Professional Documents
Culture Documents
GI - Surgical Aspects of The Esophagus
GI - Surgical Aspects of The Esophagus
Uploaded by
jalexander10060 ratings0% found this document useful (0 votes)
6 views3 pagesThis document summarizes various esophageal diseases including their location, causes, symptoms, diagnosis, and treatment. It covers hiatal hernias, achalasia, esophageal diverticula, and esophageal neoplasms. The main points are:
1) Type I hiatal hernias are the most common, often in overweight women, and cause reflux that can lead to erosion, ulcers, scarring, and strictures. Treatment focuses on lifestyle changes and medications to reduce reflux.
2) Achalasia is a failure of the lower esophageal sphincter to relax, causing painless dysphagia and regurgitation. It is diagnosed via manometry and treated with
Original Description:
Original Title
GI- Surgical Aspects of the Esophagus.docx
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThis document summarizes various esophageal diseases including their location, causes, symptoms, diagnosis, and treatment. It covers hiatal hernias, achalasia, esophageal diverticula, and esophageal neoplasms. The main points are:
1) Type I hiatal hernias are the most common, often in overweight women, and cause reflux that can lead to erosion, ulcers, scarring, and strictures. Treatment focuses on lifestyle changes and medications to reduce reflux.
2) Achalasia is a failure of the lower esophageal sphincter to relax, causing painless dysphagia and regurgitation. It is diagnosed via manometry and treated with
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
0 ratings0% found this document useful (0 votes)
6 views3 pagesGI - Surgical Aspects of The Esophagus
GI - Surgical Aspects of The Esophagus
Uploaded by
jalexander1006This document summarizes various esophageal diseases including their location, causes, symptoms, diagnosis, and treatment. It covers hiatal hernias, achalasia, esophageal diverticula, and esophageal neoplasms. The main points are:
1) Type I hiatal hernias are the most common, often in overweight women, and cause reflux that can lead to erosion, ulcers, scarring, and strictures. Treatment focuses on lifestyle changes and medications to reduce reflux.
2) Achalasia is a failure of the lower esophageal sphincter to relax, causing painless dysphagia and regurgitation. It is diagnosed via manometry and treated with
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
You are on page 1of 3
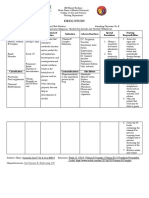
GI- Surgical Aspects of Esophageal Disease
Type/Location Cause Symptoms Diagnosis Treatment & Recurrence
HIATAL HERNIA
Type I- Sliding -Type I are more common -LES becomes incompetent and -many pts have no symptoms -suspected based on pt hx -avoid gastric stimulants
than type to by 100:1 gastric juice reflux produces a -can cause a burning epigastric or -weight loss is a feature die to -eliminate tight garments that
-predominantly in women chemical burn in the esophagus substernal pain/tightness distal esophageal stricture) ↑ intra-abdominal P
who have been pregnant -degree of mucosal injury is due to -can be confused with MI, but -hh’s and reflux esophagitis can be -do not eat/drink within
-men and women due to ↑ duration of acid contact and NOT usually pain does not radiate confirmed by fluoroscopy during a several hrs of sleeping
intra-abdominal P a disease of hyperacidity -continued inflammation of the barium swallow -sleep with the head of the bed
-Type I hiatal hernias are distal esophagus may lead to: -esophagogastric endoscopy and elevated at least 6in
often in overweight pts 1. mucosal erosion biopsy of inflamed esophagus -weight loss in obese pts
2. unlceration -manometry may show a loss of the -regular use of antacids to
3. scarring lower esophageal high pressure provide steady protection
4. stricutre area -H blockers (increase the pH
-other presentations: of the gastric juice reflux)
3. lump or feeling that food is -metoclopramide (may be
stuck beneath the xiphoid helpful when poor gastric
2. worse when the patient is emptying is a symptom)
supine or leaning over *1/3 of pts don’t respond to
3. antacid therapy frequently medical tx and ½ of those
improves the symptoms who respond will relapse and
4. alcohol, aspirin, tobacco, require surgery
and caffeine exacerbate sxs -surgery: correct anatomic
5. late dysphagia & vomiting defect and prevent reflux
usually suggest strictures (reconstruction of a valve)
Type II- -generally show no symptoms until *complications of surgery:
Para-Esophageal they incarcerate and become 1. dysphagia
ischemic 2. gas-bloat syndrome:
-symptoms present include: inability to belch/vomit
1. dysphagia 3. disruption of the repair
2. bleeding (recurrent symptoms)
3. occasional resp. distress 4. intra-abd infection
5. esophageal perforation
6. splenic injury
MOTILITY
DISORDER
Achalasia -failure of high-P zone -painless dysphagia -1st confirmed -medical tx has generally not
(LES) sphincter to relax -progressive dilation of the roentgeno-graphically by contrast been helpful
-not due to spasm proximal esophagus studies (“bird beak” appearance) -invasive endoscopy (forceful
-regurg. of undigested food and -dilation of proximal esophagus & dilation)
spitting up foul smelling poss. diverticula at any level -esophageal myotomy
secretions on leaning forward -endoscopy (must be careful to (surgical transection of m)
-weight loss avoid diverticular perforations)
-aspiration pneumonia -esophageal manometry
GI- Surgical Aspects of Esophageal Disease
Diverticulum -2nd most common of the -distal 1/3 of esophagus: -pulsion diverticula complain of: -pulsion: excision of the
-Pulsion esoph. motility disorders esophagogastric jxn problem due 1. regurgitation of recently diverticula and myotomy of
(Cervical/Zenker’s) -either pulsion or traction to chronic stricture from: swallowed food or pills the cricopharyngeal m.
-Traction depending on the mech that 1. acid reflux 2. choking *excision should always be
causes development 2. anti-reflux surgery 3. putrid breath odor accompanied by correction of
-pulsion diverticula are 3. achalasia underlying path process
related to dysfunction of
the cricopharyngeal m. -middle 1/3: almost always traction -traction: asymptomatic -traction: don’t need tx
(not related to an intrinsic
abnormality in esoph. motility),
caused by:
1. mediastinal inflammation
(inflam. nodal dis. from TB)
2. histoplasmosis (results in
scar formationcontracture
traction on esophagus)
NEOPLASMS
Benign -exceedingly rare -leiomyoma: grow progressively -leiomyoma: indent the lumen of
-Leiomyoma -leiomyomas are the most and cause dysphagia the esoph. on contrast study
common intramural tumors
(potential for malignant
degeneration is low)
Malignant -usually arises from -commonly occurs in black men in -symptoms have insidious onset, -barium contrast of the esoph. -very poor prognosis (both)
-Squamous cell c squamous epithelium association with alcohol and/or precluding early diagnosis and the *apple core lesion is -upper esophageal cancer:
-Adenocarcinoma tobacco abuse opportunity for effective tx patho-gnomonic of esoph radiotherapy is the 1˚ tx
-in other parts of the world the -as the tumor enlarges progressive carcinoma (usually requires extirpation
etiology has been related to: dysphagia becomes the -endoscopy and biopsy of lesion of esoph. en bloc w/the
1. diet predominant symptom -CT of chest and upper abdomen is larynx, permanent
2. vitamin deficiency -other symptoms: used to assess the extent of tumor tracheostomy, and restoration
3. poor oral hygiene 1. pain involvement (important to stage of swallowing- palliation)
4. surgical procedures 2. weight loss the disease) -middle 1/3: tx by a staged
5. # of premalignancies 3. difficulty swallowing procedure w/total thoracic
(burns, barrett esophagitis, 4. acquired tracheaesophageal esophagectomy & bypass
radiation, P-V syndrome, fistula (due to erosion of the -lower 1/3: esophagogastric
and esophageal diverticula) tumor in trachea/bronchus) resection & end-to-end
~10% of pts with Barrett’s develop 5. frequent pneumonia (due to anastomosis in mid chest
adenocarcinoma recurrent aspiration)
DIAPHRAGMATIC
HERNIA
Bochdalek
Larrey
TRAUMATIC
DISORDERS
Traumatic Rupture of
GI- Surgical Aspects of Esophageal Disease
the Diaphragm
Esophageal -instrumentation by endoscopic -sxs of Boerhaave’s syndrome: -tx requires aggressive surgical
Perforation and/or biopsy 1. draumatic or occult intervention
-blind nasogastric tubes 2. profound shock
-instuments designed for dilation of 3. mediastinal sepsis
strictures 4. severe chest or abd pain
-Sengstaken-Blakemore tubes 5. hypotension
(balloon dilation for achalasia) 6. diaphoresis
-Boerhaave’s syndrome 7. nausea/vomiting
(spontaneous perforation
secondary to forceful vomiting)
Ingestion of Casutic *medical emergency -alkaline containing products -inspect mouth to assess injury -neutralization and induced
Materials (drano, liquid plummer, etc.) emesis not recommended
-corrosive gastritis: due acetic acid -perform endoscopy, airway
or hydrochloric acid maintenance, and patency of
the esophagus
-NO steroids
You might also like
- Omeprazole Drug StudyDocument4 pagesOmeprazole Drug StudyjoanneNo ratings yet
- Mod 5Document8 pagesMod 5Maribel MorallosNo ratings yet
- Esophageal DiseaseDocument25 pagesEsophageal DiseasesyedtayyabrazazaidiNo ratings yet
- D. Nemis - Drug Study (Immuno - Inflamm)Document5 pagesD. Nemis - Drug Study (Immuno - Inflamm)Dianne NemisNo ratings yet
- Gerd Maam Weng CruzDocument1 pageGerd Maam Weng CruzMingoy, CarlosNo ratings yet
- Risk For Aspiration Related To Esophageal Compromise Affecting The Lower Esophageal Sphincter As Evidenced by Heart Burn.Document2 pagesRisk For Aspiration Related To Esophageal Compromise Affecting The Lower Esophageal Sphincter As Evidenced by Heart Burn.eleinsamNo ratings yet
- NCMB 312 Finals!Document25 pagesNCMB 312 Finals!Justine Dinice MunozNo ratings yet
- NCP Case Analysis GastritisDocument7 pagesNCP Case Analysis GastritisSteffi GolezNo ratings yet
- NCM 112 MSN Prelim Topic 3 Care of Clients With Gastrointestinal DisordersDocument2 pagesNCM 112 MSN Prelim Topic 3 Care of Clients With Gastrointestinal DisordersKim Erida QuezonNo ratings yet
- MEDII-6.4a Peptic-Ulcer-DiseaseDocument9 pagesMEDII-6.4a Peptic-Ulcer-DiseaseCC Samson, Caesar AnthonyNo ratings yet
- PEDIATRICS DISORDER PART 2 LECTURE MergedDocument33 pagesPEDIATRICS DISORDER PART 2 LECTURE MergedErika CadawanNo ratings yet
- Group-5 NCM-107 NCPDocument4 pagesGroup-5 NCM-107 NCPbulok netflakes100% (1)
- Asthma Nursing Care Plan NCP Ineffective Airway Clearance CompressDocument2 pagesAsthma Nursing Care Plan NCP Ineffective Airway Clearance CompressMargarette GeresNo ratings yet
- DRGDocument5 pagesDRGcalarasheanNo ratings yet
- ALBUTEROLDocument1 pageALBUTEROLAnna LaritaNo ratings yet
- KUSAIN - NCP IN NCM 112 RLE ConstipationDocument2 pagesKUSAIN - NCP IN NCM 112 RLE Constipationjay kusainNo ratings yet
- Fluid Volume Deficit R/T Diarrhea & VomitingDocument4 pagesFluid Volume Deficit R/T Diarrhea & Vomitingjisoo100% (3)
- Drug Mechanism of Action Indication Contraindication Adverse Effects Nursing ImplicationsDocument2 pagesDrug Mechanism of Action Indication Contraindication Adverse Effects Nursing ImplicationsThimiNo ratings yet
- Adobe Scan 15 Jan 2023Document1 pageAdobe Scan 15 Jan 2023Nujhat TabassumNo ratings yet
- ASSESSMENT OF THE EAR, NOSE, MOUTH AND THROAT (Chapter 12)Document4 pagesASSESSMENT OF THE EAR, NOSE, MOUTH AND THROAT (Chapter 12)Christianne CapuaNo ratings yet
- NCMB 312 Finals! (2.0)Document25 pagesNCMB 312 Finals! (2.0)Justine Dinice MunozNo ratings yet
- NCMB 312 Finals! (2.0)Document25 pagesNCMB 312 Finals! (2.0)Justine Dinice MunozNo ratings yet
- Description: Acts By: Drug Mechanism of Action Indication Contraindication Adverse Effects Nursing ImplicationsDocument2 pagesDescription: Acts By: Drug Mechanism of Action Indication Contraindication Adverse Effects Nursing ImplicationsThimiNo ratings yet
- APPENDICITISDocument15 pagesAPPENDICITISTiffany AdriasNo ratings yet
- Mefenamic Acid Drug Study FormDocument2 pagesMefenamic Acid Drug Study FormKuro Mufu100% (2)
- AMOEBIASISDocument1 pageAMOEBIASISjeromedcNo ratings yet
- NCP Nausea and VomitingDocument4 pagesNCP Nausea and VomitingKingJayson Pacman06No ratings yet
- DRUG STUDY Sa Surgery WardDocument6 pagesDRUG STUDY Sa Surgery WardDANIELLA MALARANG MELNo ratings yet
- De La Cruz DS - VITAMIN BDocument2 pagesDe La Cruz DS - VITAMIN Bspain michaelisNo ratings yet
- SURGERYDocument13 pagesSURGERYSVPSNo ratings yet
- Drug Study IMDocument2 pagesDrug Study IMAbigail BrillantesNo ratings yet
- Nursing Care Plan Assessment Diagnosis and Inference Objectives Nursing Intervention Rationale EvaluationDocument2 pagesNursing Care Plan Assessment Diagnosis and Inference Objectives Nursing Intervention Rationale Evaluationjay kusainNo ratings yet
- Irritable Bowel SyndromeDocument6 pagesIrritable Bowel SyndromeHANNAH MICOLE GAERLANNo ratings yet
- Drug StudyDocument2 pagesDrug StudyEden Astred ObilloNo ratings yet
- Drug Study Domperidone CompressDocument1 pageDrug Study Domperidone CompressAngelica TolledoNo ratings yet
- Gerd Maam Weng MingoyDocument1 pageGerd Maam Weng MingoyMingoy, CarlosNo ratings yet
- Diarrhea (AGE)Document2 pagesDiarrhea (AGE)NursesLabs.com100% (1)
- Peptic Ulcer & Metabolic SyndromeDocument9 pagesPeptic Ulcer & Metabolic SyndromeApril Mae Magos LabradorNo ratings yet
- Drug Study: Morales, Joanah M. Bsniiblk3Grp9Document25 pagesDrug Study: Morales, Joanah M. Bsniiblk3Grp9viKingS!No ratings yet
- NCP BPHDocument8 pagesNCP BPHjyaba0% (1)
- CHN RleDocument3 pagesCHN RleCarissa Mae Tapec EstradaNo ratings yet
- Final Na Jud Ni As In!Document19 pagesFinal Na Jud Ni As In!joyrena ochondraNo ratings yet
- AsthmaDocument2 pagesAsthmaNurliyana GhazaliNo ratings yet
- Risk For Deficient Fluid VolumeDocument3 pagesRisk For Deficient Fluid VolumeALEKS MONTECINO JIMENEZNo ratings yet
- Ulcerative ColitisDocument17 pagesUlcerative ColitisTiffany AdriasNo ratings yet
- Common Complaints of Diseases of The AbdomenDocument37 pagesCommon Complaints of Diseases of The AbdomenNorjetalexis Maningo CabreraNo ratings yet
- Drug Study SampleDocument5 pagesDrug Study SampleMary Shane Aragon MoraldeNo ratings yet
- NCP (BPH)Document8 pagesNCP (BPH)NataCo50% (2)
- Metoclopramide DRUG STUDYDocument2 pagesMetoclopramide DRUG STUDYErica FabrigasNo ratings yet
- Fluorescein Wall ChartDocument1 pageFluorescein Wall ChartbijujcNo ratings yet
- Prado NCPDocument4 pagesPrado NCPalleah pradoNo ratings yet
- Name: Grace AGE: 28 Gender: Female Assessment Nursing Diagnosis Objectives Nursing Intervention Rationale Evaluation Subjective: GeneralDocument2 pagesName: Grace AGE: 28 Gender: Female Assessment Nursing Diagnosis Objectives Nursing Intervention Rationale Evaluation Subjective: GeneralRainier IbarretaNo ratings yet
- NCP Format 3 CKD Chronic Kidney Disease DM Diabetes Mellitus NephropathyDocument4 pagesNCP Format 3 CKD Chronic Kidney Disease DM Diabetes Mellitus NephropathySapna thakurNo ratings yet
- NCPDocument6 pagesNCPJane CasiquinNo ratings yet
- Drug StudyDocument7 pagesDrug StudyAndrea Isabel U. O'DellNo ratings yet
- Surgery BCA Pancreas Stomach Mar 2020Document5 pagesSurgery BCA Pancreas Stomach Mar 2020Jojo MendozaNo ratings yet
- NCP For CholecystitisDocument9 pagesNCP For Cholecystitisjmravago220% (1)
- DTRDocument6 pagesDTRThessa Lonica GarciaNo ratings yet
- EsophagusDocument10 pagesEsophagusSherif shalabyNo ratings yet
- Dysphagia, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandDysphagia, A Simple Guide To The Condition, Treatment And Related ConditionsRating: 5 out of 5 stars5/5 (1)
- A Simple Guide to Gastritis and Related ConditionsFrom EverandA Simple Guide to Gastritis and Related ConditionsRating: 4.5 out of 5 stars4.5/5 (3)
- Diverticulosis, A Simple Guide to the Condition, Treatment and Related DiseasesFrom EverandDiverticulosis, A Simple Guide to the Condition, Treatment and Related DiseasesRating: 1 out of 5 stars1/5 (1)
- OET Preparation Guide and Sample Corrections by DR Che PDF VersionDocument139 pagesOET Preparation Guide and Sample Corrections by DR Che PDF Versionrajashri patilNo ratings yet
- Acid RefluxDocument15 pagesAcid RefluxhowardNo ratings yet
- Tooth Enamel Erosion-18639Document9 pagesTooth Enamel Erosion-18639Charlie McdonnellNo ratings yet
- Medicin All Nov, Sep, OctDocument98 pagesMedicin All Nov, Sep, OctMohammad BanisalmanNo ratings yet
- Gastric Versus Jejunal Feeding: Evidence or Emotion?: Nutrition Issues in Gastroenterology, Series #42Document11 pagesGastric Versus Jejunal Feeding: Evidence or Emotion?: Nutrition Issues in Gastroenterology, Series #42Giselle Pezoa WattsonNo ratings yet
- Riaz Gul AHN Unit 1Document106 pagesRiaz Gul AHN Unit 1Riaz Gul RindNo ratings yet
- Applying Pharmacogenomics in Therapeutics-2016Document307 pagesApplying Pharmacogenomics in Therapeutics-2016taha100% (2)
- Laryngomalacia: Problems With A Floppy LarynxDocument2 pagesLaryngomalacia: Problems With A Floppy LarynxfiraNo ratings yet
- Best Practices in Nutrition For Children With MyelomeningoceleDocument9 pagesBest Practices in Nutrition For Children With MyelomeningoceleLiaNo ratings yet
- OET Preparation Guide and Sample Corrections by DR CheDocument137 pagesOET Preparation Guide and Sample Corrections by DR CheNaima Tariq50% (2)
- Allopurinol Drug Study WWW RNpedia ComDocument9 pagesAllopurinol Drug Study WWW RNpedia ComifyNo ratings yet
- 3 - GerdDocument11 pages3 - GerdompriyarathNo ratings yet
- Block 3 Final: GIDocument8 pagesBlock 3 Final: GIBegNo ratings yet
- Case Study-ASTHMADocument19 pagesCase Study-ASTHMAFritzielove BayawaNo ratings yet
- Disorders of The Digestive SystemDocument108 pagesDisorders of The Digestive SystemNina Lao CamamaNo ratings yet
- BIOCHEMDocument6 pagesBIOCHEMZairene Jane del RosarioNo ratings yet
- Basic Care and Comfort (20 Items)Document11 pagesBasic Care and Comfort (20 Items)Ik-ik MiralNo ratings yet
- LPR v2Document2 pagesLPR v2Axie LauanNo ratings yet
- Gastroesophagean Reflux DiseaseDocument13 pagesGastroesophagean Reflux Diseasedenisa malinaNo ratings yet
- Hiatal HerniaDocument60 pagesHiatal Herniababi100% (1)
- GERD PPT EditedDocument33 pagesGERD PPT EditedArpit MalhotraNo ratings yet
- Annual Report 2011 Beximco PharmaDocument91 pagesAnnual Report 2011 Beximco PharmaMD ABUL KHAYERNo ratings yet
- Iqoro For Hiatus Hernia PDF 2285963640922309Document14 pagesIqoro For Hiatus Hernia PDF 2285963640922309Ben ZithaNo ratings yet
- Verrucous Antral Gastritis in Relation To Helicobacter Pylori Infection, Nutrition, and Gastric AtrophyDocument6 pagesVerrucous Antral Gastritis in Relation To Helicobacter Pylori Infection, Nutrition, and Gastric AtrophySST KNo ratings yet
- Acid Reflux Holistic Blends Solution PDFDocument10 pagesAcid Reflux Holistic Blends Solution PDFRAJAGNo ratings yet
- Study Notes For Upper GI ProblemsDocument5 pagesStudy Notes For Upper GI ProblemsPrince K. Tailey100% (1)
- Boswellia: An Evidence-Based Systematic Review by The Natural Standard Research CollaborationDocument21 pagesBoswellia: An Evidence-Based Systematic Review by The Natural Standard Research CollaborationMichael Kohlberger, BSc MScNo ratings yet
- 9780323080323 (1)Document51 pages9780323080323 (1)nsahai06No ratings yet