Professional Documents
Culture Documents
2 Pulmonary System (FINAL)
2 Pulmonary System (FINAL)
Uploaded by
kath-kathOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
2 Pulmonary System (FINAL)
2 Pulmonary System (FINAL)
Uploaded by
kath-kathCopyright:
Available Formats
Pulmonary System I
Functions
Ventilation: act of moving air in and out of the lungs (boyle’s law)
Perfusion: pulmonary blood flow
o Greatest perfusion base of the lungs because of gravity
o Normal V/Q ratio: 0.8 (ventilation: V and Perfusion: Q)
𝐹𝐸𝑉1 𝐹𝑜𝑟𝑐𝑒𝑑 𝐸𝑥𝑝𝑖𝑟𝑎𝑡𝑜𝑟𝑦 𝑉𝑜𝑙𝑢𝑚𝑒 𝑖𝑛 1 𝑠𝑒𝑐 𝐴𝑙𝑣𝑒𝑜𝑙𝑎𝑟 𝑉𝑒𝑛𝑡𝑖𝑙𝑎𝑡𝑖𝑜𝑛
= =
𝐹𝑉𝐶 𝐹𝑜𝑟𝑐𝑒𝑑 𝑉𝑖𝑡𝑎𝑙 𝐶𝑎𝑝𝑎𝑐𝑖𝑡𝑦 𝑃𝑢𝑙𝑚𝑜𝑛𝑎𝑟𝑦 𝐵𝑙𝑜𝑜𝑑 𝐹𝑙𝑜𝑤 (𝑎𝑘𝑎 𝐶𝑎𝑟𝑑𝑖𝑎𝑐 𝑂𝑢𝑡𝑝𝑢𝑡)
4𝐿/𝑚𝑖𝑛
= = 0.8
5𝐿/𝑚𝑖𝑛
Respiration: gaseous exchange
o 2 types
External Respiration: between alveoli and capillaries
Internal Respiration: between tissues and capillaries
o Arteries (O2 blood) “Ar” = Red; A-A - “Arteries Away”
o Veins (Un-O2 blood) “Vlu” = Blue; V-V – Veins Valik
Transport of O2 and CO2
Diffusion of O2 and CO2
o From higher to lower concentration
I. Upper Respiratory Tract
1. Nose (Nasal Cavity)
a. Large mucosal surface area
b. Function: filters and warms air, humidifies air
c. Vibrissae: hair in nose, filters air
2. Pharynx (Throat)
a. Three types:
i. Naso
1. (same fxn as the nose),
ii. Oro, laryngo
1. (conduits of air)
b. Respiratory & digestive system
3. Larynx (Voice Box)
a. Function: voice or sound production, ensures that air will pass through the trachea
b. Cartilages (9)
i. Thyroid (1)
ii. Cricoid (1)
iii. Arytenoid (2)
iv. Corniculate (2)
v. Cuneiform (2)
vi. Epiglottis (1)
1. Has sphincter function “Guardian of the airways”
II. Lower Respiratory Tract (LRT)
Tracheobronchial Tree (23 Generations)
Gold Rank Intensive Review Baguio Batch 2017
Pulmonary System: Anatomy, Physiology, Conditions, Rehabilitation
Conducting Zone 1. Trachea (windpipe)
2. Main Bronchi
(+) passageway of air 3. Lobar Bronchi
(-) gas exchange 4. Segmental Bronchi
5. Terminal Bronchioles
Respiratory Zone 6. Respiratory Bronchioles
aka Acinus: Functional unit 7. Alveolar ducts
of the Lungs 8. Alveolar sacs
9. Alveoli (Structural unit
(+) Passageway
of the lungs)
(+) gas exchange
10. Capillaries
MC Site of Intubation: Trachea
Emergency Site of Intubation: Pharynx
2 Zones
o Conducting Zone: only passageway, no gas exchange
o Respiratory Zone: (+) gas exchange
Functional Unit: acinus
Structural Unit: alveoli
(R) Main Bronchus: Common Area for Large Aspirated Objects
o Shorter, Wider, More Vertical in Orientation
(L) Main Bronchus
o Narrower, larger, more horizontal
Common Area for Small Aspirated Objects: Lobar Bronchi
III. Lungs
RIGHT LUNG (3) LEFT LUNG (2)
3 Lobes 2 Lobes & Lingula
Horizontal Oblique Fissures Oblique Fissure
Upper, lower
Upper, Middle, Lower
Lingula: tongue shaped upper left lobe
Layers of the Lung
1. Parietal Pleura (Outermost)
a. Membrane covering the thoracic wall
b. Sensitive to Pain
Gold Rank Intensive Review Baguio Batch 2017
Pulmonary System: Anatomy, Physiology, Conditions, Rehabilitation
2. Visceral Pleura (Innermost)
a. Membrane covering the lungs and its fissures
b. Sensitive to stretch
3. Pleural Space (between the Pleura)
a. Pressure: -4 mmHg
b. + pressure: gunshot wound, pneumothorax
c. Contains Pleural Fluid
i. Lubricates the pleurae
ii. Shock absorber
Cells in the Lungs
Types I Cells/Pneumocytes: Flat cells lining the alveoli
Type II Cells/Pneumocytes: synthesizes “Surfactant”
o Reduces the surface tension of lungs to prevent atelectasis (lung collapse)
o (-) Surfactant RDS (Respiratory Distress Syndrome) or Hyaline Membrane Disease
*Hering-Breur Reflex (bronchus, bronchioles)
o A stretch/inflation reflex that prevents over inflation of the lungs
IV. Thorax/Thoracic Cage/Rib Cage
A. Boundaries
o Anterior: Sternum “AS”
o Posterior: Thoracic Cage “PTC”
o Lateral: Ribs (12 pairs)
True ribs (ribs 1-7; connected to sternum by costal cartilages)
False Ribs (ribs 8-10; articulates 7th rib with costal cartilages)
Floating Ribs (ribs 11-12; articulates no rib; Rib 11 = T11, Rib 12 = T12)
o Superior: Thoracic Outlet
o Inferior: Diaphragm Muscles
B. Thoracic Cage Mechanisms
o Pump-Handle motion: between sternum & ribs 1-6 (↑ A/P Diameter)
o Bucket-Handle Motion: between ribs 7-10 (↑ Lateral Diameter)
o Caliper Motion: between ribs 8-12 (↑ ICS)
o Piston Action: Diaphragm Muscle (Dome Shaped muscle, moves downward during inspiration, upward
during expiration)
V. Muscles of Respiration [February Board Exam Questions]
I. Relaxed Inspiration
a. Diaphragm Muscle (Primary Muscle of respiration)
b. External Intercostals: ↑ intercostal space, between Rib 1, 2, 3
II. Forced Inspiration
S CM
U pper Trapezius
P ectoralis Major & Minor
A nterior, Middle, Posterior Scalenes (AMS)
S erratus Anterior, Serratus Posterior Superior (APS)
III. Relaxed Expiration
a. No muscle involved d/t elastic recoil of lungs and thorax
IV. Forced Expiration (eg. Coughing)
A bdominals
S erratus Posterior Inferior
I nternal Intercostals (↓ intercostal space)
Gold Rank Intensive Review Baguio Batch 2017
Pulmonary System: Anatomy, Physiology, Conditions, Rehabilitation
VI. Controls of Respiration
Pons and Medulla Oblongata (PM) – Controls of Respiration
Medulla Oblongata (MO) – Automatic Respiratory Center
I. Dorsal Respiratory Group (DRG)
a. Location: Dorsal Medulla (Nucleus Tractus Solitarius)
b. Function: Inspiration (DIN)
c. Inspiratory Ramp signal: 2 sec on, 3 sec off
II. Ventral Respiratory Group (VRG)
a. Location: Ventrolateral Medulla (Nucleus Ambiguus, Retro-ambiguus)
b. Function: Expiration (VEX) & Inspiration
III. Pneumotaxic Center
a. Location: Upper Pons (Nucleus Parabrachialis)
b. Function: limits inspiration by “switching-off” the inspiration ramp signal; controls the rate and depth of
breathing
c. Respiratory Rate: Adult 12-20 cpm
IV. Apneustic Center
a. Location: Lower pons (PULA: Pneumotaxic Upper, Lower Apneustic)
b. Function: prevents “switching-off” the Inspiratory Ramp Signal
V. Chemoreceptors
a. Central
i. Location: Ventral Medulla
ii. Stimulus: ↑ hydrogen ions, results in hyperventilation
b. Peripheral
i. Location: Carotid and Aortic bodies
ii. Stimulus: ↓ PaCO2, ↑PaCO2, Acidosis (↓ pH)
iii. Board Exam: 1st choice AOTA, 2nd Choice↓ PaO2, 3rd Choice ↑PaCO2, 4th choice Acidosis (↓ pH)
VII. Arterial Blood Gas (ABG)
pH 7.35 – 7.45
PaCO2 35-45 mmHg
HCO3 22-26 mEq/L
PaO2 80-100 mmHg
SaO2 95-100%
pH Relations (Sir Lester’s Way)
A. pH inversely related to PaCO2 (Respiratory [lungs])
o Alkalosis ↑ pH = ↓ PaCO2
o Acidosis ↓ pH = ↑ PaCO2
B. pH directly related to HCO3 (Metabolic [kidneys])
o Alkalosis ↑ pH = ↑ HCO3
o Acidosis ↓ pH = ↓ HCO3
Uncompensated Abnormal pH One Gas is Normal
Resp. Alkalosis ↑ ↓ N
Resp. Acidosis ↓ ↑ N
Metab. Alkalosis ↑ N ↑
Metab. Acidosis ↓ N ↓
Partially Compensated All Are Abnormal
Resp. Alkalosis ↑ ↓ *RC ↓
Resp. Acidosis ↓ ↑ *RC ↑
Metab. Alkalosis ↑ ↑ ↑ *RC
Metab. Acidosis ↓ ↓ ↓ *RC
Gold Rank Intensive Review Baguio Batch 2017
Pulmonary System: Anatomy, Physiology, Conditions, Rehabilitation
Fully Compensated Normal pH Abnormal Gases
Resp. Alkalosis N ↓ ↓
Resp. Acidosis N ↑ ↑
Metab. Alkalosis N ↑ ↑
Metab. Acidosis N ↓ ↓
Normal pH = 7.40
RC = Root Cause (typically higher value/lowest value)
Signs and Symptoms
Condition Signs/Symptoms Abbrev Caused By
Resp. Dizziness, Early Tetany, Numbness, Tingling,
DENTS Hyperventilation
Alkalosis Syncope
Resp. Early: Headache, Anxiety, Restlessness, Dyspnea HARDy
Hypoventilation
Acidosis Late: Disorientation (PBEQ), Somnolence, Coma DiSC
Metab. Weakness, Early Tetany, Mental Dullness, ↑ W-E-Men-
Vomiting
Alkalosis DTRs, Muscle Twitching ↑-Muscle
Metab. Nausea, Lethargy, Coma
Acidosis (+) Kussmal breathing NaLoCo Diarrhea
(↑ rate, ↑ depth, metabolic/ketoacidosis)
Buffer System (Sir Jungie’s Way)
Alkalosis Acidosis
“Mother” pH: 7.35-7.45 ↑ ↓
Respiratory PaCO2: 35-45 mmHg ↓ ↑
Metabolic HCO3: 22-26 mEq/L ↑ ↓
1. Compensation: “Yes or no”
a. Is the pH normal?
b. Is there opposing factors?
2. Legend
a. If there are “2 Yes” -> Fully compensated
b. If there is “1 Yes” -> Partially Compensated
c. If there is “2 No” -> Uncompensated
d. The value that copies pH, it is the term
VIII. Pulmonary Volumes & Capacities
TLC (6000mL) VC (4500mL) IC (3500mL) IRV (3000mL)
IRV+TV+ER+RV IRV+TV+ERV IRV+TV TV (500mL)
IC+FRC IV+ERV FRC (2500mL) ERV (1000mL)
VC+RV RV (1500mL) ERV+RV RV (1500mL)
Yo-Mi (1st Part)
IC (Three 500 IRV (3K)
VC (Four 500
[hundred]) TV (500)
TLC (6K) [hundred])
ERV (1K)
FRC (Two 500)
RV (One 500) RV (One-Five)
Chorus
IRV
VC IC (Paused)
TV
TLC
& ERV
FRC &
RV RV
Gold Rank Intensive Review Baguio Batch 2017
Pulmonary System: Anatomy, Physiology, Conditions, Rehabilitation
These are the Pulmonary Volumes N’ Capacities
IRV
VC IC (Paused)
TV
TLC
& ERV
FRC Pati
RV RV
Tidal Volume (TV – 500mL)
o Amount of air inspired or expired with each normal breath
Inspiratory Reserve Volume (IRV – 3000mL)
o Amount of air that can still be inspired in after a normal/resting inspiration
Expiratory Reserve Volume (ERV – 1000mL)
o Amount of air that can still be expired after a normal/resting expiration
Residual Volume (RV – 1500mL)
o Amount of air left inside the lungs after a forceful/maximal expiration
Inspiratory Capacity (IC – 3500mL)
o Amount of air that can be maximally inspired in after a normal/resting expiration
Functional Residual Capacity (FRC – 2500mL)
o Amount of air left inside the lungs after a normal/resting expiration
Vital Capacity (VC – 4500ml)
o Amount of air that can be maximally expired after a maximal inspiration
Total Lung Capacity (TLC – 6000mL)
o Amount of air that can be contained inside the lungs after a forceful/maximal inspiration
Volumes: ITER
o Spirometer
Cannot measure: RV, FRC, TLC
o Body Plethysmography: TLC
o Helium/Nitrogen Wash-out: FRC, RV
COPD: volumes ↑
Restrictive Lung Disease: volumes ↓
IX. O2-Hgb Dissociation Curve “Sa Hgb, Apat-Dapat-Dapat-Apat”
Gold Rank Intensive Review Baguio Batch 2017
Pulmonary System: Anatomy, Physiology, Conditions, Rehabilitation
Shift to the Right
1. ↑ Hydrogen Ions or ↓ pH
2. ↑ CO2
3. ↑ temperature
4. ↑ 2,3 DPG (Phosphoglycerate)
5. Exercise
“↑ HaCOT 23-Ex”
Shift to the Left (Only ↓ PaO2)
1. ↓ Hydrogen Ions or ↑ pH
2. ↓ CO2
3. ↑ Fetal Hgb
X. Bohr Effect “Bo-Co2 (Buko)”
↑ Binding of CO2 with Hgb
↓
Will displace O2
↓
Will promote O2 Transport
XI. Haldane Effect “Hal-O2 (Halo-Halo)”
↑ Binding of O2 with Hgb
↓
Will displace CO2
↓
Will promote CO2 Transport
XII. Pulmonary Assessment
Inspection
Auscultation
Palpation
Percussion
“InAus PaPer”
I. Inspection
Chest Deformity
Barrel Chest (2:2) AP/L Chest Ratio
Pectus Carinatum (Pigeon Chest) (Prominent Sternum)
Pectus Excavation (Funnel Chest)
Normal Anterior/Posterior, Lateral (AP/L) Chest Ratio – 1:2
Gold Rank Intensive Review Baguio Batch 2017
Pulmonary System: Anatomy, Physiology, Conditions, Rehabilitation
Chest Symmetric Expansion
1. Upper Lobes
a. PT: Front of Px
b. Thumb: Sternal Notch
c. Fingers: Above clavicles
2. Right Middle Lobe/Lingula
a. PT: Front of Px
b. Thumb: Xiphoid Process
c. Finger: Lateral Ribs
3. Lower Lobes
a. PT: Behind the Px
b. Thumb: Lower Thoracic Spines
c. Fingers: Lateral Ribs
II. Auscultation
Stethoscope
Normal Breath Sounds
1. Vesicular: soft, low pitched sound
2. Bronchial: loud, hollow/tubular, high pitched sound
3. Bronchovesicular: softer than bronchial
Abnormal/Adventitious Breath Sounds
1. Crackles (Rales): fine discontinued sounds
Ex. Hair Rubbing next to the ear or popping/fizzing soda
(+) Secretions/water
2. Wheezes: continuous high pitched sounds heard on exhalation
Ex. Asthma
3. Stridor: somewhat like muscle breath sounds d/t obstruction of pharynx, larynx, or trachea
4. Rhonchi: somewhat-like snoring d/t (+) secretions
Abnormal Breathing Patterns
1. Dyspnea: rapid rate, shallow depth, irregular rhythm
2. Tachpnea: fast rate, shallow depth, irregular rhythm
3. Bradypena: slow rate, normal to shallow depth, regular rhythm
4. Hyperventilation: fast, ↑ depth, regular rhythm
5. Apnea: absence of ventilation in expiration
6. Apneusis: absence of ventilation in inspiration
7. Cheyne Stokes (waxing & wailing): alternating ↑ & ↓ depth, apnea, regular rhythm
8. Biot’s: slow rate, shallow depth, periods of apnea, somewhat irregular rhythm
Voice Transmission Test
1. Egophony
Normal – “ee”
Abnormal – “aa” (d/t pneumonia, consolidation, pleural effusion)
2. Bronchophony “99” (PBEQ)
Normal: ↓ volume from apex to base
Gold Rank Intensive Review Baguio Batch 2017
Pulmonary System: Anatomy, Physiology, Conditions, Rehabilitation
Abnormal: constant volume from apex to base
3. Whisper Pectoriloquy
Normal: Whispered “1-2-3”
Abnormal: Loud “1-2-3”
III. Palpation
Tactile Fremitus
o Using ulnar border of hand on ICS
o Patient says “99”
o Normal Vibrations: Normal/Air-Filled Lungs
o ↓ Vibrations: hyper-inflated lungs (emphysema)
o ↑ Vibrations: hypo-inflated lungs
IV. Percussion
Using the middle fingers to tap the ICS
Normal Response: Normal/Air-filled Lungs
Hyper-resonance: Hyperinflated lungs
Hypo-resonance: hypoinflated lungs (Lung Collapse)
Dull: (+) secretions
V. Tracheal/Mediastinal Shifting
Contralateral Shifting Ipsilateral Shifting
Compressive Atelectasis Obstructive Atelectasis
Pleural Effusion Pneumonectomy
Pneumothorax Lobectomy
Hemothorax Segmental Resection
“Hinulax”
VI. Colors of Sputum
100 mL/day
Best time to collect sputum, early morning
In the lungs – secretions, outside of lungs – sputum
Clear Normal
Red (+) Blood
Rust (+) Pneumonia
Pink (+) Pulmonary Edema
Yellow Infection
Green Pus
Purple Neoplasm (Lung Cancer)
Flecked (Dark) Carbon Particles
Gold Rank Intensive Review Baguio Batch 2017
Pulmonary System: Anatomy, Physiology, Conditions, Rehabilitation
Pulmonary System II
Cases and Conditions
I. Chronic Obstructive Pulmonary Disease vs Chronic Restrictive Pulmonary Disease
Condition COPD CRPD
Chief Problem Problem with expiration Problem with inspiration
Etiology (+) Air trapping Due to ↓ lung or chest wall compliance
Affected Lung Volumes & ↑ RV ↓ VC
Capacities ↑ FRC ↓ IRV
↑ TLC ↓ TLC
V/Q Ratio < 0.8 > 0.8
Response to Bronchodilators (+) Response (-) response
Examples - Emphysema (most chronic) d/t alterations of
- Chronic Bronchitis 1. Lung Parenchyma & Pleura
- Asthma 2. Chest Wall
- Bronchiectasis 3. Neuromuscular Apparatus
- Cystic Fibrosis
II. Emphysema vs Chronic Bronchitis
Emphysema Chronic Bronchitis
Definition Over-distension of air spaces distal to the terminal Chronic, productive cough of at least 3 months
bronchioles with destruction of alveolar septa for 2 consecutive years
Cause Smoking = ↑ proteolytic enzymes
Destroys Alveolar Sacs Smoking, pollution, occupational hazard
↓ Alpha-1 Antitrypsin
AKA Pink Puffer (Emphysema) Blue Bloater (Bronchitis)
Age +⁄− 60 y/o +⁄− 50 y/o
*Elderly (Elderly) * Conting Bata (Chronic Bronchitis)
Dyspnea Severe Mild
Cough Less Prominent More Prominent
Dyspnea before cough Cough before dyspnea
Sputum Scanty, Mucoid Copious, Purulent
*Evaporated Milk *Condensed Milk
Bronchial
Less Frequent More Frequent
Infection
Body Often overweight, obese
Usually Asthenic with weight loss
Build *Chubby na blue
*Payat
*Cyanotic na baboy
X-Ray Hyper-inflated lungs (N) Sized lungs
Small Heart (R) Ventricular hypertrophy
Diaphragm: low & flat (N) Shaped Diaphragm
+⁄− bullae (pockets of air) (+) Dirty lung appearance
Cor
Rare, except at the late stages More prominent
Pulmonale
Other PE (+) Barrel Chest Cyanotic
Findings (+) Use of accessory muscles of respiration (+) peripheral edema
III. Asthma
Definition
Hypersensitivity of bronchial smooth muscle due to various stimuli resulting to widespread bronchoconstriction
Age
50% <10 years old, Male > Female (2:1)
After 30 y/o Male = Female (1:1)
Gold Rank Intensive Review Baguio Batch 2017
Pulmonary System: Anatomy, Physiology, Conditions, Rehabilitation
Triggering Factors (PBEQ)
Extrinsic
o Inhalant Allergens (Pollen, Dust)
o Food (Chocolate, Milk, Nuts, seafood, chicken, eggs, tomato)
o Animal Hair
o Feathers
o Pollution
o Climate Change
o Drug (Aspirin)
o Irritant Inhalants
Intrinsic
o Upper Respiratory Tract Infections
o Emotional Stress
o Psychological Stress
o Exercise
o Fatigue
Status Asthmaticus
Severe form of asthma
Persists from days to weeks
Px requires Mechanical Ventilator
Fatal
Signs and Symptoms
Triad: Coughing, Wheezing, Dyspnea (CWD) (PBEQ)
(+) Tachypnea
(+) Use of accessory muscles of respiration
Asthma Attack= is terminated by a cough producing a thick, stringy mucus (Kurshmann’s Spirals)
IV. Bronchiectasis
Definition
Permanent dilation of bronchi/bronchioles d/t recurrent pulmonary infections
Obstruction distal to exudation, dilatation proximal to obstruction
Most Commonly Affected
Terminal Bronchioles
2 Types
1. Saccular (Cystic): from large, proximal bronchi down to the 4th generation
2. Cylindrical (Fusiform): from 6th to 10th generations
Signs and Symptoms
Hemoptysis
Dyspnea
Fever
Coughing
V. Cystic Fibrosis (Mucoviscidosis)
Definition
Widespread abnormalities of exocrine glands
B ronchial Mucus Glands
Triad
E xocrine Cells of Pancreas
S weat Glands
*(+) defect of long-arm of chromosome #7 (the long arm is q: the short arm is p)
Signs and Symptoms
(+) productive cough leads to too much secretions leads to i(+) bronchial infections
Gold Rank Intensive Review Baguio Batch 2017
Pulmonary System: Anatomy, Physiology, Conditions, Rehabilitation
Weight Loss (malabsorption – inability of body to breakdown food)
↑ NaCl in sweat (sweat test)
X-Ray
(+) honeycomb lungs
Chronic Restrictive Pulmonary Disease
I. Interstitial Pulmonary Fibrosis
Aka: Hamman-Rich Disease
Idiopathic
Associated with smoking, family history, collagen disease
Cardinal Sign: progressive dyspnea
Death in 5-6 years after the dx
II. Pneumonia (Intra-alveolar Infection)
3 Types
A. Bacterial (Streptococcal; Most common)
B. Viral
C. Aspiration (ex. CVA, ALS; (-) Gag Reflex)
Signs and Symptoms
Fever
Chills
Cough
Chest Pain
III. Atelectasis (Lung Collapse)
2 Types
Primary (Compressive) Secondary (Obstructive)
Ex. Pleural Effusion: too
much pleural fluid lung
collapse
Give px Incentive Spirometry to help px breath
S/Sx:
↑ vibration
Hyporesonance
Asymmetric Expansion
Dyspnea
IV. Tuberculosis (TB)
Etiology
Mycobacterium Tuberculae
Incubation Period
2-10 weeks
Maximally Infectious
First 2 weeks
(isolate px in a Negative-P° room, bacteria have trouble traveling through air)
Treatment
3-12 months, average 6 months
Primary Complex (TB of Children)
Infected Active TB Adult transmits TB to Child
Gold Rank Intensive Review Baguio Batch 2017
Pulmonary System: Anatomy, Physiology, Conditions, Rehabilitation
S/Sx
Hallmark: HEMOPTYSIS
Cough
Fever
Wt. Loss
Enlargement of Lymph Nodes
Drugs (RIPES)
R ifampicin
I soniazid
P yrazinamide
E thambutol
S treptomycin
V. Pulmonary Edema
H2O in the alveoli due to unequal capillary P
Associated with Left sided heart failure, MI, Mitral Valve disease, Stenosis
S/Sx
(+) Crackles/rales
Nonproductive cough
Sputum: pink & frothy
Fever
Dyspnea
VI. Pulmonary Embolism
Definition
Lodging of large/small particles into the pulmonary venous circulation
Most Common Cause
Deep Vein Thrombosis
Other Causes
C lotting Disorder
O ral Contraceptives
V enous stasis
A ir (Trauma)
Prevention
Ankle Pumps
Positive Pulmonary Embolism Treatment
Immobilization
Signs and Symptoms
Sudden Acute Pain
Cough
Dyspnea
VII. Pleuritis & Pleural Effusion
Pleuritis: inflammation of pleura
Pleural Effusion: excessive accumulation of pleural fluid
S/Sx
Sharp/Dull Pain
Doorstop Breathing
Dyspnea
Coughing
Gold Rank Intensive Review Baguio Batch 2017
Pulmonary System: Anatomy, Physiology, Conditions, Rehabilitation
(+) Pleural Rub/Friction
Pleural Tube (P-Tube) Insertion
8th-9th ICS
VIII. Pneumothorax
Air/Gas leaking inside the pleural space
S/Sx
Sudden, Sharp Pain
Doorstop Breathing
Dyspnea
Cough
Pleural Tube (P-Tube) Insertion
2nd to 3rd ICS
IX. Severe Acute Respiratory Syndrome (SARS)
Caused By
Corona Virus
S/Sx
Fever or ↑ in temperature
Sore Throat
Dry Cough
Myalgia
Lethargy
Etiology
Direct transmission within the past 10 days
Code
“K”
MERS-CoV – Middle East Respiratory Syndrome – Corona Virus
- MERS-CoV Animal: Camel
X. Bronchogenic Carcinoma (Lung Cancer)
3 Types (SOS)
a. Small Cell (Most Fatal)
b. Oat Cell
c. Squamous Cell (Most Common)
Signs and Symptoms
Initially: Fever
(+) Hemoptysis
Fatigue
Unexplainable Weight Loss
Hoarseness
Pulmonary Rehabilitation
I. Postural Drainage (Bronchial Drainage/Chest PT)
2 Goals
1. To prevent accumulation of secretions
2. To remove secretions already there
Duration
20 – 30 minutes, Kisner; 45 minutes O’Sullivan, not more than 45-60 minutes
Gold Rank Intensive Review Baguio Batch 2017
Pulmonary System: Anatomy, Physiology, Conditions, Rehabilitation
Positions
Use of Tilt Table
Trendelenburg/T-Position: head down, feet up
o CI for recent cranial surgery bc ↑ ICP
Reverse T-Position: feet down, head up
Manual Techniques (3-5 minutes)
1. Percussion
2. Vibration
3. Shaking
Do Not Percuss Over
Bony prominence
Breast Tissue
Chest Pain
Thoracic Surgery
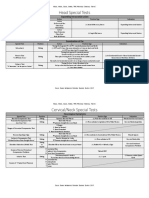
Lung Map
Right Lung Left Lung
10 Segments 8 Segments
Apical
Apical Posterior
Upper Lobes Post Anterior
Anterior Superior Lingular
Inferior Lingular
Lateral
Middle Lobe NONE
Medial
Superior (Apical) Superior (Apical)
Anterior Basal Anterior Basal
Lower Lobes Posterior Basal Posterior Basal
Lateral Basal Lateral Basal
Medial Basal Medial Basal
I. Upper Lobes
Segment Patient Position Percussion Memory Technique
Anterior Apical Sitting, leaning backward Below clavicles
Apical: Sitting
Posterior Apical Sitting, Leaning forward Above scapulae
Male: nipple area
Anterior Supine, bed flat
Female: just above breast
1/4th turn from prone on (R) side
The Only Lobe for
Left Posterior Reverse T-Position (30°-45°) (L) Scapula
Reverse T-Position
18-20 inch head elevation (large pillows)
Right Posterior 1/4th Turn from prone (L) side, bed flat (R) Scapula
Gold Rank Intensive Review Baguio Batch 2017
Pulmonary System: Anatomy, Physiology, Conditions, Rehabilitation
II. Middle Lobe/Lingula
Segment Position Percussion Technique
1/4th turn from supine on (L) side
Middle Lobe T-Position (15°-30°) Below (R) Nipple
12-16 inch foot/feet elevation The only T-Position that
1/4th turn from supine on (R) side is 15°-30°
Lingula T-Position (15°-30°) Below (L) Nipple
12-16 inch foot/feet elevation
III. Lower Lobes
Segment Position Percussion
Anterior Supine; T-Position (30°-45°) Anterior Lower Ribs
Posterior Prone; T-Position (30°-45°) Posterior Lower Ribs
Left Lateral (R) Sidelying; T-Position (30°-45°) Left Lateral Lower Ribs
Right Lateral (L) Sidelying; T-Position (30°-45°) Right Lateral Lower Ribs
Superior Prone, bed flat below the Scapulae
Gold Rank Intensive Review Baguio Batch 2017
Pulmonary System: Anatomy, Physiology, Conditions, Rehabilitation
IV. Breathing Exercises (2-3 reps)
2-3 reps to prevent hyperventilation
1. Diaphragmatic Breathing
a. Improves ventilation
2. Pursed Lip Breathing
a. For patients with dyspnea, shortness of breath, asthma
b. ↑ intrabronchial P°
c. Creates (+) P°
3. Segmental Breathing
a. For patients with atelectasis, pneumonia
b. Apply resistance to lobe with lung collapse
4. Glossopharyngeal Breathing
a. Aka Frog Breathing
b. For patients with high level SCI, post-polio syndrome
c. 8-10 gulps/gasps of air
5. Sustained Maximum Inspiration (SMI)
a. Used pre-operatively to prevent atelectasis
V. Mediastinal Breathing
CONTRALATERAL IPSILATERAL
Compressive Atelectasis Obstructive Atelectasis
Pleural Effusion Pneumonectomy
Pneumothorax Lobectomy
Hemothorax Segmental Resection
VI. Coughing
“Double Cough”
o 1st Cough: to remove secretion
o 2nd Cough: to clear the airways
o Effective up to 7th Generation (Alveolar Ducts)
o For SCI px: press 5lbs of pressure on px abdomen to help
“Endotracheal Suctioning”
o Duration 10-15 sec
o Effective up to 3rd generation (Lobar Bronchi)
“Tracheal Tickle/Stimulation”
o For infants and unconscious patients
Gold Rank Intensive Review Baguio Batch 2017
You might also like
- Instant Download Connect Core Concepts in Health 16th Edition Ebook PDF PDF ScribdDocument41 pagesInstant Download Connect Core Concepts in Health 16th Edition Ebook PDF PDF Scribdcarmine.adams474100% (48)
- BLS Handbook Final - Red CrossDocument74 pagesBLS Handbook Final - Red CrossLuis Fernando RodriguesNo ratings yet
- 26 Motor Neuron Diseases (FINAL)Document5 pages26 Motor Neuron Diseases (FINAL)kath-kathNo ratings yet
- 16 Upper Extremity (FINAL)Document30 pages16 Upper Extremity (FINAL)kath-kath100% (1)
- Tai Chi For BeginnerDocument611 pagesTai Chi For Beginnersyafiq65100% (1)
- Neurology I - Nervous System: CNS - Brain CNS - Spinal Cord Peripheral Nervous SystemDocument29 pagesNeurology I - Nervous System: CNS - Brain CNS - Spinal Cord Peripheral Nervous SystemDarla Mitu100% (2)
- Infant Medical SOAP NoteDocument1 pageInfant Medical SOAP NoteTaylor ChristianNo ratings yet
- Guideline Suicide Risk Management PDFDocument56 pagesGuideline Suicide Risk Management PDFAbu Abbas AiyubNo ratings yet
- Nursing Care Plan Format Name: - Medical Diagnosis: Myasthenia Gravis DateDocument2 pagesNursing Care Plan Format Name: - Medical Diagnosis: Myasthenia Gravis DateSheryl Ann Barit Pedines100% (1)
- 9 Digestive System (FINAL)Document6 pages9 Digestive System (FINAL)kath-kathNo ratings yet
- 5 Peripheral Vascular System (FINAL)Document4 pages5 Peripheral Vascular System (FINAL)kath-kathNo ratings yet
- 7 MSCI ModuleDocument45 pages7 MSCI ModuleCoffee MorningsNo ratings yet
- Special TestsDocument31 pagesSpecial TestsKyle OrtegaNo ratings yet
- 19 Fractures (FINAL)Document7 pages19 Fractures (FINAL)kath-kathNo ratings yet
- 8 Integumentary System (FINAL)Document11 pages8 Integumentary System (FINAL)kath-kathNo ratings yet
- 3 ReviewerDocument46 pages3 ReviewerSHINE JASMIN LAXAMANA100% (1)
- 3 Head, Neck, Back, and Spine ModuleDocument55 pages3 Head, Neck, Back, and Spine ModuleCoffee MorningsNo ratings yet
- HGD Pedia Dec 2022 Final CoachingDocument14 pagesHGD Pedia Dec 2022 Final CoachingBb PrintsNo ratings yet
- DDM 2-A5: General Anatomy Sas 1: The Upper LimbDocument7 pagesDDM 2-A5: General Anatomy Sas 1: The Upper LimbKathleen Abegail Bacay NalzaroNo ratings yet
- Basic ECG Interpretation Review Questions Flashcards - QuizletDocument5 pagesBasic ECG Interpretation Review Questions Flashcards - Quizletdina sharafNo ratings yet
- 2000 Final FebruaryDocument13 pages2000 Final FebruaryNini SisonNo ratings yet
- Ca - MS (Respiratory)Document4 pagesCa - MS (Respiratory)kyleNo ratings yet
- Studychacha Com Discuss 276610 MPT Entrance Exam Previous Ye PDFDocument11 pagesStudychacha Com Discuss 276610 MPT Entrance Exam Previous Ye PDFAahna GuptaNo ratings yet
- Renal Endo Physiology Postlec Exam June 2023Document3 pagesRenal Endo Physiology Postlec Exam June 2023NinjaNo ratings yet
- Anatomy - Head and NeckDocument18 pagesAnatomy - Head and NeckPrudhvirani ChidipothuNo ratings yet
- AHS Spotter Masterlist With AnswersDocument60 pagesAHS Spotter Masterlist With AnswersManigandanNo ratings yet
- 10 Renal System (FINAL) PDFDocument3 pages10 Renal System (FINAL) PDFJohn Juan TwanNo ratings yet
- 3.0 Grand Physiology Finals Compilation - Batch 2017Document89 pages3.0 Grand Physiology Finals Compilation - Batch 2017Sheryl Layne Lao-SebrioNo ratings yet
- Gold Rank Review Center December 2022: Postlecture Examination: Upper Extremity Orthopedic ConditionsDocument4 pagesGold Rank Review Center December 2022: Postlecture Examination: Upper Extremity Orthopedic ConditionsTed Lawrence CiscarNo ratings yet
- Giles C1 C AnsDocument23 pagesGiles C1 C AnsFlorentz DavidNo ratings yet
- Rom MMT Trunk Study Sheet 1Document3 pagesRom MMT Trunk Study Sheet 1api-242889989No ratings yet
- PGP 2015 V 11 PDFDocument10 pagesPGP 2015 V 11 PDFYadav NishaNo ratings yet
- 6 Neurology ModuleDocument46 pages6 Neurology ModuleCoffee MorningsNo ratings yet
- Lecture 11: Cerebrum: Neuroscience 1: Cerebral CirculationDocument11 pagesLecture 11: Cerebrum: Neuroscience 1: Cerebral CirculationAudrey Nicole LisingNo ratings yet
- 24 Neuroconditions (FINAL)Document14 pages24 Neuroconditions (FINAL)kath-kathNo ratings yet
- Lateral Epicondylitis: ST NDDocument2 pagesLateral Epicondylitis: ST NDMuhammad Ucuk100% (1)
- Shoulder Secial Tests Final FrontierDocument6 pagesShoulder Secial Tests Final Frontierdina sharafNo ratings yet
- 12 Sports Physiology (FINAL)Document6 pages12 Sports Physiology (FINAL)kath-kathNo ratings yet
- Miscellaneous Systemic ExamDocument9 pagesMiscellaneous Systemic ExamEDRIS SEIDNo ratings yet
- Neuroanatomy Spotters DR - KalpanaDocument53 pagesNeuroanatomy Spotters DR - KalpanaKanishk ChawlaNo ratings yet
- Check For Understanding (45 Minutes) : Nalzaro, Kathleen Abegail B. DDM 2-A5 General Anatomy Sas 2: The Lower LimbDocument9 pagesCheck For Understanding (45 Minutes) : Nalzaro, Kathleen Abegail B. DDM 2-A5 General Anatomy Sas 2: The Lower LimbKathleen Abegail Bacay NalzaroNo ratings yet
- 15 PharynxDocument9 pages15 Pharynxapi-3757921No ratings yet
- Nervous Tissue NotesDocument3 pagesNervous Tissue NotesTulibas Karl Jade J - BSN 1ENo ratings yet
- Siegelman Online Advantage 1.1Document35 pagesSiegelman Online Advantage 1.1Samantha AgustinNo ratings yet
- Myasthenia GravisDocument2 pagesMyasthenia GravisJulia SalvioNo ratings yet
- Acidosis Vs AlkalosisDocument15 pagesAcidosis Vs Alkalosisdina sharafNo ratings yet
- REVIEW SONGS LyricsDocument10 pagesREVIEW SONGS LyricsClaNo ratings yet
- Ms Drills 3Document10 pagesMs Drills 3Karen Mae Santiago AlcantaraNo ratings yet
- Reviewer PtcaDocument93 pagesReviewer PtcaCarmela Mallare100% (1)
- Neuro Master Doc SaraDocument237 pagesNeuro Master Doc SaraGokulakrishnan KrishnanNo ratings yet
- Upper Extremity (Anatomy)Document17 pagesUpper Extremity (Anatomy)Margareth Christine CusoNo ratings yet
- APK Aug991Document21 pagesAPK Aug991Kim Sean DipalacNo ratings yet
- PHYSIOLOGY COMPRE 2nd Yr - 230512 - 233623 1Document9 pagesPHYSIOLOGY COMPRE 2nd Yr - 230512 - 233623 1SANKEPALLI, PAVITHRA REDDYNo ratings yet
- Apk Mock Boards Practice Questions Set A No AnswerDocument26 pagesApk Mock Boards Practice Questions Set A No AnswerYuvienco DrecoNo ratings yet
- Anatomy - Scalp PDFDocument3 pagesAnatomy - Scalp PDFAngel Kim100% (1)
- Student Activity - Nervous SystemDocument4 pagesStudent Activity - Nervous SystemSeth Khalil LardausNo ratings yet
- Neuro Exam ReviewDocument6 pagesNeuro Exam ReviewDianne Flores100% (2)
- My Fracture NotesDocument20 pagesMy Fracture NotesZai AkmaNo ratings yet
- Neuromuscular and Nervous System 2010 With AnswersDocument13 pagesNeuromuscular and Nervous System 2010 With AnswersWenzy CruzNo ratings yet
- Med Surge 1Document39 pagesMed Surge 1rave andrei MacanayaNo ratings yet
- The Shoulder and Shoulder GirdleDocument43 pagesThe Shoulder and Shoulder GirdleMuhammad UsmanNo ratings yet
- Apk 1997Document9 pagesApk 1997Pau CMedinaNo ratings yet
- Clinical Significance of Upper LimbDocument3 pagesClinical Significance of Upper LimbflissxloveNo ratings yet
- Ue MMTDocument5 pagesUe MMTKali AceñaNo ratings yet
- Upper Limbs NOTES - BRS Anatomy, Table of Muscles and BRS Questions With Answers ExplainedDocument14 pagesUpper Limbs NOTES - BRS Anatomy, Table of Muscles and BRS Questions With Answers ExplainedJustyna PoznanskaNo ratings yet
- Elbow Special TestDocument4 pagesElbow Special TestEllaiza Astacaan100% (1)
- Q&A AprilDocument23 pagesQ&A Apriltayyabc25No ratings yet
- Respiratory System (Week 14)Document33 pagesRespiratory System (Week 14)Krisha Mabel TabijeNo ratings yet
- 21 Prosthetics (FINAL)Document7 pages21 Prosthetics (FINAL)kath-kathNo ratings yet
- 19 Fractures (FINAL)Document7 pages19 Fractures (FINAL)kath-kathNo ratings yet
- 22 Assistive Devices (FINAL)Document9 pages22 Assistive Devices (FINAL)kath-kathNo ratings yet
- 24 Neuroconditions (FINAL)Document14 pages24 Neuroconditions (FINAL)kath-kathNo ratings yet
- 17 Lower Extremity (FINAL)Document32 pages17 Lower Extremity (FINAL)kath-kath100% (1)
- 15 Head Neck Back Spine TMJ (Special Tests) (FINAL)Document8 pages15 Head Neck Back Spine TMJ (Special Tests) (FINAL)kath-kathNo ratings yet
- 12 Sports Physiology (FINAL)Document6 pages12 Sports Physiology (FINAL)kath-kathNo ratings yet
- 9 Digestive System (FINAL)Document6 pages9 Digestive System (FINAL)kath-kathNo ratings yet
- 8 Integumentary System (FINAL)Document11 pages8 Integumentary System (FINAL)kath-kathNo ratings yet
- 4 Blood Physiology (FINAL)Document8 pages4 Blood Physiology (FINAL)kath-kathNo ratings yet
- 5 Peripheral Vascular System (FINAL)Document4 pages5 Peripheral Vascular System (FINAL)kath-kathNo ratings yet
- CH 73Document18 pagesCH 73JE Yufra100% (1)
- The Epidemiology of Aimentary DiseasesDocument243 pagesThe Epidemiology of Aimentary DiseasesAlfredoNo ratings yet
- Susan Aldridge Magic Molecules How Drugs Work Cambridge University Press 1998Document1,095 pagesSusan Aldridge Magic Molecules How Drugs Work Cambridge University Press 1998KravishIQIceNo ratings yet
- Omnibus Health Guidelines For Adults 2022Document99 pagesOmnibus Health Guidelines For Adults 2022Raymunda Rauto-avilaNo ratings yet
- Compute For The Total Body Surface Area Affected by The BurnsDocument2 pagesCompute For The Total Body Surface Area Affected by The BurnsVAL ASHLIE ACEBARNo ratings yet
- Cardiac Myocytes CultureDocument6 pagesCardiac Myocytes CultureÉmerson MoreiraNo ratings yet
- BMJ k4884Document8 pagesBMJ k4884Asela SubhasingheNo ratings yet
- PNG Child Health Policy and Plan 2009 2020Document120 pagesPNG Child Health Policy and Plan 2009 2020Natalie PimbiNo ratings yet
- 01-06-2202-13-40-GMC-Information Radiodiagnosis & ImagingDocument18 pages01-06-2202-13-40-GMC-Information Radiodiagnosis & ImagingSilent StalkerNo ratings yet
- Class 5 Revision Worksheet Pa-1 (23-24)Document2 pagesClass 5 Revision Worksheet Pa-1 (23-24)palak kaurNo ratings yet
- Paediatric Exercise Science and Medicine, 2 EditionDocument669 pagesPaediatric Exercise Science and Medicine, 2 EditionFlávia AquinoNo ratings yet
- Oral Cancer and ManagementDocument148 pagesOral Cancer and ManagementFadilaNo ratings yet
- Log Book PediatricsDocument22 pagesLog Book Pediatricsرافت العواضيNo ratings yet
- Makalah Kel 2 Bhs. InggrisDocument15 pagesMakalah Kel 2 Bhs. Inggriswardi irmahNo ratings yet
- Adenosine Deaminase: Quantitative Determination of Adenosine Deaminase (ADA) in Serum and Plasma SamplesDocument1 pageAdenosine Deaminase: Quantitative Determination of Adenosine Deaminase (ADA) in Serum and Plasma Samplesmark.zac1990No ratings yet
- Normal Puerperium & PostnatalDocument38 pagesNormal Puerperium & PostnatalMrs Rehan100% (1)
- Shagoofa Rakhshanda MSC ThesisDocument83 pagesShagoofa Rakhshanda MSC ThesisAbdullah M AbdullahNo ratings yet
- Department of Health: National Drug Policy - Pharmaceutical - Pharmaceutical Management Unit 50Document315 pagesDepartment of Health: National Drug Policy - Pharmaceutical - Pharmaceutical Management Unit 50Alfred John TrinidadNo ratings yet
- Maret 2021Document36 pagesMaret 2021Muhammad Pahlan PiruzziNo ratings yet
- Congenital Cataracts: Case Presentation 2Document46 pagesCongenital Cataracts: Case Presentation 2nadyaNo ratings yet
- StomatitisDocument17 pagesStomatitis4A - Hazel Ann G. EspinolNo ratings yet
- Laboratory Diagnosis of The Anti-Phospholipid Syndrome (APS)Document32 pagesLaboratory Diagnosis of The Anti-Phospholipid Syndrome (APS)Kishore KumarNo ratings yet
- Hajj Health Management in IndonesiaDocument2 pagesHajj Health Management in IndonesiaTeguh YuwonoNo ratings yet
- Concept MapDocument13 pagesConcept MapIssa RomaNo ratings yet