activities bring on the pain?”
“How intense is the pain, on a scale of 1 to 10?”
Does it radiate into the neck, shoulder, back, or down
your arm?”
“Are there any associated symptoms like shortness of
breath, sweating, palpitations, or nausea?”
“Does it ever wake you up at night?”
66
“What do you do to make it better?”
4/13/2022 Bruke B.(PhD )
Examples:
Exertional chest pain with radiation to the left
side of the neck and down the left arm in
angina pectoris.
Sharp pain radiating into the back or into
the neck in aortic dissection.
77
4/13/2022 Bruke B.(PhD )
Palpitations: are an unpleasant awareness of the
heartbeat.
Patients use various terms : skipping, racing,
fluttering, pounding, or stopping of the heart
May result from an
irregular heartbeat,
from rapid acceleration or slowing of the heart,
or from increased forcefulness of cardiac contraction
88
4/13/2022 Bruke B.(PhD )
Shortness of breath: is a common patient concern
and may be reported as dyspnea, orthopnea, or
paroxysmal nocturnal dyspnea/PND
o Dyspnea: is an uncomfortable awareness of
breathing that is inappropriate to a given level of
exertion
o Orthopnea is dyspnea that occurs when the patient
is lying down and improves when the patient sits up.
99
4/13/2022 Bruke B.(PhD )
Orthopnea suggests
left ventricular heart failure or mitral stenosis;
it may also accompany obstructive lung disease
o Paroxysmal nocturnal dyspnea/ PND: describes
episodes of sudden dyspnea and orthopnea that
o awaken the patient from sleep,
o usually 1 or 2 hours after going to bed,
o prompting the patient to sit up, stand up, or go to a
window for air.
May be associated wheezing and coughing 10
4/13/2022 Bruke B.(PhD )
PND suggests left ventricular HF or mitral stenosis
and may be mimicked by nocturnal asthma
attacks
Edema refers to the accumulation of excessive fluid
in the interstitial tissue spaces and appears as
swelling.
11
4/13/2022 Bruke B.(PhD )
Family Hx is very important because of the
genetic links involved in many CV diseases
from early myocardial infarction,
strokes,
diabetes,
valvular heart disease,
hypertension and familial hypercholesterolemia
12
4/13/2022 Bruke B.(PhD )
PHYSICAL EXAMINATION
Blood pressure/BP
After letting the patient rest for at least 5
minutes in a quiet setting, choose a correctly sized
cuff and position the patient’s arm at heart level,
either resting on a table if seated or supported
at mid chest level if standing.
Make sure the bladder of the cuff is centered over
the brachial artery
13
4/13/2022 Bruke B.(PhD )
Inflate the cuff about 30 mm Hg above the pressure at
which the radial pulse disappears
As you deflate the cuff, listen first for the sounds of at
least two consecutive heartbeats—these mark the
systolic pressure.
Then listen for the disappearance point of the
heartbeats, which marks the diastolic pressure
14
4/13/2022 Bruke B.(PhD )
The initial part of P/E consists of inspection of the
precordium for normal patterns of rise and fall
and any abnormal markings or shape.
The chest is then palpated for
normal pulses,
thrills (humming vibrations like the throat of a purring
cat),
and heaves (lifting of the chest wall)
Thrills may indicate murmurs
Heaves may indicate enlargement of one of the
heart chambers or an abnormal vessel such as
an aneurysm 15
4/13/2022 Bruke B.(PhD )
HEART RATE
For heart rate, measure the radialpulse using the
pads of your index and middle fingers, or assess the
apical pulse using your stethoscope
The apical pulse (the point of maximum impulse) is
helpful to estimate heart size and rotation.
PMIis usually located in 5th intercostal space in
midsternal line and radiates in an arc of 1 to 2 cm.
Heightened intensity and/or displacement laterally
suggests, Left or right ventricle enlargement,
And reduced intensity may be a sign of fluid overload16
16
or pericardial effusion
4/13/2022 Bruke B.(PhD )
APICAL PULSE
17
4/13/2022 Bruke B.(PhD )
THE CAROTID
PULSE
The carotid pulse is examined for its intensity
and, concurrently with the apical pulse, for
concordance within the cardiac cycle
Decreased pulsations may be caused by
Decreased stroke volume,
Also be due to local factors in the artery such as
atherosclerotic narrowing or occlusion.
18
4/13/2022 Bruke B.(PhD )
CAROTID
PULSE
19
4/13/2022 Bruke B.(PhD )
JUGULAR VENOUS PRESSURE
is usedas an indirect measure of right atrial
pressure
Venous pressure measured at
>3 cm or possibly 4 cm above the sternal angle,
or more than 8 cm or 9 cm in total distance above the
right atrium, is considered elevated above normal
20
4/13/2022 Bruke B.(PhD )
JVP
21
4/13/2022 Bruke B.(PhD )
JVP
Increased pressure suggests
Right sided HF
or, less commonly, constrictive pericarditis, tricuspid
stenosis, or superior vena cava obstruction
22
4/13/2022 Bruke B.(PhD )
HEART SOUNDS
Auscultation with a stethoscope is used to
characterize heart sounds.
The normal heart sounds
S1 :first heart sound—closure of the mitral and
tricuspid valves and
S2: second heart sound—aortic and pulmonic
valves.
23
4/13/2022 Bruke B.(PhD )
SOUNDS…
S2 becomes split during inspiration because of delayed
closure of the pulmonic valve
prolongation of right ventricle systole secondary to an
increase in venous return
24
4/13/2022 Bruke B.(PhD )
SOUNDS…NORMAL
S1 has two components, an earlier mitral and a
later tricuspid sound.
The softer tricuspid component is heard best at
the lower left sternal border, and it is here that
you may hear a split S1
25
4/13/2022 Bruke B.(PhD )
SOUNDS…ABNORMAL
S3 :thirdheart sound; and S4: fourth heart sound;
and murmurs, are not considered normal but
provide important diagnostic information
High-pitched sounds :
S1 and S2, murmurs of aortic and mitral regurgitation,
and pericardial friction rubs are best heard with the
diaphragm.
Low-pitched sounds :
The bell is preferred for low-pitched sounds such as S3
and S4.
26
4/13/2022 Bruke B.(PhD )
SOUNDS ….S3
The S3 heart sound, or ventricular gallop, is an
abnormal low pitched sound usually heard at the
apex of the heart
Caused by rapid filling and stretching of the left
ventricle when the left ventricle is somewhat
noncompliant.
This heart sound is characteristic of
volume overloading, as in CHF(especially left-sided HF),
tricuspid or mitral valve insufficiency,
and atrial and/or ventricular septal defects
A physiologic S3 is heard commonly in children and
may persist into young adulthood 27
4/13/2022 Bruke B.(PhD )
SOUNDS….. S4
The S4 diastolic sound is a dull, low-pitched
postsystolic atrial gallop (rapid blood flow)
usually caused by reduced ventricular compliance
Present in conditions such as
aortic stenosis,
hypertension,
hypertrophic cardiomyopathies, and
coronary artery disease
28
4/13/2022 Bruke B.(PhD )
29
4/13/2022 Bruke B.(PhD )
HEART MURMURS
Murmurs are auditory vibrations heard on
auscultation, and they occur because of turbulent
blood flow within the heart chambers or
through the valves.
Timing. First decide if you are hearing a systolic
murmur, falling between S1 and S2, or a diastolic
murmur, falling between S2 and S1
30
4/13/2022 Bruke B.(PhD )
MURMURS….
Systolic murmurs are usually midsystolic or
pansystolic
A midsystolic murmur begins after S1 and stops
before S2.
Brief gaps are audible between the murmur and the
heart sounds.
A pansystolic
(holosystolic) murmur starts with S1
and stops at S2,
without a gap between murmur and heart sounds.
31
4/13/2022 Bruke B.(PhD )
MURMURS….
Murmurs generally & diastolic murmurs usually
indicate valvular heart disease
Midsystolic
murmurs most often are related to
blood flow across the semilunar (aortic and
pulmonic) valves
32
4/13/2022 Bruke B.(PhD )
33
4/13/2022 Bruke B.(PhD )
ELECTROCARDIOGRAM
The electrocardiogram (ECG or EKG) is a graphic
recording of electric potentials generated by the
heart.
records only the depolarization (stimulation) and
repolarization (recovery) potentials generated by
the atrial and ventricular myocardium
The signals are detected by means of metal
electrodes attached to the extremities and chest
wall and are then amplified and recorded by the
electrocardiograph
34
4/13/2022 Bruke B.(PhD )
ECG USE/INDICATION
ECG leads actually display the instantaneous
differences in potential between these electrodes.
ECG Detects
Arrhythmias,
Conduction disturbances, and myocardial ischemia,
Other findings related to life-threatening metabolic
disturbances (e.g., hyperkalemia)
Or increased susceptibility to sudden cardiac death
(e.g., QT prolongation syndromes).
35
4/13/2022 Bruke B.(PhD )
ECG LEADS
The standard external 12-lead ECG uses two sets of
leads:
limb and chest
Limb lead nomenclature is as follows: lead I, right
arm/left arm; lead II, right arm/left leg; lead III, left
arm/left leg.
The augmented limb leads aVR, aVL, and aVF.
Unipolar chest leads are positioned across the chest
and labeled V1 to V6.
36
4/13/2022 Bruke B.(PhD )
ECG LEADS…
V1is positioned slightly to the right of the midline
V6 is positioned in the left midaxillary line
Leads aVR and V1 are considered right sided leads
so they appear inverted
leads aVL, I, II, V5 and V6 are left-sided leads
so they appear upright on the ECG
37
4/13/2022 Bruke B.(PhD )
ECG LEADS….
Leads II, III, and aVF are inferior leads.
Leads V1 to V4 are anterior wall leads
lead I = left arm – right arm voltages,
lead II = left leg – right arm, and
lead III = left leg – left arm.
aVR = right arm, aVL = left arm, and aVF = left leg
(foot).
38
4/13/2022 Bruke B.(PhD )
ECG PAPER RECORD
Recording of the ECG has several standard
features.
The paper is divided into squares of 1 mm
Each 10 mm (10 small boxes) is equivalent to 1 mV.
Paper speed is 25 mm per second.
Each small box on the tracing paper equals 0.04
second
and each big box is 0.2 second.
39
4/13/2022 Bruke B.(PhD )
ECG READING
The ECG pattern is named alphabetically and is read
from left to right, beginning with the P wave.
P Wave
Electrical activation (depolarization) of the right
and then the left atrium as a result of discharge from
the SA nodes causes an upward or –tve deflection in
lead II called the P wave
40
4/13/2022 Bruke B.(PhD )
Basic ECG
waveforms and
intervals. Not
shown is the R-R
interval, the time
between consecutive
QRS complexes
41
4/13/2022 Bruke B.(PhD )
ECG READING….
The normal duration of P wave is up to 0.12 second,
Amplitude of 0.25 mV (i.e., 2.5 small boxes).
Since this vector points toward the positive pole of lead
II and toward the negative pole of lead aVR,
The normal P wave will be positive in lead II and negative
in lead aVR.
Activation of the atria from an ectopic pacemaker in
the lower part of either atrium or in the AV junction
region may produce retrograde P waves (negative in
lead II, positive in lead aVR)
42
4/13/2022 Bruke B.(PhD )
ECG READING….
The PR segment is created by passage of the
impulse through the AV node and the bundle of His
and its branches,
Measures the duration of effective depolarization
has a duration of 0.12 to 0.21 second
QRS Complex
primarily traces the electrical depolarization of the
ventricles.
Initially, there is a negative deflection, the Q wave,
followed by a positive deflection, the R wave, and
finally a negative deflection, the S wave
43
4/13/2022 Bruke B.(PhD )
ECG READING….
ST segment
is a plateau phase following the QRS complex
which extends from the end of the QRS complex (
the J point) to the beginning of the T wave
is normally on or slightly above the baseline.
Configuration changes, convexity upward or
downward, identify the presence of myocardial
ischemia.
Myocardial infarction (MI) is classified based on
this segment as ST elevated (STEMI) and non ST
elevated MI (NSTMI) 44
4/13/2022 Bruke B.(PhD )
ECG READING….
The QT interval
is measured from the start of the QRS complex to
the end of the T wave.
varies with heart rate and is corrected (QTc) for
heart rates greater than 60 beats per minute.
The normal QTc is less than 0.42 second in men
and 0.43 second in women.
Indicator of prolongation of effective refractory
period for example secondary to slow AV
conduction….Used to characterize TdP 45
4/13/2022 Bruke B.(PhD )
ECG READING….
T Wave
Repolarization of the ventricle
Normally proceed in the reverse direction from
depolarization (i.e., from ventricular epicardium to
endocardium).
46
4/13/2022 Bruke B.(PhD )
NORMAL ECG READING
Normal electrocardiogram from a healthy subject. Sinus rhythm is present
with a heart rate of 75 beats per minute. PR interval is 0.16 s; QRS interval
(duration) is 0.08 s; QT interval is 0.36 s; QTc is 0.40 s; the mean QRS axis is about
+70°. The precordial leads show normal R-wave progression with the transition zone
(R wave = S wave) in lead V3
47
4/13/2022 Bruke B.(PhD )
ECHOCARDIOGRAM
The echocardiogram (ECHO) is the use of
ultrasound to visualize anatomic structures,
such as the valves, within the heart and to
describe wall motion
the procedure of choice in the Dx and evaluation of
valvular dysfunction (aortic and mitral stenosis and
regurgitation and endocarditis),
wall motion abnormalities associated with ischemia,
and congenital abnormalities, such as ventricular or
atrial septal defects
48
4/13/2022 Bruke B.(PhD )
ECHO…
Images obtained from ECHO are used to
estimate
chamber wall thickness and
left ventricle ejection fraction,
assess ventricular function, a
nd detect abnormalities of the pericardium such
as effusions or thickening
49
4/13/2022 Bruke B.(PhD )
CARDIAC ENZYMES AND HORMONES
BNP >100 pg/mL (>29 pmol/L)
Important to screen HF and to monitor response to treatment
CK-MB: rises with in 4-8 hrs & returns to normal by 48-
72 hrs
◦ CK-MB 0–12 units/L
cTnT & cTnI: rises with in 2-4 hrs but remains elevated
for 7-10 days after AMI.
◦ cTnI <0.03 ng/mL; cTnI >2.0 suggests acute myocardial
injury.
Troponin is specific than CK-MB for myocardial
damage, elevated sooner and remains elevated longer
than CK-MB.
CK-MB & cTn are used in the diagnosis of MI, but cTn is
more specific and recommended than CK-MB
50
4/13/2022 Bruke B.(PhD )
You might also like
- Test Bank For Pathophysiology 6th Edition Jacquelyn L BanasikDocument3 pagesTest Bank For Pathophysiology 6th Edition Jacquelyn L BanasikKenneth Maestas100% (31)
- Medical Nutrition Therapy A Case Study Approach 5th Edition Nelms Solutions ManualDocument8 pagesMedical Nutrition Therapy A Case Study Approach 5th Edition Nelms Solutions Manualsophiechaurfqnz100% (35)
- Medicine in Brief: Name the Disease in Haiku, Tanka and ArtFrom EverandMedicine in Brief: Name the Disease in Haiku, Tanka and ArtRating: 5 out of 5 stars5/5 (1)
- Figure. Sample Review of Systems (ROS) Format From The Pantex ProgramDocument1 pageFigure. Sample Review of Systems (ROS) Format From The Pantex ProgramTimothy TurscakNo ratings yet
- Human Biology Practice Exam Questions 2020 PDFDocument2 pagesHuman Biology Practice Exam Questions 2020 PDFKage InuNo ratings yet
- Module 16 18Document3 pagesModule 16 18Mitch TorniadoNo ratings yet
- Pericardial EffusionDocument26 pagesPericardial EffusionjsenocNo ratings yet
- Straight Back Syndrome: Brit. Heart 614Document6 pagesStraight Back Syndrome: Brit. Heart 614SaZa KarrarNo ratings yet
- Tuberculous Pericardial EffusionDocument6 pagesTuberculous Pericardial EffusionLink BuiNo ratings yet
- Cardiac SoundsDocument5 pagesCardiac SoundsLaura Fonnegra MendezNo ratings yet
- Cardiothoraxic and Vascular ExaminationDocument4 pagesCardiothoraxic and Vascular ExaminationPreetha PANo ratings yet
- Pericarditis HeartDocument8 pagesPericarditis HeartjosefamdNo ratings yet
- This Study Resource Was: (Total 20 Points)Document9 pagesThis Study Resource Was: (Total 20 Points)andreaaaaamor28No ratings yet
- PARA107 Case StudyDocument6 pagesPARA107 Case StudySiobhan RiceNo ratings yet
- Cardiac Tamponade, Also Known As Pericardial Tamponade, Is AnDocument7 pagesCardiac Tamponade, Also Known As Pericardial Tamponade, Is AnSimran Josan100% (1)
- Cardio 2Document2 pagesCardio 2Erika De JesusNo ratings yet
- Sudden Death Due To Lethal Strangulation of Heart by Congenital Partial PericardiumDocument4 pagesSudden Death Due To Lethal Strangulation of Heart by Congenital Partial PericardiumwahyuekamaulyaniNo ratings yet
- Cardiology and Resuscitation-Cardiac TamponadeDocument7 pagesCardiology and Resuscitation-Cardiac Tamponadefaisal alharbiNo ratings yet
- AUSCULTACIÓN BonaguraDocument6 pagesAUSCULTACIÓN BonaguraMicaPastineNo ratings yet
- PericarditisDocument11 pagesPericarditisnathan asfahaNo ratings yet
- Pericardial DiseaseDocument11 pagesPericardial Diseasenathan asfahaNo ratings yet
- A Mistake That Has Hurt No One: Sinus MistakusDocument4 pagesA Mistake That Has Hurt No One: Sinus MistakusasclepiuspdfsNo ratings yet
- Myocardial InfarctionDocument7 pagesMyocardial InfarctionalmiasevNo ratings yet
- CHF Case PresentationDocument42 pagesCHF Case PresentationAmanuel LemiNo ratings yet
- Stenosis Pulmonal.Document21 pagesStenosis Pulmonal.syelNo ratings yet
- 07 - 01 - Assessment of Cardiovascular SystemDocument55 pages07 - 01 - Assessment of Cardiovascular SystemSalman Habeeb50% (2)
- Heart SoundDocument15 pagesHeart SoundLilian EdeniNo ratings yet
- Lecturio Cardiovascular Physical ExaminationDocument10 pagesLecturio Cardiovascular Physical ExaminationPranjali WeladiNo ratings yet
- Cardiovascular Assessment-1Document60 pagesCardiovascular Assessment-1M Razzaq100% (1)
- Cardiovascular Notes - Paediatrics ExaminationDocument5 pagesCardiovascular Notes - Paediatrics ExaminationPraveenNo ratings yet
- Bulletin 5Document5 pagesBulletin 5Resya I. NoerNo ratings yet
- The Diagnosis and Treatment of Pulmonary Valve SteDocument6 pagesThe Diagnosis and Treatment of Pulmonary Valve SteNiarti Ulan SariNo ratings yet
- Diagnosing Chest Pain Diagnosing Chest Pain: HistoryDocument4 pagesDiagnosing Chest Pain Diagnosing Chest Pain: HistorySuhaib Bin SinanNo ratings yet
- Cardiacassessmentppt 170323092148Document48 pagesCardiacassessmentppt 170323092148sasNo ratings yet
- Cardiac TamponadeDocument6 pagesCardiac TamponadeVicky XieNo ratings yet
- Coronary Artery Disease ReportDocument15 pagesCoronary Artery Disease ReportZosmita Shane GalgaoNo ratings yet
- HP Apr04 CardiacDocument0 pagesHP Apr04 CardiacdiapalupiNo ratings yet
- CardioDocument10 pagesCardioMar OrdanzaNo ratings yet
- Acute Pericarditis - Clinical Presentation and Diagnosis - UpToDateDocument37 pagesAcute Pericarditis - Clinical Presentation and Diagnosis - UpToDatemayteveronica1000No ratings yet
- PericarditisDocument11 pagesPericarditisjosefamdNo ratings yet
- Cardio Update: Functional MurmursDocument3 pagesCardio Update: Functional MurmursResya I. NoerNo ratings yet
- Preceptor: Letkol (CKM) Dr. Prihati Pujowaskito, Sp. JP (K), MMRSDocument31 pagesPreceptor: Letkol (CKM) Dr. Prihati Pujowaskito, Sp. JP (K), MMRSJuwita Valen RamadhanniaNo ratings yet
- What Is The Diagnosis and Management of Cardiac Tamponade?: by Kandan ViswalingamDocument11 pagesWhat Is The Diagnosis and Management of Cardiac Tamponade?: by Kandan ViswalingamFairuz Az ZabiedahNo ratings yet
- 1 4927329208029413644 PDFDocument578 pages1 4927329208029413644 PDFWaseem UllahNo ratings yet
- BECK's Triad (3D) : PneumothoraxDocument20 pagesBECK's Triad (3D) : PneumothoraxMichael WonggokusumaNo ratings yet
- Aneurysma AortDocument22 pagesAneurysma Aortaristya_tyaNo ratings yet
- CVS Ass'tDocument49 pagesCVS Ass'tbirkeabsaltNo ratings yet
- PX FISIK Tubuh ManusiaDocument59 pagesPX FISIK Tubuh ManusiaSheila Jessica AndavaniaNo ratings yet
- Cardiovascular Assessment (1) - StudentsDocument70 pagesCardiovascular Assessment (1) - Studentsraima ayazNo ratings yet
- CPR, EolcDocument36 pagesCPR, Eolcjinshajoseph05No ratings yet
- Murmur EvaluationDocument4 pagesMurmur EvaluationManjunath GeminiNo ratings yet
- Anatomy Review Block 1Document32 pagesAnatomy Review Block 1ngNo ratings yet
- Hiatalherniaasarare 2Document8 pagesHiatalherniaasarare 2Fernando Nagore AnconaNo ratings yet
- Congestive Heart Failure: Dr. Asif WazirDocument21 pagesCongestive Heart Failure: Dr. Asif WazirHillary BushnellNo ratings yet
- LWW BATES 10 Cardiovascular System Transcript FINALDocument11 pagesLWW BATES 10 Cardiovascular System Transcript FINALShivamNo ratings yet
- Coronary Artery Disease Case FileDocument2 pagesCoronary Artery Disease Case Filehttps://medical-phd.blogspot.comNo ratings yet
- Cardiovascular AssessmentDocument73 pagesCardiovascular AssessmentmatthewsarfrazbhattiNo ratings yet
- Tetralogyof FallotDocument43 pagesTetralogyof FallotAlyssa Marie100% (8)
- Cardio AuscultationDocument19 pagesCardio AuscultationshadabNo ratings yet
- 16 Syndr Cardiovas SystDocument11 pages16 Syndr Cardiovas Systjqpwzcg8xrNo ratings yet
- MurmursDocument10 pagesMurmursAlina KievskyNo ratings yet
- Research Paper On Heart MurmurDocument4 pagesResearch Paper On Heart Murmurnodahydomut2100% (1)
- MK Final PaperworkDocument15 pagesMK Final Paperworkapi-727427971No ratings yet
- Cardiac-Exam 08 July Article 9Document5 pagesCardiac-Exam 08 July Article 9AlexNo ratings yet
- Stroke: Bruke B. (Bpharm, MSC Clinical Pharmacy, PHD in Cardio Therapy, Clinical Pharmacy) Wcu, EthiopiaDocument50 pagesStroke: Bruke B. (Bpharm, MSC Clinical Pharmacy, PHD in Cardio Therapy, Clinical Pharmacy) Wcu, EthiopiadawitNo ratings yet
- Cardiac ArrhythmiasDocument100 pagesCardiac ArrhythmiasdawitNo ratings yet
- Integrated Therapeutics Iii Credit 4Hrs/Week: Instructor: Tamrat Legesse (B.Pharm, MSC in Clinical Pharmacy)Document145 pagesIntegrated Therapeutics Iii Credit 4Hrs/Week: Instructor: Tamrat Legesse (B.Pharm, MSC in Clinical Pharmacy)dawitNo ratings yet
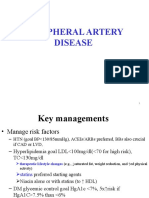
- PAD Handout 4thDocument27 pagesPAD Handout 4thdawitNo ratings yet
- Summary of ECG AbnormalitiesDocument7 pagesSummary of ECG AbnormalitiesKarin AdraiNo ratings yet
- Set-2s - Medical Selection Test Paper - 2024-2025 - Final (Medical - English)Document12 pagesSet-2s - Medical Selection Test Paper - 2024-2025 - Final (Medical - English)kkomalyadav06No ratings yet
- Andocor Cannula Cataloog 2015 PDFDocument37 pagesAndocor Cannula Cataloog 2015 PDFAhmadNo ratings yet
- Topik 4. Reading Intensive Care UnitDocument18 pagesTopik 4. Reading Intensive Care UnitioakasNo ratings yet
- Echocardiography in Hemodynamic MonitoringDocument5 pagesEchocardiography in Hemodynamic MonitoringDr.Biswajit jenaNo ratings yet
- Teaching Unit Circulatory System AICLEDocument9 pagesTeaching Unit Circulatory System AICLEJuan RuizNo ratings yet
- Classroom of The Elite - Year 2 Vol 3Document376 pagesClassroom of The Elite - Year 2 Vol 3selavi848484No ratings yet
- Perubahan Bio, Spiritual Dan Kultural Yang Lazim Terjadi Pada - Ger - Mrs Wanti - SMT Genap - March2019Document15 pagesPerubahan Bio, Spiritual Dan Kultural Yang Lazim Terjadi Pada - Ger - Mrs Wanti - SMT Genap - March2019Cahya SupriatnaNo ratings yet
- MTP 3 45-4 15hDocument15 pagesMTP 3 45-4 15hRohit Velury100% (1)
- Physiological Characteristics of NewbornDocument11 pagesPhysiological Characteristics of Newbornbhawna67% (3)
- Circulation and Blood Igcse BiologyDocument73 pagesCirculation and Blood Igcse BiologyEllie HousenNo ratings yet
- Hemodynamic MonitoringDocument25 pagesHemodynamic MonitoringMichelle Chu100% (2)
- Executive Health Check Up Package - RSPI - Pondok Indah - 2023Document20 pagesExecutive Health Check Up Package - RSPI - Pondok Indah - 2023stephanymelody123No ratings yet
- Muthia-Ahmad Basic Cardiac ElectrophysiologyDocument53 pagesMuthia-Ahmad Basic Cardiac ElectrophysiologyFikriYTNo ratings yet
- Drug StudyDocument17 pagesDrug StudyJoan RabeNo ratings yet
- Lesson Plan HeartDocument18 pagesLesson Plan HeartLoma Waghmare (Jadhav)No ratings yet
- Materi 3 - WS Exercise Stress TestDocument22 pagesMateri 3 - WS Exercise Stress TestMaria ulfahNo ratings yet
- PEDIA - TachypneaDocument12 pagesPEDIA - TachypneaAlvin Germo PasuquinNo ratings yet
- Datascope System 98xtDocument68 pagesDatascope System 98xtTiago DiasNo ratings yet
- Lab 23Document3 pagesLab 23Tyrese JamesNo ratings yet
- Mechanical Heart Valve vs. Bioprosthetic ValveDocument55 pagesMechanical Heart Valve vs. Bioprosthetic ValvePUSHPITHA PERERANo ratings yet
- PXD Bio Pyramid Long AnalisysDocument61 pagesPXD Bio Pyramid Long AnalisyspionirsamtimsedicimNo ratings yet
- Ventricular Assist Devices: K. Nirmala SSN College of EngineeringDocument40 pagesVentricular Assist Devices: K. Nirmala SSN College of EngineeringNivetha RavikumarNo ratings yet
- A Pictorial Guide For The Second Trimester Ultrasound: EducationDocument16 pagesA Pictorial Guide For The Second Trimester Ultrasound: EducationSultan AlexandruNo ratings yet
- Ocana, Carcar City, Cebu S.Y. 2017-2018 Physical Education and Health 10 First Periodical Test ExaminationDocument3 pagesOcana, Carcar City, Cebu S.Y. 2017-2018 Physical Education and Health 10 First Periodical Test ExaminationCloue Faye I. BasalloNo ratings yet
- Coronary Angiography and Left VentriculographyDocument2 pagesCoronary Angiography and Left Ventriculographyrrpandey4854No ratings yet