Professional Documents
Culture Documents
A Clinical Study of Psoriatic Arthropathy
A Clinical Study of Psoriatic Arthropathy
Uploaded by
daniel saucedoOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
A Clinical Study of Psoriatic Arthropathy
A Clinical Study of Psoriatic Arthropathy
Uploaded by
daniel saucedoCopyright:
Available Formats
Original Article
A clinical study of psoriatic arthropathy
P. V. S. Prasad, Babu Bikku, P. K. Kaviarasan, A. Senthilnathan*
Departments of Dermatology Venereology and Leprosy and *Orthopaedics, Rajah Muthiah Medical College, Annamalai University, Annamalai
Nagar, Tamilnadu, India.
Address for correspondence: Dr. P. V. S. Prasad, 88, AUTA Nagar, Sivapuri post, Annamalai Nagar - 608 002, Tamilnadu, India.
E-mail: prasaderm@hotmail.com
ABSTRACT
Background: The incidence of uncomplicated psoriasis is 1-3% in the general population. Arthritis is found in increased
frequency in psoriatic patients and its incidence is estimated to be 5-7%. Aim: To assess the prevalence of arthritis in
psoriatic patients. Methods: Four hundred and seventy-two psoriatic patients were enrolled in the study out of which 40
patients had (psoriatic) arthropathy (PsA). Severity of psoriasis was assessed by the psoriasis area and severity index
(PASI). Routine blood investigations were carried out along with radiological investigations. Results: Forty percent of
the 40 PsA patients were in the age group of 51-60 years. Seven patients out of the 40 (17.5%) psoriatic arthropathic
(PsA) patients had a family history of psoriasis. Nail involvement was observed in 37 cases (92.5%). Rheumatoid factor
was present in five out of the 40 (12.5%) PsA patients. Serum uric acid levels were above normal in eighteen out of the
40 (45%) PsA patients. Asymmetric oligoarthropathy was the most commonly observed feature in 42.5% of the 40 PsA
patients. Narrowing of joint spaces and erosions were observed in 62.5% and 45% of the 40 PsA patients. Conclusion:
There is an association between the duration of skin lesions and duration of arthropathy. Similarly the PASI score is also
directly related with arthropathy.
Key Words: Psoriasis, Psoriasis arthritica, Psoriasis arthropathica, Psoriatic arthritis, Psoriatic arthropathy
INTRODUCTION in up to 30-40% of the patients.[3] As there are very few Indian
studies on PsA,[4] we undertook this clinical study to assess the
The recognition of psoriatic arthropathy (PsA) as a separate entity prevalence of PsA in psoriatic patients.
is a relatively recent occurrence. However, Jean Louis Alibert, a
French physician, described an association between psoriasis METHODS
and arthritis in 1818[1] and Earnest Bazin and Charles Bourdillon
conducted further studies on this condition.[2] In 1973, Moll and The study was conducted in the Department of Dermatology,
Wright identified and related clinical aspects which affected both Venereology and Leprosy at a rural hospital in Tamil Nadu
the joints and the skin, defining PsA as an inflammatory arthritis, for one year. Forty psoriatic patients with PsA attending
generally with a negative rheumatoid factor and associated the outpatient department were included in the study.
with psoriasis.[2] The true prevalence of psoriasis and PsA is not Details of demographic factors, history, clinical features
known with certainty, partly because of the elusive nature of the and type of psoriasis were all recorded. The severity of
psoriatic skin lesion. The prevalence of uncomplicated psoriasis the disease and the extent of involvement were assessed
is between 1-3% in the general population. Arthritis is found by using the psoriasis area severity index (PASI). Routine
in increased frequency in psoriatic patients and its incidence investigations including those for rheumatoid factor, serum
is estimated to be 5-7%. In severe psoriasis, arthritis can occur uric acid, Venereal Disease Research Laboratory (VDRL) and
How to cite this article: Prasad PVS, Babu B, Kaviarasan PK, Senthilnathan A. A Clinical Study of Psoriatic arthropathy. Indian J Dermatol Venereol
Leprol 2007;73:166-70.
Received: July, 2006. Accepted: December, 2006. Source of Support: Nil. Conflict of interest: None declared.
166 Indian J Dermatol Venereol Leprol|May-June 2007|Vol 73|Issue 3
Prasad PVS, et al.: Clinical study of psoriatic arthropathy
enzyme-linked immuno-sorbent assay (ELISA) for human these, pitting was the most common nail change observed in
immunodeficiency virus (HIV) were done for all patients. 29 patients (72.5%). PASI score in patients with PsA is shown in
Appropriate radiological investigations were carried out in Table 5. The score ranged from 6.2 to 42.4 with a mean of 17.8
all cases. X-rays were reported both by a radiologist and an and standard deviation (SD) of 4.8. Asymmetric oligoarthropathy
orthopedic surgeon. The results were analyzed by using the was seen in 17/40 patients (42.5%). In five patients, there was an
Chi-square test. The study was conducted after obtaining overlap between asymmetric oligoarthropathy and spondylitis
permission and informed consent from the ethical committee and in another two, both asymmetric oligoarthropathy and
of the institution and all patients respectively. sacroiliitis were seen [Table 6].
RESULTS Investigations revealed positive rheumatoid factor test
results in five patients (12.5%). The serum uric acid level was
Out of 21850 patients who attended the dermatology
outpatient department of our hospital during the study
Table 1: Duration of skin disease in patients of psoriatic
period of one year, there were 472 new cases of psoriasis arthopathy
(2.16%). Forty out of the 472 patients suffered from PsA Duration of skin lesions (years) Number of cases Percentage
(8.47%). The age distribution of PsA is shown in Figure 1. <5 16 40
Sixteen out of 40 PsA patients were in the age group of 51-60 5-10 17 42.5
11-15 3 7.5
years whereas five patients belonged to the 31-40 years age >15 4 10
group. The oldest patient was 68 years while the youngest
was 34 years of age. The PsA study group comprised 34 males
Table 2: Duration of arthropathy
(85%) and six females with a male to female ratio of 5.6:1.
Duration of arthropathy Number of cases Percentage
< 6 months 13 32.5
The duration of skin disease in patients with PsA is shown 6 months -1 year 7 17.5
in Table 1. Out of forty PsA patients, 42.5% had psoriatic 1-2 years 10 25
2-3 years 2 5
skin lesions for 5-10 years and 40% for < 5 years. Thirteen > 3 years 8 20
patients (32.5%) had noticed symptoms of PsA of < six months
duration [Table 2]. Family history of psoriasis was observed
Table 3: Clinical types of psoriasis
in seven out of 40 PsA patients (17.5%). The clinical type of
Types of psoriasis Number of cases Percentage
psoriasis correlated with PsA is shown in Table 3. Chronic
Plaques with scalp lesions 18 45
plaque psoriasis with scalp psoriasis was seen in 18 patients Plaques only 11 27.5
while chronic plaque psoriasis without scalp involvement Scalp only 1 2.5
Sebopsoriasis 1 2.5
was noticed in another 11 patients. Eight PsA patients (20%)
Palmoplantar 6 15
showed Köbner’s phenomenon and a positive Auspitz sign Guttate 2 5
was seen in 33 patients. Various types of nail changes were Erythrodermic 1 2.5
observed and are shown in Table 4.
Table 4: Nail changes in patients with psoriatic arthropathy
The nail changes ranged from pitting, ridging, subungual Type of nail change Number of patients
hyperkeratosis, onycholysis, dystrophy and discoloration. Among Pitting 29
Subungual hyperkeratosis 13
Ridging 8
Discoloration and dystrophy 7
45
Onycholysis 3
40
26 patients had more than one type of nail changes
Percentage
35
30
25
20 Table 5: Psoriasis area and severity index score in psoriatic
15 arthropathy
10 Psoriasis area and Number Percentage
5
severity index score
0
31-40 41-50 51-60 61-70 < 10 6 15
10-20 12 30
Age group, years
20-30 12 30
30-40 7 17.5
Figure 1: Age distribution of psoriatic arthropathy > 40 3 7.5
Indian J Dermatol Venereol Leprol|May-June 2007|Vol 73|Issue 3 167
Prasad PVS, et al.: Clinical study of psoriatic arthropathy
Table 6: Duration of psoriasis vs duration of psoriatic
arthropathy 50
Less than 6 months 1-2 2-3 >3 Total 40
6 months –1 year years years years
Percentage
< 5 years 8 4 4 - - 16 30
5-10 years 5 1 7 3 1 17
20
10-15 years - - - - 3 3
15 years 1 3 4
10
Total 13 6 11 3 7 40
PsA- Psoriatic arthropathy, P < 0.001 0
DIP
Rheumatoid
oligoarthropathy
Sacroiliitis
oligoarthropathy
+ sacroiliitis
Asymmetric
asymmetric
above normal limits in 18 patients (45%). It ranged from 2.8-
8.1 mg/dl with a mean of 6.21 and SD of 1.44. Erythrocyte
sedimentation ratio (ESR) was raised in 21 patients (52.5%). Figure 2: Distribution types of psoriatic arthropathy
On radiological examination, 62.5% showed narrowing of
joint spaces and 45% showed erosions. The other changes 70
are shown in Figure 2. Out of the 40 PsA patients in the study 60
Percentage
group, 82.5% had psoriatic skin lesions for < 10 years, while 50
in 30 patients (75%), the duration of arthropathy was < 2 40
years. Association between the duration of skin lesions and
30
20
duration of PsA is shown in Figure 3. Similarly, PASI score in
10
relation to type of PsA is shown in Table 7. 0
Erosions
Ankylosis
Osteolysis
Osteophytes
Soft tissue
Joint space
reduction
changes
DISCUSSION
Radiological features
Prevalence of PsA in our study period is found to be 8.47%.
Prevalence of PsA in the general population could not be Figure 3: Radiological changes in psoriatic arthritis
determined, but according to Braun-Falco, it lies between
0.02 and 0.1%.[3] Moll estimated the prevalence of PsA among proportion of male patients visiting the clinic being higher.
psoriatics to be 5-7%.[5] However, the prevalence rates are Psoriatic skin lesions preceded PsA in 39 patients (97.5%),
variable and may be as high as 30–40% in psoriatic patients while in one patient, they occurred simultaneously. Similar
with severe skin manifestations. The age of onset varies from observations were made by earlier authors.[6] We also found
30-50 years, a range which is similar to that of rheumatoid that PsA is relatively rare after ten years of onset of skin
arthritis. In our study, 40% of patients were in the age group lesions. Almost all patients in this group were taking some
of 51-60 years. PsA is found most commonly in the age group disease-modifying agents, which could be the reason for
of 41-60 years and its incidence decreases towards the outer the lower prevalence in those with duration of skin lesions
limits of the range. exceeding ten years.
Rajendran from Chennai also found a peak incidence (69%) All patients who were in the fourth decade of life who
of PsA in the 4th and 5th decades of life.[4] Wright reported developed psoriasis, also developed PsA within twelve
an equal incidence of PsA in both sexes. We found a male months. Family history of psoriasis was found in 27.5% of
preponderance which could also be due to the overall patients in our study. Recent genetic studies suggest that
Table 7: Psoriasis area and severity index scores vs type of psoriatic arthropathy
Psoriasis area and Type of arthropathy
severity index score Asymmetric oligoarthritis Distal interphalangeal Rheumatoid Spinal Oligoarthritis with spinal Total
< 10 4 4 8
10-20 5 1 5 3 1 15
20-30 8 1 2 2 2 15
30-40 - - - - 1 1
> 40 - - - - 1 1
Total 17 6 7 5 5 40
P = 0.02
168 Indian J Dermatol Venereol Leprol|May-June 2007|Vol 73|Issue 3
Prasad PVS, et al.: Clinical study of psoriatic arthropathy
certain HLA antigens like B13, B17, B18, B27, DR4 and DR7 elevated.[14] We could not conduct these tests due to the lack
were found more commonly in patients with PsA than in of necessary facilities.
patients with only psoriatic lesions.[7,8] According to Finzi,
heredity is a predisposing factor in PsA.[2] Chronic plaque type Previous studies did not measure PASI scores whereas we found
of psoriasis was the most common presentation with scalp a direct correlation between a high PASI and various types of PsA.
involvement in most of the cases. Rajendran also observed Four out of six patients with DIP involvement alone had a PASI of
chronic plaque type in 81% of the patients and opined that < 10. This shows that less severe skin involvement is associated
the scalp was a hidden site.[4] with minimal joint involvement. Association of elevated PASI
scores in other types of PsA is statistically significant. However,
Köbner’s phenomenon was observed in 20% of our patients. we could not relate any specific type of joint involvement
On the basis of Köbner’s phenomenon of the skin, Moll with the severity of the skin disease. PsA is considered a sero-
et al. hypothesized that repeated micro or macro traumas negative spondyloarthropathy, a group of diseases that includes
may have a profound ‘Koebner effect’ on the joints.[9] A ankylosing spondylitis, reactive arthritis and Reiter’s syndrome
positive Auspitz sign was seen in 82.5% of the patients. This and the arthritis associated with inflammatory bowel disease.
indicated that the disease is still active in such patients. These diseases share a predilection for asymmetric peripheral
Nail changes were observed in 92.5% of cases while 65% arthritis and axial or spinal involvement.
showed more than one nail finding. A similar association
has been noticed in the earlier studies also.[10] In some As with other spondyloarthropathies, musculoskeletal
studies, the observation of nail changes in PsA patients was manifestations of PsA may also include inflammation at
considered secondary to arthritis of underlying joints.[11,12] the site attachment of tendons and ligaments (enthesitis),
Distal interphalangeal (DIP) arthropathy was commonly especially at the site of the Achilles tendon insertion and the
associated with onycholysis and dystrophic nail changes insertion of the plantar fascia into the calcaneus. Dactylitis,
in seven patients. also described as a sausage digit, may be seen. These digits
develop swelling and tenderness of the entire finger or toe
We could not correlate the type of nail change with the because of inflammation of the tendons along with the
type of psoriasis as the sample size was small and various involved joints.[15] Asymmetric oligoarthropathy was most
morphological types of nail changes were seen in a single commonly seen in our series, which was found in 42.5% cases.
patient. Although PsA is a sero-negative arthritis and the We did not encounter patients with arthritis mutilans in our
absence of rheumatoid factor is a characteristic laboratory series. Finzi also reported asymmetric oligoarthritis as the
finding, it may be present in 3% of PsA patients, which is the largest subgroup of PsA in 70% of the cases.[2]
same as its incidence in the general population.[3] We have
found 12.5% of cases testing positive for rheumatoid factor. The longer the duration of psoriasis, the more severe is the
Two of these patients had symmetric rheumatoid type of PsA. Brower suggested that the initial lesions of PsA are
arthropathy with abnormally raised ESR. These cases create marginal erosions and the narrowing of joint spaces while
a diagnostic difficulty except for the presence of typical osteolysis, ankylosis and new bone formation are seen in the
psoriatic lesions. more advanced stages of the disease.[15,16] We also correlated
the type and severity of radiologic changes and consequent
Serum uric acid levels were found to be elevated in a number damage to the joints affected with the duration of arthropathy.
of studies. This is due to increased purine metabolism due The most common radiologic changes observed in the study
to high cell turnover. Slightly elevated levels do not usually group were of joint space narrowing in 62.5% and erosions in
end up in gout. Our results were consistent with those of 45% of the patients with many patients showing more than one
Lambert and Wright who found a high prevalence of serum type of change. Long-standing cases showed more damaging
uric acid values above normal, but a mean value inside the radiologic changes like ankylosis (7.5%) and early osteolysis (5%)
normal range.[12] Hyperuricemia was noted in 41.6% of the and all these patients had psoriasis of > 3 years duration.
cases by Nigam in a study on psoriatic arthritis, indicating
extensive involvement of skin.[13] ESR values were raised in Seven patients showed only soft tissue changes with no
52.5% of cases in the study group. ESR is widely used as a obvious bony changes in the X-rays and all of them presented
nonspecific marker of joint inflammation to assess disease within the first six months of onset of arthropathic symptoms.
activity. The other laboratory indicators are α-2 globulin, β Although PsA has traditionally been viewed as a disease with
globulin and C-reactive protein, whose levels may also be a benign prognosis, radiographic evidence, as described
Indian J Dermatol Venereol Leprol|May-June 2007|Vol 73|Issue 3 169
Prasad PVS, et al.: Clinical study of psoriatic arthropathy
previously, indicates that the disease is more progressive 6. Winchester R. Psoriatic arthritis. Dermatol Clin 1995;13:779-
and destructive than what was previously thought. Although 92.
the highest rate of peripheral joint involvement in PsA 7. Moll JM, Wright V. Familial occurrence of psoriatic arthritis. Ann
Rheum Dis 1973;22:181-201.
seems to be within the first 12 months of disease onset,
8. Gladman DD, Anhorn KA, Schachter RK, Mervart H. HLA antigens
the disease has been shown to be progressive in terms of in psoriatic arthritis. J Rheumatol 1986;13:586-92.
number of joints affected and damage to those joints. It has 9. Espinoza LR, Cueller ML. Psoriatic arthritis: Management. In:
been suggested that possible indicators of poor prognosis Hochberg MC, Silman AJ, Smolen JS, Weinblatt ME, Weisman
include younger age at onset, extensive skin involvement and MH, editors. Rheumatology. 3rd ed. Mosby: London; 1998. p.
certain HLA antigens.[17] From our study, we could conclude a 1259-65.
10. Espinoza LR, Cueller ML. Psoriatic arthritis: Management. In:
direct correlation between severity of PsA and age of onset
Hochberg MC, Silman AJ, Smolen JS, Weinblatt ME, Weisman
of the disease. Ongoing research into the epidemiology MH, editors. Rheumatology. 3rd ed. Mosby: London; 1998. p.
and outcomes of PsA can provide insight into the patient 1259-65.
characteristics, such as multiple involved joints, that may be 11. Scarpa R, Oriente P, Pucino A, Torella M, Vignone L, Riccio A,
indicators of poor prognostic outcomes. et al. Psoriatic arthritis in psoriatic patients. Br J Rheumatol
1984;23:246-50.
12. Lambert JR, Wright V. Serum uric acid levels in psoriatic arthritis.
REFERENCES
Ann Rheuma Dis 1977;36:234-7.
13. Nigam P, Singh DS, Matreja VS, Saxena HN. Psoriatic arthritis:
1. Moll JM. Psoriatic arthritis. In: Mier PD, Peter CM, Vande, editors. A clinical radiological study. J Dermatol 1980;7:55-9.
Text book of Psoriasis. 1st ed. Churchill Livingstone: New York; 14. Gladman DD, Shukett R, Russel ML, Thorne JC, Schachter
1986. p. 55-83. RK. Psoriatic arthritis: An analysis of 220 patients. Q J Med
2. Finzi AF, Gibelli E. Psoriatic arthritis. Int J Dermatol 1991;30:1- 1987;62:127-41.
7. 15. Ruderman EM, Tamber S. Psoriatic arthritis: Prevalence,
3. Braun-Falco O, Ruzicka T. Psoriatic arthritis. Int J Dermatol diagnosis and review of therapy for the dermatologists.
1994;33:320-2. Dermatol Clin 2004;22:477-80.
4. Rajendran CP, Ledge SG, Rani KP, Mahadevan R. Psoriatic 16. Brower AC, Allman RM. Pencil pointing: A vascular pattern of
arthritis. JAPI 2003;51:1065-8. deossification. Radiographics 1983;3:315-8.
5. Moll JM, Wright V. Psoriatic arthritis. Semin Arthritis Rheum 17. Moll JM. The clinical spectrum of psoriatic arthritis. Clin Orthop
1973;3:55-78. 1979;143:66-75.
170 Indian J Dermatol Venereol Leprol|May-June 2007|Vol 73|Issue 3
You might also like
- Applying The WALANT Technique To Surgical Treatment of Distal Radius FracturesDocument6 pagesApplying The WALANT Technique To Surgical Treatment of Distal Radius Fracturesdaniel saucedoNo ratings yet
- DSU 22317 PracticalDocument31 pagesDSU 22317 PracticalCo2I 36Rohini ShewalkarNo ratings yet
- 3D-Shapes Symmetry Patterns-Term2 WorksheetDocument3 pages3D-Shapes Symmetry Patterns-Term2 Worksheetmahroof50% (2)
- Psoriasis StudyDocument10 pagesPsoriasis StudyQamar AzeezNo ratings yet
- Kes 187Document6 pagesKes 187Giancarlo SanteNo ratings yet
- Age-Related Changes in Dry Eye Syndrome: A Retrospective Cohort StudyDocument3 pagesAge-Related Changes in Dry Eye Syndrome: A Retrospective Cohort StudyOktiYuviaNo ratings yet
- Eritroderma EpidemiologyDocument6 pagesEritroderma EpidemiologyAhmad Ligar SuhermanNo ratings yet
- Clinicopathological Correlation in Erythroderma: Original ArticleDocument5 pagesClinicopathological Correlation in Erythroderma: Original ArticleStella SunurNo ratings yet
- Granulomatous Epididymo-Orchitis: Diagnosis by Fine Needle AspirationDocument4 pagesGranulomatous Epididymo-Orchitis: Diagnosis by Fine Needle AspirationAnonymous tlIQeKLriNo ratings yet
- Psoriatic Arthritis Professor Neil McHugh - Management of Psoriatic Arthritis - 0Document48 pagesPsoriatic Arthritis Professor Neil McHugh - Management of Psoriatic Arthritis - 0S Sinha Ray100% (1)
- Rematik Fever Post StreptococcusDocument4 pagesRematik Fever Post StreptococcusHajrin PajriNo ratings yet
- Clinico-Etiological Spectrum of Pancytopenia in Hospitalized ChildrenDocument4 pagesClinico-Etiological Spectrum of Pancytopenia in Hospitalized ChildrenNurul Huda KowitaNo ratings yet
- The Association of Autoimmune Thyroid Disease (AITD) With Psoriatic Disease: A Prospective Cohort Study, Systematic Review and Meta-AnalysisDocument13 pagesThe Association of Autoimmune Thyroid Disease (AITD) With Psoriatic Disease: A Prospective Cohort Study, Systematic Review and Meta-AnalysisLidwina ApyakaNo ratings yet
- Histopathology and Clinico-Histopathological CorreDocument8 pagesHistopathology and Clinico-Histopathological CorreRodrigo MoraesNo ratings yet
- Dermoscopy To Differentiate Guttate Psoriasis From A MimickerDocument6 pagesDermoscopy To Differentiate Guttate Psoriasis From A MimickeryelsiNo ratings yet
- JurnalDocument6 pagesJurnalRoby martinus bayaNo ratings yet
- Clinical Profile of Acute Rheumatic Fever Patients Attending A Tertiary Care Hospital in Eastern Bihar, IndiaDocument4 pagesClinical Profile of Acute Rheumatic Fever Patients Attending A Tertiary Care Hospital in Eastern Bihar, IndiaraniaulfahNo ratings yet
- Erythroderma. A Clinical and Etiological Study of 103 PatientsDocument9 pagesErythroderma. A Clinical and Etiological Study of 103 PatientsDewi NurhayatiNo ratings yet
- Diagnosis of Breast Cancer Using Neural Network ApproachDocument8 pagesDiagnosis of Breast Cancer Using Neural Network ApproachNavneet YadavNo ratings yet
- Atrophoderma of Pasini and Pierini - A Clinical and Histopathological Study - Saleh2008Document7 pagesAtrophoderma of Pasini and Pierini - A Clinical and Histopathological Study - Saleh2008Andrés WunderwaldNo ratings yet
- Positive Effects of Hydrogen-Water Bathing in Patients of Psoriasis and Parapsoriasis en PlaquesDocument8 pagesPositive Effects of Hydrogen-Water Bathing in Patients of Psoriasis and Parapsoriasis en PlaquesEstetika MedikNo ratings yet
- Cutaneous SarcoidosisDocument5 pagesCutaneous SarcoidosisWei Sheng ChongNo ratings yet
- Journal Reading Clinicopathological Study of Lichen Amyloidosis - Kartika Mega Utami BouwDocument4 pagesJournal Reading Clinicopathological Study of Lichen Amyloidosis - Kartika Mega Utami BouwmarinNo ratings yet
- To Study Haematological Profile of Enteric Fever Patients.: International Journal of Current Research in Medical SciencesDocument6 pagesTo Study Haematological Profile of Enteric Fever Patients.: International Journal of Current Research in Medical SciencesAnonymous hF9HwHVuqNo ratings yet
- Risiko Kemati An Pada Kasus-Kasus Leptospirosis: Data Dari Kabupaten Bantul 2012-2017Document6 pagesRisiko Kemati An Pada Kasus-Kasus Leptospirosis: Data Dari Kabupaten Bantul 2012-2017arifjo7999No ratings yet
- International Journal of Infectious DiseasesDocument3 pagesInternational Journal of Infectious DiseasesPendidikan Dokter Unsyiah 2015No ratings yet
- Axial Psoriatic Arthritis An UpdateDocument10 pagesAxial Psoriatic Arthritis An Updateproject zoroNo ratings yet
- Association Between Vasomotor Rhinitis and Irritable Bowel SyndromeDocument7 pagesAssociation Between Vasomotor Rhinitis and Irritable Bowel SyndromedeaNo ratings yet
- Poster PPKI ACTHDocument2 pagesPoster PPKI ACTHvictoryNo ratings yet
- Contact Sensitizers in Dyshidrotic Eczema: Original ArticleDocument5 pagesContact Sensitizers in Dyshidrotic Eczema: Original Articledrian pamungkasNo ratings yet
- 7 Rare Cases in IndiaDocument5 pages7 Rare Cases in IndiaNarendran KumaravelNo ratings yet
- 679 1364 1 SMDocument5 pages679 1364 1 SMRetno ManggalihNo ratings yet
- Zadeh 2002Document5 pagesZadeh 2002Gus MahlerNo ratings yet
- Erythroderma: A Clinicopathological Study of 102 Cases: Original ArticleDocument6 pagesErythroderma: A Clinicopathological Study of 102 Cases: Original Article568563No ratings yet
- IJORL Volume 26 Issue 4 Pages 245-249Document5 pagesIJORL Volume 26 Issue 4 Pages 245-249adrianussetNo ratings yet
- Faktor-Faktor Yang Mempengaruhi Mortalitas Pasien ARDS Di Rumah Sakit Cipto Mangunkusumo JakartaDocument8 pagesFaktor-Faktor Yang Mempengaruhi Mortalitas Pasien ARDS Di Rumah Sakit Cipto Mangunkusumo JakartaTiwi NaloleNo ratings yet
- IJD Volume 24 Issue 3 Pages 214-219Document6 pagesIJD Volume 24 Issue 3 Pages 214-219Risky PerdanaNo ratings yet
- Exclusion Criteria: ResultsDocument4 pagesExclusion Criteria: ResultsRina FebriatiNo ratings yet
- Clinical Study of Psoriasis Occurring Over The Age of 60 Years: Is Elderly-Onset Psoriasis A Distinct Subtype?Document6 pagesClinical Study of Psoriasis Occurring Over The Age of 60 Years: Is Elderly-Onset Psoriasis A Distinct Subtype?DwityaOktinaDewiNo ratings yet
- Prevalence of Hypospadias Patients With Undescended TestisDocument5 pagesPrevalence of Hypospadias Patients With Undescended TestisIJPHSNo ratings yet
- Shift Work: A Risk Factor For Central Serous ChorioretinopathyDocument7 pagesShift Work: A Risk Factor For Central Serous ChorioretinopathysampleNo ratings yet
- Psoriasis - Dr. SunardiDocument65 pagesPsoriasis - Dr. SunardiAntari Puspita PrimanandaNo ratings yet
- Medip, IJCP-1084 ODocument5 pagesMedip, IJCP-1084 OshamaaroubaNo ratings yet
- Master ErysipelasDocument20 pagesMaster Erysipelaszul090No ratings yet
- 16 JMSCRDocument7 pages16 JMSCRVani Junior LoverzNo ratings yet
- Clinical Profile, Etiology and Histopathology of Patients With Erythroderma in South IndiaDocument5 pagesClinical Profile, Etiology and Histopathology of Patients With Erythroderma in South IndiaAditya FmfNo ratings yet
- Drug Allergy Clinical Characteristics in PediatricsDocument5 pagesDrug Allergy Clinical Characteristics in PediatricsnadyaNo ratings yet
- Simple Clinical Indicators For Early Psoriatic Arthritis Detection.Document3 pagesSimple Clinical Indicators For Early Psoriatic Arthritis Detection.pancholarpancholarNo ratings yet
- Rheumatoid Arthritis-Associated Aortitis: A Case Report and Literature ReviewDocument7 pagesRheumatoid Arthritis-Associated Aortitis: A Case Report and Literature ReviewMuhammad RaflirNo ratings yet
- Ophthalmic Manifestations of Paederus DermatitisDocument7 pagesOphthalmic Manifestations of Paederus Dermatitisvaleria lindaNo ratings yet
- Profile of Tinea Corporis and Tinea Cruris in Dermatovenereology Clinic of Tertiery Hospital: A Retrospective StudyDocument6 pagesProfile of Tinea Corporis and Tinea Cruris in Dermatovenereology Clinic of Tertiery Hospital: A Retrospective StudyRose ParkNo ratings yet
- A Study of Mean Platelet Volume As A Prognostic Marker in SepsisDocument3 pagesA Study of Mean Platelet Volume As A Prognostic Marker in SepsisIjsrnet EditorialNo ratings yet
- Max Appendicitis Score: A New Diagnostic Score For Diagnosing Acute AppendicitisDocument4 pagesMax Appendicitis Score: A New Diagnostic Score For Diagnosing Acute Appendicitismuhammad ajiNo ratings yet
- Epidemiological Profile of Colombian Patients With Rheumatoid Arthritis in A Specialized Care ClinicDocument6 pagesEpidemiological Profile of Colombian Patients With Rheumatoid Arthritis in A Specialized Care Clinicfrancisca yañezNo ratings yet
- Henoch SchonleinDocument8 pagesHenoch Schonleindinu_maria95No ratings yet
- The Clinical Significance of Perilimbal Conjunctival Pigmentation in Vernal ConjunctivitisDocument4 pagesThe Clinical Significance of Perilimbal Conjunctival Pigmentation in Vernal ConjunctivitisNafhyraJunetNo ratings yet
- Clinical Characteristics of Sibling Patients With Comitant StrabismusDocument4 pagesClinical Characteristics of Sibling Patients With Comitant StrabismusAmparito SanchezNo ratings yet
- File 2Document18 pagesFile 2Ikke PrihatantiNo ratings yet
- Antiphospholipid Syndrome Associated With Infections - Clinical and Microbiological Characteristics of 100 PatientsDocument6 pagesAntiphospholipid Syndrome Associated With Infections - Clinical and Microbiological Characteristics of 100 PatientsKelly de GuzmanNo ratings yet
- Study On Etiological Profile of Patients With PapilloedemaDocument7 pagesStudy On Etiological Profile of Patients With PapilloedemaIJAR JOURNALNo ratings yet
- Pyoderma Gangrenosum: A Clinico-Epidemiological Study: Date of Web Publication 2-Dec-2016Document8 pagesPyoderma Gangrenosum: A Clinico-Epidemiological Study: Date of Web Publication 2-Dec-2016Sandara ParkNo ratings yet
- Ojsadmin, 171Document7 pagesOjsadmin, 171Test Music CopyrightNo ratings yet
- Dosage of Local Anesthesia in Wide Awake Hand SurgeryDocument4 pagesDosage of Local Anesthesia in Wide Awake Hand Surgerydaniel saucedoNo ratings yet
- Estandares de Ramases - Revisión NarrativaDocument15 pagesEstandares de Ramases - Revisión Narrativadaniel saucedoNo ratings yet
- Wide-Awake Local Anesthesia With No Tourniquet AnDocument11 pagesWide-Awake Local Anesthesia With No Tourniquet Andaniel saucedoNo ratings yet
- Mobile Wimax: Sector Antenna Installation ManualDocument17 pagesMobile Wimax: Sector Antenna Installation ManualjbonvierNo ratings yet
- Design Fabrication and Evaluation of A MDocument92 pagesDesign Fabrication and Evaluation of A Mphillip chirongweNo ratings yet
- Q2 Math 6Document7 pagesQ2 Math 6JUVY PONTILLASNo ratings yet
- A Comparison Between LDPE and HDPE Cable Insulation Properties Following Lightning Impulse AgeingDocument4 pagesA Comparison Between LDPE and HDPE Cable Insulation Properties Following Lightning Impulse AgeingGilang Satria PasekaNo ratings yet
- Sun Cluster 3.1 Administration ES-338Document540 pagesSun Cluster 3.1 Administration ES-338Vinod PatilNo ratings yet
- Week6 (Aco and Pso)Document55 pagesWeek6 (Aco and Pso)Karim Abd El-GayedNo ratings yet
- NCERT Class 10 Mathematics PDFDocument369 pagesNCERT Class 10 Mathematics PDFArnab GangopadhyayNo ratings yet
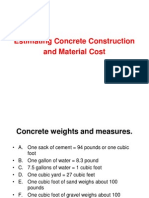
- Estimating Concrete Material Fuller MethodDocument17 pagesEstimating Concrete Material Fuller MethodOliver BrownNo ratings yet
- Physics Notes Form 5Document221 pagesPhysics Notes Form 5tonikay219No ratings yet
- Chilled Ceilings/Beams SystemsDocument8 pagesChilled Ceilings/Beams SystemsShazia Farman Ali QaziNo ratings yet
- Hyundai Azera 2016 Ecu Pin OutDocument14 pagesHyundai Azera 2016 Ecu Pin OutReza Varamini100% (1)
- Corto CircuitoDocument30 pagesCorto CircuitoManuel RochaNo ratings yet
- Running Minio in Minikube GitHubDocument4 pagesRunning Minio in Minikube GitHubJuan Carlos AlvarezNo ratings yet
- International Standard: Series 1 Freight Containers - Corner and Intermediate Fittings - SpecificationsDocument11 pagesInternational Standard: Series 1 Freight Containers - Corner and Intermediate Fittings - Specificationssandeep@homeNo ratings yet
- Ultrasonic Testing Ut Q Bank A-13Document9 pagesUltrasonic Testing Ut Q Bank A-13kingstonNo ratings yet
- IT ELECTIVE 2 Midterm HandoutsDocument82 pagesIT ELECTIVE 2 Midterm Handoutsjohnny sinsNo ratings yet
- Dav Institute of Engineering and Technology JalandharDocument52 pagesDav Institute of Engineering and Technology JalandharAbhijit SinghNo ratings yet
- Angular Measurement - Phan Van HanDocument24 pagesAngular Measurement - Phan Van Han손종인No ratings yet
- General AnesthesiaDocument2 pagesGeneral AnesthesiadhaineyNo ratings yet
- FILE 20220107 222239 Solutions - IGO-2021Document36 pagesFILE 20220107 222239 Solutions - IGO-2021Nhân DuyNo ratings yet
- Voltage Drop & Cable Sizing & Electrical LoadDocument26 pagesVoltage Drop & Cable Sizing & Electrical Loadfd270% (1)
- I. Absolute Value Functions: Math 150 - Topic 2 Piecewise-Defined FunctionsDocument6 pagesI. Absolute Value Functions: Math 150 - Topic 2 Piecewise-Defined Functionsrohitrgt4uNo ratings yet
- IMCA-Event-2017!06!14 - Presentation 5 - Synthetic Fibre SlingsDocument30 pagesIMCA-Event-2017!06!14 - Presentation 5 - Synthetic Fibre SlingsRanga Swami ReddyNo ratings yet
- 3-1 Extrema On An IntervalDocument9 pages3-1 Extrema On An IntervalAbbyNo ratings yet
- 1972 Motorola Semiconductor Library Second Edition Vol3Document657 pages1972 Motorola Semiconductor Library Second Edition Vol3BapeNo ratings yet
- Unwinding StationDocument34 pagesUnwinding StationDeniMestiWidiantoNo ratings yet
- Spec Sheet SD200Document8 pagesSpec Sheet SD200Yohanes ArgamNo ratings yet
- Active Suspension System With Preview ControlDocument5 pagesActive Suspension System With Preview Controlrudey18No ratings yet