Professional Documents
Culture Documents
Bupropion
Bupropion
Uploaded by
RJ HOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Bupropion
Bupropion
Uploaded by
RJ HCopyright:
Available Formats
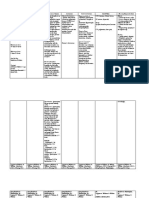
BUPROPION
Synonyms
Wellbutrin®, Zyban®, Contrave® (combination with naltrexone), amfebutamone
Description
Used in treatment of depression and attention deficit hyperactivity disorders, and as an aid to smoking cessation.
Available in Canada as sustained release (SR) and extended release (XL) tablets. Immediate release (IR) formulations
are also available in the US.
Toxicity in a single patient in this dose range. Occurrence of
Bupropion commonly causes sinus tachycardia, seizures or coma increased with higher doses and
hypertension, agitation and GI symptoms. Large when the ingested dose was unknown. Authors
overdoses can result in seizures (single or multiple), recommended referral to a healthcare facility if the
QRS prolongation, ventricular dysrhythmias and ingested dose was greater than 10 mg/kg (a single
cardiac arrest. Cardiac arrest is often fatal. tablet in a small child) or if the dose was unknown.
Aggressive GI decontamination and early transfer to
an ECMO centre should be considered in large Case Reports
overdoses. A 23-year-old ingested 15 g bupropion XL and by 4
hours post ingestion had HR 135, BP 140/72 with
Mechanism of Toxicity confusion, diaphoresis, abnormal movements,
A cathinone derivative, structurally similar to hypertonicity, clonus, and had a 30-second
amphetamines and bath salts. Bupropion and its generalized tonic-clonic seizure. He was intubated on
active metabolite inhibit reuptake of dopamine and arrival to ER. ECG showed sinus tachycardia, QRS
norepinephrine (minimally inhibits serotonin 114 ms, terminal R wave in aVR. QRS continued to
reuptake). No significant anticholinergic or widen despite repeated boluses of sodium
monoamine oxidase inhibitor activity. Mechanism for bicarbonate and BP worsened. ECMO was started at
seizures and cardiotoxicity is unclear. QRS widening 9.5 hours post ingestion and continued for 42 hours.
may be due to cardiac myocyte gap junction inhibition By day 5, patient was walking independently and
rather than sodium channel blockade. recovered without sequelae.
See Case Reports. A 41-year-old ingested 18 g bupropion XL and
presented to hospital within 2 hours post ingestion.
Toxic Dose Ten hours post ingestion patient had 2 seizures; by
Variable. 11 hours post ingestion patient developed apnea and
Adult: In a review of bupropion overdoses in 385 asystole after a 3rd seizure. Following resuscitation,
patients, 12-57 years, seizures were reported in 11% ECG showed QRS 0.156 sec which initially
of patients. Doses associated with seizures ranged responded to sodium bicarbonate boluses. Recurrent
from 600 mg up to 18 g; seizures were most common QRS widening over the next 10 hours was followed
with > 2.5 g bupropion alone or when bupropion, by another cardiac arrest. Patient was resuscitated
irrespective of dose, was taken with other stimulants. but remained unresponsive requiring pressor support.
Deaths attributed to bupropion alone have typically By 36 hours post ingestion patient had suffered 2
involved large ingestions resulting in multiple more cardiac arrests; resuscitation was discontinued.
uncontrolled seizures rapidly progressing to A 31-year-old ingested 13.5 g bupropion SR with
ventricular dysrhythmias, cardiogenic shock, and ethanol and by 6 hours post ingestion exhibited
cardiac arrest. However, as little as 1.5 g SR in an agitation, tachycardia, hypertension, tremor, dystonia,
adult has resulted in recurrent, prolonged seizures hyperreflexia and clonus. Coma, recurrent seizures
and cardiac arrest. Patient recovered following and wide complex tachycardia developed requiring
resuscitation and ICU supportive care. sedation, intubation and ventilation. Patient recovered
With therapeutic doses up to 450 mg per day, with intensive care.
incidence of seizures is approximately 0.4%. In a A 14-year-old ingested 1.5-3 g bupropion and by 5-6
review of unintentional bupropion medication errors in hours post ingestion developed vomiting, drowsiness,
491 adults, the risk of having a seizure with doses slurred speech, hallucinations and sinus tachycardia.
ranging from 600 -1200 mg was 0.6% (median time Patient had two single seizures within the first 24
was 9.6 hrs post ingestion; range 2 hrs -21.5 hrs post hours. At 18 hours post ingestion, patient experienced
ingestion). a brief self-limiting episode of extreme agitation and
Pediatric: Ingestion of > 10 mg/kg in young children combativeness. Patient recovered without sequelae.
can result in toxicity. A 17-year-old ingested 2 tablets of 300 mg and had a
US poison control centres reported 6,000 pediatric single seizure at 11.5 hrs post ingestion. Patient
bupropion exposures over a 7-year period. With recovered without sequelae.
doses up to 10 mg/kg, a few children developed
tachycardia, irritability, drowsiness, ataxia,
hallucinations, lethargy and tremor. Seizures occurred
Poison Management Manual (PMM)
BC Drug and Poison Information Centre, Vancouver, BC
604-682-5050 or 1-800-567-8911 www.dpic.org
July 2019
BUPROPION - 2
Pharmacokinetics Confusion, dizziness, hallucinations (auditory,
Well absorbed. Peak plasma levels (therapeutic visual) paresthesias, slurred speech,
dosing) reached within 3 hours following ingestion of extrapyramidal symptoms and psychosis may
SR form; 5 hours after XL form; and 1.5 hours after IR also be seen.
form. Peak may be delayed following overdose. GI: Vomiting (common), nausea, empty tablet
Pharmacobezoars and empty tablet shells have been shells can appear in emesis or stool.
seen in emesis as late as 7-8 hours post ingestion. Fluid/Lytes/Acid-Base: Hypokalemia,
Extensively metabolized to active metabolites. hypophosphatemia, metabolic acidosis.
Elimination half-life of bupropion with therapeutic Musculoskeletal: Choreoathetosis, increased
dosing is 21 hours (range 8-36 hours); half-life of muscle tone, clonus, dystonia.
active metabolites ranges from 20-37 hours. Lab: False positive urine toxicology screen for
amphetamines.
Clinical Effects
Inhalation: Insufflation of crushed tablets can Treatment
result in seizures; most occur within first 8 hours. 1. Asymptomatic patients should have continuous
Sinus tachycardia is present in most patients who cardiac monitoring and monitoring of vital signs
seize. for 18 hours. An ECG should be done on
Injection: Injection can result in systemic signs. presentation and prior to discharge. Children
Severe skin lesions and vascular complications ingesting more than 10 mg/kg or adults
have been reported. Inadvertent intra-arterial ingesting 600 mg or more should be observed
injection of bupropion and cocaine into the and monitored in a health care facility.
vertebral artery resulted in a fatal brainstem
infarct. 2. Symptomatic patients should be monitored for at
Ingestion: least 12 hours after resolution of symptoms.
General: Vomiting, seizures, agitation, tremor,
hallucinations, sinus tachycardia and QTc 3. Activated charcoal may be useful several hours
prolongation are common and may be delayed. after ingestion. For large overdoses, aggressive
Seizures are often delayed; usually within 18 GI decontamination should be considered. If
hours of exposure. Single seizures are most patient needs to be intubated for management
common; seizures are typically brief with no long- of agitation or seizures, WBI should be started
term sequelae. Multiple seizures may occur; once airway is protected.
status epilepticus is uncommon except in large
overdoses. Neurologic effects such as agitation, 4. Protect airway and assist ventilation as needed.
tremors, hallucinations often are observed prior Consider early intubation for control of agitation
to seizure activity. or seizures.
With large overdoses multiple seizures can
progress rapidly to cardiovascular toxicity and 5. Maintain fluid and electrolyte balance.
death.
HEENT: Mydriasis (common); pupils may be 6. Monitor vital signs; obtain an initial ECG and
fixed and dilated in large overdoses. electrolytes. Monitor blood gases in
CVS: Sinus tachycardia (common), prolonged symptomatic patients. Repeat ECG; QRS and
QTc interval (common, may be delayed). QT prolongation may be delayed.
Hypertension and hypotension (less common)
can also occur. Widened QRS complex, 7. Sinus tachycardia rarely requires treatment. QTc
ventricular dysrhythmias, cardiogenic shock, prolongation should be closely monitored and
asystole and death may occur following large electrolytes corrected as needed.
overdoses. Cardiac arrest from bupropion is
often fatal. QRS widening may be due to 8. Hypotension unresponsive to IV fluids may
inhibition of cardiac myocyte gap junction require vasopressors. Hypertension does not
inhibition rather than sodium channel blockade. usually require treatment.
Neurologic: Lethargy (common), agitation
(common), tremors (common), generalized 9. Agitation and seizures should be treated
seizures (common, may be delayed), status aggressively with IV benzodiazepines. Consider
epilepticus (large overdoses). With large early intubation and sedation with propofol or
overdoses multiple seizures can progress rapidly midazolam infusion for patients with more than a
to cardiovascular toxicity and death. Pupils may single seizure. Avoid phenytoin as it is not
be fixed and dilated in large overdoses. effective and may worsen cardiac toxicity.
In one study, 40/41 patients developed
neurologic symptoms such as agitation, tremors,
and hallucinations prior to having a seizure.
Poison Management Manual (PMM)
BC Drug and Poison Information Centre, Vancouver, BC
604-682-5050 or 1-800-567-8911 www.dpic.org
July 2019
BUPROPION - 3
10. Wide complex tachycardia (QRS > 0.1 sec) 13. IV lipid emulsion therapy can be considered for
should be treated initially with IV sodium cardiogenic shock or cardiac arrest refractory to
bicarbonate boluses. QRS widening may not standard ACLS protocols in centres where
respond to sodium bicarbonate boluses as the ECMO is not available. Note: Lipid emulsion
mechanism is thought to be due to myocyte gap therapy can result in acute pancreatitis, interfere
junction inhibition rather than sodium channel with a number of lab investigations, and impede
blockade. performance of ECMO or hemodialysis.
See Lipid Emulsion Antidote monograph.
11. Standard supportive measures (ACLS protocols,
sodium bicarbonate boluses) should be used but 14. Hemodialysis is not useful in enhancing
are unlikely to be effective. Lipid emulsion elimination of bupropion but may be required in
therapy or ECMO should be considered (see critically ill patients.
below).
12. Early referral to a centre with ECMO capabilities
should be considered with large overdoses.
Key Points
Asymptomatic patients should have continuous cardiac monitoring and monitoring of vital signs for a
minimum of 18 hours. An ECG should be done on presentation and prior to discharge. Children ingesting
more than 10 mg/kg or adults ingesting 600 mg or more should be observed and monitored in a health care
facility.
Symptomatic patients should be monitored for at least 12 hours after resolution of symptoms.
Early intubation, aggressive GI decontamination and early transfer to an ECMO centre should be considered
in large overdoses.
Delayed and recurrent dose-related seizures are common (first seizure may be delayed for up to 18 hours).
Seizures following insufflation usually occur within the first 8 hours.
Treatment is symptomatic and supportive with aggressive management of agitation and seizures using IV
benzodiazepines, barbiturates, propofol. Consider early intubation and sedation with propofol or midazolam
infusion for patients with more than a single seizure.
Sinus tachycardia and QTc interval prolongation are common, may be delayed and rarely require treatment.
QRS prolongation, life-threatening dysrhythmias, cardiogenic shock, asystole and death can occur following
large overdoses.
QRS prolongation should be managed initially with IV sodium bicarbonate boluses. However, it may not
respond to bicarbonate as the mechanism may not be due to sodium channel blockade.
Standard supportive measures (ACLS protocols, sodium bicarbonate boluses) should be used but are
unlikely to be effective.
ECMO may be helpful for patients not responding to standard ACLS protocols.
If ECMO is unavailable, IV lipid emulsion therapy should be considered. Note: Lipid emulsion therapy can
result in acute pancreatitis, interfere with some lab investigations, and impede performance of ECMO or
hemodialysis.
Poison Management Manual (PMM)
BC Drug and Poison Information Centre, Vancouver, BC
604-682-5050 or 1-800-567-8911 www.dpic.org
July 2019
You might also like
- Course Task #3: AnswerDocument5 pagesCourse Task #3: AnswerAria100% (3)
- Aerobics ManualDocument33 pagesAerobics ManualGabriela Radulescu0% (1)
- Case Scenario For Community Health NursingDocument5 pagesCase Scenario For Community Health Nursinghemihema100% (1)
- Drug Card PropofolDocument1 pageDrug Card PropofolBenNo ratings yet
- Pain Agitation & Delirium PDFDocument46 pagesPain Agitation & Delirium PDFhuong LNo ratings yet
- Drug Study NewDocument4 pagesDrug Study NewJehannah Dayanara Berdan HayudiniNo ratings yet
- Naplex Complete Study Outline A Topic-Wise Approach DiabetesFrom EverandNaplex Complete Study Outline A Topic-Wise Approach DiabetesRating: 4 out of 5 stars4/5 (3)
- ClearPoint Healthcare KPIsDocument19 pagesClearPoint Healthcare KPIsJosue Paz100% (1)
- Iadt02i6p480 PDFDocument3 pagesIadt02i6p480 PDFVandanaNo ratings yet
- Salbutamol Drug Study Generic Name: Brand NameDocument4 pagesSalbutamol Drug Study Generic Name: Brand NameLyn ConsingNo ratings yet
- 8 Propofol Drug StudyDocument4 pages8 Propofol Drug Studyshadow gonzalez100% (1)
- Drug Study GentamicinDocument3 pagesDrug Study GentamicinEARL GERALD RICAFRANCANo ratings yet
- Drug Study ON Cabergolin EDocument4 pagesDrug Study ON Cabergolin ESimran SimzNo ratings yet
- Drug Study (Haloperidol)Document3 pagesDrug Study (Haloperidol)Mae Ann Bueno CastillonNo ratings yet
- Obat Ayu (Anestesi)Document11 pagesObat Ayu (Anestesi)Ayu PratiwiNo ratings yet
- Propofol Drug StudyDocument3 pagesPropofol Drug StudyAngelica shane Navarro100% (2)
- Status EpilepticusDocument3 pagesStatus EpilepticusVandeosNo ratings yet
- Presentation 2Document20 pagesPresentation 2Muhammad UmairNo ratings yet
- Brajac - ProtocolDocument13 pagesBrajac - Protocolthanh ngôNo ratings yet
- AcetaminophenDocument5 pagesAcetaminophenAnonNo ratings yet
- ZofranOndansetron Dr. A. Alisher PPT 14.08.2011 LECTURE... IFTARDocument58 pagesZofranOndansetron Dr. A. Alisher PPT 14.08.2011 LECTURE... IFTARAlisher Agzamov100% (1)
- Evaluation and Management of Delayed Awakening or Emergence From AnaesthesiaDocument19 pagesEvaluation and Management of Delayed Awakening or Emergence From AnaesthesiaMuhammad UmairNo ratings yet
- Drug Study: Adult: Induction: 40 MGDocument2 pagesDrug Study: Adult: Induction: 40 MGpretty_mary100% (4)
- Organophosphate Poisoning 2Document12 pagesOrganophosphate Poisoning 2Diana MurguiaNo ratings yet
- Drug StudyDocument3 pagesDrug StudyCyril_Cybernat_1553No ratings yet
- COPD - Drug FormularyDocument32 pagesCOPD - Drug FormularyCharles BayogNo ratings yet
- PoisoningDocument36 pagesPoisoningsalah almozahemNo ratings yet
- Ipratroprium Drug CardDocument3 pagesIpratroprium Drug CardXiaoDuckyNo ratings yet
- Common Poisonings (Toxidromes) 1 1 1Document131 pagesCommon Poisonings (Toxidromes) 1 1 1ram7676No ratings yet
- Afebrile SeizuresDocument6 pagesAfebrile SeizuresKristoffer EscletoNo ratings yet
- Chlorpromazine Drug StudyDocument10 pagesChlorpromazine Drug Studyshadow gonzalezNo ratings yet
- AminophyllineDocument3 pagesAminophyllineAmna Kazmi ShehzadNo ratings yet
- Final Salbu-IpraDocument3 pagesFinal Salbu-IpraGwyn RosalesNo ratings yet
- Drug Study: PART 1: To Be Completed Prior To Clinical ExperienceDocument5 pagesDrug Study: PART 1: To Be Completed Prior To Clinical ExperienceFrozanSNo ratings yet
- Amiodarone Drug StudyDocument3 pagesAmiodarone Drug StudyDexter Niel Ortilano CPAC-SNNo ratings yet
- Management of Pain, Agitation, Delirium, and Neuromuscular Blockade in Adult Intensive Care Unit PatientsDocument48 pagesManagement of Pain, Agitation, Delirium, and Neuromuscular Blockade in Adult Intensive Care Unit PatientsJeremy HamptonNo ratings yet
- Seven Ps For RSI BOARDDocument2 pagesSeven Ps For RSI BOARDJames BrownNo ratings yet
- Oct 12 El Intoxicado Grave Skolnik 2020Document16 pagesOct 12 El Intoxicado Grave Skolnik 2020lfc2086No ratings yet
- v087p00407 PDFDocument4 pagesv087p00407 PDFPuang PhakNo ratings yet
- Citilin® (Amp) : Korea United Pharm Pharma 3 Nootropics & NeurotonicsDocument6 pagesCitilin® (Amp) : Korea United Pharm Pharma 3 Nootropics & NeurotonicsdipenhydramineNo ratings yet
- Ct8 Electrolyte and Acid-Base ImbalancesDocument4 pagesCt8 Electrolyte and Acid-Base ImbalancesAlondra VelascoNo ratings yet
- Albuterol (Salbutamol)Document3 pagesAlbuterol (Salbutamol)Mae Ann Bueno CastillonNo ratings yet
- Drug Study (Cimetidine)Document5 pagesDrug Study (Cimetidine)Frances JaynoNo ratings yet
- Drug 3Document2 pagesDrug 3Nicholas TagleNo ratings yet
- Generic Name Indication Mechanism of Action Classification Side Effects/Adverse Drug Reactions Nursing ResponsibilitiesDocument2 pagesGeneric Name Indication Mechanism of Action Classification Side Effects/Adverse Drug Reactions Nursing ResponsibilitiesNicholas TagleNo ratings yet
- Caso 2 ToxicologiaDocument3 pagesCaso 2 ToxicologiaIza ÁlvarezNo ratings yet
- Open Presentation 74Document17 pagesOpen Presentation 74jonathan paghubasanNo ratings yet
- Lec 4 CNSDocument12 pagesLec 4 CNShusainozelNo ratings yet
- Stiff Person Syndrome and AnesthesiaDocument15 pagesStiff Person Syndrome and AnesthesiaFarhan AshrafNo ratings yet
- 107 FullDocument3 pages107 FullAdam HamidNo ratings yet
- Iligan - DiazepamDocument6 pagesIligan - DiazepamJamaicah IliganNo ratings yet
- Icm 2 Week 6Document34 pagesIcm 2 Week 6Syaimee Annisa AzzahraNo ratings yet
- Menometrorrhagia and Tachyarrhythmia After Using Oral and Topical GinsengDocument4 pagesMenometrorrhagia and Tachyarrhythmia After Using Oral and Topical Ginsengkartika adyaniNo ratings yet
- College of Nursing: Cebu Normal UniversityDocument3 pagesCollege of Nursing: Cebu Normal UniversityGwyn RosalesNo ratings yet
- Metoclopramide DRUG STUDYDocument2 pagesMetoclopramide DRUG STUDYErica FabrigasNo ratings yet
- Drug StudyDocument32 pagesDrug StudyJoanne Bernadette Aguilar100% (1)
- Drug 2Document4 pagesDrug 2Abie Jewel Joy RoqueNo ratings yet
- Cases Colorectal CancerDocument18 pagesCases Colorectal CancerMariam HeshamNo ratings yet
- DRUG STUDY - FurosemideDocument2 pagesDRUG STUDY - FurosemideVANESSA PAULA ALGADORNo ratings yet
- Drug Information Worksheet: Hypertension - 40 Twice DailyDocument57 pagesDrug Information Worksheet: Hypertension - 40 Twice DailyMichelle Davis-JacksonNo ratings yet
- CT Week8Document4 pagesCT Week8Princess Laira CañeteNo ratings yet
- 08 .麻醉用藥 - 邱全秀Document62 pages08 .麻醉用藥 - 邱全秀kenny631653No ratings yet
- A Case Report and Overview of Organophosphate (OP) PoisoningDocument5 pagesA Case Report and Overview of Organophosphate (OP) PoisoningDhruva PatelNo ratings yet
- M7 LN Behavioural Measures of Animal Welfare PDFDocument7 pagesM7 LN Behavioural Measures of Animal Welfare PDFXz RiveraNo ratings yet
- CFTDocument14 pagesCFTNandeesh Kumar.bNo ratings yet
- GRADE HandbookDocument75 pagesGRADE HandbookEzequiel ZacañinoNo ratings yet
- Advocacy Letter-Amy JohnsDocument2 pagesAdvocacy Letter-Amy Johnsapi-239145075No ratings yet
- v07p0681 PDFDocument6 pagesv07p0681 PDFAzizaNo ratings yet
- Atlas BacteriologieDocument104 pagesAtlas BacteriologieMarian Neagu100% (2)
- Learning Strand I - EnglishDocument19 pagesLearning Strand I - EnglishMaricel MaapoyNo ratings yet
- SHSS Placement Brochure 09 - 11Document31 pagesSHSS Placement Brochure 09 - 11healthsutraNo ratings yet
- Rizal Act3&4Document26 pagesRizal Act3&4ma.antonette orsalNo ratings yet
- Nakimuli2016 Article TheBurdenOfMaternalMorbidityAnDocument8 pagesNakimuli2016 Article TheBurdenOfMaternalMorbidityAnPriscilla AdetiNo ratings yet
- Healthcare in TechnologyDocument29 pagesHealthcare in TechnologySHRAVYA MANJUNATHNo ratings yet
- 15Jan2014NIC HSBC FAQDocument14 pages15Jan2014NIC HSBC FAQgetnkNo ratings yet
- Case-Control Study DesignDocument11 pagesCase-Control Study Designmusa onyango obuyaNo ratings yet
- 2013 (4 6-59)Document18 pages2013 (4 6-59)Dani GarnidaNo ratings yet
- Physiology Lecture 3Document28 pagesPhysiology Lecture 3Muhammad Khubaib AzeemNo ratings yet
- The Stolen Bacillus and Other Incidents by Wells, H. G. (Herbert George), 1866-1946Document127 pagesThe Stolen Bacillus and Other Incidents by Wells, H. G. (Herbert George), 1866-1946Gutenberg.org100% (1)
- List of Pharma DrugsDocument6 pagesList of Pharma DrugsAndreaSanchezNo ratings yet
- Kode Diagnosa Rekam MedikDocument3 pagesKode Diagnosa Rekam MedikRahadian SuryantaNo ratings yet
- Assignment of Pathology 401: Submitted byDocument5 pagesAssignment of Pathology 401: Submitted byaymen gulzarNo ratings yet
- Operating RoomDocument9 pagesOperating RoomMarie Ashley CasiaNo ratings yet
- Thi thử Anh Chuyên Vĩnh Phúc lần 1 tháng 5-2012Document6 pagesThi thử Anh Chuyên Vĩnh Phúc lần 1 tháng 5-2012Trường Học Số100% (1)
- Community Health Nursing (CHN) - Heart of Nursing PH PDFDocument8 pagesCommunity Health Nursing (CHN) - Heart of Nursing PH PDFFahtma Irene Faye AnayatinNo ratings yet
- Virtual Microbiology Classroom !: Do Yourself A Favor. Use TheDocument30 pagesVirtual Microbiology Classroom !: Do Yourself A Favor. Use Thevibha_sNo ratings yet
- Differential Diagnosis: Giant Cystic Abdominal Masses in Children and Adolescents: UltrasonicDocument5 pagesDifferential Diagnosis: Giant Cystic Abdominal Masses in Children and Adolescents: UltrasonicGoran MaliNo ratings yet
- Anthonela - Terán SebastiánDocument5 pagesAnthonela - Terán SebastiánJuleyssiNo ratings yet
- Origin of The Pantaneiro Horse in Brazil: Additional Keywords Palabras Clave AdicionalesDocument11 pagesOrigin of The Pantaneiro Horse in Brazil: Additional Keywords Palabras Clave AdicionalesmmbasquesNo ratings yet
- Cataract Manual VISION2020 PDFDocument80 pagesCataract Manual VISION2020 PDFdrsneha222 thoratNo ratings yet