Professional Documents
Culture Documents
Pulp Reactions To Different Preparation Techniques On Teeth Exhibiting Periodontal Disease
Pulp Reactions To Different Preparation Techniques On Teeth Exhibiting Periodontal Disease
Uploaded by
MAYRA ALEJANDRA BAHAMON TRUJILLOOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pulp Reactions To Different Preparation Techniques On Teeth Exhibiting Periodontal Disease
Pulp Reactions To Different Preparation Techniques On Teeth Exhibiting Periodontal Disease
Uploaded by
MAYRA ALEJANDRA BAHAMON TRUJILLOCopyright:
Available Formats
Journal of Oral Rehabilitation 2000 27; 93– 102
Pulp reactions to different preparation techniques on teeth
exhibiting periodontal disease
A. ZO8 LLNER* & P. GAENGLER† *Department of Prosthodontics, and the †Department of Conservative Dentistry, School
of Dental Medicine, University of Witten/Herdecke, Alfred Herrhausen Str. 50, 58448 Witten, Germany
SUMMARY To evaluate the histopathological out-
come of two preparation techniques (featheredge pathologically rated according to the BRD criteria
preparation/shoulder preparation) on teeth ex- comprising the parameters (i) Bacterial invasion, (ii)
hibiting pulp reactions due to age and periodontal Regenerative parameters, (iii) Degenerative
disease, 11 teeth were prepared for full veneer parameters. Degenerative reactions were more cor-
crowns. Laboratory made resin crowns were fixed related with tooth preparation than with advanced
with a zinc phosphate cement for a period of 90 periodontal disease. The severity of endondontal
days. After extraction, adjacent pulpal areas were reactions depends more on remaining dentin thick-
histo- ness than on the type of preparation.
Introduction Material and methods
Pulp reactions to preparation techniques are still a Eleven teeth with positive reactions to sensitivity test-
major concern in restorative and prosthodontic den- ing, no or minimal carious lesions, advanced periodon-
tistry. According to many longitudinal investigations tal destruction, and therefore scheduled for extraction,
there is a high rate of primarily vital teeth exhibiting were prepared for full veneer crowns with the pa-
typical signs of endodontal complications following tient’s consent using two different preparation tech-
dental restorations. According to Bergenholtz and Ny- niques. The featheredge preparation, limited to the
man (1984), up to 15% of teeth showed negative enamel/dentin junction, was used in experimental
results to sensitivity testing, including periapical infl- group 1, including 13 sites. The shoulder preparation,
ammatory lesions, 4 – 13 years after crown preparation. extended deep into the dentin, was used in experi-
Different factors may accumulate and lead to these mental group 2, including nine sites. Either one or
dramatic changes of the endodontium, including age, both preparation techniques were applied. The control
abrasion/attrition, periodontal disease, carious lesions group 3 with no experimental preparations consisted
as natural occurring phenomena and pulp damage of four teeth of the same patient with the same level
caused by dental procedures and materials. Therefore, of periodontal destruction. Detailed information con-
it was the aim of the present investigation to compare cerning the results of the clinical investigation and the
the influence of different preparation techniques, like type of preparation is summarized in Table 1. Labora-
shoulder preparation and featheredge preparation, to tory made crowns (Visio Gem®*) were fixed with zinc
investigate further the reactions to bacterial invasion, phosphate cement (Harvard®†). The frequent clinical
to characterize the reactions of the pulp in correlation control included sensitivity testing, percussion testing
to the remaining dentin thickness, taking into account
the already predamaged pulp, and finally to conclude
* Espe, Am Griesberg 2, 82229 Seefeld, Germany.
clinical recommendations concerning pulp †
Richter & Hoffmann Harvard Dental, Johannisberger Str. 24,
degeneration. 14197 Berlin, Germany.
© 2000 Blackwell Science Ltd 93
94 A . Z O8 L L N E R & P . G A E N G L E R
Table 1. Overview: clinical documentation of prepared teeth and control group
Age Probing depth Recession Attachment loss
Tooth Sex (years) Site Preparation technique (mm) (mm) (mm)
11 Female 50 Buccal Featheredge preparation 3 2 5
Oral Featheredge preparation 3 3 6
12 Female 50 — Control 4 1 5
12 Male 62 Buccal Featheredge preparation 4 1 5
Oral Featheredge preparation 4 1 5
13 Female 50 Mesial Featheredge preparation 4 2 6
Distal Featheredge preparation 4 2 6
17 Male 62 Buccal Shoulder preparation 4 3 7
Oral Shoulder preparation 4 3 7
21 Female 50 Buccal Shoulder preparation 3 3 6
Oral Featheredge preparation 3 2 5
21 Male 62 Buccal Shoulder preparation 3 2 5
Oral Shoulder preparation 3 2 5
22 Female 50 — Control 5 2 7
23 Female 50 Buccal Shoulder preparation 4 2 6
Oral Featheredge preparation 4 3 7
25 Female 50 — Control 6 0 6
25 Male 62 Buccal Shoulder preparation 3 2 5
Oral Featheredge preparation 3 2 5
32 Male 62 Buccal Featheredge preparation 3 4 7
Oral Shoulder preparation 3 4 7
34 Male 62 Buccal Featheredge preparation 3 1 4
Oral Featheredge preparation 3 1 4
37 Male 62 — Control 4 6 10
42 Male 62 Buccal Featheredge preparation 3 3 6
Oral Shoulder preparation 3 3 6
and pain history. The teeth were carefully extracted shoulder (Fig. 1) and the thickness of the remaining
after 90 days under local anesthesia and the roots dentin (Fig. 2) at three different levels: D1—inner part
were cut off under permanent water cooling for rapid of the margin, shortest distance to the pulp; D2—in-
penetration of 5% buffered, neutral formalin. The ner margin, following the direction of the dentin
specimens were then decalcified in HNO3, embedded tubules to the pulp and D3—end of the preparation,
in paraffin, serially sectioned at 5 mm and stained with following the direction of the dentin tubules to the
haematoxilin – eosin, azan and according to J. Hopkins pulp.
for the detection of bacteria. Adjacent pulpal areas of
each section were histopathologically rated (micro-
scope: DMRM‡) according to the BRD criteria (Table 2)
Results
comprising the parameters (i) Bacterial invasion, (ii)
Regenerative parameters, (iii) Degenerative parame- The mean extension of the shoulder preparation into
ters. The endodontal reactions localized in the crown, the dentin was 0.8 mm. Table 3 demonstrates the corre-
in the root or adjacent to the prepared margin were lation of bacteria in dentin tubules and the type of
separately rated. The quantitative measurement of preparation. Bacterial invasion occurs in both types:
video-based pictures of each section (screen: KX- featheredge preparation and shoulder preparation (Fig.
14P1§; camera: CF11/1¶) included the width of the 3). The correlation of grade of bacterial invasion to
‡
irritation dentin (Table 4) as an example for the en-
Leica, Lilienthalstr. 39–45, 64625 Bensheim, Germany.
§
Sony, 7-35 Kitashinagawa 6-chome, Shinagawa-ku, Tokyo 141,
dodontal reactions shows no significant results. The
Japan. histopathological changes of the endodontal areas adja-
¶
Kappa, Kleines Feld, 37130 Gleichen, Germany. cent to the rating points D1–D3 are summarized in
© 2000 Blackwell Science Ltd, Journal of Oral Rehabilitation 27; 93–102
PULP REACTIONS TO CROWN PREPARATIONS 95
Table 2. BRD coding criteria
I Bacterial invasion
Grade 0: No signs of bacterial invasion
Grade 1: Moderate bacterial invasion along prepared margins
Grade 2: Moderate invasion in isolated dentin tubules
Grade 3: Severe invasion in most dentin tubules
Grade 4: Infection of necrotic pulp areas
II Regenerative paramenters of the endodontium
1. Regular irritation dentin
Grade 0: No signs of irritation dentin
Grade 1: Regular irritation dentin, localized in defined areas, no tendency to obliteration, well marked zone of uncalcified
dentin (predentin)
Grade 2: Regular irritation dentin, circumpulpal, no tendency to obliteration, well marked zone of uncalcified dentin (pre-
dentin)
Grade 3: Regular irritation dentin, tendency to obliteration, reduction or absence of uncalcified dentin (predentin)
2. Transient inflammation cells in pulpal tissue
Grade 0: No signs of inflammation cells
Grade 1: Isolated chronical and/or acute inflammation cells, fibroblast rich connective tissue (mesenchymal character)
Grade 2: Isolated chronical and/or acute inflammation cells, collagen rich connective tissue (loss of mesechymal character,
reduction of pulpoblasts and fibroblasts, isolated denticles)
III Degenerative parameters of the endodontium
1. Irregular irritation dentin
Grade 0: No signs of irregular irritation dentin
Grade 1: Irregular direction of dentin tubules, moderate numeric reduction of odontoblast processes, localized
Grade 2: Increase of irregular direction of dentin tubules, severe numeric reduction of odontoblast processes, localized
Grade 3: Severe irregularities in the direction of dentin tubules and/or loss of odontoblast processes, localized or circumpulpal
Grade 4: Mainly osteodentin, circumpulpal
Grade 5: Only osteodentin with inclusion of tissue, circumpulpal
Grade 6: Tendency to obliteration with areas of homogenous mineralisation, circumpulpal
2. Tissue necrosis
Grade 0: No signs of tissue necrosis
Grade 1: Isolated areas of tissue necrosis, localized and/or included by hard tissue
Grade 2: Extensive tissue necrosis (crown pulp)
Grade 3: Tissue necrosis reaching/including root pulp
3. Dentin resorption
Grade 0: No signs of dentin resorption
Grade 1: Isolated dentin resorption in crown dentin
Grade 2: Isolated dentin resorption in root dentin
Grade 3: Severe dentin resorption (internal granuloma)
4. Denticles
Grade 0: No signs of denticles
Grade 1: Fibrodenticles, isolated
Grade 2: Cellular fibrodenticles, isolated
Grade 3: Severe amount of denticles (free and/or attached), localised in crown pulp
Grade 4: Severe amount of denticles (free and/or attached), reaching the root pulp
5. Inflammation
Grade 0: No signs of inflammation cells
Grade 1: Isolated infiltration of chronical and/or acute inflammation cells
Grade 2: Infiltration of large areas of the pulp, tendency of demarcation
Grade 3: Severe infiltration without demarcation
Grade 4: Isolated abscesses
Grade 5: Large abcess (for example crown pulp)
© 2000 Blackwell Science Ltd, Journal of Oral Rehabilitation 27; 93 – 102
96 A . Z O8 L L N E R & P . G A E N G L E R
Fig. 1. Quantitative measurement: width of the shoulder (s).
Fig. 2. Quantitative measurement: remaining dentin thickness at
rating point D1, D2, D3.
Table 5. The most severe degenerative changes occur
in the area next to the rating point D2. The irregular
dentin is more pronounced in group 1 and group 2
irritation dentin formation is characterized by grade 3
compared with control group 3. A significant differen-
(out of 6): severe irregularities in the course of dentin
tiation between the two techniques was not possible.
tubules and/or loss of odontoblastic processes. The
Comparing pulp reactions and the remaining dentin
mean grade for the featheredge preparation is 1.6
thickness (Table 7), three groups were formed: up to
(Fig. 4) and for the shoulder preparation 1.8 (Fig. 5).
2 mm, between 2.1 and 2.5 mm and more than
More pronounced pathological changes like osteo- 2.5 mm. Especially, the endodontal reactions to less
dentin formation were not observed. Because of this remaining dentin thickness are characterized by
reaction pattern, Tables 6 – 9 refer only to this pulp severe irregular irritation dentin formation and total
area adjacent to rating point D2. The correlation of absence of regular irritation dentin formation. This is
the two preparation techniques and the control group in sharp contrast to less pathological changes in cases
(Table 6) clearly documents that regular irritation of thicker remaining dentin. The mean ratings of 0.6
dentin formation is less pronounced both in group 1 and 1.1 demonstrate very normal regular irritation
(featheredge preparation, mean BRD grading 0.5) and dentin formation and only moderate irregular irrita-
in group 2 (shoulder preparation, mean BRD grading tion dentin formation. Taking first the featheredge
0.4) compared with the control group 3 (mean BRD preparation, Table 8 shows the rating of endodontal
grading 1.2). In contrast to this, the irregular irritation reactions in different areas of the pulp: crown pulp,
© 2000 Blackwell Science Ltd, Journal of Oral Rehabilitation 27; 93–102
PULP REACTIONS TO CROWN PREPARATIONS 97
tion (crown pulp, area of the margin at point D2) 1.8
Table 3. Bacterial invasion into dentin tubules and type of
(Fig. 6)
preparation
BRD grading
Discussion
Mean Minimum Maximum
Earlier methodological prospective in vivo studies
Group 1 (featheredge 1.3 0 3
preparation) used graded classifications for the estimation of
Group 2 (shoulder prepa- 1.0 0 3 (pathological) pulpal changes, including the parame-
ration)
ters of inflammatory cell response, soft tissue organi-
zation, dentin bridge formation and bacterial staining,
as already suggested by Langeland et al. (1966),
slightly modified and confirmed for recent studies by
margin (D2) and root pulp. The most severe degener- Pameijer & Stanley (1995). Warfinge (1986) tried
ative reactions occurred in the crown pulp (irregular to introduce morphometric methods for the evalua-
irritation dentin, mean BRD grading 1.5) and in the tion of inflammatory responses. As a consequence,
area of the margin at point D2 (mean BRD grading pathological degenerative reactions are well defined
1.6). The results for the shoulder preparation (Table for teeth primarily exhibiting no pathological changes
9) document the same tendency with slightly different of the endodont, like in short-term biocompatibility
mean BRD gradings: irregular irritation dentin forma- testing for dental materials and methods defined in
Fig. 3. J. Hopkins stain (×320), isolated
bacteria in dentin tubules (BRD grade 2).
Table 4. Bacterial invasion
into dentin tubules and BRD grading
irritation dentin formation
Bacterial invasion Grade 0 Grade 1 Grade 2 Grade 3
Regular irritation dentin (mean/min/max) 0.0/0/0 0.7/0/1 0.0/0/0 0.0/0/0
Irregular irritation dentin (mean/min/max) 2.0/1/3 1.3/0/3 2.3/1/3 2.5/2/3
© 2000 Blackwell Science Ltd, Journal of Oral Rehabilitation 27; 93 – 102
98 A . Z O8 L L N E R & P . G A E N G L E R
(shoulder preparation)
Group 2
0.4/0/1
1.8/0/3
(featheredge preparation)
Group 1
Area D3
0.6/0/1
1.2/0/3
(shoulder preparation)
Group 2
0.4/0/1
1.8/0/3
(featheredge preparation)
Table 5. Irritation dentin formation at pulp areas adjacent to D1, D2, D3 (see Fig. 2)
Group 1
Area D2
0.5/0/1
1.6/0/3
Fig. 4. Azan stain ( × 1), featheredge preparation, overview. (shoulder preparation)
ISO/EN 7405 (1997). The suggested semi-quantitative
Group 2
classification proposes to consider the cumulative effect
0.3/0/1
1.3/0/3
caused by longstanding marginal periodontitis and dif-
ferent preparation techniques. It takes into account
(featheredge preparation)
that pulp changes are mainly localized and strongly
correlated to the place of origin of the causing irritant
in agreement with the design for human pulp studies
BRD grading
described by Stanley (1968). Therefore, the feath-
eredge preparation and the shoulder preparation were
Area D1
Group 1
0.5/0/1
1.3/0/3
investigated on one tooth, this experimental approach
enables the direct comparison of the histopathological
Irregular irritation dentin
outcome of these techniques on the predamaged pulp.
Regular irritation dentin
The criteria used for the evaluation of the sections are
(mean/min/max)
(mean/min/max)
based on well-defined terms in general pathology (Un-
derwood, 1982) concerning degeneration and regen-
eration, including especially, pulp tissue changes owing
to the physiological ageing process (Schroeder,
1993a,b).
© 2000 Blackwell Science Ltd, Journal of Oral Rehabilitation 27; 93–102
PULP REACTIONS TO CROWN PREPARATIONS 99
The regular irritation dentin formation is a (Brännström & Nyborg, 1971; Mjör, 1974). Tron-
natural phenomenon and a typical feature in early stad & Langeland (1971) proved that bacterial inva-
carious lesions (Gängler, 1996) and following mild sion into opened dentin tubules in omnivorous
physiological abrasion and attrition (Schwarz & Gän- teeth via abrasion is a natural occurring phe-
gler, 1998). In contrast to regular irritation dentin, nomenon. The results of both groups in this study
the irregular irritation dentin formation represents exploiting different preparation techniques con-
the numeric reduction or even loss of odondoblasts, firm experimental studies in pigs, where pulp reac-
and therefore fewer cells and their processes are re- tions correlate better with the material toxicity and
sponsible for dentin formation (Langeland et al., the remaining dentin thickness of dentin than
1975). This is the first sign of degeneration followed with the microbial invasion into dentin tubules
by the formation of fibrodenticles, osteodentin forma- (Schwarz & Gängler, 1998). Because of the non-
tion and/or dentin resorption by activation of odonto- correlation of presence and absence of bacteria with
clasts. Finally, the tissue necrosis of smaller or larger the pulp reactions in both groups, other factors
pulp areas is the degenerative result of crossing are responsible for the intensity of degenerative
the point of no return of cell reactivity. Without changes.
doubt, isolated or confluenting abcesses (grade 4/5) The results document that the remaining dentin
are signs of inflammation and they represent at least thickness is strictly correlated to the severity of
a sublethal trauma of the pulp tissue. In contrast
degenerative parameters while different preparation
to these undoubted degenerative features, isolated
techniques do not demonstrate clearly different
infiltration of chronic and/or acute inflammation cells
endodontal reactions. According to the conclusions
does not characterize per se a degenerative pro-
of Smulson & Sieraski (1989), it is confirmed that
cess. In general pathology, the reversibility of acute
the amount of 2 mm and more remaining dentin
and/or chronic inflammation is well described (Un-
seems to be the critical factor in determining the
derwood, 1982) and a prerequisite of a normal
degree of pulp response. However, in contradiction to
healing process. However, this regenerative poten-
their statement, that the shortest distance between
tial of connective tissue is limited in inflammatory
the prepared dentin margin and the pulp is decisive
pulp responses. This is why the appearance of inflam-
for the severity of inflammatory reactions (Smulson
matory cells to local irritants even in short-term
& Sieraski 1989), it is demonstrated in this study that
biocompatibility testing as defined in ISO/EN 7405
the critical remaining thickness of dentin follows the
(1997) is classified as a potentially degenerative
direction of dentin tubules. From the experi-
process.
Concerning the interpretation of the BRD gradings, mental and control results presented it is concluded
the results of the control group are in agreement that pulp changes due to periodontal disease are
with those of a previous investigation (Zoellner et superimposed by typical mainly degenerative re-
al., 1997) on incisors exhibiting periodontal disease sponses following crown preparation. Different pre-
and occlusal attrition. Pulp reactions due to severe paration techniques and various bacterial invasion
marginal periodontitis are mainly characterized by levels do not correlate with the severity of histo-
extensive regular irritation dentin formation with pathological changes. From a clinical point of view,
some tendency to reduced numbers of odonto- the remaining dentin thickness is the most important
blasts. Therefore, pulp responses to different prepara- factor of the cumulative effects including period-
tion techniques were clearly distinguished concerning ontal disease or type of preparation technique leading
the area as well as the intensity of degenerative to possible endodontal complications after crown
changes. preparation. The application of different preparation
These degenerative reactions my be caused by techniques on one tooth considering not only techni-
bacterial infection due to microleakage occurring un- cal requirements for the crown fabrication but pri-
der crowns fixed with zinc phosphate cement (Gold- marily general and individual morphological tooth
man et al., 1992). However, the influence of bacteria characteristics like enamel and dentin thickness is
as the main irritant is controversially disputed . recommended.
© 2000 Blackwell Science Ltd, Journal of Oral Rehabilitation 27; 93 – 102
100 A. ZOELLNER & P. GAENGLER
Fig. 5. Azan stain ( ×64),
magnification from Fig. 4, irregular
irritation dentin formation (BRD grade
2) at rating point D2.
Table 6. Pulp reactions to different preparation techniques
BRD grading
Group 1 (featheredge preparation) Group 2 (shoulder preparation) Group 3 (control group)
(mean/min/max) (mean/min/max) (mean/min/max)
Regular irritation dentin 0.5/0/1 0.4/0/1 1.2/1/2
Irregular irritation dentin 1.6/0/3 1.8/0/3 0.8/0/1
Resorption 0.1/0/1 0.0/0/0 0.0/0/0
Denticles 0.1/0/1 0.1/0/1 0.5/0/3
Inflammation 0.1/0/1 0.0/0/0 0.0/0/0
Table 7. Pulp reactions and remaining dentin thickness
BRD grading
B2 mm 2–2.5 mm \2.5 mm Control group
(mean/min/max) (mean/min/max) (mean/min/max) (mean/min/max)
Regular irritation dentin 0.0/0/0 0.5/0/1 0.6/0/1 1.1/ 0/1
Irregular irritation dentin 2.8/2/3 1.2/0/3 1.4/0/3 0.8/0/1
Resorption 0.2/0/1 0.0/0/0 0.0/0/0 0.0/0/0
Denticles 0.0/0/0 0.1/0/1 0.1/0/1 0.5/0/3
Inflammation 0.0/0/0 0.0/0/0 0.1/0/1 0.0/0/0
Table 8. Pulp reactions in BRD grading
different areas: featheredge
preparation Crown Margin (D2) Root
(mean/min/max) (mean/min/max) (mean/min/max)
Regular irritation dentin 0.6/0/1 0.4/0/1 0.9/0/1
Irregular irritation dentin 1.5/0/3 1.6/0/3 0.7/0/2
Resorptions 0.0/0/0 0.1/0/1 0.0/0/0
Denticles 0.0/0/0 0.1/0/1 0.0/0/0
Inflammation 0.0/0/0 0.1/0/1 0.0/0/0
© 2000 Blackwell Science Ltd, Journal of Oral Rehabilitation 27; 93–102
P U L P R E A C T I O N S T O C R O WN P R E P AR A T I O N S 101
BRD grading Table 9. Pulp reactions in
different areas: shoulder
Crown Margin (D2) Root preparation
(mean/min/max) (mean/min/max) (mean/min/max)
Regular irritation dentin 0.5/0/1 0.4/0/1 0.6/0/1
Irregular irritation dentin 1.8/0/3 1.8/0/3 1.0/0/2
Resorptions 0.0/0/0 0.0/0/0 0.0/0/0
Denticles 0.0/0/0 0.1/0/1 0.0/0/0
Inflammation 0.0/0/0 0.0/0/0 0.0/0/0
Fig. 6. Azan stain (× 6.25), shoulder
preparation, overview showing a mes-
enchymal pulp tissue with irregular
irritation dentin formation (BRD
grade 1) at rating point D2.
References sium on Operative Dentistry), Nijmegen, Netherlands, pp.
173.
BERGENHOLTZ, G. & NYMAN, S. (1984) Endodontic complications LANGELAND, L., GUTTUSO, J., JEROME, D.R. & LANGELAND, K. (1966)
following periodontal and prosthetic treatment of patients with Histologic and clinical comparison of Addent with silicate
advanced periodontal disease. Journal Periodontology, 55, 63. cements and cold-curing materials. Journal of the American Dental
BRÄNNSTRÖM, M. & NYBORG, H. (1971) The presence of bacteria in Association, 72, 373.
cavities filled with silicate cement and composite resin materials. MJÖR, I.A. (1974) The penetration of bacteria into experimentally
Swedish Dental Journal, 64, 149. exposed human coronal dentin. Scandinavian Journal of Dental
GÄNGLER, P. (1996) Lehrbuch der konservierenden Zahnheilkunde, 3rd Research, 82, 191.
edn, 147. Ullstein Mosby, Berlin. PAMEIJER, C.H. & STANLEY, H.E. (1995) Pulp reactions to a bonding
GOLDMAN, K., LAOSONTHORN, P. & WHITE, R. (1992) Microleak- agent. American Journal of Dentistry, 8, 140.
age-full crowns and dental pulp. Journal of Endodontics, 18, SCHROEDER, H. (1993a) Altersveränderung der Pulpakammer und
473. ihrer Wandung in menschlichen Eckzähnen. Schweizer Monatss-
ISO/EN 7405 (1997) Preclinical evaluation of biocompatibility of chrift Zahnmedizin, 103, 141.
medical devices used in dentistry: test methods. Revision of SCHROEDER, H. (1993b) Altersveränderungen an Zahnhart- und
ISO/TR 7405. Geneva. Weichgeweben des Menschen. Deutsche Zahnärztliche Zeitschrift,
LANGELAND, K., ANDERSON, D.M., COTTON, W.R. and SHKLAIR, I.L. 48, 607.
(1975) Microbiological aspects of dentine caries and their pulpal SCHWARZ, U. & GÄNGLER, P. (1998) Der Einfluß des bakteriellen
sequelae. In: Proceedings of the International Symposium on Mikroleakage an Glasionomerzementfüllungen auf den
Amalgam and Tooth-coloured Restorative Mater. University of Entzündungszustand der Zahnpulpa. Deutsche Zahnärztliche
Nijmegen, Netherlands. Paper presented at OPDENT (Sympo- Zeitschrift, 53, 374.
© 2000 Blackwell Science Ltd, Journal of Oral Rehabilitation 27; 93 – 102
102 A. ZOELLNER & P. GAENGLER
SMULSON, M.H. & SIERASKI, S.M. (1989) Histopathology and studies in human and monkey teeth. Swedish Dental Journal,
diseases of the pulp. In: Endodontic Therapy (ed. F.S. Weine), 39, 1.
4th edn, 134. Mosby Company, St. Louis. ZOELLNER, A., DIPPEL, C. & GAENGLER, P. (1997) Pulpal histo-
STANLEY, H.R. (1968) Design for a human pulp study. I. Oral pathology of incisors exhibiting periodontal disease and oc-
Surgery Oral Medicine Oral Pathology, 25, 633. clusal attrition. Journal Dental Research, 5, 1128.
TRONSTAD, L. & LANGELAND, K. (1971) Effect of attrition on
subjacent dentin and pulp. Journal Dental Research, 50, 17.
UNDERWOOD, J.C.E. (1982) General and Systemic Pathology, 43. Correspondence: Dr. Axel Zöllner, School of Dental Medicine,
Churchill Livingstone, New York. University of Witten/Herdecke, Alfred Herrhausen Str. 50,
WARFINGE, J. (1986) Dental pulp inflammation; experimental 58448 Witten, Germany. E-mail: dagmark@uni-wh.de
© 2000 Blackwell Science Ltd, Journal of Oral Rehabilitation 27; 93–102
You might also like
- PMDC NEB Exam Past PapersDocument29 pagesPMDC NEB Exam Past PapersShawn Parker65% (20)
- PMDC Guidelines For CME PDFDocument12 pagesPMDC Guidelines For CME PDFkhoooban67% (3)
- National Board Questions Pediatric DentistryDocument50 pagesNational Board Questions Pediatric DentistryVerghese George MNo ratings yet
- Primaryandpermanentdiff 161130020329 PDFDocument46 pagesPrimaryandpermanentdiff 161130020329 PDFyour tubeNo ratings yet
- 0 Full Mouth RehabDocument4 pages0 Full Mouth RehabfriciliaNo ratings yet
- Full Mouth Rehabilitation of Early Childhood Caries: A Case ReportDocument4 pagesFull Mouth Rehabilitation of Early Childhood Caries: A Case ReportSKRYBE LOLNo ratings yet
- Retdem Day5.1Document4 pagesRetdem Day5.18xx8pjxfctNo ratings yet
- Of Dental Sciences: Original ArticleDocument4 pagesOf Dental Sciences: Original ArticleIntan Nur FajriNo ratings yet
- Association Between Oral Frailty and SarcopeniaDocument6 pagesAssociation Between Oral Frailty and SarcopeniaJuciara MouraNo ratings yet
- Caries Experience in PrimaryDocument7 pagesCaries Experience in PrimaryRista LewiyonahNo ratings yet
- OAJDS16000237Document5 pagesOAJDS16000237Dr FarhatNo ratings yet
- 20 TH JC - SindhuDocument9 pages20 TH JC - SindhuDadi SindhuNo ratings yet
- Studies On Dental Erosion: An in Vivo-In Vitro Model of Endogenous Dental Erosion - Its Application To Testing Protection by Fluoride Gel ApplicationDocument5 pagesStudies On Dental Erosion: An in Vivo-In Vitro Model of Endogenous Dental Erosion - Its Application To Testing Protection by Fluoride Gel Applicationعبدالعزيز بدرNo ratings yet
- 1.9 Mouth and ThroatDocument1 page1.9 Mouth and ThroatJerreca DasasNo ratings yet
- Early Childhood Caries: A Case Report of An Extensive RehabilitationDocument4 pagesEarly Childhood Caries: A Case Report of An Extensive RehabilitationHanh LeNo ratings yet
- Chlorhexidine Application in Adhesive Procedures: A Meta-Regression AnalysisDocument8 pagesChlorhexidine Application in Adhesive Procedures: A Meta-Regression AnalysisdrvenegascesfamromeralNo ratings yet
- Angle Orthod. 2020 90 1 100-108Document9 pagesAngle Orthod. 2020 90 1 100-108brookortontiaNo ratings yet
- (CR) Early Childhood Caries A Case Report of An Extensive Rehabilitation (2018)Document3 pages(CR) Early Childhood Caries A Case Report of An Extensive Rehabilitation (2018)MuabhiNo ratings yet
- The Up To 21-Year Clinical Outcome and Survival of Feldspathic Porcelain Veneers: Accounting For ClusteringDocument9 pagesThe Up To 21-Year Clinical Outcome and Survival of Feldspathic Porcelain Veneers: Accounting For ClusteringAlexander L. Contreras PairaNo ratings yet
- Goldenfunetal 18 CasoclinicoDocument4 pagesGoldenfunetal 18 Casoclinicotrongnguyen2232000No ratings yet
- Facial Soft Tissue Changes After Nonsurgical Rapid Maxillary Expansion: A Systematic Review and Meta-AnalysisDocument10 pagesFacial Soft Tissue Changes After Nonsurgical Rapid Maxillary Expansion: A Systematic Review and Meta-AnalysismalifaragNo ratings yet
- Assessment of Clinical Success of Three Sealants: Embrace-Wetbond, Clinpro, and Helioseal-F in Permanent Molars: An in Vivo StudyDocument7 pagesAssessment of Clinical Success of Three Sealants: Embrace-Wetbond, Clinpro, and Helioseal-F in Permanent Molars: An in Vivo StudyABNo ratings yet
- Cleft Lip and PalateDocument27 pagesCleft Lip and PalatejolibeecaldonaNo ratings yet
- Dental Age As Indicator of AdolescenceDocument16 pagesDental Age As Indicator of AdolescenceEstaf EmkeyzNo ratings yet
- Genetic Basis of Oral Health Conditions - Alexandre Rezende Vieira - (2019)Document110 pagesGenetic Basis of Oral Health Conditions - Alexandre Rezende Vieira - (2019)Neelesh S JadhavNo ratings yet
- 2020 Martinelli Tongue PositionDocument8 pages2020 Martinelli Tongue PositionYesenia PaisNo ratings yet
- efecte peroxidDocument91 pagesefecte peroxidCatalinBojeNo ratings yet
- 2020 Hadler-Olsen Double Vs Single Primary Tooth Extraction in Interceptive Treatment of Palatally Displaced CaninesDocument7 pages2020 Hadler-Olsen Double Vs Single Primary Tooth Extraction in Interceptive Treatment of Palatally Displaced CaninesDiego Andres Hincapie HerreraNo ratings yet
- 1 s2.0 S1883195813000340 MainDocument5 pages1 s2.0 S1883195813000340 MainMaria FrolaNo ratings yet
- Jad 2021 06 s0513Document13 pagesJad 2021 06 s0513jennifer rodriguezNo ratings yet
- Curve of Spee and Its Relationship With Dentoskeletal MorphologyDocument7 pagesCurve of Spee and Its Relationship With Dentoskeletal MorphologyKanchit SuwanswadNo ratings yet
- Ramos Martins en InglesDocument8 pagesRamos Martins en InglesCamila MillarNo ratings yet
- Outcome of Orthodontic Palatal Plate Therapy For Orofacial Dysfunction in Children With Down Syndrome - A Systematic ReviewDocument7 pagesOutcome of Orthodontic Palatal Plate Therapy For Orofacial Dysfunction in Children With Down Syndrome - A Systematic Reviewnatashanascimento.odontoNo ratings yet
- Surgical OrthodonticsDocument301 pagesSurgical Orthodonticsdr_nilofervevai2360100% (4)
- Bjorl: Cephalometric Evaluation of The Oropharyngeal Space in Children With Atypical DeglutitionDocument6 pagesBjorl: Cephalometric Evaluation of The Oropharyngeal Space in Children With Atypical DeglutitionJudith Alexandra Castro GaeteNo ratings yet
- Resin-Modified Glass Ionomer Cement and A Resin-Based Material As Occlusal SealantsDocument10 pagesResin-Modified Glass Ionomer Cement and A Resin-Based Material As Occlusal Sealantsudingigs2002No ratings yet
- Elgheriani 2003Document5 pagesElgheriani 2003renatamendesodontologiaNo ratings yet
- 21-Podj PDFDocument4 pages21-Podj PDFNgakan OkaNo ratings yet
- Clinical Behavior of Posterior Fixed Partial Dentures With A Biologically Oriented Preparation Technique: A 5-Year Randomized Controlled Clinical TrialDocument7 pagesClinical Behavior of Posterior Fixed Partial Dentures With A Biologically Oriented Preparation Technique: A 5-Year Randomized Controlled Clinical TrialBarbie S.No ratings yet
- Art. Odontoped BDocument8 pagesArt. Odontoped BfarlyblancoNo ratings yet
- Effects of Fixed Labial Orthodontic Appliances On Speech Sound ProductionDocument6 pagesEffects of Fixed Labial Orthodontic Appliances On Speech Sound ProductiondanielaNo ratings yet
- Turkish PopulationDocument5 pagesTurkish PopulationSahana RangarajanNo ratings yet
- Microhardness of Intracoronal Dentin Exposed To BleachingDocument5 pagesMicrohardness of Intracoronal Dentin Exposed To BleachingUnlikely QuestionsNo ratings yet
- ApplegateDocument5 pagesApplegateCristinaNo ratings yet
- Effects of Glass Ionomer Sealants in Newly Erupted First Molars After 5 Years: A Pilot StudyDocument6 pagesEffects of Glass Ionomer Sealants in Newly Erupted First Molars After 5 Years: A Pilot Studypaper kitaNo ratings yet
- Effect of Grape Seed Extract On Remineralization oDocument4 pagesEffect of Grape Seed Extract On Remineralization oGeanel DimarucutNo ratings yet
- Articulo 12Document9 pagesArticulo 12lyes BrionesNo ratings yet
- Pedodontics and Preventive DentistryDocument9 pagesPedodontics and Preventive DentistrySajith KanjiraikalNo ratings yet
- Oral Biofilm Activity Culture Testing and Caries Experience in School Children PDFDocument1 pageOral Biofilm Activity Culture Testing and Caries Experience in School Children PDFAdriana CastilloNo ratings yet
- Bopt PanizDocument9 pagesBopt PanizIvan CarreraNo ratings yet
- Kilic 2021 - Evaluation of The Effects of Different Remineralisation Agents On Initial EnamelDocument9 pagesKilic 2021 - Evaluation of The Effects of Different Remineralisation Agents On Initial EnamelkiabetmotaNo ratings yet
- Does The Presence of Maxillary Midline Diastema Influence The Perception of Dentofacial Esthetics in Video Analysis?Document7 pagesDoes The Presence of Maxillary Midline Diastema Influence The Perception of Dentofacial Esthetics in Video Analysis?parakhrishabh8No ratings yet
- Cecchin 2012Document6 pagesCecchin 2012Stefani TCNo ratings yet
- 2015-IAPD Glasgow Poster Abstracts PDFDocument206 pages2015-IAPD Glasgow Poster Abstracts PDFMirel TomaNo ratings yet
- 2021 Is Sjogren's Syndrome A Risk Factor-Contraindication For Dental Implants An Umbrella ReviewDocument10 pages2021 Is Sjogren's Syndrome A Risk Factor-Contraindication For Dental Implants An Umbrella ReviewmrsilNo ratings yet
- Dexibuprofen PDFDocument6 pagesDexibuprofen PDFAshok KpNo ratings yet
- Bimaxillary Dentoalveolar Protrusion - Traits and Orthodontic CorrectionDocument7 pagesBimaxillary Dentoalveolar Protrusion - Traits and Orthodontic CorrectionAzra NadhiraNo ratings yet
- Indices For Assessment of Periodontal DiseasesDocument107 pagesIndices For Assessment of Periodontal DiseasesShivi KhattriNo ratings yet
- In Vivo Preservation of The Hybrid Layer by Chlorhexidine: Research ReportsDocument5 pagesIn Vivo Preservation of The Hybrid Layer by Chlorhexidine: Research ReportsMayra Ortiz HerreraNo ratings yet
- Journal of Cranio-Maxillo-Facial SurgeryDocument6 pagesJournal of Cranio-Maxillo-Facial SurgeryKihyun YooNo ratings yet
- Oro Motor Articulation ExercicesDocument11 pagesOro Motor Articulation Exercicessudha182kNo ratings yet
- Burbridge2007 NoDocument6 pagesBurbridge2007 NoKatherine VilchezNo ratings yet
- Traumatic Dental Injuries in Children: A Clinical Guide to Management and PreventionFrom EverandTraumatic Dental Injuries in Children: A Clinical Guide to Management and PreventionNo ratings yet
- Orthognathic Surgery As Class III Skeletal TreatmentDocument7 pagesOrthognathic Surgery As Class III Skeletal TreatmentMAYRA ALEJANDRA BAHAMON TRUJILLONo ratings yet
- Mitsiadis 2005Document4 pagesMitsiadis 2005MAYRA ALEJANDRA BAHAMON TRUJILLONo ratings yet
- PIIS0092867424001272Document36 pagesPIIS0092867424001272MAYRA ALEJANDRA BAHAMON TRUJILLONo ratings yet
- Longevity and Reasons For Failure of Sandwich and Total-Etch Posterior Composite Resin RestorationsDocument7 pagesLongevity and Reasons For Failure of Sandwich and Total-Etch Posterior Composite Resin RestorationsMAYRA ALEJANDRA BAHAMON TRUJILLONo ratings yet
- Nihms 1731170Document18 pagesNihms 1731170MAYRA ALEJANDRA BAHAMON TRUJILLONo ratings yet
- 1 s2.0 S221244382100062XDocument6 pages1 s2.0 S221244382100062XMAYRA ALEJANDRA BAHAMON TRUJILLONo ratings yet
- Ultrastructural Correlates of in Vivo/in Vitro Bond Degradation in Self-Etch AdhesivesDocument5 pagesUltrastructural Correlates of in Vivo/in Vitro Bond Degradation in Self-Etch AdhesivesMAYRA ALEJANDRA BAHAMON TRUJILLONo ratings yet
- Structure, Composition, and Mechanical Properties ofDocument5 pagesStructure, Composition, and Mechanical Properties ofMAYRA ALEJANDRA BAHAMON TRUJILLONo ratings yet
- In Uence of Cavity Dimension and Restoration Methods On The Cusp de Ection of Premolars in Composite RestorationDocument8 pagesIn Uence of Cavity Dimension and Restoration Methods On The Cusp de Ection of Premolars in Composite RestorationMAYRA ALEJANDRA BAHAMON TRUJILLONo ratings yet
- Microshear Fatigue Testing of Tooth/Adhesive Interfaces: Marc BraemDocument5 pagesMicroshear Fatigue Testing of Tooth/Adhesive Interfaces: Marc BraemMAYRA ALEJANDRA BAHAMON TRUJILLONo ratings yet
- Of Resin-Dentin Bonds In: DegradationDocument7 pagesOf Resin-Dentin Bonds In: DegradationMAYRA ALEJANDRA BAHAMON TRUJILLONo ratings yet
- 27 ResumenDocument2 pages27 ResumenMAYRA ALEJANDRA BAHAMON TRUJILLONo ratings yet
- In Vivo Preservation of The Hybrid Layer by Chlorhexidine: Research ReportsDocument6 pagesIn Vivo Preservation of The Hybrid Layer by Chlorhexidine: Research ReportsMAYRA ALEJANDRA BAHAMON TRUJILLONo ratings yet
- Bonding To Caries-Affected Dentin: Masatoshi Nakajima, Sitthikorn Kunawarote, Taweesak Prasansuttiporn, Junji TagamiDocument13 pagesBonding To Caries-Affected Dentin: Masatoshi Nakajima, Sitthikorn Kunawarote, Taweesak Prasansuttiporn, Junji TagamiMAYRA ALEJANDRA BAHAMON TRUJILLONo ratings yet
- Effect of Caries-Affected Dentin Hardness On The Shear Bond Strength of Current AdhesivesDocument11 pagesEffect of Caries-Affected Dentin Hardness On The Shear Bond Strength of Current AdhesivesMAYRA ALEJANDRA BAHAMON TRUJILLONo ratings yet
- Bonding To Root Caries by A Self-Etching Adhesive System Containing MDPBDocument3 pagesBonding To Root Caries by A Self-Etching Adhesive System Containing MDPBMAYRA ALEJANDRA BAHAMON TRUJILLONo ratings yet
- Retention of Removable Complete Dentures Made With Different Posterior Palatal Seal Techniques and Oral Health Quality of Life: A Clinical StudyDocument5 pagesRetention of Removable Complete Dentures Made With Different Posterior Palatal Seal Techniques and Oral Health Quality of Life: A Clinical StudyZachary DuongNo ratings yet
- Biologic Width & Emergence ProfileDocument33 pagesBiologic Width & Emergence ProfileNirav RathodNo ratings yet
- Robinson 1915Document14 pagesRobinson 1915SankhyaNo ratings yet
- Dental Morphology (111 RDS) : Lab ManualDocument34 pagesDental Morphology (111 RDS) : Lab ManualNatalia CojocaruNo ratings yet
- September Questions - ابطال الديجيتال PDFDocument164 pagesSeptember Questions - ابطال الديجيتال PDFQq qNo ratings yet
- VeneersDocument54 pagesVeneersjquin3100% (1)
- Journal of Oral and Maxillofacial Surgery, Medicine, and PathologyDocument6 pagesJournal of Oral and Maxillofacial Surgery, Medicine, and PathologyVirginia BujorNo ratings yet
- 108下牙周期末Document10 pages108下牙周期末新手冒險家No ratings yet
- Dentists From New YorkDocument3 pagesDentists From New YorkMD SHAHIN MIANo ratings yet
- CHN ReportDocument16 pagesCHN Reportash aliNo ratings yet
- Minimal Intervention DentistryDocument76 pagesMinimal Intervention DentistryRishab Sharma100% (1)
- 10 1016@j Ijom 2020 03 008Document12 pages10 1016@j Ijom 2020 03 008runit nangaliaNo ratings yet
- Immediate Implant Placement in Molar Extraction Socket A Systematic Review and Meta-AnalysisDocument12 pagesImmediate Implant Placement in Molar Extraction Socket A Systematic Review and Meta-AnalysisrachmadyNo ratings yet
- Brenda Gamez, SDH: Rotation ExperiencesDocument2 pagesBrenda Gamez, SDH: Rotation Experiencesapi-507804349No ratings yet
- Unilateral Removable Partial Dentures: PracticeDocument6 pagesUnilateral Removable Partial Dentures: Practicesekar alifaNo ratings yet
- Castroflorio T. 2013Document7 pagesCastroflorio T. 2013CLAUDIA PATRICIA ROSALES BASANTENo ratings yet
- Dental StainsDocument30 pagesDental StainsArtur Radvanszki100% (1)
- Supportive Periodontal TherapyDocument53 pagesSupportive Periodontal TherapymenaxieNo ratings yet
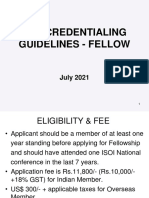
- FellowshipDocument7 pagesFellowshipVivek LathNo ratings yet
- Removable Functional Appliances IIDocument121 pagesRemovable Functional Appliances IIdr_nilofervevai2360100% (1)
- Dental Update - May 2022Document88 pagesDental Update - May 2022Ahmed Abou FoulNo ratings yet
- Oral Hygiene ProjectDocument8 pagesOral Hygiene Projecttanvirahmed0% (1)
- Dental Practice Marketing and Ad 101Document16 pagesDental Practice Marketing and Ad 101D.WorkuNo ratings yet
- Oral Care in IndiaDocument10 pagesOral Care in IndiaSHRINIVAS SNo ratings yet
- MDS Selection ListDocument5 pagesMDS Selection ListMangesh SandeNo ratings yet
- Introduction of PedodonticsDocument27 pagesIntroduction of PedodonticsSudeep M. ChoudharyNo ratings yet