Professional Documents
Culture Documents
Electrolitos y Acido Base DM Correspondencia
Electrolitos y Acido Base DM Correspondencia
Uploaded by
ULICES QUINTANACopyright:
Available Formats
You might also like
- Abfm 2011-2016 Ite ExamsDocument499 pagesAbfm 2011-2016 Ite ExamsJames Moore44% (9)
- Aerobics ManualDocument33 pagesAerobics ManualGabriela Radulescu0% (1)
- List of Medical Triads and Pentads - WikipediaDocument3 pagesList of Medical Triads and Pentads - WikipediaSubhajitPaul100% (1)
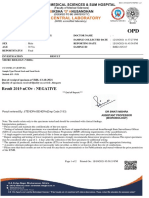
- Patient Name Doctor Name Pat Reg Id Sample Collected Date SEX Reporting Date AGE Sample Id ReportstatusDocument2 pagesPatient Name Doctor Name Pat Reg Id Sample Collected Date SEX Reporting Date AGE Sample Id ReportstatusThushar P kumarNo ratings yet
- Advanced Life Support - A0 PDFDocument1 pageAdvanced Life Support - A0 PDFiulia-uroNo ratings yet
- Perka - Uji BE - Draf 6 Nov 2017Document11 pagesPerka - Uji BE - Draf 6 Nov 2017Rizqi AdistraNo ratings yet
- New England Journal Medicine: The ofDocument15 pagesNew England Journal Medicine: The ofFerry Fawzi AnnorNo ratings yet
- DM 2Document8 pagesDM 2Roberto AlexiNo ratings yet
- Nej Mo A 2306691Document11 pagesNej Mo A 2306691Ulises DantánNo ratings yet
- White NEJM Examine Sep13Document9 pagesWhite NEJM Examine Sep13Kamalia LayalNo ratings yet
- White NEJM Examine Sep13Document9 pagesWhite NEJM Examine Sep13Kamalia LayalNo ratings yet
- Erythrodermic Pemphigus Foliaceus A Rare Refractory Variant 2016Document1 pageErythrodermic Pemphigus Foliaceus A Rare Refractory Variant 2016JohnNo ratings yet
- TRT + DM2Document10 pagesTRT + DM2Dr. Ivan MateusNo ratings yet
- Teplizumab or Snake OilDocument11 pagesTeplizumab or Snake OilChanukya GvNo ratings yet
- Asthma BiologicsDocument10 pagesAsthma BiologicsDmitri KaramazovNo ratings yet
- Cardiovascular and Renal Outcomes With Efpeglenatide in Type 2 DiabetesDocument12 pagesCardiovascular and Renal Outcomes With Efpeglenatide in Type 2 DiabetesAntonella Angulo CruzadoNo ratings yet
- Cardiovascular and Renal Outcomes With Efpeglenatide in Type 2 DiabetesDocument12 pagesCardiovascular and Renal Outcomes With Efpeglenatide in Type 2 DiabetesMoeez AkramNo ratings yet
- Lixisenatide in Patients With Type 2 Diabetes and Acute Coronary SyndromeDocument11 pagesLixisenatide in Patients With Type 2 Diabetes and Acute Coronary SyndromeMoeez AkramNo ratings yet
- Manejo IncidentalomasDocument3 pagesManejo IncidentalomasAlexandra FreireNo ratings yet
- Lixisenatide in Patients With Type 2 Diabetes and Acute Coronary SyndromeDocument11 pagesLixisenatide in Patients With Type 2 Diabetes and Acute Coronary SyndromeAndi Soraya PurnamandaNo ratings yet
- 2008.clin Chem - RantnerDocument7 pages2008.clin Chem - RantnertwkangNo ratings yet
- Fluid Infusion Rates For Pediatric Diabetic Ketoacidosis: David R. Freyer, D.ODocument4 pagesFluid Infusion Rates For Pediatric Diabetic Ketoacidosis: David R. Freyer, D.OFiya Putri ZadaNo ratings yet
- Kushchayeva 2019Document13 pagesKushchayeva 2019pelinNo ratings yet
- Estado Glicometabólico Peso Pessoas NegrasDocument10 pagesEstado Glicometabólico Peso Pessoas NegrasSuiane Costa FerreiraNo ratings yet
- REWIND TrialDocument10 pagesREWIND Trialhenry hernandezNo ratings yet
- A Phase 3 Trial of L-Glutamine in SickleDocument10 pagesA Phase 3 Trial of L-Glutamine in SicklemisheckmkayNo ratings yet
- Hipoglucemia en DBT2Document20 pagesHipoglucemia en DBT2YERIEL ZAMBRANONo ratings yet
- Diagnosis and Management of Glutaric Aciduria Type I - Revised RecommendationsDocument18 pagesDiagnosis and Management of Glutaric Aciduria Type I - Revised RecommendationsMoroianu Irina-GabrielaNo ratings yet
- Barroso 2003Document16 pagesBarroso 2003Yna MoradoNo ratings yet
- TX Lupus ComentarioDocument2 pagesTX Lupus ComentarioGabriel VargasNo ratings yet
- American J Hematol - 2007 - Mistry - Consequences of Diagnostic Delays in Type 1 Gaucher Disease The Need For GreaterDocument6 pagesAmerican J Hematol - 2007 - Mistry - Consequences of Diagnostic Delays in Type 1 Gaucher Disease The Need For GreatererenNo ratings yet
- qt4c13q7gw PDFDocument19 pagesqt4c13q7gw PDFAb Al-mamariNo ratings yet
- Los Loci Genéticos de La Diabetes Tipo 2Document23 pagesLos Loci Genéticos de La Diabetes Tipo 2Cristhian RodriguezNo ratings yet
- Nej Mo A 2307563Document12 pagesNej Mo A 2307563Sussette SánchezNo ratings yet
- Cardiovascular and Renal Outcomes With Empagliflozin in Heart FailureDocument12 pagesCardiovascular and Renal Outcomes With Empagliflozin in Heart FailureSandra PargaNo ratings yet
- Antioxidant Supplementation and Premature Rupture of The Membranes A Planned Secondary AnalysisDocument8 pagesAntioxidant Supplementation and Premature Rupture of The Membranes A Planned Secondary AnalysisizulNo ratings yet
- ALHALLAK 2023 A Pilot Study On The Co Existence of Diabetes and EndometriosisDocument10 pagesALHALLAK 2023 A Pilot Study On The Co Existence of Diabetes and EndometriosisCristiane HermesNo ratings yet
- Example of A Research Paper On DiabetesDocument5 pagesExample of A Research Paper On Diabetesijsgpibkf100% (1)
- Prolonged Therapy of Advanced Chronic Hepatitis C With Low-Dose PeginterferonDocument13 pagesProlonged Therapy of Advanced Chronic Hepatitis C With Low-Dose PeginterferonDwinkha Agita PNo ratings yet
- Hyperemesis Gravidarum Is Not A Negative Contributing Factor For Postpartum Bone Mineral DensityDocument4 pagesHyperemesis Gravidarum Is Not A Negative Contributing Factor For Postpartum Bone Mineral DensityRubiahSheBiachNo ratings yet
- Macroangipatia DiabeticaDocument6 pagesMacroangipatia DiabeticaMarcos Chusin MontesdeocaNo ratings yet
- Toxicity of RadiotherapyDocument6 pagesToxicity of RadiotherapyAlejandra Cejudo MartinezNo ratings yet
- Emailing Expression of KGF-1 and KGF-2 in Skin Wounds ADocument12 pagesEmailing Expression of KGF-1 and KGF-2 in Skin Wounds ARimaWulansariNo ratings yet
- 1 s2.0 S2531137920313067 MainDocument4 pages1 s2.0 S2531137920313067 MainDinda NajwaNo ratings yet
- SPW Diazoxide CholinDocument10 pagesSPW Diazoxide CholinlailagsazNo ratings yet
- Degludec Vs GlargineDocument10 pagesDegludec Vs GlargineJessica ElizabethNo ratings yet
- Statin Intolerance, Bempedoic Acid, and Cardiovascular OutcomesDocument4 pagesStatin Intolerance, Bempedoic Acid, and Cardiovascular OutcomesAnderson Joel GomezNo ratings yet
- Noninvasive Magnetic Resonance Imaging of Microvascular Changes in Type 1 DiabetesDocument6 pagesNoninvasive Magnetic Resonance Imaging of Microvascular Changes in Type 1 DiabetesAndrés Esteban Quezada VenegasNo ratings yet
- Fostamatinib For The Treatment of Warm Antibody Autoimmune Hemolytic Anemia Phase 2Document9 pagesFostamatinib For The Treatment of Warm Antibody Autoimmune Hemolytic Anemia Phase 2Maria Eugenia VelisNo ratings yet
- Nej MC 2201160Document3 pagesNej MC 2201160Πάνος ΣταγήςNo ratings yet
- AAFP 2016 AnswerDocument88 pagesAAFP 2016 AnswerAbdirahman AliNo ratings yet
- Serum Apelin: A New Marker of Early Atherosclerosis in Children With Type 1 Diabetes MellitusDocument5 pagesSerum Apelin: A New Marker of Early Atherosclerosis in Children With Type 1 Diabetes MellitusAssifa RidzkiNo ratings yet
- Ada Cvd-Renalcompendium Fin-WebDocument32 pagesAda Cvd-Renalcompendium Fin-WebJoseph Antonio Apaza GómezNo ratings yet
- Gala Lopez2018Document38 pagesGala Lopez2018Flip Flop ChartNo ratings yet
- Therapeutic Advances in Alcohol Associated HepatitDocument12 pagesTherapeutic Advances in Alcohol Associated HepatitCláudia SilvaNo ratings yet
- Type 2 Diabetes: Remy Boussageon, Matthieu Roustit, Francois Gueyffier, Benoit V Tudrej, Michaela B RehmanDocument1 pageType 2 Diabetes: Remy Boussageon, Matthieu Roustit, Francois Gueyffier, Benoit V Tudrej, Michaela B Rehmaniin setiyanaNo ratings yet
- Nej Mo A 0911123nnnnnnnnDocument11 pagesNej Mo A 0911123nnnnnnnnRoni ArmandaNo ratings yet
- CovidDocument12 pagesCovidSamuel GasparNo ratings yet
- LeaderDocument12 pagesLeaderMoeez AkramNo ratings yet
- HISTOMOROFOMEDocument6 pagesHISTOMOROFOMEMayra PereiraNo ratings yet
- Seminar: Epidemiology and Global Trends in Type 2 DiabetesDocument18 pagesSeminar: Epidemiology and Global Trends in Type 2 DiabetesRoopaNo ratings yet
- CNCR 21619Document7 pagesCNCR 21619Syed Shah MuhammadNo ratings yet
- Gastroparesis: A Comprehensive Approach to Evaluation and ManagementFrom EverandGastroparesis: A Comprehensive Approach to Evaluation and ManagementAnna IbeleNo ratings yet
- Neuroendocrine Tumors: Surgical Evaluation and ManagementFrom EverandNeuroendocrine Tumors: Surgical Evaluation and ManagementJordan M. CloydNo ratings yet
- Torts Digest CasesDocument30 pagesTorts Digest CasesJoshua SantosNo ratings yet
- Deep Vein Thrombosis (DVT) : Education For NursesDocument26 pagesDeep Vein Thrombosis (DVT) : Education For NursesVashNo ratings yet
- Lecture 2 MLTDocument24 pagesLecture 2 MLTAbood dot netNo ratings yet
- Case Presentation On Systemic Lupus Erythematosus (SLE) : Presented By: Mahitha Karimsetti 616175802018 Pharm. D InternDocument35 pagesCase Presentation On Systemic Lupus Erythematosus (SLE) : Presented By: Mahitha Karimsetti 616175802018 Pharm. D Internsrija vijjapuNo ratings yet
- Pnpa Application Form R-2009Document2 pagesPnpa Application Form R-2009Paul BadsNo ratings yet
- Physiology Lecture 3Document28 pagesPhysiology Lecture 3Muhammad Khubaib AzeemNo ratings yet
- RPT 148Document37 pagesRPT 148Christopher Scott RoseNo ratings yet
- Long Acting Injectable Cabotegravir GuideDocument22 pagesLong Acting Injectable Cabotegravir GuidesyafiqjaizNo ratings yet
- Thi thử Anh Chuyên Vĩnh Phúc lần 1 tháng 5-2012Document6 pagesThi thử Anh Chuyên Vĩnh Phúc lần 1 tháng 5-2012Trường Học Số100% (1)
- AIA HS Gold Elite BrochureDocument12 pagesAIA HS Gold Elite BrochureBensam JoysonNo ratings yet
- PneumoniaDocument53 pagesPneumoniaAtif100% (1)
- Karkidaka Rakesh PDFDocument5 pagesKarkidaka Rakesh PDFmail meNo ratings yet
- Cat World January 2019Document84 pagesCat World January 2019Ziad El SamadNo ratings yet
- AmpkDocument9 pagesAmpkEgieAprianNo ratings yet
- Genetic Mutation Research Student HandoutDocument9 pagesGenetic Mutation Research Student Handoutapi-369085916No ratings yet
- Albumin - Globulin RatioDocument6 pagesAlbumin - Globulin RatioaboelqasimkaramNo ratings yet
- Tomotherapy For Cancer Treatment in Chennai - Apollo Proton Cancer CentreDocument1 pageTomotherapy For Cancer Treatment in Chennai - Apollo Proton Cancer CentreShhanya Madan BhatiaNo ratings yet
- An Innovative Technique To Treat Epulis Fissuratum: A Case ReportDocument5 pagesAn Innovative Technique To Treat Epulis Fissuratum: A Case ReportMichelle VelezNo ratings yet
- Herbal Plants Tamil Names and UsesDocument2 pagesHerbal Plants Tamil Names and UsesBalaji Venktesh100% (1)
- Anatomy MCQ SBA eMRCSDocument121 pagesAnatomy MCQ SBA eMRCSTowhid HasanNo ratings yet
- Lab 2Document22 pagesLab 2fgnjdgnNo ratings yet
- Welcome and Business Update Suzanne BarnesDocument21 pagesWelcome and Business Update Suzanne BarnesjthanNo ratings yet
- Family Enterobacteriaceae: By: Paul Aeron E. Bansil, RMTDocument44 pagesFamily Enterobacteriaceae: By: Paul Aeron E. Bansil, RMTMaria Cecilia FloresNo ratings yet
- Approved AbbreviationsDocument5 pagesApproved AbbreviationsAdelNo ratings yet
- Alternatives Jan 29Document40 pagesAlternatives Jan 29alternativesononly100% (3)
- Health Science and Food Choices PTC March 2019Document101 pagesHealth Science and Food Choices PTC March 2019IliaNo ratings yet
Electrolitos y Acido Base DM Correspondencia
Electrolitos y Acido Base DM Correspondencia
Uploaded by
ULICES QUINTANAOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Electrolitos y Acido Base DM Correspondencia
Electrolitos y Acido Base DM Correspondencia
Uploaded by
ULICES QUINTANACopyright:
Available Formats
Correspondence
scenario in favor of the STAN technology, there 1. Westgate J, Harris M, Curnow JS, Greene KR. Plymouth ran-
domized trial of cardiotocogram only versus ST waveform plus
was still no difference in the primary outcome cardiotocogram for intrapartum monitoring in 2400 cases. Am
or the operative-delivery rate. We stand by our J Obstet Gynecol 1993;169:1151-60.
study. 2. Amer-Wåhlin I, Hellsten C, Norén H, et al. Cardiotocogra-
phy only versus cardiotocography plus ST analysis of fetal elec-
Michael A. Belfort, M.D., Ph.D. trocardiogram for intrapartum fetal monitoring: a Swedish ran-
Baylor College of Medicine domised controlled trial. Lancet 2001;358:534-8.
Houston, TX 3. Ojala K, Vääräsmäki M, Mäkikallio K, Valkama M, Tekay A.
belfort@bcm.edu A comparison of intrapartum automated fetal electrocardiogra-
phy and conventional cardiotocography — a randomised con-
George R. Saade, M.D. trolled study. BJOG 2006;113:419-23.
University of Texas Medical Branch 4. Westerhuis ME, Visser GH, Moons KG, et al. Cardiotocogra-
Galveston, TX phy plus ST analysis of fetal electrocardiogram compared with
cardiotocography only for intrapartum monitoring: a random-
Elizabeth A. Thom, Ph.D. ized controlled trial. Obstet Gynecol 2010;115:1173-80.
George Washington University Biostatistics Center 5. FIGO Subcommittee on Standards in Perinatal Medicine.
Washington, DC Guidelines for the use of fetal monitoring. Int J Gynaecol Obstet
1987;25:159-67.
Since publication of their article, the authors report no fur-
ther potential conflict of interest. DOI: 10.1056/NEJMc1513251
Electrolyte and Acid–Base Disturbances in Diabetes Mellitus
To the Editor: Palmer and Clegg (Aug. 6 issue)1 2. Graber ML, Shreeve WW, Ma R-M, Richards J, Pierson RN Jr.
Hyperkalemia in advanced diabetes: potassium retention or cell
provide a comprehensive review of electrolyte transport adaptation? A case control study with body composi-
disturbances in patients with diabetes. To ex- tion analysis. Int J Body Compos Res 2004;2:93-8.
plain the presence of hyperkalemia in patients DOI: 10.1056/NEJMc1511638
with type 4 renal tubular acidosis, the authors
adopt the classic explanation of potassium reten- To the Editor: Palmer and Clegg summarize
tion due to defective potassium secretion; this the major issues regarding electrolyte and acid–
defective secretion has been confirmed in exper- base disturbances in patients with diabetes mel-
iments. litus. Recent studies show that sodium–glucose
To directly test the hypothesis of potassium cotransporter type 2 (SGLT2) inhibitors may also
retention as the explanation for hyperkalemia, lead to ketoacidosis. The Food and Drug Admin-
my colleagues and I measured total-body potas- istration (FDA) recently released a warning re-
sium in a cohort of patients with type 4 renal garding the risk of ketoacidosis associated with
tubular acidosis and found that, if anything, SGLT2 inhibitors.1,2 From March 2013 through
total-body potassium was low in these patients.2 June 2014, the FDA Adverse Event Reporting Sys-
Our result is not consistent with renal potassium tem database identified 20 episodes of acidosis
retention as the major cause of hyperkalemia, associated with SGLT2 inhibitors; these episodes
and it points to a more generalized problem with were reported as ketoacidosis, diabetic ketoaci-
potassium transport in all cells as a more likely dosis, or ketosis.1 All the patients required emer-
explanation that suggests that efforts to augment gency department visits or were hospitalized.
potassium secretion may actually be deleterious if Most cases of ketoacidosis associated with SGLT2
total-body potassium is already low. inhibitors occurred in patients with type 2 diabe-
Mark L. Graber, M.D. tes who had mildly elevated blood glucose con-
centrations, whereas diabetic ketoacidosis was
RTI International
Durham, NC most common in patients with type 1 diabetes
graber.mark@gmail.com who had considerably elevated blood glucose
No potential conflict of interest relevant to this letter was re- concentrations.
ported. It is important to be aware of this potentially
serious complication of SGLT2 inhibitors and
1. Palmer BF, Clegg DJ. Electrolyte and acid–base disturbances
in patients with diabetes mellitus. N Engl J Med 2015;373:548- consider discontinuing these agents in patients
59. who have metabolic acidosis. In addition, it is
n engl j med 373;25 nejm.org December 17, 2015 2481
The New England Journal of Medicine
Downloaded from nejm.org at LATROBE UNIVERSITY on December 18, 2015. For personal use only. No other uses without permission.
Copyright © 2015 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
important that all cases of ketoacidosis involving Martijn C.G.J. Brouwers, Ph.D.
SGLT2 inhibitors be reported to the MedWatch Maastricht University Medical Center
Maastricht, the Netherlands
program of the FDA. martijn.brouwers@maastrichtuniversity.nl
Angela M. Righi, Pharm.D. No potential conflict of interest relevant to this letter was re-
Michael J. Peeters, Pharm.D. ported.
University of Toledo Medical Center 1. Murphy R, Turnbull DM, Walker M, Hattersley AT. Clinical
Toledo, OH features, diagnosis and management of maternally inherited
angela.righi@utoledo.edu diabetes and deafness (MIDD) associated with the 3243A>G mito-
chondrial point mutation. Diabet Med 2008;25:383-99.
Bryan Dotson, Pharm.D. 2. Madiraju AK, Erion DM, Rahimi Y, et al. Metformin sup-
Harper University Hospital presses gluconeogenesis by inhibiting mitochondrial glycero-
Detroit, MI phosphate dehydrogenase. Nature 2014;510:542-6.
3. Brouwers MC, Ham JC, Wisse E, et al. Elevated lactate levels
No potential conflict of interest relevant to this letter was re-
in patients with poorly regulated type 1 diabetes and glycogenic
ported.
hepatopathy: a new feature of Mauriac syndrome. Diabetes Care
2015;38:e11-2.
1. FDA drug safety communication: FDA warns that SGLT2 in-
hibitors for diabetes may result in a serious condition of too DOI: 10.1056/NEJMc1511638
much acid in the blood. May 15, 2015 (http://www .fda
.gov/
Drugs/DrugSafety/ucm446845.htm).
2. Taylor SI, Blau JE, Rother KI. SGLT2 inhibitors may predis-
pose to ketoacidosis. J Clin Endocrinol Metab 2015;100:2849-52. To the Editor: A simpler and potentially more
reliable clinical approach to determine whether
DOI: 10.1056/NEJMc1511638
the lower sodium concentration is purely dilu-
tional after hyperglycemia-induced osmotic fluid
To the Editor: In their article, Palmer and Clegg shifts involves the estimation of the effective os-
rightfully mention ketoacidosis and metformin molality (or tonicity), in milliosmoles per kilo-
use as potential causes of lactic acidosis in pa- gram, calculated as (2 × [Na+]) + ([glucose] ÷ 18),
tients with diabetes. However, physicians may where Na+ denotes sodium (measured in milli-
encounter other diabetes-related causes of hyper- moles per liter) and glucose is measured in mil-
lactatemia. ligrams per deciliter.1 In patients with euvolemic
First, maternally inherited diabetes and deaf- hyperglycemia, the smaller contribution of a
ness and the syndrome of mitochondrial en- lower sodium concentration to the osmolality is
cephalomyopathy, lactic acidosis, and strokelike offset by an increased contribution to the osmo-
episodes are overlapping mitochondrial syn- lality by the elevated glucose concentration. An
dromes, both of which are caused by the effective osmolality that deviates from the nor-
m.3243A→G mutation. It is estimated that ap- mal range indicates an abnormal hydration sta-
proximately 1% of all patients with diabetes have tus. Patients with dehydration have an elevated
this mutation.1 Metformin may aggravate hyper- effective osmolality reflecting the free-water
lactatemia in these patients, since it also affects deficit, whereas patients with excess free water
intracellular redox potential.2 Indeed, the plasma would have a lower-than-normal effective osmo-
lactate level was substantially elevated (to 7.8 mmol lality and could be expected to have persistent
per liter) and subsequently decreased (but did hyponatremia, even after correction of the hyper-
not normalize) after discontinuation of metfor- glycemia.
min in one of my patients who had maternally Sumit Mohan, M.D., M.P.H.
inherited diabetes and deafness. Columbia University Medical Center
Second, my colleagues and I recently observed New York, NY
elevated plasma lactate levels (up to 10 mmol per sm2206@cumc.columbia.edu
liter) in young adult patients with poorly con- No potential conflict of interest relevant to this letter was re-
ported.
trolled type 1 diabetes and glycogenic hepa-
topathy. Additional analyses suggested that the 1. Gennari FJ. Serum osmolality: uses and limitations. N Engl
hyperlactatemia was caused by an acquired mito- J Med 1984;310:102-5.
chondrial defect, most likely because of poor DOI: 10.1056/NEJMc1511638
glucose control, since plasma lactate levels re-
turned to normal levels after strict glucose The authors reply: Graber cites studies involv-
regulation.3 ing patients with advanced diabetes that suggest
2482 n engl j med 373;25 nejm.org December 17, 2015
The New England Journal of Medicine
Downloaded from nejm.org at LATROBE UNIVERSITY on December 18, 2015. For personal use only. No other uses without permission.
Copyright © 2015 Massachusetts Medical Society. All rights reserved.
Correspondence
that hyperkalemia caused by impaired renal ex- contrast, the osmotic diuretic effect can worsen
cretion is not reflective of increased body stores renal function and cause hyperkalemia, particu-
but may occur with decreased total-body potas- larly when administered to patients with hypo-
sium content. A poor correlation exists between volemia who are receiving blockers of the renin–
the plasma potassium concentration and total- angiotensin–aldosterone system.
body potassium content.1 Techniques that in- We agree with Brouwers that lactic acidosis
clude skeletal-muscle biopsies indicate that body that is not easily explainable in a patient with
stores of potassium are either normal or reduced diabetes mellitus may occur. Such cases should
in patients with chronic kidney disease.2 These prompt consideration of more unusual causes.
contradictory results may be reconciled by con- Mohan argues that calculation of effective
sidering the clinical setting. For example, a true osmolality is potentially a more reliable approach
potassium deficit, correctable by potassium sup- to estimate changes in the sodium concentra-
plements, occurs during the course of advancing tion after normalization of plasma glucose con-
renal failure when it is accompanied by vomiting, centrations. This equation may provide a rapid
high-dose diuretic therapy, and low potassium initial clue as to the patient’s hydration status.
intake. Abnormalities of membrane transport However, like other correction factors, the equa-
occur in renal failure, impairing the ability to tion lacks precision because it does not account
maintain a normal intracellular potassium con- for the 4 to 5 liters of intracellular water in tissues
tent. Stores that are decreased because of this where glucose uptake is not insulin-dependent
mechanism are not correctable with the use of and the effects of volume status on the transfer
potassium supplements. Total-body potassium of fluid from the intracellular into the extracel-
deficits that are refractory to supplements also lular space. These issues are discussed more
occur with decreased muscle mass in patients in fully in the Supplementary Appendix, available
whom the cellular potassium concentration is with the full text of our article at NEJM.org.
normal. These various types of low reserves fre- Biff F. Palmer, M.D.
quently coexist, making any generalized conclu- University of Texas Southwestern Medical Center
sion regarding body stores difficult. Dallas, TX
A thorough investigation of precipitating biff.palmer@utsouthwestern.edu
events is of critical importance in the manage- Deborah J. Clegg, Ph.D
ment of hyperglycemic crises. In this regard, Cedars–Sinai Medical Center
Righi et al. call attention to recent reports link- Beverly Hills, CA
ing the use of SGLT2 inhibitors to the onset of Since publication of their article, the authors report no fur-
ther potential conflict of interest.
diabetic ketoacidosis. Inhibition of glucose–
sodium cotransport by these drugs increases 1. van Ypersele de Strihou C. Potassium homeostasis in renal
both the flow and delivery of sodium to the failure. Kidney Int 1977;11:491-504.
2. Palmer BF. Potassium metabolism in chronic kidney dis-
distal nephron, yet renal potassium wasting and ease. In:Kimmel P, Rosenberg M, eds. Chronic renal disease.
hypokalemia have not been major side effects. New York:Elsevier, 2015:381-90.
Decreased aldosterone levels due to inhibition of 3. Thomson SC, Rieg T, Miracle C, et al. Acute and chronic ef-
fects of SGLT2 blockade on glomerular and tubular function in
renin release through tubuloglomerular feed- the early diabetic rat. Am J Physiol Regul Integr Comp Physiol
back, the use of renin–angiotensin system block- 2012;302:R75-R83.
ers, or both probably account for this effect.3 In DOI: 10.1056/NEJMc1511638
Examination of the Retina
To the Editor: As students of medicine, we sented. In particular, we raise concerns regard-
found the video “Examination of the Retina”1 ing the recommendation that clinical suspicion
and accompanying text to be helpful to our during direct funduscopy warrants an ophthal-
understanding of this basic clinical examination. mic referral for a dilated-eye examination. Screen-
However, we wonder about the indications to ing retinal examinations with a dilated pupil can
perform a dilated-eye examination that were pre- be safely performed in primary care.
n engl j med 373;25 nejm.org December 17, 2015 2483
The New England Journal of Medicine
Downloaded from nejm.org at LATROBE UNIVERSITY on December 18, 2015. For personal use only. No other uses without permission.
Copyright © 2015 Massachusetts Medical Society. All rights reserved.
You might also like
- Abfm 2011-2016 Ite ExamsDocument499 pagesAbfm 2011-2016 Ite ExamsJames Moore44% (9)
- Aerobics ManualDocument33 pagesAerobics ManualGabriela Radulescu0% (1)
- List of Medical Triads and Pentads - WikipediaDocument3 pagesList of Medical Triads and Pentads - WikipediaSubhajitPaul100% (1)
- Patient Name Doctor Name Pat Reg Id Sample Collected Date SEX Reporting Date AGE Sample Id ReportstatusDocument2 pagesPatient Name Doctor Name Pat Reg Id Sample Collected Date SEX Reporting Date AGE Sample Id ReportstatusThushar P kumarNo ratings yet
- Advanced Life Support - A0 PDFDocument1 pageAdvanced Life Support - A0 PDFiulia-uroNo ratings yet
- Perka - Uji BE - Draf 6 Nov 2017Document11 pagesPerka - Uji BE - Draf 6 Nov 2017Rizqi AdistraNo ratings yet
- New England Journal Medicine: The ofDocument15 pagesNew England Journal Medicine: The ofFerry Fawzi AnnorNo ratings yet
- DM 2Document8 pagesDM 2Roberto AlexiNo ratings yet
- Nej Mo A 2306691Document11 pagesNej Mo A 2306691Ulises DantánNo ratings yet
- White NEJM Examine Sep13Document9 pagesWhite NEJM Examine Sep13Kamalia LayalNo ratings yet
- White NEJM Examine Sep13Document9 pagesWhite NEJM Examine Sep13Kamalia LayalNo ratings yet
- Erythrodermic Pemphigus Foliaceus A Rare Refractory Variant 2016Document1 pageErythrodermic Pemphigus Foliaceus A Rare Refractory Variant 2016JohnNo ratings yet
- TRT + DM2Document10 pagesTRT + DM2Dr. Ivan MateusNo ratings yet
- Teplizumab or Snake OilDocument11 pagesTeplizumab or Snake OilChanukya GvNo ratings yet
- Asthma BiologicsDocument10 pagesAsthma BiologicsDmitri KaramazovNo ratings yet
- Cardiovascular and Renal Outcomes With Efpeglenatide in Type 2 DiabetesDocument12 pagesCardiovascular and Renal Outcomes With Efpeglenatide in Type 2 DiabetesAntonella Angulo CruzadoNo ratings yet
- Cardiovascular and Renal Outcomes With Efpeglenatide in Type 2 DiabetesDocument12 pagesCardiovascular and Renal Outcomes With Efpeglenatide in Type 2 DiabetesMoeez AkramNo ratings yet
- Lixisenatide in Patients With Type 2 Diabetes and Acute Coronary SyndromeDocument11 pagesLixisenatide in Patients With Type 2 Diabetes and Acute Coronary SyndromeMoeez AkramNo ratings yet
- Manejo IncidentalomasDocument3 pagesManejo IncidentalomasAlexandra FreireNo ratings yet
- Lixisenatide in Patients With Type 2 Diabetes and Acute Coronary SyndromeDocument11 pagesLixisenatide in Patients With Type 2 Diabetes and Acute Coronary SyndromeAndi Soraya PurnamandaNo ratings yet
- 2008.clin Chem - RantnerDocument7 pages2008.clin Chem - RantnertwkangNo ratings yet
- Fluid Infusion Rates For Pediatric Diabetic Ketoacidosis: David R. Freyer, D.ODocument4 pagesFluid Infusion Rates For Pediatric Diabetic Ketoacidosis: David R. Freyer, D.OFiya Putri ZadaNo ratings yet
- Kushchayeva 2019Document13 pagesKushchayeva 2019pelinNo ratings yet
- Estado Glicometabólico Peso Pessoas NegrasDocument10 pagesEstado Glicometabólico Peso Pessoas NegrasSuiane Costa FerreiraNo ratings yet
- REWIND TrialDocument10 pagesREWIND Trialhenry hernandezNo ratings yet
- A Phase 3 Trial of L-Glutamine in SickleDocument10 pagesA Phase 3 Trial of L-Glutamine in SicklemisheckmkayNo ratings yet
- Hipoglucemia en DBT2Document20 pagesHipoglucemia en DBT2YERIEL ZAMBRANONo ratings yet
- Diagnosis and Management of Glutaric Aciduria Type I - Revised RecommendationsDocument18 pagesDiagnosis and Management of Glutaric Aciduria Type I - Revised RecommendationsMoroianu Irina-GabrielaNo ratings yet
- Barroso 2003Document16 pagesBarroso 2003Yna MoradoNo ratings yet
- TX Lupus ComentarioDocument2 pagesTX Lupus ComentarioGabriel VargasNo ratings yet
- American J Hematol - 2007 - Mistry - Consequences of Diagnostic Delays in Type 1 Gaucher Disease The Need For GreaterDocument6 pagesAmerican J Hematol - 2007 - Mistry - Consequences of Diagnostic Delays in Type 1 Gaucher Disease The Need For GreatererenNo ratings yet
- qt4c13q7gw PDFDocument19 pagesqt4c13q7gw PDFAb Al-mamariNo ratings yet
- Los Loci Genéticos de La Diabetes Tipo 2Document23 pagesLos Loci Genéticos de La Diabetes Tipo 2Cristhian RodriguezNo ratings yet
- Nej Mo A 2307563Document12 pagesNej Mo A 2307563Sussette SánchezNo ratings yet
- Cardiovascular and Renal Outcomes With Empagliflozin in Heart FailureDocument12 pagesCardiovascular and Renal Outcomes With Empagliflozin in Heart FailureSandra PargaNo ratings yet
- Antioxidant Supplementation and Premature Rupture of The Membranes A Planned Secondary AnalysisDocument8 pagesAntioxidant Supplementation and Premature Rupture of The Membranes A Planned Secondary AnalysisizulNo ratings yet
- ALHALLAK 2023 A Pilot Study On The Co Existence of Diabetes and EndometriosisDocument10 pagesALHALLAK 2023 A Pilot Study On The Co Existence of Diabetes and EndometriosisCristiane HermesNo ratings yet
- Example of A Research Paper On DiabetesDocument5 pagesExample of A Research Paper On Diabetesijsgpibkf100% (1)
- Prolonged Therapy of Advanced Chronic Hepatitis C With Low-Dose PeginterferonDocument13 pagesProlonged Therapy of Advanced Chronic Hepatitis C With Low-Dose PeginterferonDwinkha Agita PNo ratings yet
- Hyperemesis Gravidarum Is Not A Negative Contributing Factor For Postpartum Bone Mineral DensityDocument4 pagesHyperemesis Gravidarum Is Not A Negative Contributing Factor For Postpartum Bone Mineral DensityRubiahSheBiachNo ratings yet
- Macroangipatia DiabeticaDocument6 pagesMacroangipatia DiabeticaMarcos Chusin MontesdeocaNo ratings yet
- Toxicity of RadiotherapyDocument6 pagesToxicity of RadiotherapyAlejandra Cejudo MartinezNo ratings yet
- Emailing Expression of KGF-1 and KGF-2 in Skin Wounds ADocument12 pagesEmailing Expression of KGF-1 and KGF-2 in Skin Wounds ARimaWulansariNo ratings yet
- 1 s2.0 S2531137920313067 MainDocument4 pages1 s2.0 S2531137920313067 MainDinda NajwaNo ratings yet
- SPW Diazoxide CholinDocument10 pagesSPW Diazoxide CholinlailagsazNo ratings yet
- Degludec Vs GlargineDocument10 pagesDegludec Vs GlargineJessica ElizabethNo ratings yet
- Statin Intolerance, Bempedoic Acid, and Cardiovascular OutcomesDocument4 pagesStatin Intolerance, Bempedoic Acid, and Cardiovascular OutcomesAnderson Joel GomezNo ratings yet
- Noninvasive Magnetic Resonance Imaging of Microvascular Changes in Type 1 DiabetesDocument6 pagesNoninvasive Magnetic Resonance Imaging of Microvascular Changes in Type 1 DiabetesAndrés Esteban Quezada VenegasNo ratings yet
- Fostamatinib For The Treatment of Warm Antibody Autoimmune Hemolytic Anemia Phase 2Document9 pagesFostamatinib For The Treatment of Warm Antibody Autoimmune Hemolytic Anemia Phase 2Maria Eugenia VelisNo ratings yet
- Nej MC 2201160Document3 pagesNej MC 2201160Πάνος ΣταγήςNo ratings yet
- AAFP 2016 AnswerDocument88 pagesAAFP 2016 AnswerAbdirahman AliNo ratings yet
- Serum Apelin: A New Marker of Early Atherosclerosis in Children With Type 1 Diabetes MellitusDocument5 pagesSerum Apelin: A New Marker of Early Atherosclerosis in Children With Type 1 Diabetes MellitusAssifa RidzkiNo ratings yet
- Ada Cvd-Renalcompendium Fin-WebDocument32 pagesAda Cvd-Renalcompendium Fin-WebJoseph Antonio Apaza GómezNo ratings yet
- Gala Lopez2018Document38 pagesGala Lopez2018Flip Flop ChartNo ratings yet
- Therapeutic Advances in Alcohol Associated HepatitDocument12 pagesTherapeutic Advances in Alcohol Associated HepatitCláudia SilvaNo ratings yet
- Type 2 Diabetes: Remy Boussageon, Matthieu Roustit, Francois Gueyffier, Benoit V Tudrej, Michaela B RehmanDocument1 pageType 2 Diabetes: Remy Boussageon, Matthieu Roustit, Francois Gueyffier, Benoit V Tudrej, Michaela B Rehmaniin setiyanaNo ratings yet
- Nej Mo A 0911123nnnnnnnnDocument11 pagesNej Mo A 0911123nnnnnnnnRoni ArmandaNo ratings yet
- CovidDocument12 pagesCovidSamuel GasparNo ratings yet
- LeaderDocument12 pagesLeaderMoeez AkramNo ratings yet
- HISTOMOROFOMEDocument6 pagesHISTOMOROFOMEMayra PereiraNo ratings yet
- Seminar: Epidemiology and Global Trends in Type 2 DiabetesDocument18 pagesSeminar: Epidemiology and Global Trends in Type 2 DiabetesRoopaNo ratings yet
- CNCR 21619Document7 pagesCNCR 21619Syed Shah MuhammadNo ratings yet
- Gastroparesis: A Comprehensive Approach to Evaluation and ManagementFrom EverandGastroparesis: A Comprehensive Approach to Evaluation and ManagementAnna IbeleNo ratings yet
- Neuroendocrine Tumors: Surgical Evaluation and ManagementFrom EverandNeuroendocrine Tumors: Surgical Evaluation and ManagementJordan M. CloydNo ratings yet
- Torts Digest CasesDocument30 pagesTorts Digest CasesJoshua SantosNo ratings yet
- Deep Vein Thrombosis (DVT) : Education For NursesDocument26 pagesDeep Vein Thrombosis (DVT) : Education For NursesVashNo ratings yet
- Lecture 2 MLTDocument24 pagesLecture 2 MLTAbood dot netNo ratings yet
- Case Presentation On Systemic Lupus Erythematosus (SLE) : Presented By: Mahitha Karimsetti 616175802018 Pharm. D InternDocument35 pagesCase Presentation On Systemic Lupus Erythematosus (SLE) : Presented By: Mahitha Karimsetti 616175802018 Pharm. D Internsrija vijjapuNo ratings yet
- Pnpa Application Form R-2009Document2 pagesPnpa Application Form R-2009Paul BadsNo ratings yet
- Physiology Lecture 3Document28 pagesPhysiology Lecture 3Muhammad Khubaib AzeemNo ratings yet
- RPT 148Document37 pagesRPT 148Christopher Scott RoseNo ratings yet
- Long Acting Injectable Cabotegravir GuideDocument22 pagesLong Acting Injectable Cabotegravir GuidesyafiqjaizNo ratings yet
- Thi thử Anh Chuyên Vĩnh Phúc lần 1 tháng 5-2012Document6 pagesThi thử Anh Chuyên Vĩnh Phúc lần 1 tháng 5-2012Trường Học Số100% (1)
- AIA HS Gold Elite BrochureDocument12 pagesAIA HS Gold Elite BrochureBensam JoysonNo ratings yet
- PneumoniaDocument53 pagesPneumoniaAtif100% (1)
- Karkidaka Rakesh PDFDocument5 pagesKarkidaka Rakesh PDFmail meNo ratings yet
- Cat World January 2019Document84 pagesCat World January 2019Ziad El SamadNo ratings yet
- AmpkDocument9 pagesAmpkEgieAprianNo ratings yet
- Genetic Mutation Research Student HandoutDocument9 pagesGenetic Mutation Research Student Handoutapi-369085916No ratings yet
- Albumin - Globulin RatioDocument6 pagesAlbumin - Globulin RatioaboelqasimkaramNo ratings yet
- Tomotherapy For Cancer Treatment in Chennai - Apollo Proton Cancer CentreDocument1 pageTomotherapy For Cancer Treatment in Chennai - Apollo Proton Cancer CentreShhanya Madan BhatiaNo ratings yet
- An Innovative Technique To Treat Epulis Fissuratum: A Case ReportDocument5 pagesAn Innovative Technique To Treat Epulis Fissuratum: A Case ReportMichelle VelezNo ratings yet
- Herbal Plants Tamil Names and UsesDocument2 pagesHerbal Plants Tamil Names and UsesBalaji Venktesh100% (1)
- Anatomy MCQ SBA eMRCSDocument121 pagesAnatomy MCQ SBA eMRCSTowhid HasanNo ratings yet
- Lab 2Document22 pagesLab 2fgnjdgnNo ratings yet
- Welcome and Business Update Suzanne BarnesDocument21 pagesWelcome and Business Update Suzanne BarnesjthanNo ratings yet
- Family Enterobacteriaceae: By: Paul Aeron E. Bansil, RMTDocument44 pagesFamily Enterobacteriaceae: By: Paul Aeron E. Bansil, RMTMaria Cecilia FloresNo ratings yet
- Approved AbbreviationsDocument5 pagesApproved AbbreviationsAdelNo ratings yet
- Alternatives Jan 29Document40 pagesAlternatives Jan 29alternativesononly100% (3)
- Health Science and Food Choices PTC March 2019Document101 pagesHealth Science and Food Choices PTC March 2019IliaNo ratings yet