Professional Documents
Culture Documents
Checklist Administering Ophthalmic Instillations
Checklist Administering Ophthalmic Instillations
Uploaded by
Janna LacastesantosCopyright:
Available Formats
You might also like
- Administering An IntradermalDocument7 pagesAdministering An IntradermalCzarina Mae Quinones TadeoNo ratings yet
- Best Practices Procedure For Instillation of Eye DropsDocument1 pageBest Practices Procedure For Instillation of Eye DropsRahul ModiNo ratings yet
- Oral MedicationDocument30 pagesOral MedicationPetit NacarioNo ratings yet
- Administering Ophthalmic InstillationsDocument3 pagesAdministering Ophthalmic InstillationsFarsee AdilNo ratings yet
- Eent Group 3Document31 pagesEent Group 3Leonifel BersaminaNo ratings yet
- Administering An Intradermal InjectionDocument3 pagesAdministering An Intradermal Injectionco230847No ratings yet
- Week 7Document53 pagesWeek 7MICHAEL ANDRE COROSNo ratings yet
- Administering Oral Medications: Melendez, Anna Carmela PDocument19 pagesAdministering Oral Medications: Melendez, Anna Carmela PAnna Carmela P. MelendezNo ratings yet
- Administering A Subcutaneous InjectionDocument4 pagesAdministering A Subcutaneous Injectionco230847No ratings yet
- ID-IM-SQ-E ToolDocument9 pagesID-IM-SQ-E TooltriciacamilleNo ratings yet
- Administering An Intramuscular InjectionDocument4 pagesAdministering An Intramuscular Injectionco230847No ratings yet
- Administering Opthalmic MedicationsDocument6 pagesAdministering Opthalmic MedicationsJulianne B. Dela CruzNo ratings yet
- Checklist Administering An Intramuscular InjectionDocument3 pagesChecklist Administering An Intramuscular InjectionCAMPOSANO, JHANNA MARIENo ratings yet
- Assessing The Nose and SinusesDocument2 pagesAssessing The Nose and SinusesAccey RamirezNo ratings yet
- Administering Opthalmic MedicationsDocument5 pagesAdministering Opthalmic MedicationsAnika PleñosNo ratings yet
- Checklist Credes ProphylaxisDocument1 pageChecklist Credes ProphylaxisAliza AlyyNo ratings yet
- Topical AdministrationDocument36 pagesTopical AdministrationSilpa Jose TNo ratings yet
- Administration Eye DropsDocument13 pagesAdministration Eye DropsyaraNo ratings yet
- P-19 Administering-Ophthalmic-InstallationDocument3 pagesP-19 Administering-Ophthalmic-InstallationJeleeey AlarconNo ratings yet
- Administering Ophthalmic MedicationsDocument2 pagesAdministering Ophthalmic MedicationsRoxi MalaqueNo ratings yet
- Eye Ear Med Instillation Procedure RationaleDocument6 pagesEye Ear Med Instillation Procedure Rationaleyuuki konnoNo ratings yet
- Checklist-Medication 2Document7 pagesChecklist-Medication 2michelleciubalbarbosa16No ratings yet
- Assessment Nose SinusesDocument2 pagesAssessment Nose SinusesSyphar IndasanNo ratings yet
- Clinical Learning Skills Laboratory: College of NursingDocument3 pagesClinical Learning Skills Laboratory: College of NursingBeverly DatuNo ratings yet
- Checklist Opthalmic MedDocument3 pagesChecklist Opthalmic MedamaNo ratings yet
- RLE PrelimsDocument8 pagesRLE PrelimsNicole VallejosNo ratings yet
- Level 2 2nd Sem ChecklistDocument31 pagesLevel 2 2nd Sem ChecklistMart Juaresa YambaoNo ratings yet
- Eye Instillation Procedure Guide NursingDocument3 pagesEye Instillation Procedure Guide NursingTrisha ApillanesNo ratings yet
- SL PNCM 1079 Administering An Intramuscular InjectionDocument3 pagesSL PNCM 1079 Administering An Intramuscular Injectionpreciouslagundi226No ratings yet
- Eye Swabbing and Instillation of Eye DropDocument4 pagesEye Swabbing and Instillation of Eye Dropsinuaish syaNo ratings yet
- Module-Intradermal Etool PDFDocument7 pagesModule-Intradermal Etool PDFErika Danalle ArceoNo ratings yet
- Procedure: Administering An Intradermal Injection For Skin TestDocument3 pagesProcedure: Administering An Intradermal Injection For Skin TestSofia AmistosoNo ratings yet
- Administering An Intramuscular InjectionDocument3 pagesAdministering An Intramuscular InjectionPattNo ratings yet
- Administering IntradermalDocument4 pagesAdministering IntradermalNezukoNo ratings yet
- Eye Irrig RDDocument3 pagesEye Irrig RDJames Kristopher RebayaNo ratings yet
- Preparing Meds From Ampules and VialsDocument7 pagesPreparing Meds From Ampules and VialsZyra ObedencioNo ratings yet
- GuidesDocument10 pagesGuidesJClaudz PilapilNo ratings yet
- IntradermalDocument7 pagesIntradermalKyle Dapulag100% (1)
- Checklist For Motuth Neck and EyesDocument7 pagesChecklist For Motuth Neck and EyesWylyn Mae VisqueraNo ratings yet
- Medication AdministrationDocument15 pagesMedication AdministrationbasheNo ratings yet
- Parenteral PRDocument4 pagesParenteral PRGlecy CastañaresNo ratings yet
- Administering Intradermal InjectionDocument17 pagesAdministering Intradermal InjectionPattNo ratings yet
- Republic of The Philippines: Tarlac State University College of Science Nursing DepartmentDocument26 pagesRepublic of The Philippines: Tarlac State University College of Science Nursing DepartmentMaxeneDhale100% (1)
- Parenteral Catheterization Enema ChecklistDocument8 pagesParenteral Catheterization Enema ChecklistJessoliver GalvezNo ratings yet
- Activity 2 Updated MurilloDocument22 pagesActivity 2 Updated MurilloAraw GabiNo ratings yet
- Medication AdministrationDocument88 pagesMedication AdministrationKBD100% (1)
- Medication AdministrationDocument100 pagesMedication AdministrationMJ Jomoc ArejolaNo ratings yet
- Mark King Joseph P. Cordovilla - Mid1a - CP100 - Module 9Document5 pagesMark King Joseph P. Cordovilla - Mid1a - CP100 - Module 9Mark king Joseph CordovillaNo ratings yet
- Preparing Med From A Vial ChecklistDocument5 pagesPreparing Med From A Vial ChecklistRalf FiedalinoNo ratings yet
- PARENTERAL MEDICATION Manual and Checklist 1Document14 pagesPARENTERAL MEDICATION Manual and Checklist 1Hazel Shaine BaybayanNo ratings yet
- PERFORMANCE CRITERIA CHECKLIST Oral Otic Optic Parenteral Drug AdministrationDocument3 pagesPERFORMANCE CRITERIA CHECKLIST Oral Otic Optic Parenteral Drug AdministrationRayzl GacayanNo ratings yet
- PRS InjectionsDocument3 pagesPRS InjectionsLuke SmithNo ratings yet
- Administering Medication Via A Small-Volume NebulizerDocument2 pagesAdministering Medication Via A Small-Volume NebulizerJerilee SoCute WattsNo ratings yet
- MedicationDocument9 pagesMedicationtolchakebede163No ratings yet
- ID IM ChecklistDocument2 pagesID IM Checklistzmv627j7kgNo ratings yet
- Administering Oral Medications 1Document7 pagesAdministering Oral Medications 1co230847No ratings yet
- Small Volume Neb Checklist 2Document3 pagesSmall Volume Neb Checklist 2Katelinne DabucolNo ratings yet
- Subcutaneus Injection TechniqueDocument4 pagesSubcutaneus Injection TechniqueReza Fitra Kusuma NegaraNo ratings yet
- Survival Skills: How to Survive Anything and Anywhere in the World (A Comprehensive Guide to Preparing for and Overcoming Challenges of Earthquakes)From EverandSurvival Skills: How to Survive Anything and Anywhere in the World (A Comprehensive Guide to Preparing for and Overcoming Challenges of Earthquakes)No ratings yet
- UX Uvex Stealth Uvex Catalog 2012 HRDocument59 pagesUX Uvex Stealth Uvex Catalog 2012 HRLuis Márquez SánchezNo ratings yet
- Twisted Wedding by B. B. HamelDocument345 pagesTwisted Wedding by B. B. Hamelbansodesnehal1616No ratings yet
- Jurnal 6Document7 pagesJurnal 6ayuNo ratings yet
- Betadine® 5%sterile OphthalmicPrep Solution (Povidone-Iodine Ophthalmic Solution) (0.5% Available Iodine)Document1 pageBetadine® 5%sterile OphthalmicPrep Solution (Povidone-Iodine Ophthalmic Solution) (0.5% Available Iodine)ferhat karaağaçNo ratings yet
- The Effect of Xanthophyll Supplementation Upon Macular Pigment and Glare Photostress RecoveryDocument5 pagesThe Effect of Xanthophyll Supplementation Upon Macular Pigment and Glare Photostress RecoveryashurarayNo ratings yet
- Form 1-A (See Rules 5 (1), (3), 7,10 (A), 14 (D), and 18 (D) ) : Certificate of Medical FitnessDocument1 pageForm 1-A (See Rules 5 (1), (3), 7,10 (A), 14 (D), and 18 (D) ) : Certificate of Medical FitnesskawaljitNo ratings yet
- Focus Data Action Responce: Risk For Injury Related To Vision or As Evidence byDocument2 pagesFocus Data Action Responce: Risk For Injury Related To Vision or As Evidence byChiara FajardoNo ratings yet
- Hyphema in GoatDocument3 pagesHyphema in GoatMuhammad HasnainNo ratings yet
- 23 Facts About Your EyesDocument6 pages23 Facts About Your EyesRatnaPrasadNalamNo ratings yet
- VitriolageDocument3 pagesVitriolageSandeep BansalNo ratings yet
- Multex SDS GBR Ver. 03.00Document8 pagesMultex SDS GBR Ver. 03.00FBNo ratings yet
- BS-C SDSDocument8 pagesBS-C SDSBoston BabasaNo ratings yet
- Physical Exmination Head To ToeDocument28 pagesPhysical Exmination Head To ToeJoshNo ratings yet
- 9 Electrical Jack HammerDocument3 pages9 Electrical Jack HammersizweNo ratings yet
- ProP Ophthalmic Examination Made EasyDocument5 pagesProP Ophthalmic Examination Made EasyRosario AyalaNo ratings yet
- Basic Rigging and Slinging (Slide Show) Update DECEMBER 2009Document111 pagesBasic Rigging and Slinging (Slide Show) Update DECEMBER 2009hk331984No ratings yet
- Posh Training Schedule - MHQ - 230227 - 135741Document13 pagesPosh Training Schedule - MHQ - 230227 - 135741Sugirtha PrabhaNo ratings yet
- Neuro Vital Signs FormDocument2 pagesNeuro Vital Signs FormAbegail TabuniagNo ratings yet
- EENT NotesDocument12 pagesEENT NotesMhae TabasaNo ratings yet
- Special Senses (Reviewer!!)Document3 pagesSpecial Senses (Reviewer!!)Madelle Capending DebutonNo ratings yet
- Black Russian Terrier: Official UKC Breed StandardDocument3 pagesBlack Russian Terrier: Official UKC Breed StandardBulyovszky DettiNo ratings yet
- 13 Areas of Assessment FrejDocument3 pages13 Areas of Assessment FrejJoMa TuazonNo ratings yet
- Orthoptic Eval and Treatment in Orbital FracturesDocument10 pagesOrthoptic Eval and Treatment in Orbital Fractureslaljadeff12No ratings yet
- Msds Baseline 2019Document3 pagesMsds Baseline 2019Sariman SalimNo ratings yet
- Material Safety Data Sheet: F112 Surfactant F112Document8 pagesMaterial Safety Data Sheet: F112 Surfactant F112sajad gohariNo ratings yet
- Bes700 Bes710 en Ru A5 260819Document36 pagesBes700 Bes710 en Ru A5 260819Евгений МаркеловNo ratings yet
- 9040bs Msds EnglishDocument5 pages9040bs Msds EnglishUtilities2No ratings yet
- Laser For Cataract SurgeryDocument2 pagesLaser For Cataract SurgeryAnisah Maryam DianahNo ratings yet
- Cambridge International Advanced Subsidiary and Advanced LevelDocument8 pagesCambridge International Advanced Subsidiary and Advanced LevelhbuzdarNo ratings yet
- Scoring PSGDocument23 pagesScoring PSGMilky UniqueNo ratings yet
Checklist Administering Ophthalmic Instillations
Checklist Administering Ophthalmic Instillations
Uploaded by
Janna LacastesantosOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Checklist Administering Ophthalmic Instillations
Checklist Administering Ophthalmic Instillations
Uploaded by
Janna LacastesantosCopyright:
Available Formats
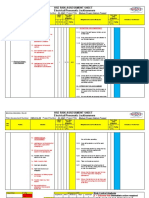
Ateneo de Zamboanga University
COLLEGE OF NURSING
PERFORMANCE EVALUATION CHECKLIST
NAME: _____________________________________ DATE PERFORMED: _________________
YEAR & SECTION: ______________
ADMINISTERING OPHTHALMIC INSTILLATIONS
Definition: Ophthalmic drug administration is the administration of a drug to the eyes,
most typically as an eye drop formulation. May also use as a form of lotions,
ointment, suspension or contact lens solution.
Purpose: 1. For the treatment of disease
2. For symptomatic release of symptoms
3. For diagnostic purpose
4. As aid to surgical procedures
PREPARATION 1 2 3 4 5
Assess:
The appearance of eye and surrounding
structures for lesions, exudate, erythema, or
swelling.
The location and nature of any discharge,
lacrimation, and swelling of the eyelids or of the
lacrimal gland.
Client complaints such as itching, burning pain,
blurred vision, and photophobia.
Client behavior such as squinting, blinking
excessively, frowning, or rubbing the eyes.
Determine:
If assessment data influence the administration of
the medication.
Assemble equipment:
Clean gloves
Sterile, absorbent sponges soaked in sterile
normal saline
Medication
Sterile eye dressing (pad), as needed, and paper
eye tape to secure it
For irrigation, add:
Irrigating solution (e.g., normal saline) and
irrigating syringe or tubing;
Dry, sterile absorbent sponges
Moisture-resistant towel
Basin (e.g., emesis basin).
Check the Medicine Administration Record (MAR) for
the drug name, dose, and strength. Also confirm the
prescribed frequency of the instillation and which eye
is to be treated.
Know why the client is receiving the medication, the
drug classification, contraindications, usual dose
range, side effects, and nursing considerations for
administering and evaluating the intended outcomes
of the medication.
PROCEDURE
1. Compare the label on the medication tube or bottle
with the medication record, and check the expiration
date.
2. If necessary, calculate the medication dosage.
3. Introduce yourself and verify the client’s identity.
Explain to the client what you are going to do, why it
is necessary, and how the client can cooperate.
4. Perform hand hygiene and observe other appropriate
infection control procedures.
5. Provide for client privacy.
Prepare the client.
6. Assist the client to a comfortable position, either
sitting or lying.
7. Clean the eyelid and the eyelashes.
8. Put on clean gloves.
Administer the eye medication.
9. Check the ophthalmic preparation for the name,
strength, and number of drops, if a liquid is used.
Draw the correct number of drops into the shaft of
the dropper, if a dropper is used. If ointment is used,
discard the first bead.
10. Instruct the client to look up to the ceiling. Give the
client a dry, sterile, absorbent sponge.
11. Expose the lower conjunctival sac by placing the
thumb or fingers of your non dominant hand on the
client’s cheekbone, just below the eye, and gently
drawing down the skin on the cheek. If the tissues
are edematous, handle the tissues carefully to avoid
damaging them.
12. Holding the medication in the dominant hand, place
your hand on client’s forehead to stabilize your hand.
Instill the correct number of drops onto the outer third
of the lower conjunctival sac. Hold the dropper 1–2
cm (0.4–0.8 inches) above the sac;
OR
13. Holding the tube above the lower conjunctival sac,
squeeze 2 cm (0.8 inches) of ointment from the tube
into the lower conjunctival sac from the inner canthus
outward.
14. Instruct the client to close eyelids but not to squeeze
them shut.
15. For liquid medications, press firmly or have the client
press firmly on the nasolacrimal duct for at least 30
seconds.
Variation Irrigation
PROCEDURE
16. Place absorbent pads under the head, neck, and
shoulders. Place an emesis basin next to the eye to
catch drainage.
17. Expose the lower conjunctival sac. Or, to irrigate in
stages, first hold the lower lid down, then hold the
upper lid up. Exert pressure on the bony
prominences of the cheekbone and beneath the
eyebrow when holding the eyelids.
18. Fill and hold the eye irrigator about 2.5 cm (1 inch)
above the eye.
19. Irrigate the eye, directing the solution onto the lower
conjunctival sac and from the inner canthus to the
outer canthus.
20. Irrigate until the solution leaving the eye is clear (no
discharge is present), or until all the solution has
been used.
21. Instruct the client to close and move the eye
periodically.
22. Clean and dry the eyelids as needed. Wipe the
eyelids gently from the inner to the outer canthus to
collect excess medication.
23. Apply an eye pad, if needed, and secure it with paper
eye tape.
Assess the client’s response.
24. Assess responses immediately after the instillation or
irrigation, and again after the medication should have
acted.
Document all relevant assessments and
interventions.
25. Include the name of the drug or irrigating solution,
the strength, the number of drops, if it was a liquid
medication, the time, and the response of the client.
TOTAL
________________________
Clinical Instructor
(Sign over printed name)
You might also like
- Administering An IntradermalDocument7 pagesAdministering An IntradermalCzarina Mae Quinones TadeoNo ratings yet
- Best Practices Procedure For Instillation of Eye DropsDocument1 pageBest Practices Procedure For Instillation of Eye DropsRahul ModiNo ratings yet
- Oral MedicationDocument30 pagesOral MedicationPetit NacarioNo ratings yet
- Administering Ophthalmic InstillationsDocument3 pagesAdministering Ophthalmic InstillationsFarsee AdilNo ratings yet
- Eent Group 3Document31 pagesEent Group 3Leonifel BersaminaNo ratings yet
- Administering An Intradermal InjectionDocument3 pagesAdministering An Intradermal Injectionco230847No ratings yet
- Week 7Document53 pagesWeek 7MICHAEL ANDRE COROSNo ratings yet
- Administering Oral Medications: Melendez, Anna Carmela PDocument19 pagesAdministering Oral Medications: Melendez, Anna Carmela PAnna Carmela P. MelendezNo ratings yet
- Administering A Subcutaneous InjectionDocument4 pagesAdministering A Subcutaneous Injectionco230847No ratings yet
- ID-IM-SQ-E ToolDocument9 pagesID-IM-SQ-E TooltriciacamilleNo ratings yet
- Administering An Intramuscular InjectionDocument4 pagesAdministering An Intramuscular Injectionco230847No ratings yet
- Administering Opthalmic MedicationsDocument6 pagesAdministering Opthalmic MedicationsJulianne B. Dela CruzNo ratings yet
- Checklist Administering An Intramuscular InjectionDocument3 pagesChecklist Administering An Intramuscular InjectionCAMPOSANO, JHANNA MARIENo ratings yet
- Assessing The Nose and SinusesDocument2 pagesAssessing The Nose and SinusesAccey RamirezNo ratings yet
- Administering Opthalmic MedicationsDocument5 pagesAdministering Opthalmic MedicationsAnika PleñosNo ratings yet
- Checklist Credes ProphylaxisDocument1 pageChecklist Credes ProphylaxisAliza AlyyNo ratings yet
- Topical AdministrationDocument36 pagesTopical AdministrationSilpa Jose TNo ratings yet
- Administration Eye DropsDocument13 pagesAdministration Eye DropsyaraNo ratings yet
- P-19 Administering-Ophthalmic-InstallationDocument3 pagesP-19 Administering-Ophthalmic-InstallationJeleeey AlarconNo ratings yet
- Administering Ophthalmic MedicationsDocument2 pagesAdministering Ophthalmic MedicationsRoxi MalaqueNo ratings yet
- Eye Ear Med Instillation Procedure RationaleDocument6 pagesEye Ear Med Instillation Procedure Rationaleyuuki konnoNo ratings yet
- Checklist-Medication 2Document7 pagesChecklist-Medication 2michelleciubalbarbosa16No ratings yet
- Assessment Nose SinusesDocument2 pagesAssessment Nose SinusesSyphar IndasanNo ratings yet
- Clinical Learning Skills Laboratory: College of NursingDocument3 pagesClinical Learning Skills Laboratory: College of NursingBeverly DatuNo ratings yet
- Checklist Opthalmic MedDocument3 pagesChecklist Opthalmic MedamaNo ratings yet
- RLE PrelimsDocument8 pagesRLE PrelimsNicole VallejosNo ratings yet
- Level 2 2nd Sem ChecklistDocument31 pagesLevel 2 2nd Sem ChecklistMart Juaresa YambaoNo ratings yet
- Eye Instillation Procedure Guide NursingDocument3 pagesEye Instillation Procedure Guide NursingTrisha ApillanesNo ratings yet
- SL PNCM 1079 Administering An Intramuscular InjectionDocument3 pagesSL PNCM 1079 Administering An Intramuscular Injectionpreciouslagundi226No ratings yet
- Eye Swabbing and Instillation of Eye DropDocument4 pagesEye Swabbing and Instillation of Eye Dropsinuaish syaNo ratings yet
- Module-Intradermal Etool PDFDocument7 pagesModule-Intradermal Etool PDFErika Danalle ArceoNo ratings yet
- Procedure: Administering An Intradermal Injection For Skin TestDocument3 pagesProcedure: Administering An Intradermal Injection For Skin TestSofia AmistosoNo ratings yet
- Administering An Intramuscular InjectionDocument3 pagesAdministering An Intramuscular InjectionPattNo ratings yet
- Administering IntradermalDocument4 pagesAdministering IntradermalNezukoNo ratings yet
- Eye Irrig RDDocument3 pagesEye Irrig RDJames Kristopher RebayaNo ratings yet
- Preparing Meds From Ampules and VialsDocument7 pagesPreparing Meds From Ampules and VialsZyra ObedencioNo ratings yet
- GuidesDocument10 pagesGuidesJClaudz PilapilNo ratings yet
- IntradermalDocument7 pagesIntradermalKyle Dapulag100% (1)
- Checklist For Motuth Neck and EyesDocument7 pagesChecklist For Motuth Neck and EyesWylyn Mae VisqueraNo ratings yet
- Medication AdministrationDocument15 pagesMedication AdministrationbasheNo ratings yet
- Parenteral PRDocument4 pagesParenteral PRGlecy CastañaresNo ratings yet
- Administering Intradermal InjectionDocument17 pagesAdministering Intradermal InjectionPattNo ratings yet
- Republic of The Philippines: Tarlac State University College of Science Nursing DepartmentDocument26 pagesRepublic of The Philippines: Tarlac State University College of Science Nursing DepartmentMaxeneDhale100% (1)
- Parenteral Catheterization Enema ChecklistDocument8 pagesParenteral Catheterization Enema ChecklistJessoliver GalvezNo ratings yet
- Activity 2 Updated MurilloDocument22 pagesActivity 2 Updated MurilloAraw GabiNo ratings yet
- Medication AdministrationDocument88 pagesMedication AdministrationKBD100% (1)
- Medication AdministrationDocument100 pagesMedication AdministrationMJ Jomoc ArejolaNo ratings yet
- Mark King Joseph P. Cordovilla - Mid1a - CP100 - Module 9Document5 pagesMark King Joseph P. Cordovilla - Mid1a - CP100 - Module 9Mark king Joseph CordovillaNo ratings yet
- Preparing Med From A Vial ChecklistDocument5 pagesPreparing Med From A Vial ChecklistRalf FiedalinoNo ratings yet
- PARENTERAL MEDICATION Manual and Checklist 1Document14 pagesPARENTERAL MEDICATION Manual and Checklist 1Hazel Shaine BaybayanNo ratings yet
- PERFORMANCE CRITERIA CHECKLIST Oral Otic Optic Parenteral Drug AdministrationDocument3 pagesPERFORMANCE CRITERIA CHECKLIST Oral Otic Optic Parenteral Drug AdministrationRayzl GacayanNo ratings yet
- PRS InjectionsDocument3 pagesPRS InjectionsLuke SmithNo ratings yet
- Administering Medication Via A Small-Volume NebulizerDocument2 pagesAdministering Medication Via A Small-Volume NebulizerJerilee SoCute WattsNo ratings yet
- MedicationDocument9 pagesMedicationtolchakebede163No ratings yet
- ID IM ChecklistDocument2 pagesID IM Checklistzmv627j7kgNo ratings yet
- Administering Oral Medications 1Document7 pagesAdministering Oral Medications 1co230847No ratings yet
- Small Volume Neb Checklist 2Document3 pagesSmall Volume Neb Checklist 2Katelinne DabucolNo ratings yet
- Subcutaneus Injection TechniqueDocument4 pagesSubcutaneus Injection TechniqueReza Fitra Kusuma NegaraNo ratings yet
- Survival Skills: How to Survive Anything and Anywhere in the World (A Comprehensive Guide to Preparing for and Overcoming Challenges of Earthquakes)From EverandSurvival Skills: How to Survive Anything and Anywhere in the World (A Comprehensive Guide to Preparing for and Overcoming Challenges of Earthquakes)No ratings yet
- UX Uvex Stealth Uvex Catalog 2012 HRDocument59 pagesUX Uvex Stealth Uvex Catalog 2012 HRLuis Márquez SánchezNo ratings yet
- Twisted Wedding by B. B. HamelDocument345 pagesTwisted Wedding by B. B. Hamelbansodesnehal1616No ratings yet
- Jurnal 6Document7 pagesJurnal 6ayuNo ratings yet
- Betadine® 5%sterile OphthalmicPrep Solution (Povidone-Iodine Ophthalmic Solution) (0.5% Available Iodine)Document1 pageBetadine® 5%sterile OphthalmicPrep Solution (Povidone-Iodine Ophthalmic Solution) (0.5% Available Iodine)ferhat karaağaçNo ratings yet
- The Effect of Xanthophyll Supplementation Upon Macular Pigment and Glare Photostress RecoveryDocument5 pagesThe Effect of Xanthophyll Supplementation Upon Macular Pigment and Glare Photostress RecoveryashurarayNo ratings yet
- Form 1-A (See Rules 5 (1), (3), 7,10 (A), 14 (D), and 18 (D) ) : Certificate of Medical FitnessDocument1 pageForm 1-A (See Rules 5 (1), (3), 7,10 (A), 14 (D), and 18 (D) ) : Certificate of Medical FitnesskawaljitNo ratings yet
- Focus Data Action Responce: Risk For Injury Related To Vision or As Evidence byDocument2 pagesFocus Data Action Responce: Risk For Injury Related To Vision or As Evidence byChiara FajardoNo ratings yet
- Hyphema in GoatDocument3 pagesHyphema in GoatMuhammad HasnainNo ratings yet
- 23 Facts About Your EyesDocument6 pages23 Facts About Your EyesRatnaPrasadNalamNo ratings yet
- VitriolageDocument3 pagesVitriolageSandeep BansalNo ratings yet
- Multex SDS GBR Ver. 03.00Document8 pagesMultex SDS GBR Ver. 03.00FBNo ratings yet
- BS-C SDSDocument8 pagesBS-C SDSBoston BabasaNo ratings yet
- Physical Exmination Head To ToeDocument28 pagesPhysical Exmination Head To ToeJoshNo ratings yet
- 9 Electrical Jack HammerDocument3 pages9 Electrical Jack HammersizweNo ratings yet
- ProP Ophthalmic Examination Made EasyDocument5 pagesProP Ophthalmic Examination Made EasyRosario AyalaNo ratings yet
- Basic Rigging and Slinging (Slide Show) Update DECEMBER 2009Document111 pagesBasic Rigging and Slinging (Slide Show) Update DECEMBER 2009hk331984No ratings yet
- Posh Training Schedule - MHQ - 230227 - 135741Document13 pagesPosh Training Schedule - MHQ - 230227 - 135741Sugirtha PrabhaNo ratings yet
- Neuro Vital Signs FormDocument2 pagesNeuro Vital Signs FormAbegail TabuniagNo ratings yet
- EENT NotesDocument12 pagesEENT NotesMhae TabasaNo ratings yet
- Special Senses (Reviewer!!)Document3 pagesSpecial Senses (Reviewer!!)Madelle Capending DebutonNo ratings yet
- Black Russian Terrier: Official UKC Breed StandardDocument3 pagesBlack Russian Terrier: Official UKC Breed StandardBulyovszky DettiNo ratings yet
- 13 Areas of Assessment FrejDocument3 pages13 Areas of Assessment FrejJoMa TuazonNo ratings yet
- Orthoptic Eval and Treatment in Orbital FracturesDocument10 pagesOrthoptic Eval and Treatment in Orbital Fractureslaljadeff12No ratings yet
- Msds Baseline 2019Document3 pagesMsds Baseline 2019Sariman SalimNo ratings yet
- Material Safety Data Sheet: F112 Surfactant F112Document8 pagesMaterial Safety Data Sheet: F112 Surfactant F112sajad gohariNo ratings yet
- Bes700 Bes710 en Ru A5 260819Document36 pagesBes700 Bes710 en Ru A5 260819Евгений МаркеловNo ratings yet
- 9040bs Msds EnglishDocument5 pages9040bs Msds EnglishUtilities2No ratings yet
- Laser For Cataract SurgeryDocument2 pagesLaser For Cataract SurgeryAnisah Maryam DianahNo ratings yet
- Cambridge International Advanced Subsidiary and Advanced LevelDocument8 pagesCambridge International Advanced Subsidiary and Advanced LevelhbuzdarNo ratings yet
- Scoring PSGDocument23 pagesScoring PSGMilky UniqueNo ratings yet