Professional Documents
Culture Documents
Blood Gases
Blood Gases
Uploaded by
Faith0 ratings0% found this document useful (0 votes)
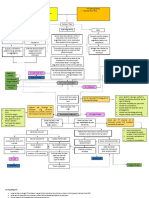
15 views3 pages1. This document defines key terms and parameters related to blood gas analysis and acid-base balance, including the bicarbonate-carbonic acid buffer system, partial pressure of carbon dioxide (pCO2), and classifications of acid-base imbalances.
2. Key parameters evaluated in blood gas analysis include pH, pCO2, and bicarbonate levels, which can indicate whether acid-base imbalances are caused by respiratory or metabolic factors.
3. Acid-base imbalances like metabolic acidosis and alkalosis can have serious consequences if not addressed, including cardiac arrest in cases of severe acidosis or tetany and respiratory failure in alkalosis. Precise blood gas measurement and
Original Description:
CINICAL CHEMISTRY
Blood Gases
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Document1. This document defines key terms and parameters related to blood gas analysis and acid-base balance, including the bicarbonate-carbonic acid buffer system, partial pressure of carbon dioxide (pCO2), and classifications of acid-base imbalances.
2. Key parameters evaluated in blood gas analysis include pH, pCO2, and bicarbonate levels, which can indicate whether acid-base imbalances are caused by respiratory or metabolic factors.
3. Acid-base imbalances like metabolic acidosis and alkalosis can have serious consequences if not addressed, including cardiac arrest in cases of severe acidosis or tetany and respiratory failure in alkalosis. Precise blood gas measurement and
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
0 ratings0% found this document useful (0 votes)
15 views3 pagesBlood Gases
Blood Gases
Uploaded by
Faith1. This document defines key terms and parameters related to blood gas analysis and acid-base balance, including the bicarbonate-carbonic acid buffer system, partial pressure of carbon dioxide (pCO2), and classifications of acid-base imbalances.
2. Key parameters evaluated in blood gas analysis include pH, pCO2, and bicarbonate levels, which can indicate whether acid-base imbalances are caused by respiratory or metabolic factors.
3. Acid-base imbalances like metabolic acidosis and alkalosis can have serious consequences if not addressed, including cardiac arrest in cases of severe acidosis or tetany and respiratory failure in alkalosis. Precise blood gas measurement and
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
You are on page 1of 3
Blood Gases CARBONIC ACID (H2CO3 )
TERMS AND ABBREVIATIONS: ● This fraction of blood, plasma or serum
Acids Includes the undissociated carbonic acid
● substance that can yield a hydrogen ion (H) and the physically dissolved anhydrous
or hydronium ion when dissolved in water C02. Since CO2 concentration is higher
Base than HCO3. The symbol cdCO2 (conc. of
● substance that can yield hydroxyl ions (OH) dissolved C02) is frequently used and is
Buffer measured from pCO2 multiplied by the
● combination of a weak acid or weak base solubility coefficient of' CO2.
and its salt, is a system that resists changes ● Normal range is from 1.05 –1.45 mmol/L.
in pH PARTIAL PRESSURE OF C02 (pC02)
● effectiveness of a buffer: ● The pressure or tension exerted by C02 gas
- pK of the buffering system dissolved in blood. It is an index of efficiency
- pH of the environment of gas exchange in the lungs and not a
● Plasma – bicarbonate-carbonic acid buffer measure of C02 concentration in the blood.
system; pK of 6.1 ● Normal range is 35 - 45 mmHg.
BICARBONATE-CARBONIC ACID BUFFER CARBON DIOXIDE COMBINING POWER (CO2
SYSTEM combining power)
● Principal mammalian buffer system ● The value of the CO2 combining power Is
● Acids combine with Bicarbonates in the an index of the amount of CO2 that can be
blood bound by serum, plasma, or whole blood as
- Neutral Salts (Bicarbonate Salts) HCO3 at a pCO2 of 40 mmHg at 25
- Carbonic Acid (Weak Acid) degrees Celcius.
● H2CO3 unstable, changing to H2O and ● Normal range is 24 - 30 mmol/L.
CO2 in fluid TOTAL CARBON DIOXIDE CONCENTRATION
PHOSPHATE BUFFER SYSTEM (ctCO2)
● 2,3-diphosphoglycerate – Phosphate form ● Formerly known as C02 content, which
that acts as a buffer refers to the total concentration of C02 in
● It increases the amount of NaHCO3 in ECF the blood consisting of ionized HC03, C03,
(more alkaline) carbamino compound) and unionized
● 16% of the non-bicarbonate buffer value fraction (H2C03) and physically dissolved
of Erythrocytes C02.
HEMOGLOBIN-OXYHEMOGLOBIN ● Normal range is 21 - 28 mmol/L.
BUFFER SYSTEM pH
● Maintains pH level (Venous and Arterial a. The negative logarithm of hydrogen ion
Blood) activity with a normal average range of
● 1 gram of Hemoglobin carries 1.39 mL of 7.35-7.45
Oxygen Major factors regulating blood pH:
PROTEIN BUFFER SYSTEM 1. Chemical buffers
● Proteins can exist in 2 forms: H+ protein, B 2. Respiratory regulatory mechanism
Protein 3. Renal regulatory mechanism
● Capability to bind or release excess Henderson-Hasselbalch Equation
Hydrogen as required
● Plasma proteins (Charges on their surface)
- pH > pI – (-) charge
- pH < pI – (+) charge
BICARBONATE (HCO3)
● The second largest fraction of the anions
in the plasma. It includes the ionized
bicarbonate (HC03), carbonate and the
carbamino compounds. Normal range is
from 21 - 28 mmol/L (21 -- 28 meq/L)
BLOOD COLLECTION FOR BLOOD pH
GAS AND pH ANALYSIS ● PH electrode
1. The pCO2 of air (0.2mmHg) Is much less ● Principle: Based on polarographic principle
than that of the blood (38 mmHg) so that ● Use of PH meters
when blood is exposed to air, the ctCO2 and ● Henderson - Hasselbach equation
pCO2 decreases; and the pH increases, ● Nomogram and Slide Rule
thus it is a must to collect, transfer and ● Siggard -Anderson Alignment nomogram
manipulate blood for blood gas analysis in ct C02:
condition where air Is avoided or at least ● Manometric Method Using Natelson
kept at a minimum level. Microgasometer
a. Arterial blood is the more preferred ● Principle:
specimen for blood gas analysis because it - Carbon dioxide is released front
is of more uniform composition than venous HC03 by the addition of lactic add.
blood. This is due to the metabolic diversity The C02 and other gases are,
composing venous samples extracted under a partial vacuum.
The pressure difference at constant
value before and after absorption of
C02 by NaOH Is the amount of C02
present in the sample.
● Venous and Capillary (Skin punctured)
Blood
- These specimens can also used for
blood gas analysis provided that they
undergo arterialization
Method of Determination
p02
● Clark p02 electrode
● Principle: Based on amperometric or
polarographic measurement of oxygen. Alternative Method
● Gasometric analysis ● Principle
● Calculation from oxygen saturation, pH and - Involves the release of C02 gas when
temperature by means of the standard 02 the sample is added to H2S04 with
dissociation curve. subsequent monitoring of this release
● Transcutaneous monitoring with a pair of pCO2 electrodes
pC02 (reference and sample electrodes).
● Use of pCO2 electrode The rate of change in pH of the buffer
- Principle: Based on pH inside the pCO2 electrodes is a
measurement of a stationary measure of the concentration of its
NaHCO3 solution which is in CO2 In the Sample
equilibrium with the test solution and Conditions for analysis:
the test via a CO2 permeable 1. All procedures should be considered “STAT”
membrane. - If delayed 20-30 mins: pH lowers by
● Use of Henderson Hasselbach equation 0.01
from pH and total carbon dioxide. - Avoid glycolysis
● From a measured pH value interpolated in 2. Specimen must be kept at anaerobic
the C02 equilibrium curve. condition
3. Specimen w/c cannot be analyzed
immediately must be placed in an ice slurry
ACID-BASE DISTURBANCES Consequences of Acid- Base Imbalance:
Acidosis - General term applied for any condition ● In Alkalosis, tetany ensues due to.
where the pH of the blood and the bicarbonate hypocalcemia, which can lead to death
concentration of the blood are below normal. because of respiratory muscle spasm.
Alkalosis ● In Acidosis, there is an inhibition of the
● General term applied for any condition with neural mechanisms which will then lead to
an increase in blood pH (above normal coma. A blood pH of 6.9 has been proven
range) characterized by an elevation in the fatal
H+ ion accepting buffer of the plasma
(UC03) and a reduction in the H+ ion
substances (H2CO3)
Classification of Acid-Base Imbalance
● Metabolic Alkalosis
● Metabolic Acidosis
● Respiratory Alkalosis
● Respiratory Acidosis
Metabolic Acidosis
● Caused by bicarbonate deficiency
● Production of increased amount of acid –
diabetic ketoacidosis, lactic acidosis PARAMETERS OF INTEREST
(alcoholism), renal failure and diarrhea Evaluate (normal pH - 7.35-7.45)
● Compensation: Hyperventilation ● <7.35 - acidosis
● (+) Hyperkalemia and hyperchloremia ● >7.45 – alkalosis
*In DKA→normochloremic Evaluate the ventilation (Lungs)
Metabolic Alkalosis ● pC02 - 35 - 45 mm Hg
● Caused by bicarbonate excess ● < 35 respiratory alkalosis
● Conditions: Vomiting with the loss of ● > 45 respiratory acidosis
chloride from the stomach Evaluate the metabolic Process (kidneys)
● Compensation: Hypoventilation ● HC03 = 22-26 meq/L
● For every 10 meq/L rise in bicarbonates, the ● < 22 - metabolic acidosis
pCO2 rises by 6 mmHg ● >26 – metabolic alkalosis
● (+) hypokalemia, hypochloremia
● pCO2 drops 1-1.3 mmHg per mEq/L fall in ● Determine which is the Primary (1°) and
HCO3- compensating disorder
Respiratory Acidosis - pH
● Excessive CO2 accumulation ● Determine the degree of compensation
● Conditions: Chronic obstructive pulmonic - non- compensatory
disease (COPD), myasthenia gravis, CNS - partial compensatory
disease, drug overdose (morphine, - complete compensation
barbiturates and opiates), pneumonia ● pO2 = 81 - 100 mmHg (adequate
● Compensation: retention of bicarbonates oxygenation)
● Bicarbonate rises 1 meq/L for each 10 ● p02 Hypoxemia:
mmHg rise in pCO2 - mild = 61 - 80
Respiratory Alkalosis - moderate = 41 - 60
● Due to excessive carbon dioxide loss - severe = 40 or less
● Conditions: Anxiety, severe pain, aspirin
overdose, hepatic cirrhosis
● Compensation: decreased reabsorption
● Bicarbonate falls 2 meq/L for each 10
mmHg fall in pCO2
● (+) Hypokalemia
You might also like
- Doctors NoteDocument3 pagesDoctors Notenanaikunga100% (1)
- Activity 2 Case Study of PneumoniaDocument13 pagesActivity 2 Case Study of PneumoniaEdelweiss Marie Cayetano100% (1)
- Review Article: Sodium Bicarbonate Therapy in Patients With Metabolic AcidosisDocument14 pagesReview Article: Sodium Bicarbonate Therapy in Patients With Metabolic AcidosisMuhammad Arif Nur SyahidNo ratings yet
- Sodium Bicarbonate Therapy in Patients With Metabolic AcidosisDocument13 pagesSodium Bicarbonate Therapy in Patients With Metabolic AcidosisSeptiandry Ade Putra100% (2)
- Acid Base Disorder Practice Problems Notes by Giuls 30Document6 pagesAcid Base Disorder Practice Problems Notes by Giuls 30marcoNo ratings yet
- Draft ACID BASEDocument5 pagesDraft ACID BASEkimmynemil80No ratings yet
- Arterial Blood GasDocument33 pagesArterial Blood GaskartikaparamitaNo ratings yet
- Transport of Carbon DioxideDocument9 pagesTransport of Carbon DioxideBarkat ShazliNo ratings yet
- Gas Analyser: How It Works A Presentation With A Hint of Spanish Accent Andreu Roca Bajona - June 2020Document22 pagesGas Analyser: How It Works A Presentation With A Hint of Spanish Accent Andreu Roca Bajona - June 2020Sihome ThodireNo ratings yet
- Blood Gas AnalysisDocument5 pagesBlood Gas Analysissraji64No ratings yet
- 3.5 Blood Gas Analysis RevDocument28 pages3.5 Blood Gas Analysis RevDaniel HikaNo ratings yet
- UNIT: PH and Blood GasesDocument14 pagesUNIT: PH and Blood Gasesbiddyusmc100% (2)
- Acid BaseDocument37 pagesAcid Basechngwq93100% (1)
- Blood GasesDocument51 pagesBlood Gasesrbm121415chyNo ratings yet
- Acid-Base BalanceDocument7 pagesAcid-Base BalanceMichelle Mae JulianaNo ratings yet
- Blood Gas Analysis: Respiratory DisordersDocument15 pagesBlood Gas Analysis: Respiratory DisordersYogeshRavalNo ratings yet
- Abg SakshiDocument59 pagesAbg SakshiSakshi GuptaNo ratings yet
- ABG Lab TestingDocument22 pagesABG Lab TestingRhenjay Ferrer LagoyNo ratings yet
- Acid Base and Electrolyte BalanceDocument6 pagesAcid Base and Electrolyte BalanceMuhammad Hamza AlviNo ratings yet
- Acid-Base Balance, Dr. MiaDocument45 pagesAcid-Base Balance, Dr. MiaeuiskurNo ratings yet
- Blood Gas AnalyzerDocument25 pagesBlood Gas AnalyzerYashod WelgamaNo ratings yet
- Respiratory Monitoring BackupDocument51 pagesRespiratory Monitoring BackupmohammedNo ratings yet
- Arterial Blood Gases: Laboratory InsightsDocument9 pagesArterial Blood Gases: Laboratory InsightsYusuf NugrohoNo ratings yet
- Acid-Base Balance & Blood GasesDocument39 pagesAcid-Base Balance & Blood GasesSulaiman TahsinNo ratings yet
- Arterial Blood Gas Analysis: DR - Rakesh Chandra Chaurasia PGT 3 Ims, Bhu Moderator: DR - Manjaree Mishra Asset - ProfDocument64 pagesArterial Blood Gas Analysis: DR - Rakesh Chandra Chaurasia PGT 3 Ims, Bhu Moderator: DR - Manjaree Mishra Asset - ProfArmaanjeet SinghNo ratings yet
- 3.5 Blood Gas AnalysisDocument26 pages3.5 Blood Gas AnalysisSelemon MulatuNo ratings yet
- Blood Gases and Acid-Base BalanceDocument11 pagesBlood Gases and Acid-Base BalanceREMAN ALINGASANo ratings yet
- Acid Base BalanceDocument79 pagesAcid Base Balancecaballerodarlene83No ratings yet
- Acid Base BalanceDocument76 pagesAcid Base BalanceSobha MatthewNo ratings yet
- Blue Doodle Project PresentationDocument21 pagesBlue Doodle Project PresentationJaya KerupaaNo ratings yet
- Transportasi Gas RespirasiDocument48 pagesTransportasi Gas RespirasiAdriyan SikumalayNo ratings yet
- Arterial Blood Gas - ppt1Document53 pagesArterial Blood Gas - ppt1Madhuri100% (2)
- abg-151118185050-lva1-app6891Document52 pagesabg-151118185050-lva1-app6891RAMJIBAN YADAVNo ratings yet
- Lect-13-Chemical BiosensorsDocument37 pagesLect-13-Chemical BiosensorsmeharNo ratings yet
- Arterial Blood GasesDocument10 pagesArterial Blood GasesSoumya BhattacharyaNo ratings yet
- ABG Lecture PDFDocument11 pagesABG Lecture PDFbianca maaliwNo ratings yet
- Transportasi O2-CO2Document37 pagesTransportasi O2-CO2JoshuaRobertoPratamaNo ratings yet
- Acid Base BalanceDocument18 pagesAcid Base BalanceRichard PoonNo ratings yet
- Arterial Blood Gas: AnalysisDocument51 pagesArterial Blood Gas: Analysisnaven100% (2)
- Blood Gases, PH and Buffer SystemsDocument108 pagesBlood Gases, PH and Buffer SystemssilcmtgNo ratings yet
- Acidosis Alkalosis BiochemistryDocument31 pagesAcidosis Alkalosis BiochemistryliyaNo ratings yet
- ABG Analysis - Acid-Base BalanceDocument7 pagesABG Analysis - Acid-Base BalanceItharshan IndreswaranNo ratings yet
- Arterial Blood Gas.Document4 pagesArterial Blood Gas.Sathish KumarNo ratings yet
- Blood Gas AnalysisDocument52 pagesBlood Gas AnalysisKresna Dharma SuryanaNo ratings yet
- Arterial Blood GasDocument6 pagesArterial Blood GasnsfanfoinNo ratings yet
- CC Lec 7 Blood GasesDocument10 pagesCC Lec 7 Blood GasesJunea SeeNo ratings yet
- Blood Gases: Finals Day 1 PrfbremnerDocument27 pagesBlood Gases: Finals Day 1 PrfbremnerFrances FranciscoNo ratings yet
- Abg InterpretationDocument52 pagesAbg InterpretationCirugia Cardiovascular NeivaNo ratings yet
- ABGS Arterial Blood GasesDocument27 pagesABGS Arterial Blood GasesMuhammad asif samiNo ratings yet
- abg-interpretationDocument52 pagesabg-interpretationRAMJIBAN YADAVNo ratings yet
- Arterial Blood GAS InterpretationDocument25 pagesArterial Blood GAS Interpretationliyahanna02No ratings yet
- Arterial Blood Gas Analysis - Hand OutsDocument3 pagesArterial Blood Gas Analysis - Hand OutsRANo ratings yet
- Review: A of Blood PH and Blood-Gas AnalysisDocument16 pagesReview: A of Blood PH and Blood-Gas AnalysisAndreas C'ahaan ZaoldyeckNo ratings yet
- Arterial Blood Gas and PHDocument58 pagesArterial Blood Gas and PHlexthom balayantoNo ratings yet
- Mtap421 BloodgasesDocument11 pagesMtap421 BloodgasesNhelomar ManlinconNo ratings yet
- Arterial Blood Gas (Abg) Analysis: Submitted ToDocument5 pagesArterial Blood Gas (Abg) Analysis: Submitted ToRumela ChakrabortyNo ratings yet
- Acid Base BalaneceDocument11 pagesAcid Base BalaneceHAMMYER ALROKHAMINo ratings yet
- An Introduction To Acid-Base BalanceDocument39 pagesAn Introduction To Acid-Base BalanceFloydRushNo ratings yet
- Abg PalicDocument82 pagesAbg PalicHarry James PotterNo ratings yet
- Fisio 2Document6 pagesFisio 2anaNo ratings yet
- L04a BldgasDocument43 pagesL04a Bldgasyoyowong512No ratings yet
- Trace ElementsDocument5 pagesTrace ElementsFaithNo ratings yet
- Legal Aspects of Drug TestingDocument3 pagesLegal Aspects of Drug TestingFaith100% (1)
- Drug Test Specimen Collection and AccessioningDocument4 pagesDrug Test Specimen Collection and AccessioningFaithNo ratings yet
- Tumor MarkersDocument5 pagesTumor MarkersFaithNo ratings yet
- Non Spore Forming, Nonbranching Catalase Positive BacilliDocument5 pagesNon Spore Forming, Nonbranching Catalase Positive BacilliFaithNo ratings yet
- EnterobacteriaceaeDocument12 pagesEnterobacteriaceaeFaithNo ratings yet
- Staphylococcus and MicrococcusDocument6 pagesStaphylococcus and MicrococcusFaithNo ratings yet
- NonfermentersDocument3 pagesNonfermentersFaithNo ratings yet
- Miscellaneous BacteriaDocument5 pagesMiscellaneous BacteriaFaithNo ratings yet
- Tubular ReabsorptionDocument24 pagesTubular ReabsorptionAnonymous t5TDwdNo ratings yet
- ElectrocardiogramDocument4 pagesElectrocardiogramazeeroNo ratings yet
- Approach To PolytraumaDocument46 pagesApproach To PolytraumaAyush ChaliseNo ratings yet
- Comparison of Stethoscope Bell and Diaphragm, And.9Document6 pagesComparison of Stethoscope Bell and Diaphragm, And.9kunichiwa chaNo ratings yet
- Ie Format OlfuDocument8 pagesIe Format OlfuJonathan ZapantaNo ratings yet
- Kunjungan Pasien 2Document25 pagesKunjungan Pasien 2LelyNo ratings yet
- Plant Growth QuizDocument5 pagesPlant Growth QuizEsther Suan-LancitaNo ratings yet
- Histology of Heart and Vessels - ANAT3888 - 2023Document41 pagesHistology of Heart and Vessels - ANAT3888 - 2023RachaelNo ratings yet
- Kyphoscoliosis 2018 ARCDocument36 pagesKyphoscoliosis 2018 ARCLOK rNo ratings yet
- Anaesthesia in Obese PatientsDocument72 pagesAnaesthesia in Obese PatientsPraveen RamasamyNo ratings yet
- Slid CH13Document93 pagesSlid CH13Senior TitopecNo ratings yet
- The Lymphatic System and Body DefensesDocument74 pagesThe Lymphatic System and Body DefensesWyncess Joy Unza CamiloNo ratings yet
- Interpretting ABG SuccessfullyDocument15 pagesInterpretting ABG Successfullyanimathz100% (1)
- The Cardiac System LOBDocument3 pagesThe Cardiac System LOBbdhhuhddNo ratings yet
- Concept MapDocument4 pagesConcept MapDud AccNo ratings yet
- Lectire-Hypoxia 2020Document21 pagesLectire-Hypoxia 2020Bol Dhalbeny Malual100% (1)
- Sleep of College StudentsDocument24 pagesSleep of College StudentsPrachi PathakNo ratings yet
- Basic Prov Itls Study Guide 7thedDocument12 pagesBasic Prov Itls Study Guide 7thedDave Amarasinghe0% (1)
- Procedural Sedation and AnalgesiaDocument30 pagesProcedural Sedation and AnalgesiashoibyNo ratings yet
- Metabolisme Calsium Dan Hormon PTHDocument71 pagesMetabolisme Calsium Dan Hormon PTHzeddNo ratings yet
- Daftar Pustaka-Wps OfficeDocument2 pagesDaftar Pustaka-Wps OfficeRezha July prakosoNo ratings yet
- Nursing Care Plans For Cruris Fracture: Case 1Document9 pagesNursing Care Plans For Cruris Fracture: Case 1susanti santaliaNo ratings yet
- Curriculum Development For Integrated Teaching (Module) - MBBS Phase I StudentsDocument8 pagesCurriculum Development For Integrated Teaching (Module) - MBBS Phase I StudentsjuvemaNo ratings yet
- SGBAU B.Pharm 1 SEM Human-Anatomy-n-Physiology-I 2018Document2 pagesSGBAU B.Pharm 1 SEM Human-Anatomy-n-Physiology-I 2018Abhay DeulkarNo ratings yet
- Basic Life Support: Dr. Aatir Fayyaz Nishtar Medical University MultanDocument42 pagesBasic Life Support: Dr. Aatir Fayyaz Nishtar Medical University MultanShahzeb KhanNo ratings yet
- Chapter 10Document16 pagesChapter 10nfnf otupyooorefnNo ratings yet
- Week 8: Stages of Labor and Delivery, Danger Signs of LaborDocument7 pagesWeek 8: Stages of Labor and Delivery, Danger Signs of LaborABEGAIL BALLORANNo ratings yet
- Genetic Biomarkers For The Risk of Seizures in Long QT SyndromeDocument9 pagesGenetic Biomarkers For The Risk of Seizures in Long QT SyndromeР. МөнхжинNo ratings yet